Festschrift Dr Hazim Safi Larry Hollier MD FACS






- Slides: 35
Festschrift Dr. Hazim Safi Larry Hollier, MD, FACS, FACC, FRCS (Eng) Professor of Surgery and Chancellor LSU Health Sciences Center New Orleans, La
Thoracoabdominal Aortic Aneurysms Paraplegia – Paraplegia is one of the most feared complications of therapeutic intervention for thoracic and thoracoabdominal aortic disease
Thoracoabdominal Aortic Aneurysms Crawford 1986* Extent II Th. AAA – 189 patients Neurologic deficit – 28. 3 % Procedure: – Proximal aortic clamping – No shunt or bypass – Intercostal artery reimplantation +/*Crawford, et al. J Vasc Surg 1986; 3: 389 -404
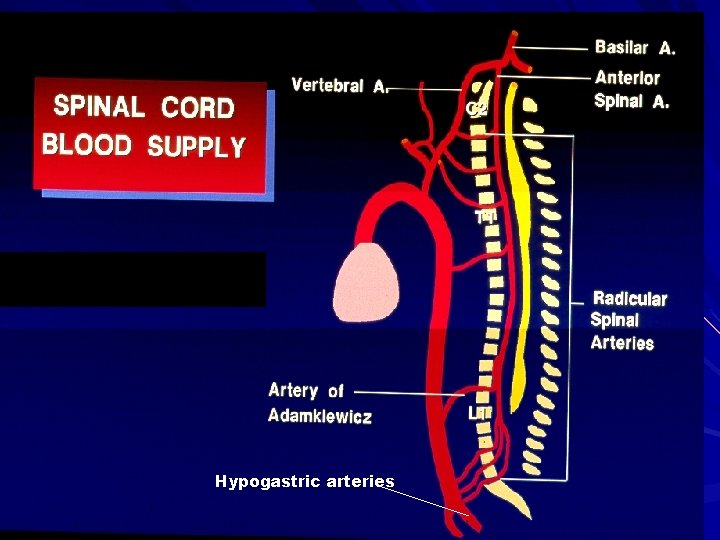
Thoracoabdominal Aortic Aneurysms Acute Paraplegia – Acute paraplegia is usually due to severe prolonged spinal cord ischemia Prolonged clamp time Inadequate bypass or perfusion pressure Failure to revascularize critical intercostals Failure to revascularize hypogastric arteries
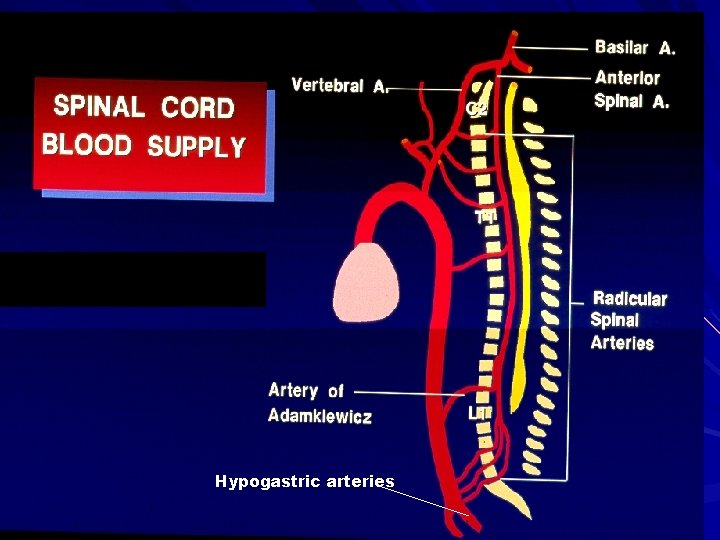
Hypogastric arteries

