FETAL MONITORING ANTE AND INTRAPARTUM DR OSHINOWO M
- Slides: 41
FETAL MONITORING ANTE AND INTRAPARTUM DR. OSHINOWO M. B; B. S, FRCOG OBSTETRICIAN/GYNAECOLOGIST
INTRODUCTION • The aim of ANC – Ensure maternal well being – Ensure Fetal well being • Identifying risks factors • Monitoring of certain parameters ie Weight, BP, Urinalysis, Blood sugar (if necessary)
ANTEPARTUM • PHYSICAL • BIOCHEMICAL • ELECTRONIC
PHYSICAL FUNDAL HEIGHT – SMALL FOR DATE • OLIGOHYDRAMNIOS • IUGR • IUD – LARGE FOR DATE • MULTIPLE GESTATION • POLYHYDRAMNIOS • FIBROIDS
ULTRASONOGRAPHY • Comes in 2 D, 3 D and recently 4 D modes • Demonstrates features like Fetal anatomy, fetal weight, fetal movement, placental location, amniotic fluid volume • Helpful in specialized procedures like amniocentesis, Chorionic villus sampling, Biophysical profile, Fetal doppler, Fetal echocardiogram etc
GROWTH ULTRASOUND • Performed every 3 to 4 weeks • Fetus at risk of fetal growth restrictions secondary to medical conditions of pregnancy or fetal abnormalities
FETAL MOVEMENT ASSESSMENT • Normal: 10 movements/fetal kicks in 12 hours (Cardiff count to ten) • Decreased fetal movement may precede fetal death by days • Mothers should be encouraged to keep a FKC especially in high risks patients
