Fetal Wellbeing and Antenatal Monitoring And CTG PRESENTED
Fetal Wellbeing and Antenatal Monitoring And CTG PRESENTED BY: DR HARIPADA DAS 2 ND YEAR PGT DEPARTMENT OF OBST. & GYNAE RKMSP, KOLKATA MODERATED BY: PROF(DR) SAJAL DATTA PROFESSOR, RKMSP
Antenatal Monitoring Why? Who? How?
WHY ? • Two thirds of fetal deaths occur before the onset of labor. • Many antepartum deaths occur in women at risk for uteroplacental insufficiency. • Ideal test: allows intervention before fetal death or damage from asphyxia. • Preferable: treat disease process and allow fetus to go to term.
Antenatal monitoring • Uteroplacental insufficiency • Inadequate delivery of nutritive or respiratory substances to appropriate fetal tissues. • Inadequate exchange within the placenta due to decreased blood flow, decreased surface area or increased membrane thickness. • Inadequate maternal delivery of nutrients or oxygen to the placenta or to problems of inadequate fetal uptake.
Antenatal monitoring • Theoretical scheme of fetal deterioration • Fetal well being • Fetal growth retardation (Marginal placental respiratory function) • Fetal hypoxia with stress (Decreasing respiratory function) • Some residual effects of intermittent hypoxia (profound respiratory compromise) • Asphyxia • Death