Intercostal reimplantation
Thoracoabdominal Aortic Aneurysms Delayed-onset Paraplegia – Usually occurs 12 -72 hours post-op – Delayed-onset paraplegia is usually due to secondary insult to an ischemia-sensitized spinal cord Cord edema with decreased perfusion Injury secondary to activated cytokines

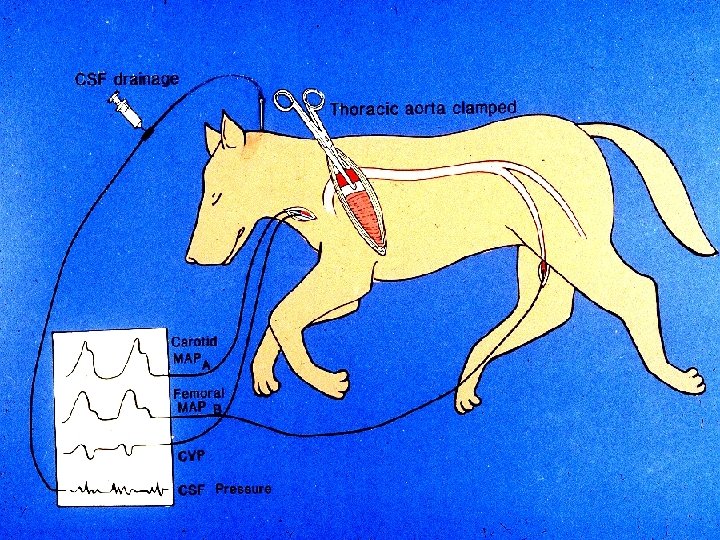
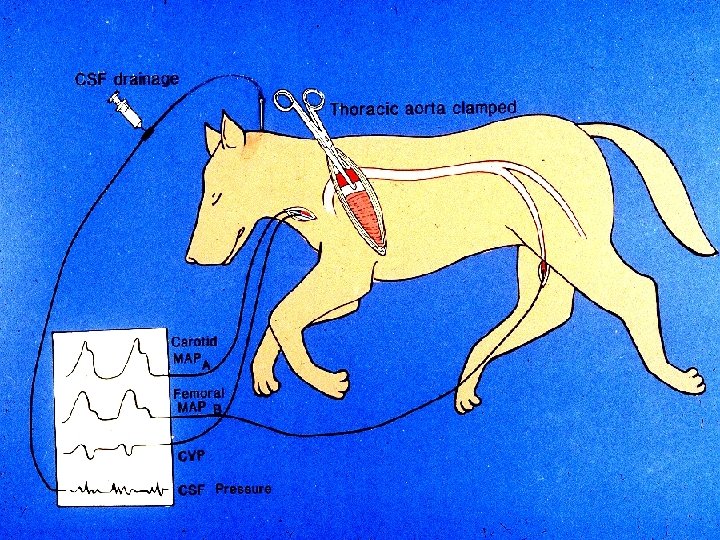
Thoracoabdominal Aortic Aneurysms Spinal cord edema in closed space – Ischemia and reperfusion of the spinal cord results in subsequent edema of the cord – The spinal canal functions as a Starling resistor – When the cord swells in the closed space of the spinal canal, CSF pressure rises – Increased CSF pressure reduces perfusion of the spinal cord

Thoracoabdominal Aortic Aneurysms
Thoracoabdominal Aortic Aneurysms
Thoracoabdominal Aortic Aneurysms

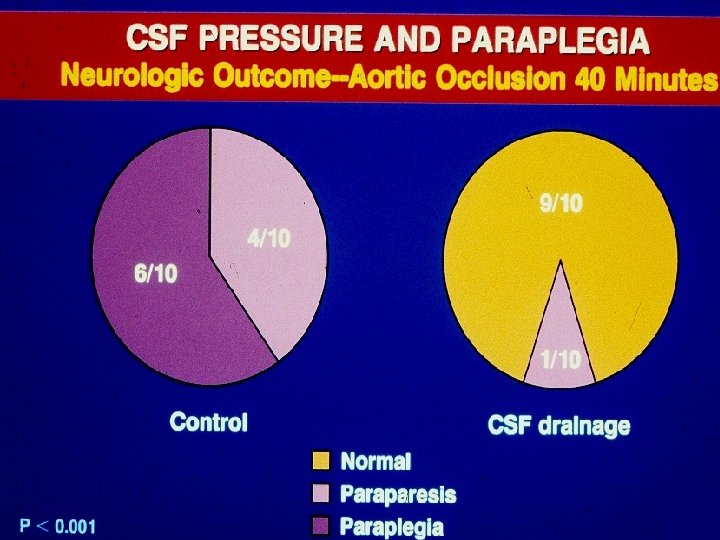
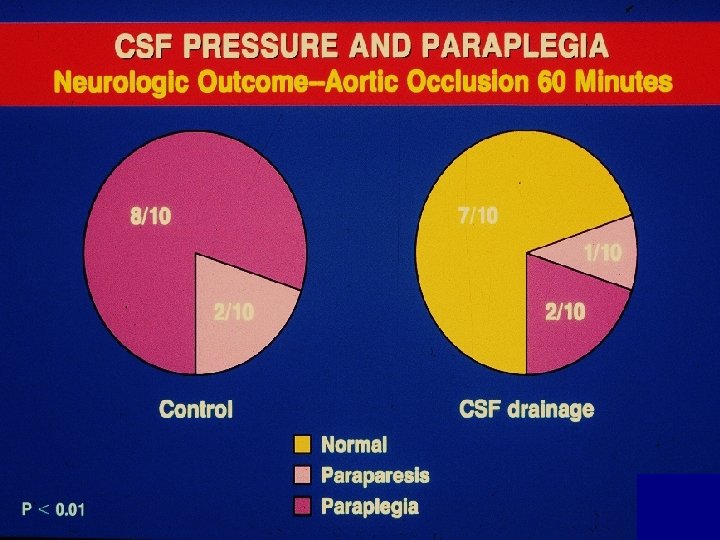
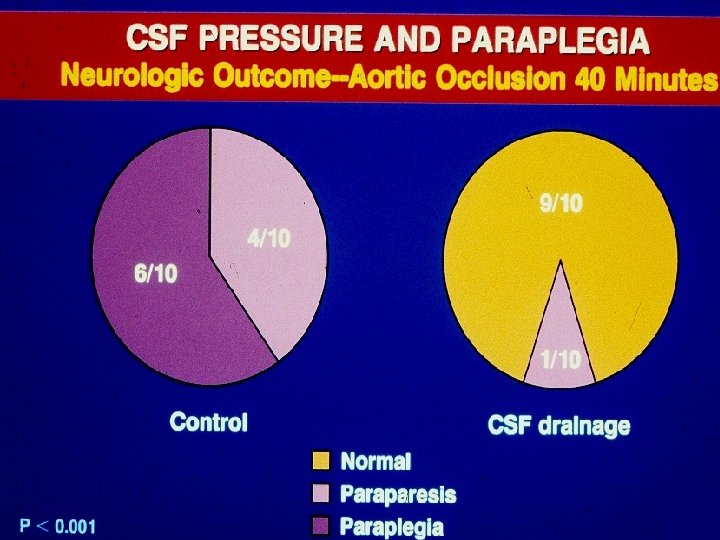
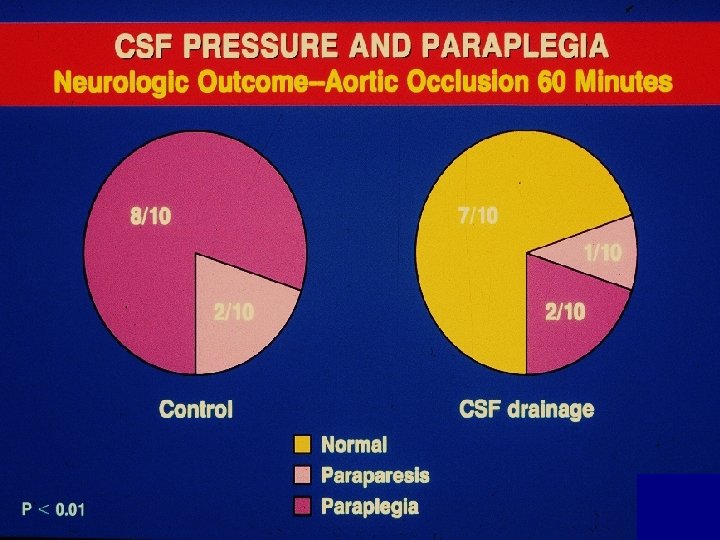
