FERTILIZATION PREGNANCY AND BIRTH Fertilization Where Fallopian tube
FERTILIZATION, PREGNANCY AND BIRTH
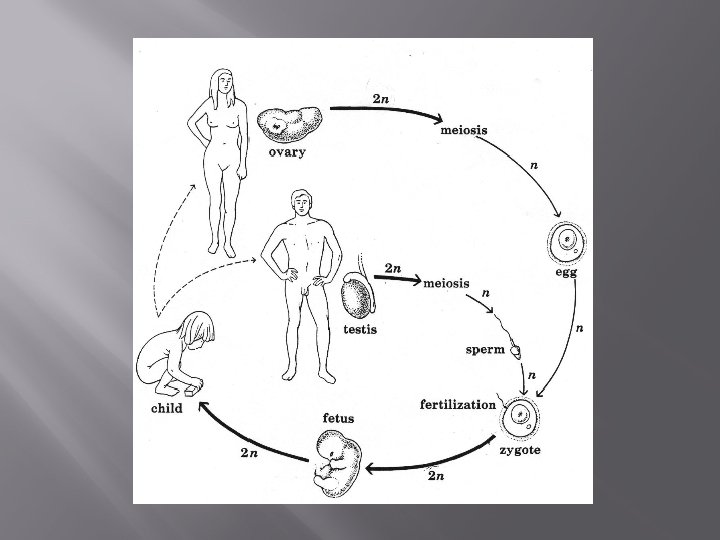

Fertilization � � Where? Fallopian tube What? Union of sperm and secondary oocyte Secondary oocyte completes development to become fertlized ovum (zygote) Zygote receives 23 chromosomes from each sex cell
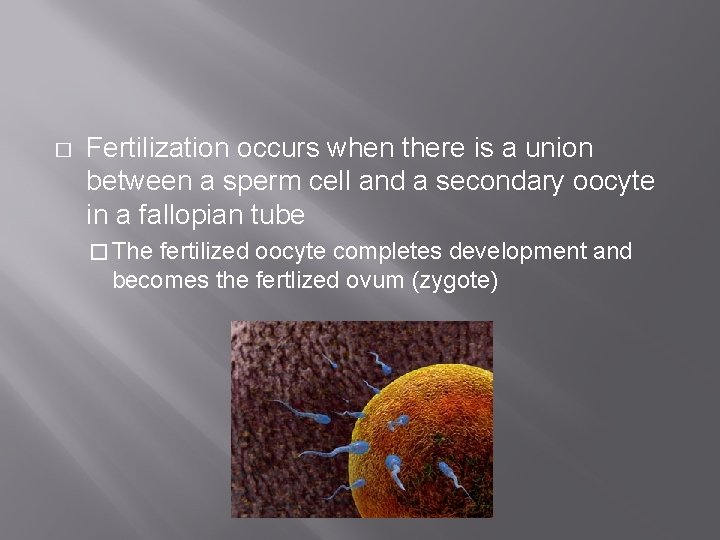
� Fertilization occurs when there is a union between a sperm cell and a secondary oocyte in a fallopian tube � The fertilized oocyte completes development and becomes the fertlized ovum (zygote)
� ~500 million sperm ejaculated during intercourse � 150 -300 million travel through cervix to uterus Only a few hundred reach the fallopian tube �Several sperm attach to outer edge of ovulated oocyte, only one sperm fuses with it

Preventing Polyspermy � Contact and fusion causes ion channels to open in the eggs plasma membrane � This allows sodium ions to flow into the egg � This alters the membrane potential (depolarization) � Occurs within 1 -3 seconds after sperm binds � Prevents additional sperm from fusing with the eggs plasma membrane
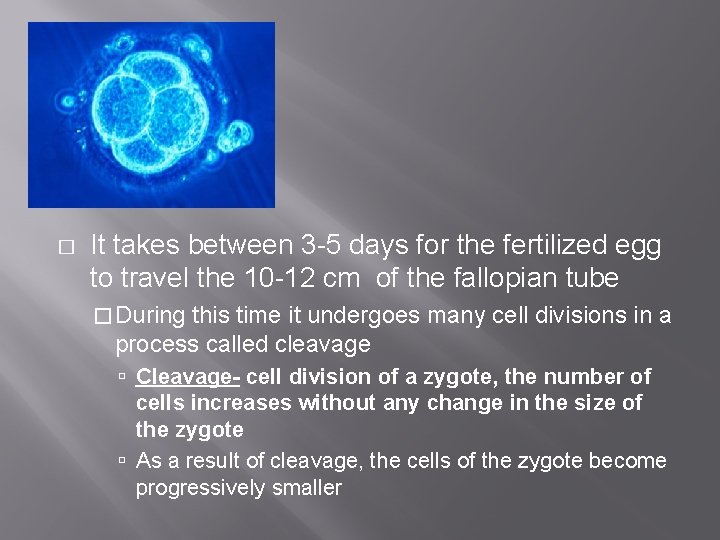
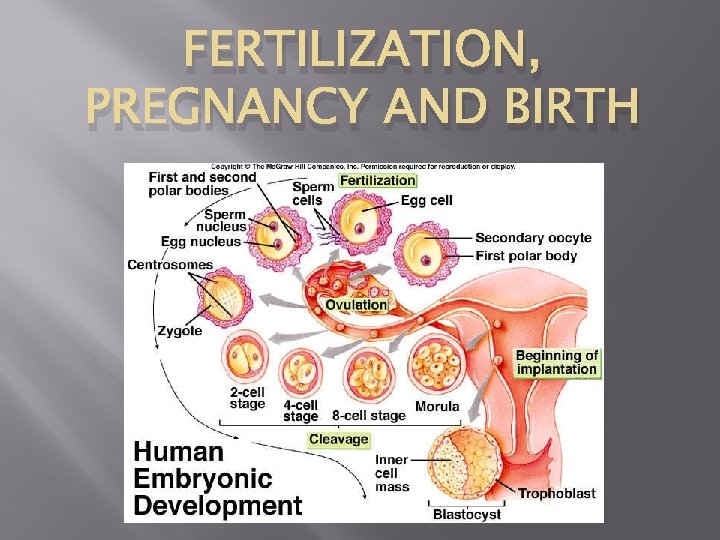
� It takes between 3 -5 days for the fertilized egg to travel the 10 -12 cm of the fallopian tube � During this time it undergoes many cell divisions in a process called cleavage Cleavage- cell division of a zygote, the number of cells increases without any change in the size of the zygote As a result of cleavage, the cells of the zygote become progressively smaller
