Fetal and Neonatal Physiology Fetal and Neonatal Physiology


- Slides: 36
Fetal and Neonatal Physiology
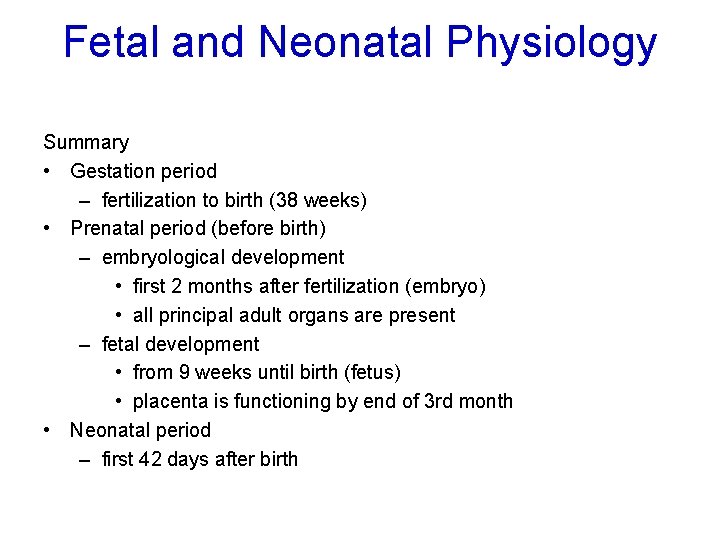
Fetal and Neonatal Physiology Summary • Gestation period – fertilization to birth (38 weeks) • Prenatal period (before birth) – embryological development • first 2 months after fertilization (embryo) • all principal adult organs are present – fetal development • from 9 weeks until birth (fetus) • placenta is functioning by end of 3 rd month • Neonatal period – first 42 days after birth
Fetal & Neonatal physiology • Discussion • Fetal development • Functioning of the child immediately after birth • Growth and development through the early year of life • Fetal growth and functional development of organs system
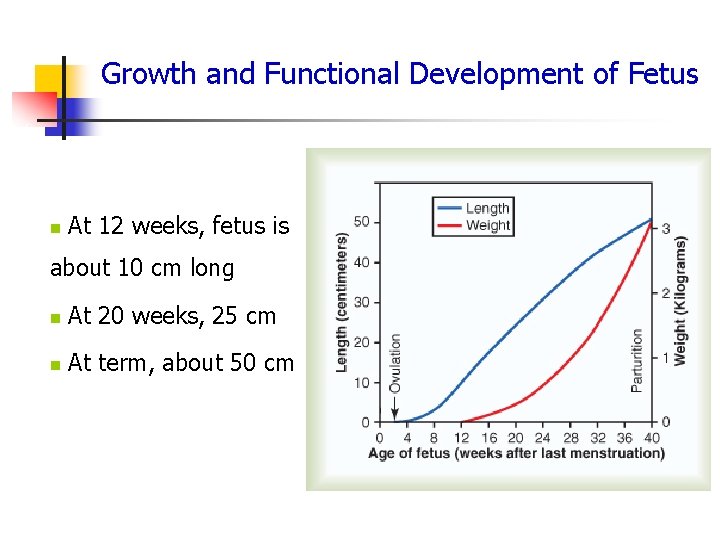
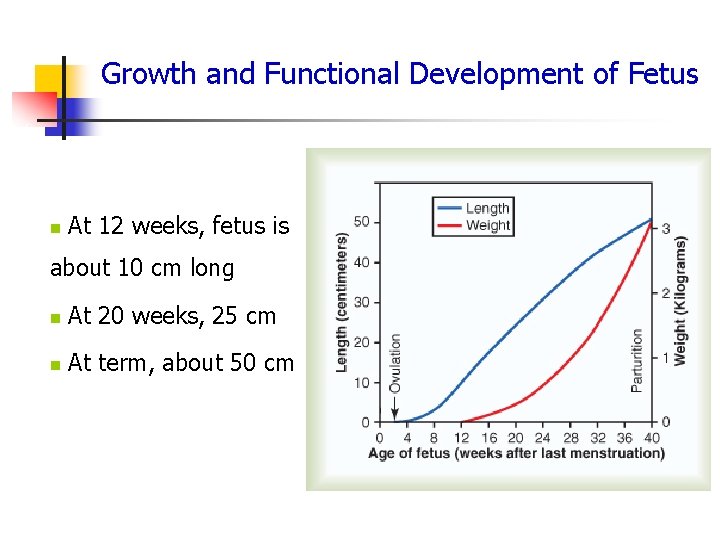
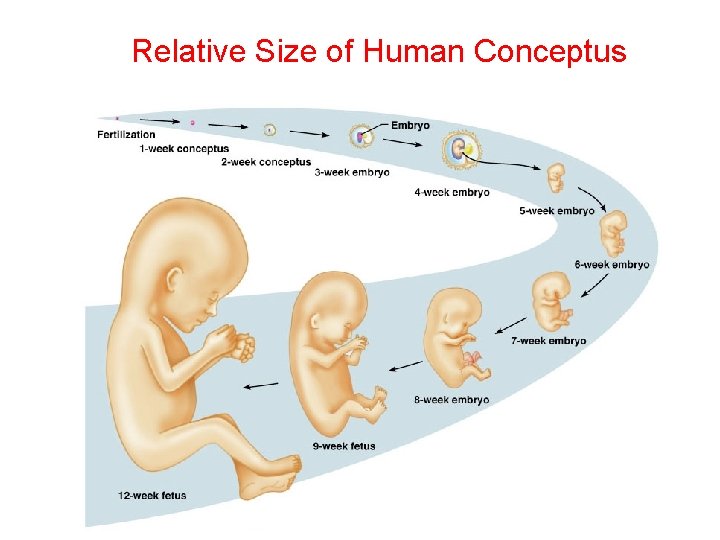
Growth and Functional Development of Fetus n At 12 weeks, fetus is about 10 cm long n At 20 weeks, 25 cm n At term, about 50 cm
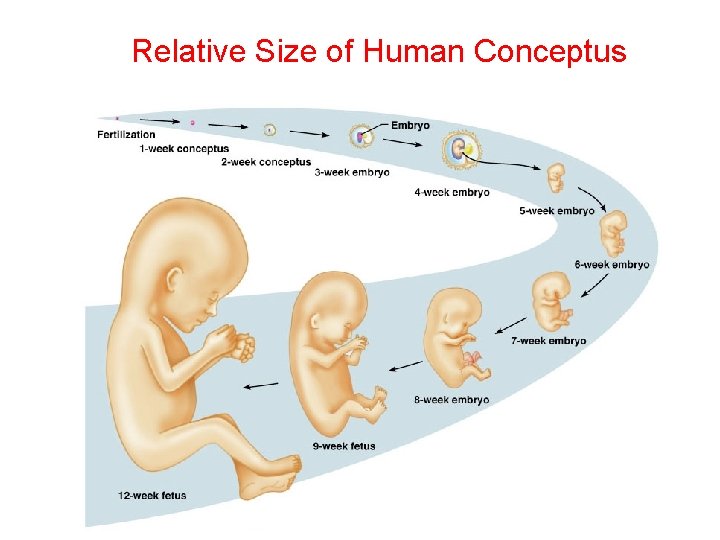
Relative Size of Human Conceptus
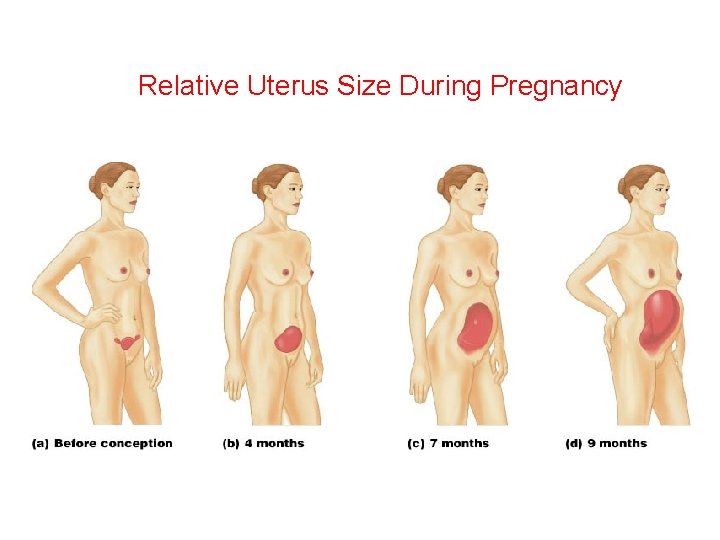
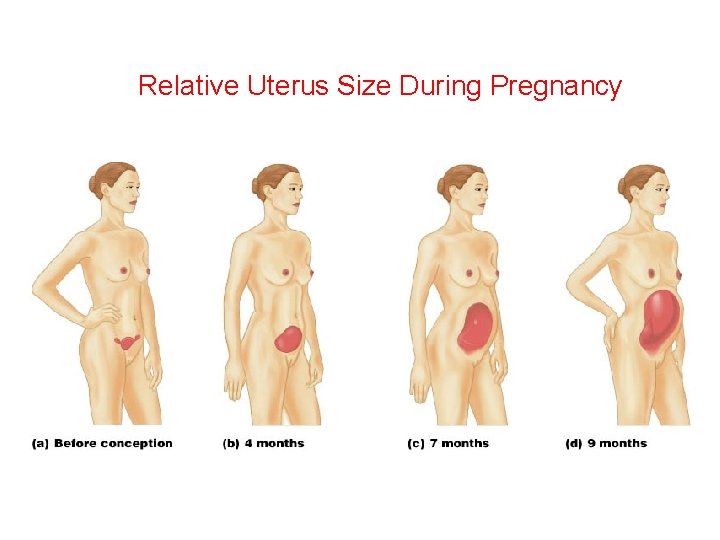
Relative Uterus Size During Pregnancy