Thoracoabdominal Aortic Aneurysms Thoracic aortic occlusion significantly increases spinal fluid pressure and decreases spinal cord perfusion Drainage of CSF increases spinal cord perfusion pressure and decreases the incidence of paraplegia “CSF drainage may be a useful adjunct to prevent paraplegia following Th. AAA repair. ” *Mc. Cullough, Hollier, Nugent. J Vasc Surg 1988; 7: 153 -60
Thoracoabdominal Aortic Aneurysms Crawford 1990* – Prospective randomized study of CSF drainage to prevent paraplegia 98 patients (48 drainage; 52 controls) Neurologic deficit: 30% drainage vs. 33% controls *Crawford, et al. J Vasc Surg 1990; 13: 36 -46
Thoracoabdominal Aortic Aneurysms Crawford 1990* – Prospective randomized study of CSF drainage to prevent paraplegia 98 patients (48 drainage; 52 controls) Neurologic deficit: 30% drainage vs. 33% controls “Protocol…limited to withdrawal of a maximum of 50 ml of CSF in excess of loss during insertion of the catheter. ” *Crawford, et al. J Vasc Surg 1990; 13: 36 -46
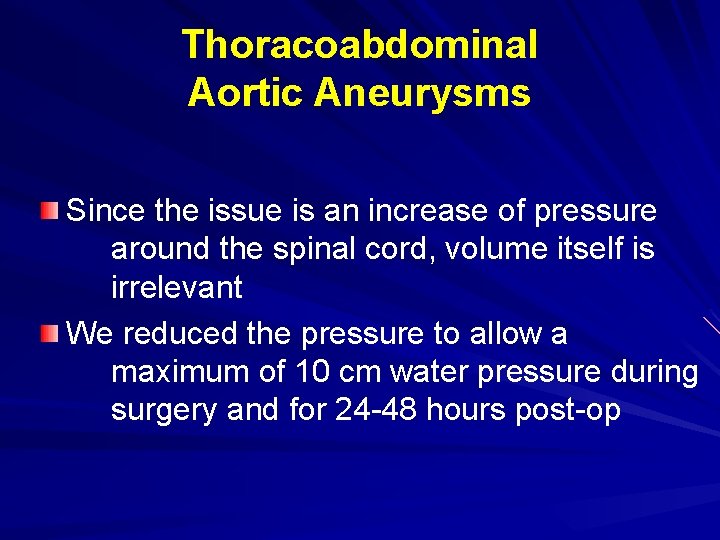