NON STRESS TEST (NST) • Assesses fetal movements with FHR acceleration • Reactive/Reassuring NST: 2 or more FHR accelerations at least 15 bpm above the baseline lasting at least 15 secs in a 20 mins period • Non reassuring NST may suggest fetal acidosis – What to do depends on gestational age
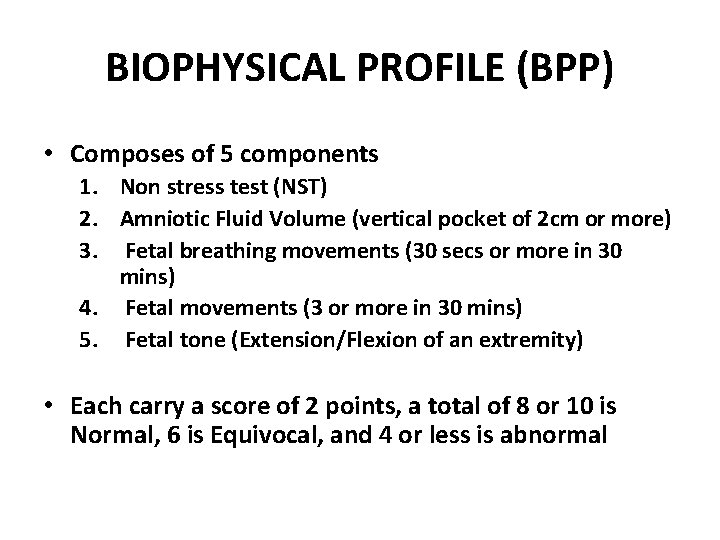
BIOPHYSICAL PROFILE (BPP) • Composes of 5 components 1. Non stress test (NST) 2. Amniotic Fluid Volume (vertical pocket of 2 cm or more) 3. Fetal breathing movements (30 secs or more in 30 mins) 4. Fetal movements (3 or more in 30 mins) 5. Fetal tone (Extension/Flexion of an extremity) • Each carry a score of 2 points, a total of 8 or 10 is Normal, 6 is Equivocal, and 4 or less is abnormal
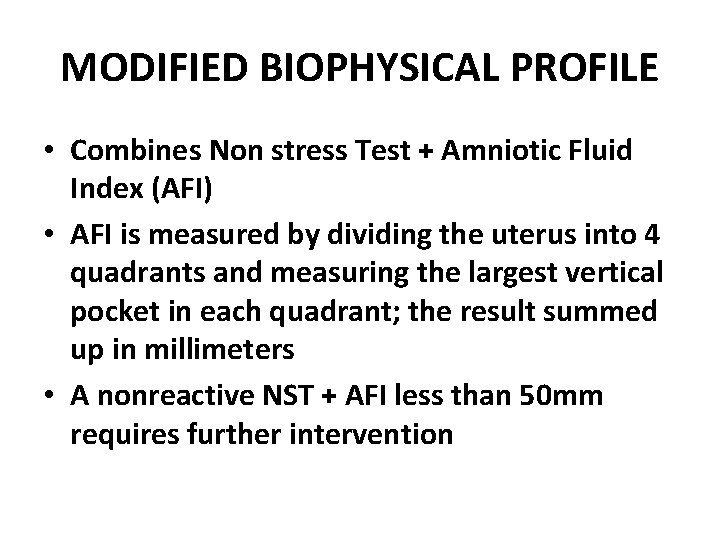
MODIFIED BIOPHYSICAL PROFILE • Combines Non stress Test + Amniotic Fluid Index (AFI) • AFI is measured by dividing the uterus into 4 quadrants and measuring the largest vertical pocket in each quadrant; the result summed up in millimeters • A nonreactive NST + AFI less than 50 mm requires further intervention
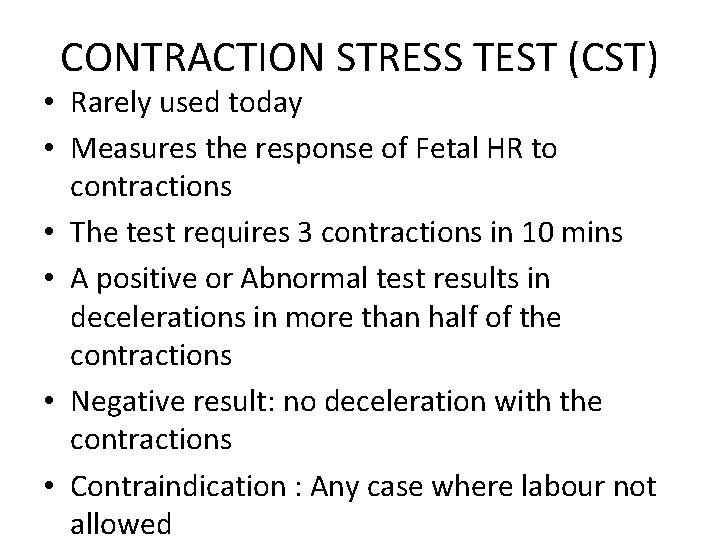