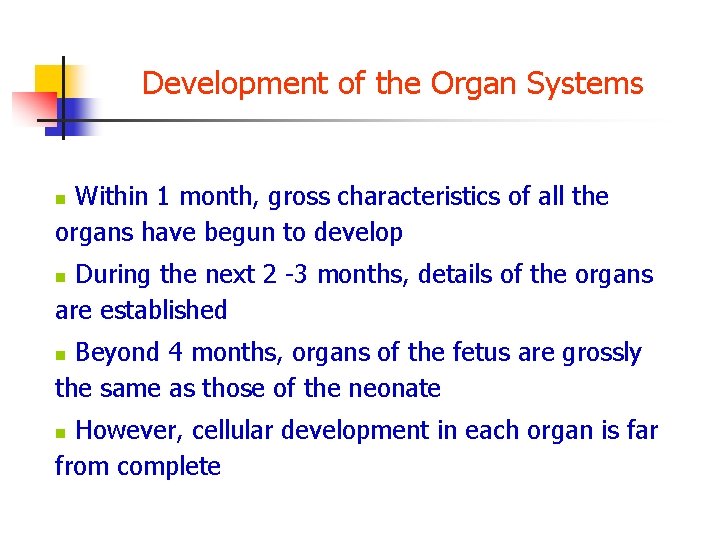
Development of the Organ Systems Within 1 month, gross characteristics of all the organs have begun to develop n During the next 2 -3 months, details of the organs are established n Beyond 4 months, organs of the fetus are grossly the same as those of the neonate n However, cellular development in each organ is far from complete n
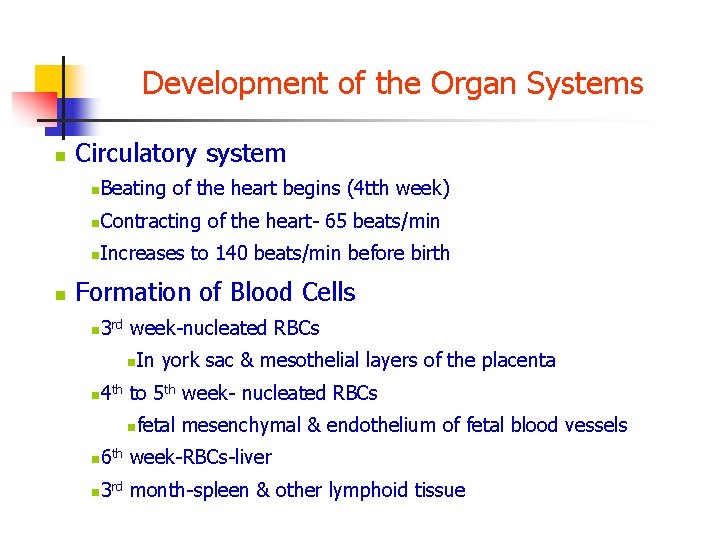
Development of the Organ Systems n n Circulatory system n Beating of the heart begins (4 tth week) n Contracting of the heart- 65 beats/min n Increases to 140 beats/min before birth Formation of Blood Cells 3 week-nucleated RBCs n rd n In york sac & mesothelial layers of the placenta 4 to 5 th week- nucleated RBCs n th n fetal mesenchymal & endothelium of fetal blood vessels 6 week-RBCs-liver n th 3 month-spleen & other lymphoid tissue n rd
Development of the Organ Systems 3 month onwards q rd n n Principle source RBCs & most of WBC - bone marrow n Lymphocytes & plasma cells- lymphoid tissue Respiratory System n No respiratory activity during fetal life n No air to breath in amniotic fluid n Lungs are completely deflated n Inhibition ! Prevents filling of the lungs with fluids and debris from meconium excreted by fetus’s git into the amniotic fluid n