Thoracoabdominal Aortic Aneurysms Since the issue is an increase of pressure around the spinal cord, volume itself is irrelevant We reduced the pressure to allow a maximum of 10 cm water pressure during surgery and for 24 -48 hours post-op

CSF Drainage
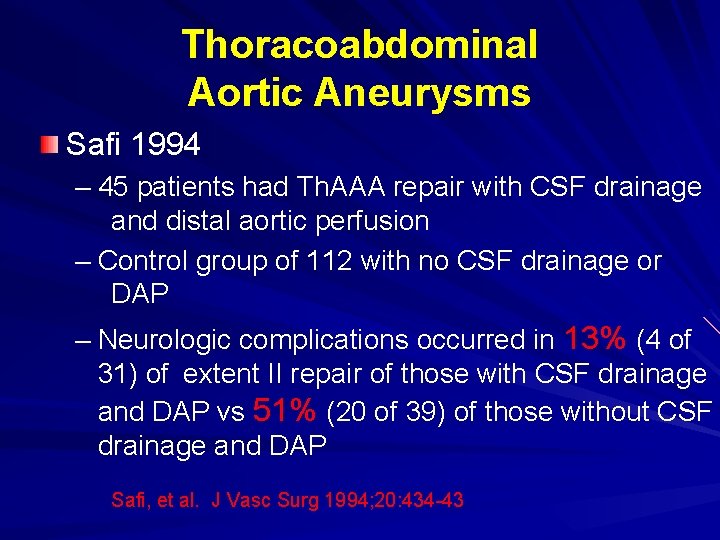
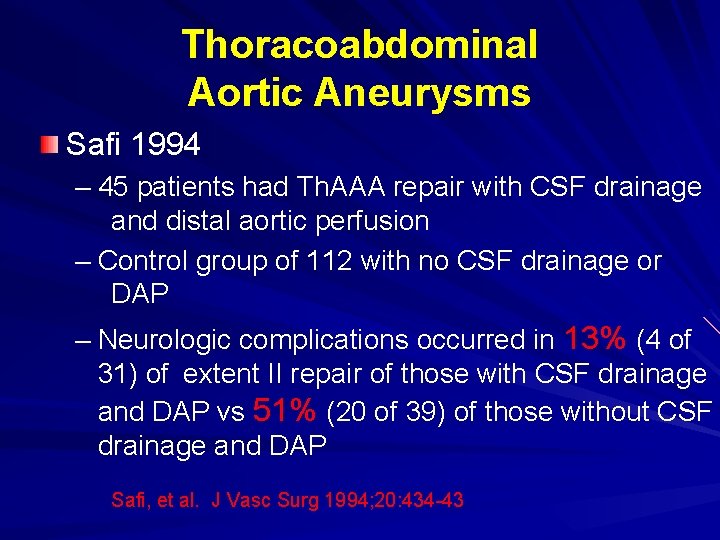
Thoracoabdominal Aortic Aneurysms Safi 1994 – 45 patients had Th. AAA repair with CSF drainage and distal aortic perfusion – Control group of 112 with no CSF drainage or DAP – Neurologic complications occurred in 13% (4 of 31) of extent II repair of those with CSF drainage and DAP vs 51% (20 of 39) of those without CSF drainage and DAP Safi, et al. J Vasc Surg 1994; 20: 434 -43
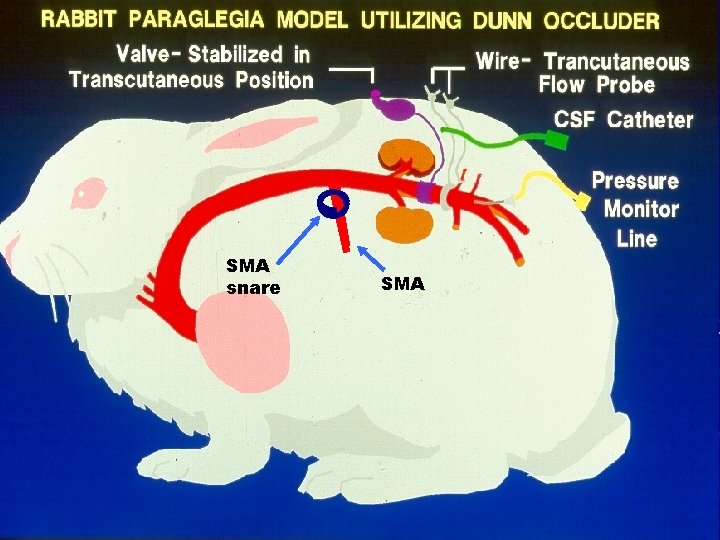
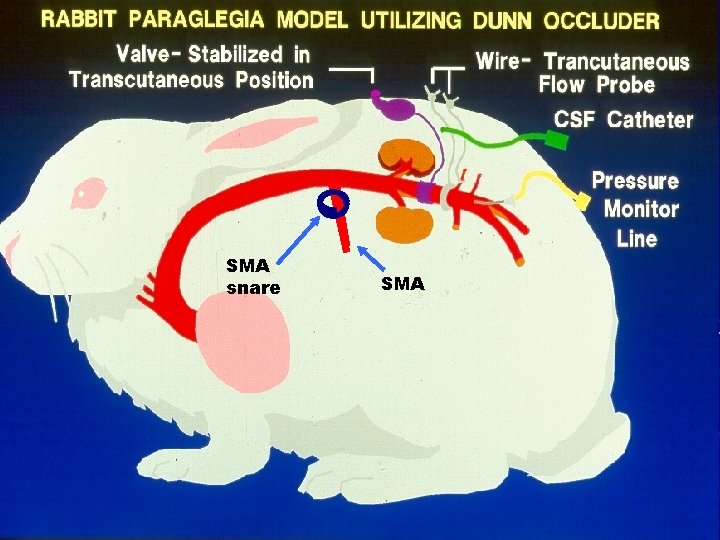
SMA snare SMA
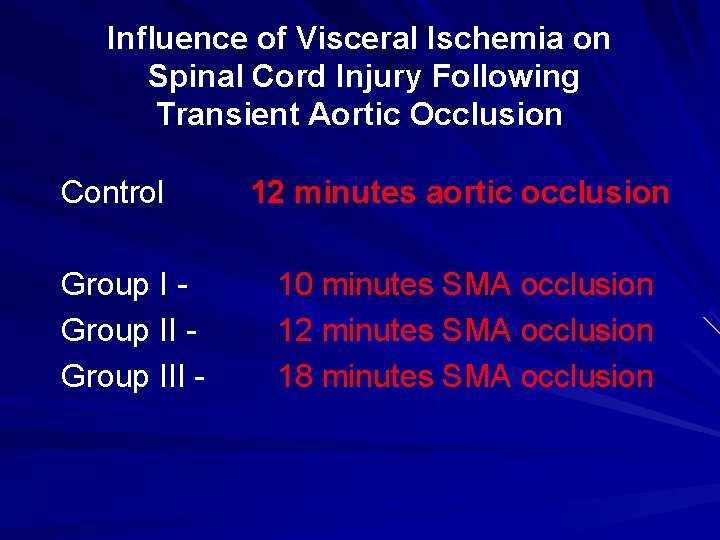
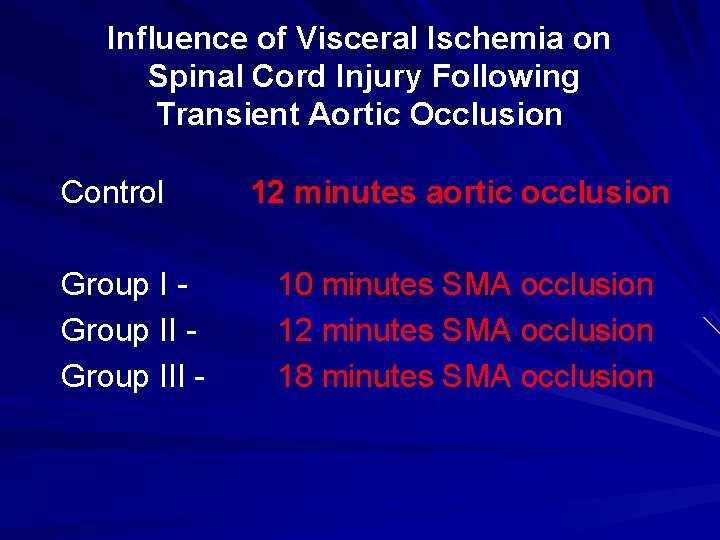
Influence of Visceral Ischemia on Spinal Cord Injury Following Transient Aortic Occlusion Control Group III - 12 minutes aortic occlusion 10 minutes SMA occlusion 12 minutes SMA occlusion 18 minutes SMA occlusion
