Fertility and the management of scrotal injury Jackson

- Slides: 11
Fertility and the management of scrotal injury Jackson Kirkman-Brown Science Lead & Hon Reader BWH & Uo. B
Background • Mid 2009 soldier, having spoken to a friend who was a GP, asked for sperm storage • @2 months post injury - total orchidectomy • no sperm present 2 2
Three main challenges? • Improvement of patient-specific treatment – including in the field – evolution and validation of techniques • ID and reduction of threat injury poses to fertility • Increase safe and effective fertility options
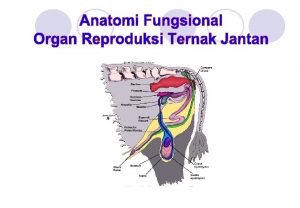
• What currently happens in Birmingham – Contact when signal arrives (18 -24 h before) – Team prepare for case – Medical review / request – Procedure (generally) on 1 st theatre visit • The procedure – Retrieval by Urologist of: • vas deferens • epididymal tissue

Observed original patterns of blast injury to the testis Level of injury Description % A Loss of gonad to ext. ring 25 B Head of epididymis spared 30 C Head and body of epididymis and upper pole testis spared 10 B D Lower pole testis + epididymal tail loss 5 C E Scrotal skin laceration 20 F Scrotal contusion only 10 A D F E
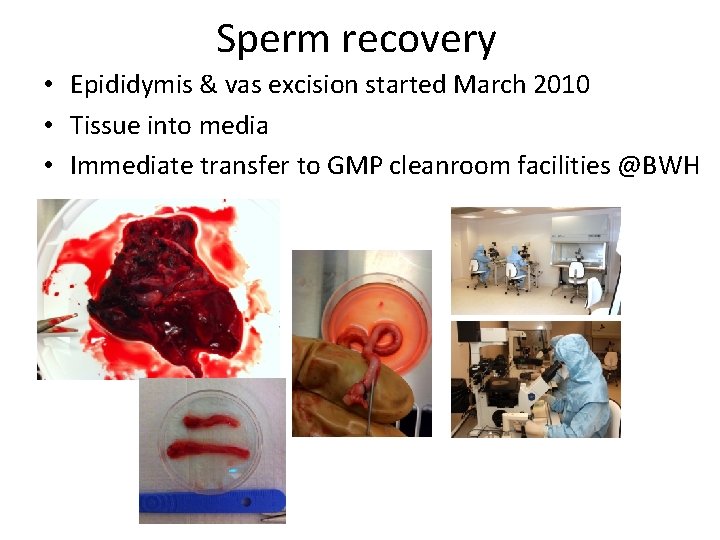
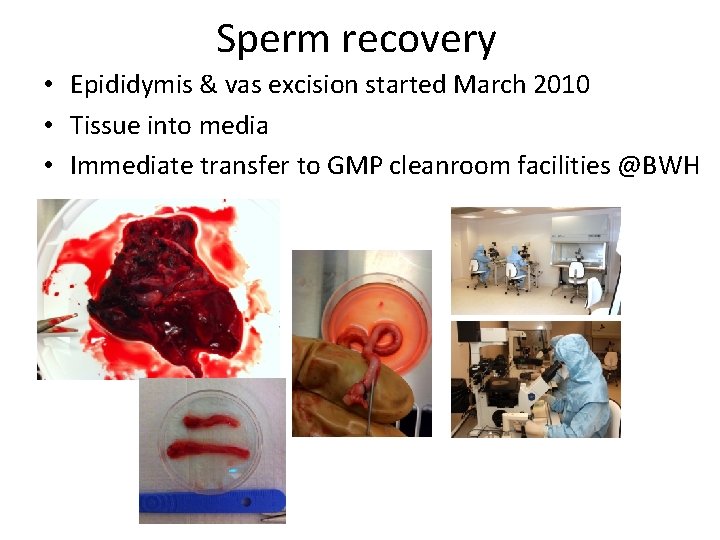
Sperm recovery • Epididymis & vas excision started March 2010 • Tissue into media • Immediate transfer to GMP cleanroom facilities @BWH
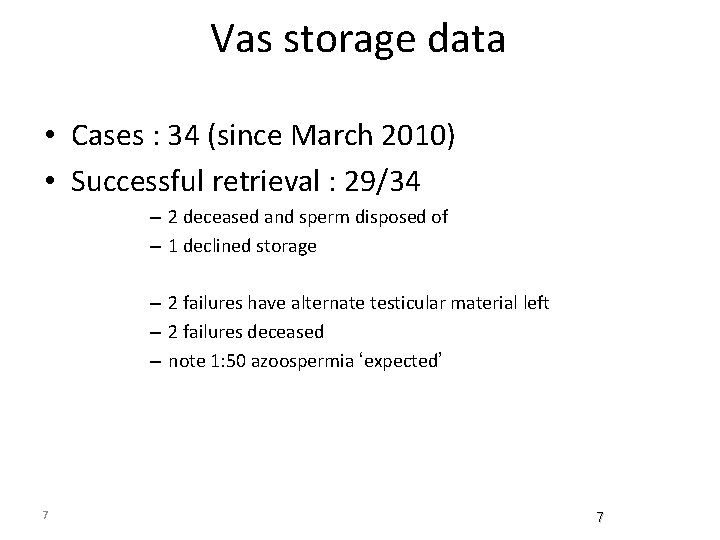
Vas storage data • Cases : 34 (since March 2010) • Successful retrieval : 29/34 – 2 deceased and sperm disposed of – 1 declined storage – 2 failures have alternate testicular material left – 2 failures deceased – note 1: 50 azoospermia ‘expected’ 7 7
So what does this currently mean for an individual in the future? ? • Treatments using intra-cytoplasmic sperm injection • Future re-checks? • No sperm available for storage = support and other treatment options
Successes • Ongoing – Patients positive about system – Systems now established and in place – Number of those with sperm banked are currently seeking treatment – Two couples have ongoing pregnancies
The future • Pelvic protection has had huge effect in reducing the number of testicular losses and the severity • Understand the short and long-term effects of blast to the testis • Blast with fragmentation / rupture • Blast without rupture • Can we further evolve protection • Ongoing androgenic and spermatogenic function
Thank you This is a real interdisciplinary team effort, key colleagues: Wendy Ross, Michelle Jewell, Yongjian Chen, Ingride Krasauskaite and BWFC Team Dr Sue Avery & James Lawford-Davies John Clark, Vic Long, Steve Jeffrey, Ian Sargeant Military Burns & Plastics team; Sir Keith Porter Uh. B Urology Team especially Richard Viney; Steve Cumley & Uh. B management Davendra Sharma, David Woods, Peter Wink, Rhodri Phillip, Wendy Frappell-Cooke Wendy Williams, Richard Broadbridge, Jo Palmer