Female Sexual Anatomy Boys have a Penis And
Female Sexual Anatomy
Boys have a Penis… And girls have…? • What questions do you have about male or female anatomy? (write down & hand in)
Click here… An important difference between the clitoris and the penis is that the clitoris A. Cannot undergo erection B. Has no functions other than sexual pleasure C. Has no cover that is equivalent to the foreskin of the penis D. Has relatively few nerve endings compared to the penis
Click here… Women A. After experiencing the refractory period can once again achieve orgasm. B. Experience multiple orgasms regularly. C. Are physiologically able to be orgasmic immediately after orgasm. D. Must achieve orgasm to fell emotionally satisfied and fulfilled.
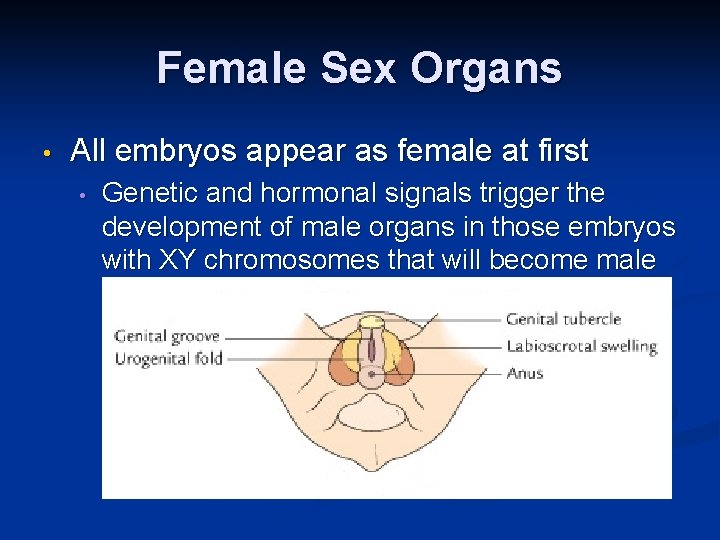
Female Sex Organs • All embryos appear as female at first • Genetic and hormonal signals trigger the development of male organs in those embryos with XY chromosomes that will become male
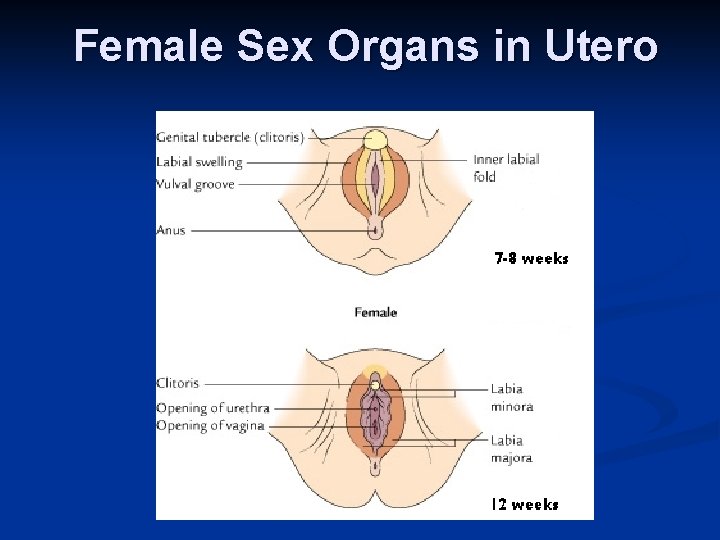
Female Sex Organs in Utero
Female Sex Organs • In spite of all that is known about female sex organs, some anatomical questions remain unknown or disputed • • • Range in clitoral size Existence and function of the G-spot Placement of nerves in the pelvic cavity
Female Sex Organs • • Sex organs serve a reproductive function Also serve other functions: • • Bringing pleasure to self Giving pleasure to others May serve to attract potential sexual partners Sharing of genital sexuality can play a bonding role in relationships
External Structures • External female genitals: • • • mons pubis clitoris labia majora labia minora These genitals are collectively known as the vulva • Often referred to as “vagina, ” yet the vagina is an internal structure
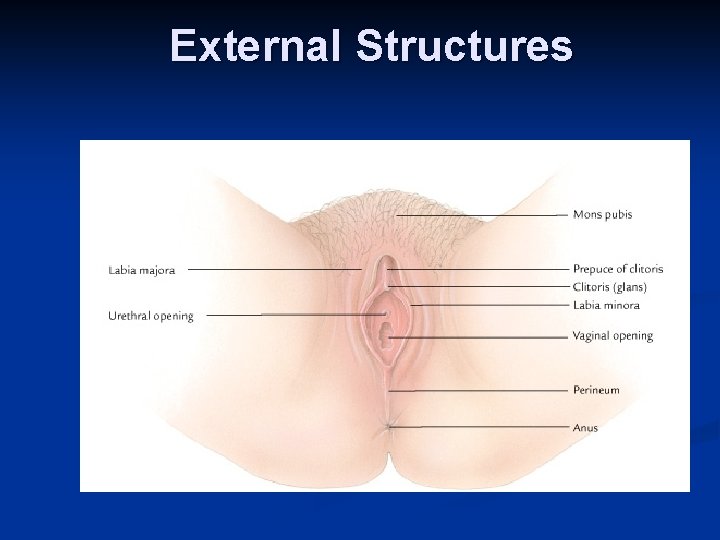
External Structures