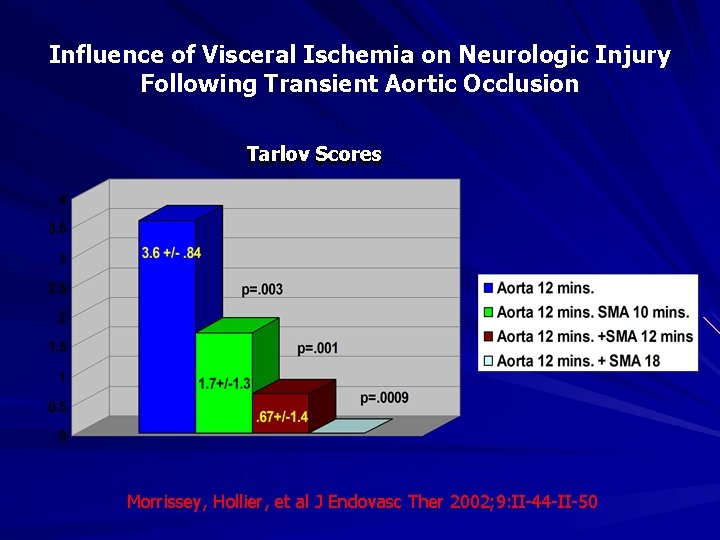
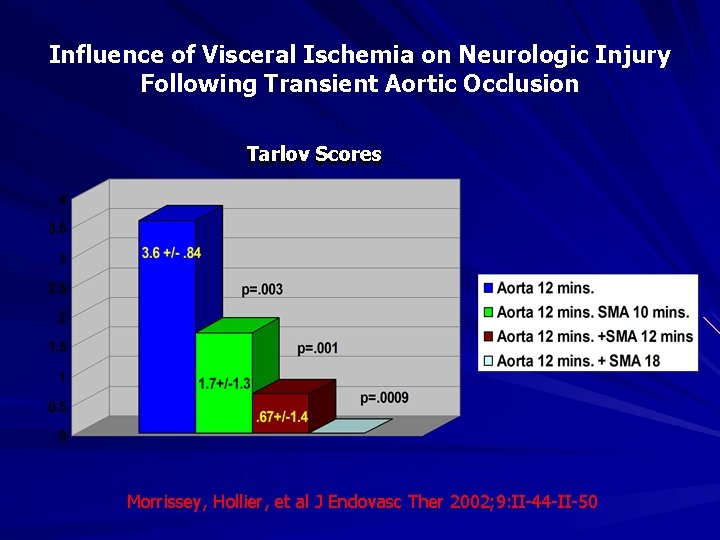
Influence of Visceral Ischemia on Neurologic Injury Following Transient Aortic Occlusion Tarlov Scores Morrissey, Hollier, et al J Endovasc Ther 2002; 9: II-44 -II-50
Thoracoabdominal Aortic Aneurysms Delayed-onset Paraplegia – Due to: Intermediate level of cord ischemia intraoperatively with progressive post-op cord edema and increasing CSF pressure Prolonged gut ischemia with intra-operative activation of cytokines and secondary spinal cord injury (apoptosis, direct cytokine injury, non-reflow phenomenon)
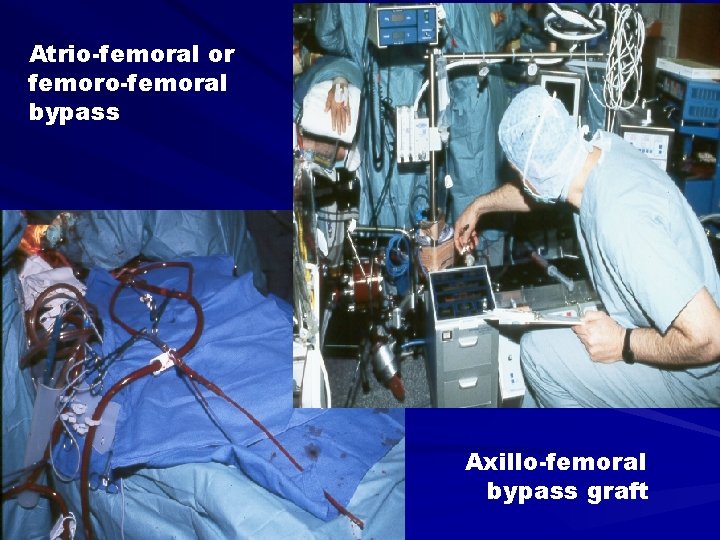
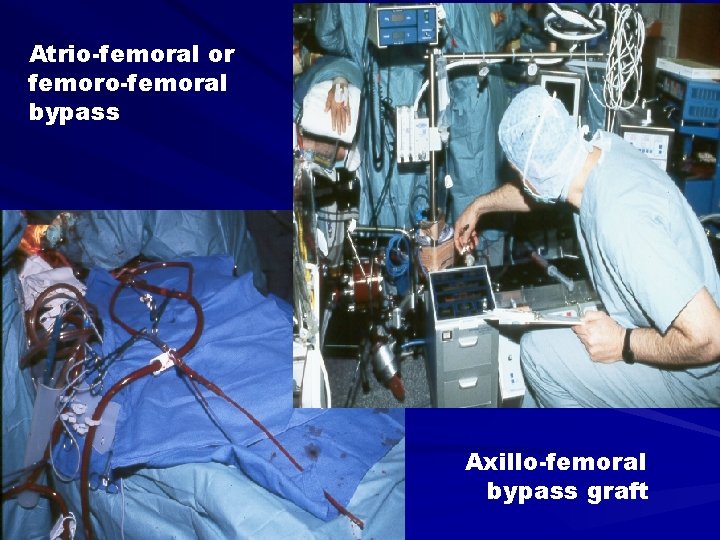
Atrio-femoral or femoro-femoral bypass Axillo-femoral bypass graft
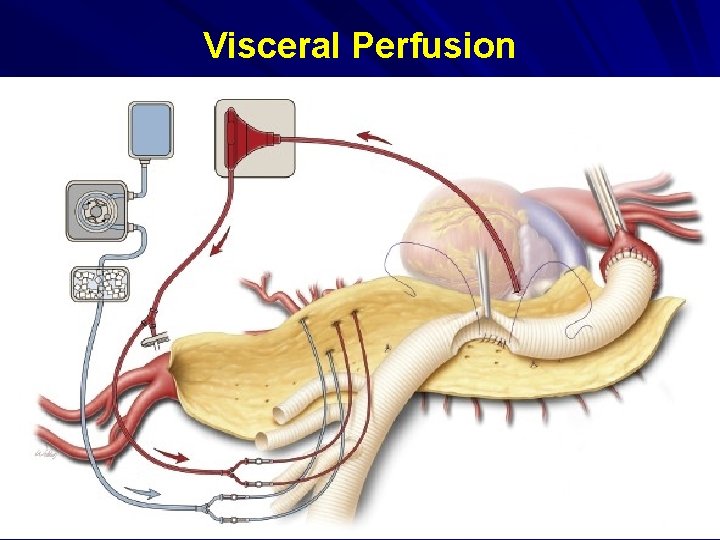
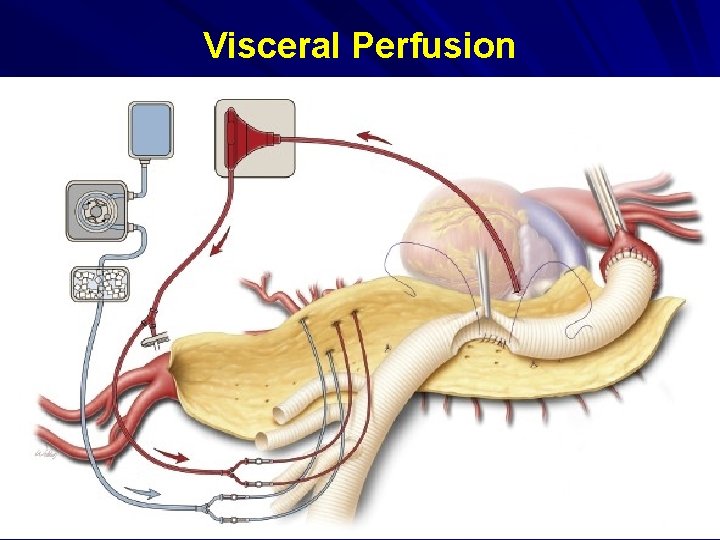
Visceral Perfusion

Visceral Perfusion
Thoracoabdominal Aortic Aneurysms Adjunctive Modalities ØSelective intercostal reimplantation ØCSF Drainage ØShunt or bypass ØMinimize visceral ischemia