Development of the Organ Systems n Nervous system n n 3 rd to 4 th month n Spinal cord and brain stem reflexes are present n Cerebral cortex is immature n Myelinization of major tracts completed 1 yr of postnatal life Gastrointestinal n by midpregnancy n Fetus ingests and absorbs large quantities of amniotic fluid n Last 2 -3 months - function approaches that of normal neonate n Formation of meconium during the last 2 -3 months
Development of the Organ Systems n Kidneys n 2 nd trimester- urine excretion n n Oligohydramnios n n Accounts 70 -80 % of amniotic fluid Reduced formation of amniotic fluids Ø Abnormal kidney development Ø Severe impairment of kidney function Renal control systems regulation of fetal e. c. f volume & electrolyte balances, esp acid base balance are almost non-existent until late fetal life n n Do not reach full development until a few months after birth
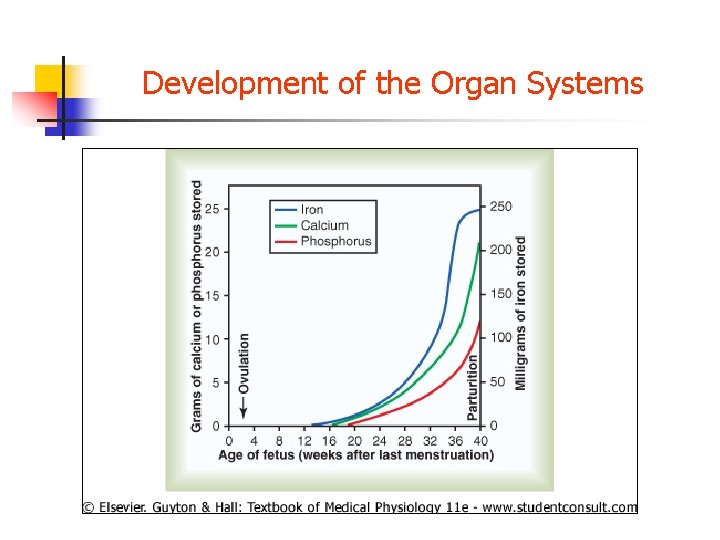
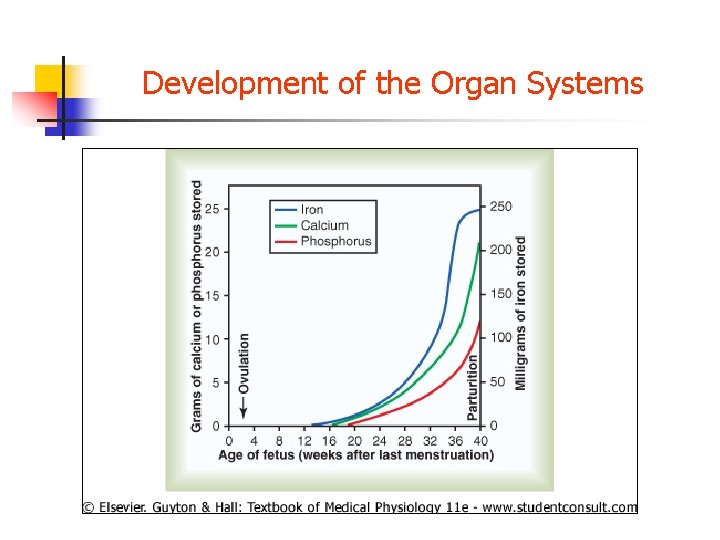