Mons Pubis • Latin for “pubic mound: ” • • The pad of fatty tissue that covers the area of the pubic bone about 6” below navel. Pubic hair grows on mons pubis beginning in puberty In many women, this area is sensitive to stimulation Also called mons veneris
Clitoris • The Clitoris is the center of sexual arousal in the female • • Contains a high concentration of nerve endings Exquisitely sensitive to stimulation • • • glans clitoris: the shaft of the clitoris Clitoral hood: covers glans when clitoris not engorged Structurally analogous to penis, though sole function of the clitoris is sexual arousal, primarily via indirect stimulation
Clitoris • Clitoris also has an internal structure • • • Two 3. 5” long branches called crura contain two corpora cavernosa: hollow chambers that fill with blood and swell during arousal The clitoris when stimulated • • Enlarges initially, then retracts beneath hood just before and during orgasm Follows same pattern with repeated orgasms, though swelling is less pronounced
Labia Majora and Minora • Labia Majora – “outer lips” n Two folds of spongy flesh extending from the mons pubis to the perineum and enclosing the labia minora, clitoris, urethral opening, and vaginal entrance n Outer: covered with pubic hair; pigmented n Inner: hairless; oil glands • Engorge with blood if excited
Labia Majora and Minora • Labia Minora • • • Small folds within the labia majora that meet above the clitoris to form the clitoral hood No hair, many oil glands; darken if sexually aroused They vary in appearance from woman to woman They are sensitive to the touch and swell during sexual arousal They enclose the “vestibule: ” the vaginal opening
External genitals during sexual arousal • • Clitoris becomes erect Labia minora widen Vestibule (vaginal opening) becomes visible Bartholin’s glans (located in the vestibule) secrete small amount of moisture