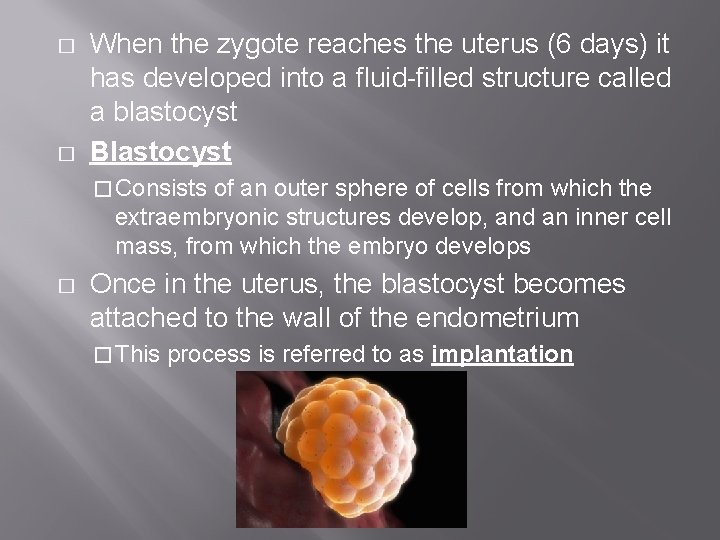
� � When the zygote reaches the uterus (6 days) it has developed into a fluid-filled structure called a blastocyst Blastocyst � Consists of an outer sphere of cells from which the extraembryonic structures develop, and an inner cell mass, from which the embryo develops � Once in the uterus, the blastocyst becomes attached to the wall of the endometrium � This process is referred to as implantation
� 4 days after fertilization, zygote becomes an embryo � After the 8 th week of pregnancy the zygote is referred to as a fetus � For the pregnancy to continue, menstruation cannot occur �A shedding of the endometrium would expel the embryo from the uterus
Changes to Accomodate Pregnancy � The problem: � Estrogen and progesterone must remain high to prevent menstruation � High levels of these hormones have a negative feedback effect on the secretion of gonadotropic hormones LH levels must remain high to sustain the corpus luteum If the corpus luteum deteriorates, the levels of estrogen and progesterone drop which stimulates uterine contractions and endometrium shedding
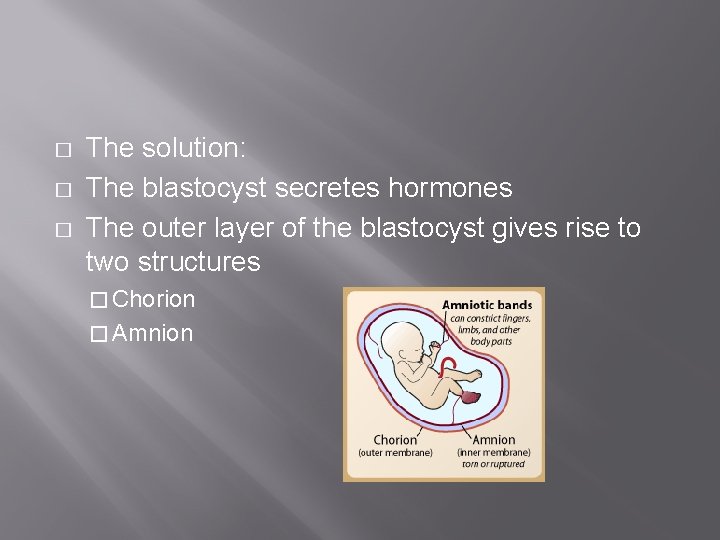
� � � The solution: The blastocyst secretes hormones The outer layer of the blastocyst gives rise to two structures � Chorion � Amnion
� Chorion � Produces human chorionic gonadotropic hormone (h. CG) � This hormone maintains the corpus luteum for the first 3 months of pregnancy � Corpus luteum continues to produce progesterone and estrogen which maintains the endometrium � h. CG levels in the urine indicates pregnancy � Amnion � Fluid filled extraembryonic structure