Development of the Organ Systems n n Fetal Metabolism n Glucose is the sole source of energy n Special problems about Ca, PO 4, Fe and Vit metabolism Metabolism of Calcium and Phosphate n 12 th-40 th accumulates n n Period of rapid n ossification of fetal bones n Weight gain of the fetus Accumulation of iron 3 weeks onwards n rd n Stored in the form of Hb n Used for RBCs formation n Most stored in the liver
Development of the Organ Systems n §Vitamin utilization and storage §B vitamins (B 12 & folic acid) §Formation of RBC & nervous tissues §Overall growth of fetus §Vit C §Intracellular substrate formation §Bone matrix §Fibers of connective tissue §Vitamins D §Is needed for normal bone growth §Is stored in the liver
Development of the Organ Systems • Vit E • Normal development of embryo • Its absence • Early stage abortion in animal studies • Vit K • Formation of Factor VII, prothrombin, other blood coagulation factors
Development of the Organ Systems
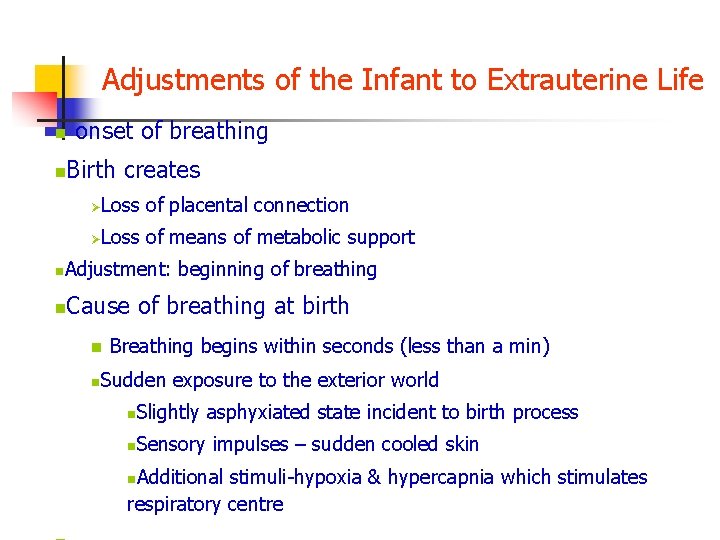
Adjustments of the Infant to Extrauterine Life n n onset of breathing Birth creates Loss of placental connection Ø Loss of means of metabolic support Ø n Adjustment: beginning of breathing n Cause of breathing at birth n n Breathing begins within seconds (less than a min) Sudden exposure to the exterior