FEMALE REPRODUCTIVE ORGANS DR STUTI TANDON ASSISTANT PROFESSOR
- Slides: 63
FEMALE REPRODUCTIVE ORGANS DR. STUTI TANDON ASSISTANT PROFESSOR DEPARTMENT OF ANATOMY CIMS&H
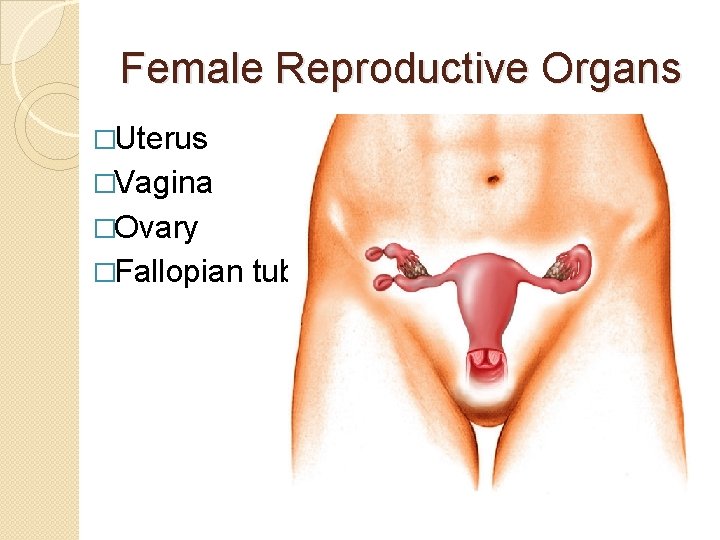
Female Reproductive Organs �Uterus �Vagina �Ovary �Fallopian tube
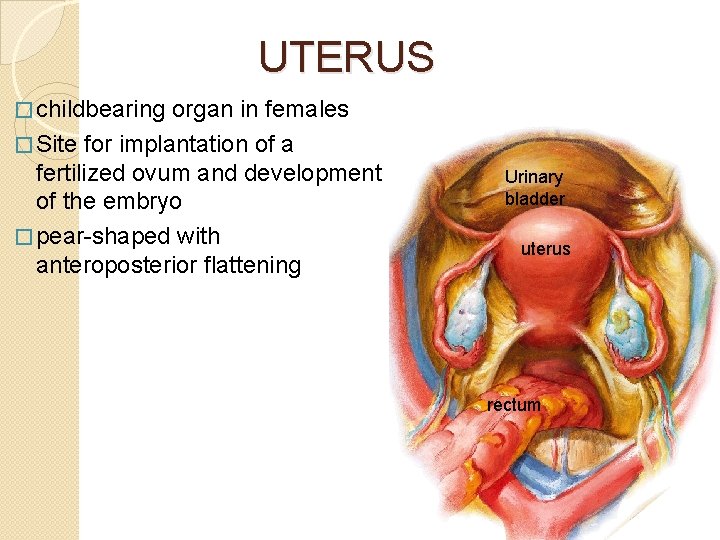
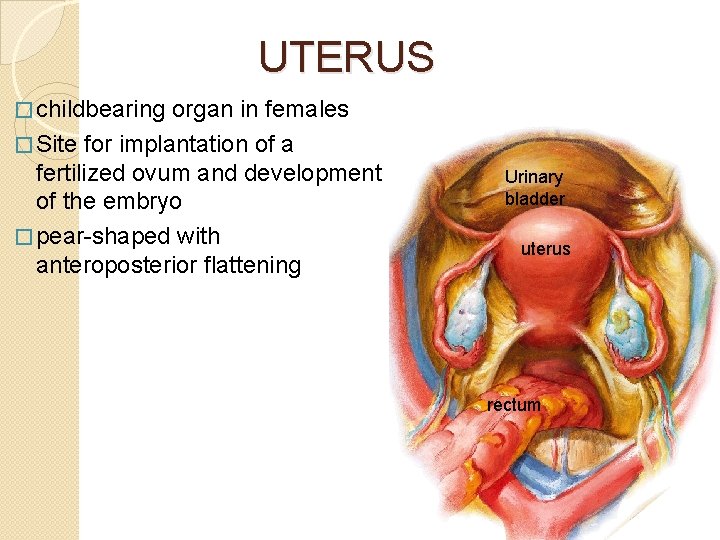
UTERUS � childbearing organ in females � Site for implantation of a fertilized ovum and development of the embryo � pear-shaped with anteroposterior flattening Urinary bladder uterus rectum
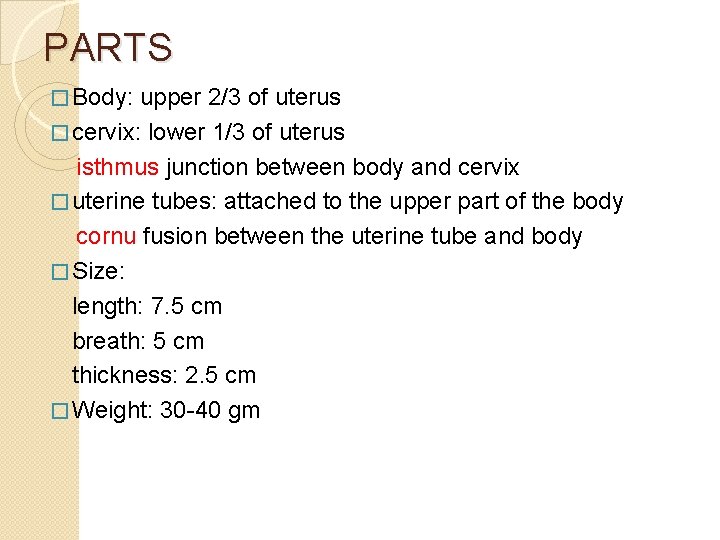
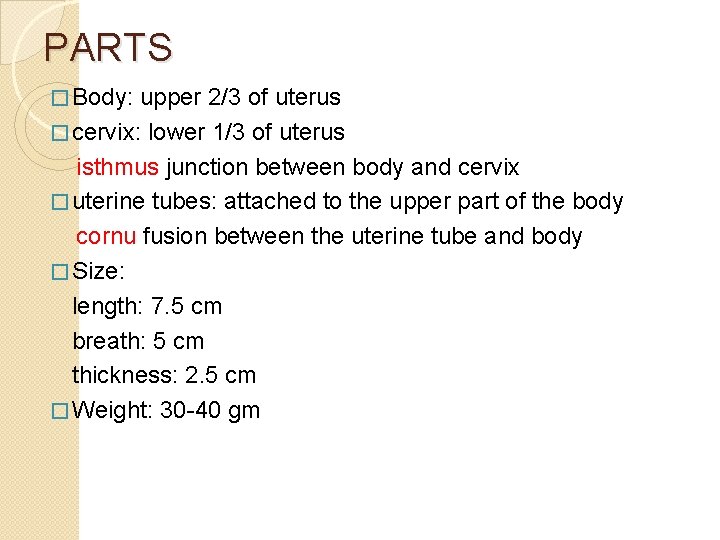
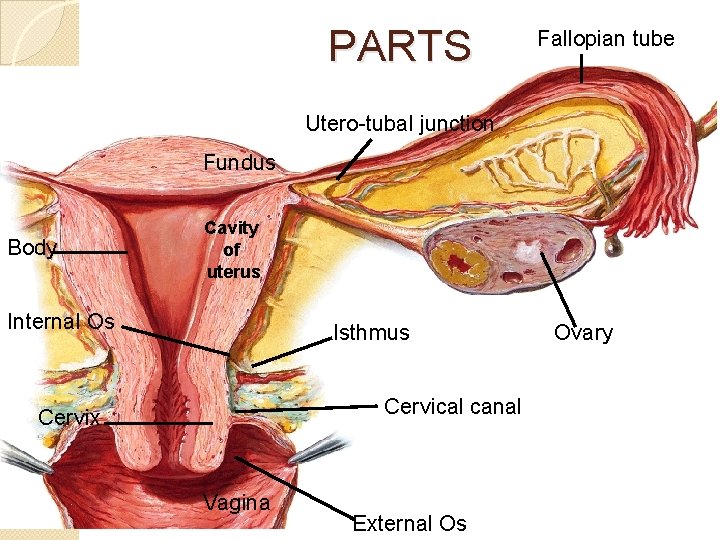
PARTS � Body: upper 2/3 of uterus � cervix: lower 1/3 of uterus isthmus junction between body and cervix � uterine tubes: attached to the upper part of the body cornu fusion between the uterine tube and body � Size: length: 7. 5 cm breath: 5 cm thickness: 2. 5 cm � Weight: 30 -40 gm
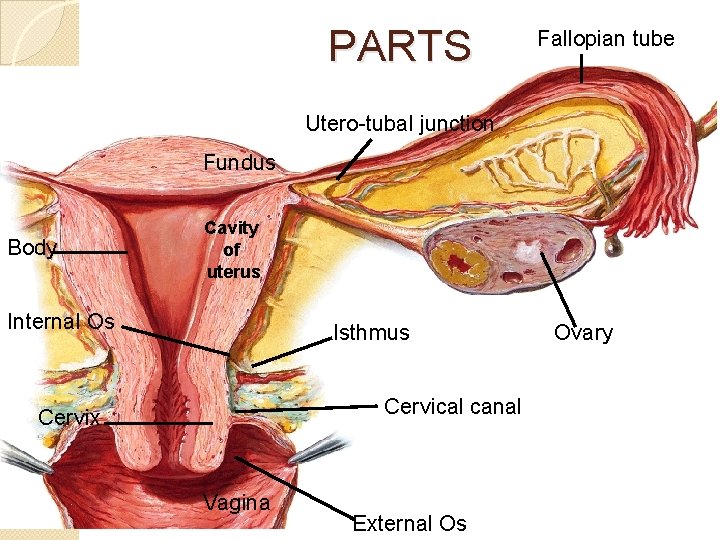
PARTS Fallopian tube Utero-tubal junction Fundus Body Cavity of uterus Internal Os Isthmus Cervical canal Cervix Vagina External Os Ovary
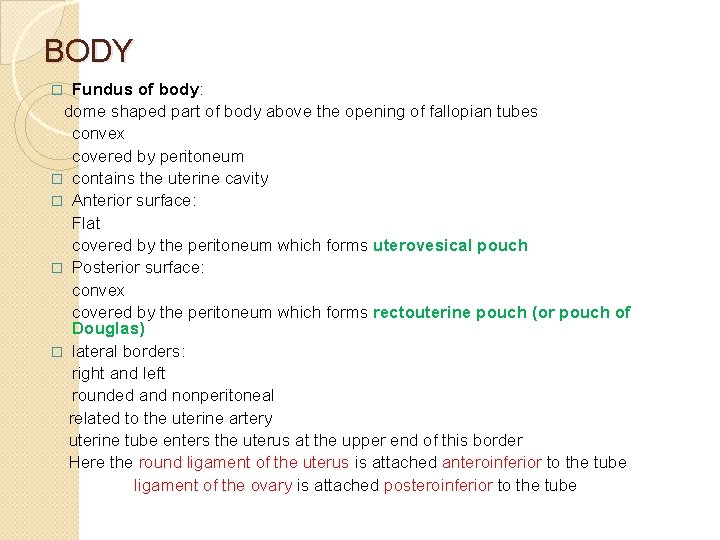
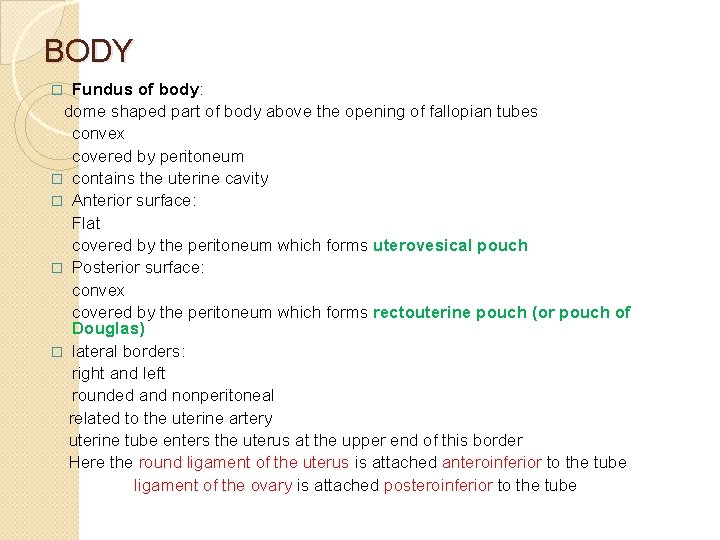
BODY Fundus of body: dome shaped part of body above the opening of fallopian tubes convex covered by peritoneum � contains the uterine cavity � Anterior surface: Flat covered by the peritoneum which forms uterovesical pouch � Posterior surface: convex covered by the peritoneum which forms rectouterine pouch (or pouch of Douglas) � lateral borders: right and left rounded and nonperitoneal related to the uterine artery uterine tube enters the uterus at the upper end of this border Here the round ligament of the uterus is attached anteroinferior to the tube ligament of the ovary is attached posteroinferior to the tube �
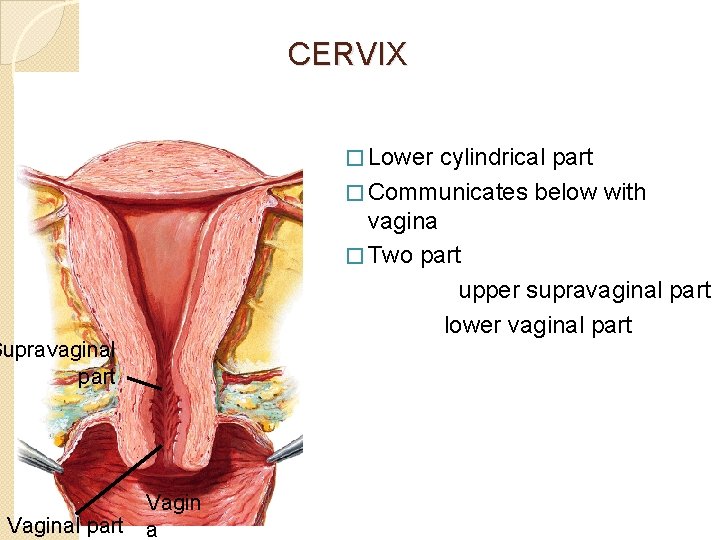
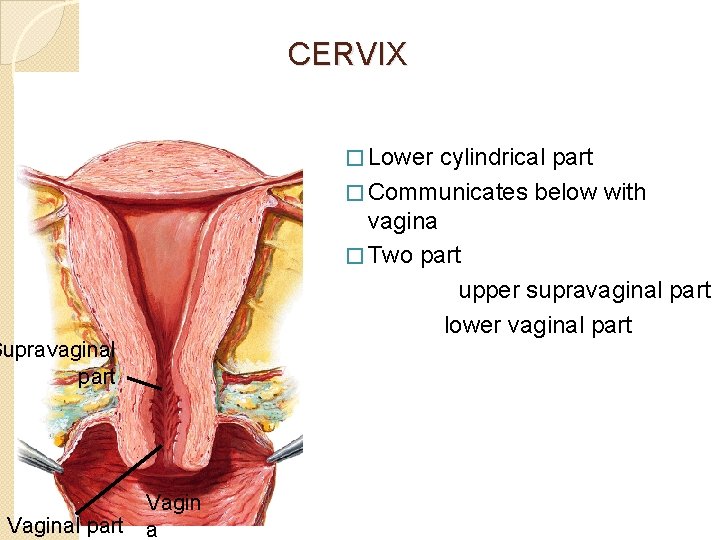
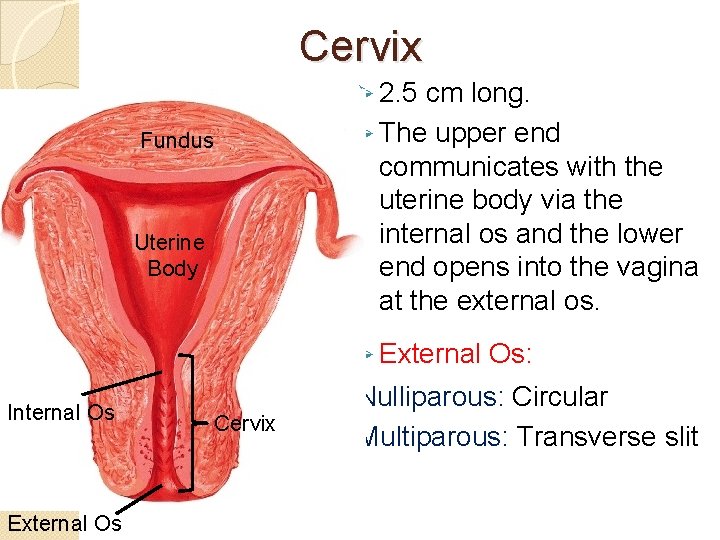
CERVIX � Lower Supravaginal part Vaginal part a cylindrical part � Communicates below with vagina � Two part upper supravaginal part lower vaginal part
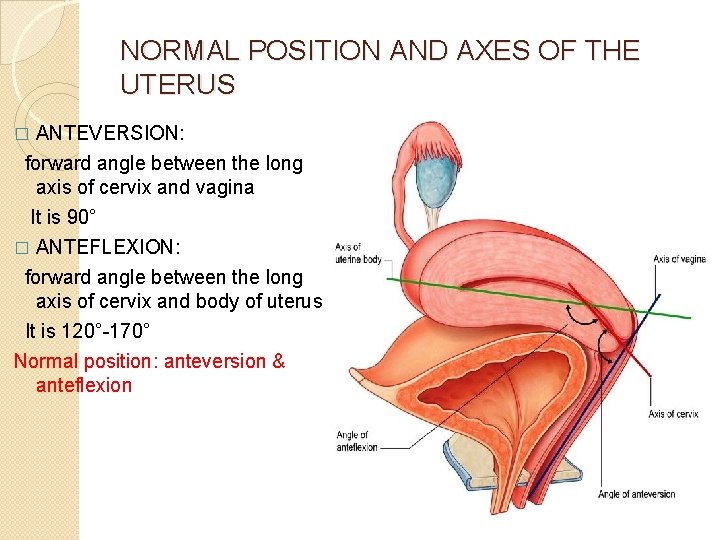
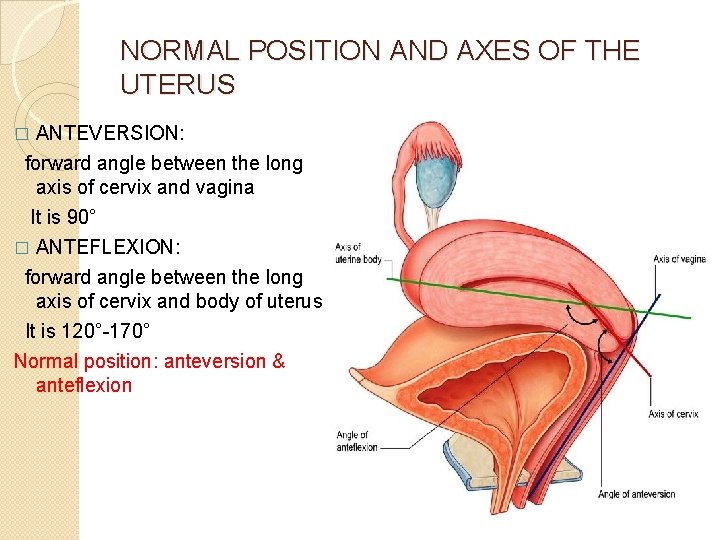
NORMAL POSITION AND AXES OF THE UTERUS ANTEVERSION: forward angle between the long axis of cervix and vagina It is 90° � ANTEFLEXION: forward angle between the long axis of cervix and body of uterus It is 120°-170° Normal position: anteversion & anteflexion �
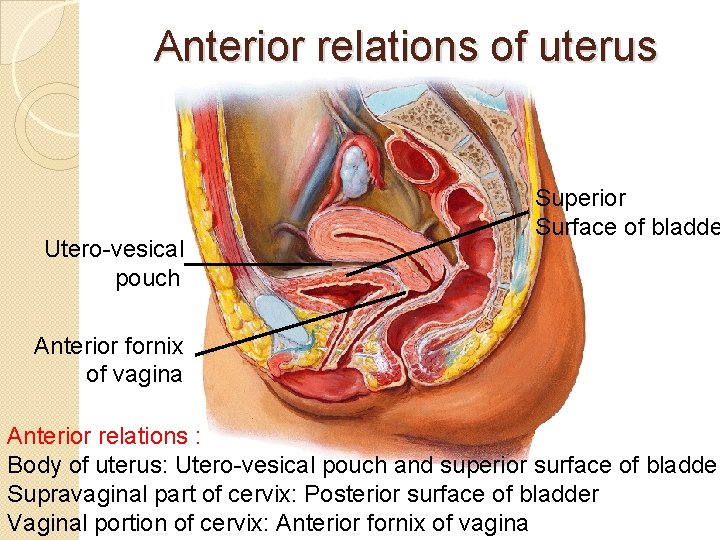
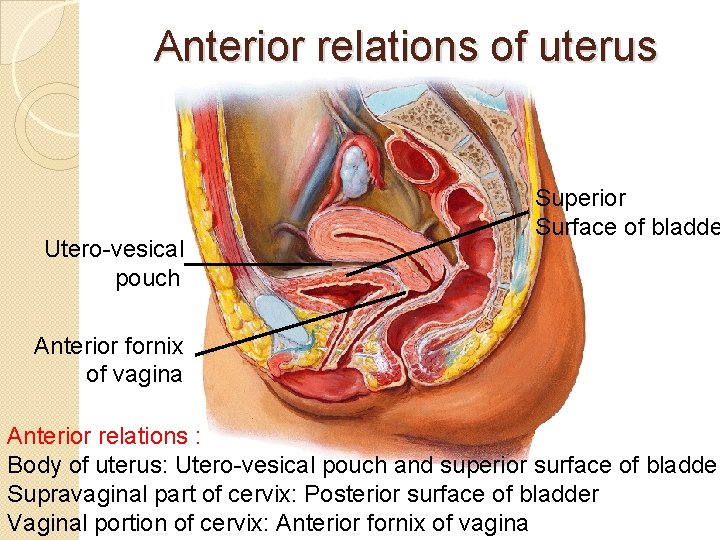