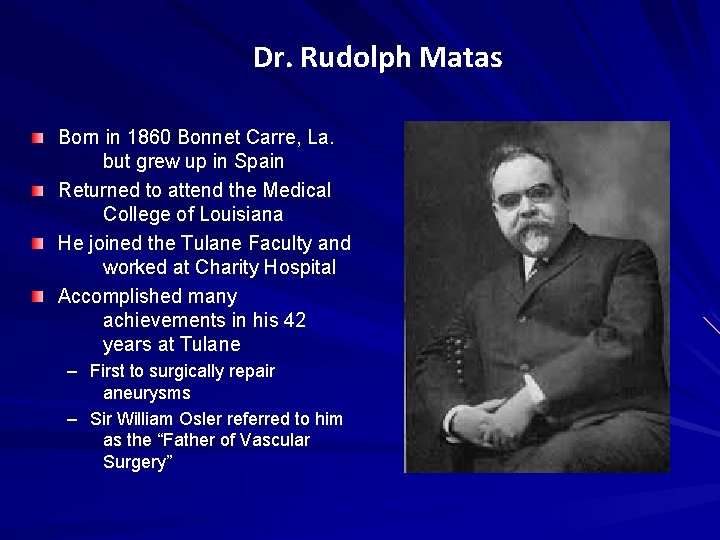
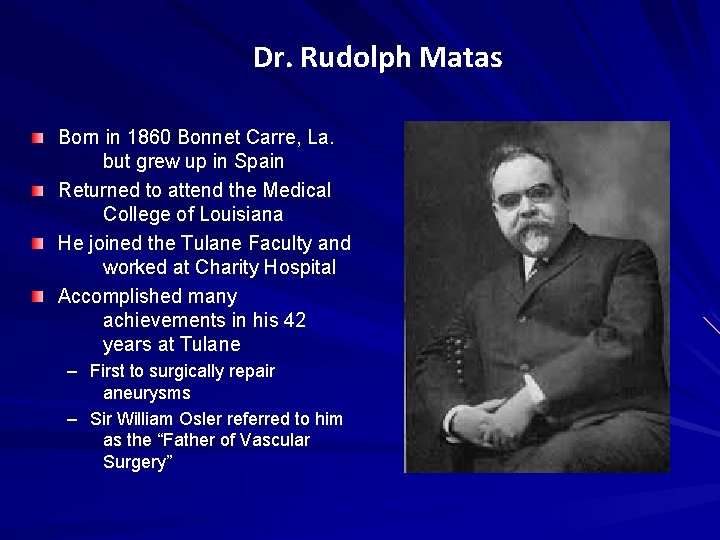
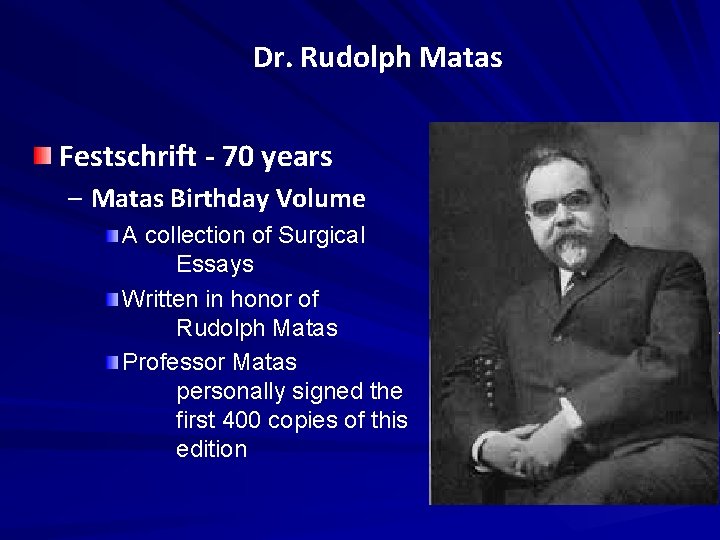
Dr. Rudolph Matas Born in 1860 Bonnet Carre, La. but grew up in Spain Returned to attend the Medical College of Louisiana He joined the Tulane Faculty and worked at Charity Hospital Accomplished many achievements in his 42 years at Tulane – First to surgically repair aneurysms – Sir William Osler referred to him as the “Father of Vascular Surgery”
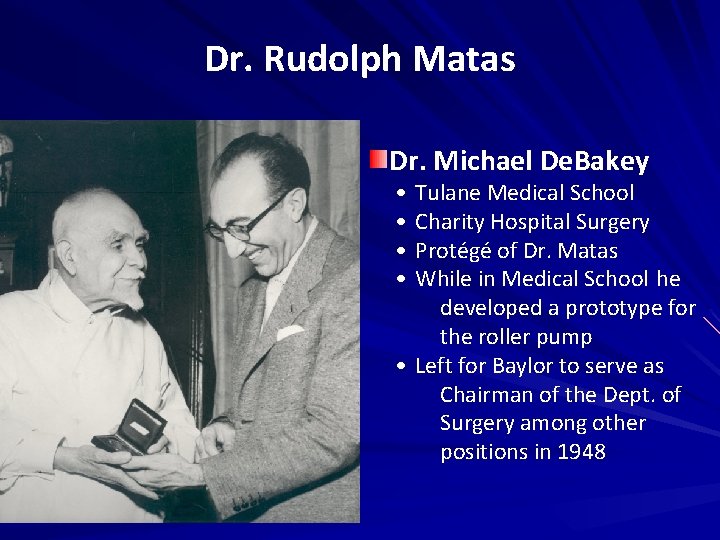
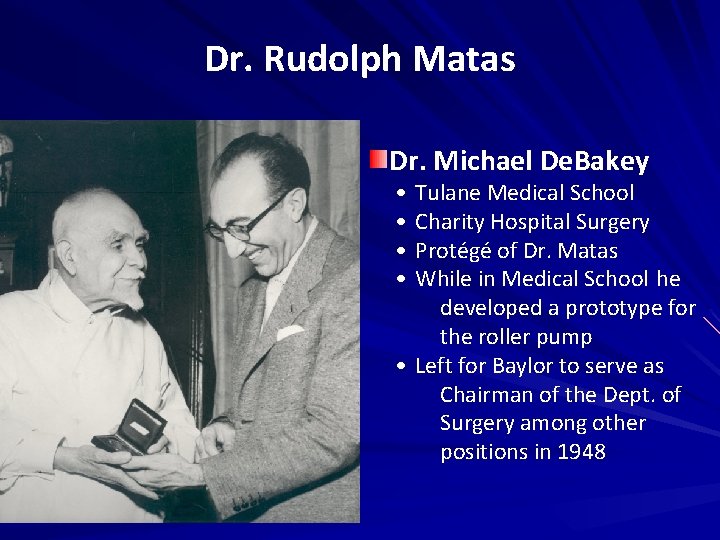
Dr. Rudolph Matas Dr. Michael De. Bakey • • Tulane Medical School Charity Hospital Surgery Protégé of Dr. Matas While in Medical School he developed a prototype for the roller pump • Left for Baylor to serve as Chairman of the Dept. of Surgery among other positions in 1948
Dr. Rudolph Matas Isidore Cohn, Sr. wrote a biography of Matas in 1960 and had a large collection of Matas’ papers Isidore Cohn, Jr. was my mentor and on his death, these papers were given to LSU Health Sciences Center