CONTRACTION STRESS TEST (CST) • Rarely used today • Measures the response of Fetal HR to contractions • The test requires 3 contractions in 10 mins • A positive or Abnormal test results in decelerations in more than half of the contractions • Negative result: no deceleration with the contractions • Contraindication : Any case where labour not allowed
DOPPLER STUDIES • Assesses multi-vessel evaluation of fetal status • Can be used to assess a compromised fetus i. e growth restriction • Functions as a diagnostic tool that alerts the clinician
INTRAPARTUM FETAL MONITORING
Baseline Fetal Heart Rate (FHR) – Is the mean level of the FHR when this is stable, excluding accelerations and decelerations – It is determined over a time period of 5 -10 minutes, expressed as beats per minute (bpm) NOTE: Preterm fetuses tend to have values towards the upper end of the normal range 14
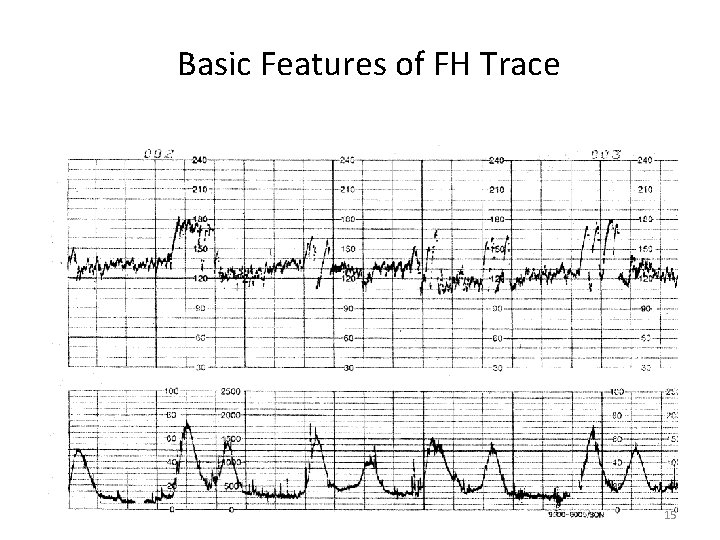
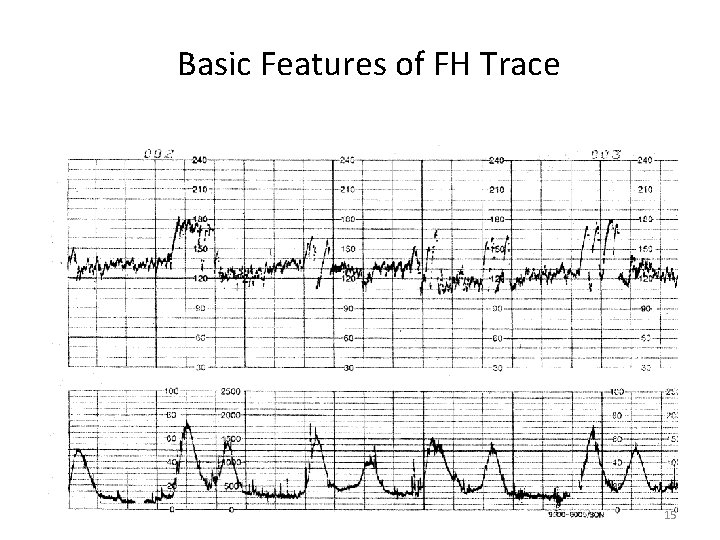
Basic Features of FH Trace 15
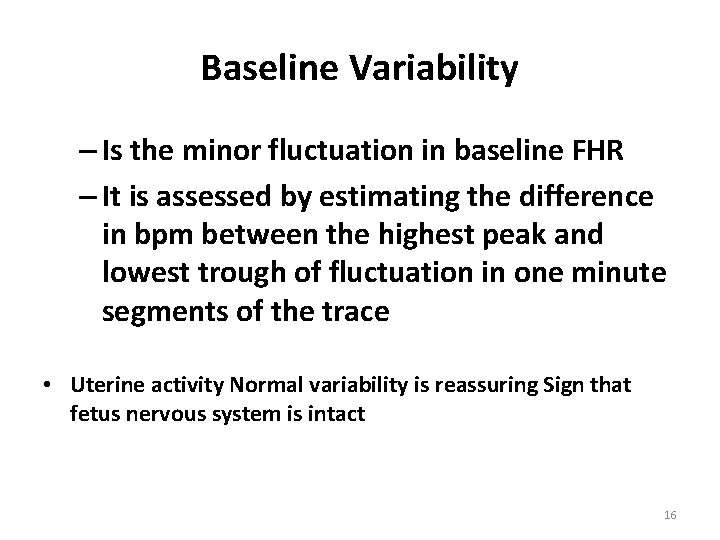
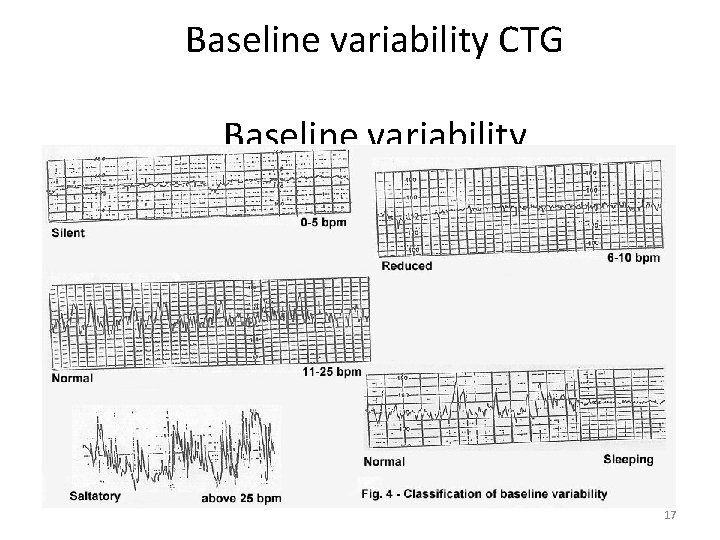
Baseline Variability – Is the minor fluctuation in baseline FHR – It is assessed by estimating the difference in bpm between the highest peak and lowest trough of fluctuation in one minute segments of the trace • Uterine activity Normal variability is reassuring Sign that fetus nervous system is intact 16