Internal Structures • • Vagina: from Latin word for sheath 4 inch, thin-walled accordion-like tube from the introitus to the cervix, tilted back; organ of intercourse and canal for menses and babies; lubricant secreted from vaginal wall openings when engorged; first 1/3 contains many nerve endings, inner 2/3 has little nerves
Internal Structures • Two reproductive functions of vagina • • • Introitus: the lower third of the vagina • • Encompasses penis during coitus (vaginal intercourse) Birth canal The majority of the vagina’s nerve endings are there Hymen: named for Roman god of marriage • a thin membrane that partially covers introitus prior to first intercourse or other insertion

Internal Structures
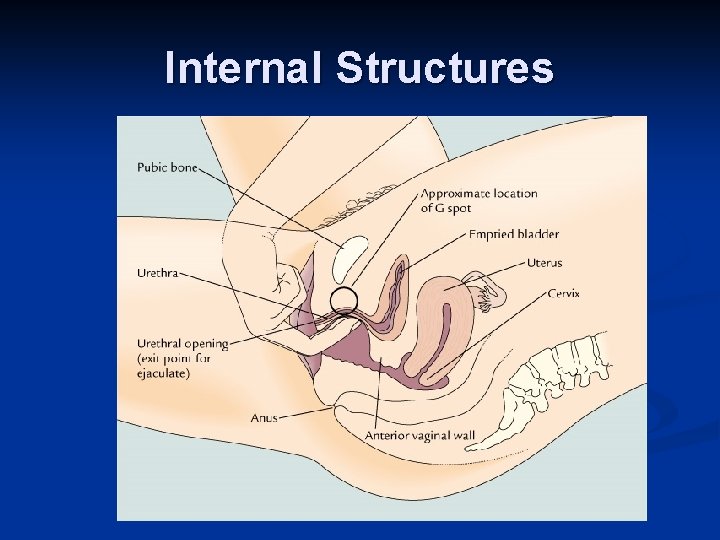
Internal Structures • Grafenberg Spot (G-spot) • • • An erotically sensitive area on front wall of the vagina mid-way between pubic bone and cervix Existence somewhat controversial Female ejaculation – powerful orgasms and expulsion of fluid (up to 4 ounces) due to stimulation of the G-spot in some women; may be Skene’s glands fluid

Internal Structures • Uterus: a hollow, thick-walled (1 -inch) muscular organ between bladder & rectum • • • Accommodates developing fetus during pregnancy Only 3” by 3” in women who have not given birth Inner lining of uterine walls known as endometrium Contractions to expel menses and fetus Cervix: the tapered end of the uterus, extends and opens into the vagina • • Secretes mucous to help or impede sperm, depending on the monthly cycle; menstrual fluid travels through Os – opening leading into the uterus
Internal Structures
Internal Structures • Ovaries: gonads that produce gametes • • Produce egg cells (oocytes; ova) for reproduction (250, 000 ova each) Two ovaries; size and shape of large almonds Ovaries release oocytes in a process called ovulation Fallopian tubes: • • • Also known as uterine tubes of oviducts One tube extends toward each ovary They fan over the ovaries, and carry oocytes into the uterus during ovulation