Dr. Rudolph Matas
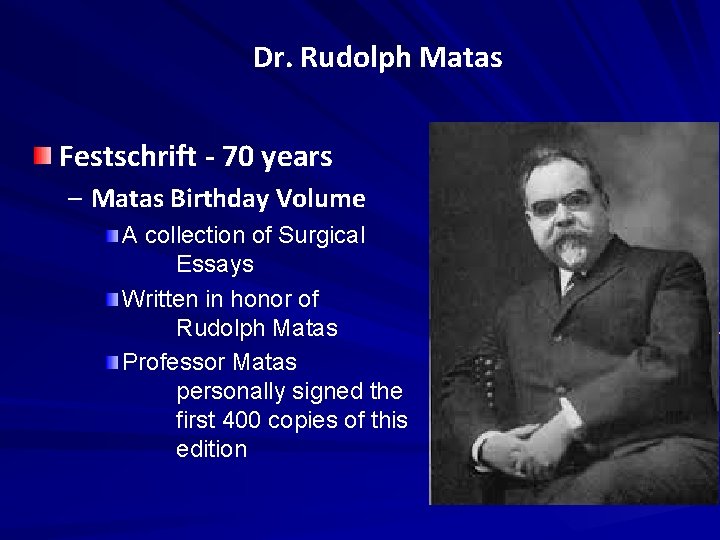
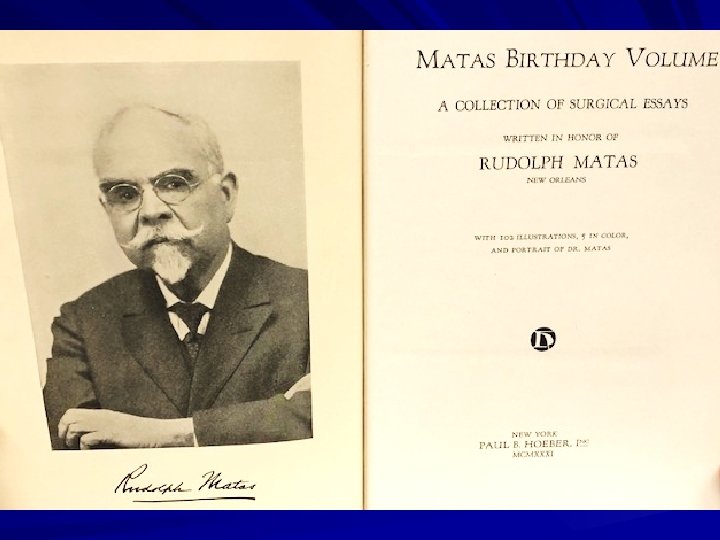
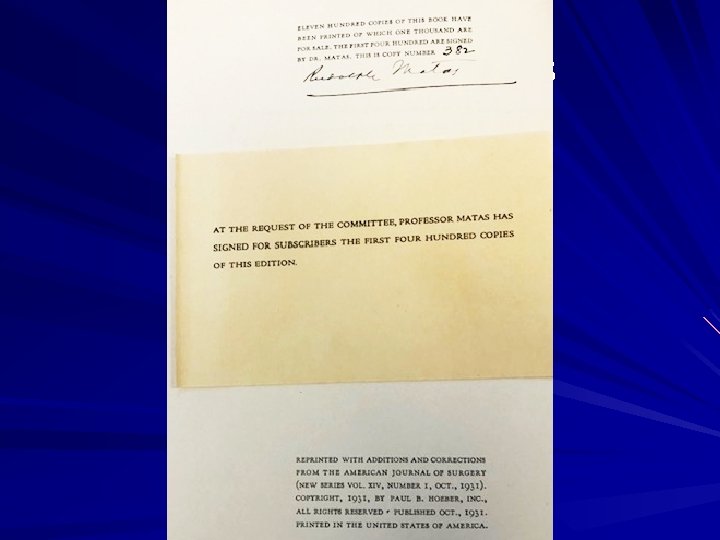
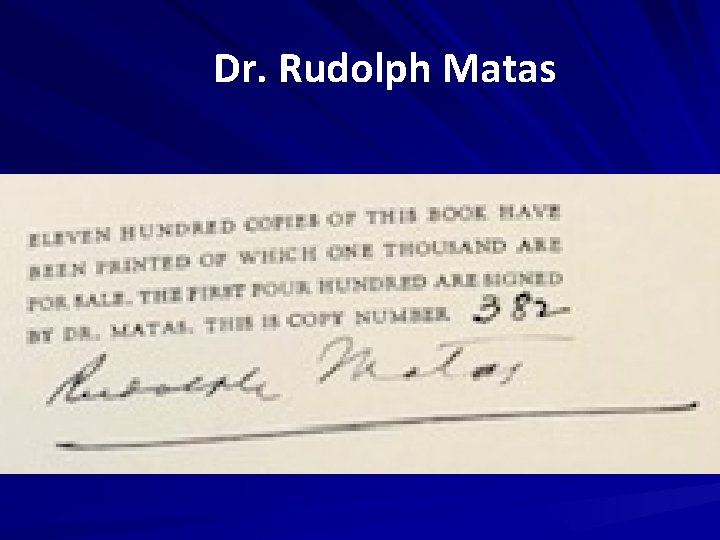
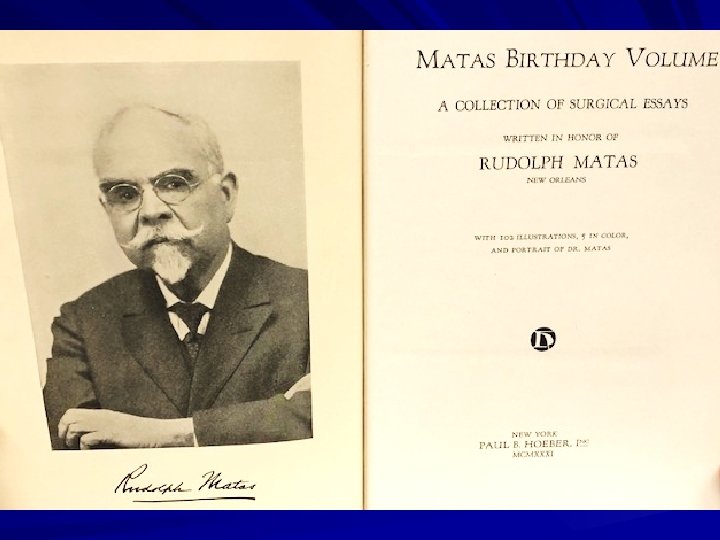
Dr. Rudolph Matas Festschrift - 70 years – Matas Birthday Volume A collection of Surgical Essays Written in honor of Rudolph Matas Professor Matas personally signed the first 400 copies of this edition
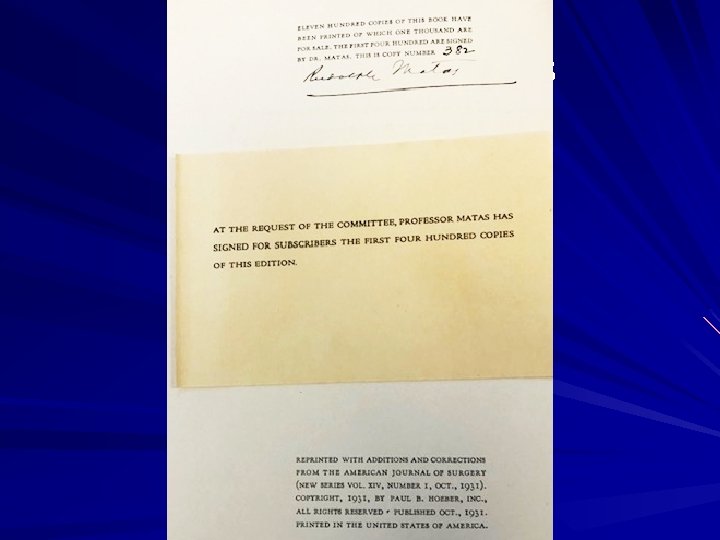
Dr. Rudolph Matas
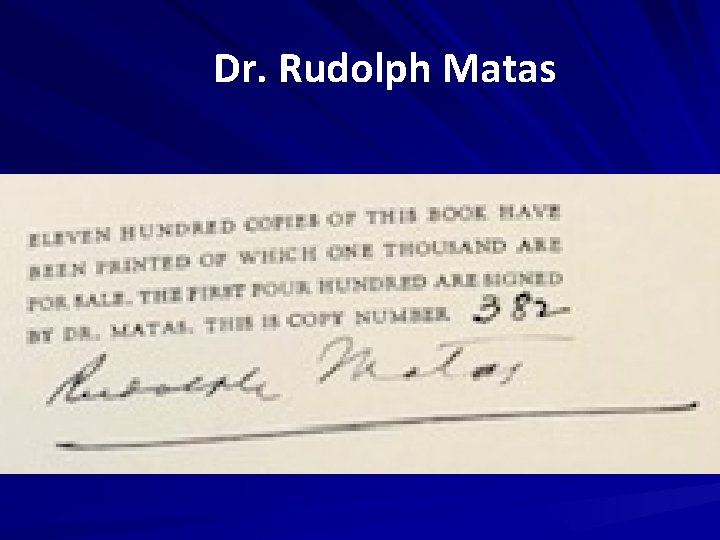
Dr. Rudolph Matas
Festschrift Dr. Hazim Safi Larry Hollier, MD, FACS, FACC, FRCS (Eng) Professor of Surgery and Chancellor LSU Health Sciences Center New Orleans, La
 Larry hollier md
Larry hollier md Mark hollier
Mark hollier Og'iz bo'shlig'ida ovqat hazm bo'lishi
Og'iz bo'shlig'ida ovqat hazm bo'lishi Facs
Facs Fluorescence-activated cell sorting (facs)
Fluorescence-activated cell sorting (facs) Facs
Facs Facs
Facs Measuring cup
Measuring cup Facs
Facs Justfacs
Justfacs Flow cytometria vizsgálat
Flow cytometria vizsgálat Classes of shock
Classes of shock Bu facs core
Bu facs core Food safety poster
Food safety poster Louay safi
Louay safi Louay safi
Louay safi Louay safi
Louay safi Cast metal restorations
Cast metal restorations Imad salamey
Imad salamey Rapport de stage ciment du maroc safi
Rapport de stage ciment du maroc safi Louay safi
Louay safi Cast metal restoration definition
Cast metal restoration definition Louay m. safi
Louay m. safi Louay safi
Louay safi Gsmh ve gsyih arasındaki fark nedir
Gsmh ve gsyih arasındaki fark nedir Safi furniture
Safi furniture Larry bridgesmith
Larry bridgesmith Utsa cs vdi
Utsa cs vdi Larry apke
Larry apke Larry frevert
Larry frevert I must have drunk four cups of cocoa
I must have drunk four cups of cocoa Larry winner
Larry winner Larry rubio
Larry rubio Larry lion alphafriend
Larry lion alphafriend Larry burkett budget percentages
Larry burkett budget percentages Larry's bad habit
Larry's bad habit