Female Reproductive System Dr Holly NashRule Female Reproductive




- Slides: 66
Female Reproductive System Dr. Holly Nash-Rule
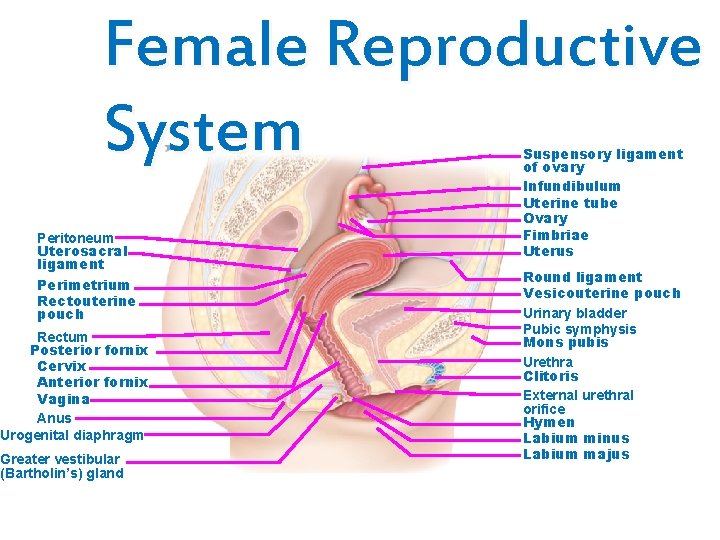
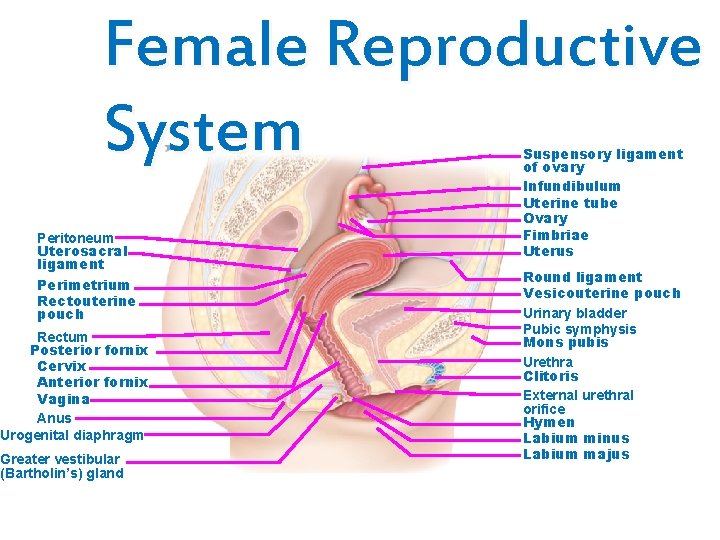
Female Reproductive System Peritoneum Uterosacral ligament Perimetrium Rectouterine pouch Rectum Posterior fornix Cervix Anterior fornix Vagina Anus Urogenital diaphragm Greater vestibular (Bartholin’s) gland Suspensory ligament of ovary Infundibulum Uterine tube Ovary Fimbriae Uterus Round ligament Vesicouterine pouch Urinary bladder Pubic symphysis Mons pubis Urethra Clitoris External urethral orifice Hymen Labium minus Labium majus
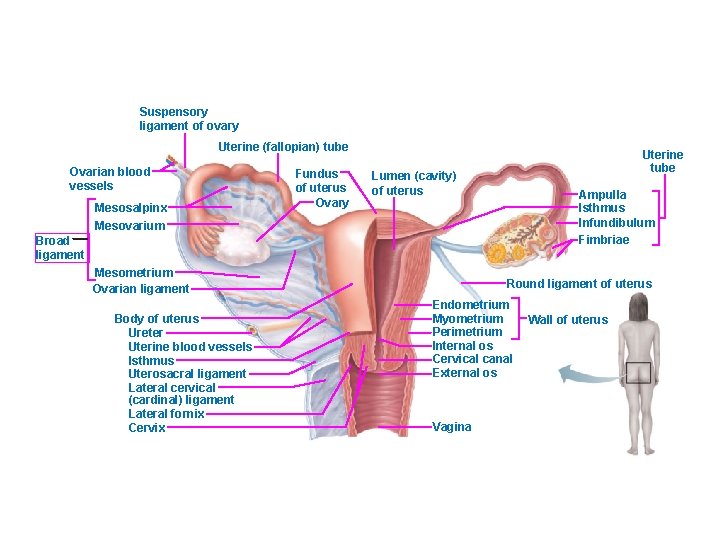
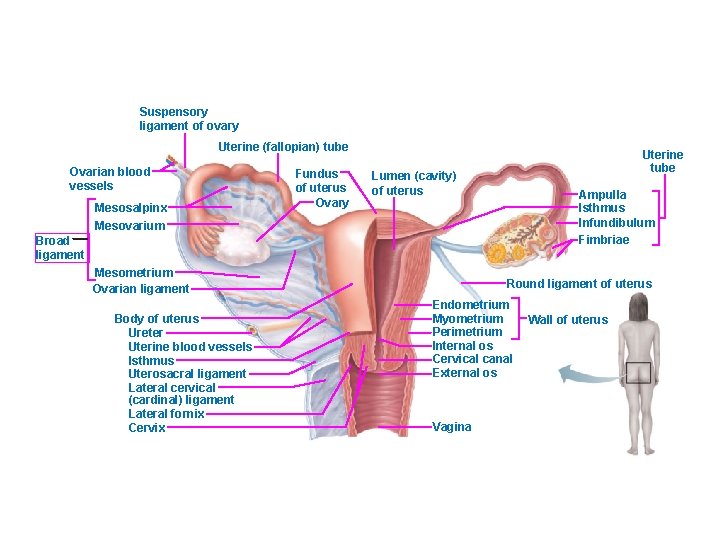
Suspensory ligament of ovary Uterine (fallopian) tube Ovarian blood vessels Mesosalpinx Fundus of uterus Ovary Uterine tube Lumen (cavity) of uterus Ampulla Isthmus Infundibulum Fimbriae Mesovarium Broad ligament Mesometrium Ovarian ligament Body of uterus Ureter Uterine blood vessels Isthmus Uterosacral ligament Lateral cervical (cardinal) ligament Lateral fornix Cervix Round ligament of uterus Endometrium Myometrium Perimetrium Internal os Cervical canal External os Vagina Wall of uterus
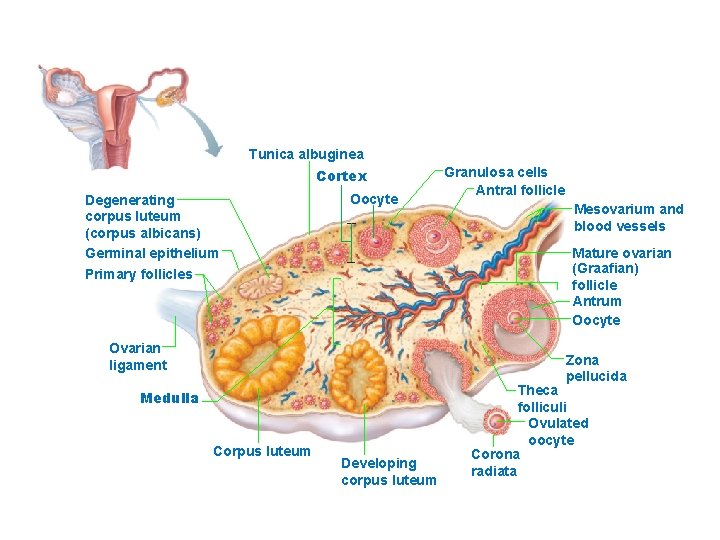
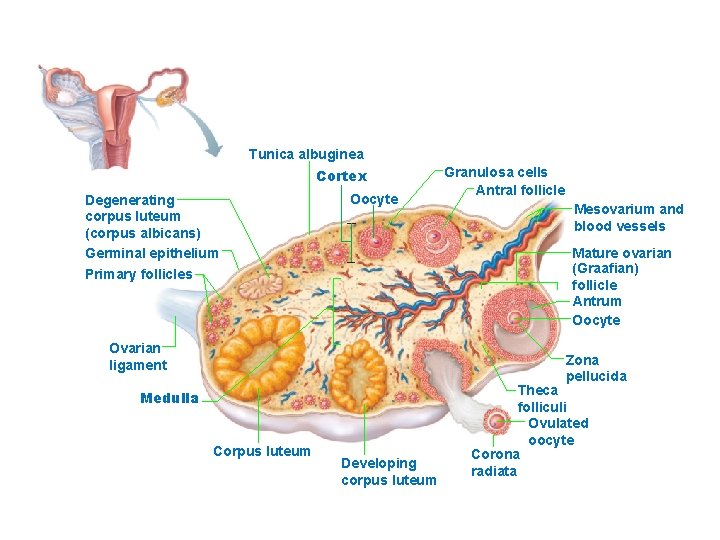
Tunica albuginea Cortex Degenerating corpus luteum (corpus albicans) Germinal epithelium Oocyte Granulosa cells Antral follicle Mesovarium and blood vessels Mature ovarian (Graafian) follicle Antrum Oocyte Primary follicles Ovarian ligament Zona pellucida Medulla Corpus luteum Developing corpus luteum Theca folliculi Ovulated oocyte Corona radiata
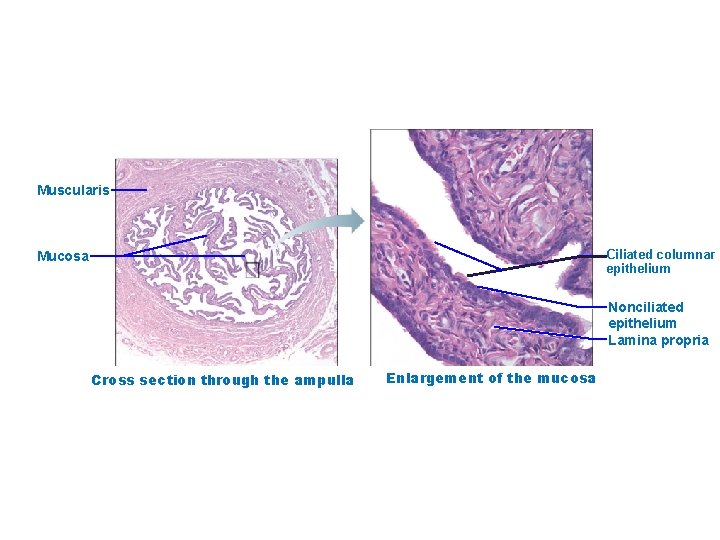
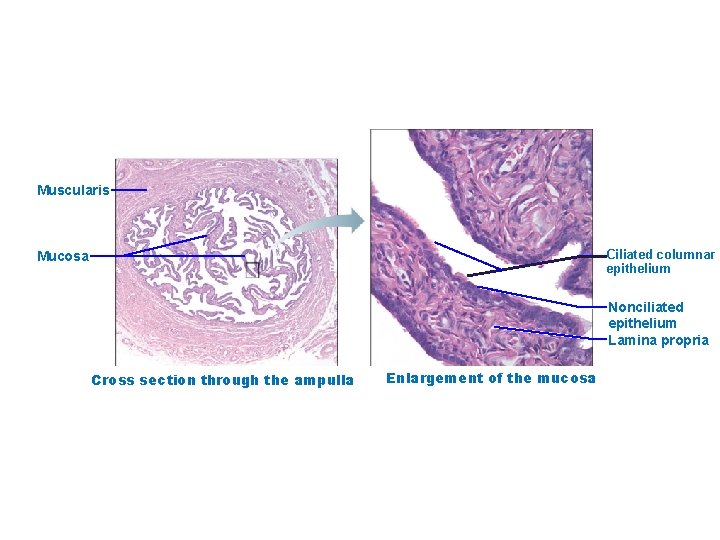
Muscularis Ciliated columnar epithelium Mucosa Nonciliated epithelium Lamina propria Cross section through the ampulla Enlargement of the mucosa
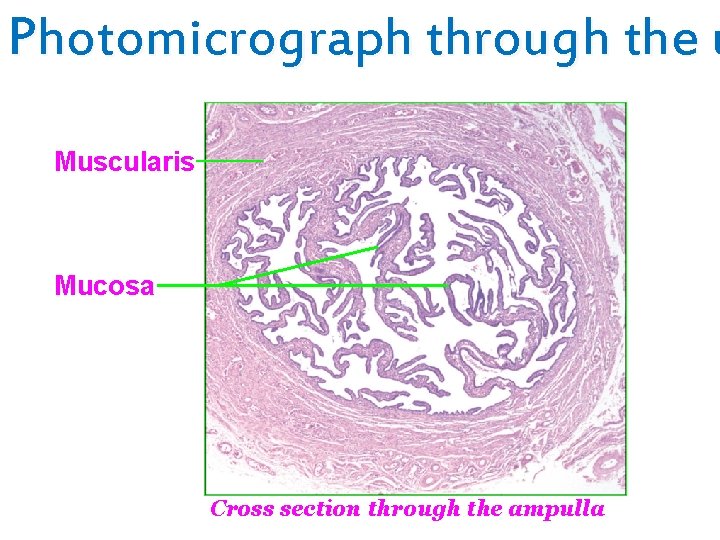
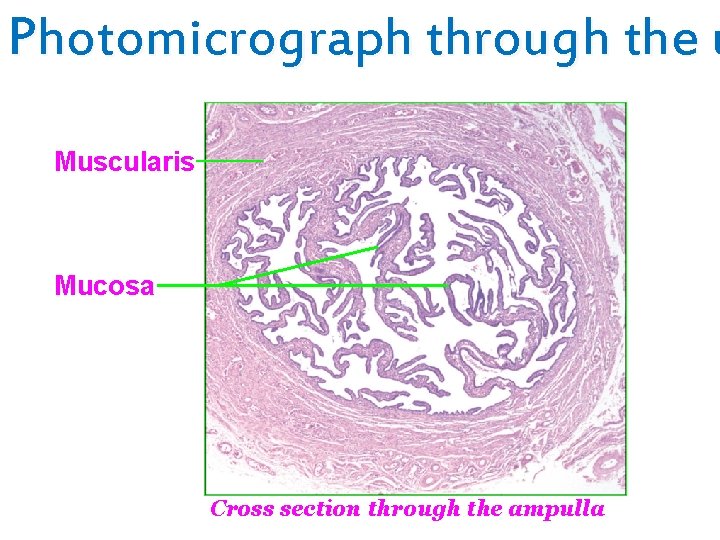
Photomicrograph through the u Muscularis Mucosa Cross section through the ampulla
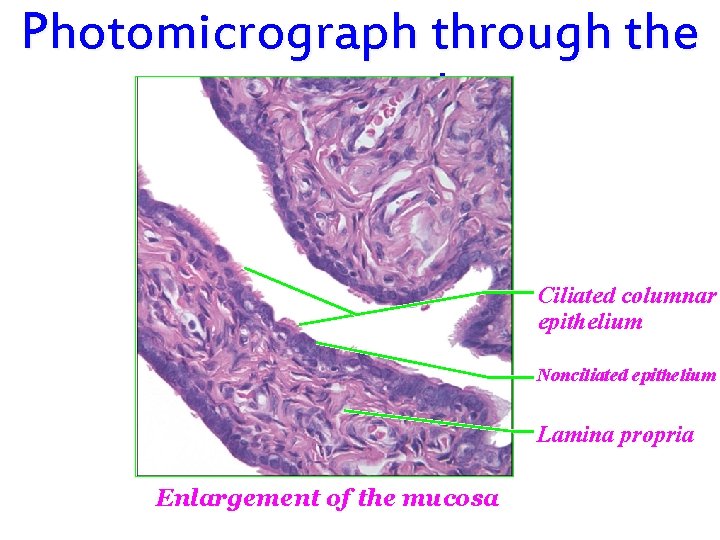
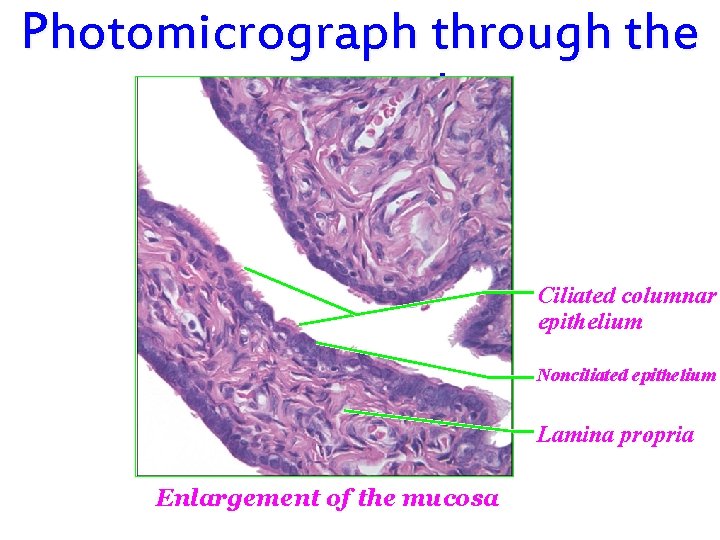
Photomicrograph through the uterine tube. Ciliated columnar epithelium Nonciliated epithelium Lamina propria Enlargement of the mucosa
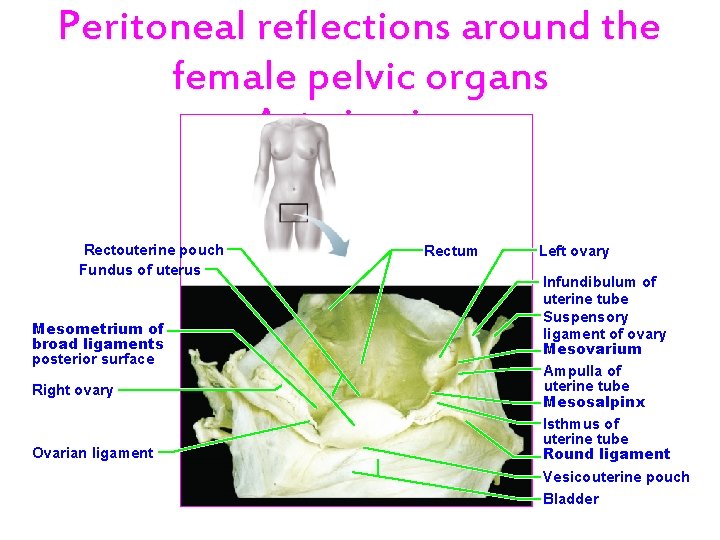