Figure 5. 3 The female internal reproductive system (side view).
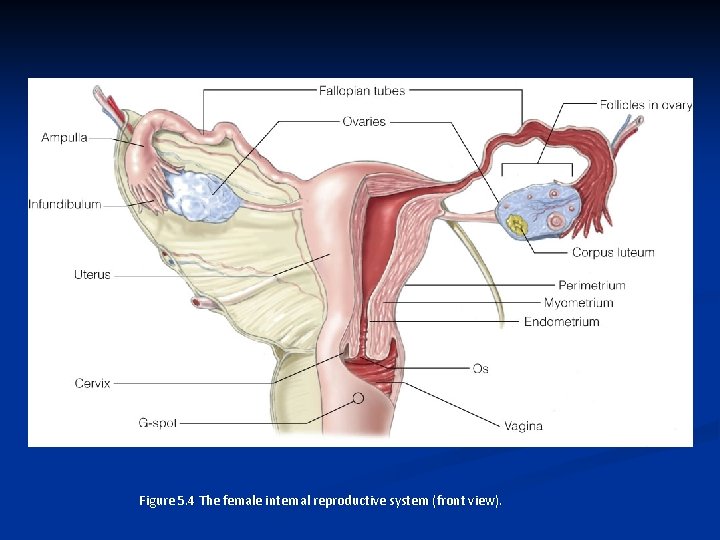
Figure 5. 4 The female internal reproductive system (front view).
Other Structures • • Urethra: tube through which urine passes Urethral opening Perineum: area between genitals and anus Pelvic floor
Other Structures • Anus: opening of rectum • • • Contains two sphincters (circular muscles that open and close like valves) Some women and men find that the tissue of the anus is erotically sensitive The lining of the rectum is fragile • if engaging in anal sex play care must be taken not to rupture the delicate tissues
Other Structures • Breasts: both women and men have them • • • Reproductive function of female breasts is to nourish offspring through lactation Composed of fatty tissue and 15 -25 lobes that radiate around a central nipple Areola: the ring of darkened skin around nipple Nipples get erect in response to touch, cold, or sexual arousal Many (not all) women find breast stimulation pleasurable.
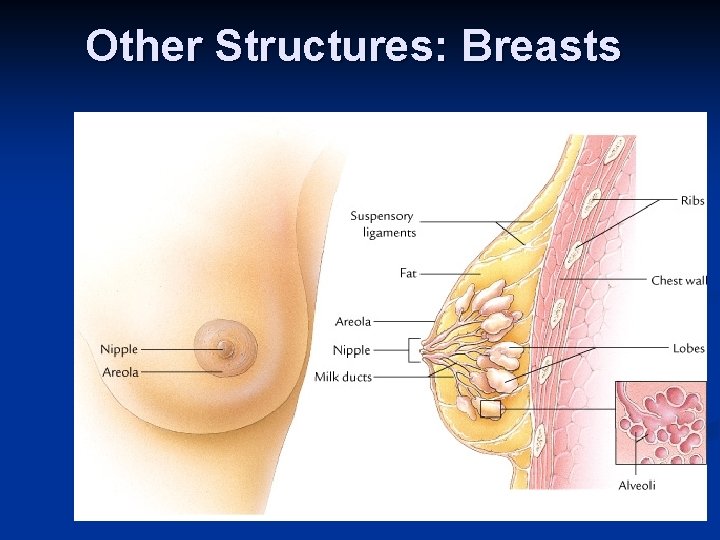
Other Structures: Breasts
Other Sex Organs Skin, lips, ears, back of knee, armpit, base of neck, brain n Any area can be arousing depending on the type of stimulation and the perceptions of the recipient n

Female Puberty n n n Begins anywhere from 8 to 15 years of age Earlier onset of menstruation may be due to being overweight; can vary with race Puberty lasts about 3 to 5 years Begins when pituitary gland initiates release of FSH and LH, which increases the ovaries production of estrogen Increased size of Fallopian tubes, uterus, vagina, breasts, buttocks, thighs
Female Puberty (Cont. ) Pelvis widens n Pubic hair grows n During puberty (usually 11 or 12 years), ovulation commences n Menarche occurs during this time as well, although it may be a few months before or after ovulation begins n

Female Sexual Physiology: Reproductive Hormones • Hormones: chemical substances that serve as messengers • Gonadotropins act directly on gonads • • Estrogens: affect maturation of reproductive organs, menstruation, and pregnancy Progesterone: helps maintain the uterine lining
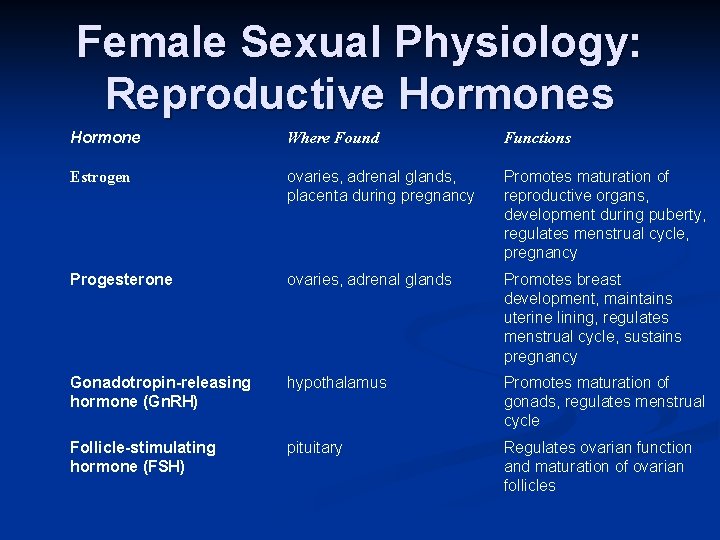
Female Sexual Physiology: Reproductive Hormones Hormone Where Found Functions Estrogen ovaries, adrenal glands, placenta during pregnancy Promotes maturation of reproductive organs, development during puberty, regulates menstrual cycle, pregnancy Progesterone ovaries, adrenal glands Promotes breast development, maintains uterine lining, regulates menstrual cycle, sustains pregnancy Gonadotropin-releasing hormone (Gn. RH) hypothalamus Promotes maturation of gonads, regulates menstrual cycle Follicle-stimulating hormone (FSH) pituitary Regulates ovarian function and maturation of ovarian follicles