Who? • Conditions placing the fetus at risk for UPI • Preeclampsia, chronic hypertension, • Collagen vascular disease, diabetes mellitus, renal disease, • Fetal or maternal anemia, blood group sensitization, • Hyperthyroidism, thrombophilia, cyanotic heart disease, • Postdate pregnancy, • Fetal growth restriction
How? • Methods for antepartum fetal assessment • • • Fetal movement counting Assessment of uterine growth Antepartum fetal heart rate testing Biophysical profile Doppler velocimetry
Fetal movement counting • Maternal perception of a decrease in fetal movements / change in the pattern of fetal movements may be a sign of impending fetal compromise. • Cardiff “count to ten” : 10 movements in 12 hours. • Kick charts • No robust evidence. •
Reduced fetal movements • First episode: monitoring by CTG • Persistent: USg for growth, umbilical artery Doppler(UAD), CTG 2 to 3 times per week • Absent : • No FH: confirm by USG • FH present: growth scan and UAD
Tests for RFM • Cochrane data for CTG • • Increased hospitalisation, additional tests & elective delivery No benefit in outcome Interpretation errors False reassurance • UAD has been shown to be predictive of perinatal compromise in high risk pregnancies mainly FGR
Symphysiofundal height • General rule: fundal height in centimeters will equal the weeks of gestation. • Exceptions: maternal obesity, multiple gestation, polyhydramnios, abnormal fetal lie, oligohydramnios, low fetal station, and fetal growth restriction. • Customized chart : Abnormalities of fundal height should lead to further investigation. • Accuracy: poor?
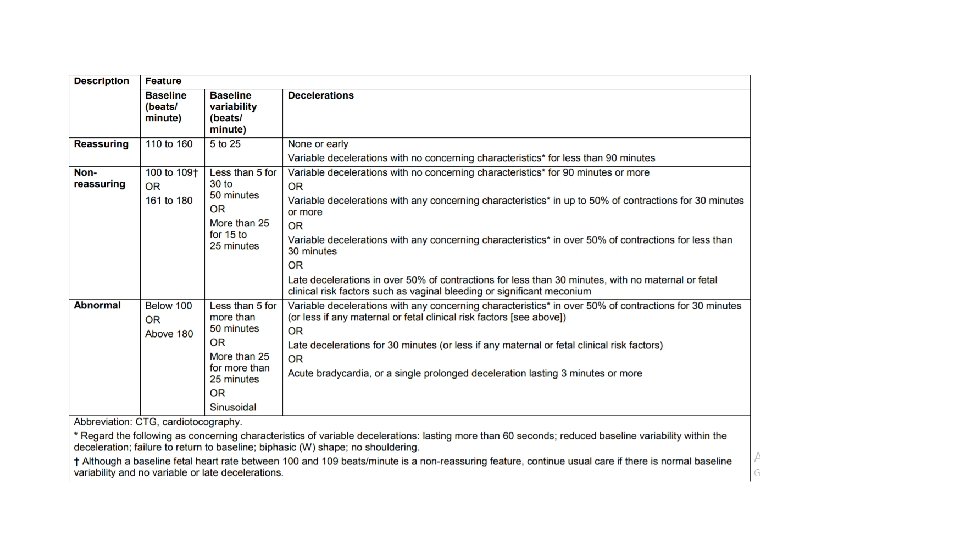
NONSTRESS TESTS AND CTG Describe fetal heart rate acceleration in response to fetal movement as a sign of fetal health. Most widely used primary testing method for assessment of fetal well-being. Incorporated into the biophysical profile testing system Reactivity Indicates normal autonomic function and CNS alertness and activity>>>>> Absent depicts CNS depression due to hypoxia , drugs, fetal sleep, or congenital anomaly Ideally done after 32 weeks Indications: All high risk pregnancies Decrease or loss of FM Post datism Less fetal kick count Unexplained fetal loss in previous pregnancy • Variables : Baseline heart rate ( normal 110 -160 bpm) Variability (5 -25 bpm) Presence or absence of acceleration Presence or absence of decelerations • • •
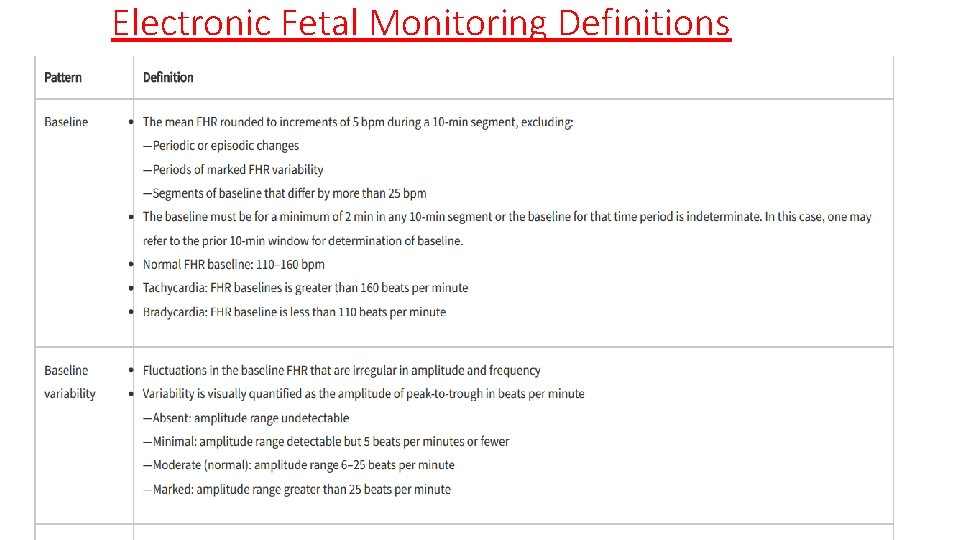