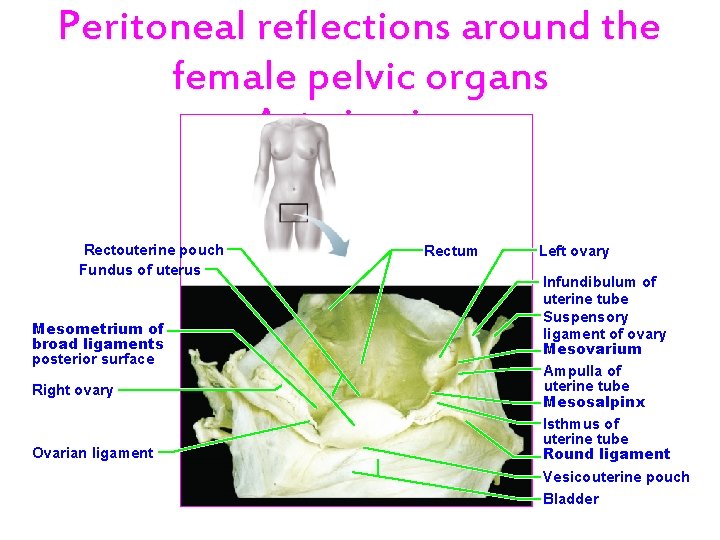
Peritoneal reflections around the female pelvic organs Anterior view. Rectouterine pouch Fundus of uterus Mesometrium of broad ligaments posterior surface Right ovary Ovarian ligament Rectum Left ovary Infundibulum of uterine tube Suspensory ligament of ovary Mesovarium Ampulla of uterine tube Mesosalpinx Isthmus of uterine tube Round ligament Vesicouterine pouch Bladder
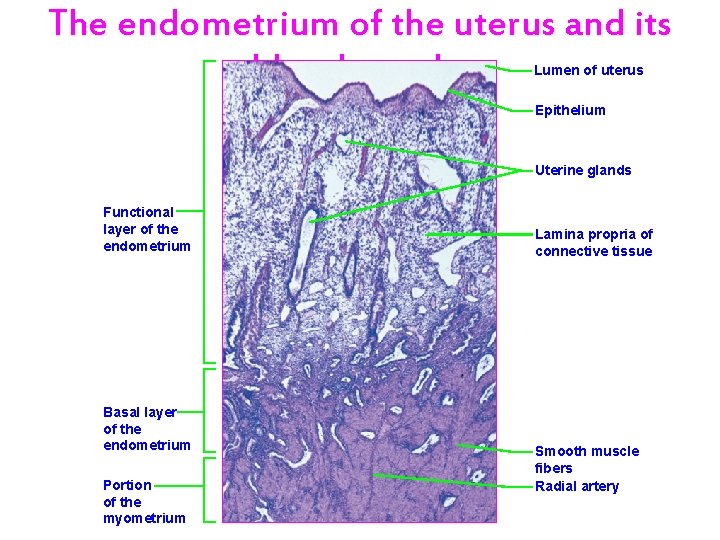
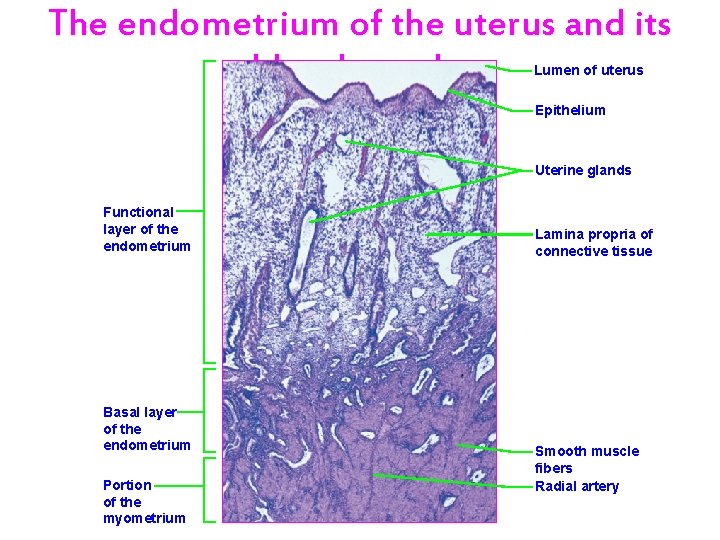
The endometrium of the uterus and its blood supply. Lumen of uterus Epithelium Uterine glands Functional layer of the endometrium Basal layer of the endometrium Portion of the myometrium Lamina propria of connective tissue Smooth muscle fibers Radial artery
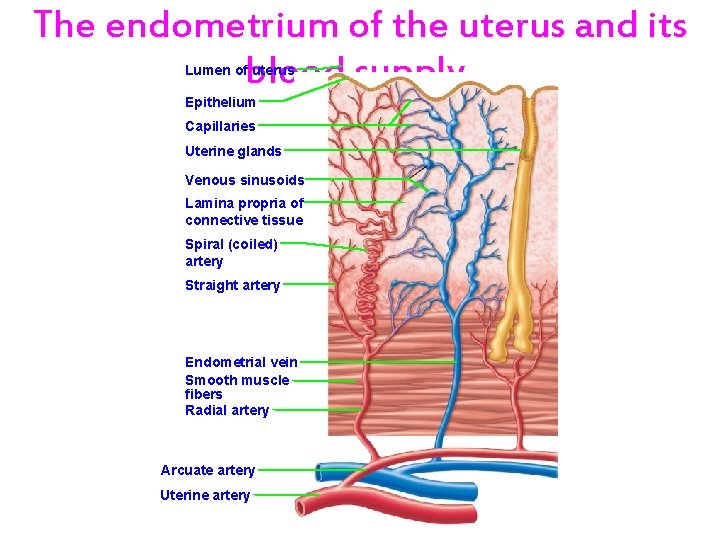
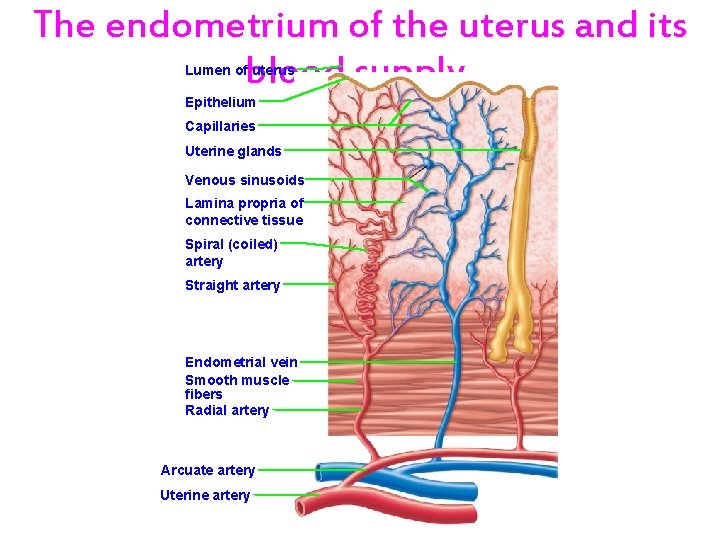
The endometrium of the uterus and its blood supply. Lumen of uterus Epithelium Capillaries Uterine glands Venous sinusoids Lamina propria of connective tissue Spiral (coiled) artery Straight artery Endometrial vein Smooth muscle fibers Radial artery Arcuate artery Uterine artery
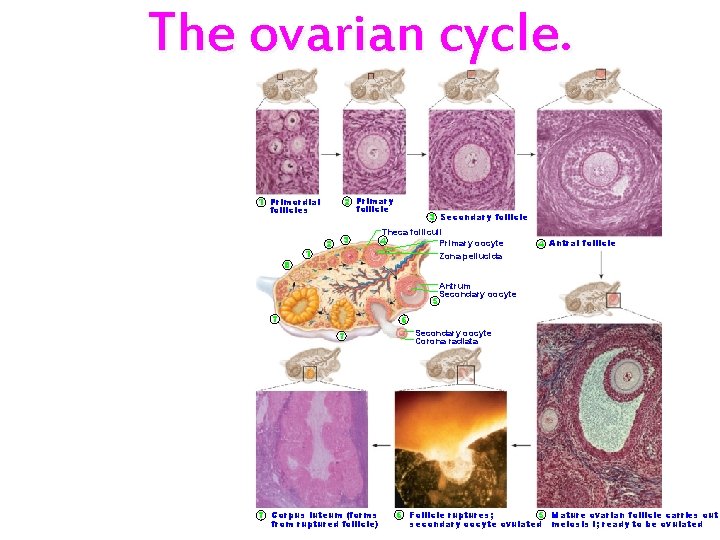
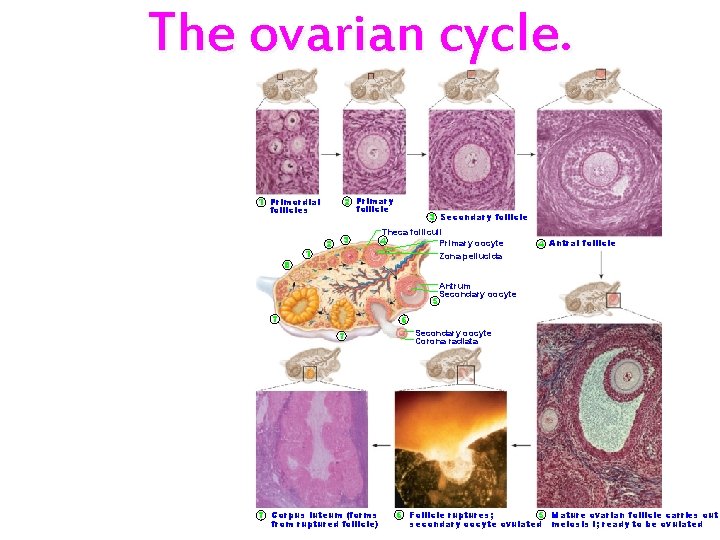
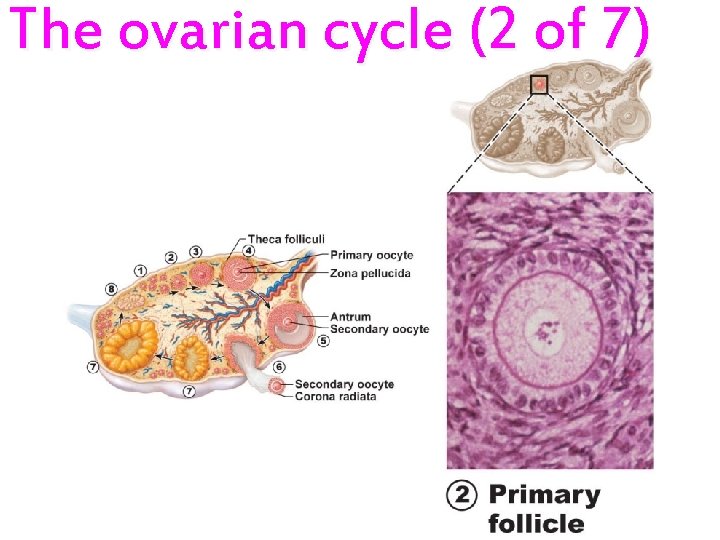
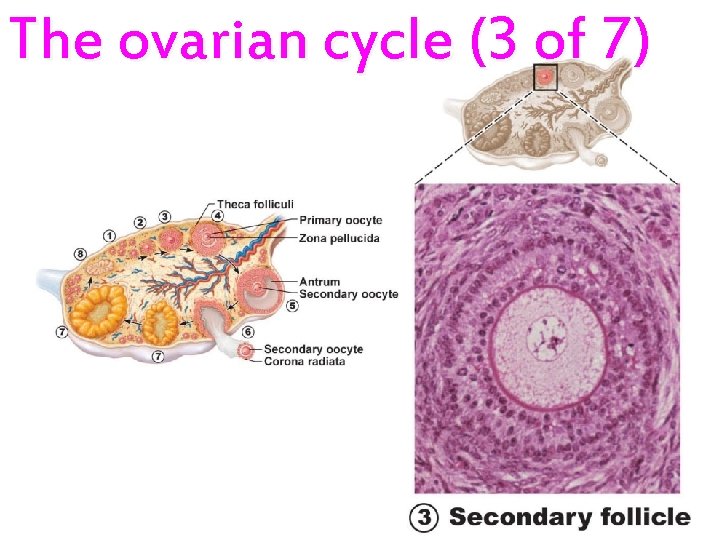
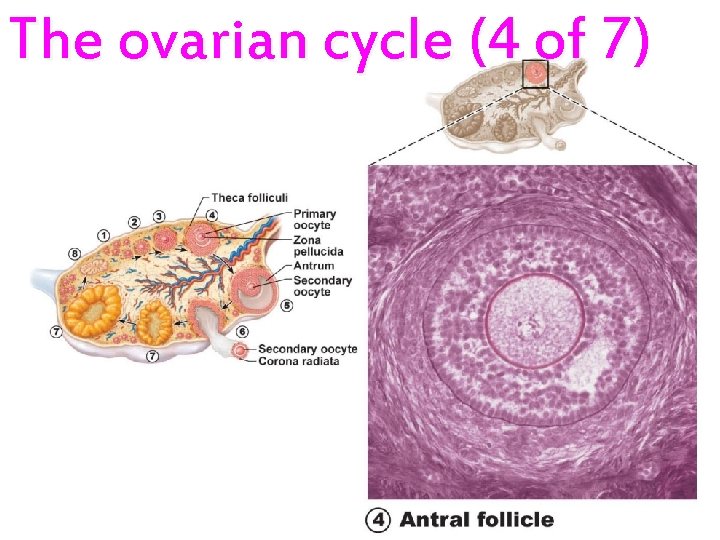
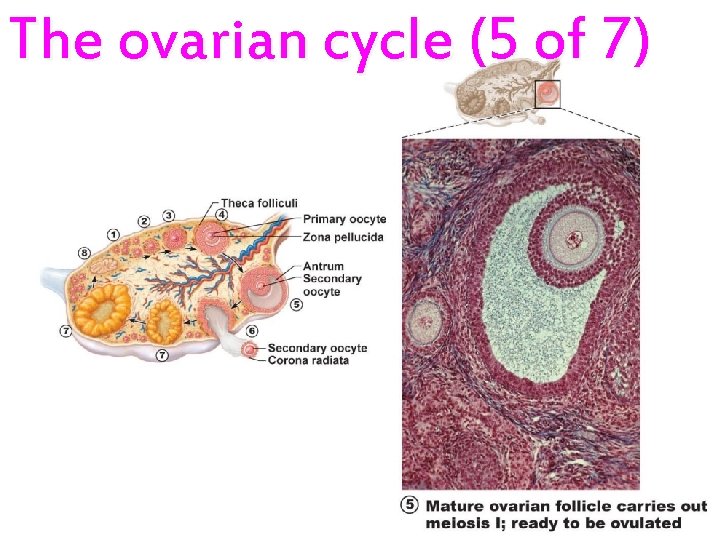
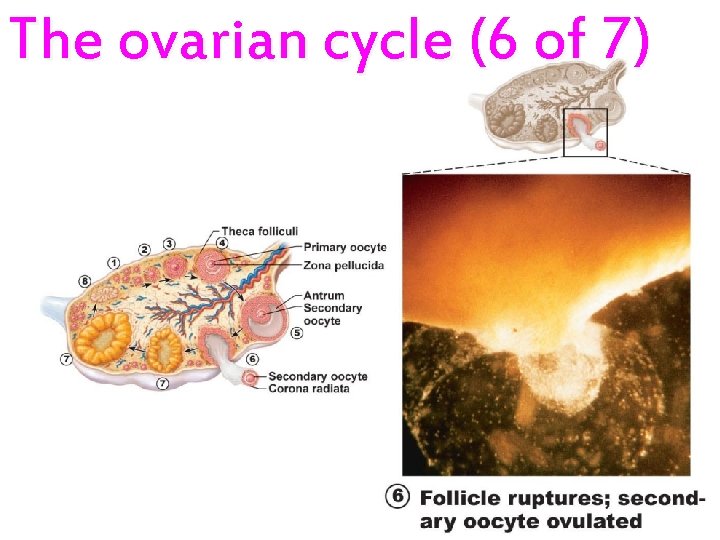
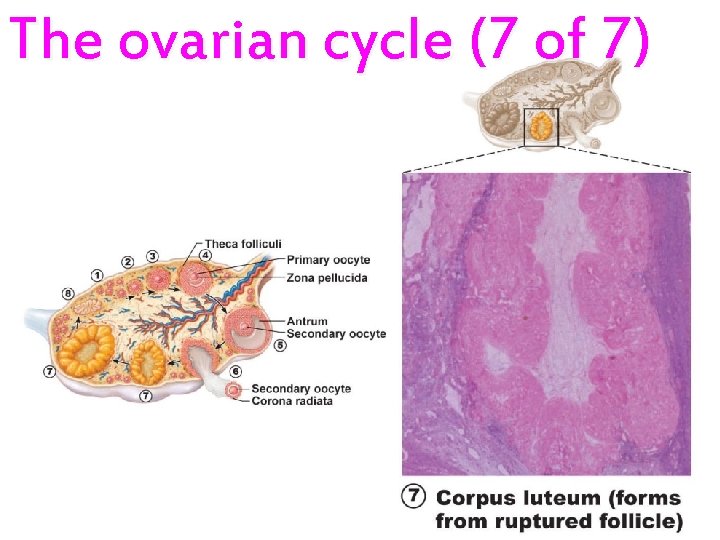
The ovarian cycle. 2 Primary follicle 1 Primordial follicles 8 1 2 3 3 Secondary follicle Theca folliculi 4 Primary oocyte 4 Antral follicle Zona pellucida 5 7 Antrum Secondary oocyte 6 7 7 Corpus luteum (forms from ruptured follicle) Secondary oocyte Corona radiata 6 Follicle ruptures; 5 Mature ovarian follicle carries out secondary oocyte ovulated meiosis I; ready to be ovulated
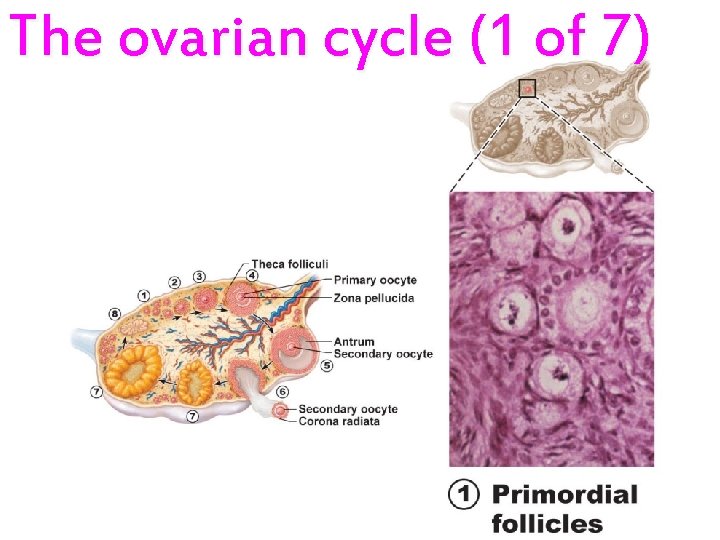
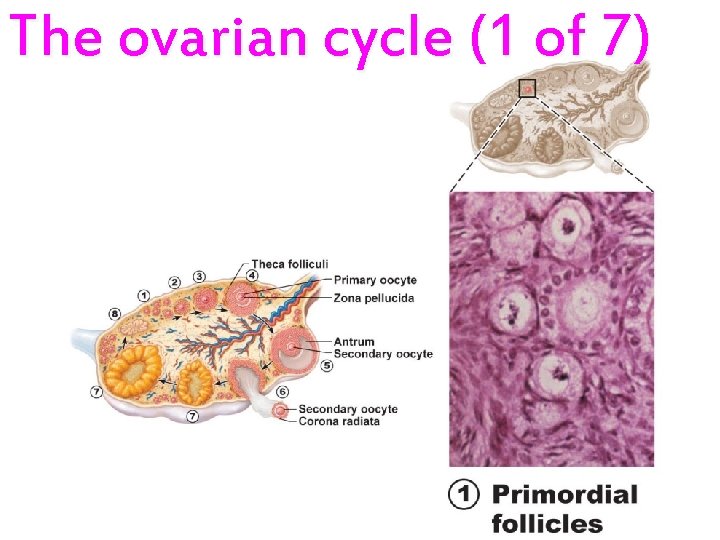
The ovarian cycle (1 of 7)
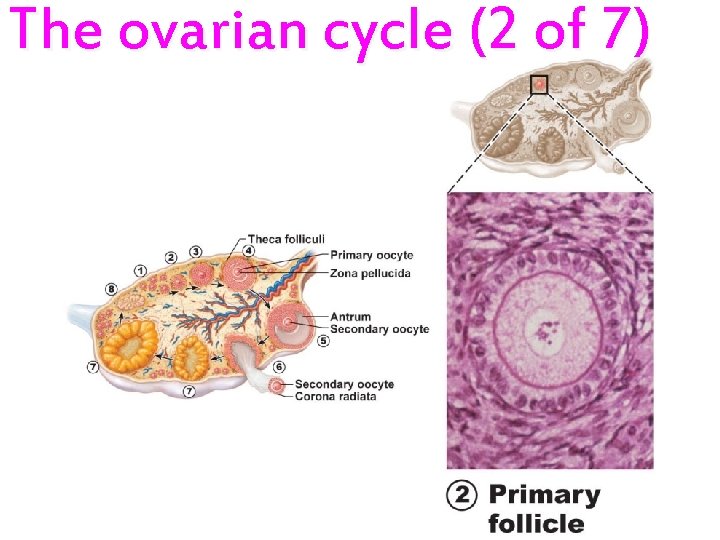
The ovarian cycle (2 of 7)
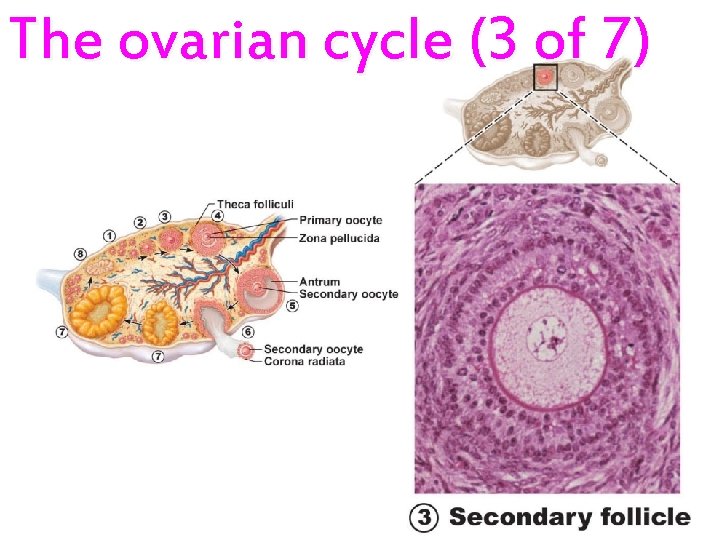
The ovarian cycle (3 of 7)
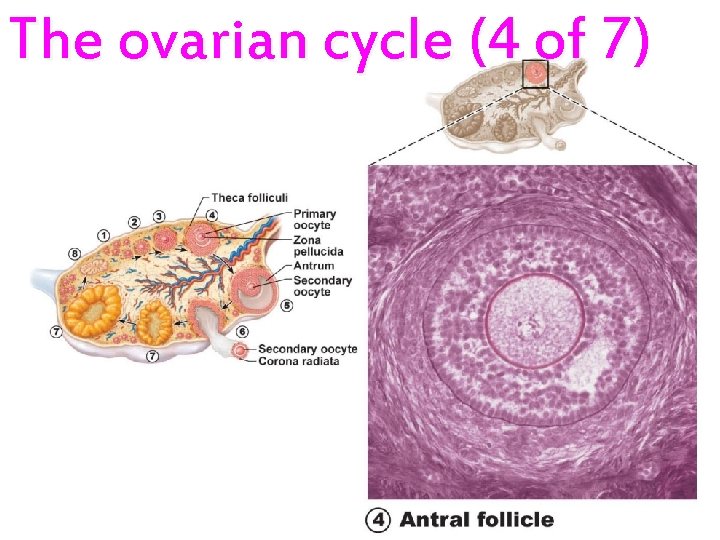
The ovarian cycle (4 of 7)
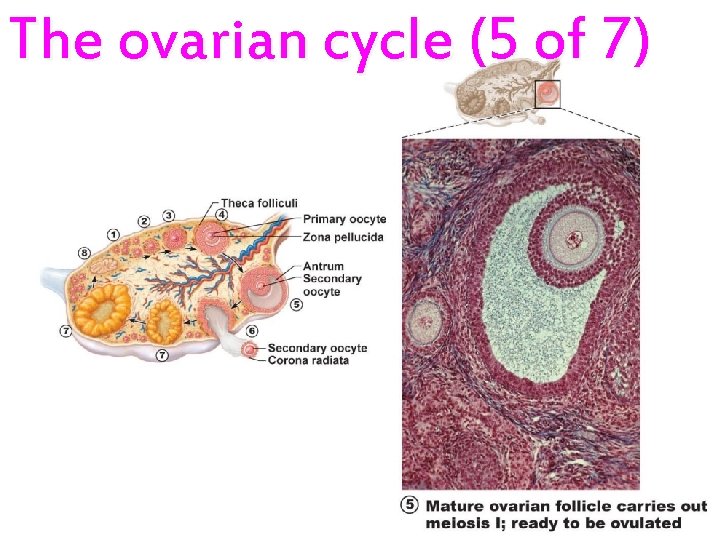
The ovarian cycle (5 of 7)
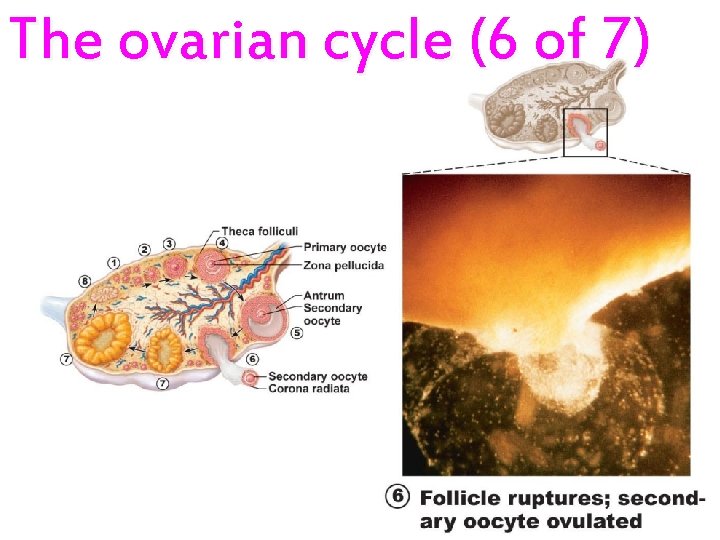
The ovarian cycle (6 of 7)
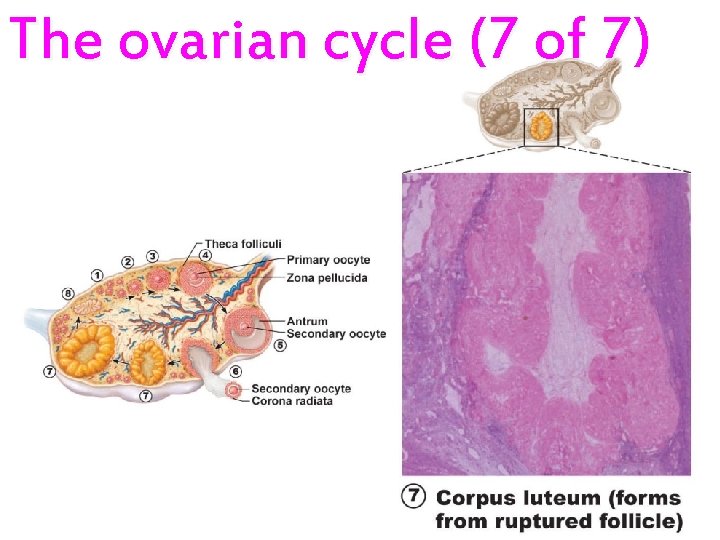