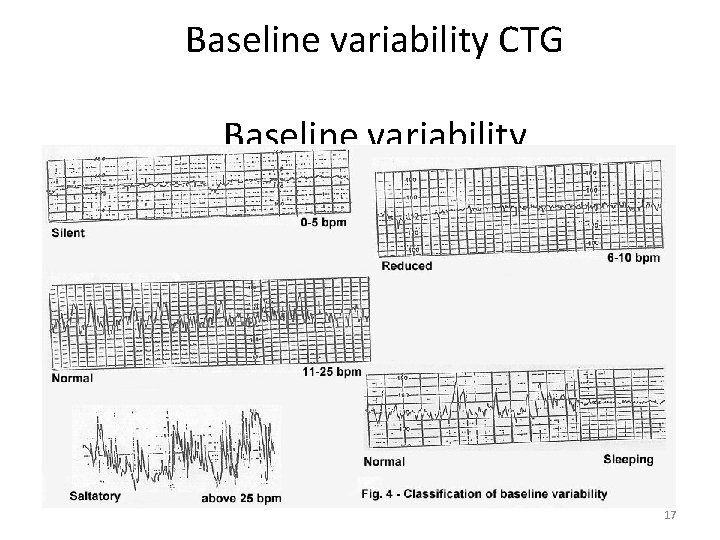
Baseline variability CTG Baseline variability 17
2 types of Variability Short- Term variability or Beat to Beat variability • Is the difference between successive heartbeats or the moment Long Term Variability • Is wider fluctuations • Over one (1) minute that causes wavy appearance in the monitor • Absent - No fluctuation Minimal - 5 bpm or less Moderate/Normal – 5 bpm to 25 18
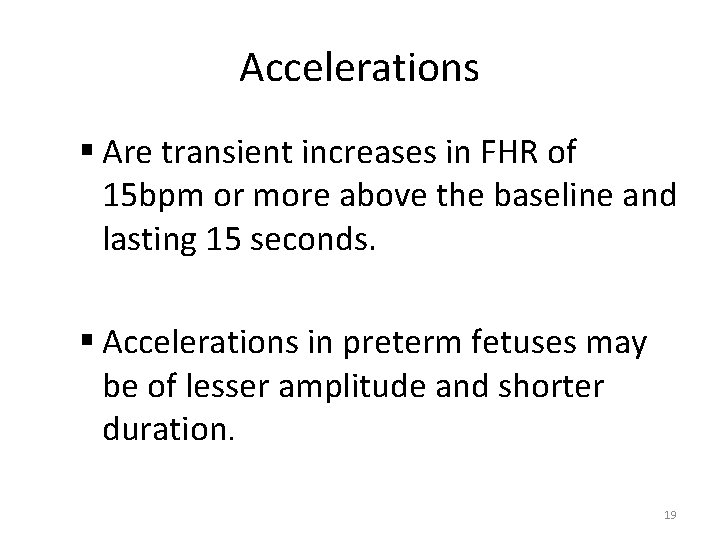
Accelerations § Are transient increases in FHR of 15 bpm or more above the baseline and lasting 15 seconds. § Accelerations in preterm fetuses may be of lesser amplitude and shorter duration. 19
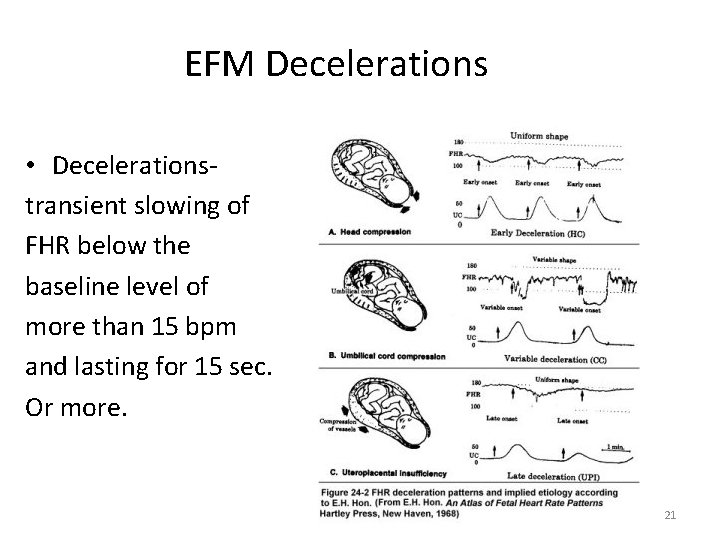
Decelerations § Are transient episodes of decrease of FHR below the baseline of more than 15 bpm lasting at least 15 seconds, which are: § Early, Variable and Delayed § Time relationships with contraction cycle may be variable but most commonly occur simultaneously with contractions. 20
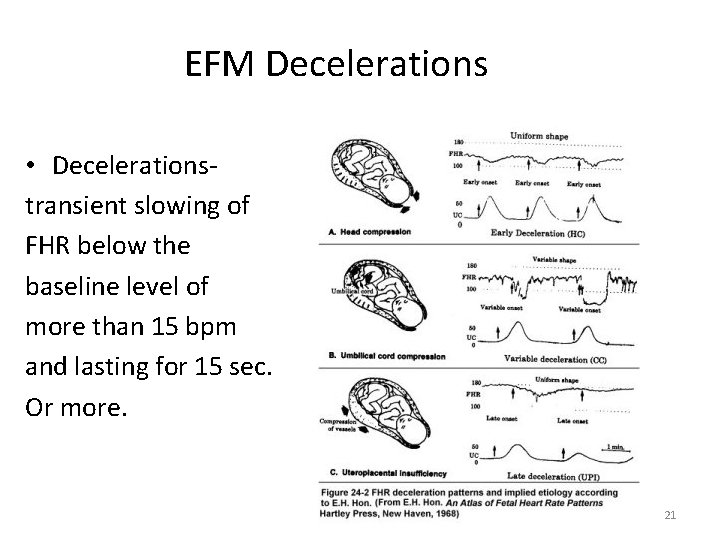
EFM Decelerations • Decelerationstransient slowing of FHR below the baseline level of more than 15 bpm and lasting for 15 sec. Or more. 21