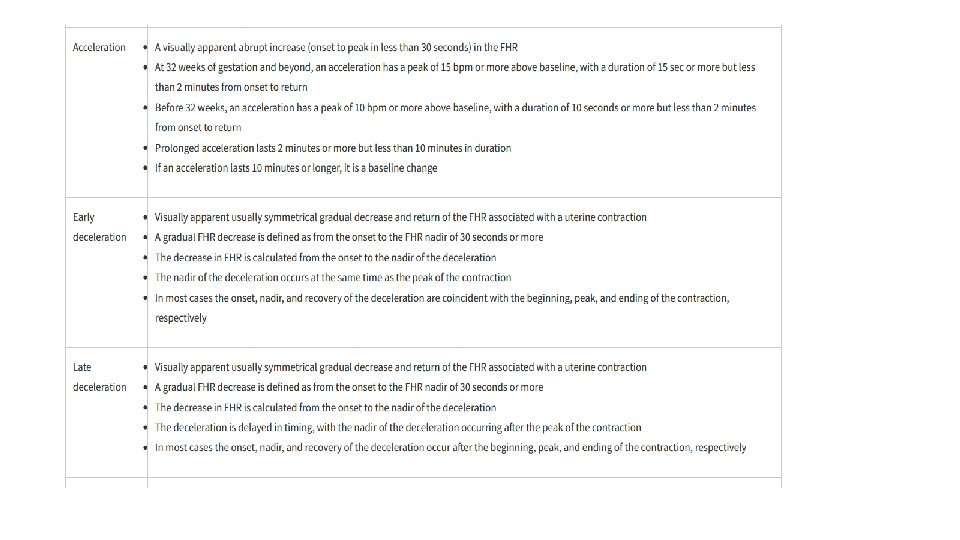
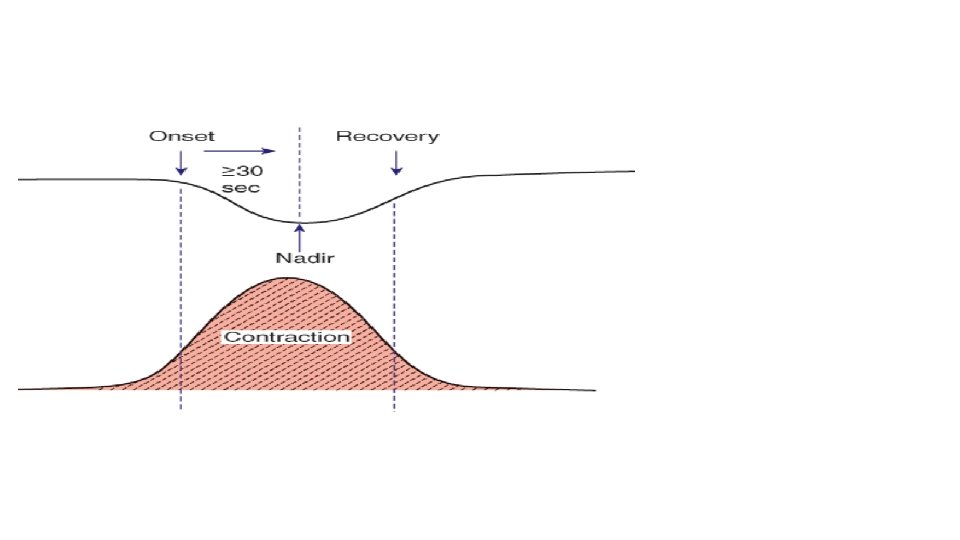
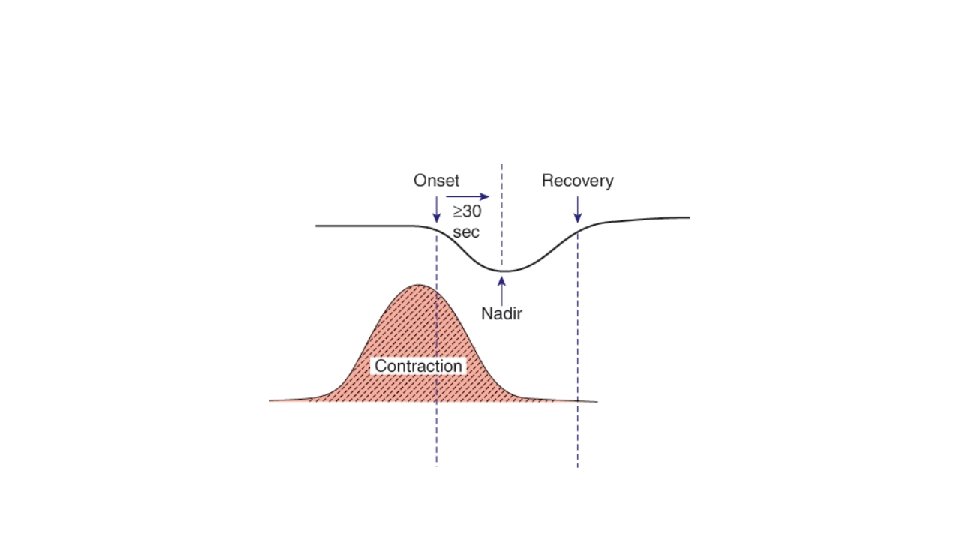
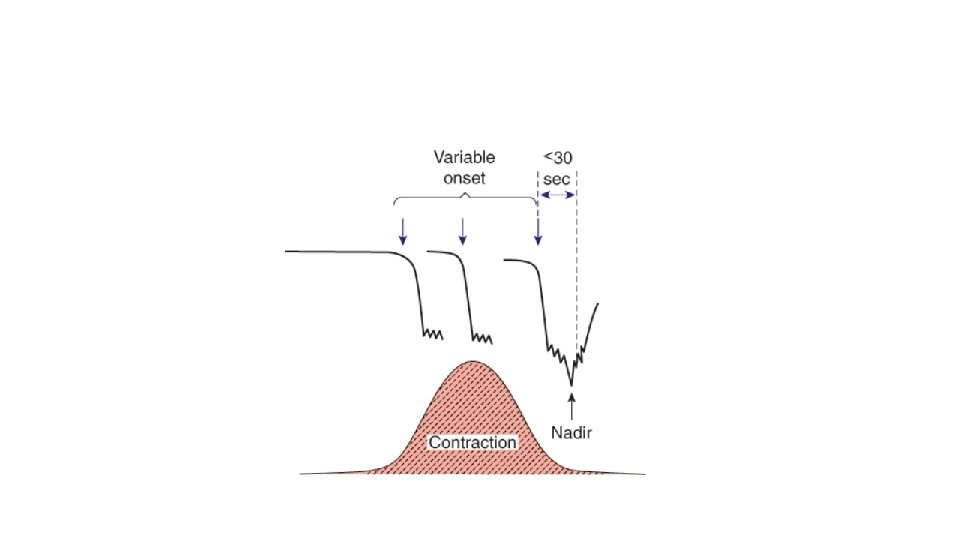
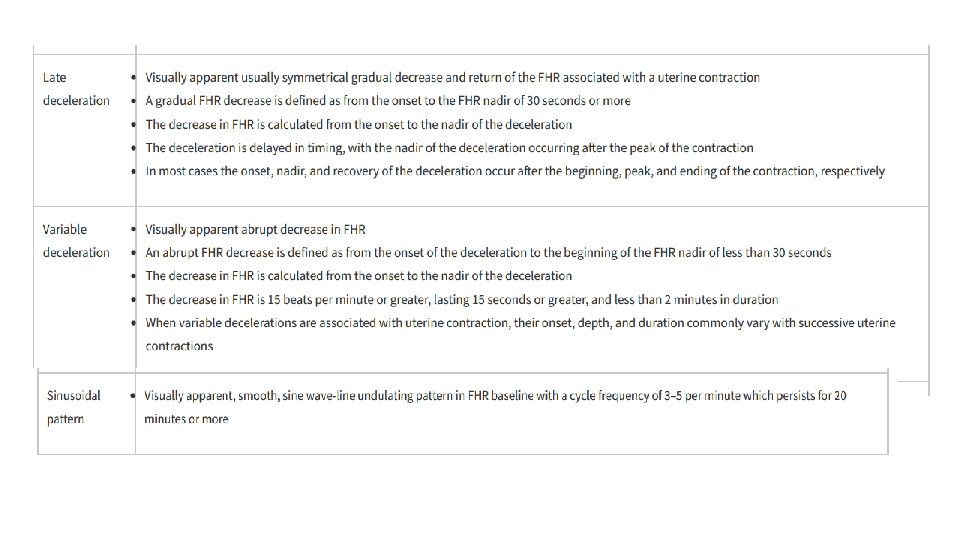
Electronic Fetal Monitoring Definitions
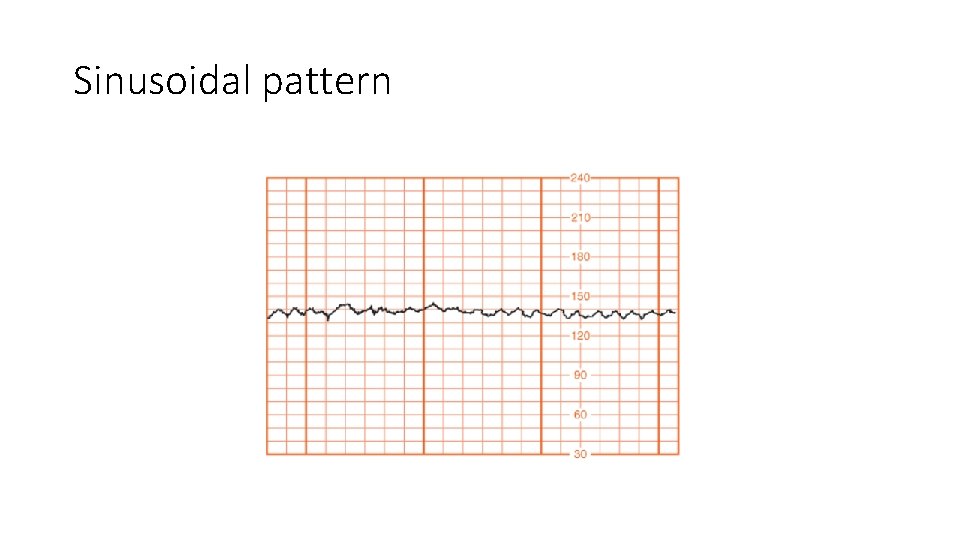
Sinusoidal pattern
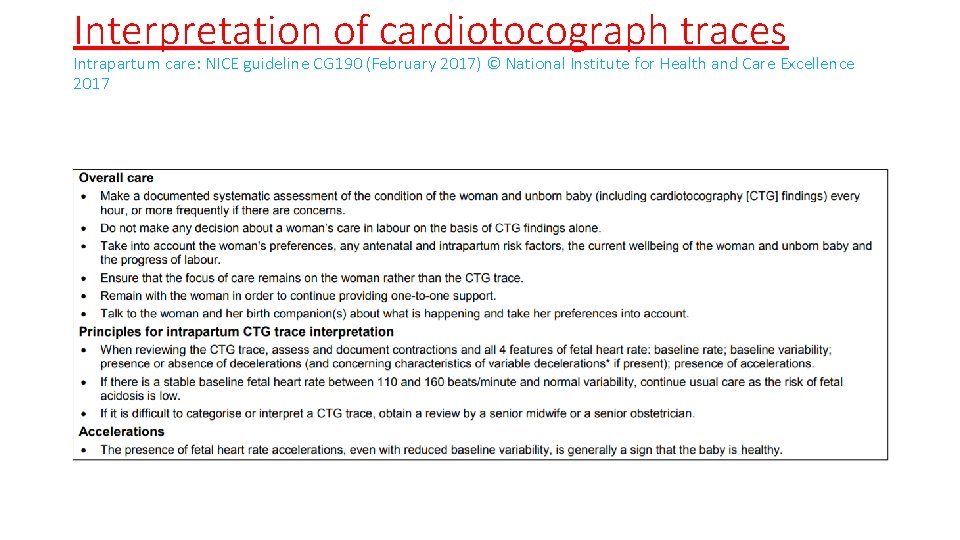
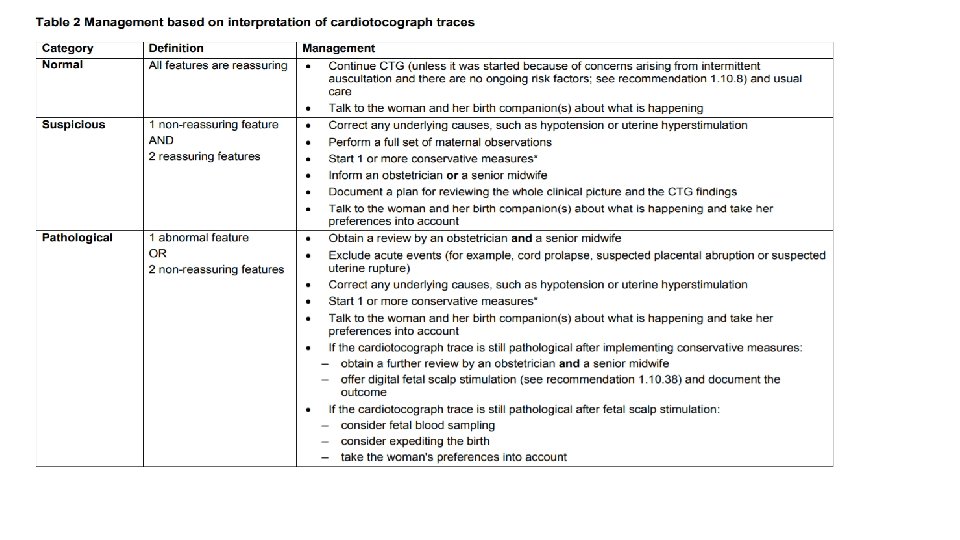
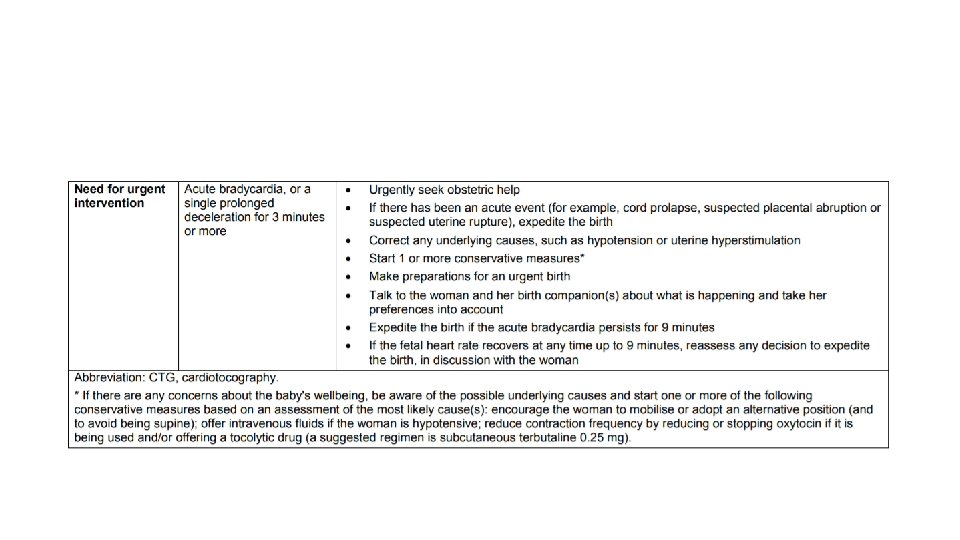
Interpretation of cardiotocograph traces Intrapartum care: NICE guideline CG 190 (February 2017) © National Institute for Health and Care Excellence 2017
CTG monitor • Cochrane: • Antenatal CTG has no significant effect on perinatal outcome or interventions such as early elective delivery • NICE: • Evidence does not support the routine use of antenatal electronic fetal heart rate monitoring for fetal assessment in women with an uncomplicated pregnancy and therefore it should not be offered routinely •
Antenatal CTG • Perinatal mortality: 6. 2/1000 • False positive rate: 50% • False negative rate: 3. 2 / 1000
Fetal Acoustic Stimulation Test(FAST) & Vibro Acoustic Stimulation Test(VAST) • Done by an artificial larynx, 80 -100 db for 2 -3 seconds • Healthy fetus responds by startle response followed by acceleration of fetal heart rate • Reduces the testing time and false positive by 2% • Disadvantage: low resource and costly