The ovarian cycle (7 of 7)
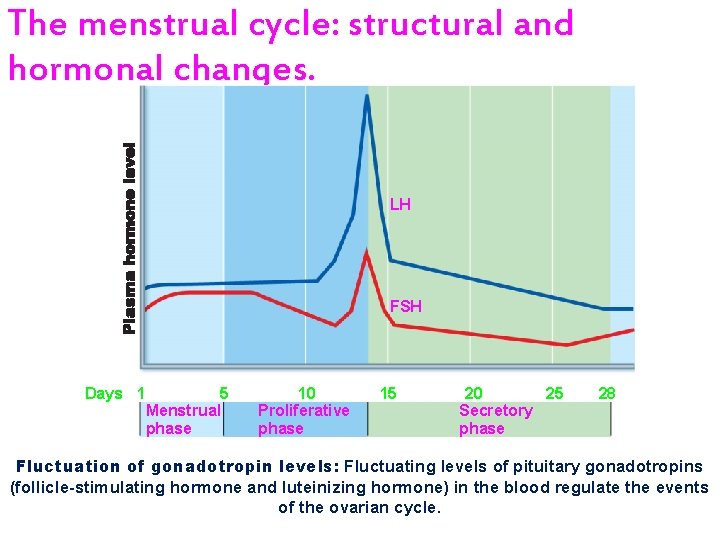
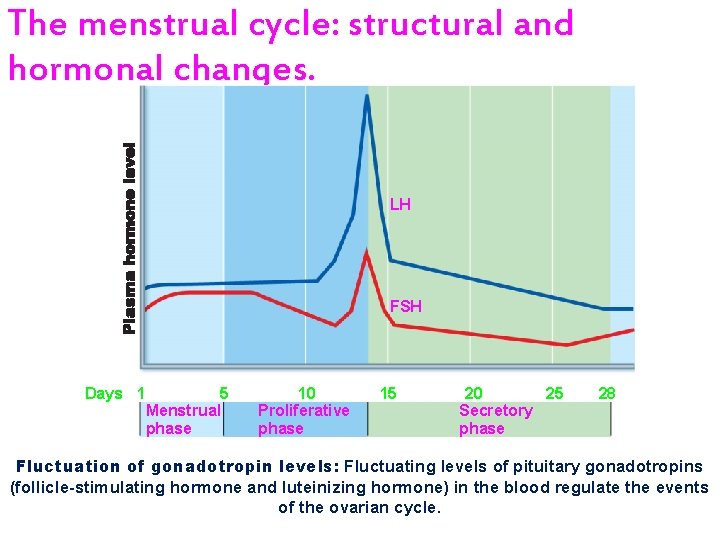
The menstrual cycle: structural and hormonal changes. LH FSH Days 1 5 Menstrual phase 10 Proliferative phase 15 20 25 Secretory phase 28 Fluctuation of gonadotropin levels: Fluctuating levels of pituitary gonadotropins (follicle-stimulating hormone and luteinizing hormone) in the blood regulate the events of the ovarian cycle.
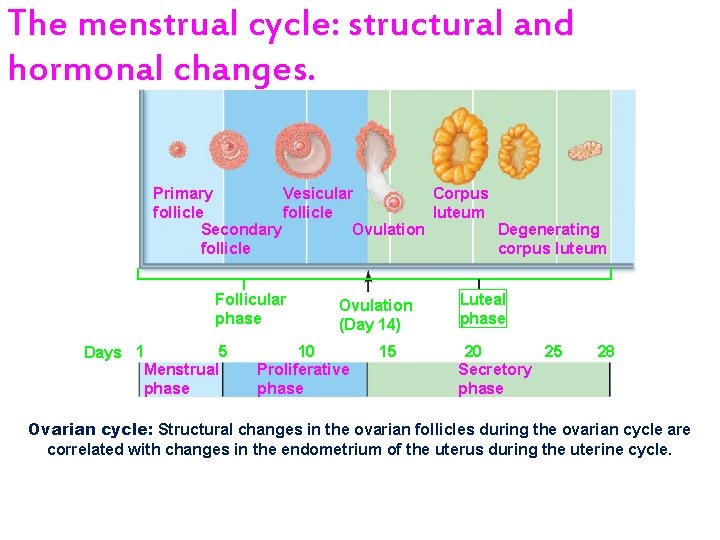
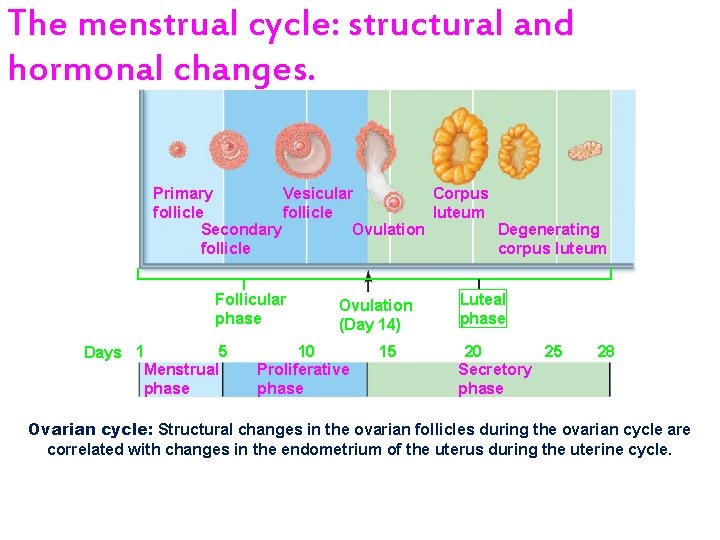
The menstrual cycle: structural and hormonal changes. Primary Vesicular Corpus follicle luteum Secondary Ovulation Degenerating follicle corpus luteum Follicular phase 5 Days 1 Menstrual phase Ovulation (Day 14) 10 Proliferative phase 15 Luteal phase 20 25 Secretory phase 28 Ovarian cycle: Structural changes in the ovarian follicles during the ovarian cycle are correlated with changes in the endometrium of the uterus during the uterine cycle.
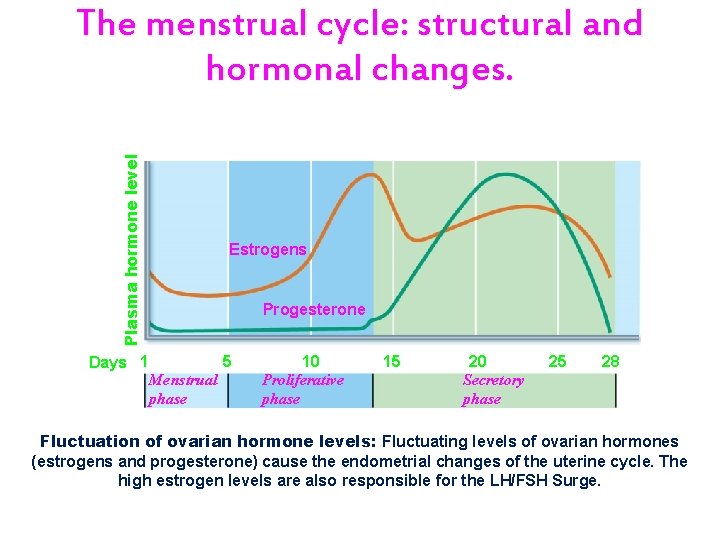
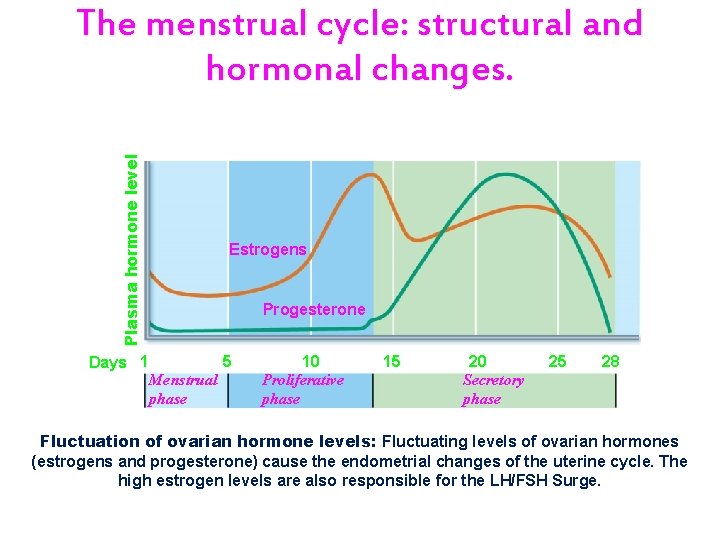
Plasma hormone level The menstrual cycle: structural and hormonal changes. Days 1 Estrogens Progesterone Menstrual phase 5 10 Proliferative phase 15 20 Secretory phase 25 28 Fluctuation of ovarian hormone levels: Fluctuating levels of ovarian hormones (estrogens and progesterone) cause the endometrial changes of the uterine cycle. The high estrogen levels are also responsible for the LH/FSH Surge.
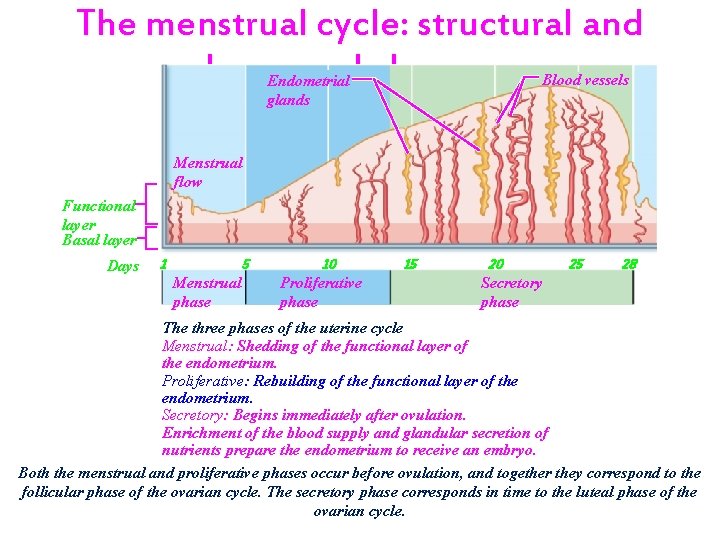
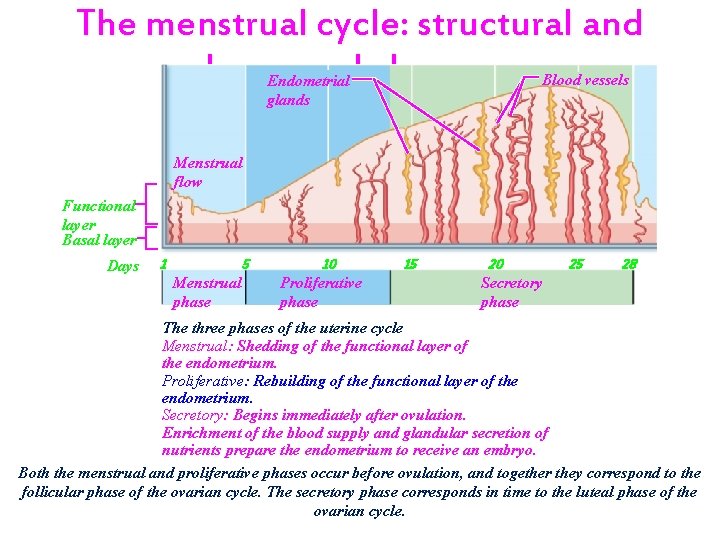
The menstrual cycle: structural and hormonal changes. Blood vessels Endometrial glands Menstrual flow Functional layer Basal layer Days 1 5 Menstrual phase 10 Proliferative phase 15 20 25 28 Secretory phase The three phases of the uterine cycle Menstrual: Shedding of the functional layer of the endometrium. Proliferative: Rebuilding of the functional layer of the endometrium. Secretory: Begins immediately after ovulation. Enrichment of the blood supply and glandular secretion of nutrients prepare the endometrium to receive an embryo. Both the menstrual and proliferative phases occur before ovulation, and together they correspond to the follicular phase of the ovarian cycle. The secretory phase corresponds in time to the luteal phase of the ovarian cycle.