world n Slightly asphyxiated state incident to birth process n Sensory impulses – sudden cooled skin Additional stimuli-hypoxia & hypercapnia which stimulates respiratory centre n
Adjustments of the Infant to Extrauterine Life Delayed or abnormal breathing at birth (danger of hypoxia) n n n Hypoxia frequently occurs because of n Compression of the umbilical cord n Premature separation of placenta n Excessive contraction of the uterus n Excessive anaesthesia of the mother Degree of hypoxia that an infant can tolerate n Failure to breath 4 m-death in adults >8 -10 permanent/serious brain impairment including death in neonates n n Damage-thalamus, inferior colliculi, brain stem n Areas associated with motor functions of the body
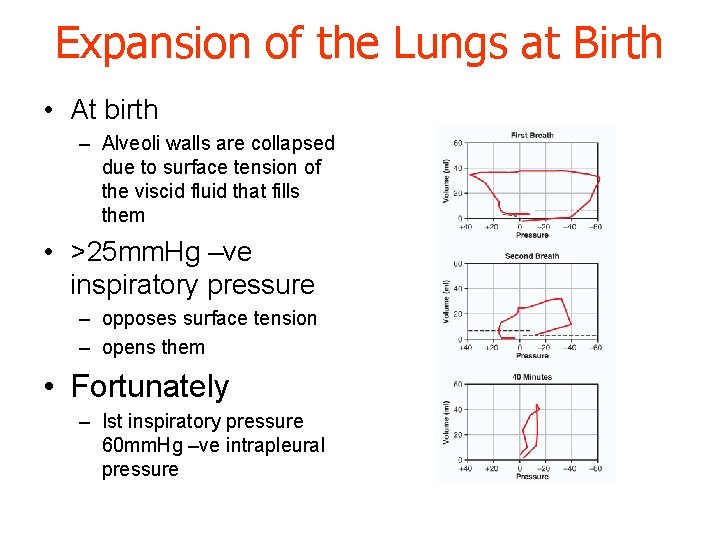
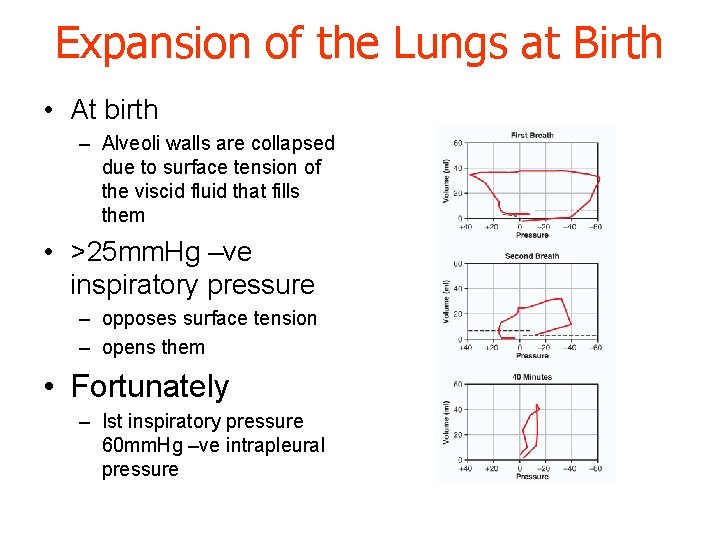
Expansion of the Lungs at Birth • At birth – Alveoli walls are collapsed due to surface tension of the viscid fluid that fills them • >25 mm. Hg –ve inspiratory pressure – opposes surface tension – opens them • Fortunately – Ist inspiratory pressure 60 mm. Hg –ve intrapleural pressure
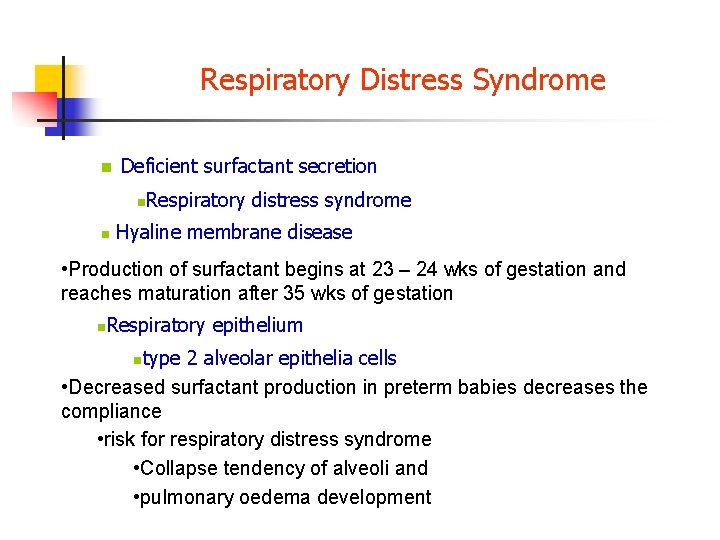