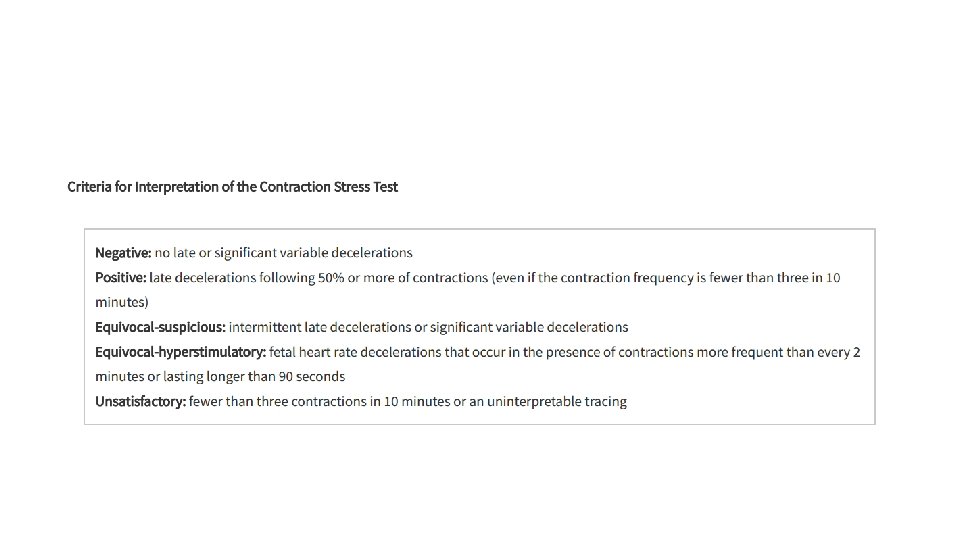
CONTRACTION STRESS TESTING • Based on the response of fetal heart rate to uterine contractions • If fetus is with suboptimal oxygenation uterine contractions will cause fetal heart rate deceleration • Methods: oxytocin challenge test Nipple stimulation test • Indications: Non-reactive NST • CONTRAINDICATIONS: Preterm laour or impending preterm labour PPROM H/O extensive uterine surgery or classic cs • Placenta previa, multiple gestation, vasa previa, cervical incompetency Risks: Unexpected iud(RARELY DONE)
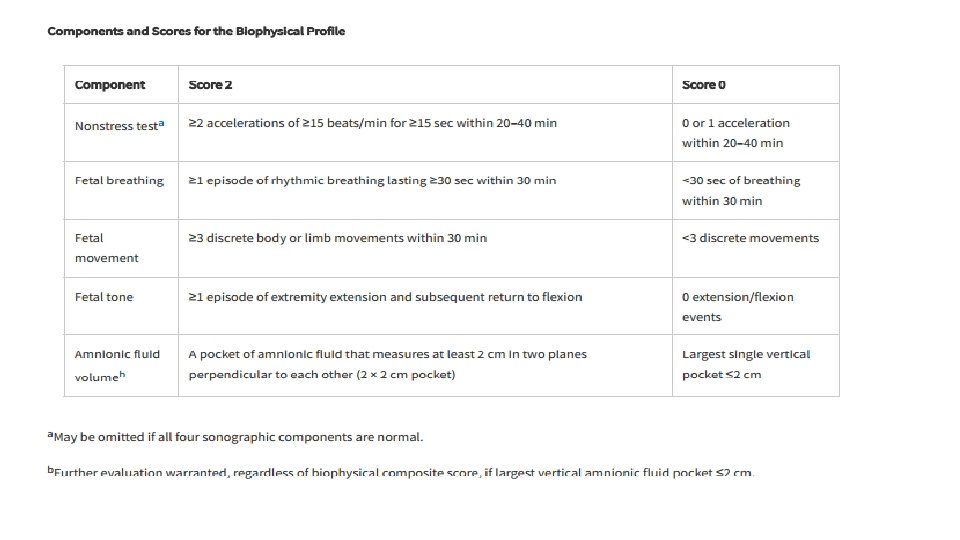
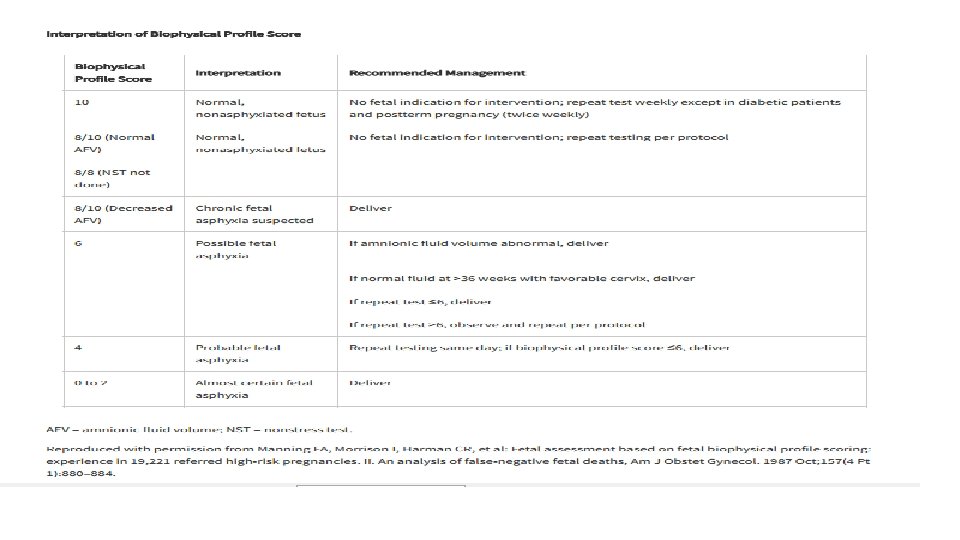
BIOPHYSICAL PROFILE v. Proposed by Manning and colleagues (1980) v. More accurate means of assessing fetal health than a single element. vrequire 30 to 60 minutes vmost common identifiable causes of fetal death in a normal biophysical profile include fetomaternal hemorrhage, umbilical cord accidents, and placental abruption (Dayal, 1999). vcomponents assessed: (1) heart rate acceleration, (2) breathing, (3) movements, (4) tone, and (5) amnionic fluid volume.