Anterior relations of uterus Utero-vesical pouch Superior Surface of bladde Anterior fornix of vagina Anterior relations : Body of uterus: Utero-vesical pouch and superior surface of bladder Supravaginal part of cervix: Posterior surface of bladder Vaginal portion of cervix: Anterior fornix of vagina
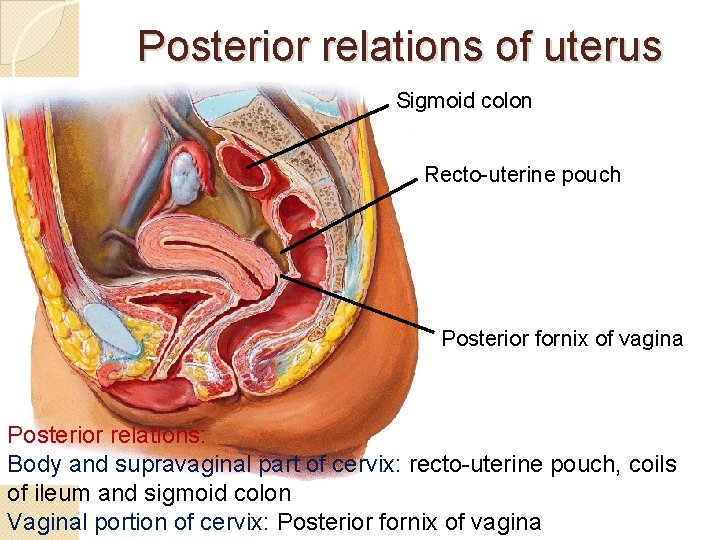
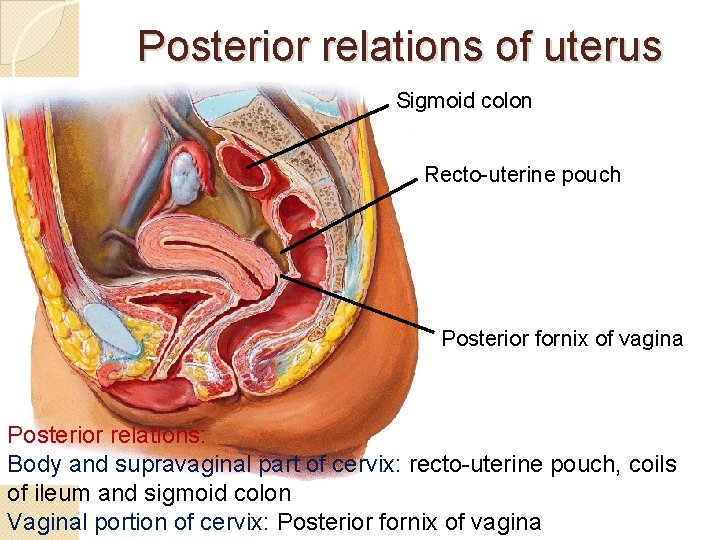
Posterior relations of uterus Sigmoid colon Recto-uterine pouch Posterior fornix of vagina Posterior relations: Body and supravaginal part of cervix: recto-uterine pouch, coils of ileum and sigmoid colon Vaginal portion of cervix: Posterior fornix of vagina
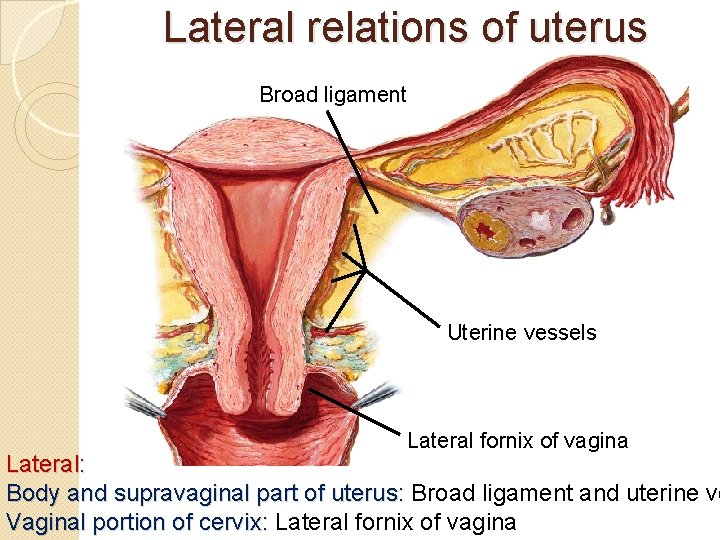
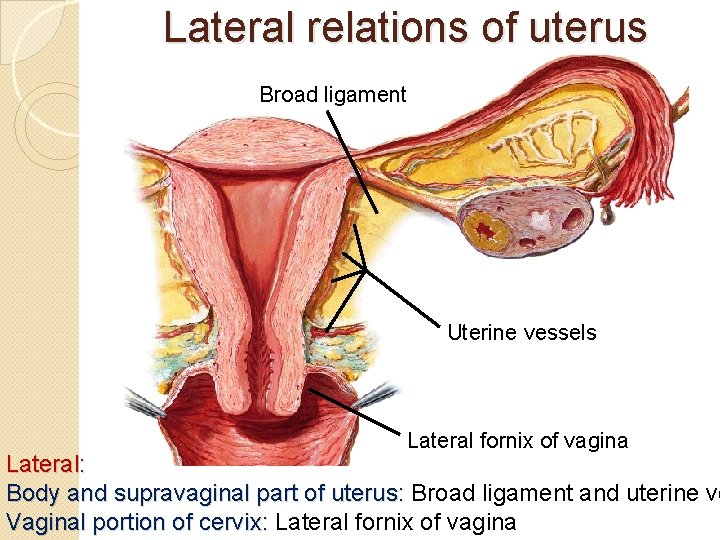
Lateral relations of uterus Broad ligament Uterine vessels Lateral fornix of vagina Lateral: Body and supravaginal part of uterus: Broad ligament and uterine ve Vaginal portion of cervix: Lateral fornix of vagina
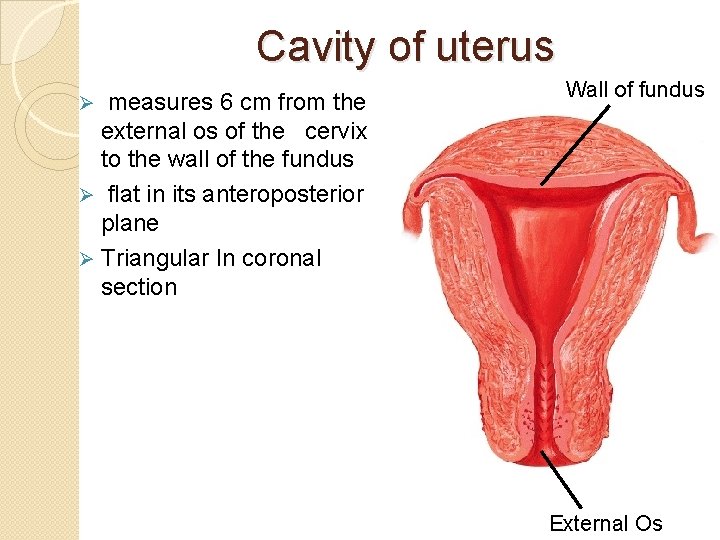
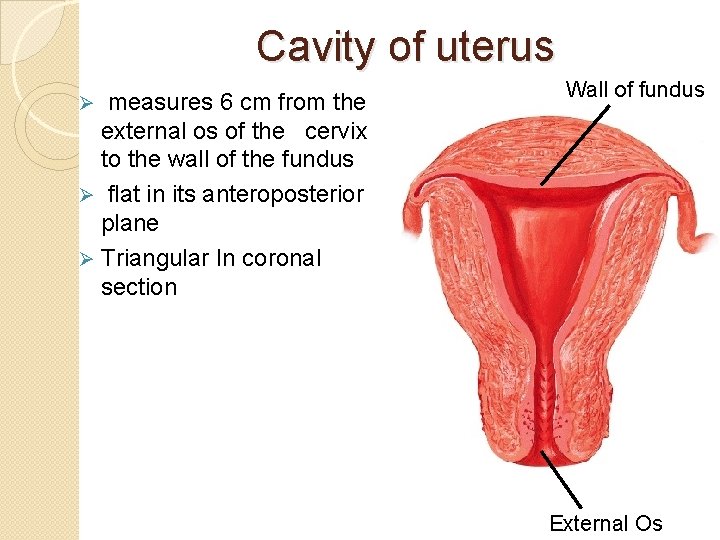
Cavity of uterus measures 6 cm from the external os of the cervix to the wall of the fundus Ø flat in its anteroposterior plane Ø Triangular In coronal section Ø Wall of fundus External Os
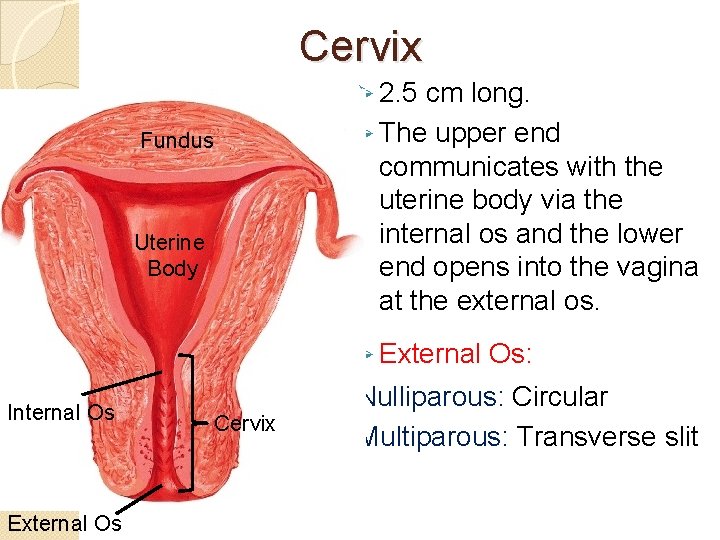
Cervix Ø 2. 5 cm long. Ø The upper end communicates with the uterine body via the internal os and the lower end opens into the vagina at the external os. Fundus Uterine Body Ø External Internal Os External Os Cervix Os: Nulliparous: Circular Multiparous: Transverse slit
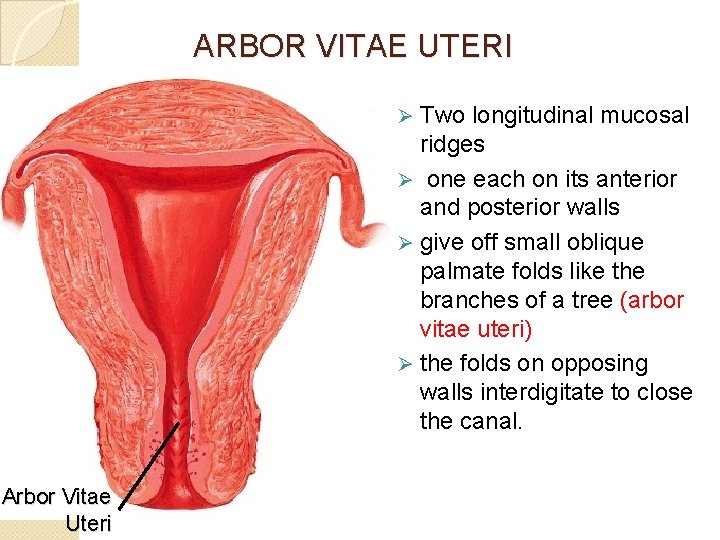
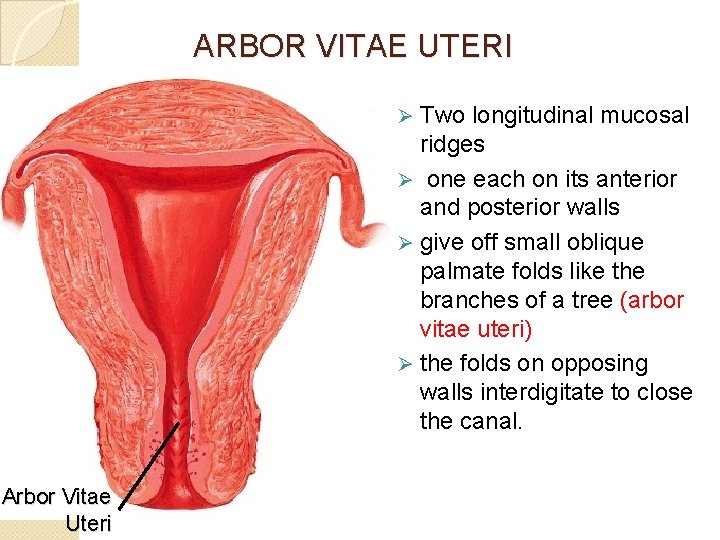
ARBOR VITAE UTERI Two longitudinal mucosal ridges Ø one each on its anterior and posterior walls Ø give off small oblique palmate folds like the branches of a tree (arbor vitae uteri) Ø the folds on opposing walls interdigitate to close the canal. Ø Arbor Vitae Uteri
STRUCTURE OF UTERUS � wall of the body of uterus consists of three layers � From superficial to deep these are: � 1. Perimetrium: � peritoneal covering of the uterus � derived from broad ligament. � 2. Myometrium: � thickest layer � consists of compactly arranged smooth muscle bundles. � 3. Endometrium: � mucosal lining of the body of the Uterus � shows cyclic changes
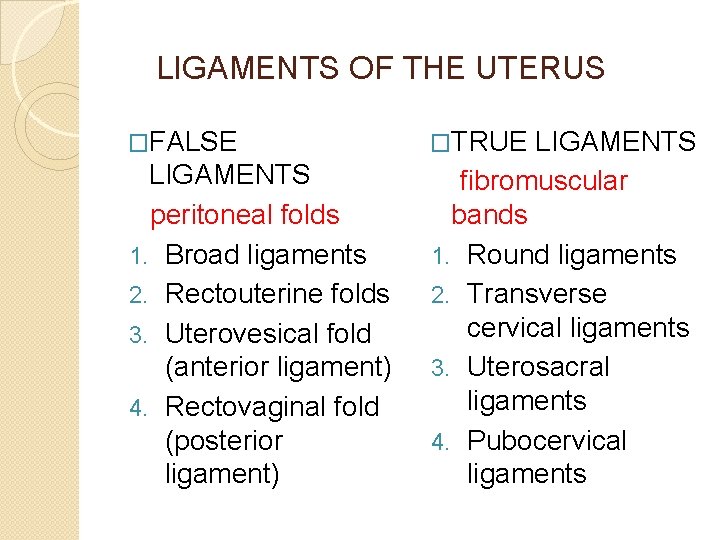
LIGAMENTS OF THE UTERUS �FALSE LIGAMENTS peritoneal folds 1. Broad ligaments 2. Rectouterine folds 3. Uterovesical fold (anterior ligament) 4. Rectovaginal fold (posterior ligament) �TRUE LIGAMENTS fibromuscular bands 1. Round ligaments 2. Transverse cervical ligaments 3. Uterosacral ligaments 4. Pubocervical ligaments
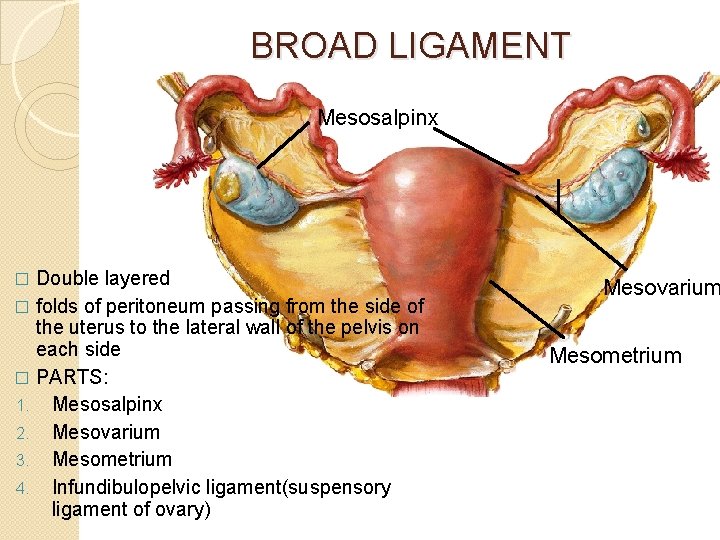
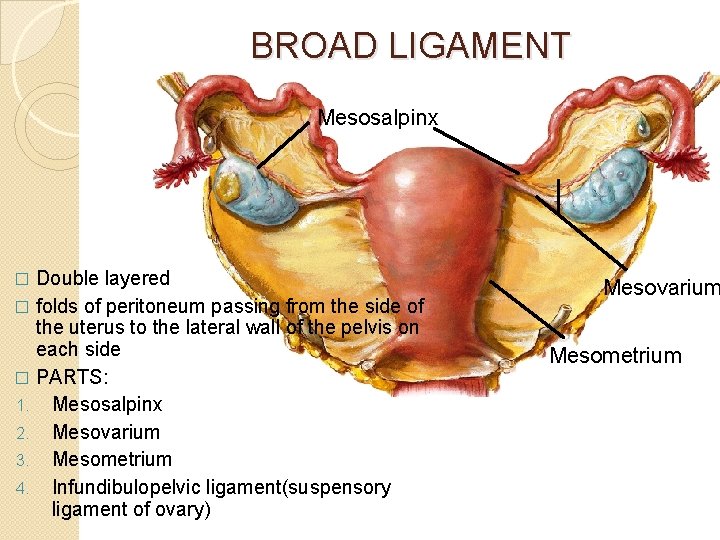