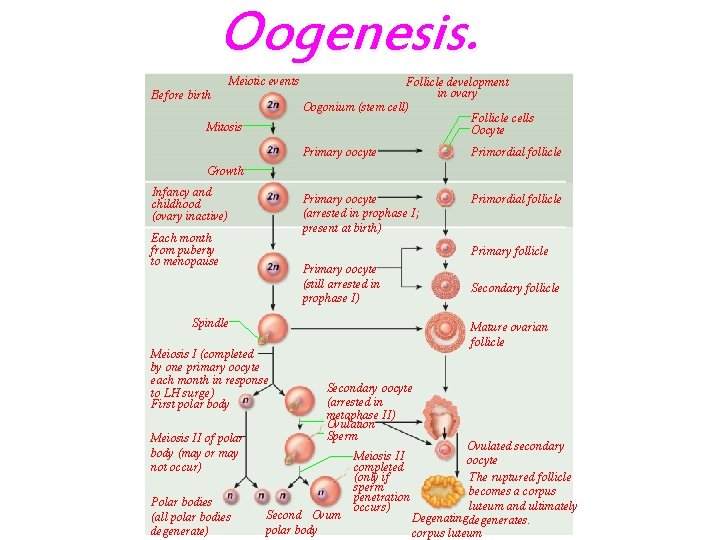
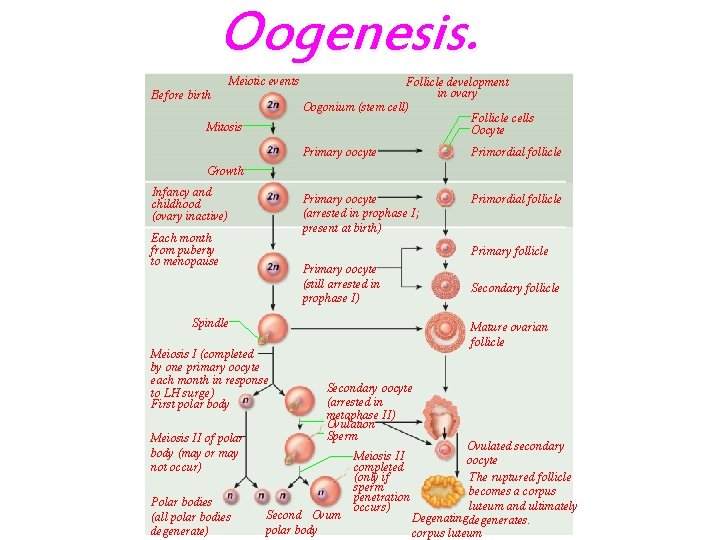
Oogenesis. Meiotic events Before birth Mitosis Follicle development in ovary Oogonium (stem cell) Follicle cells Oocyte Primary oocyte Primordial follicle Primary oocyte (arrested in prophase I; present at birth) Primordial follicle Growth Infancy and childhood (ovary inactive) Each month from puberty to menopause Primary follicle Primary oocyte (still arrested in prophase I) Secondary follicle Spindle Meiosis I (completed by one primary oocyte each month in response to LH surge) First polar body Meiosis II of polar body (may or may not occur) Polar bodies (all polar bodies degenerate) Mature ovarian follicle Secondary oocyte (arrested in metaphase II) Ovulation Sperm Second Ovum polar body Meiosis II completed (only if sperm penetration occurs) Ovulated secondary oocyte The ruptured follicle becomes a corpus luteum and ultimately Degenatingdegenerates. corpus luteum
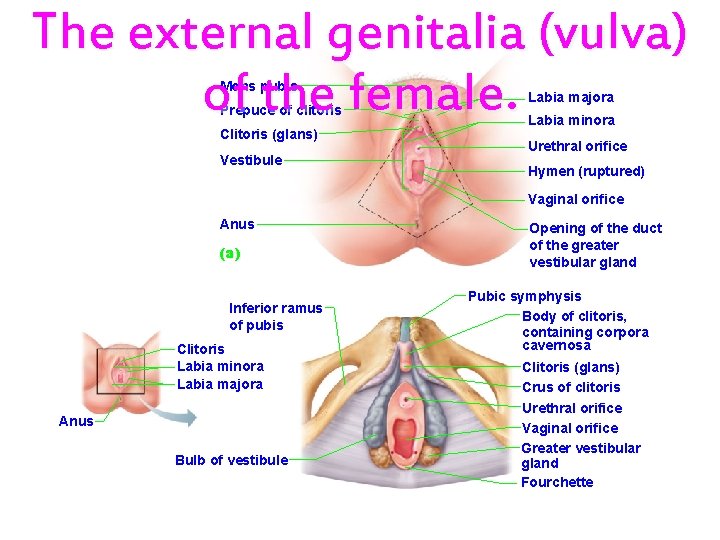
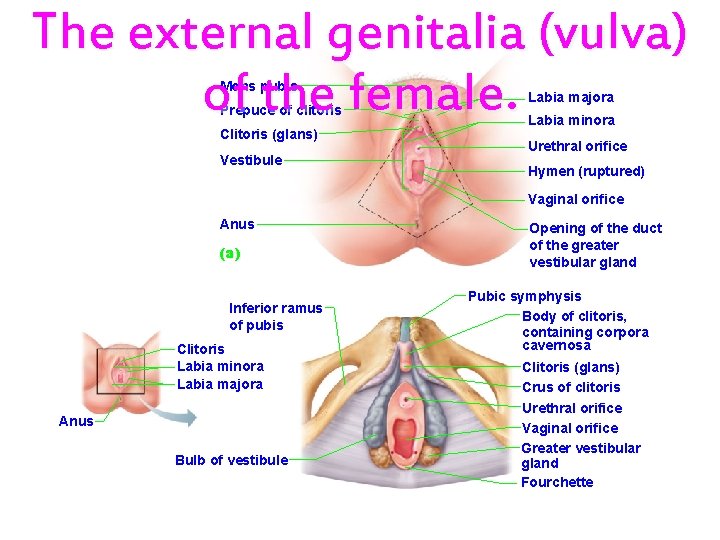
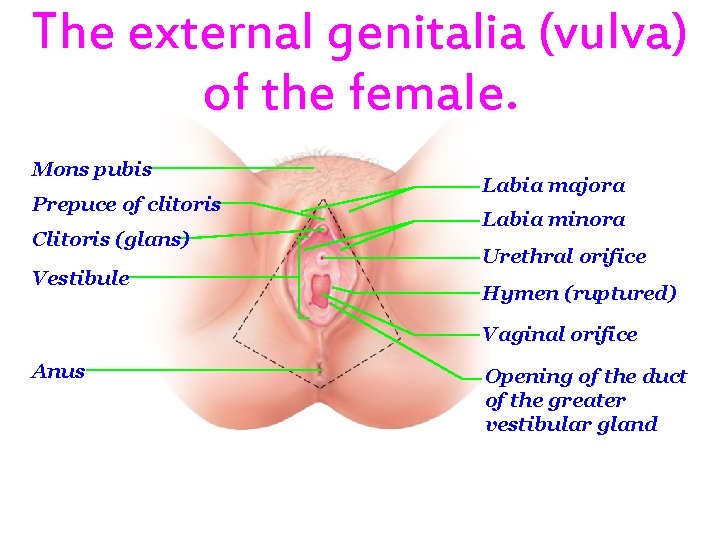
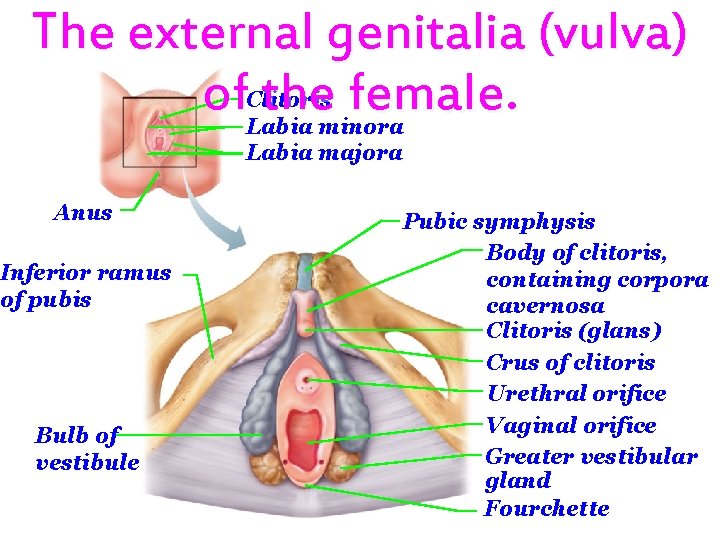
The external genitalia (vulva) of the female. Mons pubis Prepuce of clitoris Clitoris (glans) Vestibule Labia majora Labia minora Urethral orifice Hymen (ruptured) Vaginal orifice Anus (a) Inferior ramus of pubis Clitoris Labia minora Labia majora Anus Bulb of vestibule Opening of the duct of the greater vestibular gland Pubic symphysis Body of clitoris, containing corpora cavernosa Clitoris (glans) Crus of clitoris Urethral orifice Vaginal orifice Greater vestibular gland Fourchette
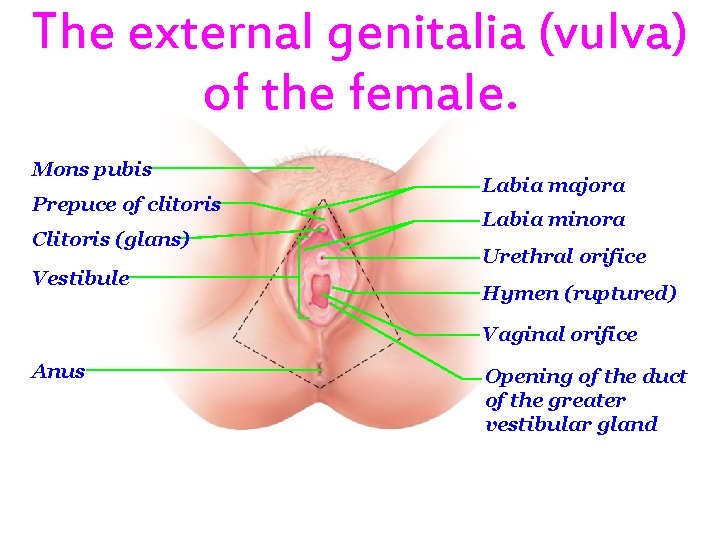
The external genitalia (vulva) of the female. Mons pubis Prepuce of clitoris Clitoris (glans) Vestibule Labia majora Labia minora Urethral orifice Hymen (ruptured) Vaginal orifice Anus Opening of the duct of the greater vestibular gland
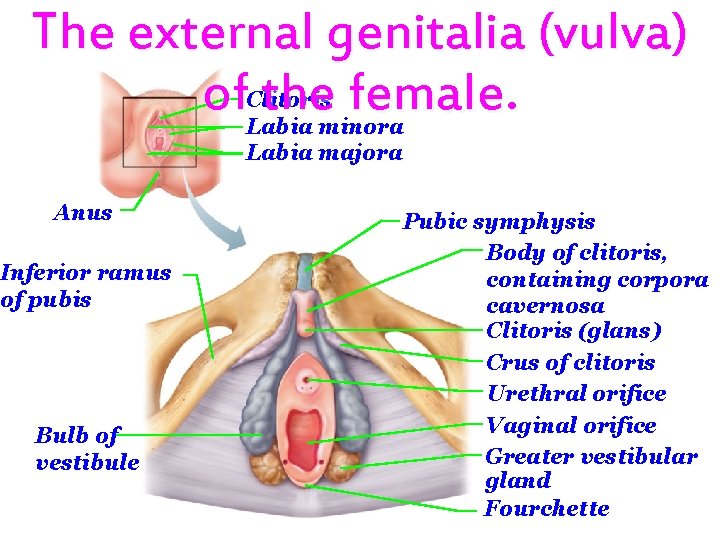
The external genitalia (vulva) of the female. Clitoris Labia minora Labia majora Anus Inferior ramus of pubis Bulb of vestibule Pubic symphysis Body of clitoris, containing corpora cavernosa Clitoris (glans) Crus of clitoris Urethral orifice Vaginal orifice Greater vestibular gland Fourchette
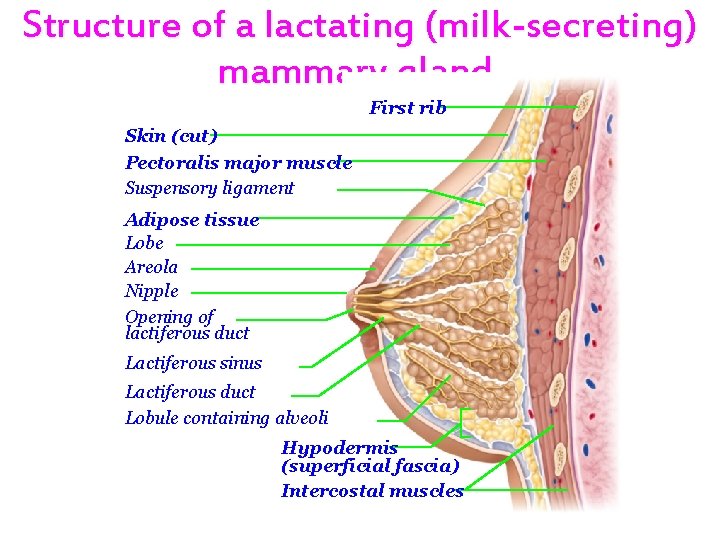
Structure of a lactating (milksecreting) mammary gland.
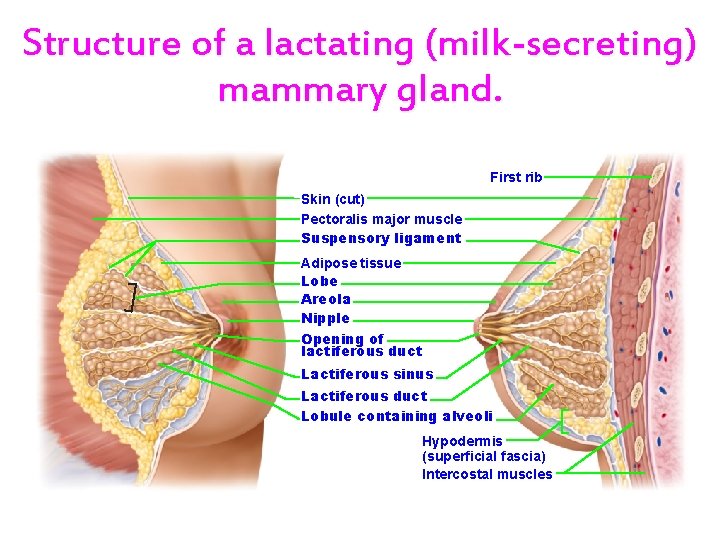
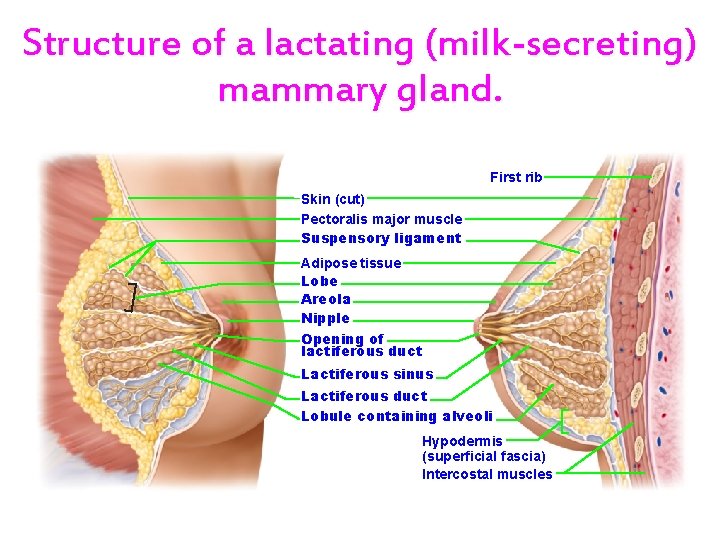
Structure of a lactating (milk-secreting) mammary gland. First rib Skin (cut) Pectoralis major muscle Suspensory ligament Adipose tissue Lobe Areola Nipple Opening of lactiferous duct Lactiferous sinus Lactiferous duct Lobule containing alveoli Hypodermis (superficial fascia) Intercostal muscles

Structure of a lactating (milk-secreting) mammary gland. Skin (cut) Pectoralis major muscle Suspensory ligament Adipose tissue Lobe Areola Nipple Opening of lactiferous duct Lactiferous sinus Lactiferous duct Lobule containing alveoli
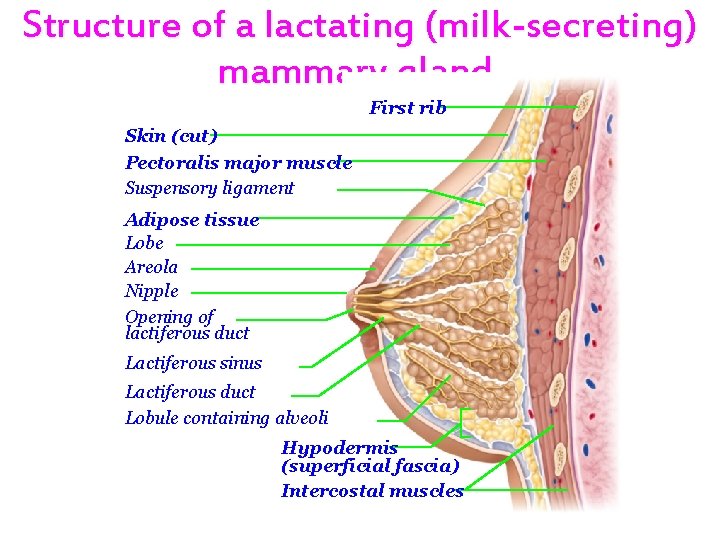