Respiratory Distress Syndrome n Deficient surfactant secretion n n Respiratory distress syndrome Hyaline membrane disease • Production of surfactant begins at 23 – 24 wks of gestation and reaches maturation after 35 wks of gestation n Respiratory epithelium type 2 alveolar epithelia cells • Decreased surfactant production in preterm babies decreases the compliance • risk for respiratory distress syndrome • Collapse tendency of alveoli and • pulmonary oedema development n

Circulatory Readjustments at Birth Special anatomical structure of fetal circulation • During fetal life – Lungs are non functional – Liver is partial functional • It is not necessary the heart to pump blood thru either of them – Much blood pumped thru the placenta • oxygenation
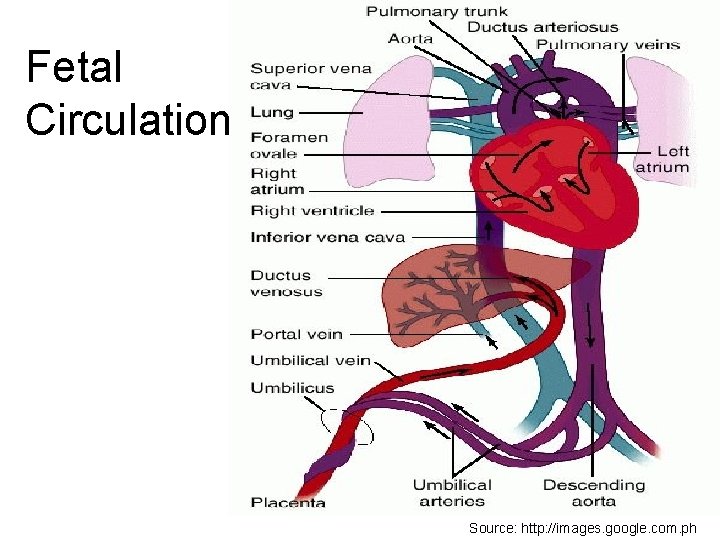
CARDIOVASCULAR SYSTEM Fetal Circulation • Nutrients for growth and development are delivered from the umbilical vein in the umbilical cord → placenta → fetal heart
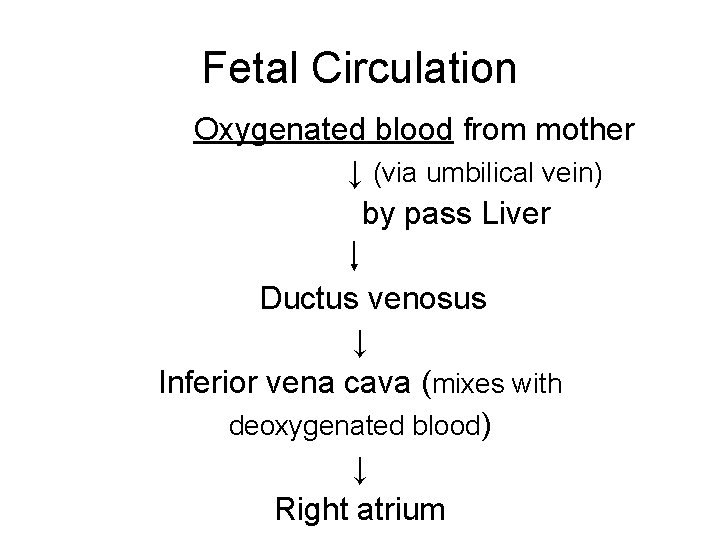
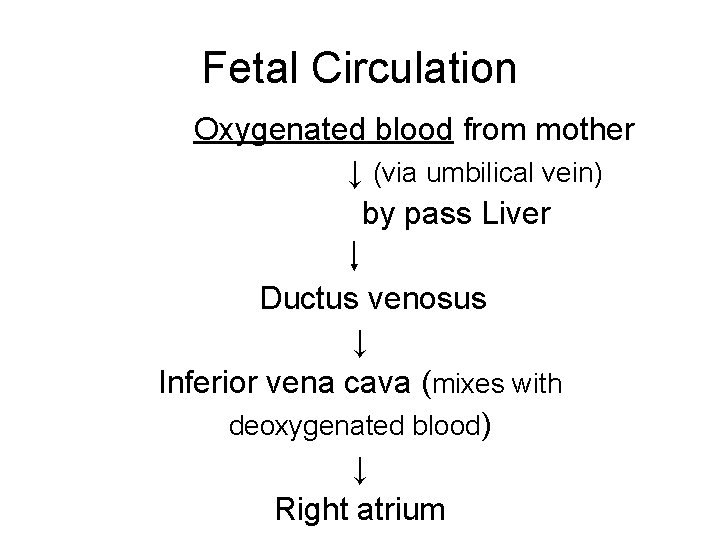
Fetal Circulation Oxygenated blood from mother ↓ (via umbilical vein) by pass Liver Ductus venosus ↓ Inferior vena cava (mixes with deoxygenated blood) ↓ Right atrium
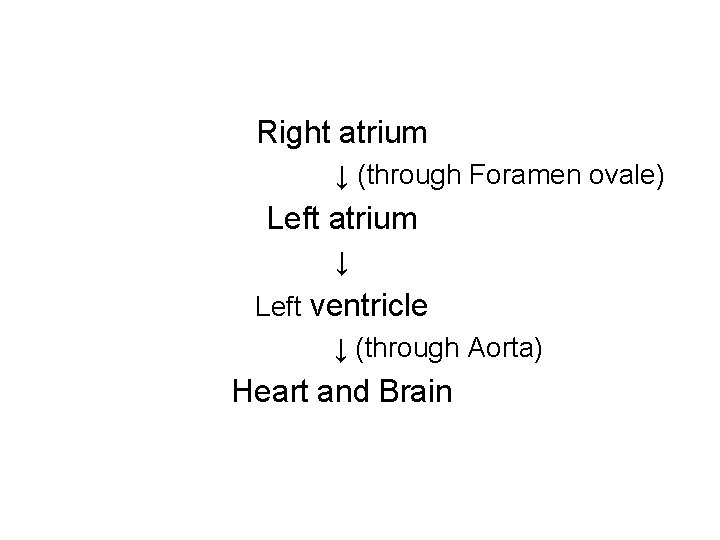