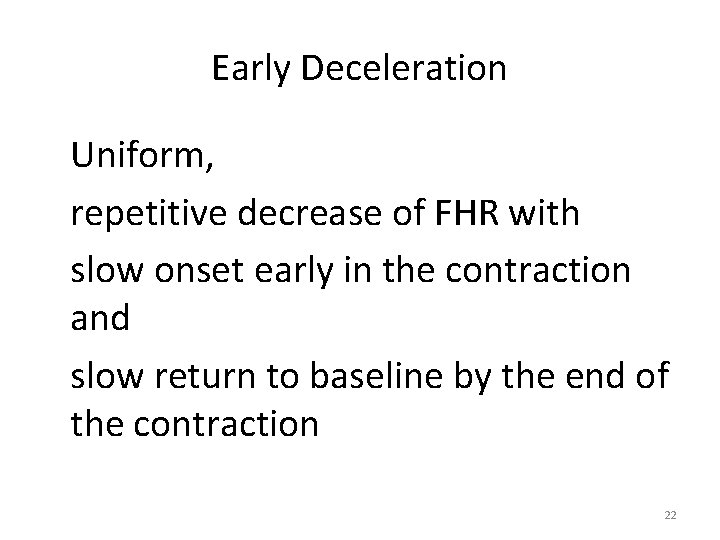
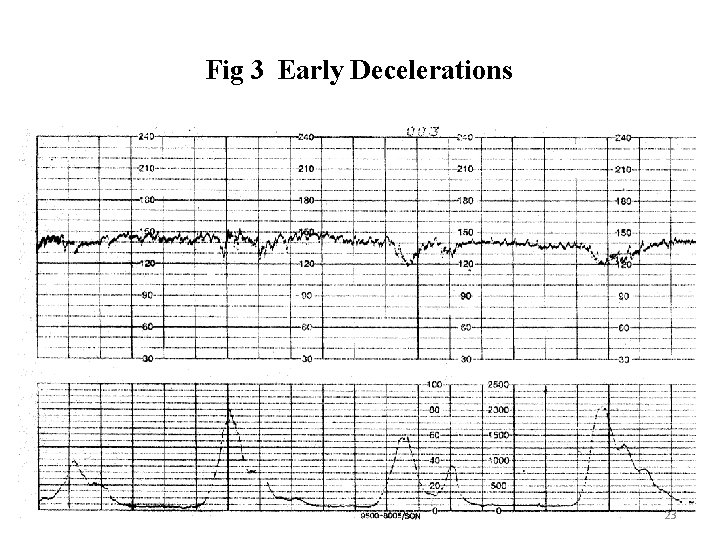
Early Deceleration Uniform, repetitive decrease of FHR with slow onset early in the contraction and slow return to baseline by the end of the contraction 22
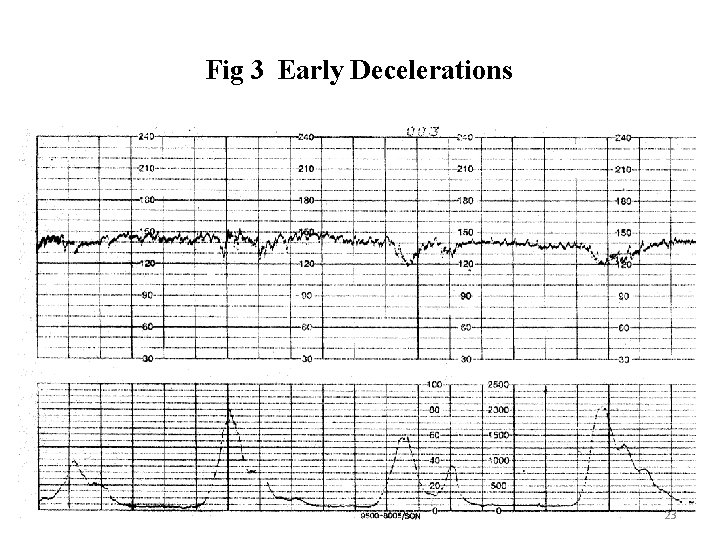
Fig 3 Early Decelerations 23
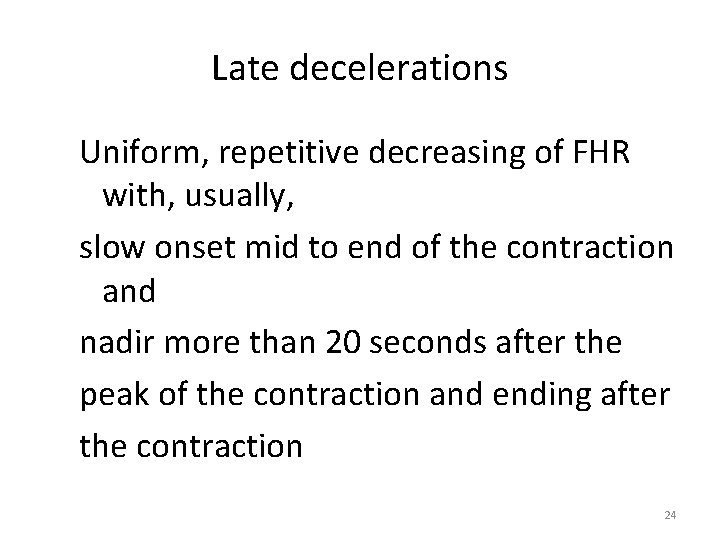
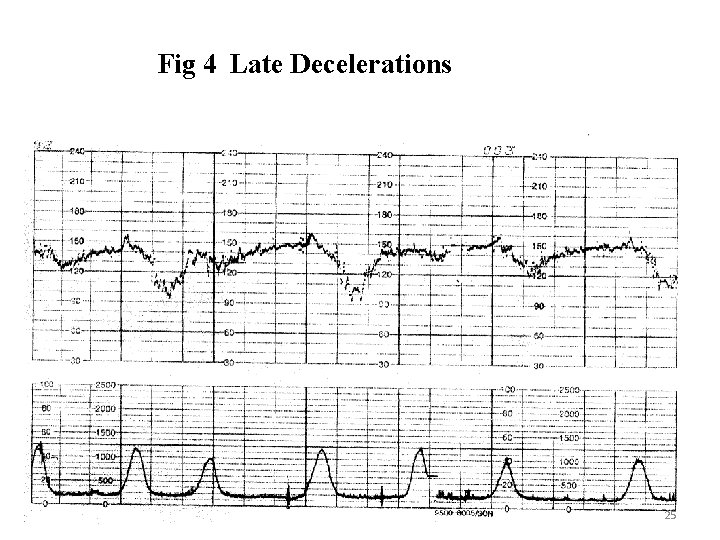
Late decelerations Uniform, repetitive decreasing of FHR with, usually, slow onset mid to end of the contraction and nadir more than 20 seconds after the peak of the contraction and ending after the contraction 24
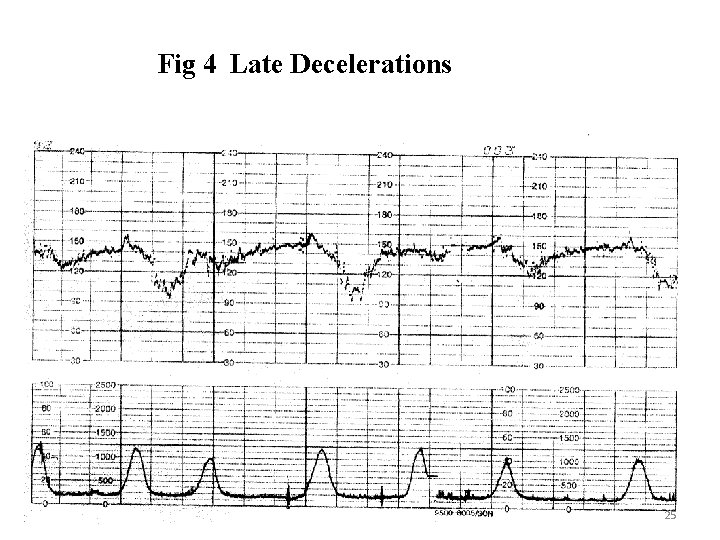
Fig 4 Late Decelerations 25
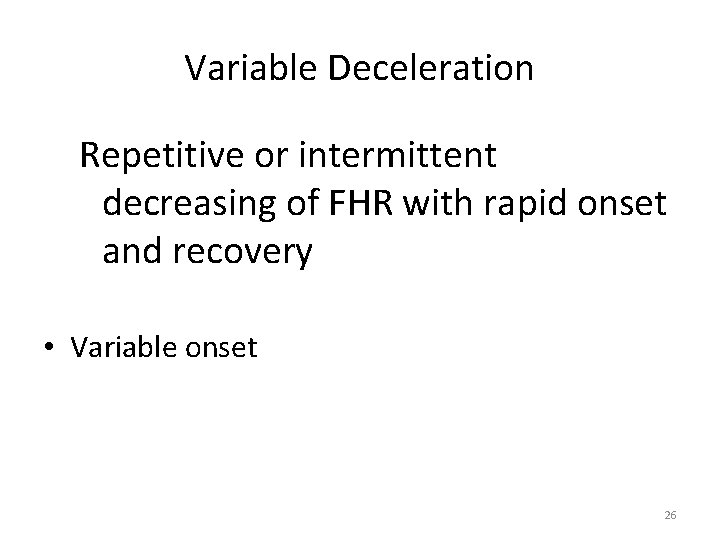
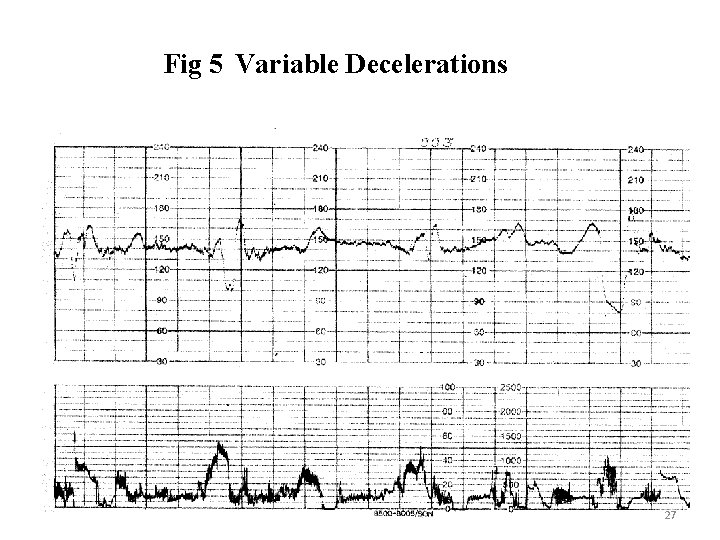
Variable Deceleration Repetitive or intermittent decreasing of FHR with rapid onset and recovery • Variable onset 26
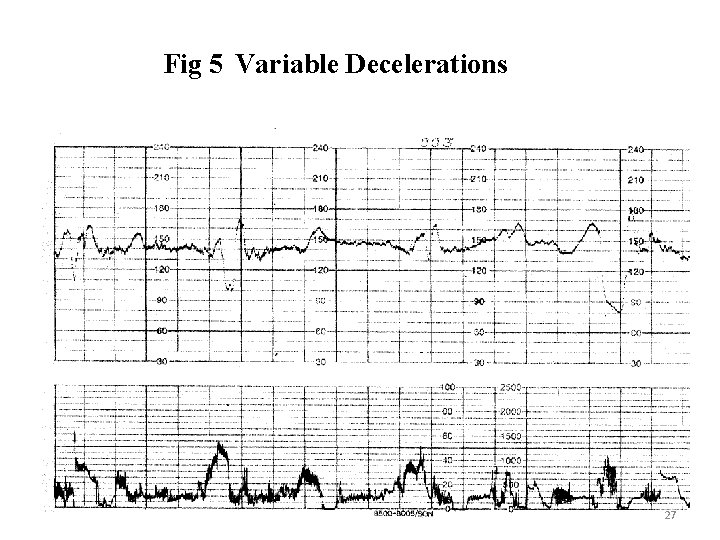
Fig 5 Variable Decelerations 27
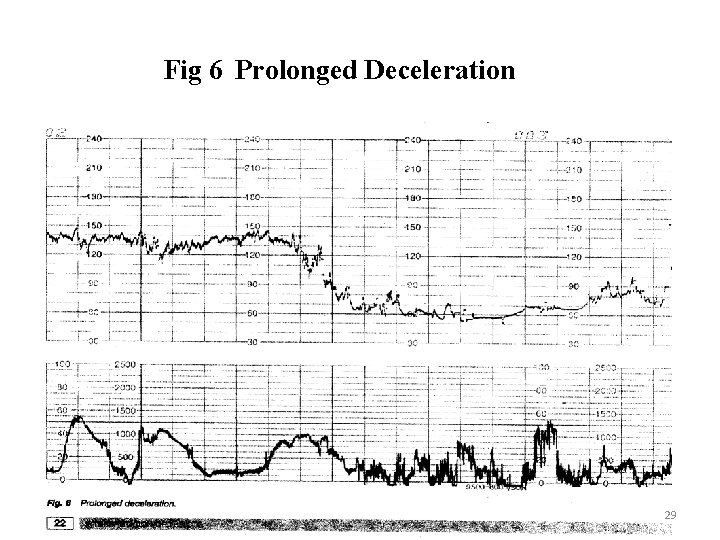
Prolonged Decelerations § Decrease of FHR below the baseline of more than 15 bpm for longer than 90 seconds but less than 5 minutes § Is pathological when crosses 2 contractions i. e 3 mins § Reduction in Oxygen transfer to placenta § Associated with poor neonatal outcome 28