FETAL BREATHING • Paradoxical chest wall movement - In the newborn or adult, the opposite occurs -might be coughing to clear amnionic fluid debris • appears to be essential for normal lung development • two types: 1. gasps or sighs : frequency of 1 to 4 per minute. 2. Irregular bursts of breathing : up to 240 cycles per minute. associated with rapid eye movement. • might reflect fetal health • Affected by hypoxia, hypoglycemia, sound stimuli, cigarette smoking, amniocentesis, impending preterm labor, gestational age, the fetal heart rate itself, and labor—during which it is normal for respiration to cease. • It is episodic with diurnal variation • evaluation to diagnose absent respiratory motion may require long periods of observation. upto 122 min • fetal breathing has become a component of the biophysical profile.
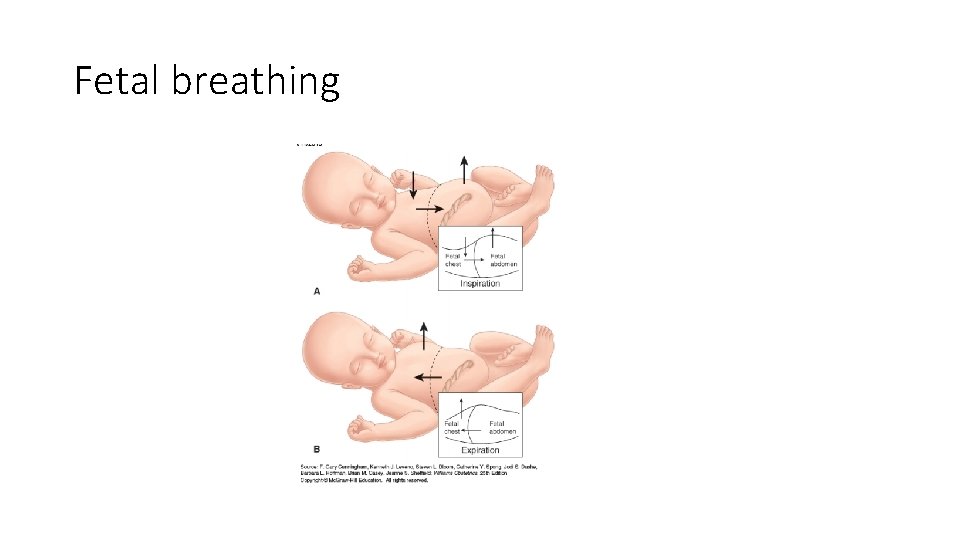
Fetal breathing
FETAL MOVEMENTS • Passive unstimulated fetal activity commences by 7 wks & becomes coordinated by 8 wks • Organised between 20 and 30 wks • Matured by 36 wks • Nijhuis and colleagues (1982) described four fetal behavioral states: State 1 F is a quiescent state—quiet sleep—with a narrow oscillatory bandwidth of the fetal heart rate. State 2 F includes frequent gross body movements, continuous eye movements, and wider oscillation of the fetal heart rate. This state is analogous to rapid eye movement (REM) or active sleep in the neonate. State 3 F includes continuous eye movements in the absence of body movements and no heart rate accelerations. The existence of this state is disputed (Pillai, 1990 a). State 4 F is one of vigorous body movement with continuous eye movements and heart rate accelerations. This state corresponds to the awake state in newborns. • Fetuses spend most of their time in states 1 F and 2 F and is associated with urine production and bladder volume
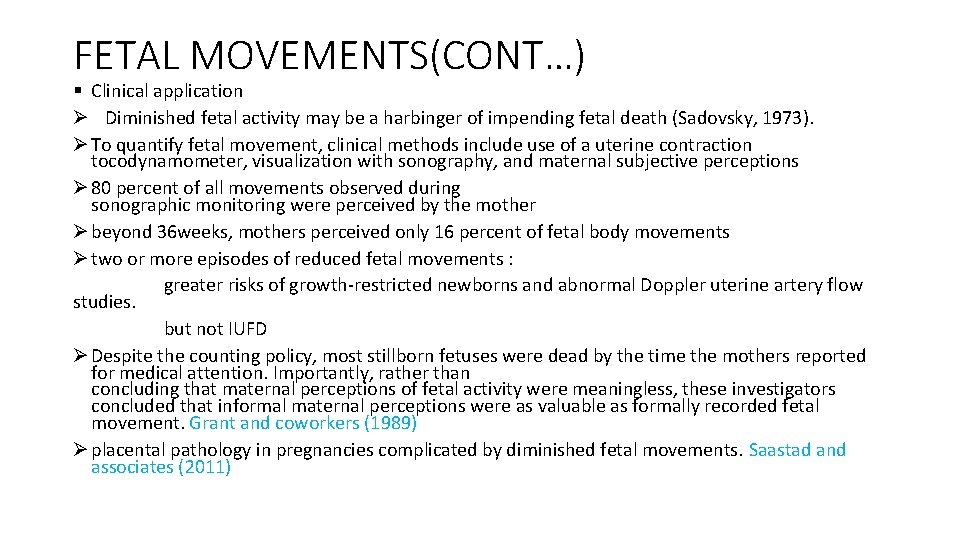
FETAL MOVEMENTS(CONT…) § Clinical application Ø Diminished fetal activity may be a harbinger of impending fetal death (Sadovsky, 1973). Ø To quantify fetal movement, clinical methods include use of a uterine contraction tocodynamometer, visualization with sonography, and maternal subjective perceptions Ø 80 percent of all movements observed during sonographic monitoring were perceived by the mother Ø beyond 36 weeks, mothers perceived only 16 percent of fetal body movements Ø two or more episodes of reduced fetal movements : greater risks of growth-restricted newborns and abnormal Doppler uterine artery flow studies. but not IUFD Ø Despite the counting policy, most stillborn fetuses were dead by the time the mothers reported for medical attention. Importantly, rather than concluding that maternal perceptions of fetal activity were meaningless, these investigators concluded that informal maternal perceptions were as valuable as formally recorded fetal movement. Grant and coworkers (1989) Ø placental pathology in pregnancies complicated by diminished fetal movements. Saastad and associates (2011)