Female Sexual Physiology: Reproductive Hormones Hormone Where Found Functions Luteinizing hormone (LH) pituitary Assists in production of estrogen and progesterone, regulates maturation of ovarian follicles, triggers ovulation Human chorionic gonadotropin (HCG) embryo and placenta Helps sustain pregnancy Testosterone adrenal glands and ovaries Helps stimulate sexual interest Oxytocin hypothalamus stimulates uterine contractions in childbirth Prolactin pituitary stimulates milk production Prostaglandins all body cells mediate hormone response, stimulate muscle contractions

Menstruation n Uterine lining is shed if no pregnancy; tissue and blood exit the introitus

Figure 5. 7 The ovarian and menstrual cycles.

The Ovarian Cycle • 3 Phases: • Follicular phase: Days 1 -10 • • Ovulatory phase: Days 11 -14 • • Hormones signal 10 to 20 follicles to grow on ovaries; Estrogen matures one oocyte Oocyte undergoes cell division; Follicle wall thins and ruptures; oocyte enters abdominal cavity near fimbrae of fallopian tube Luteal phase: Days 14 -28 • Estrogen levels drop; egg travels through fallopian tube towards uterus

The Ovarian Cycle
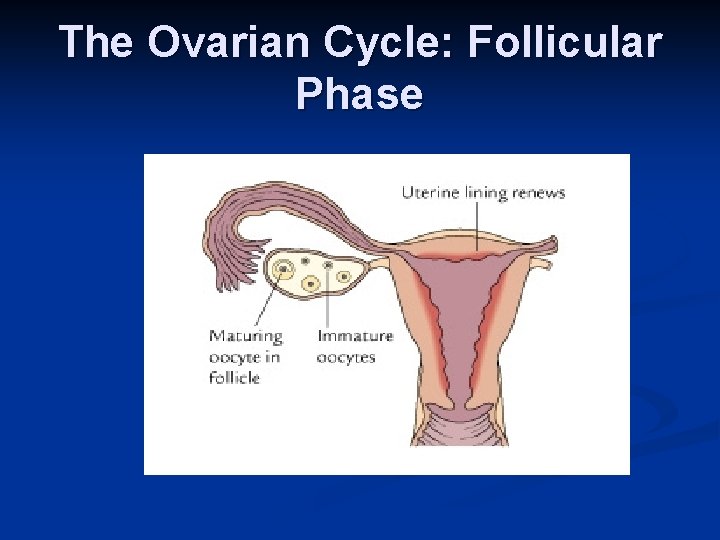
The Ovarian Cycle: Follicular Phase
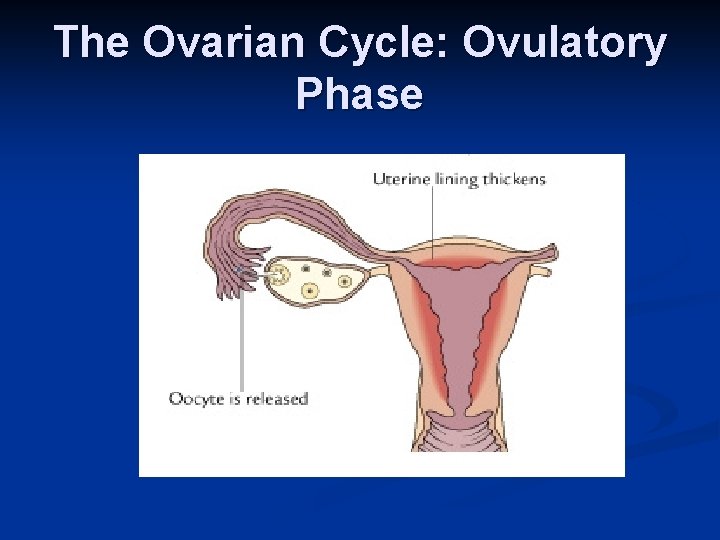
The Ovarian Cycle: Ovulatory Phase
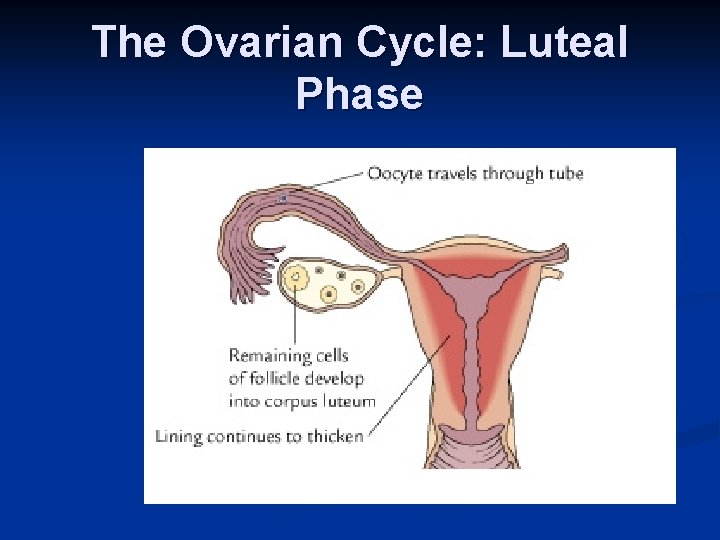
The Ovarian Cycle: Luteal Phase
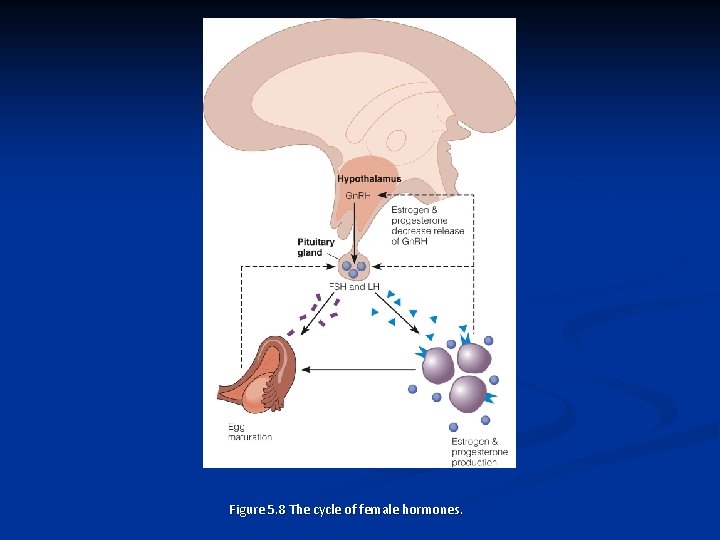
Figure 5. 8 The cycle of female hormones.