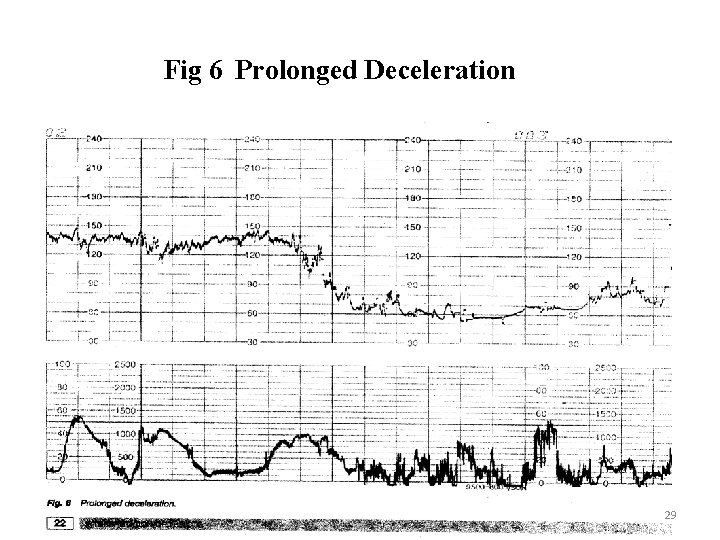
Fig 6 Prolonged Deceleration 29
Prolonged Decelerations CAUSES • • Cord prolapse. Maternal hypertension Uterine Hypertonia Followed by a VE or ARM or SROM with High presenting part 30
Normal antenatal CTG trace § The normal antenatal CTG is associated with a low probability of fetal compromise and has the following features: § Baseline fetal heart rate (FHR) is between 110 -160 bpm § Variability of FHR is between 5 -25 bpm § Decelerations are absent or early § Accelerations x 2 within 20 minutes 31
Non-reassuring CTG trace Is where any of the following is present: § The presence of two or more features is considered abnormal as these may be associated with fetal compromise and require further action § Baseline FHR is between 100 -109 bpm or between 161 -170 bpm § Variability of FHR is reduced (3 -5 bpm for >40 minutes) 32
Abnormal CTG trace The following features are very likely to be associated with significant fetal compromise and require further action– Two of the features described in non-reassuring CTG trace are present, OR – Baseline FHR is <100 bpm or >170 bpm – Variability is absent or <3 bpm – Variability is sinusoidal – Decelerations are prolonged for >3 minutes / late / have complicated variables 33