Structure of a lactating (milk-secreting) mammary gland. First rib Skin (cut) Pectoralis major muscle Suspensory ligament Adipose tissue Lobe Areola Nipple Opening of lactiferous duct Lactiferous sinus Lactiferous duct Lobule containing alveoli Hypodermis (superficial fascia) Intercostal muscles
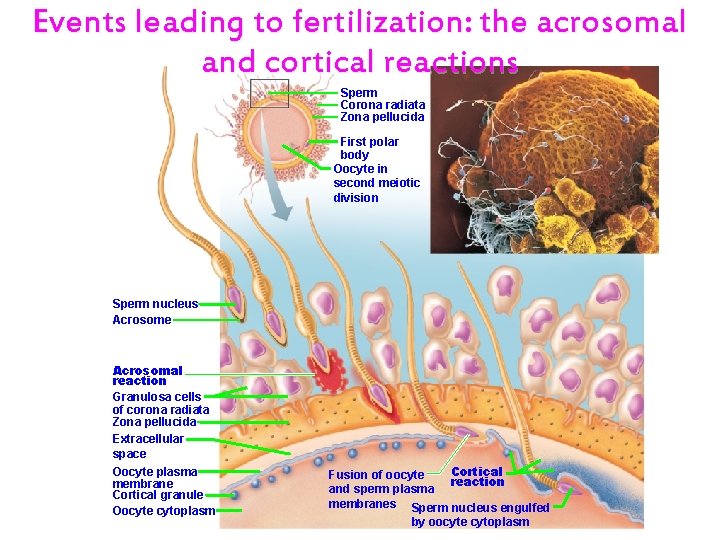
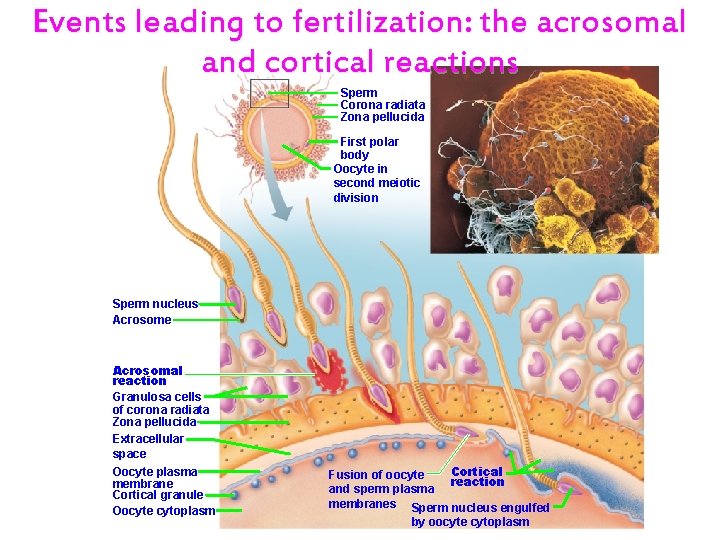
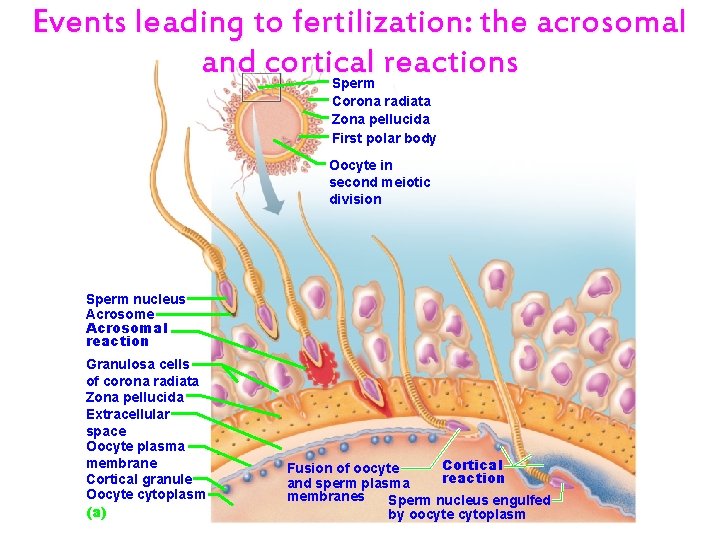
Events leading to fertilization: the acrosomal and cortical reactions Sperm Corona radiata Zona pellucida First polar body Oocyte in second meiotic division Sperm nucleus Acrosome Acrosomal reaction Granulosa cells of corona radiata Zona pellucida Extracellular space Oocyte plasma membrane Cortical granule Oocyte cytoplasm Cortical Fusion of oocyte reaction and sperm plasma membranes Sperm nucleus engulfed by oocyte cytoplasm
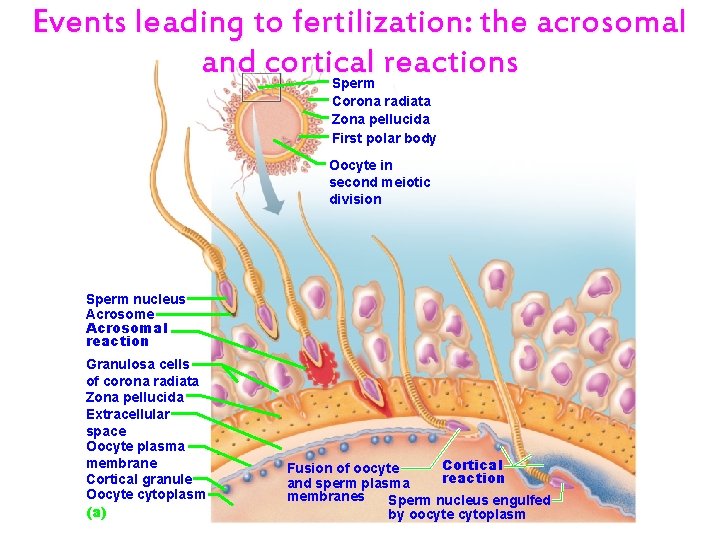
Events leading to fertilization: the acrosomal and cortical reactions Sperm Corona radiata Zona pellucida First polar body Oocyte in second meiotic division Sperm nucleus Acrosome Acrosomal reaction Granulosa cells of corona radiata Zona pellucida Extracellular space Oocyte plasma membrane Cortical granule Oocyte cytoplasm (a) Cortical Fusion of oocyte reaction and sperm plasma membranes Sperm nucleus engulfed by oocyte cytoplasm
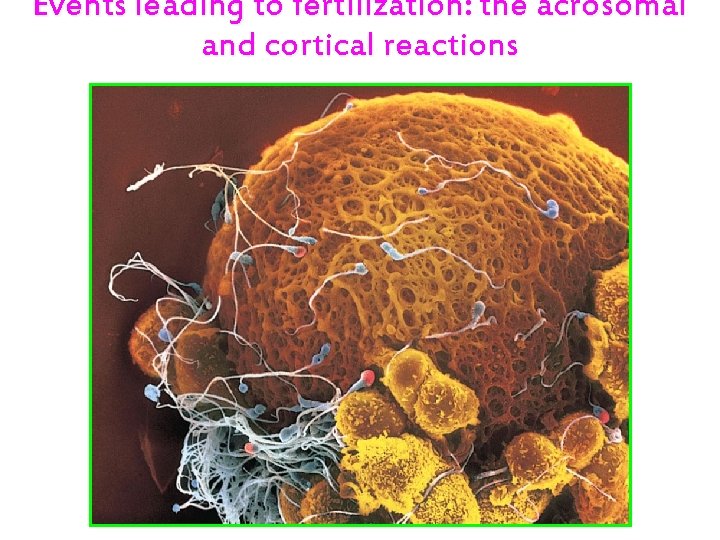
Events leading to fertilization: the acrosomal and cortical reactions
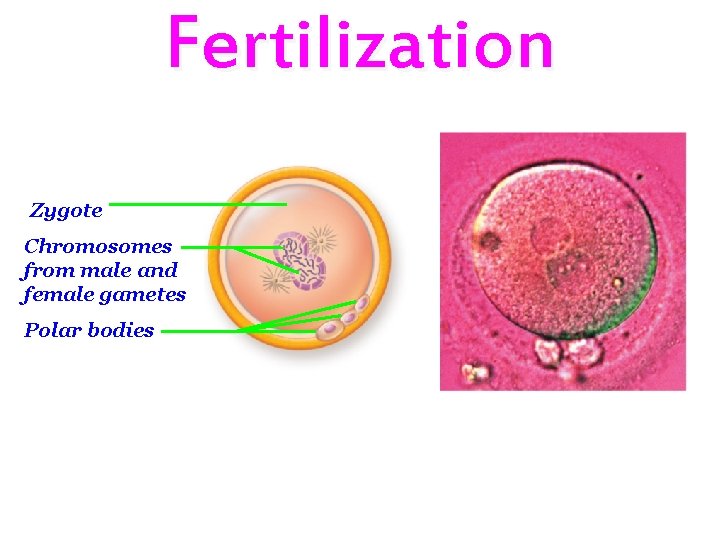
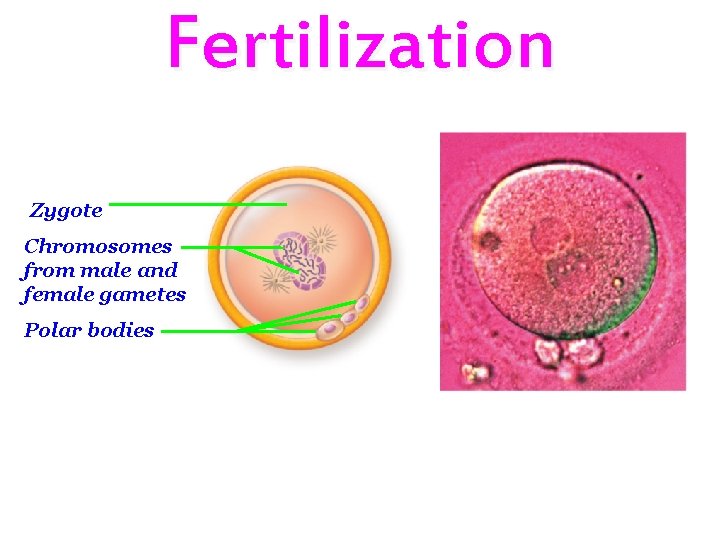
Fertilization Zygote Chromosomes from male and female gametes Polar bodies
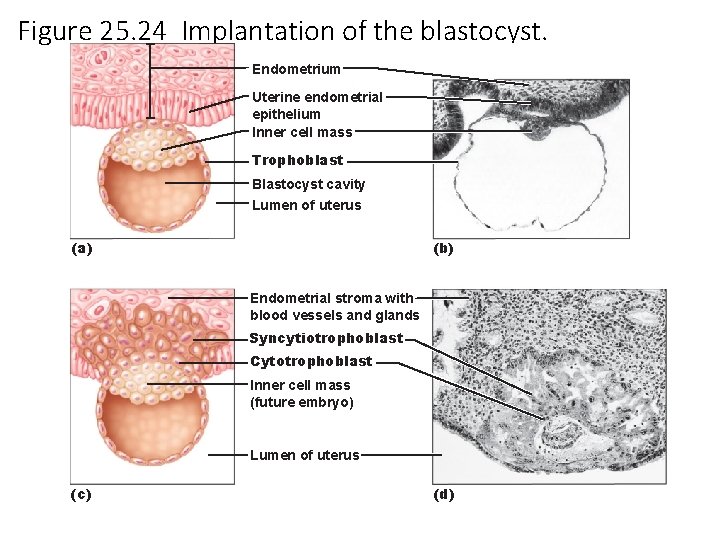
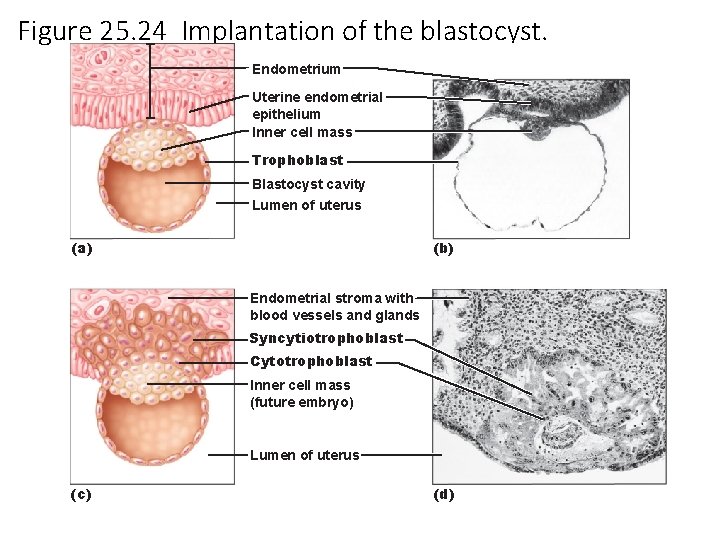
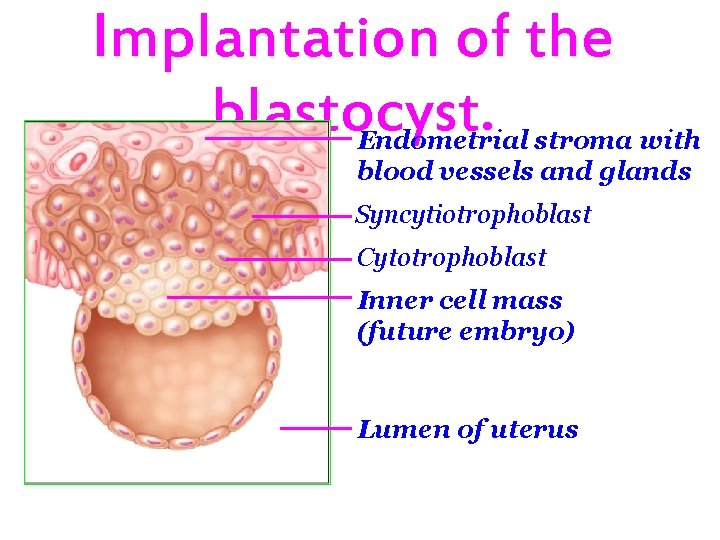
Figure 25. 24 Implantation of the blastocyst. Endometrium Uterine endometrial epithelium Inner cell mass Trophoblast Blastocyst cavity Lumen of uterus (a) (b) Endometrial stroma with blood vessels and glands Syncytiotrophoblast Cytotrophoblast Inner cell mass (future embryo) Lumen of uterus (c) (d)
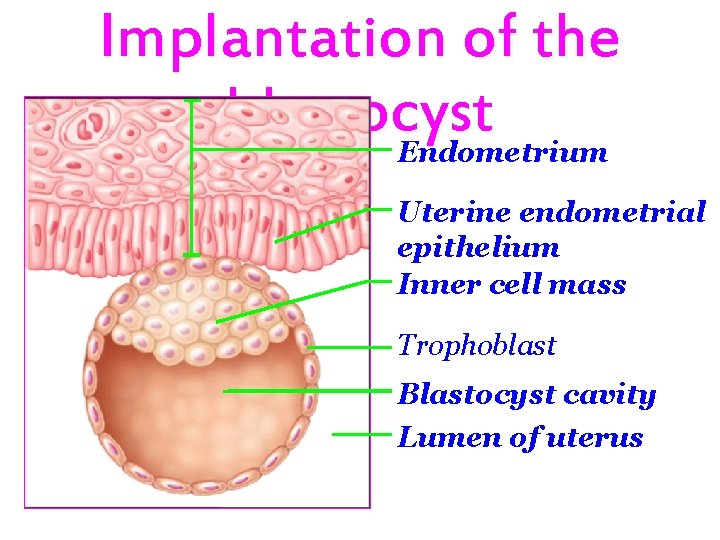
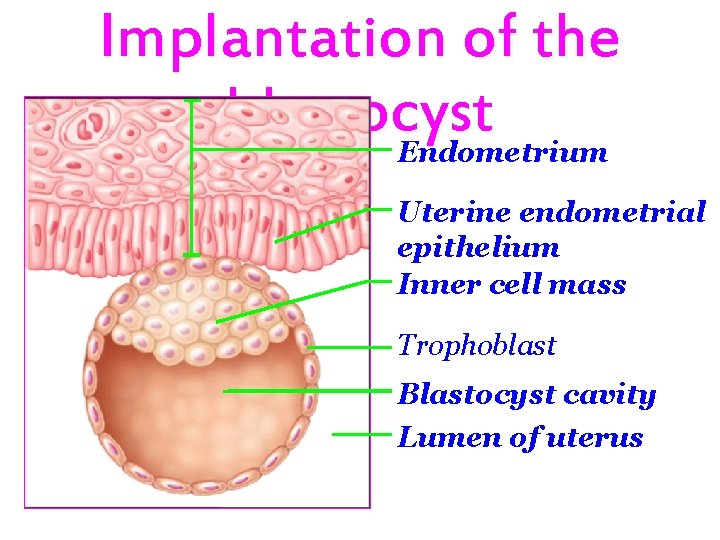
Implantation of the blastocyst Endometrium Uterine endometrial epithelium Inner cell mass Trophoblast Blastocyst cavity Lumen of uterus
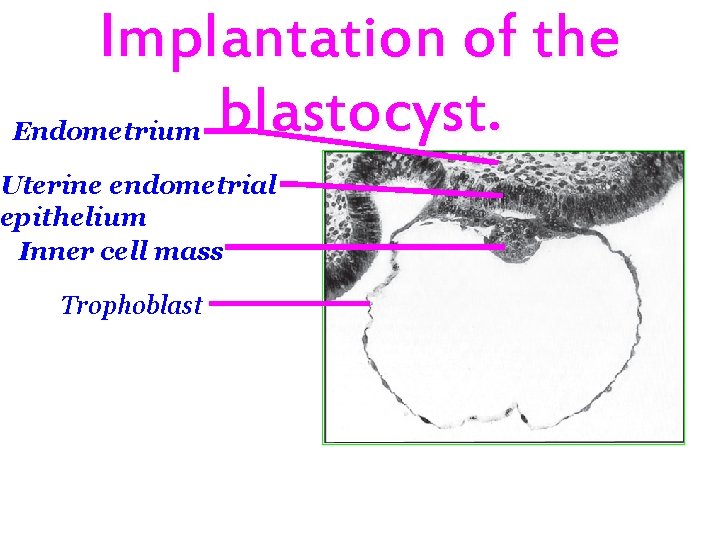
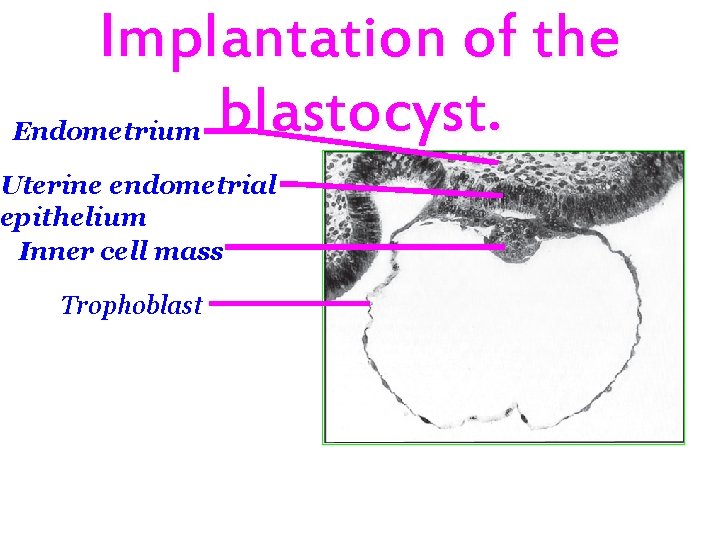
Implantation of the blastocyst. Endometrium Uterine endometrial epithelium Inner cell mass Trophoblast
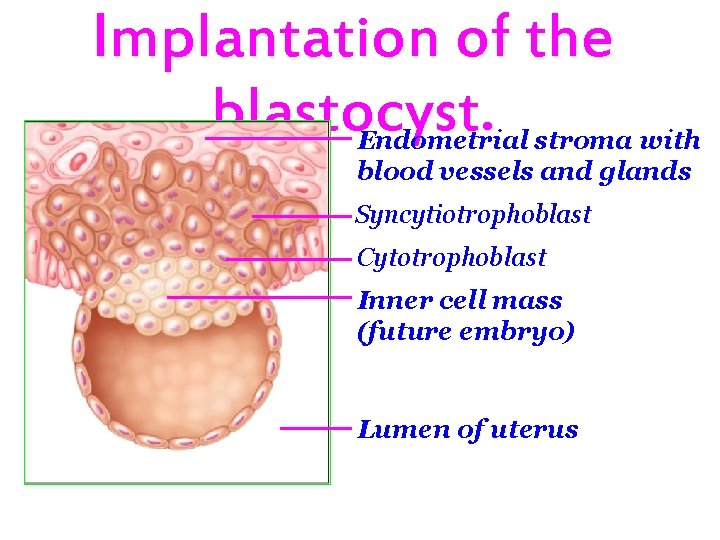
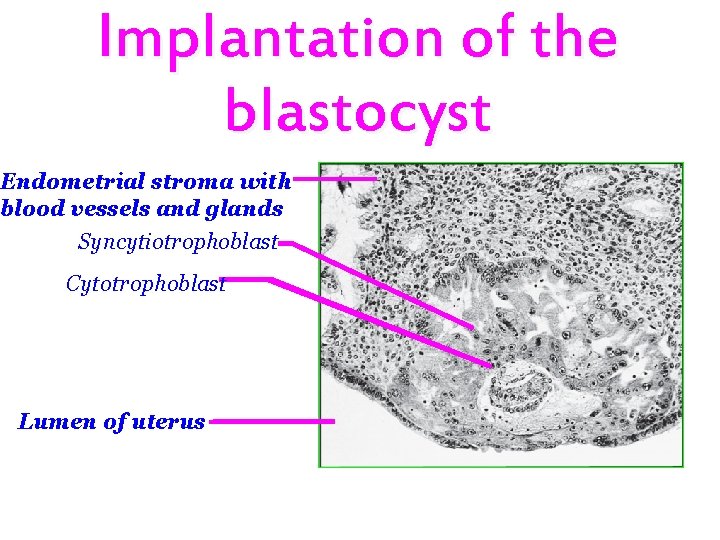
Implantation of the blastocyst. Endometrial stroma with blood vessels and glands Syncytiotrophoblast Cytotrophoblast Inner cell mass (future embryo) Lumen of uterus
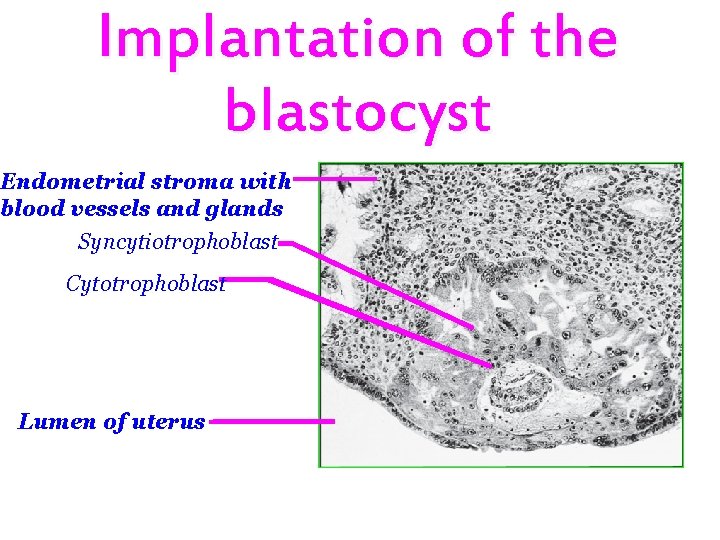
Implantation of the blastocyst Endometrial stroma with blood vessels and glands Syncytiotrophoblast Cytotrophoblast Lumen of uterus
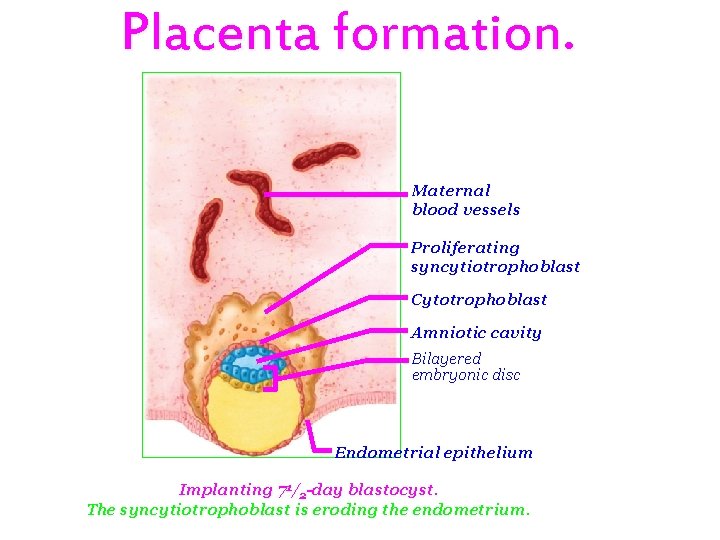
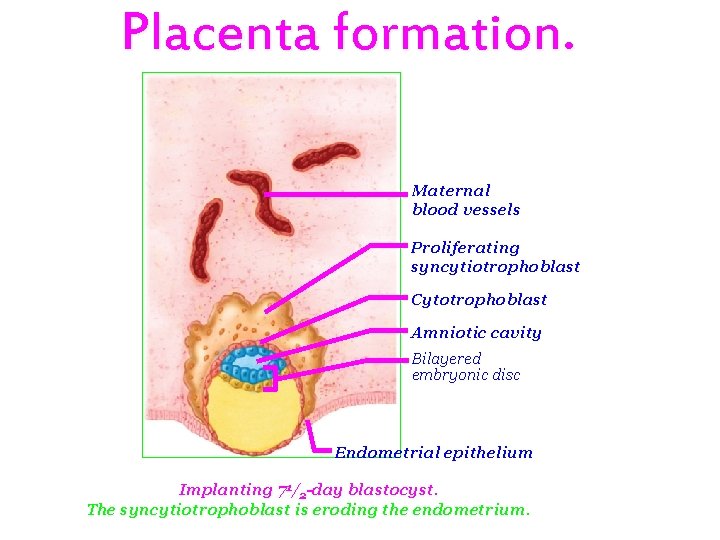
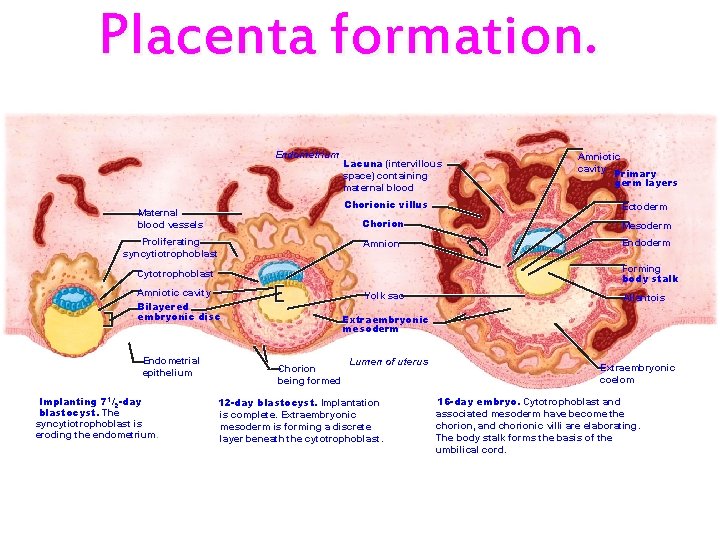
Placenta formation. Maternal blood vessels Proliferating syncytiotrophoblast Cytotrophoblast Amniotic cavity Bilayered embryonic disc Endometrial epithelium Implanting 71/2 -day blastocyst. The syncytiotrophoblast is eroding the endometrium.