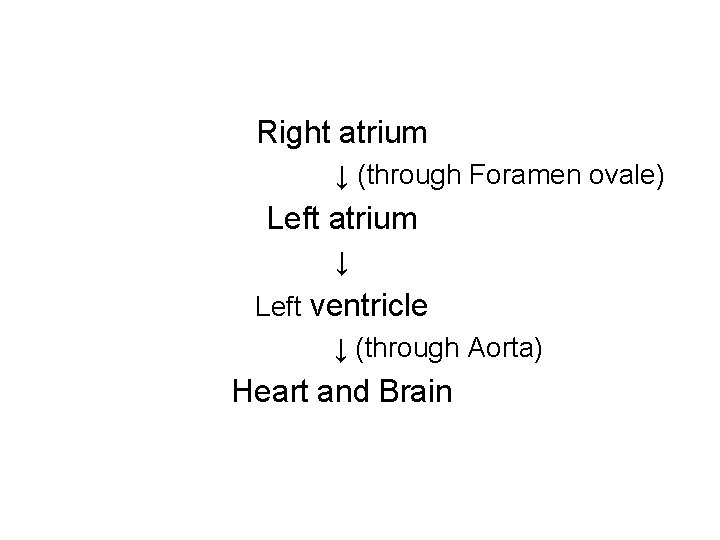
Right atrium ↓ (through Foramen ovale) Left atrium ↓ Left ventricle ↓ (through Aorta) Heart and Brain
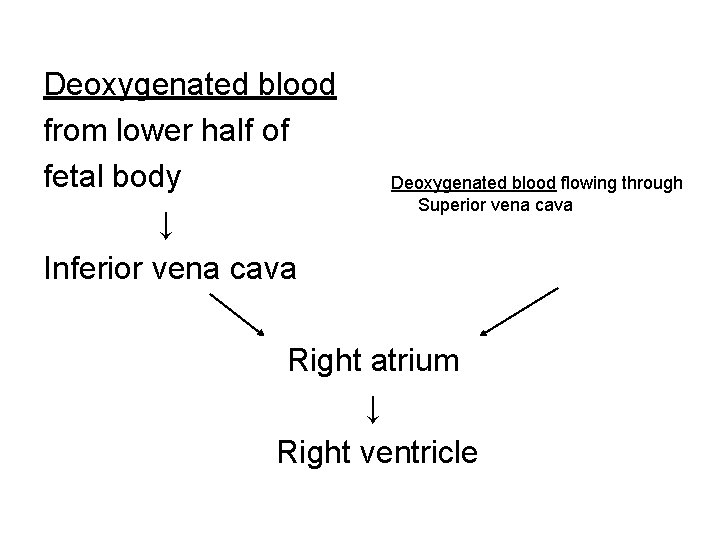
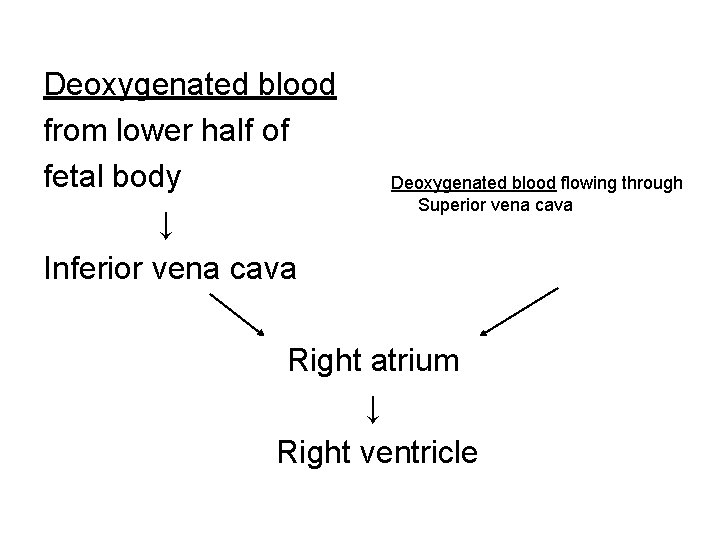
Deoxygenated blood from lower half of fetal body ↓ Inferior vena cava Deoxygenated blood flowing through Superior vena cava Right atrium ↓ Right ventricle
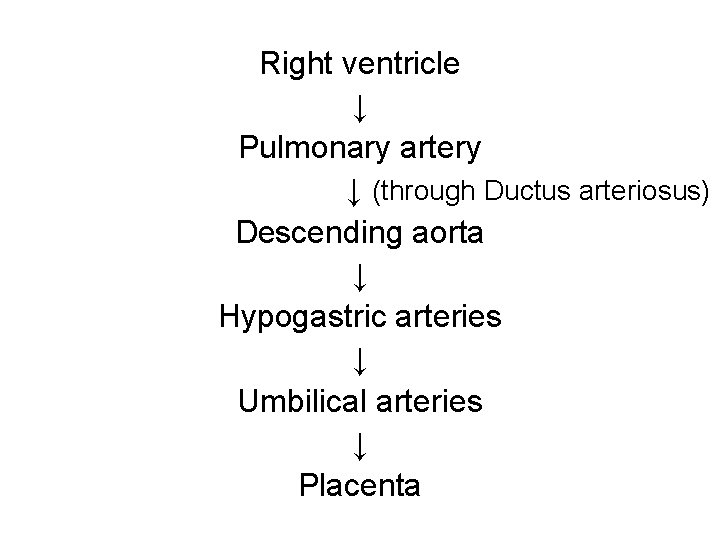
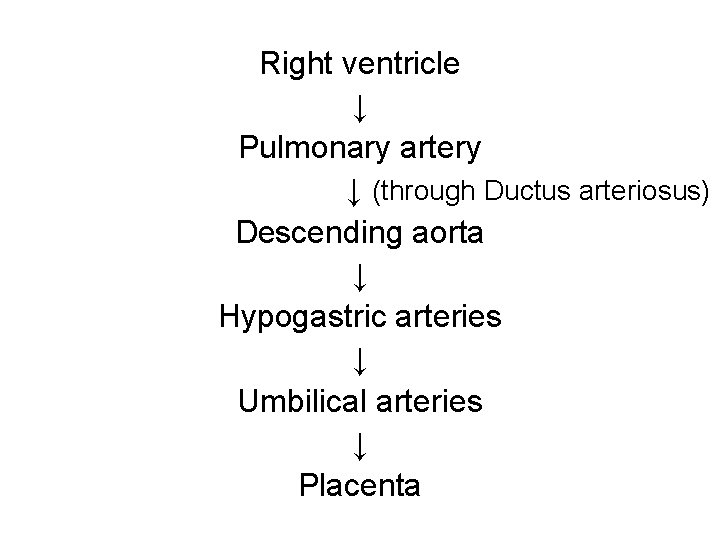
Right ventricle ↓ Pulmonary artery ↓ (through Ductus arteriosus) Descending aorta ↓ Hypogastric arteries ↓ Umbilical arteries ↓ Placenta
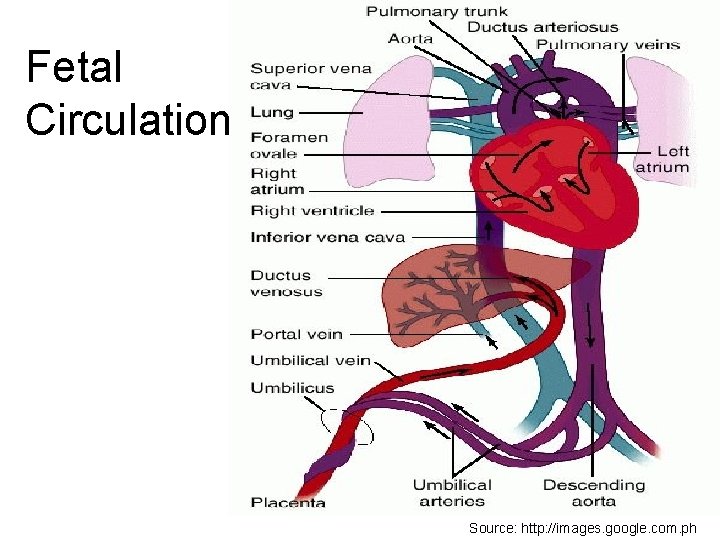
Fetal Circulation Source: http: //images. google. com. ph

Differences in Fetal and Adult Circulation 1 st difference: • Presence of shunts which allow oxygenated blood to bypass the right ventricle and pulmonary circulation, flow directly to the left ventricle, and for the aorta to supply the heart and brain • 3 shunts: - Ductus venosus - Foramen ovale - Ductus arteriosus
Differences in Fetal and Adult Circulation 2 nd difference: • Ventricles of the fetal heart work in parallel compared to the adult heart which works in sequence.