BROAD LIGAMENT Mesosalpinx Double layered � folds of peritoneum passing from the side of the uterus to the lateral wall of the pelvis on each side � PARTS: 1. Mesosalpinx 2. Mesovarium 3. Mesometrium 4. Infundibulopelvic ligament(suspensory ligament of ovary) � Mesovarium Mesometrium
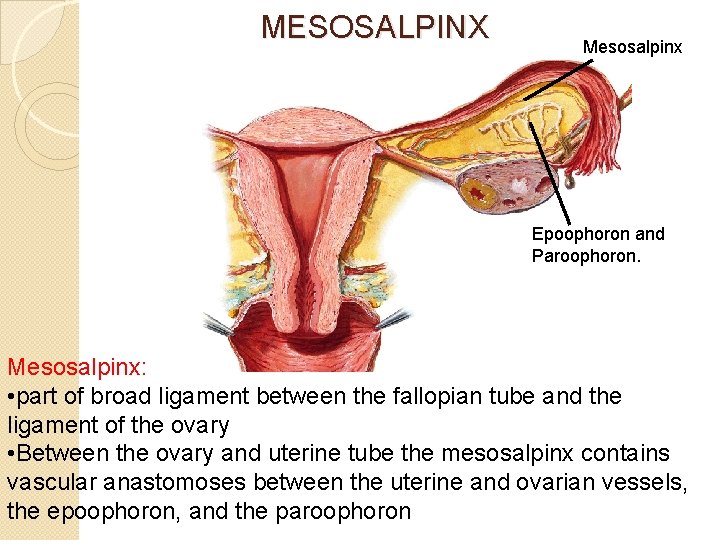
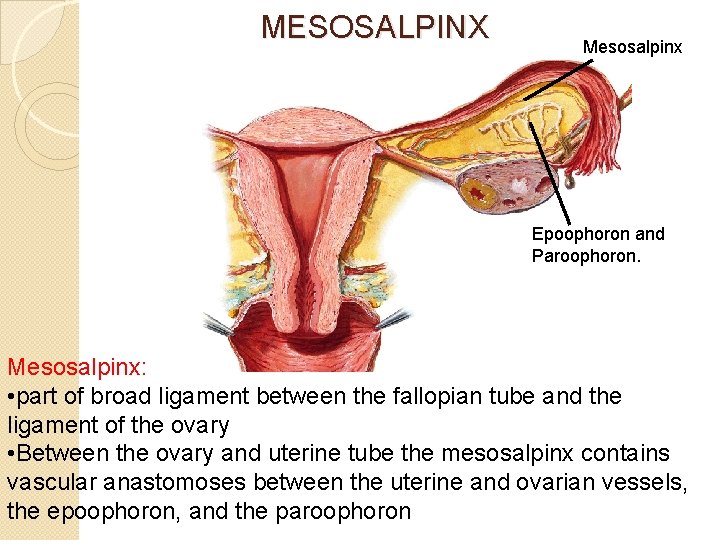
MESOSALPINX Mesosalpinx Epoophoron and Paroophoron. Mesosalpinx: • part of broad ligament between the fallopian tube and the ligament of the ovary • Between the ovary and uterine tube the mesosalpinx contains vascular anastomoses between the uterine and ovarian vessels, the epoophoron, and the paroophoron
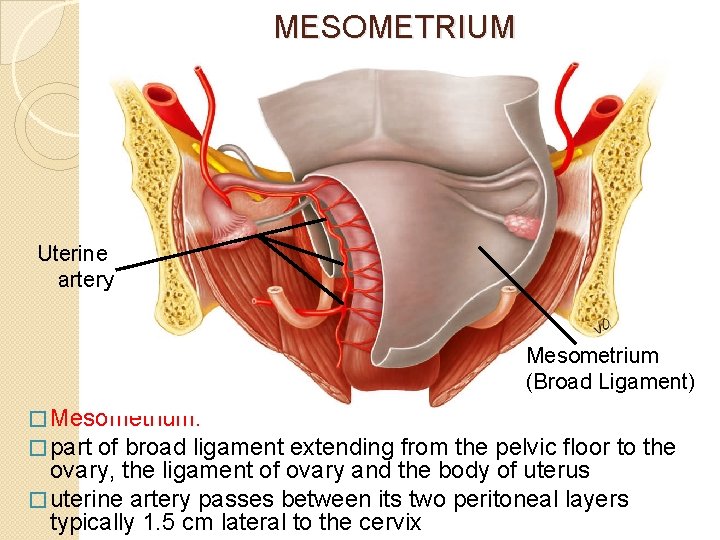
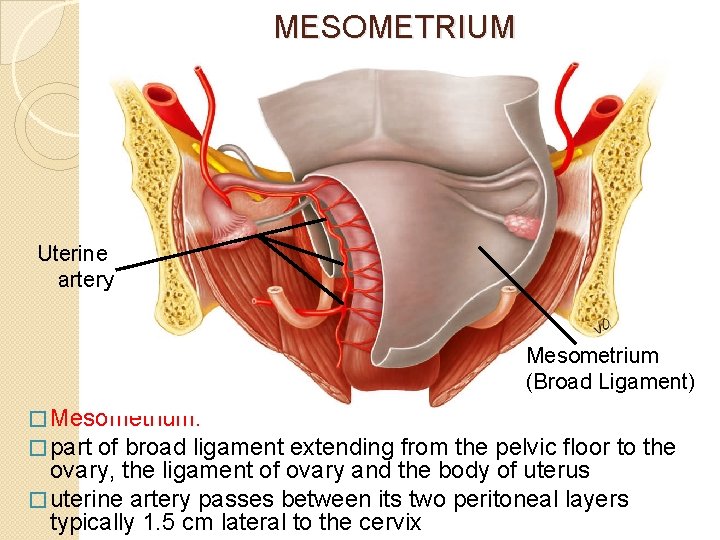
MESOMETRIUM Uterine artery Mesometrium (Broad Ligament) � Mesometrium: � part of broad ligament extending from the pelvic floor to the ovary, the ligament of ovary and the body of uterus � uterine artery passes between its two peritoneal layers typically 1. 5 cm lateral to the cervix
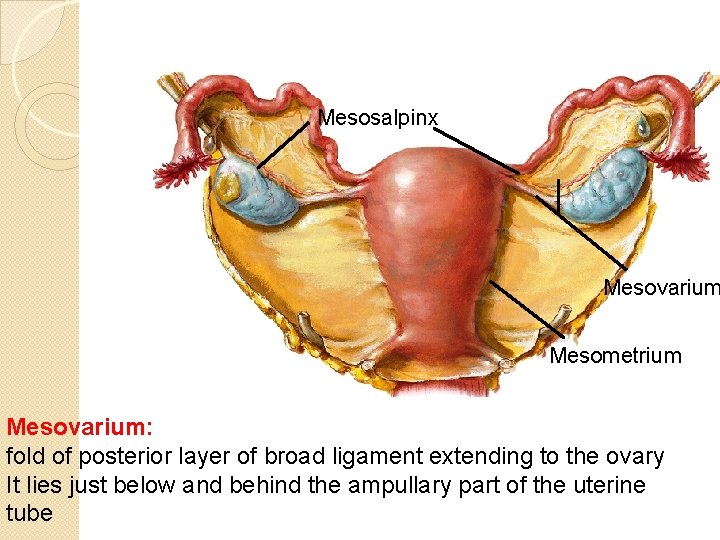
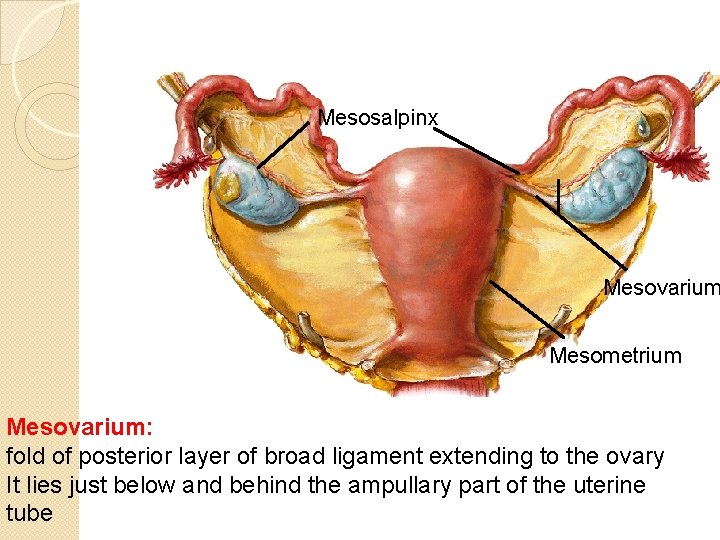
Mesosalpinx Mesovarium Mesometrium Mesovarium: fold of posterior layer of broad ligament extending to the ovary It lies just below and behind the ampullary part of the uterine tube
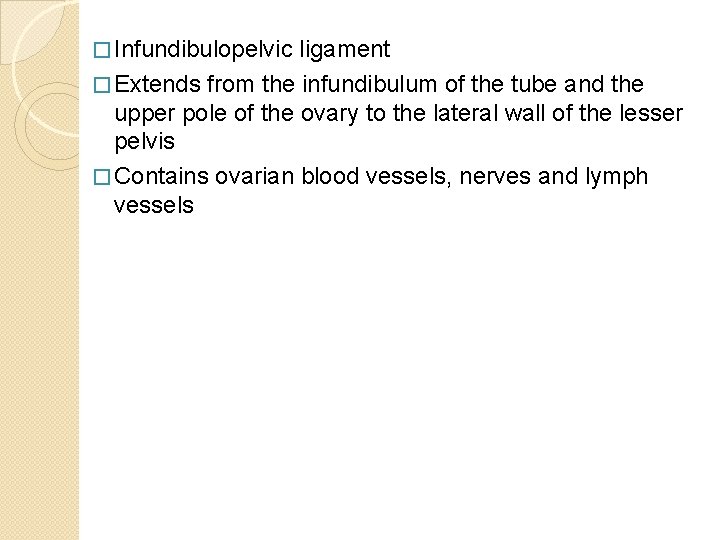
� Infundibulopelvic ligament � Extends from the infundibulum of the tube and the upper pole of the ovary to the lateral wall of the lesser pelvis � Contains ovarian blood vessels, nerves and lymph vessels
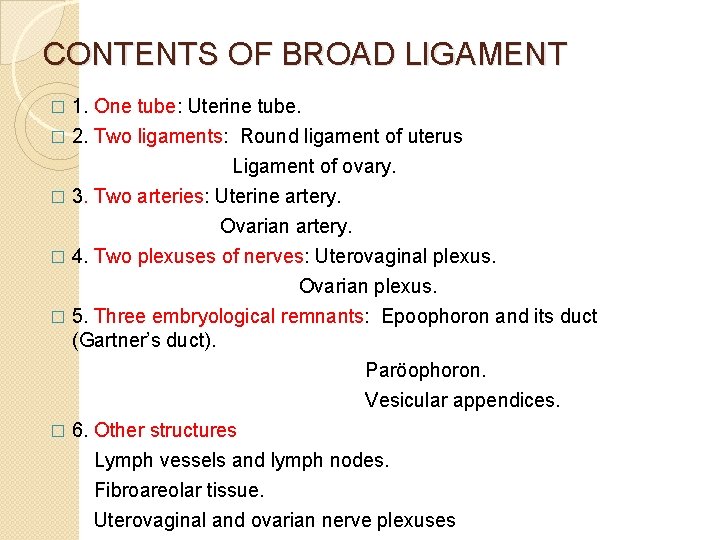
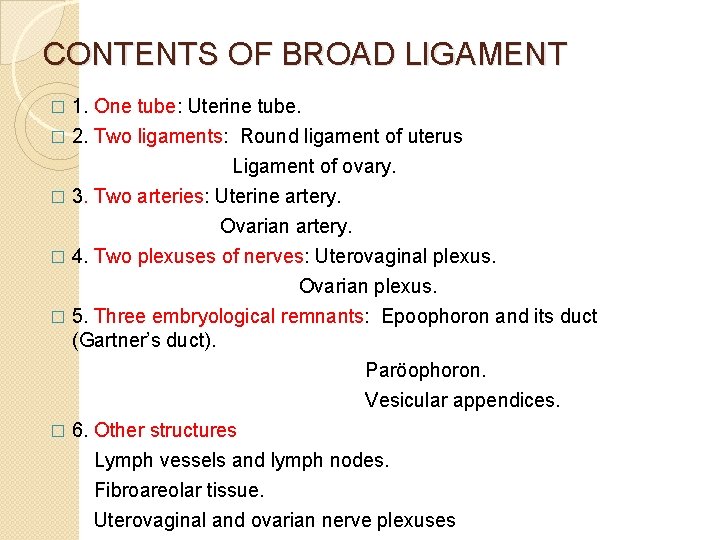
CONTENTS OF BROAD LIGAMENT 1. One tube: Uterine tube. � 2. Two ligaments: Round ligament of uterus � Ligament of ovary. � 3. Two arteries: Uterine artery. Ovarian artery. � 4. Two plexuses of nerves: Uterovaginal plexus. Ovarian plexus. � 5. Three embryological remnants: Epoophoron and its duct (Gartner’s duct). Paröophoron. Vesicular appendices. � 6. Other structures Lymph vessels and lymph nodes. Fibroareolar tissue. Uterovaginal and ovarian nerve plexuses
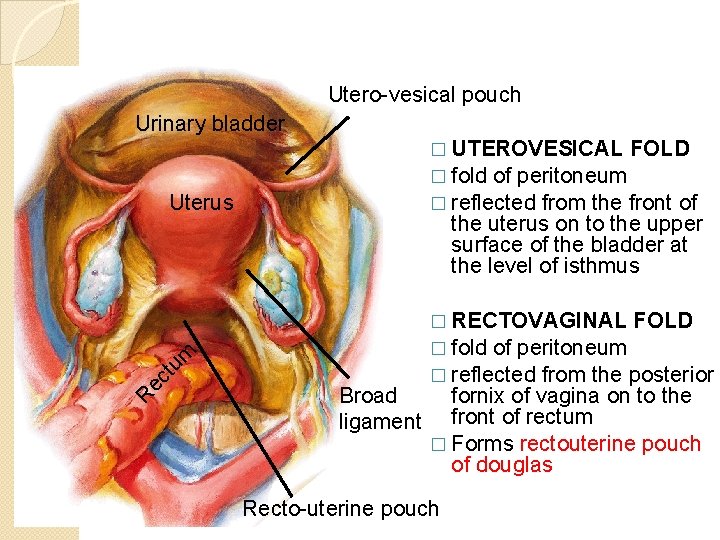
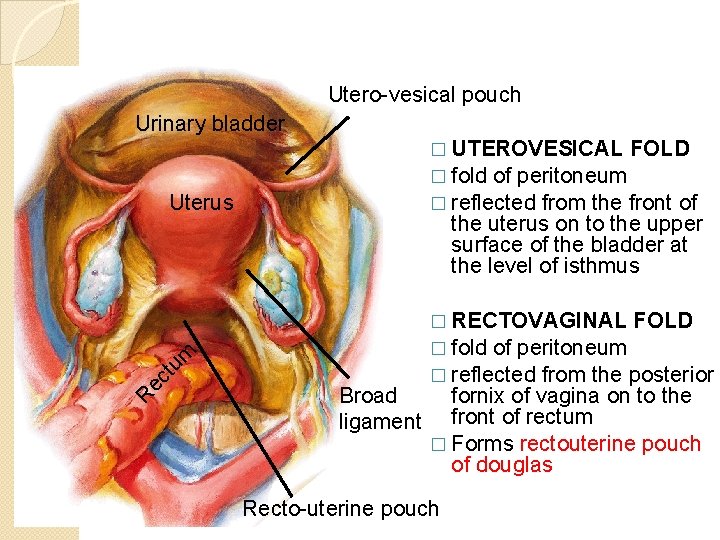
Utero-vesical pouch Urinary bladder � UTEROVESICAL FOLD � fold of peritoneum � reflected from the front of Uterus R ec tu m the uterus on to the upper surface of the bladder at the level of isthmus Broad ligament � RECTOVAGINAL FOLD � fold of peritoneum � reflected from the posterior fornix of vagina on to the front of rectum � Forms rectouterine pouch of douglas Recto-uterine pouch
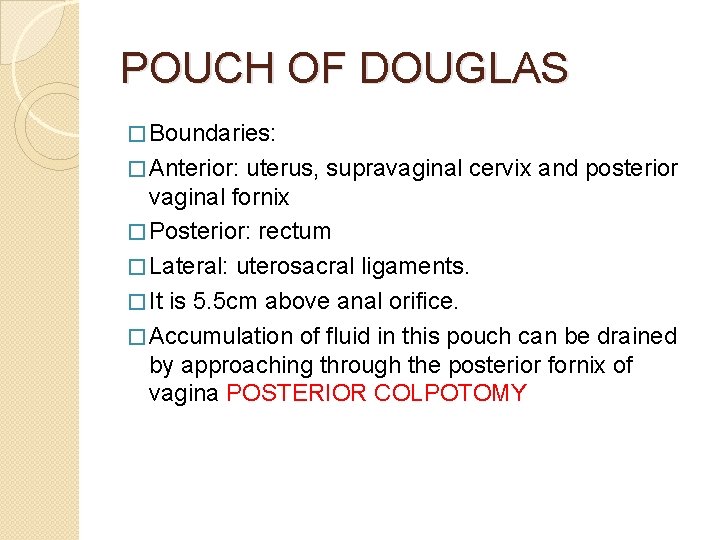
