Fetal Blood Sampling in early labour is there
Fetal Blood Sampling in early labour: is there an increased risk of operative delivery and fetal morbidity BJOG 2011; 118: 849 -855 A Critical appraisal by Mojisola Oniah Nidhi Nandan 03/06/11
Aims and Objectives • To determine whether the rate of caesarean section was increased in women who had FBS in early labour • To gain experience in critically appraising a retrospective cohort paper
Introduction • Fetal blood sampling(FBS) plays a part in assessing fetal wellbeing during labour. • Sensitivity for the prediction of fetal compromise is significantly increased by its use. • FBS significantly reduces the rate of emergency caeserean section for fetal distress • It is an invasive procedure done in the left lateral position. It requires passing an amnioscope into the cervix in the presence of ruptured membranes. • The fetal scalp is incised and blood is collected into a heparinized capillary tube. The sample is then analyzed to determine the fetal Ph and base excess. • It is taken that a result of >7. 20 is normal and anything less than that should prompt immediate delivery.
Clinical Question • Does Fetal Blood Sampling in early labour increase the risk of operative delivery and fetal morbidity?
Guidelines • NICE guidelines recommend that FBS be performed in the presence of a ‘Pathological’ CTG where delivery is contemplated because of the abnormal fetal heart pattern. • Data from the 1990 s suggest that FBS is used in about 5% of labours
Paper selected • Heazell A, Riches J, Hopkins L, Myers J. Fetal blood sampling(FBS) in early labour: is there an increased risk of operative delivery and fetal morbidity? BJOG 2011; 118: 849855 • Paper was selected because we didn’t have much time but we wanted to analyse a paper that was current, relevant and easy to analyse.
Aim of the study • They hypothesized that women undergoing FBS in early labour (cervical dilatation <3 cm) were less likely to achieve a vaginal delivery than women undergoing FBS in established labour (cervical dilatation >4 cm) • They also hypothesized that repeat FBS was not associated with an increased rate of operative delivery or adverse neonatal outcomes. • The objective of the study was to analyze a group of consecutive women who underwent FBS in labour to address these hypotheses and to determine whether repeated FBS was associated with poorer neonatal outcomes.
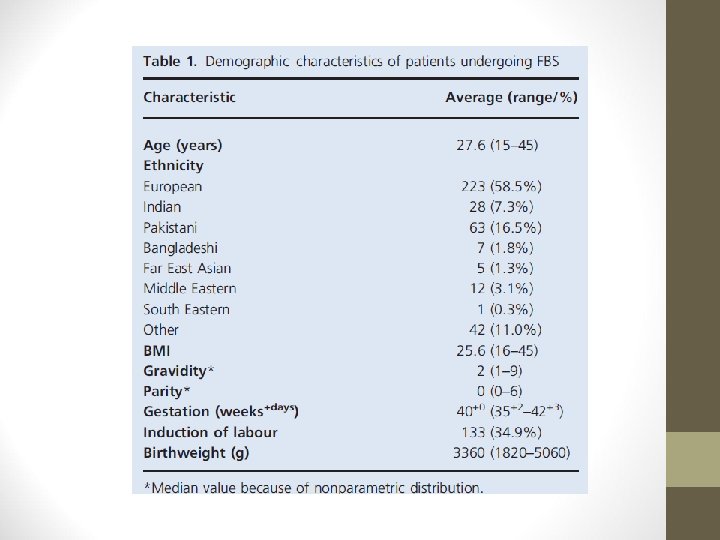
Methods • A retrospective cohort study. • Women undergoing FBS in labour at 2 hospitals: Royal Blackburn Hospital and St Mary's Hospital Manchester. • Time scale: March 2008 – June 2009 • A minimum sample size of 380 women was calculated on the basis that approximately 12% of women would have an FBS at <3 cm.
Methods • Case notes were identified using patient hospital no obtained from the blood gas analyser. • The case notes were then obtained and relevant data collected. • Statistical analysis was carried out using spss v 16. 0.