Amniotes � � Embryos of birds, reptiles and mammals develop in a fluid-filled sac in a shell or the uterus Organisms with these adaptations are called amniotes
� During amniote development, 4 extraembryonic membranes form around the embryo � chorion : functions in gas exchange � amnion: encloses the amniotic fluid � yolk sac : encloses the yolk � allantois: disposes of waste products and contributes to gas exchange
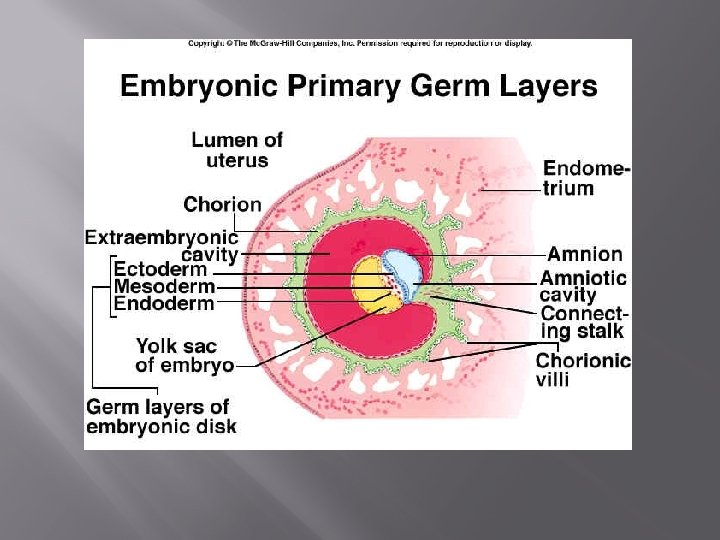
� Between the amnion and the fetus is the amniotic cavity � It is a fluid filled sac that insulates the embryo, and later the fetus, protecting it from infection, dehydration, impact and changes in temperature
� � The extraembryonic coelum is a fluid filled space between the amnion and chorion By the second week of the pregnancy, the yolk sac forms beneath the embryo (there is no yolk) � This is the site of early red blood cell formation � Later contributes to the primitive digestive tract
� Cells from the embryo and endometrium combine to form the placenta � It allows for the exchange of materials between mother and embryo � At four months it starts to produce estrogen and progesterone � The secretion of progesterone from the placenta prevents ovulation (can’t get pregnant while pregnant)
� The placenta is richly supplied with blood vessels � Projections called chorionic villi ensure that there a large number of blood vessels from the fetus that are exposed to maternal blood
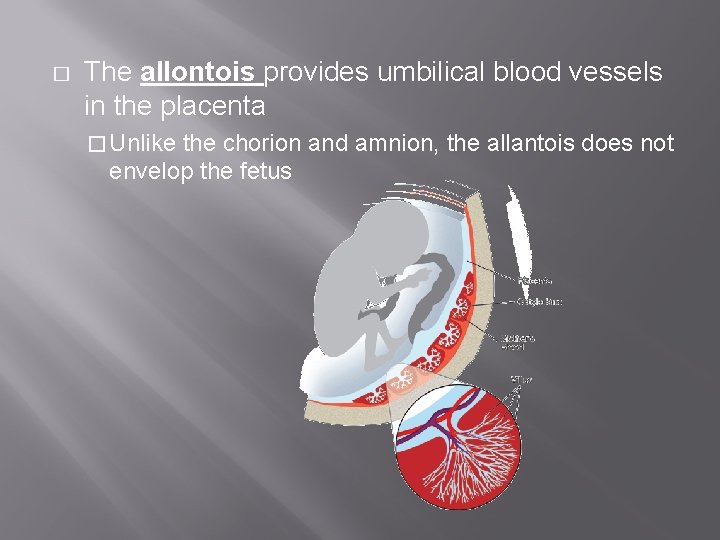
� The allontois provides umbilical blood vessels in the placenta � Unlike the chorion and amnion, the allantois does not envelop the fetus