POUCH OF DOUGLAS � Boundaries: � Anterior: uterus, supravaginal cervix and posterior vaginal fornix � Posterior: rectum � Lateral: uterosacral ligaments. � It is 5. 5 cm above anal orifice. � Accumulation of fluid in this pouch can be drained by approaching through the posterior fornix of vagina POSTERIOR COLPOTOMY
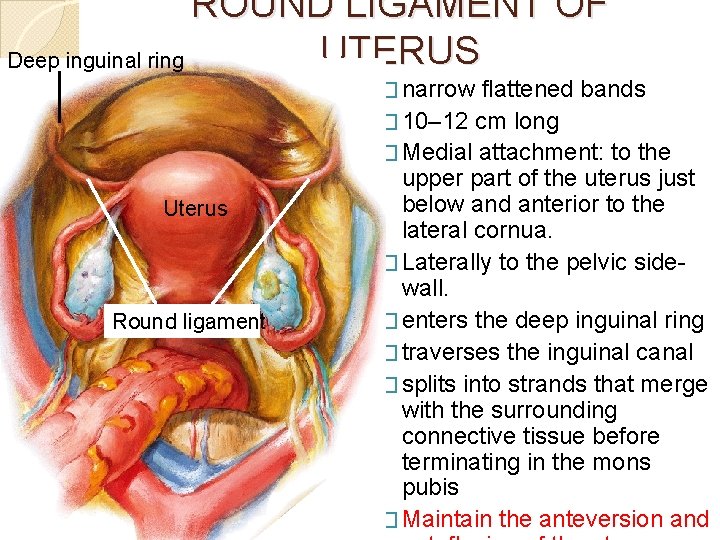
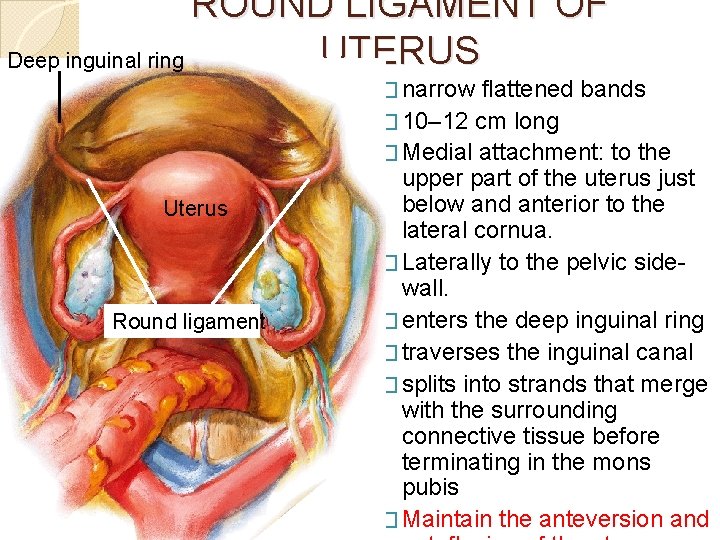
ROUND LIGAMENT OF UTERUS Deep inguinal ring � narrow Uterus Round ligament flattened bands � 10– 12 cm long � Medial attachment: to the upper part of the uterus just below and anterior to the lateral cornua. � Laterally to the pelvic sidewall. � enters the deep inguinal ring � traverses the inguinal canal � splits into strands that merge with the surrounding connective tissue before terminating in the mons pubis � Maintain the anteversion and
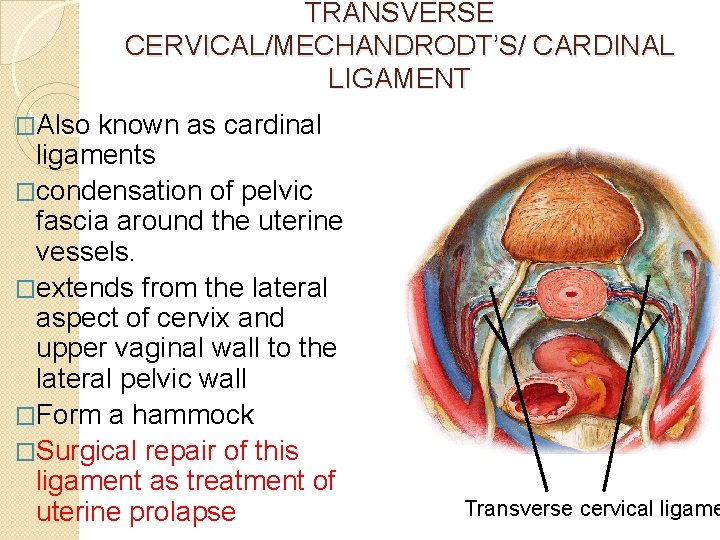
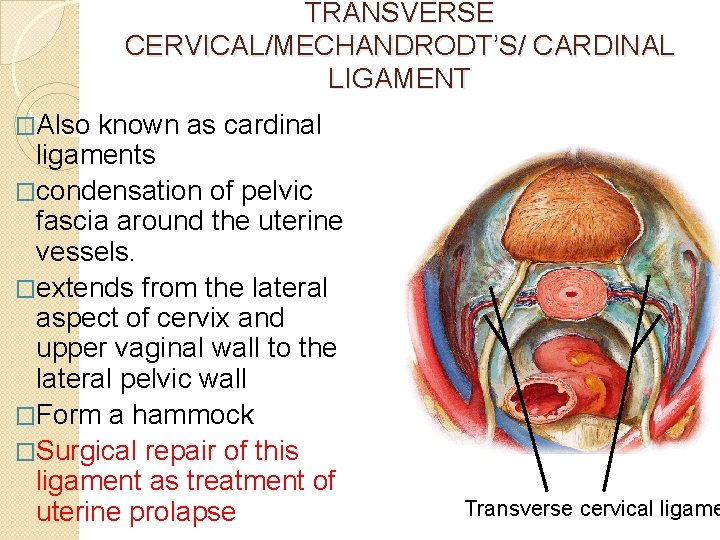
TRANSVERSE CERVICAL/MECHANDRODT’S/ CARDINAL LIGAMENT �Also known as cardinal ligaments �condensation of pelvic fascia around the uterine vessels. �extends from the lateral aspect of cervix and upper vaginal wall to the lateral pelvic wall �Form a hammock �Surgical repair of this ligament as treatment of uterine prolapse Transverse cervical ligame
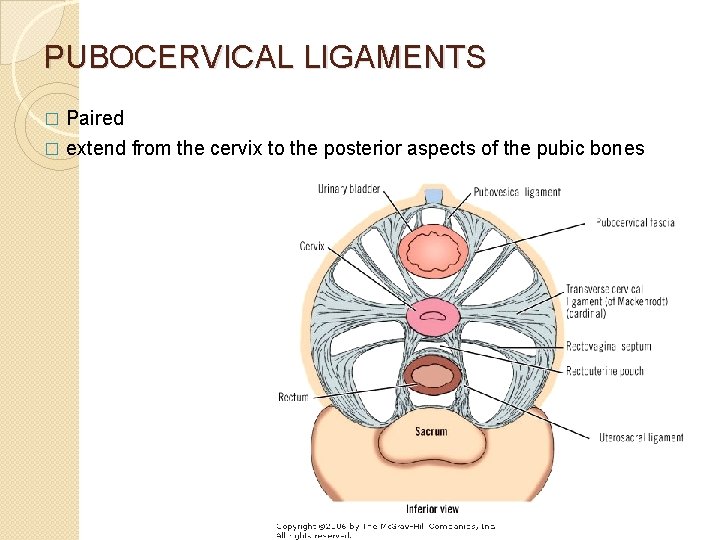
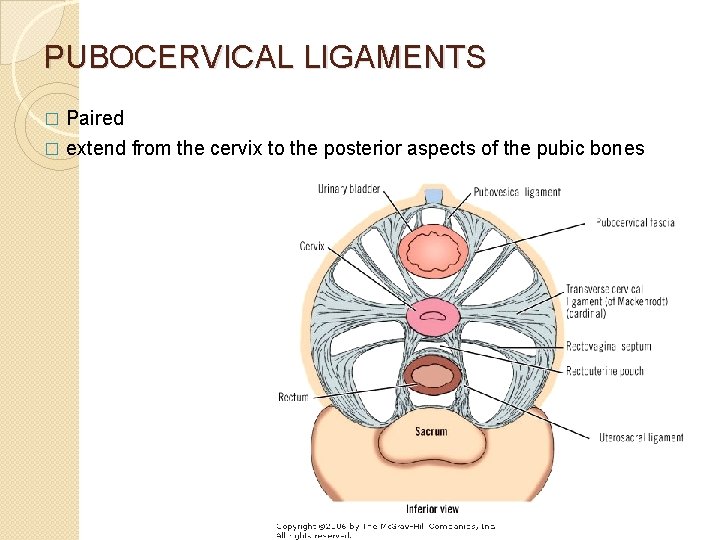
PUBOCERVICAL LIGAMENTS Paired � extend from the cervix to the posterior aspects of the pubic bones �
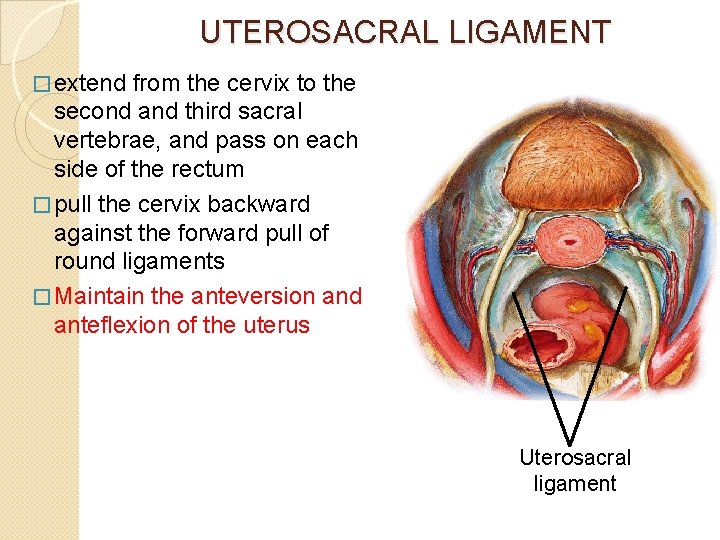
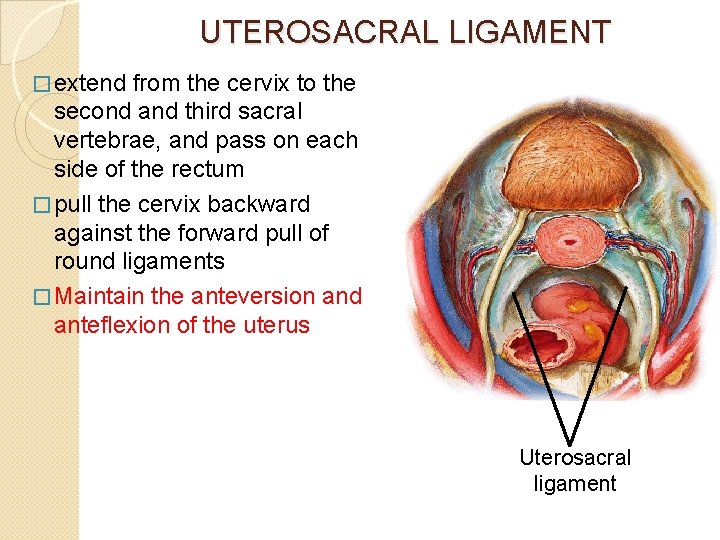
UTEROSACRAL LIGAMENT � extend from the cervix to the second and third sacral vertebrae, and pass on each side of the rectum � pull the cervix backward against the forward pull of round ligaments � Maintain the anteversion and anteflexion of the uterus Uterosacral ligament
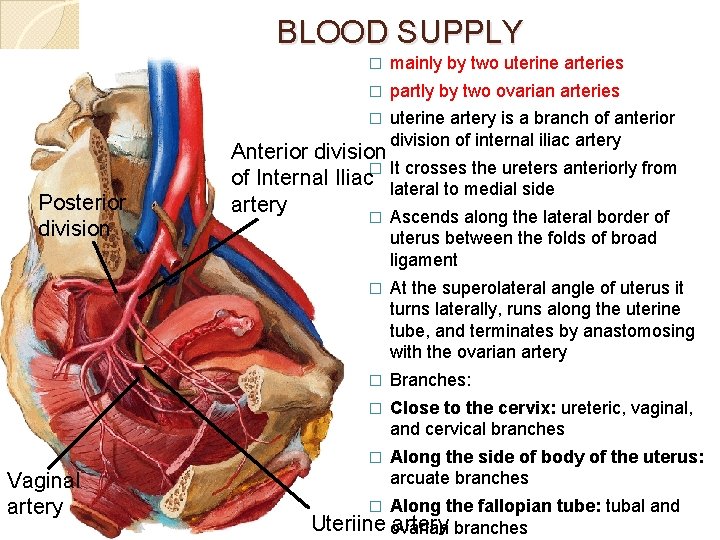
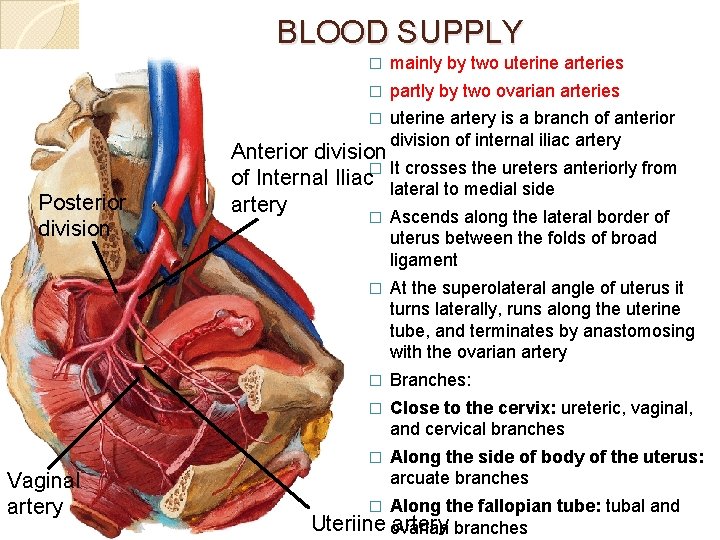
BLOOD SUPPLY Posterior division Vaginal artery � mainly by two uterine arteries � partly by two ovarian arteries � uterine artery is a branch of anterior division of internal iliac artery Anterior division � It crosses the ureters anteriorly from of Internal Iliac lateral to medial side artery � Ascends along the lateral border of uterus between the folds of broad ligament � At the superolateral angle of uterus it turns laterally, runs along the uterine tube, and terminates by anastomosing with the ovarian artery � Branches: � Close to the cervix: ureteric, vaginal, and cervical branches � Along the side of body of the uterus: arcuate branches Along the fallopian tube: tubal and Uteriine ovarian artery branches �
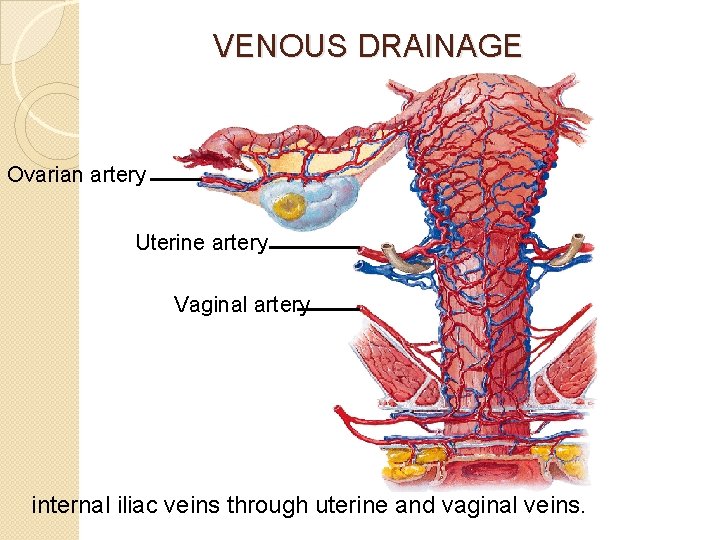
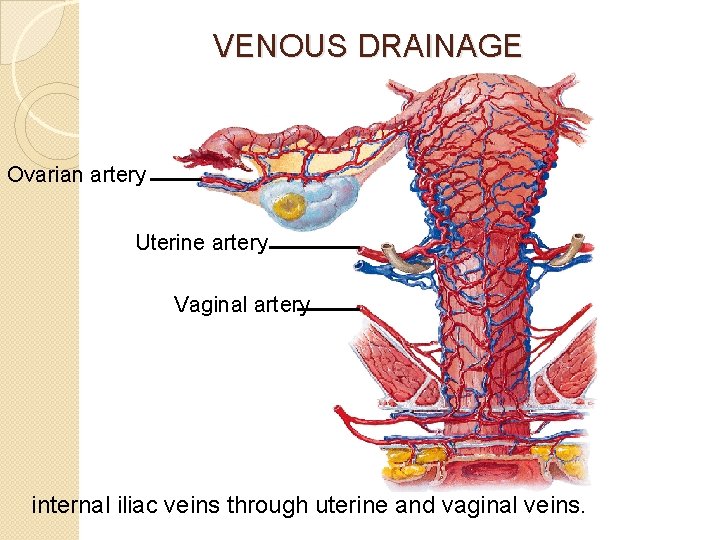
VENOUS DRAINAGE Ovarian artery Uterine artery Vaginal artery internal iliac veins through uterine and vaginal veins.