DISADVANTAGE • Labour intensive test • Takes 30 -60 min • Requires usg trained person • Management based on score, clinical finding not incorporated
Modified Biophysical Profile • To avoid disadvantages of BPH Clark and co-authors(1989) developed modified BPH • COMBINES Non-stress test(NST) and Amniotic fluid index (AFI) • It takes only 10 min • Indicates long term placental function • Interpretation : normal: NST-reactive AFI>5 cm abnormal: NST: nonreactive or AFI 5 cm or less
Ultrasound • Quick, non-invasive procedure, easy interpretation • Customised fetal growth charts (serial scans) • Liquor volume • Placental function • Doppler study • Abnormal results correlate with increased risk of stillbirth and neonatal morbidity in selected pregnancies
AMNIONIC FLUID VOLUME • It is included into virtually all schemes in which fetal health is assessed (Frøen, 2008). • diminished uteroplacental perfusion may lead to lower fetal renal blood flow, decreased urine production, and ultimately, oligohydramnios • the deepest vertical pocket measurement, as opposed to the AFI, to diagnose oligohydramnios is associated with a reduction in unnecessary interventions without an increase in adverse perinatal outcomes (Nabhan, 2008; Reddy, 2014, ACOG, 2016) •
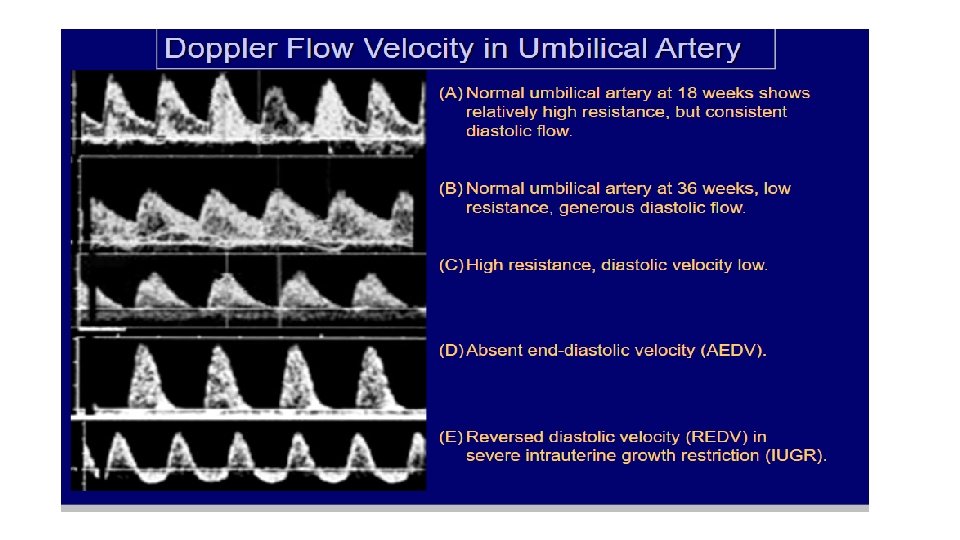
DOPPLER STUDIES OF VARIOUS VESSELS • Not beneficial for routine fetal surveillance • Important for IUGR • abnormal waveforms (60 to 70 percent need to be obliterated) correlated with placental villous hypovascularity. • Obliteration increases afterload and leads to fetal hypoxemia. • This in turn leads to ventricular dilation and redistribution of middle cerebral artery blood flow. Ultimately, pressure rises in the ductus venosus. • Clinically, abnormal Doppler waveforms in the ductus venosus are a late finding due to chronic hypoxemia. • cont…. .
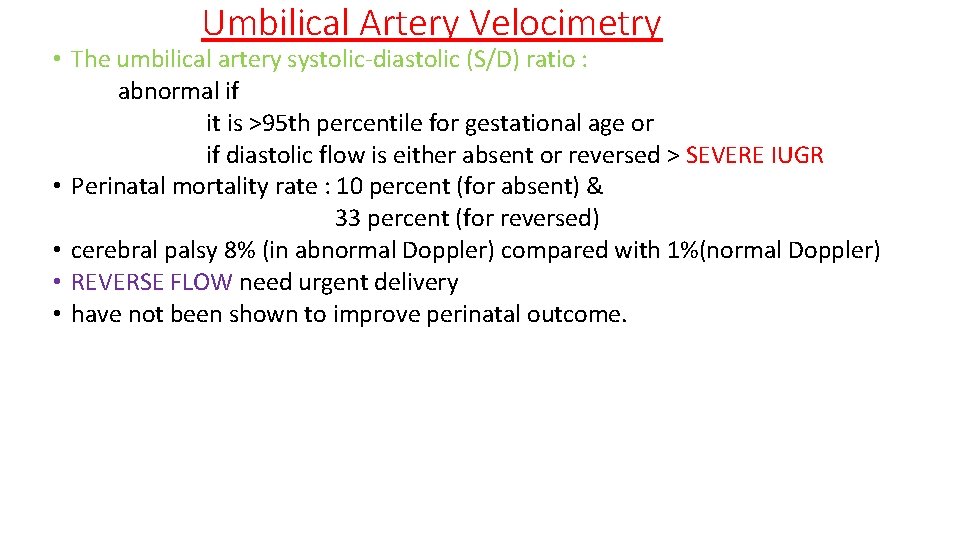
Umbilical Artery Velocimetry • The umbilical artery systolic-diastolic (S/D) ratio : abnormal if it is >95 th percentile for gestational age or if diastolic flow is either absent or reversed > SEVERE IUGR • Perinatal mortality rate : 10 percent (for absent) & 33 percent (for reversed) • cerebral palsy 8% (in abnormal Doppler) compared with 1%(normal Doppler) • REVERSE FLOW need urgent delivery • have not been shown to improve perinatal outcome.