� The placenta provides an interface for exchange between mother and fetus � Nutrients and oxygen diffuse from the mother’s blood into the blood of the developing fetus � Wastes move from the fetus to the mother � The umbilical cord connects the embryo with the placenta
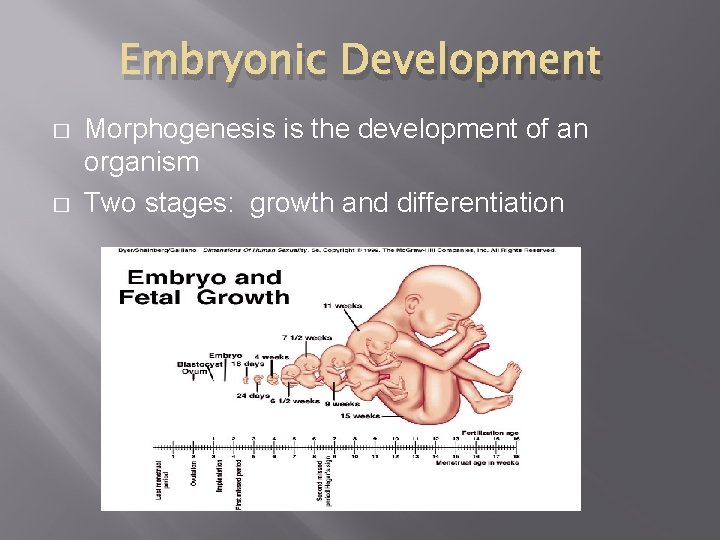
Embryonic Development � � Morphogenesis is the development of an organism Two stages: growth and differentiation
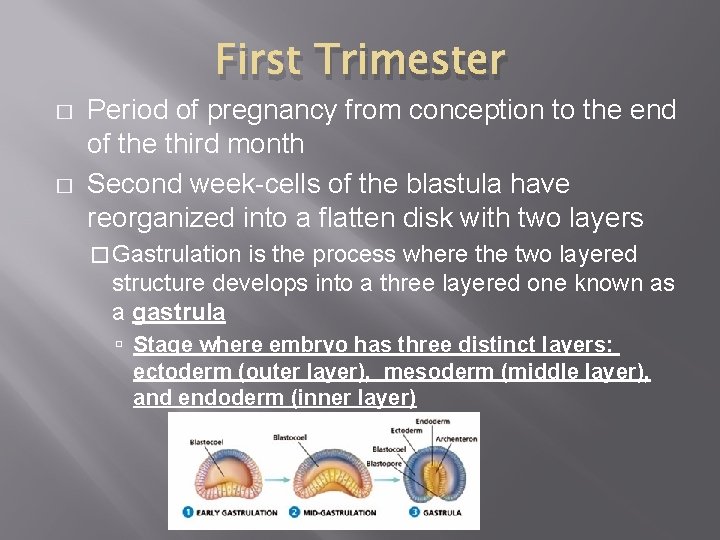
First Trimester � � Period of pregnancy from conception to the end of the third month Second week-cells of the blastula have reorganized into a flatten disk with two layers � Gastrulation is the process where the two layered structure develops into a three layered one known as a gastrula Stage where embryo has three distinct layers: ectoderm (outer layer), mesoderm (middle layer), and endoderm (inner layer)
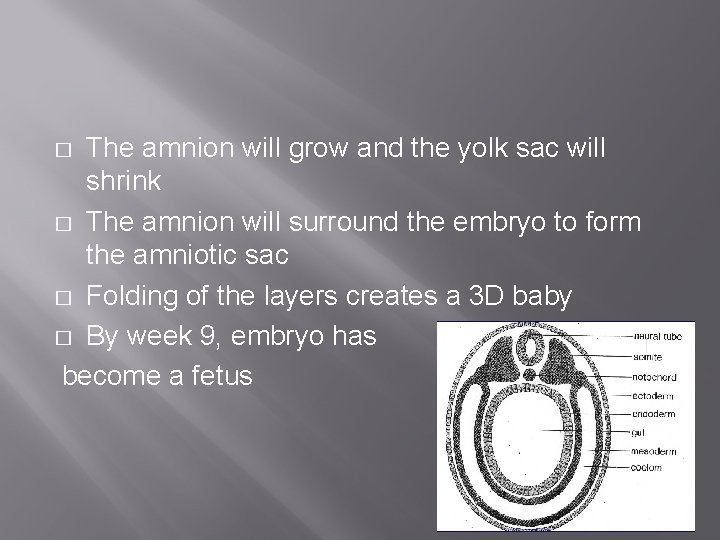
The amnion will grow and the yolk sac will shrink � The amnion will surround the embryo to form the amniotic sac � Folding of the layers creates a 3 D baby � By week 9, embryo has become a fetus �
Second Trimester � � Period of rapid growth! Organ systems mature Movements become strong and more frequent Baby turns head down due to gravity Third Trimester � � Muscle tone develops from moving Eyelids begin opening
Sex Determination � � � 1987 researchers located the sex determination gene on the Y chromosome SRY (Sex-determining region of the Y chromosome) is the gene mostly responsible for the male phenotype in humans In presence of SRY gene, in the 7 th week the developing gonads become testis � Testis direct subsequent male development