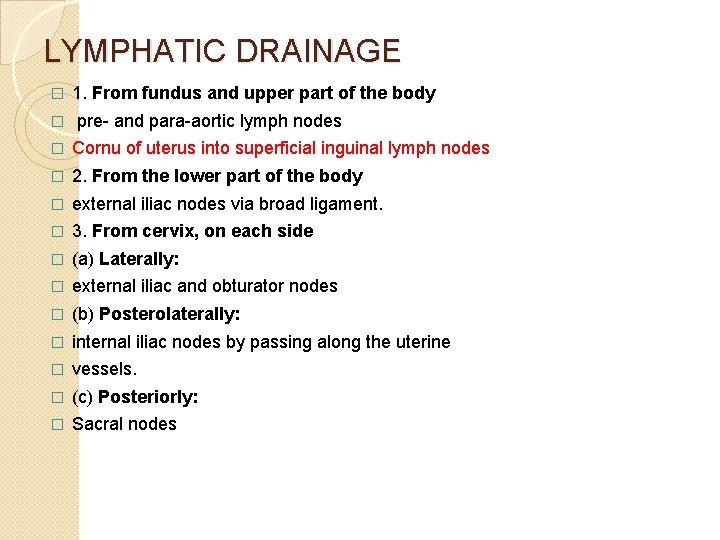
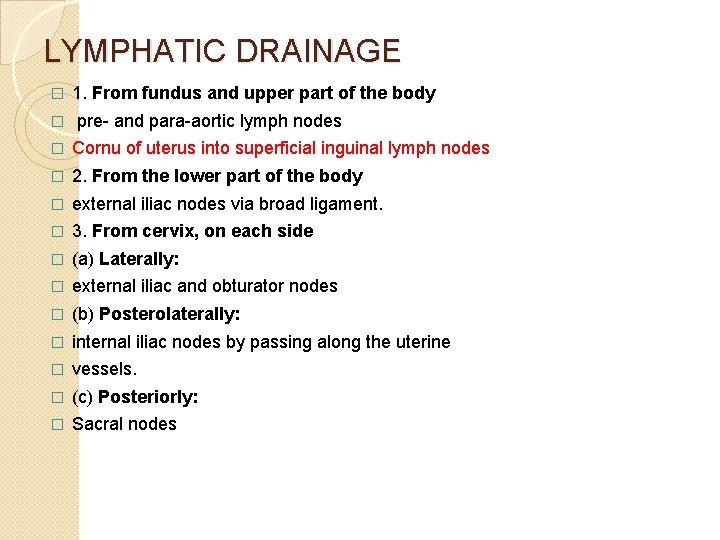
LYMPHATIC DRAINAGE � � 1. From fundus and upper part of the body pre- and para-aortic lymph nodes � Cornu of uterus into superficial inguinal lymph nodes � 2. From the lower part of the body � external iliac nodes via broad ligament. � 3. From cervix, on each side � (a) Laterally: � external iliac and obturator nodes � (b) Posterolaterally: � internal iliac nodes by passing along the uterine � vessels. � (c) Posteriorly: � Sacral nodes
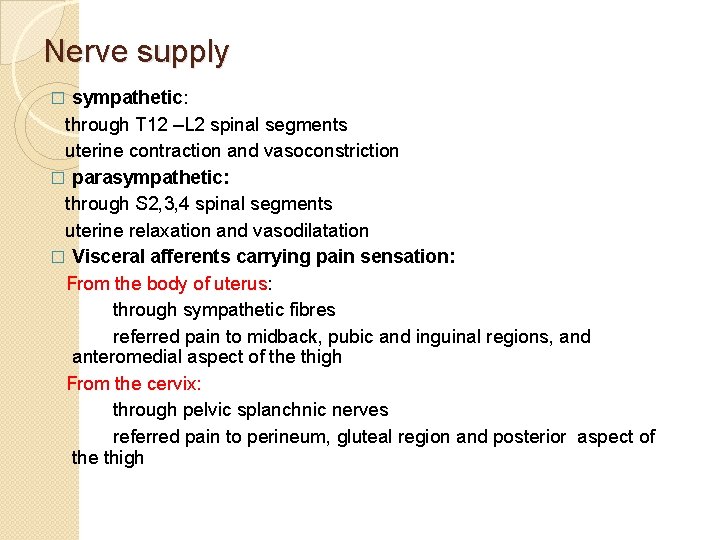
Nerve supply sympathetic: through T 12 –L 2 spinal segments uterine contraction and vasoconstriction � parasympathetic: through S 2, 3, 4 spinal segments uterine relaxation and vasodilatation � Visceral afferents carrying pain sensation: From the body of uterus: through sympathetic fibres referred pain to midback, pubic and inguinal regions, and anteromedial aspect of the thigh From the cervix: through pelvic splanchnic nerves referred pain to perineum, gluteal region and posterior aspect of the thigh �
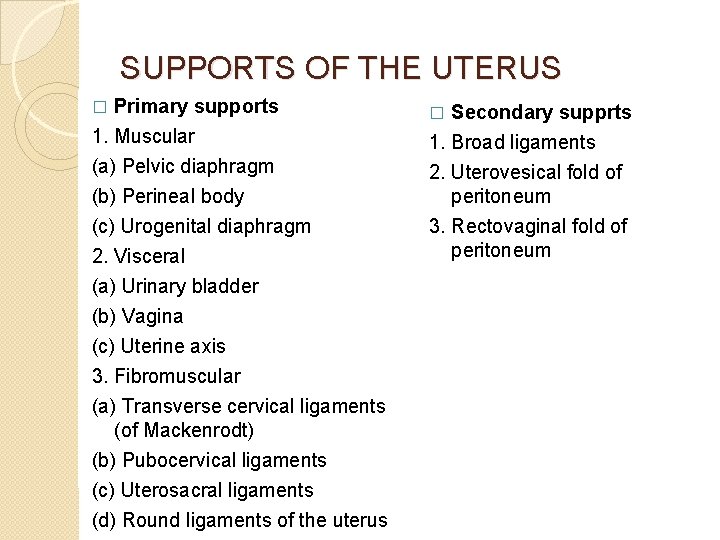
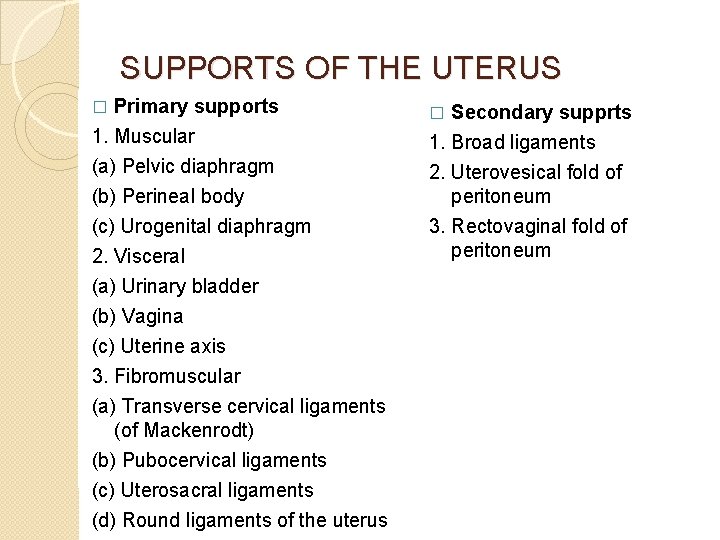
SUPPORTS OF THE UTERUS Primary supports 1. Muscular � � (a) Pelvic diaphragm (b) Perineal body (c) Urogenital diaphragm 2. Visceral (a) Urinary bladder (b) Vagina 2. Uterovesical fold of peritoneum 3. Rectovaginal fold of peritoneum (c) Uterine axis 3. Fibromuscular (a) Transverse cervical ligaments (of Mackenrodt) (b) Pubocervical ligaments (c) Uterosacral ligaments (d) Round ligaments of the uterus Secondary supprts 1. Broad ligaments
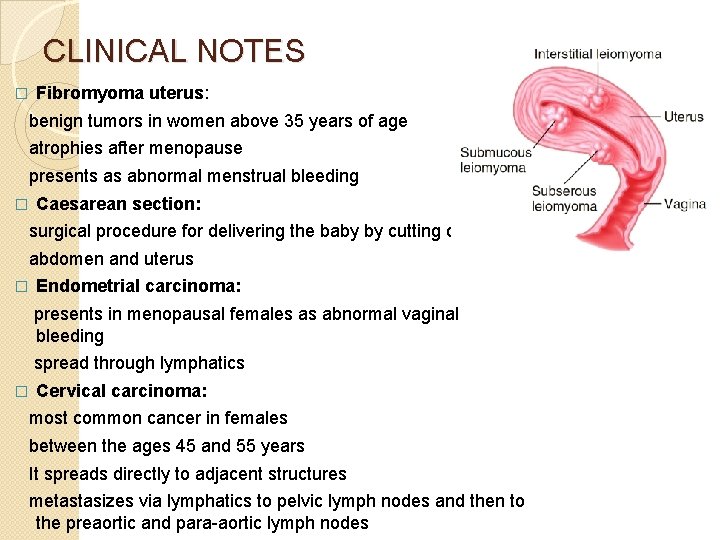
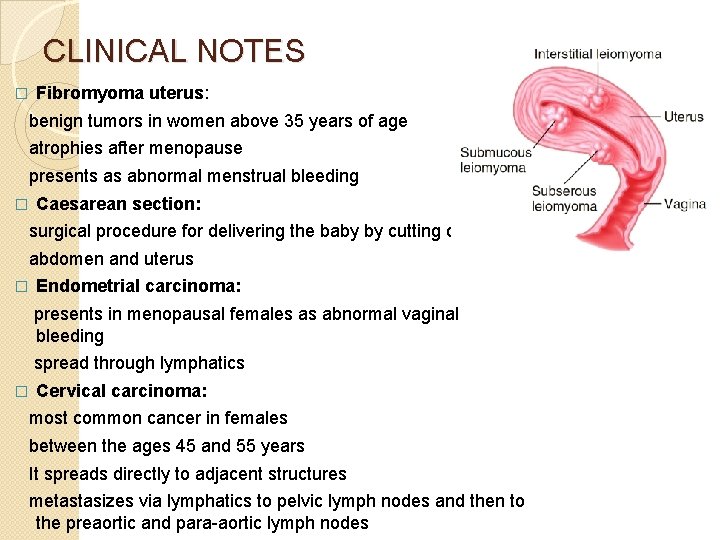
CLINICAL NOTES � Fibromyoma uterus: benign tumors in women above 35 years of age atrophies after menopause presents as abnormal menstrual bleeding � Caesarean section: surgical procedure for delivering the baby by cutting open the abdomen and uterus � Endometrial carcinoma: presents in menopausal females as abnormal vaginal bleeding spread through lymphatics � Cervical carcinoma: most common cancer in females between the ages 45 and 55 years It spreads directly to adjacent structures metastasizes via lymphatics to pelvic lymph nodes and then to the preaortic and para-aortic lymph nodes
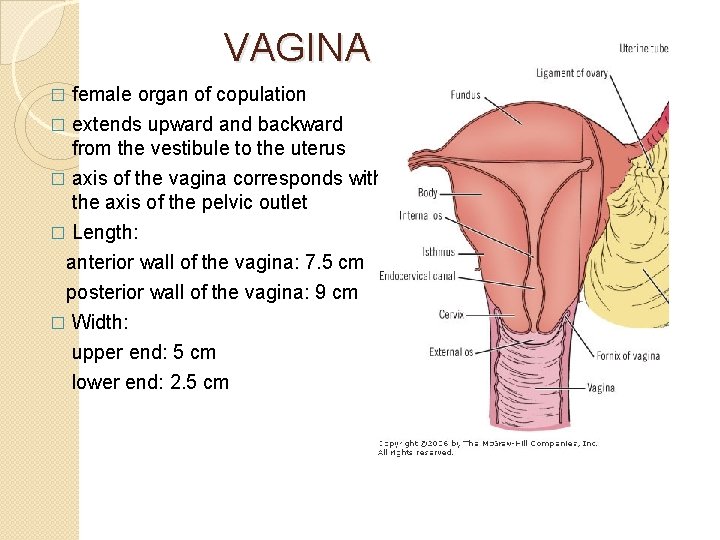
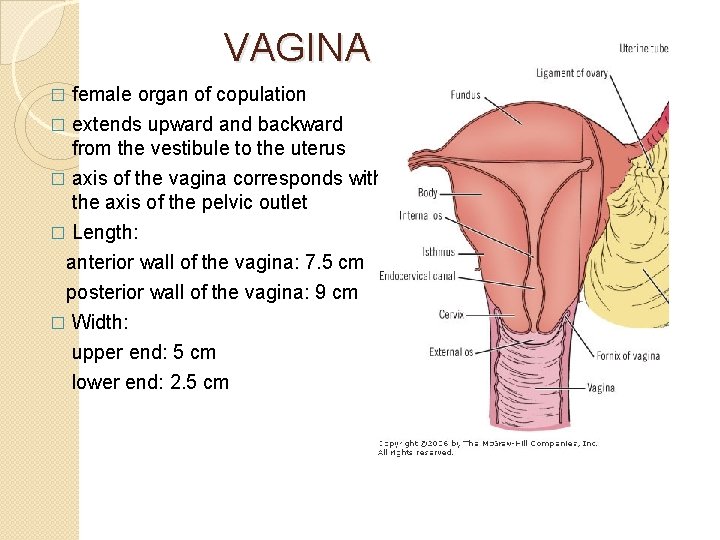
VAGINA female organ of copulation � extends upward and backward from the vestibule to the uterus � axis of the vagina corresponds with the axis of the pelvic outlet � Length: anterior wall of the vagina: 7. 5 cm posterior wall of the vagina: 9 cm � Width: upper end: 5 cm lower end: 2. 5 cm �
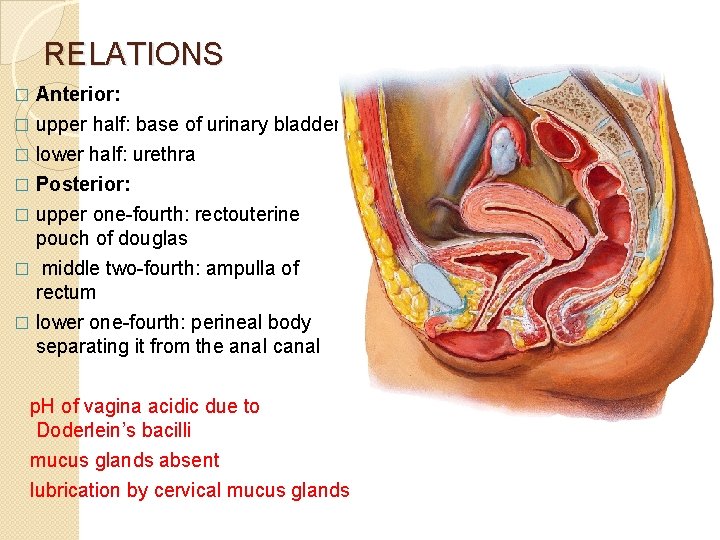
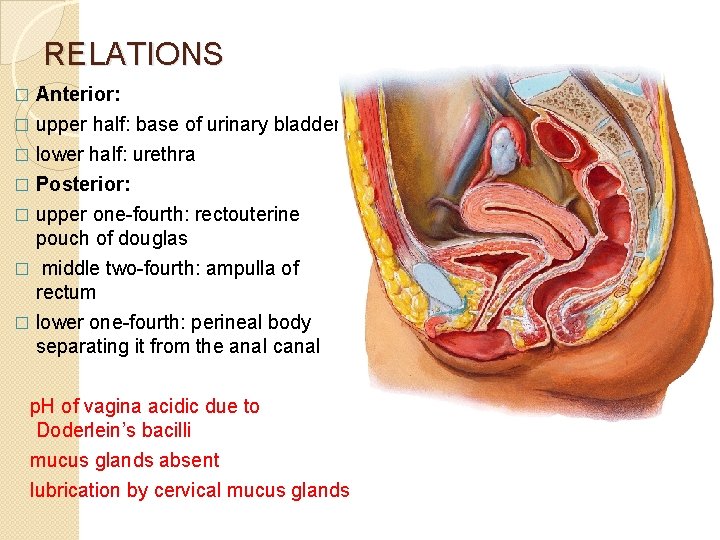
RELATIONS Anterior: � upper half: base of urinary bladder. � lower half: urethra � Posterior: � upper one-fourth: rectouterine pouch of douglas � middle two-fourth: ampulla of rectum � lower one-fourth: perineal body separating it from the anal canal � p. H of vagina acidic due to Doderlein’s bacilli mucus glands absent lubrication by cervical mucus glands
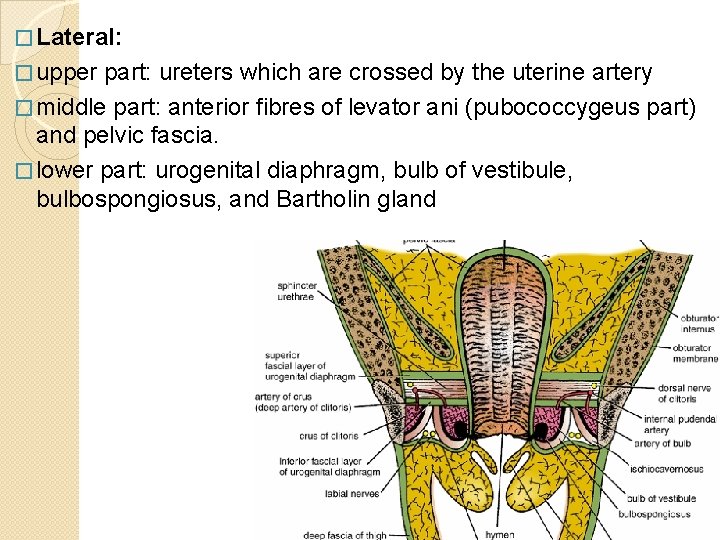
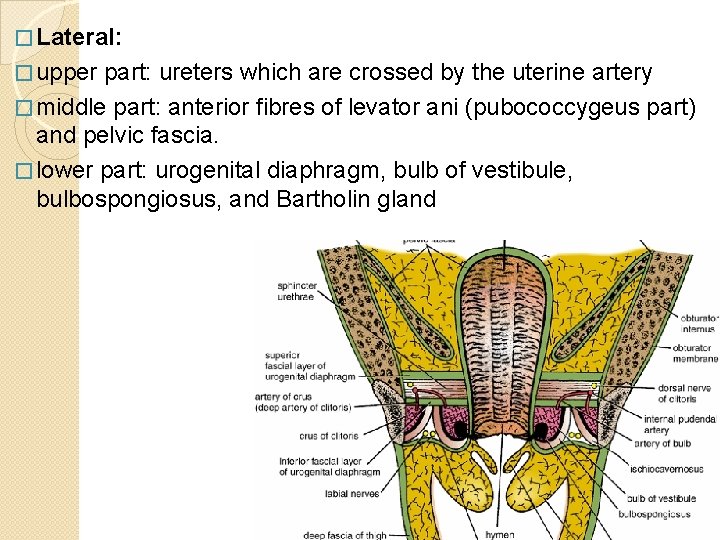
� Lateral: � upper part: ureters which are crossed by the uterine artery � middle part: anterior fibres of levator ani (pubococcygeus part) and pelvic fascia. � lower part: urogenital diaphragm, bulb of vestibule, bulbospongiosus, and Bartholin gland
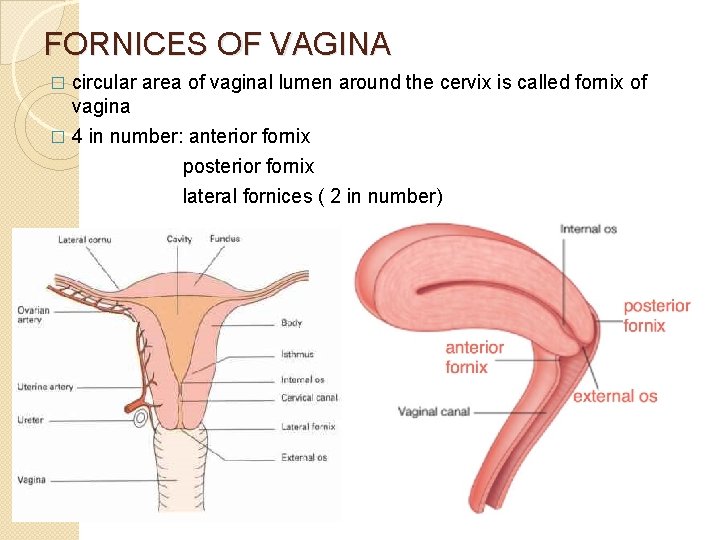
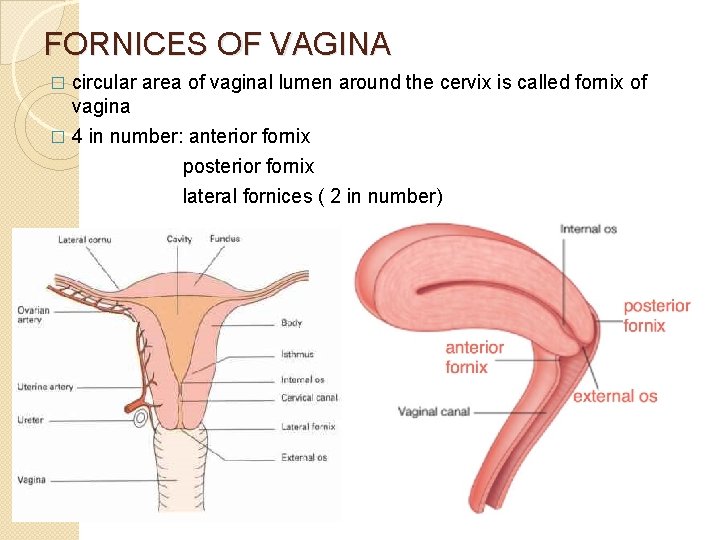
FORNICES OF VAGINA � circular area of vaginal lumen around the cervix is called fornix of vagina � 4 in number: anterior fornix posterior fornix lateral fornices ( 2 in number)
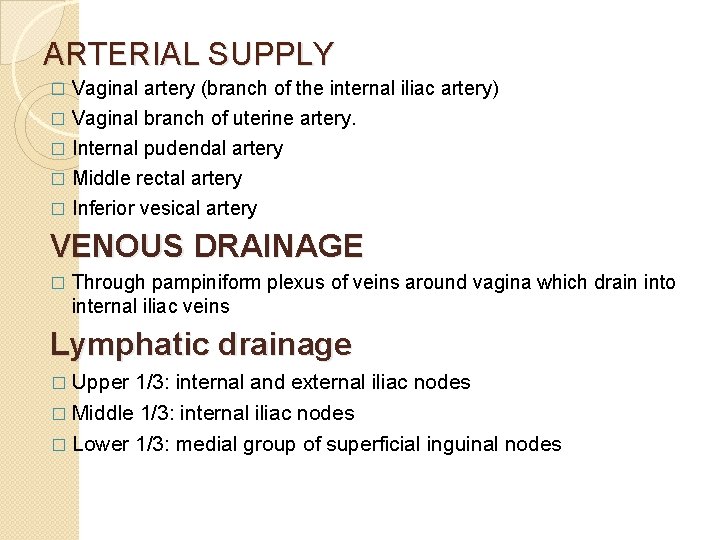
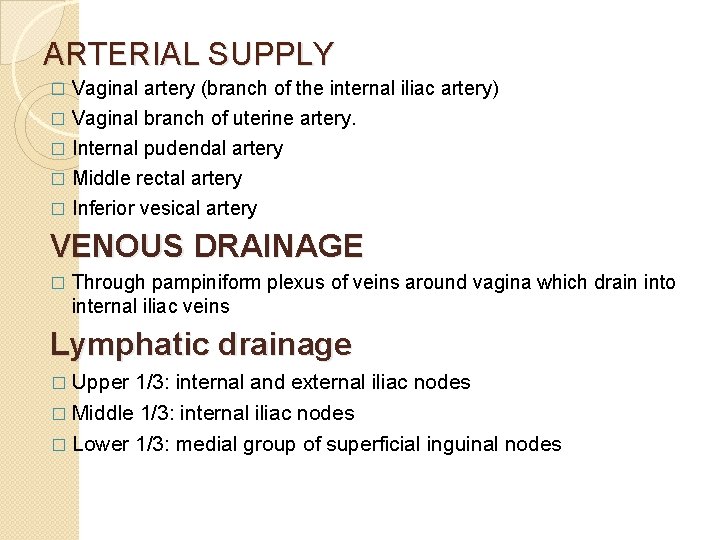
ARTERIAL SUPPLY Vaginal artery (branch of the internal iliac artery) � Vaginal branch of uterine artery. � Internal pudendal artery � Middle rectal artery � Inferior vesical artery � VENOUS DRAINAGE � Through pampiniform plexus of veins around vagina which drain into internal iliac veins Lymphatic drainage � Upper 1/3: internal and external iliac nodes � Middle 1/3: internal iliac nodes � Lower 1/3: medial group of superficial inguinal nodes
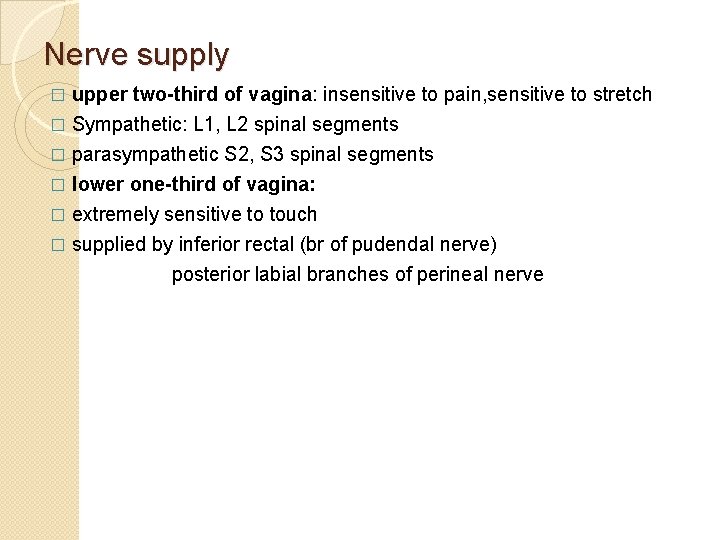
Nerve supply upper two-third of vagina: insensitive to pain, sensitive to stretch � Sympathetic: L 1, L 2 spinal segments � parasympathetic S 2, S 3 spinal segments � lower one-third of vagina: � extremely sensitive to touch � supplied by inferior rectal (br of pudendal nerve) posterior labial branches of perineal nerve �
CLINICAL NOTES � Vaginitis: infection of vagina common in children and old women (after menopause) � Culdocentesis: clinical procedure in which a needle is passed through the posterior fornix of vagina into the rectouterine pouch of Douglas
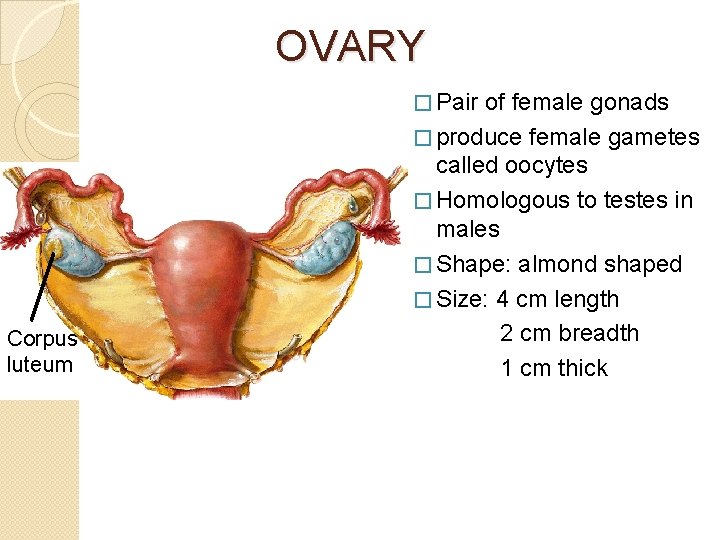
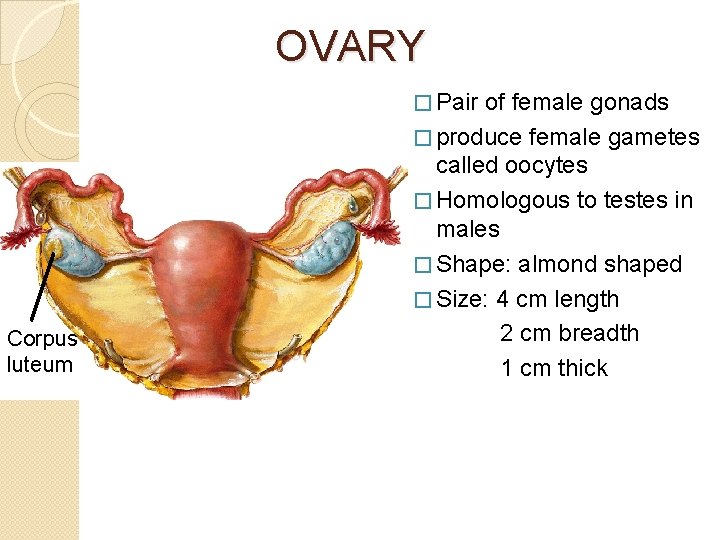
OVARY � Pair Corpus luteum of female gonads � produce female gametes called oocytes � Homologous to testes in males � Shape: almond shaped � Size: 4 cm length 2 cm breadth 1 cm thick