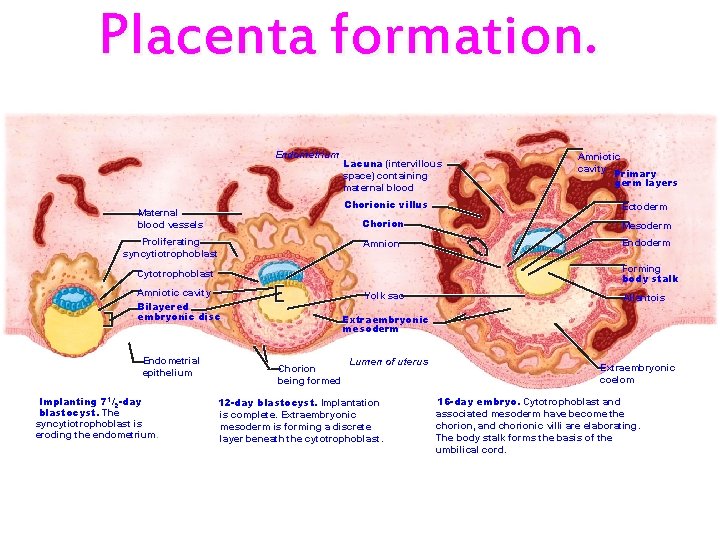
Placenta formation. Endometrium Maternal blood vessels Proliferating syncytiotrophoblast Lacuna (intervillous space) containing maternal blood Chorionic villus Ectoderm Chorion Mesoderm Amnion Endoderm Forming body stalk Cytotrophoblast Amniotic cavity Bilayered embryonic disc Endometrial epithelium Implanting 71/2 -day blastocyst. The syncytiotrophoblast is eroding the endometrium. Amniotic cavity Primary germ layers Yolk sac Allantois Extraembryonic mesoderm Chorion being formed Lumen of uterus 12 -day blastocyst. Implantation is complete. Extraembryonic mesoderm is forming a discrete layer beneath the cytotrophoblast. Extraembryonic coelom 16 -day embryo. Cytotrophoblast and associated mesoderm have become the chorion, and chorionic villi are elaborating. The body stalk forms the basis of the umbilical cord.
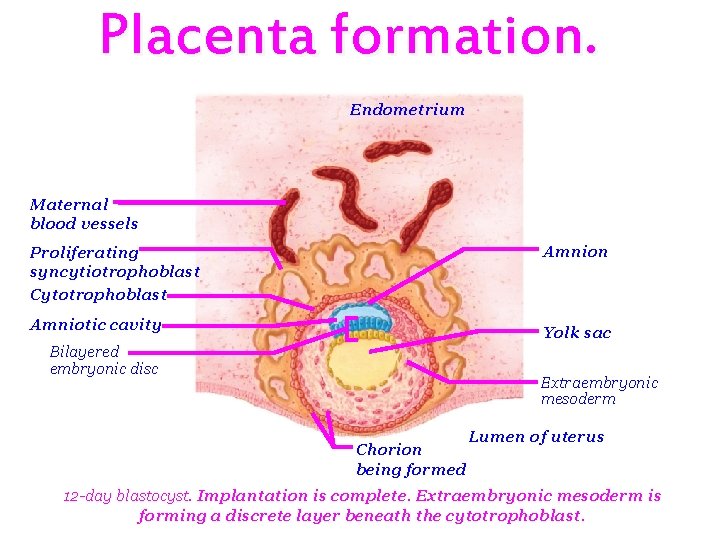
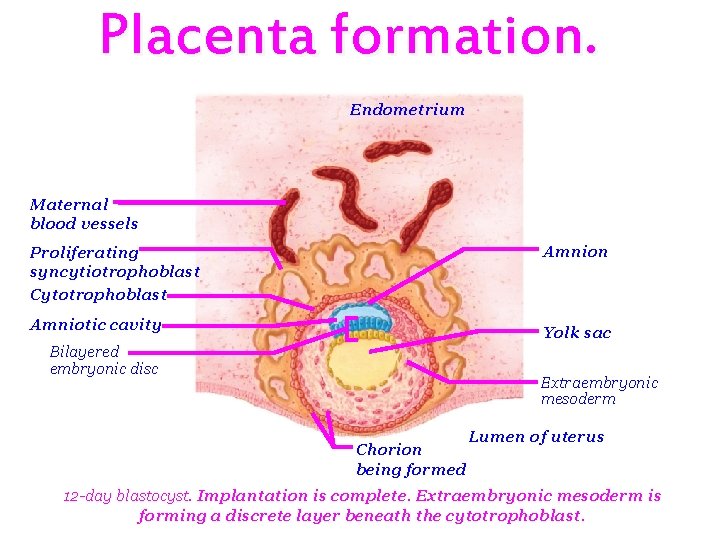
Placenta formation. Endometrium Maternal blood vessels Proliferating syncytiotrophoblast Cytotrophoblast Amnion Amniotic cavity Yolk sac Bilayered embryonic disc Extraembryonic mesoderm Chorion being formed Lumen of uterus 12 -day blastocyst. Implantation is complete. Extraembryonic mesoderm is forming a discrete layer beneath the cytotrophoblast.
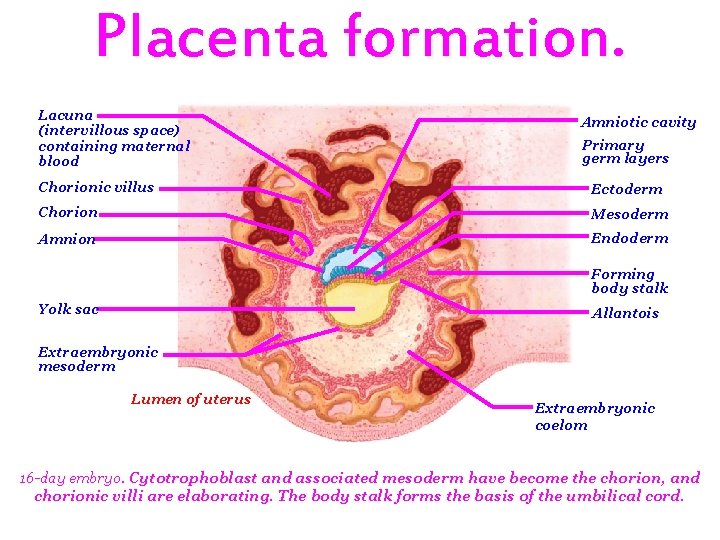
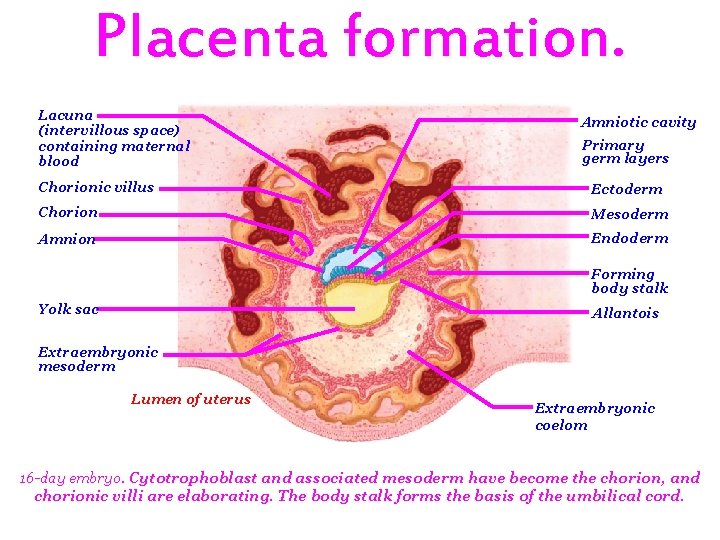
Placenta formation. Lacuna (intervillous space) containing maternal blood Amniotic cavity Primary germ layers Chorionic villus Ectoderm Chorion Mesoderm Amnion Endoderm Forming body stalk Yolk sac Allantois Extraembryonic mesoderm Lumen of uterus Extraembryonic coelom 16 -day embryo. Cytotrophoblast and associated mesoderm have become the chorion, and chorionic villi are elaborating. The body stalk forms the basis of the umbilical cord.
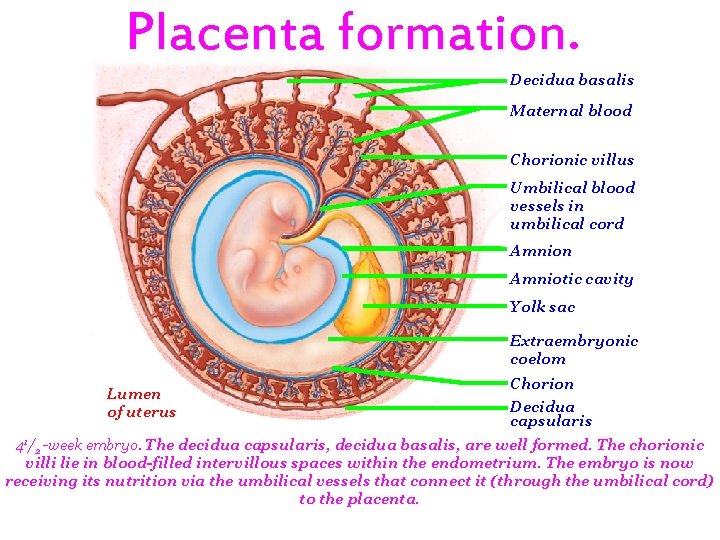
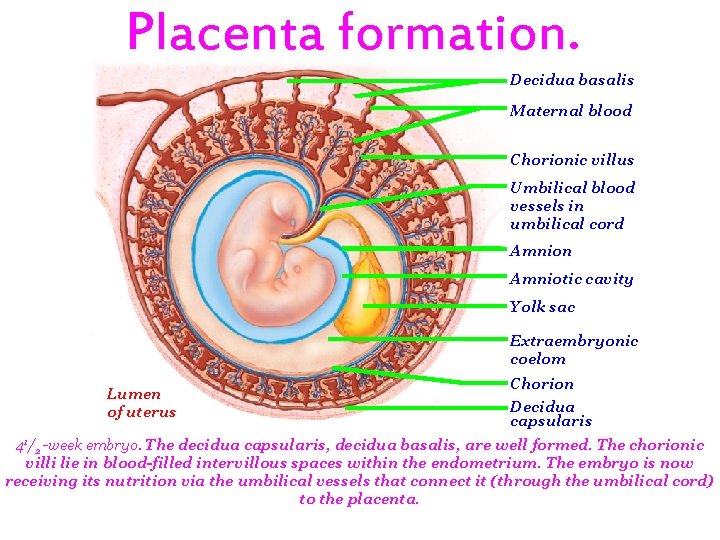
Placenta formation. Decidua basalis Maternal blood Chorionic villus Umbilical blood vessels in umbilical cord Amnion Amniotic cavity Yolk sac Extraembryonic coelom Lumen of uterus Chorion Decidua capsularis 41/2 -week embryo. The decidua capsularis, decidua basalis, are well formed. The chorionic villi lie in blood-filled intervillous spaces within the endometrium. The embryo is now receiving its nutrition via the umbilical vessels that connect it (through the umbilical cord) to the placenta.
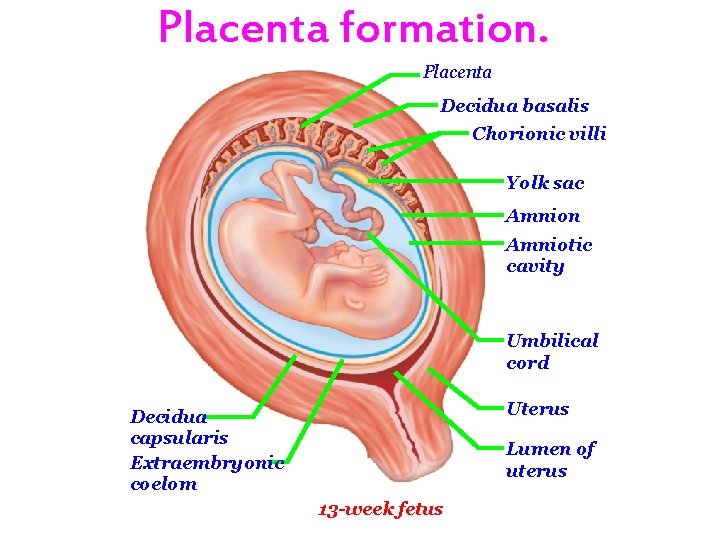
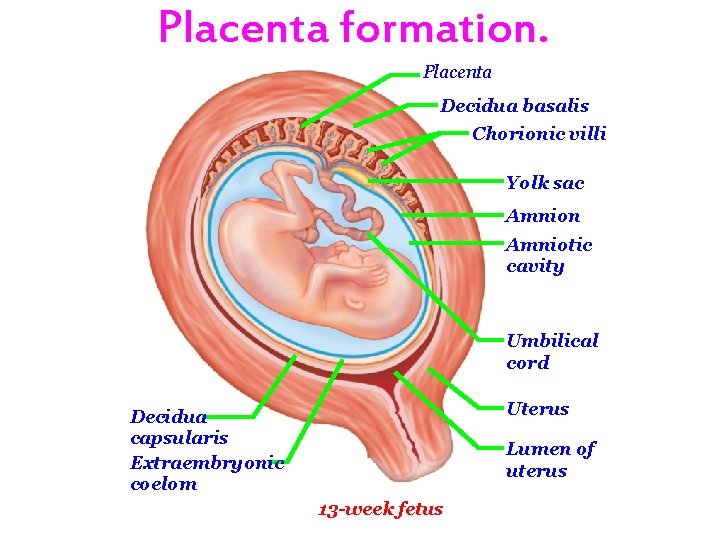
Placenta formation. Placenta Decidua basalis Chorionic villi Yolk sac Amnion Amniotic cavity Umbilical cord Uterus Decidua capsularis Extraembryonic coelom Lumen of uterus 13 -week fetus