Process Preparation – Determine indication for fetal monitoring – Discuss fetal monitoring with the woman and obtain permission to commence – Perform abdominal examination to determine lie and presentation – Give the woman the opportunity to empty her bladder – The woman should be in an upright or lateral position (not supine) 34
Process Preparation • Check the accurate date and time has been set on the CTG machine, and paper speed is set at 1 cm per minute • CTGs must be labelled with the mother’s name, her number and date / time of commencement • Maternal heart rate must be recorded on the CTG at commencement of the CTG in order to differentiate between maternal and fetal heart rates 35
ASSESSING THE CTG USING DR C M BRAVADO • Determine risk if the woman is a high or low obstetric risk. This sets the background for the interpretation • C Assess the frequency and quality of Contractions per 10 minutes. • M Assess fetal Movements, presence of Meconium and Maternal observations • Bra Determine Baseline Rate and compare with earlier rate if possible. • V Assess baseline Variability, is it normal, increased or reduced. • A Are Accelerations present in response to fetal movements or contractions • D If Decelerations are present, what are their characteristics. • O Give an overall classification for the CTG • • • Normal Suspicious Pathological 36
FETAL SCALP BLOOD SAMPLING • Useful in the presence of a non reassuring CTG • A scalp blood sample for p. H or lactate determination • Specificity is high ( A normal value rules out asphyxia) • The sensitivity and positive predictive value of a low scalp p. H in identifying a newborn with Hypoxic-ischaemic encephalopathy is low
FETAL PULSE OXIMETRY • Measures fetal oxygenation during labour • It is performed using a sensor placed transcervically against the fetal cheek • Normal values btw 35% and 65% • Metabolic acidosis develops when the value falls below 30% for at least 10 -15 mins
CONCLUSION • The well being of any pregnancy begins preconception with adequate counselling of mothers with medical conditions • Pregnancy monitoring begins early in the gestation • Early and frequent prenatal care allows the care provider to screen the population to identify pregnancies at risk, afterall
“A NORMAL DELIVERY IS ONE IN WHICH THE MOTHER AND THE BABY ARE IN GOOD CONDITION REGARDLESS OF THE MODE OF DELIVERY”
THANK YOU FOR LISTENING