Location � lies in the ovarian fossa on the lateral pelvic wall � Boundaries of ovarian fossa anterior: external iliac vessels posterior: ureter and internal iliac vessels inferior: uterine tubes
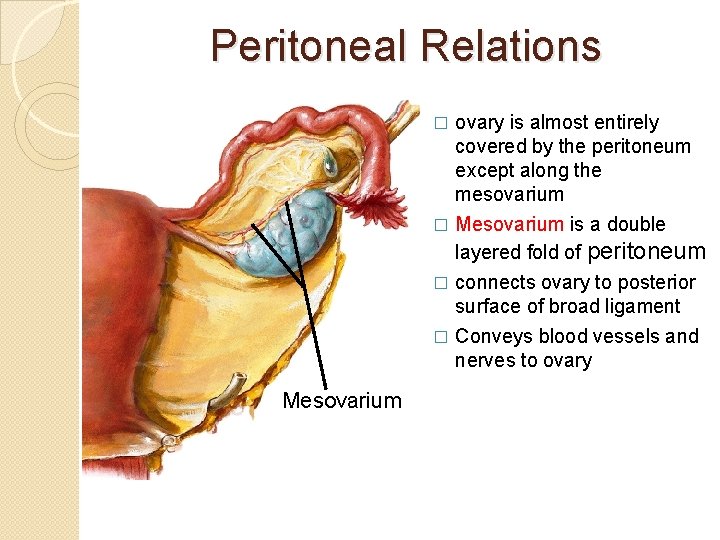
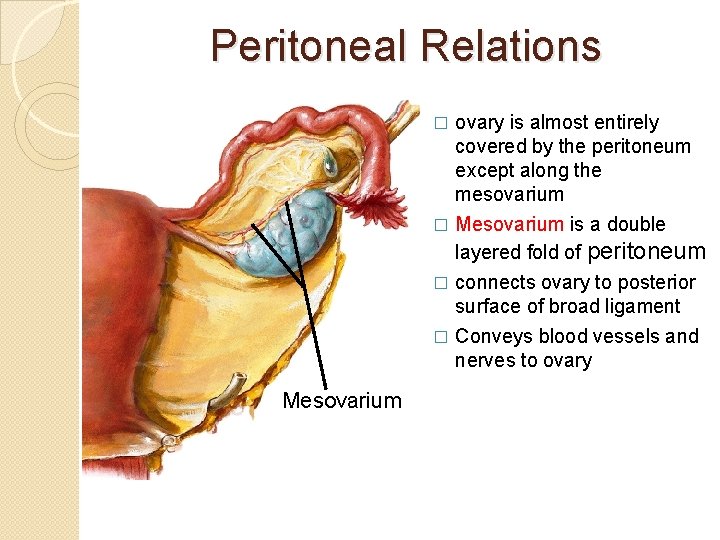
Peritoneal Relations ovary is almost entirely covered by the peritoneum except along the mesovarium � Mesovarium is a double layered fold of peritoneum � connects ovary to posterior surface of broad ligament � Conveys blood vessels and nerves to ovary � Mesovarium
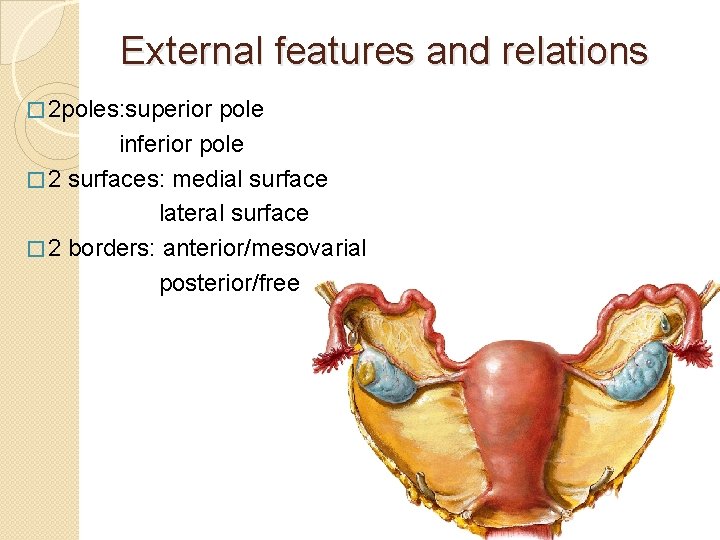
External features and relations � 2 poles: superior pole inferior pole � 2 surfaces: medial surface lateral surface � 2 borders: anterior/mesovarial posterior/free
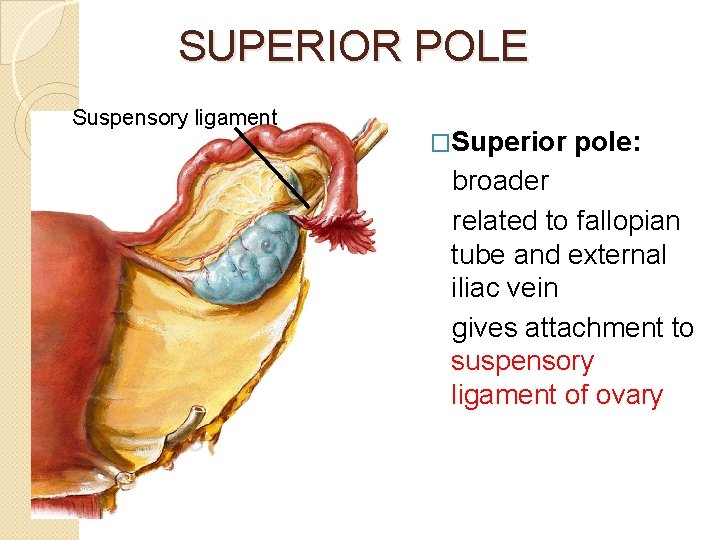
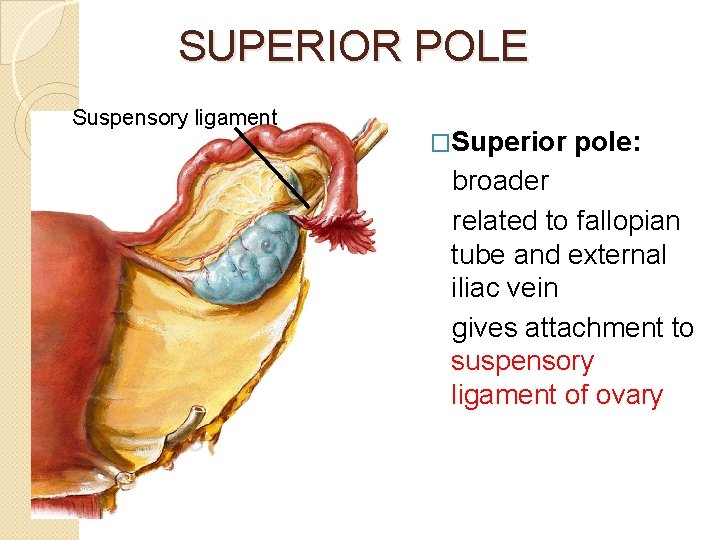
SUPERIOR POLE Suspensory ligament �Superior pole: broader related to fallopian tube and external iliac vein gives attachment to suspensory ligament of ovary
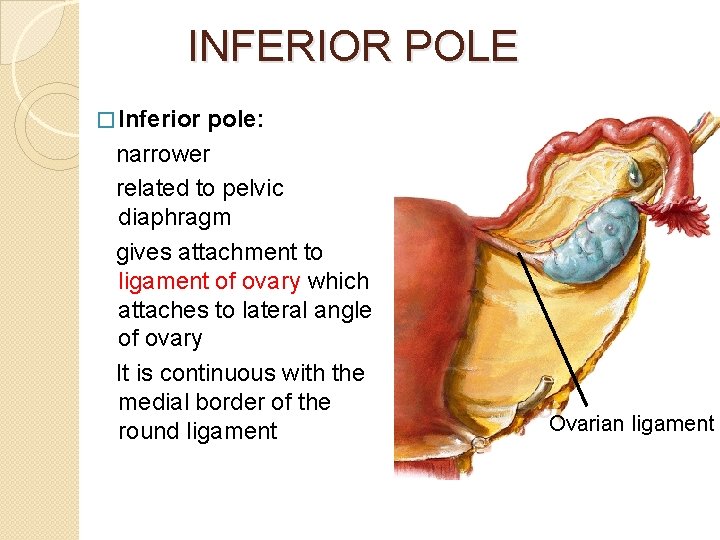
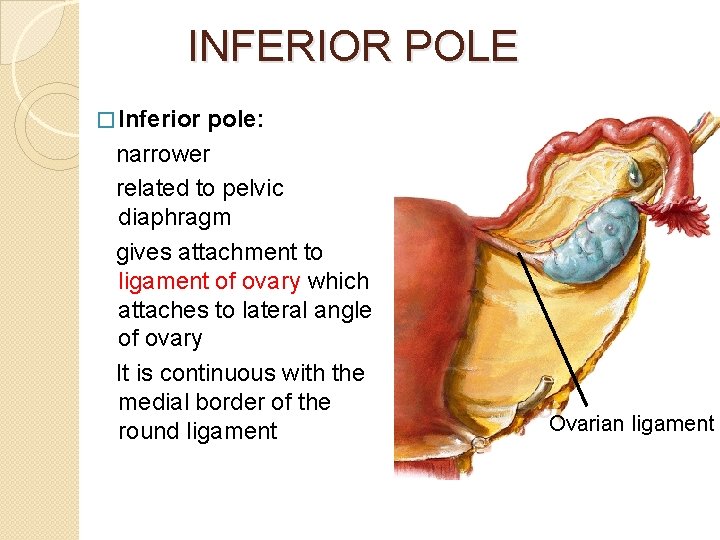
INFERIOR POLE � Inferior pole: narrower related to pelvic diaphragm gives attachment to ligament of ovary which attaches to lateral angle of ovary It is continuous with the medial border of the round ligament Ovarian ligament
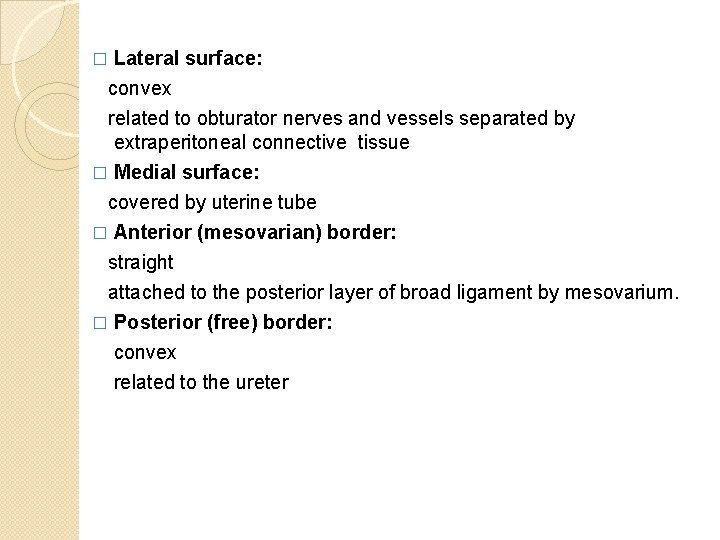
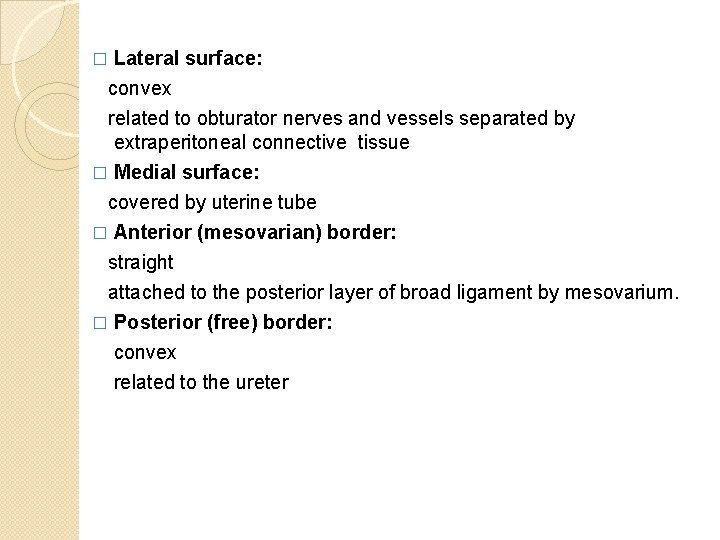
� Lateral surface: convex related to obturator nerves and vessels separated by extraperitoneal connective tissue � Medial surface: covered by uterine tube � Anterior (mesovarian) border: straight attached to the posterior layer of broad ligament by mesovarium. � Posterior (free) border: convex related to the ureter
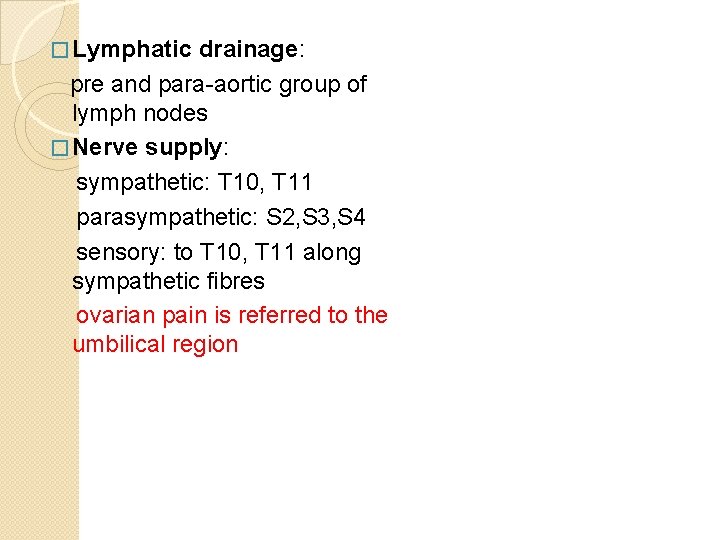
� Lymphatic drainage: pre and para-aortic group of lymph nodes � Nerve supply: sympathetic: T 10, T 11 parasympathetic: S 2, S 3, S 4 sensory: to T 10, T 11 along sympathetic fibres ovarian pain is referred to the umbilical region
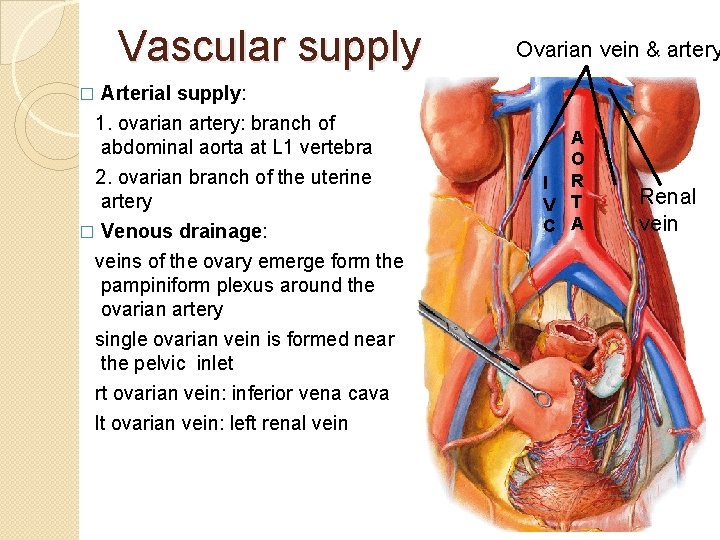
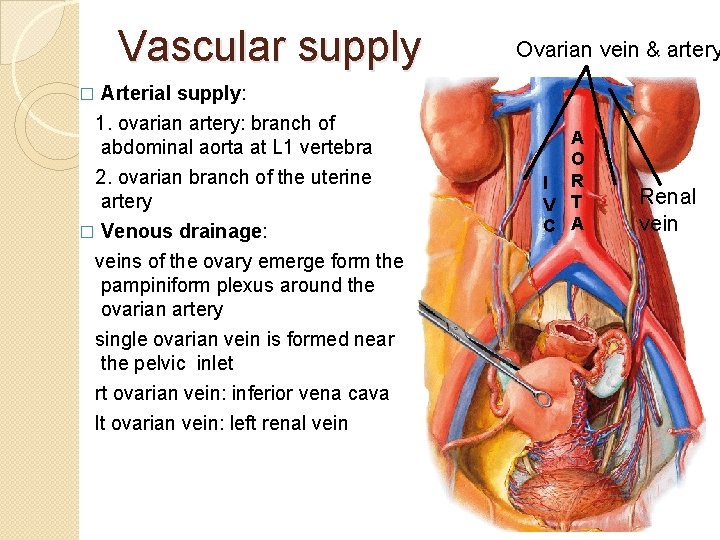
Vascular supply Arterial supply: 1. ovarian artery: branch of abdominal aorta at L 1 vertebra 2. ovarian branch of the uterine artery � Venous drainage: veins of the ovary emerge form the pampiniform plexus around the ovarian artery single ovarian vein is formed near the pelvic inlet rt ovarian vein: inferior vena cava lt ovarian vein: left renal vein Ovarian vein & artery � A O I R V T C A Renal vein