Vascular relationships in the placenta. Placenta Chorionic villi Decidua basalis Maternal arteries Maternal veins Myometrium Umbilical cord Decidua capsularis Uterus Lumen of uterus Chorionic villus containing fetal capillaries Maternal blood in lacuna (intervillous space) Fetal arteriole Fetal venule Amnion Umbilical cord Stratum basalis of endometrium Maternal portion of placenta (decidua basalis) Fetal portion of placenta (chorion) Umbilical arteries Umbilical vein Connection to yolk sac
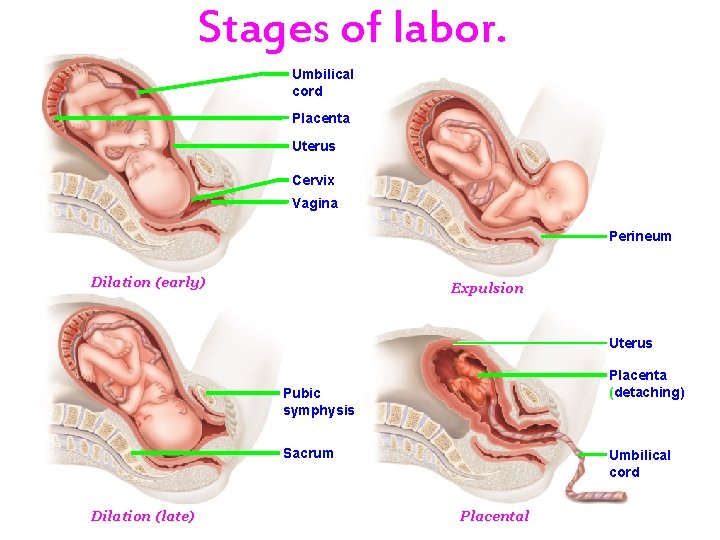
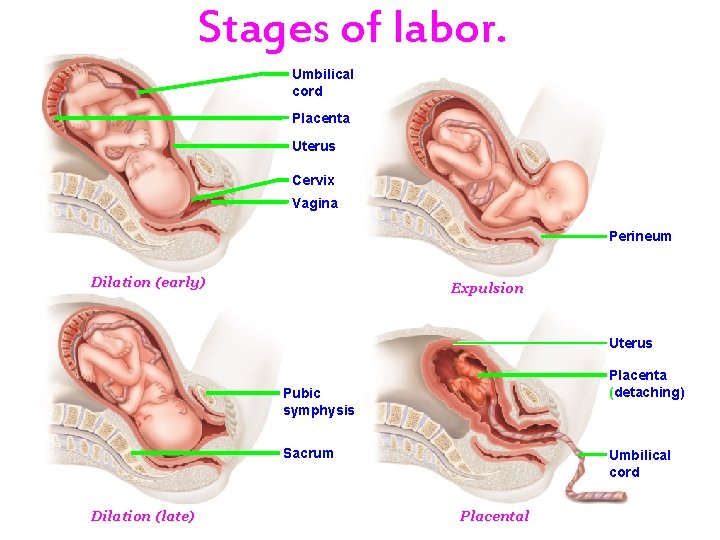
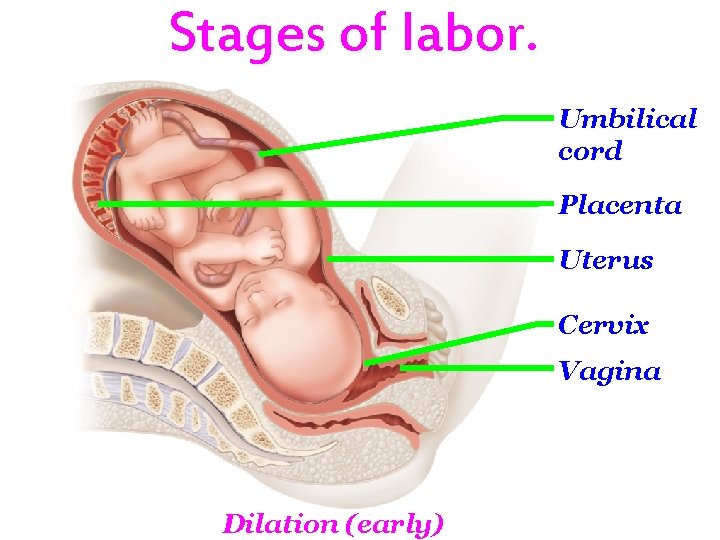
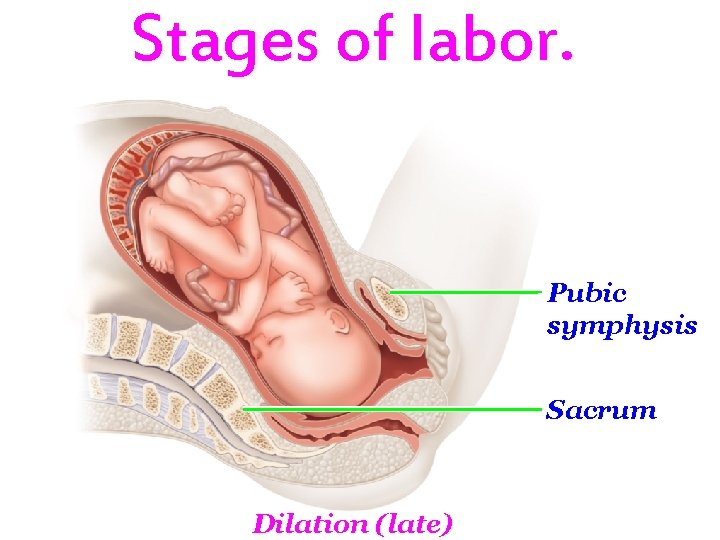
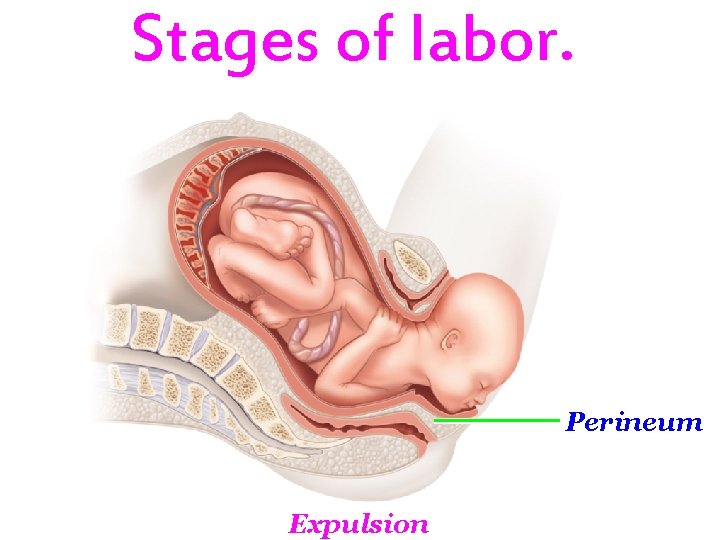
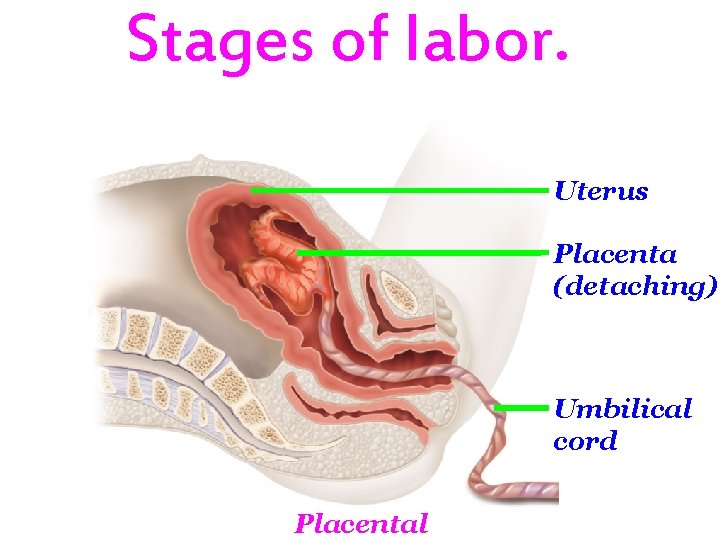
Stages of labor. Umbilical cord Placenta Uterus Cervix Vagina Perineum Dilation (early) Expulsion Uterus Placenta (detaching) Pubic symphysis Sacrum Dilation (late) Umbilical cord Placental
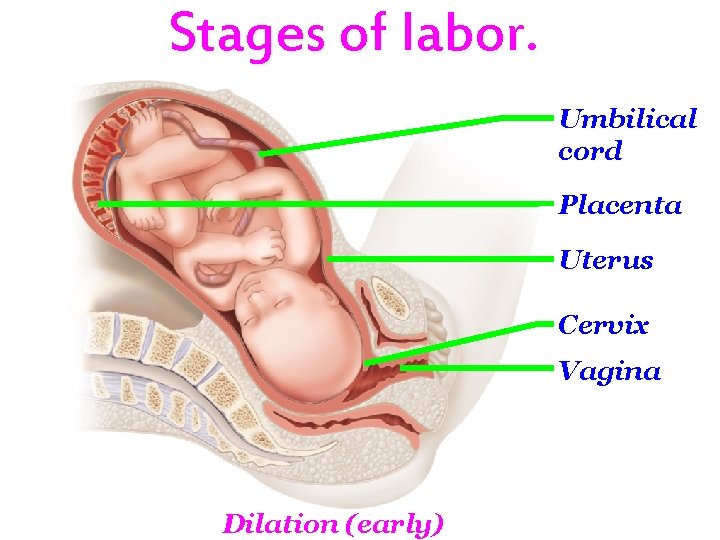
Stages of labor. Umbilical cord Placenta Uterus Cervix Vagina Dilation (early)
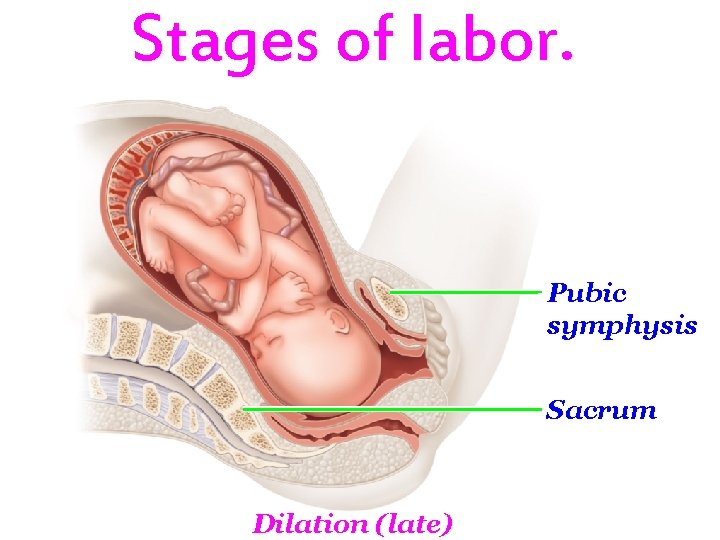
Stages of labor. Pubic symphysis Sacrum Dilation (late)
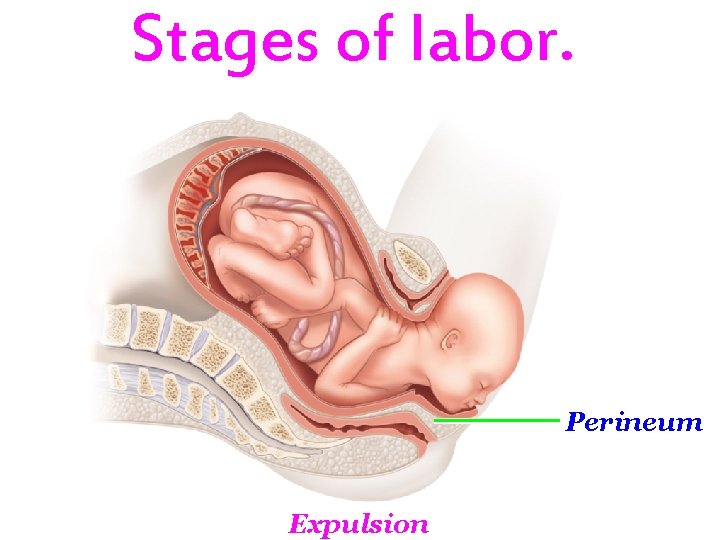
Stages of labor. Perineum Expulsion
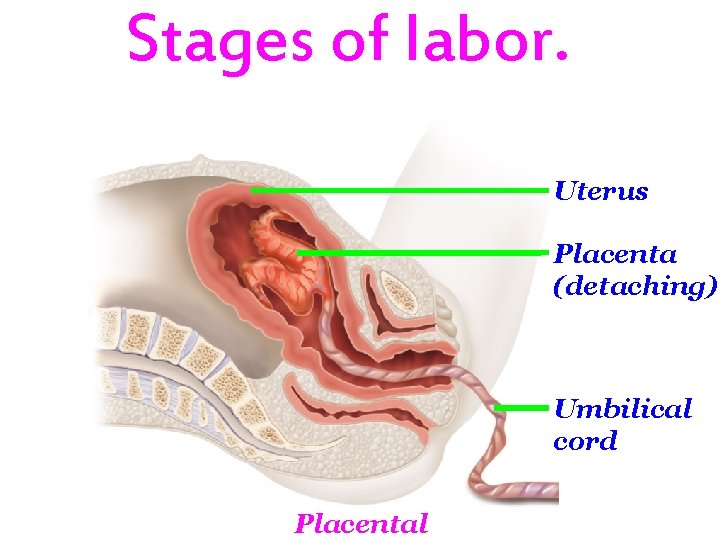
Stages of labor. Uterus Placenta (detaching) Umbilical cord Placental

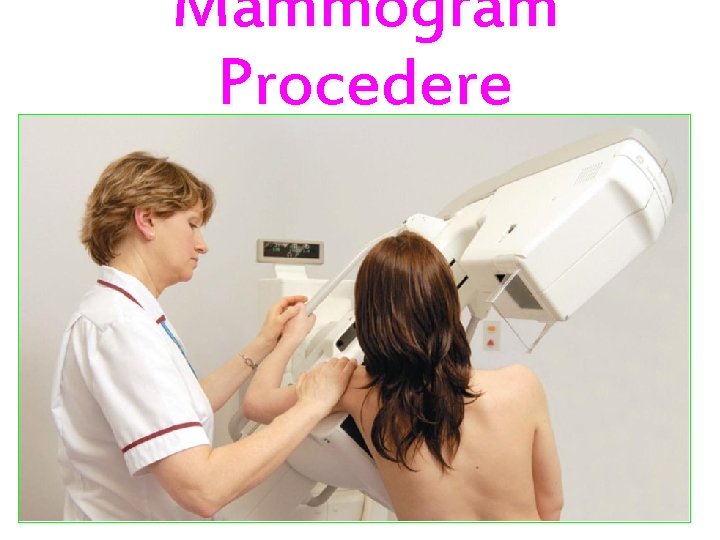
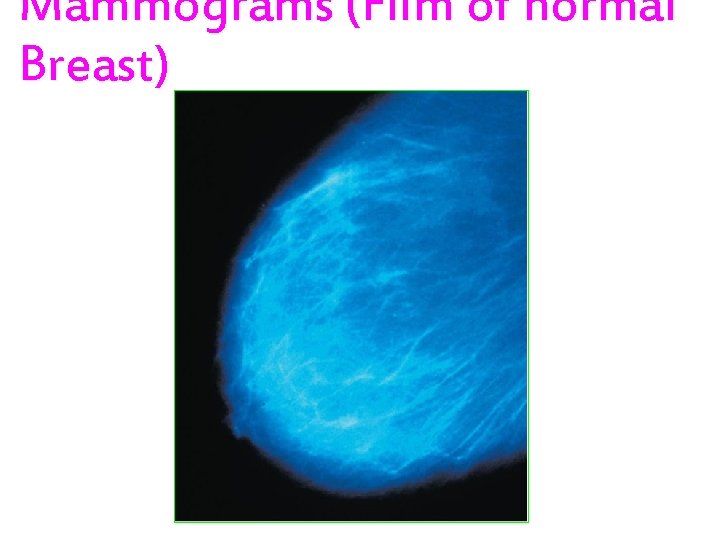
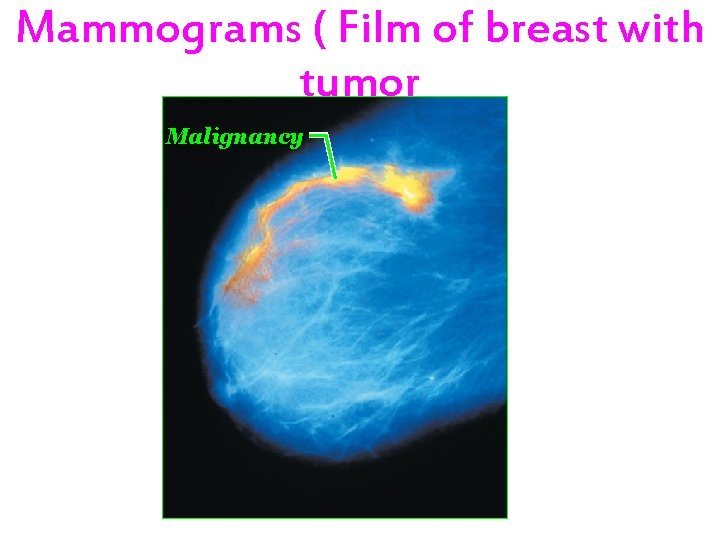
Mammograms. Mammogram procedure Malignancy Film of normal breast Film of breast with tumor
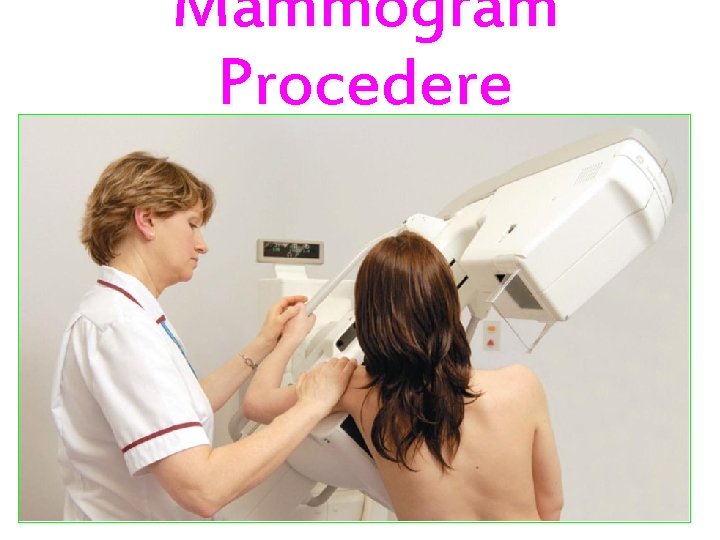
Mammogram Procedere
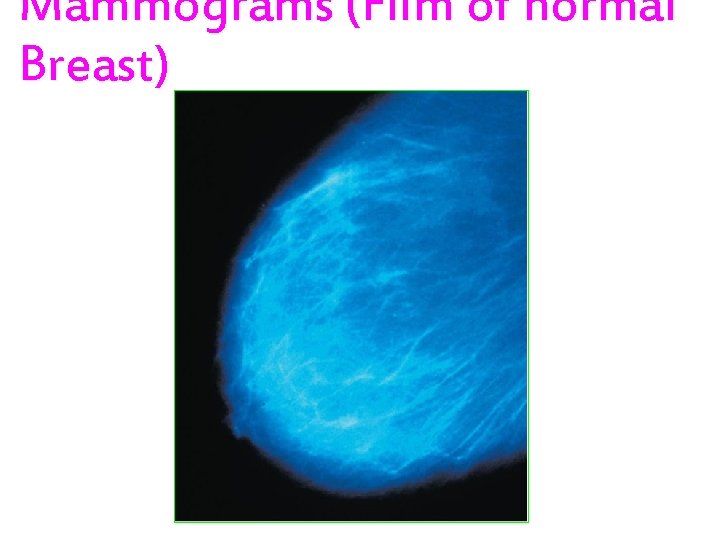
Mammograms (Film of normal Breast)
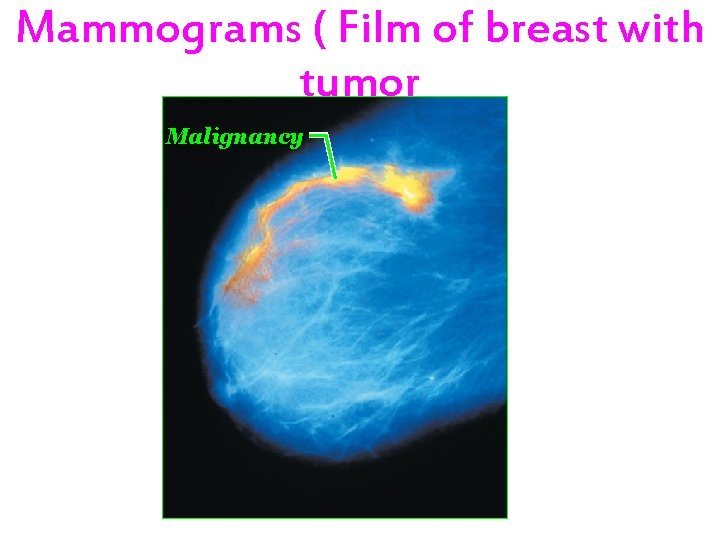
Mammograms ( Film of breast with tumor Malignancy
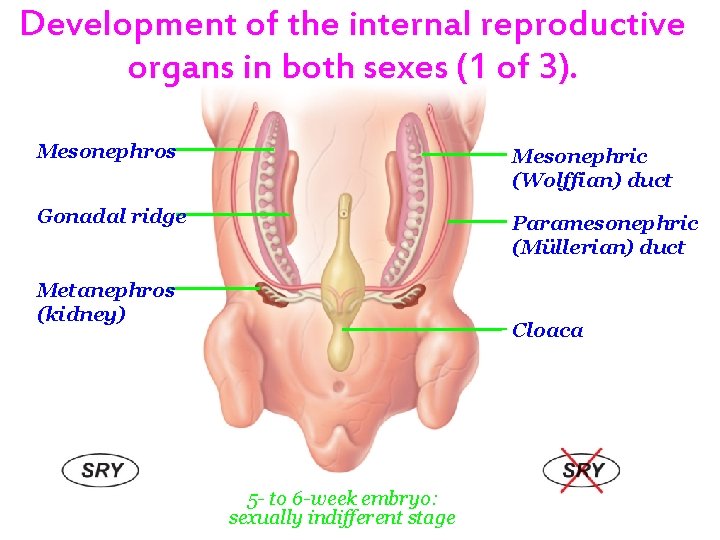
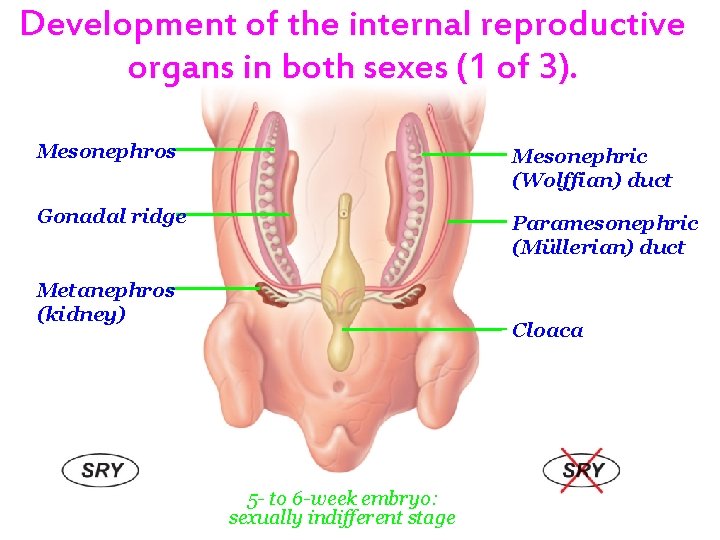
Development of the internal reproductive organs in both sexes (1 of 3). Mesonephros Mesonephric (Wolffian) duct Gonadal ridge Paramesonephric (Müllerian) duct Metanephros (kidney) Cloaca 5 - to 6 -week embryo: sexually indifferent stage
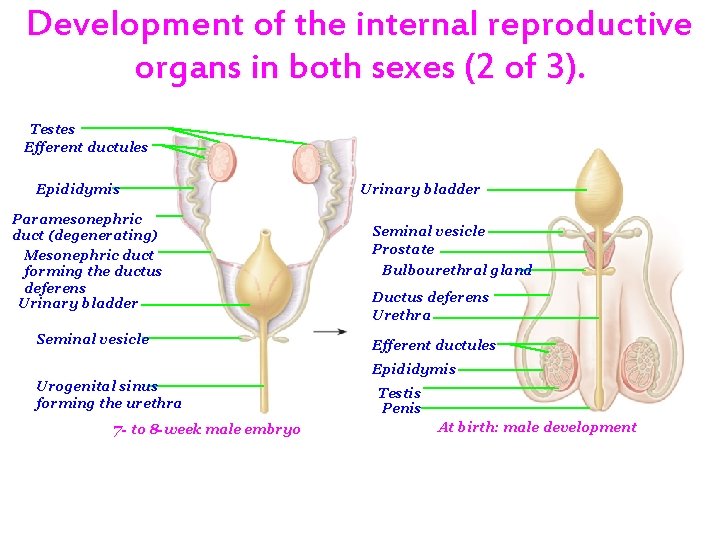
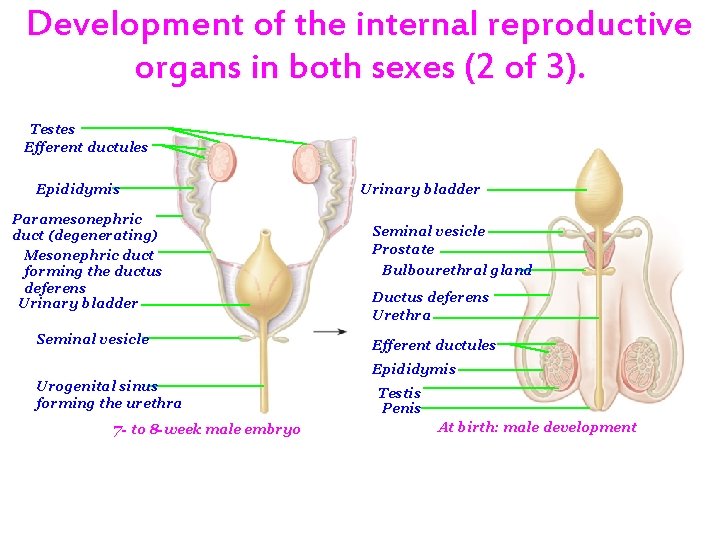
Development of the internal reproductive organs in both sexes (2 of 3). Testes Efferent ductules Epididymis Paramesonephric duct (degenerating) Mesonephric duct forming the ductus deferens Urinary bladder Seminal vesicle Prostate Bulbourethral gland Ductus deferens Urethra Efferent ductules Epididymis Urogenital sinus forming the urethra 7 - to 8 -week male embryo Testis Penis At birth: male development