Differences in Fetal and Adult Circulation • Fetal cardiac output per unit weight is 3 times higher than that of an adult at rest. • This compensated for low O 2 content of fetal blood. • Is accomplished by ↑ heart rate and ↓ peripheral resistance
Changes After Birth • Clamped cord + fetal lung expansion = constricting and collapsing of umbilical vessels, ductus arteriosus, foramen ovale, ductus venosus • Fetal circulation changes to that of an adult
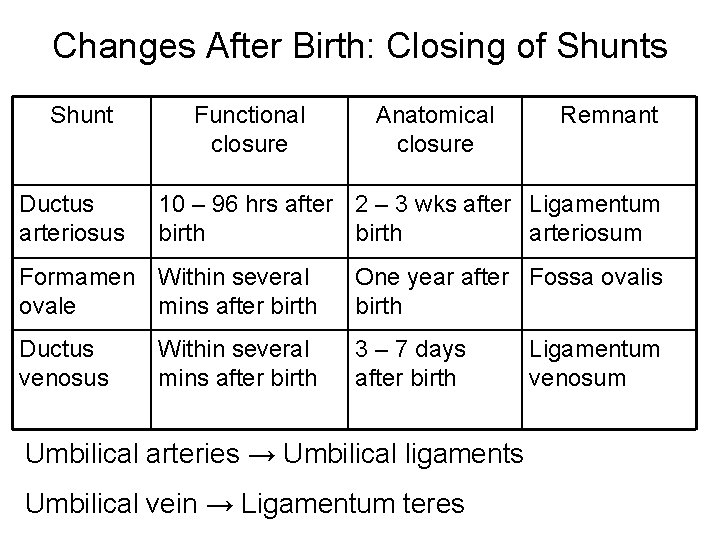
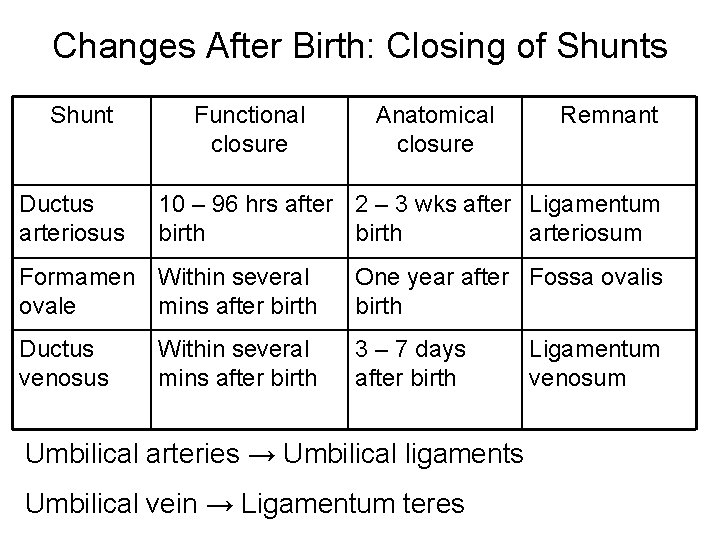
Changes After Birth: Closing of Shunts Shunt Ductus arteriosus Functional closure Anatomical closure Remnant 10 – 96 hrs after 2 – 3 wks after Ligamentum birth arteriosum Formamen Within several ovale mins after birth One year after Fossa ovalis birth Ductus venosus 3 – 7 days after birth Within several mins after birth Umbilical arteries → Umbilical ligaments Umbilical vein → Ligamentum teres Ligamentum venosum
Changes After Birth • Maintenance of ductus arteriosus depends on: - difference in blood pressure bet. Pulmonary artery and aorta - difference in O 2 tension of blood passing through ductus. ↑ p O 2 = stops flow. Mediated through prostaglandins.
Special Functional Problems in the Neonate Instability of various hormonal and neurogenic control systems n n Immature development of the organs Control systems have not adjusted to the new way of life n n Respiratory system n Circulation n Git n Renal etc
Special Problems of Prematurity Instability of the homeostatic control systems in the premature infant n n Instability of acid-base balance Low blood protein because of immature liver development & hypoproteinemic edema n n Inability of the infant to regulate calcium levels n Variability of blood glucose levels n Instability of body temperature n Temperature tends to approach the surroundings
Special Problems of Prematurity Danger of Blindness Caused by Excess Oxygen Therapy in the Premature Infant n n Respiratory distress and hypoxia Excessive oxygen therapy in treating premature infants may lead to blindness n Too much oxygen stops the growth of new blood vessels in the retina n n Growth of great mass of vessels n when oxygen therapy stops n Retrolental fibroplasia n Breathing air with 40% O 2 would be physiologic
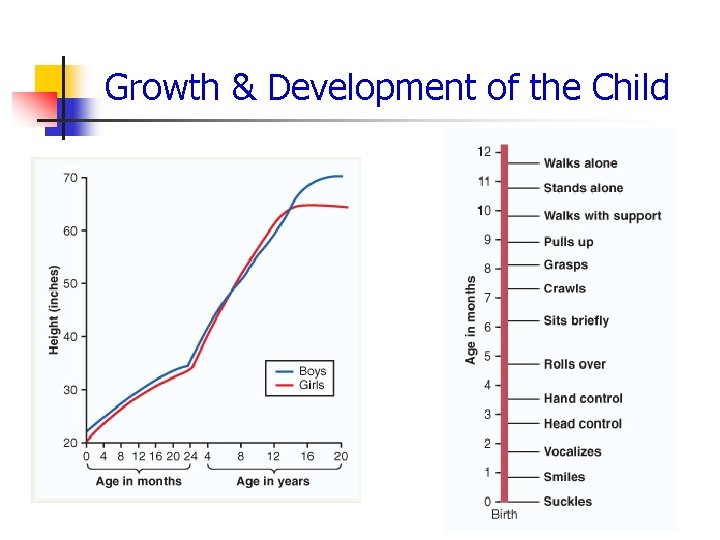
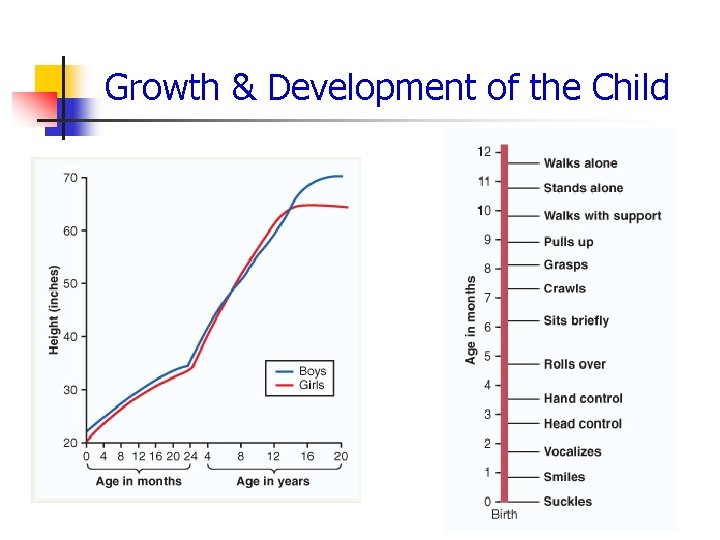
Growth & Development of the Child