Menstruation

The Menstrual Cycle • 3 Phases: • Menstrual phase (about 3 -5 days) • • • Proliferative phase (about 9 days) • • • Endometrium is shed Endometrial tissue, mucous, other secretions, and 2 -5 oz. Blood is expelled through vagina Endometrium thickens, clear thin mucus secreted Ends with ovulation Secretory phase (14 days) • • endometrium prepares for arrival of fertilized ovum If no fertilization, ends with shedding of endometrium

Menstrual Effects • Emotional, physical, or behavioral changes • • • The vast majority of women notice in the week prior to menstruation More severe symptoms are associated with Pre. Menstrual Syndrome (PMS) Dysmenorrhea • • pelvic cramping and pain during menstruation Caused by prostaglandins, a type of hormone
Variations in Menstruation n Amenorrhea – absence of menstruation Primary amenorrhea – never begins menstruation; physical, health, emotional causes n Secondary amenorrhea – menses cease before reaching menopause; pregnancy, lifestyle, emotional, physical causes n n Menorrhagia – excessive menses; oral contraceptives can help control

Variations in Menstruation (Cont. ) Dysfunctional uterine bleeding (DUB) – bleeding for long periods, or intermittent bleeding; hormonal, lifestyle, physical causes n Dysmenorrhea – painful menstruation; caused by inflammations, constipation, psychological stress; recommend medication, relaxation, yoga, massage, and stress relief n

Variations in Menstruation (Cont. ) Premenstrual Syndrome (PMS) – physical or emotional symptoms that occur during the last few weeks of the menstrual cycle n Premenstrual Dysphoric Disorder (PMDD) – mood, behavioral, somatic, and cognitive symptoms; medication (SSRIs) and lifestyle changes provide relief n

Variations in Menstruation (Cont. ) n Risk factors for PMS and PMDD: history of depression, sexual abuse, PTSD, smoking, ethnicity
Menstrual Manipulation and Suppression n n Women can experience up to 450 periods Ways to stem growth of the endometrium: n Continuous birth control pills n Progesterone intrauterine devices n Injections Can relieve many physical symptoms related to menstruation Some see menses as indicating health No medical basis to avoid sex during a period
Menopause A woman’s final menstrual period n Climacteric – period of decreased estrogen production and menstruation stops; 40 -58 years, average 51 years n Typically have irregular cycles, rather than a sudden stop n Sexual glands decrease in size n Secondary sex characteristics change n
Menopause (Cont. ) Hormonal changes – hot flashes, headaches, sleep disturbances n Sexual complaints n Menopause can be induced by surgically removing the ovaries; doctors try to keep at least one in if surgery is necessary n
Menopause (Cont. ) Hormone replacement therapy – was a standard treatment, but there a lot of health risks and not typically used today n Nutritional, vitamin, and herbal remedies are commonly used today n

Female Sexual Response Models • Masters & Johnson 4 Phase Model: • • excitement plateau orgasm resolution
Female Sexual Response Models • Kaplan’s Tri-Phasic Model • • • Desire Excitement Orgasm
Female Sexual Response Models • Loulan’s Sexual Response Model: • Incorporates biological & affective dimensions • • • Willingness Desire Excitement Engorgement Orgasm Pleasure

Desire: Mind or Matter? • Desire is the psychological component of sexual arousal. • A complex interaction between • • • Thoughts and feelings Sensory organs Neural responses Hormonal reactions Occurs throughout many parts of the body

Women’s Sexual Excitement • • Sweating: moistening of vaginal walls Tenting: inner 2/3 of vagina expands Labia may enlarge or flatten & separate Clitoris swells Breathing and heart rate increase Nipples become erect, breasts may enlarge Uterus elevates
Women’s Sexual Excitement • As excitement increases • • Clitoris retracts beneath clitoral hood Vaginal opening decreases by about 1/3 Outer third of vagina becomes more congested, forming the orgasmic platform. Continued stimulation brings orgasm: • Rhythmic contractions of the vagina, uterus, and pelvic muscles accompanied by pleasurable sensation.
Female Reproductive and Sexual Health Gynecological Health Concerns n Cancer of the Female Reproductive Organs n