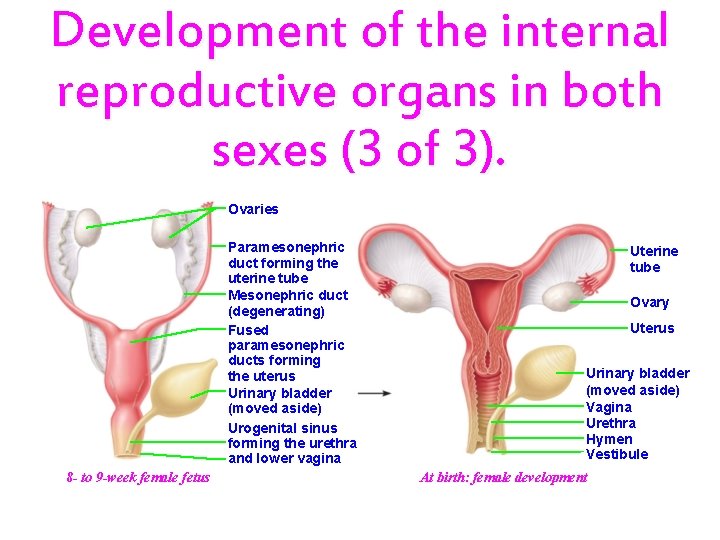
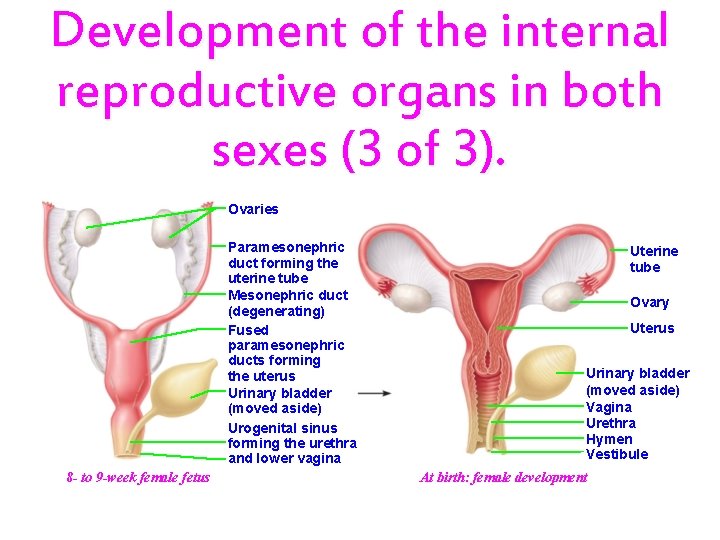
Development of the internal reproductive organs in both sexes (3 of 3). Ovaries Paramesonephric duct forming the uterine tube Mesonephric duct (degenerating) Fused paramesonephric ducts forming the uterus Urinary bladder (moved aside) Urogenital sinus forming the urethra and lower vagina 8 - to 9 -week female fetus Uterine tube Ovary Uterus Urinary bladder (moved aside) Vagina Urethra Hymen Vestibule At birth: female development
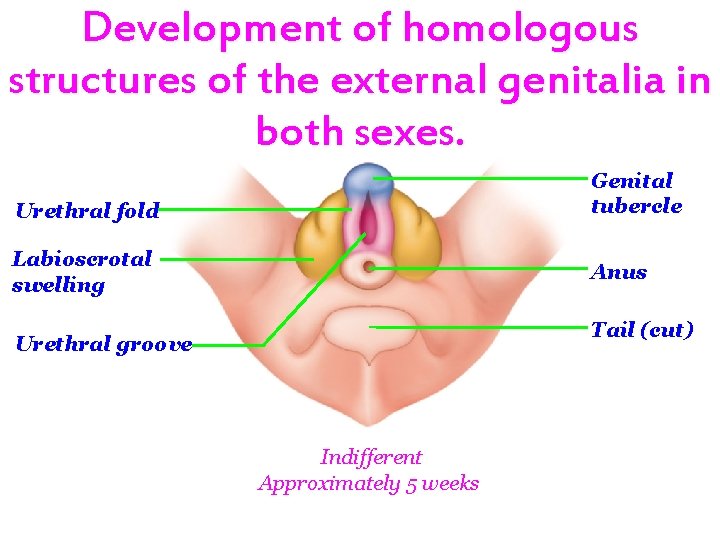
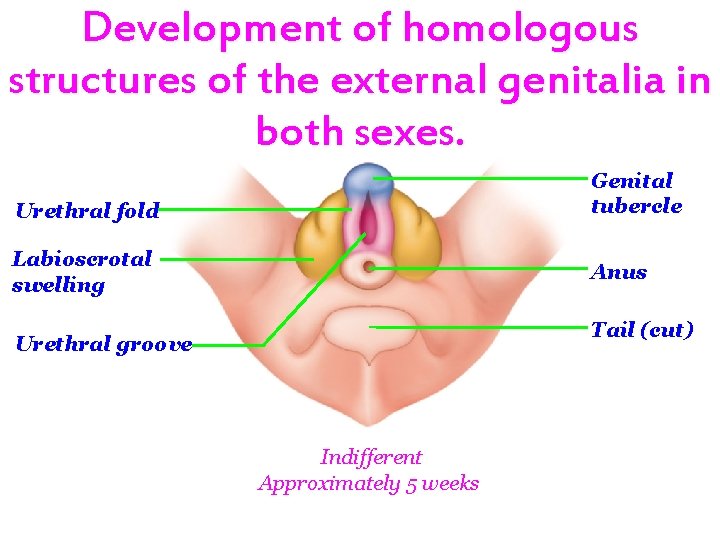
Development of homologous structures of the external genitalia in both sexes. Genital tubercle Urethral fold Labioscrotal swelling Anus Tail (cut) Urethral groove Indifferent Approximately 5 weeks
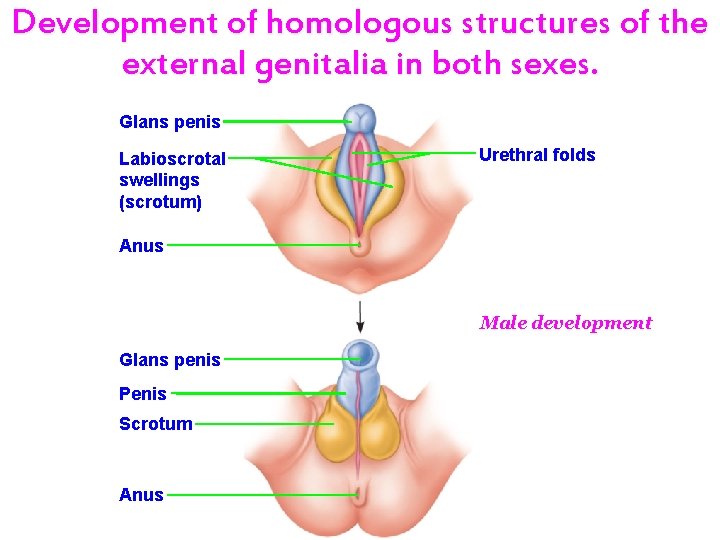
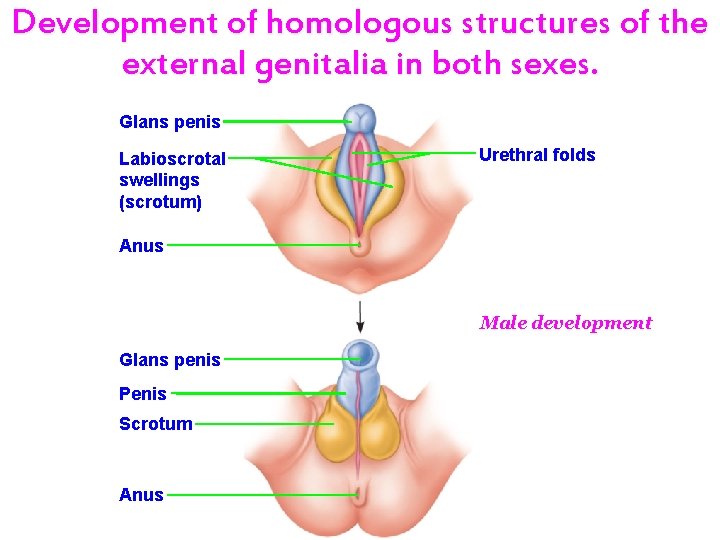
Development of homologous structures of the external genitalia in both sexes. Glans penis Labioscrotal swellings (scrotum) Urethral folds Anus Male development Glans penis Penis Scrotum Anus
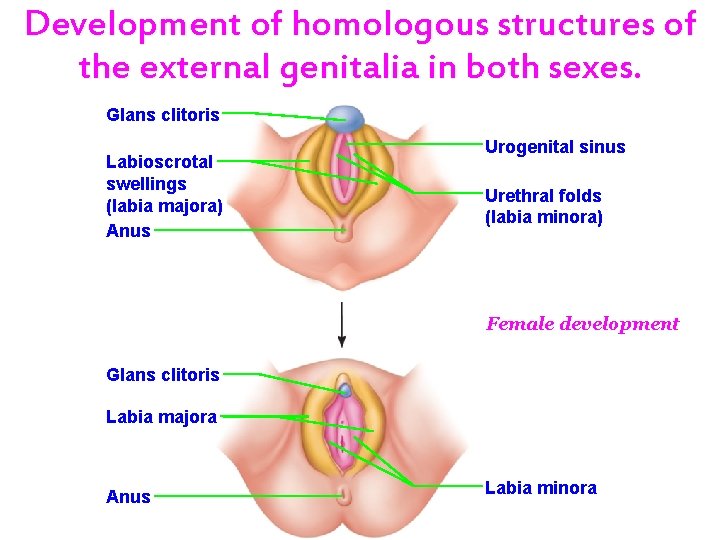
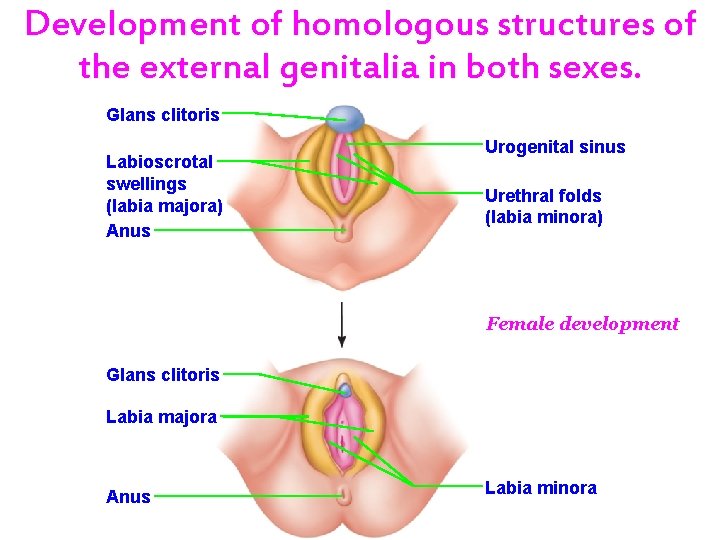
Development of homologous structures of the external genitalia in both sexes. Glans clitoris Labioscrotal swellings (labia majora) Anus Urogenital sinus Urethral folds (labia minora) Female development Glans clitoris Labia majora Anus Labia minora
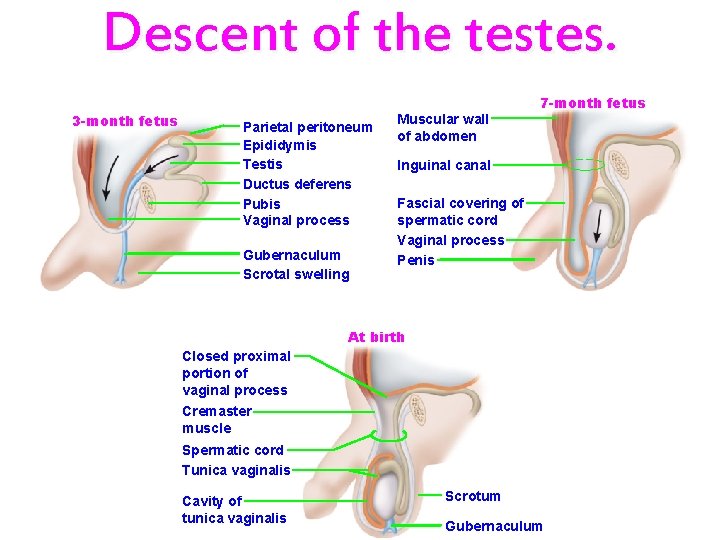
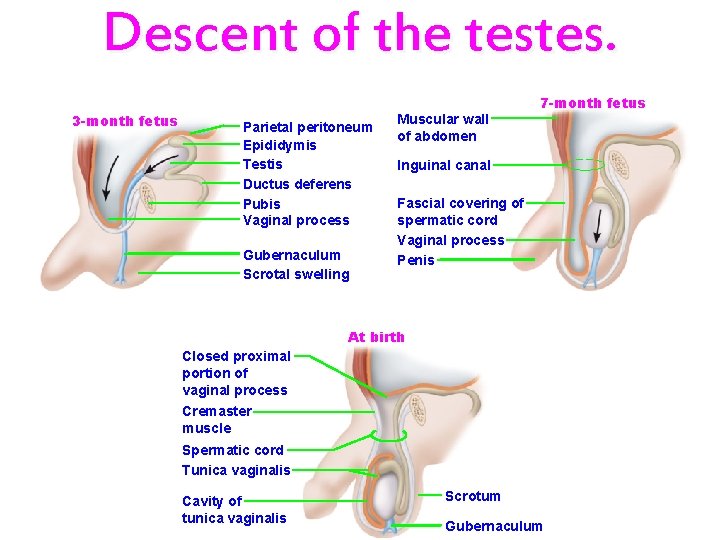
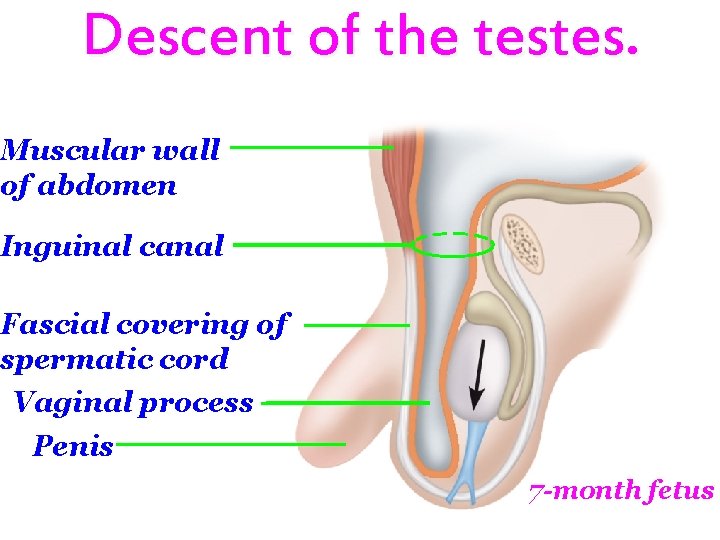
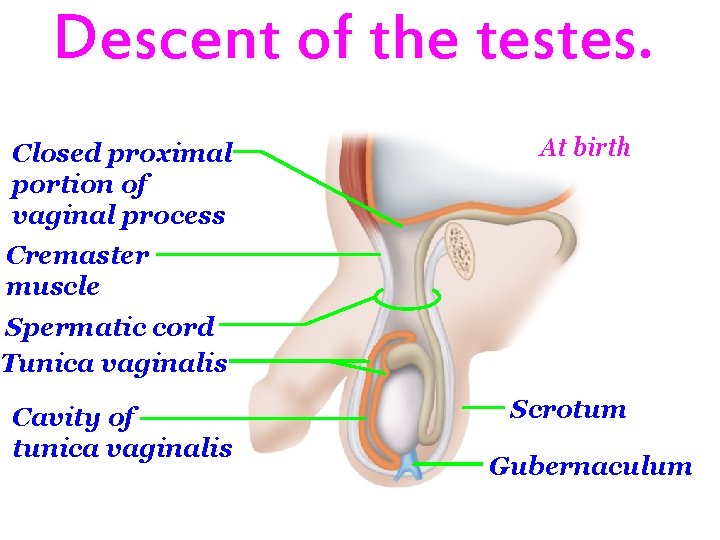
Descent of the testes. 3 -month fetus Parietal peritoneum Epididymis Testis Ductus deferens Pubis Vaginal process Gubernaculum Scrotal swelling Muscular wall of abdomen 7 -month fetus Inguinal canal Fascial covering of spermatic cord Vaginal process Penis At birth Closed proximal portion of vaginal process Cremaster muscle Spermatic cord Tunica vaginalis Cavity of tunica vaginalis Scrotum Gubernaculum
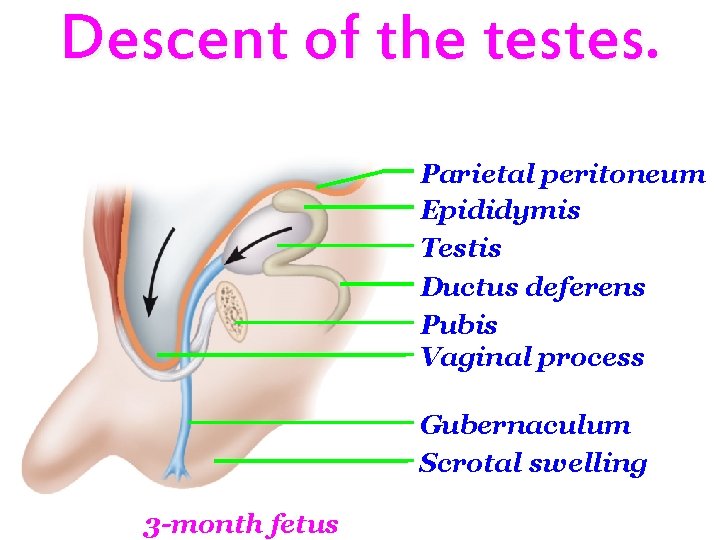
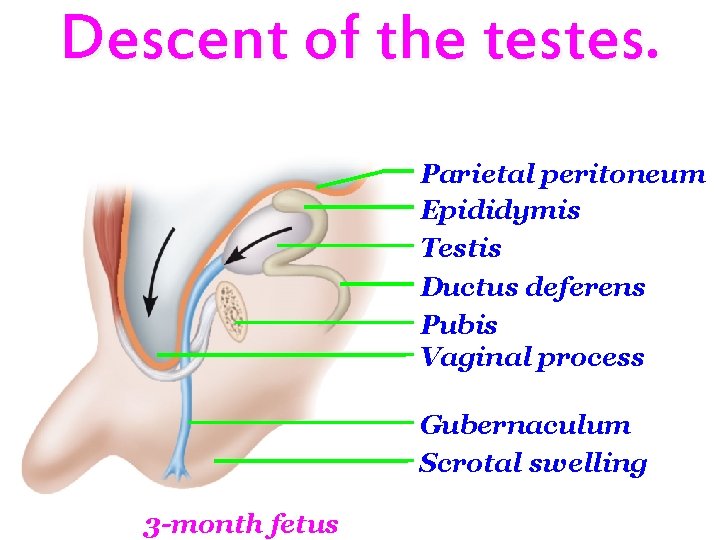
Descent of the testes. Parietal peritoneum Epididymis Testis Ductus deferens Pubis Vaginal process Gubernaculum Scrotal swelling 3 -month fetus
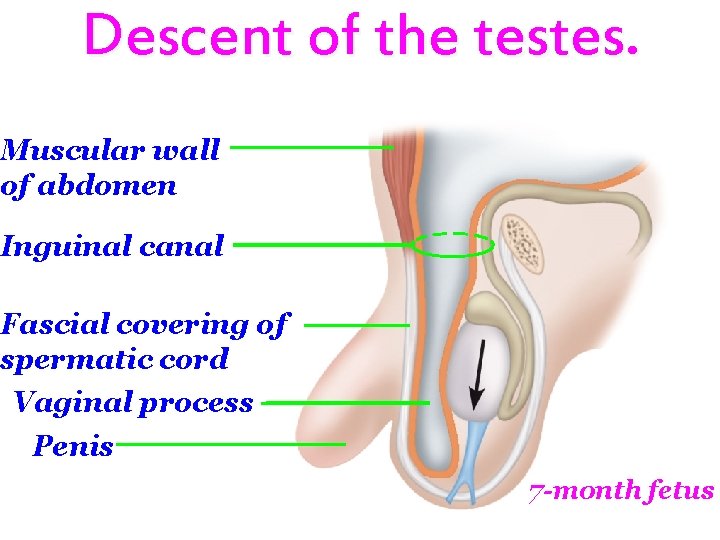
Descent of the testes. Muscular wall of abdomen Inguinal canal Fascial covering of spermatic cord Vaginal process Penis 7 -month fetus
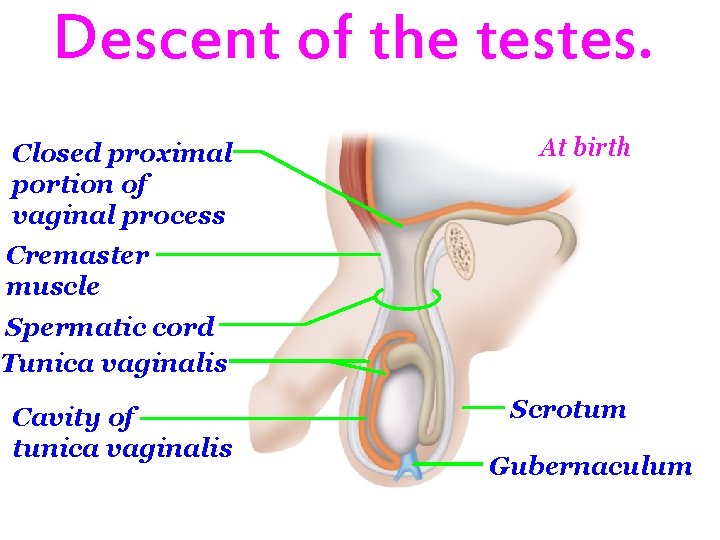
Descent of the testes. Closed proximal portion of vaginal process At birth Cremaster muscle Spermatic cord Tunica vaginalis Cavity of tunica vaginalis Scrotum Gubernaculum

h T E e d n