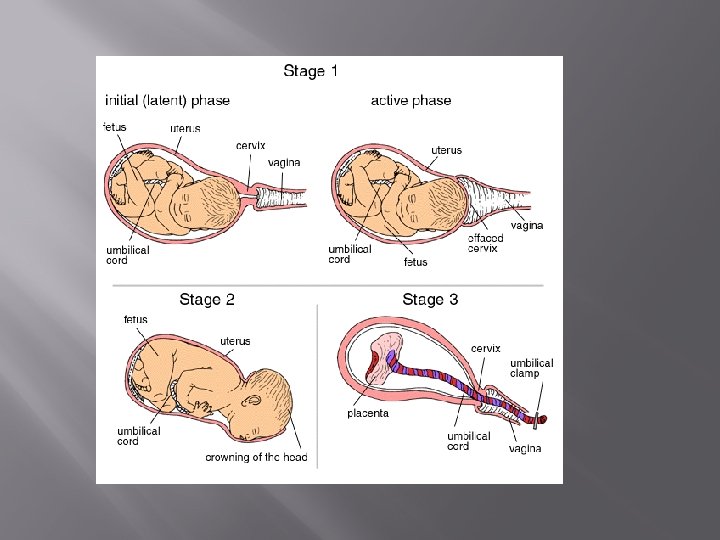
Birth � � ~ 266 days after implantation uterine contractions start Cervix thins and dilates Amnion is forced through birth canal, rupturing, acting as a lubricant Uterine contractions move the baby through the birth canal
Birth � Relaxin � Secreted by the placenta prior to labour causes pelvic muscles and ligaments to loosen and cervix to soften � Oxytocin � Secreted from the pituitary causes uterine contractions
Lactation � � � During pregnancy: Elevated levels of estrogen and progesterone prepare the breast for milk production Each breast � Contain 20 lobes of glandular tissue Each supplied with a duct that carries fluid towards the nipple
Hormones controlling lactation � Prolactin � Hormone secreted from the pituitary gland � Stimulates the glands in breast to produce fluids � � � Estrogen and progesterone drop after birth, lowering prolactin, but increases prolactin activity because the progesterone-induced inhibition is relieved Initially produces colostrum; substance resembling milk but contains no milk fat Few days after birth prolactin stimulates the production of breast milk
� � Milk produced in glandular tissue must be forced into the milk ducts Suckling from newborn stimulates nerve endings in the areola Sensory nerves carry information to the pituitary gland, causing the relase of oxytocin Oxytocin causes weak smooth muscle contractions in the breast forcing milk into the ducts
- Slides: 33