Female Reproductive and Sexual Health (Cont. ) Genital self-exams are recommended for women to be familiar with their genitals and any possible abnormalities n Routine gynecological examinations recommended once menstruating n Medical history and checkup n Pelvic examination (internal and external) n Breast examination n Pap smear – cervical swab n

Gynecological Health Concerns n Most prevalent: Endometriosis n Toxic Shock Syndrome n Uterine Fibroids n Vulvodynia n Vaginal Infections n

Endometriosis Endometrial cells deposit outside of the uterus n Will engorge/weaken with the menstrual cycle n Symptoms: painful periods, lower abdominal or pelvic pain, pain on defecation, pain during intercourse n Typically childless women between 25 and 40 n

Toxic Shock Syndrome n n Caused by prolonged use of a single tampon which creates a buildup and subsequent infection of bacteria Symptoms: fever, diarrhea, vomiting, sore throat, muscle ache, rash, May cause: dizziness, respiratory distress, kidney failure, heart failure, death Avoid by changing tampons regularly, using less absorbent tampons, using sanitary pads

Uterine Fibroids n n Hard tissue masses in the uterus; size range Affect 20 -40% (maybe 77%) of women over 35 years Symptoms: pelvic pain and pressure, heavy cramping, heavy or prolonged bleeding, constipation, frequent urination, painful sex Treatment: hormones, drugs, laser therapy, surgery, cryotherapy
Vulvodynia n n n Chronic pain and soreness of the vulva Symptoms: vaginal burning, itching, rawness, stinging, stabbing of vagina/vulva The pain may be intermittent or constant Cause is unknown Treatment: biofeedback, drugs, dietary changes, nerve blocks, surgery, pelvic floor muscle strengthening
Infections n Non-sexually transmitted infections can occur n n n Bartholin’s glands Urinary tract May be due to poor hygiene practices and/or frequent intercourse Treated by draining infected gland (if necessary) and use of antibiotics Douches change the vaginal p. H level and can increase risk of infection
Cancer of the Female Reproductive Organs Breast n Uterine n Cervical n Endometrial n Ovarian n
Breast Cancer n n n Worldwide, the most common cancer One in 7 American women will develop it Risk factors: fat intake, aging, early menarche, prolonged estrogen, inactive lifestyle, alcohol consumption, genetics Breastfeeding, early pregnancy reduces risk Early detection is critical: breast selfexaminations, gynecological checkups, mammography
Breast Cancer Symptoms: breast lump, breast pain, nipple discharge, puckering of skin, change in nipple shape n If untreated, the cancer will spread to other parts of the body n Treatment: partial/modified mastectomy, radical mastectomy, lumpectomy, radiation, chemotherapy n
Cervical Cancer n n n 1 in 130 American women Pap smear is used for detection; should be screened every year by 21 years of age High cure rates Risk factors: early intercourse, many sexual partners, teenage mothers, cervicitis, genital viral infections, extended oral contraceptive use Treatment: surgery, radiation, hysterectomy

Endometrial Cancer Symptoms: abnormal bleeding, spotting n Detection most successful with dilation and curettage n Treatment: surgery, radiation, hormones, chemotherapy n Over 90% survival rate n Oral contraceptives decrease risk n
Ovarian Cancer n n Less common than breast, uterine cancers Most deadly Symptoms: few early signs, ovarian cyst, slight abdominal discomfort, appetite loss, indigestion, abdominal swelling, nausea, vomiting Risk factors: childlessness, early menopause, high-fat diet, higher SES, lactose-intolerant, use talc powder on the vulva

Ovarian Cancer (Cont. ) n n Decreased risk with having children and using birth control pills, tubal ligation Detection techniques: blood tests, pelvic exams, ultrasound Unfortunately, most diagnosed after cancer has spread beyond the ovary because of the lack of early warning signs Treatment: remove ovaries, radiation, chemotherapy
- Slides: 75