Details of the Study
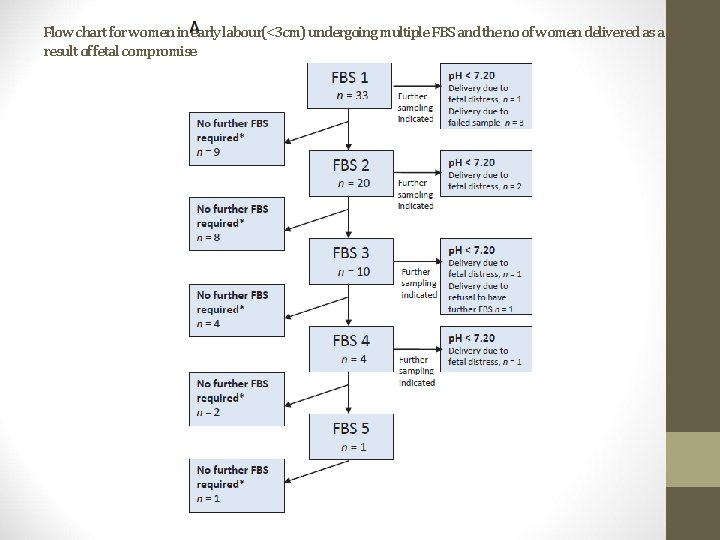
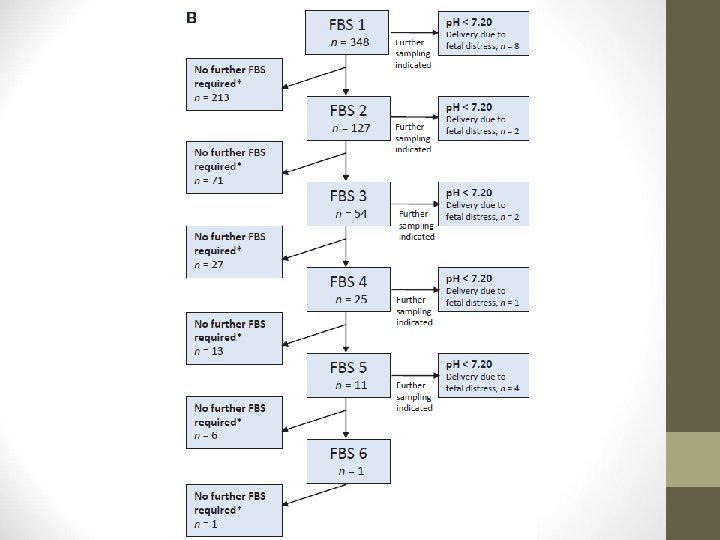
Flow chart for women in early labour(<3 cm) undergoing multiple FBS and the no of women delivered as a result of fetal compromise
Outcomes of labours • 31% of women had CS (37. 3% cat 1), 36. 7%had instrumental delivery and 32. 4% had a spontaneous vaginal delivery. • 48. 4%of women who had FBS performed at 3 cm had a vaginal delivery compared with 71. 9% of women who were >4 cm at there first FBS. • The proportions of nulliparous women (59. 1%) who required FBS in early labour and were ultimately delivered by CS was higher that of parous women(36. 4%) • Women who required 2 or more FBS(n=147) had an odds ratio for CS of 1. 71(95% CI 1. 37 -2. 13) compared to those requiring a single sample(n=234). • Of women giving birth vaginally the odds ratio for instrumental delivery compared with normal delivery was not statistically significant for women undergoing first FBS at 3 cm dilation or for 2 or more FBS.
Fetal outcomes • All babies were born alive. • Mean birthweight 3360 g and 5. 8% had a BW <2500 g. • There was no significant differences in umbilical Ph and BE values between women with first FBS at <3 cm and those at >4 cm dilatation. • 23 (6. 9%)infants were admitted to NICU. • There was no increased likelihood of NICU admission for a first FBS at <3 cm • Infants undergoing >3 FBS were slightly more likely to be admitted to NICU(OR 2. 69; 95% CI 1. 09 -6. 64)
Critical appraisal • Did the study address a clearly focused issue? YES: they wanted to see if FBS in early labour was associated with an increased risk of operative delivery and fetal morbidity. • Did the authors use an appropriate method to answer their question? YES: Used a retrospective cohort study
Critical Appraisal • Was the cohort recruited in an acceptable way? YES: No of women who had FBS performed was collected from the blood gas analyser machines on the delivery suite. No of women for the study was adequate • Was the exposure accurately measured to minimize bias? As it was a retrospective study all the women in the cohort group had a FBS performed and recorded and this would minimise bias
• Was the outcome accurately measured to minimise bias? YES: The outcome was
• Have the authors identified all important confounding factors? YES: They looked at demographics-age, ethnicity, BMI, parity, gestation, whether labour was induced, previous caeserean section. They considered the fact some patients might have that other factors precipitating the need for C/S eg Failure to progress, and the fact that an FBS may not have been performed for other reasons like unable to get sample or the patient declined the procedure. • Didn’t consider maternal illness or fetal complications
• Was the follow up of subjects complete enough? Cant tell: From the study we cant tell in terms of neonatal morbidity how long the babies were followed up
• What are the results of the study? This study has shown that women commencing FBS in early labour(i. e < 3 cm cervical dilatation), or requiring 2 or more FBS procedures, have an increased risk of proceeding to caesarean section rather than vaginal delivery. • How precise is the estimate risk? For the women undergoing FBS in early labour the incresed risk of delivery by C /S compared to those in established labour is modest(OR 1. 71; 95%CI 1. 04 -3. 13) Similarly , women undergoing 2 or more FBS were at increased risk of C/S(OR 1. 71; 95% CI 1. 37 -2. 13)
• Do you believe the results? YES
• Can the results be applied to the local population? YES: • Do the results of the study fit with other available evidence?
Conclusion
- Slides: 24