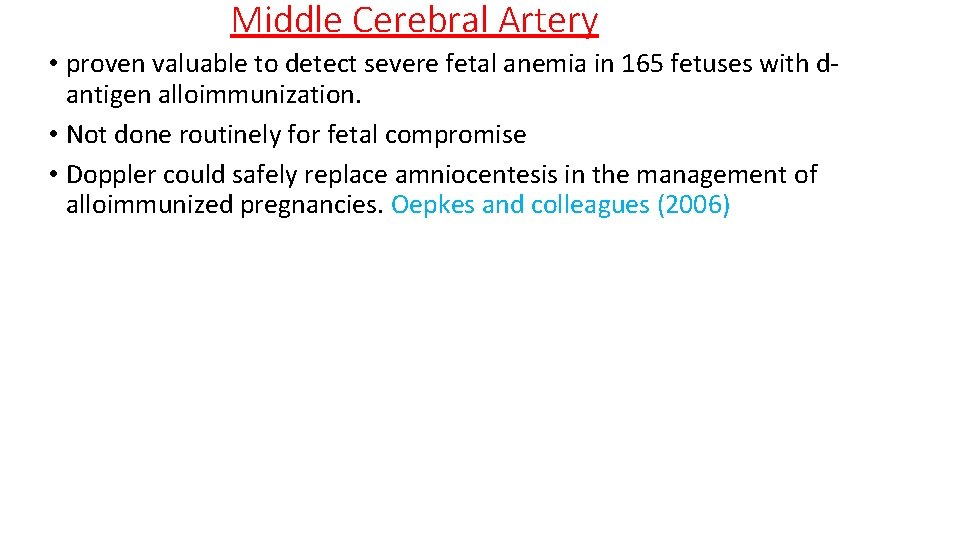
Middle Cerebral Artery • proven valuable to detect severe fetal anemia in 165 fetuses with dantigen alloimmunization. • Not done routinely for fetal compromise • Doppler could safely replace amniocentesis in the management of alloimmunized pregnancies. Oepkes and colleagues (2006)
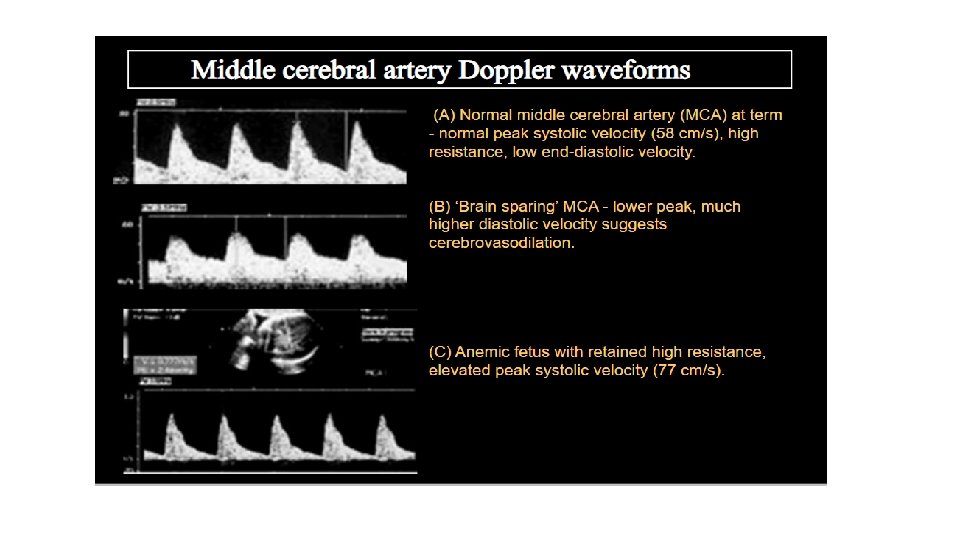
DUCTUS VENOSUS • Best predictor of perinatal outcome. • late finding because these fetuses had already sustained irreversible multiorgan damage due to hypoxemia. • Also, gestational age at delivery was a major determinant of perinatal outcome independent of ductus venosus flow. 36% to 5% in 26 -29 wks and 30 -33 wks • Specifically, absent or reversed flow in the ductus venosus was associated with profound generalized fetal metabolic collapse. • severely abnormal flow >>>>it is too late because the fetus is already near death. >>>>Not routinely recommended Uterine Artery Doppler Should not be considered standard practice in either low- or high-risk populations.
MISCELLANEOUS • FETAL SCALP TEST STIMULATION: Painful stimulus to scalp causes fetal heart rate acceleration • Fetal ECG:
Biochemical Methods • 1. FETAL BLOOD SAMPLING • Done to avoid unnecessary lscs due to abnormal EFM • Unfortunately in india it is not very famous • Indications : atypical or abnormal tracing on EFM Thick meconium stained liquor • Contraindications: If spontaneous VD is imminent or instrumental delivery is possible During or soon after an episodes of prolonged bradycardia when an ominous FHS trace necessitates immediate delivery In HIV positive woman Need early delivery a/w failure to pregress of labour
Interpretation of fetal p. H • >7. 25 ---No acidosis. But if CTG is still abnormal, repeat test after 1 hr • 7. 20 -7. 25 ----If not delivered repeat within 1 hr • <7. 20 ---acidosis, need urgent delivery Vacuum extractor should be avoided within 1 hr to prevent cephalohematoma
Cont…. • 2. Fetal Pulse Oxymetry • Measures fetal oxyhemoglobin • Sensor is placed in fetal cheek after ARM • Normal 40 -70% • <30%----abnormal
Cont… • 3. Fetal Blood Lactate • Indicator of anerobic respiration • value: Normal---<2. 8 mmol/L Suspicious---2. 9 -3. 08 mmol/L Abnormal--->3. 08 4. Near Infrared Spectroscopy
. Thank you
- Slides: 51