CLINICAL NOTES OVARIAN TORSION: severe abdominal pain due to abnormally long mesovarium and suspensory ligament of the ovary � OVARIAN PROLAPSE: into pouch of douglas � OVARIAN CYST: large cyst presents with abdominal pain and distension � OVARIAN CANCER: 20% of all gynaecological cancers � OVARIAN DYSGENESIS: seen in turner’s syndrome � ECTOPIC OVARIES: ovaries may fail to descent into pelvis may be seen in inguinal canal or labia majora �
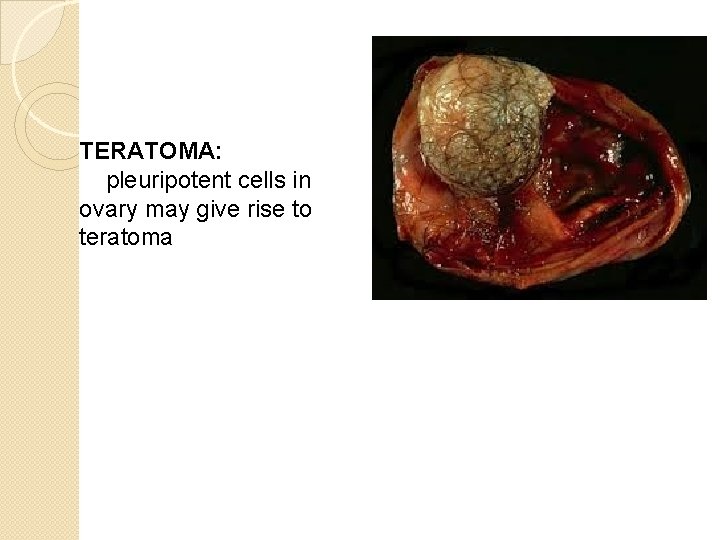
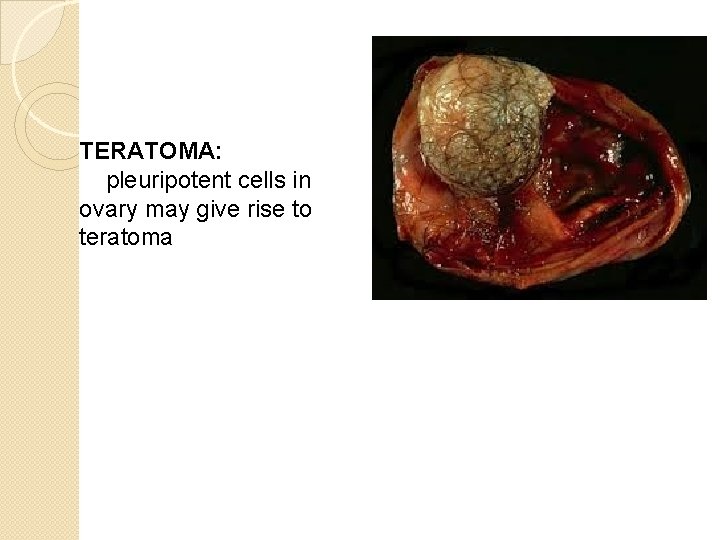
TERATOMA: pleuripotent cells in ovary may give rise to teratoma
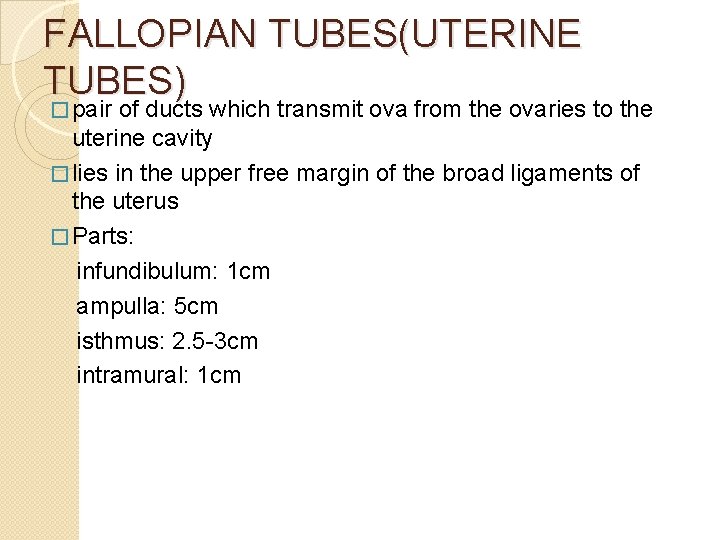
FALLOPIAN TUBES(UTERINE TUBES) � pair of ducts which transmit ova from the ovaries to the uterine cavity � lies in the upper free margin of the broad ligaments of the uterus � Parts: infundibulum: 1 cm ampulla: 5 cm isthmus: 2. 5 -3 cm intramural: 1 cm
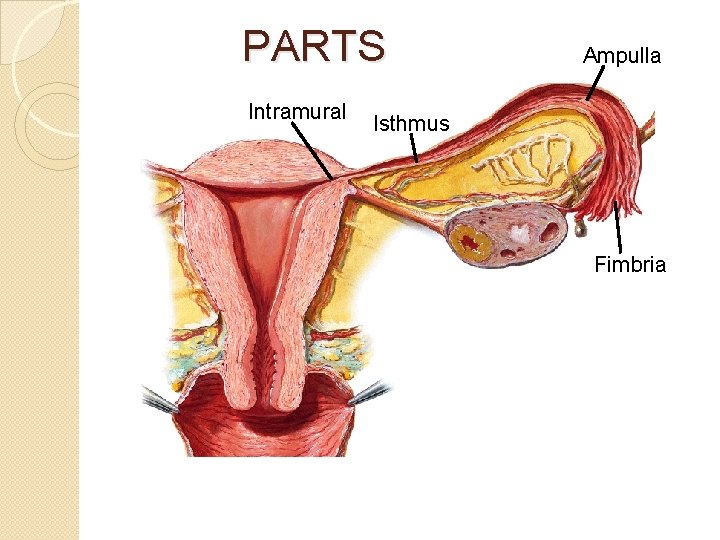
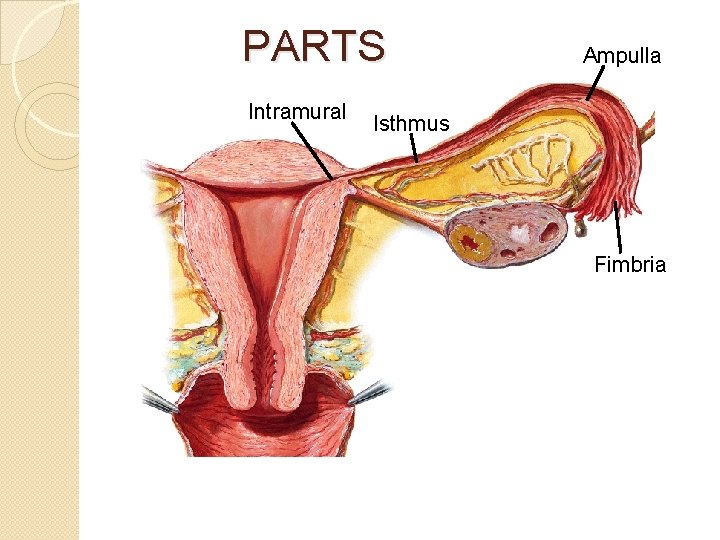
PARTS Intramural Ampulla Isthmus Fimbria
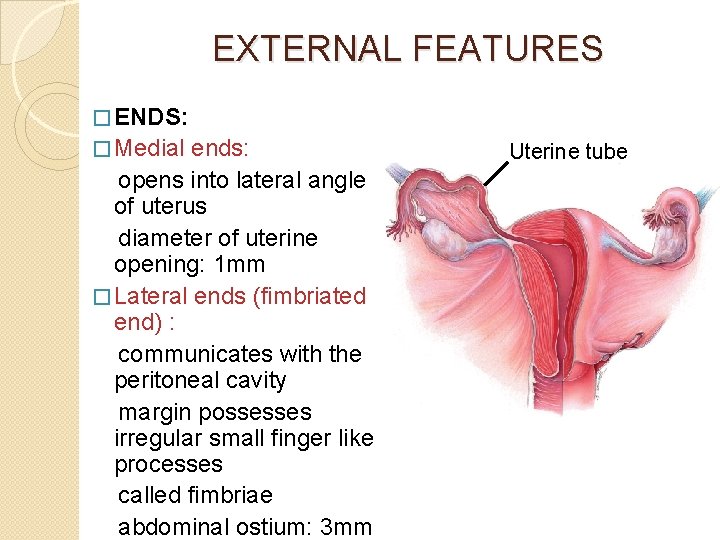
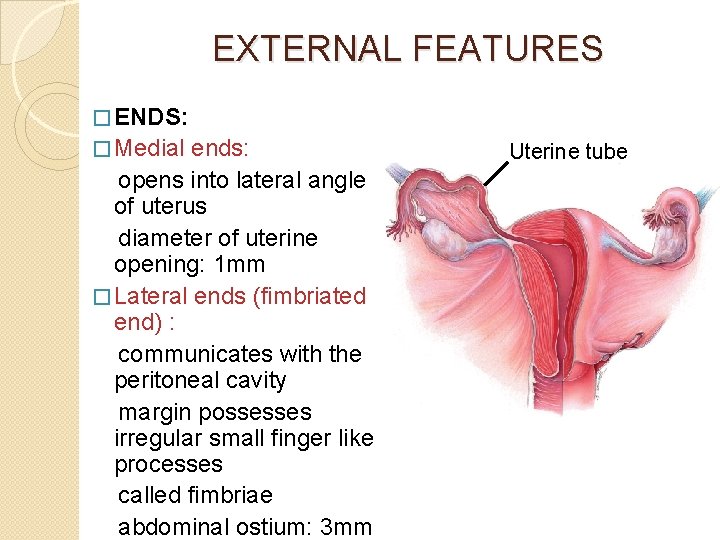
EXTERNAL FEATURES � ENDS: � Medial ends: opens into lateral angle of uterus diameter of uterine opening: 1 mm � Lateral ends (fimbriated end) : communicates with the peritoneal cavity margin possesses irregular small finger like processes called fimbriae abdominal ostium: 3 mm Uterine tube
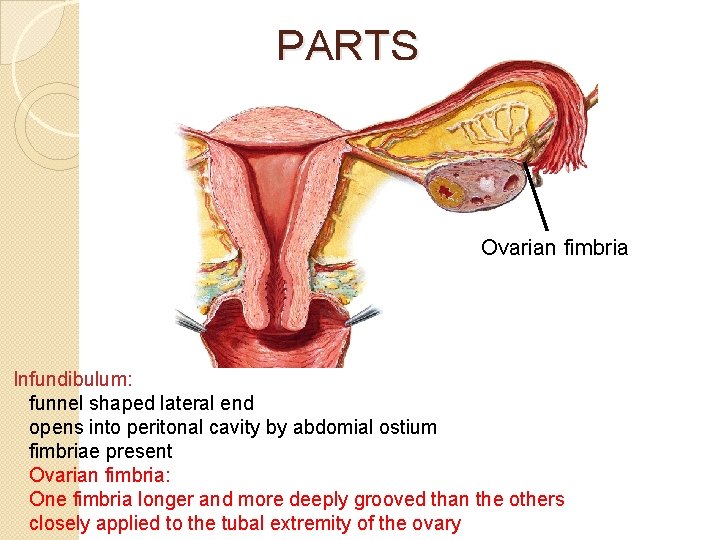
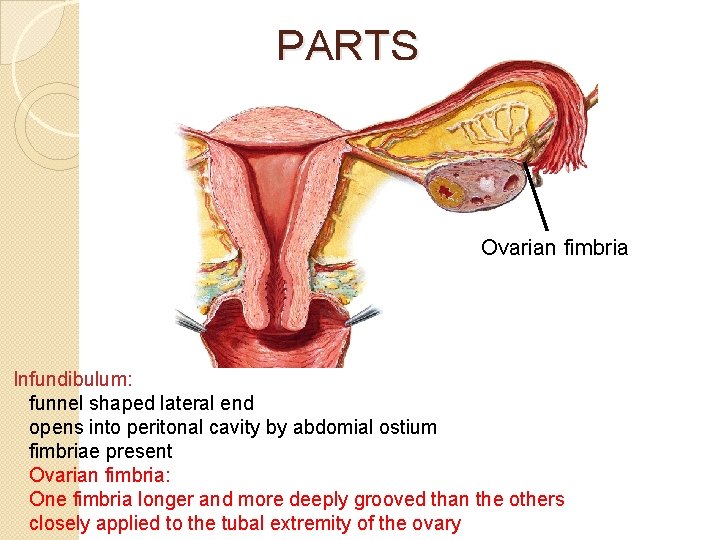
PARTS Ovarian fimbria Infundibulum: funnel shaped lateral end opens into peritonal cavity by abdomial ostium fimbriae present Ovarian fimbria: One fimbria longer and more deeply grooved than the others closely applied to the tubal extremity of the ovary
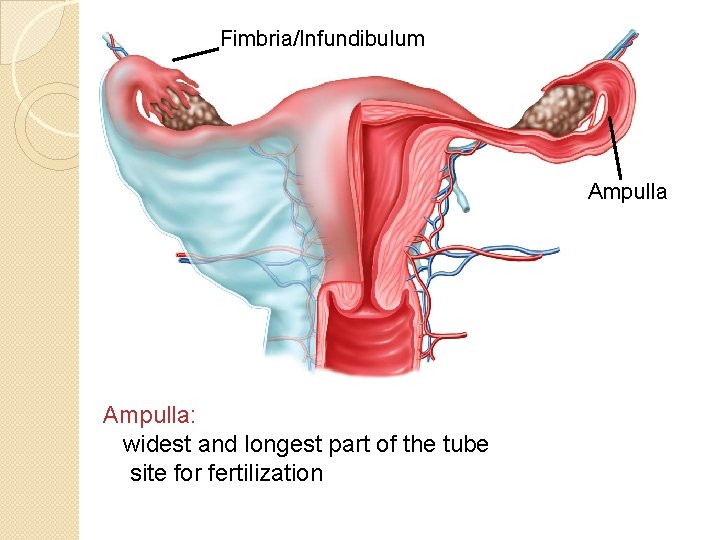
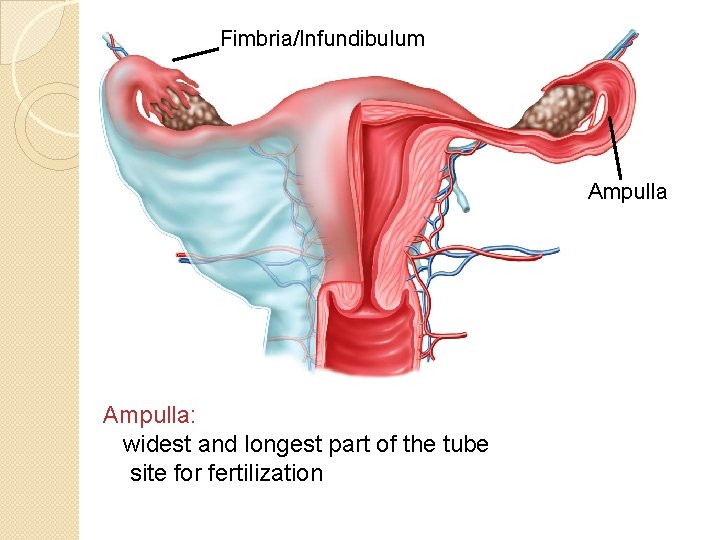
Fimbria/Infundibulum Ampulla: widest and longest part of the tube site for fertilization
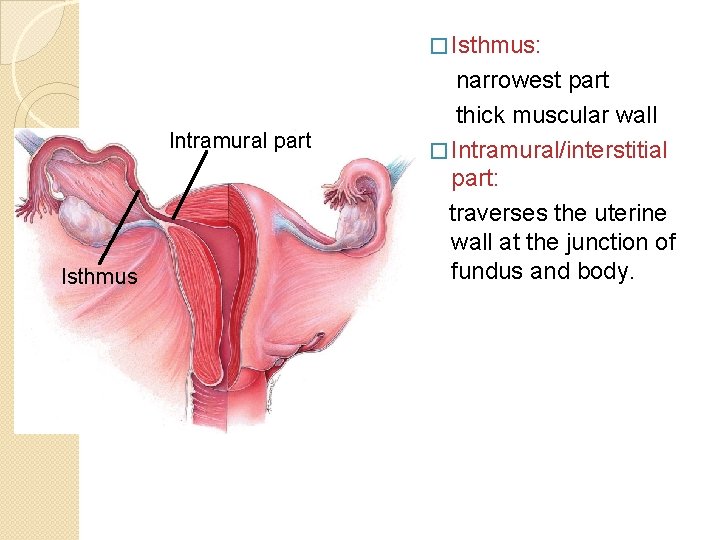
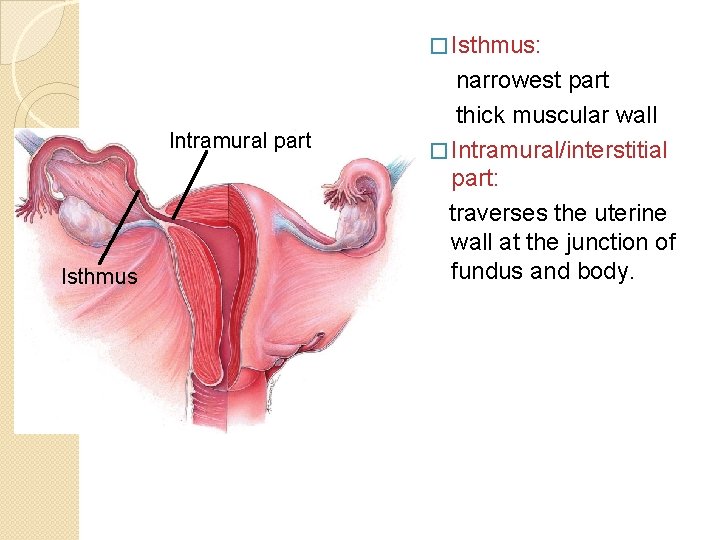
� Isthmus: Intramural part Isthmus narrowest part thick muscular wall � Intramural/interstitial part: traverses the uterine wall at the junction of fundus and body.
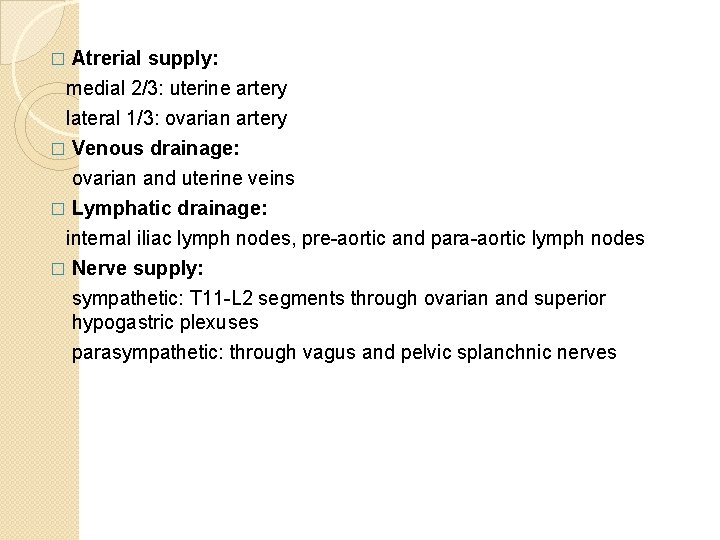
� Atrerial supply: medial 2/3: uterine artery lateral 1/3: ovarian artery � Venous drainage: ovarian and uterine veins � Lymphatic drainage: internal iliac lymph nodes, pre-aortic and para-aortic lymph nodes � Nerve supply: sympathetic: T 11 -L 2 segments through ovarian and superior hypogastric plexuses parasympathetic: through vagus and pelvic splanchnic nerves
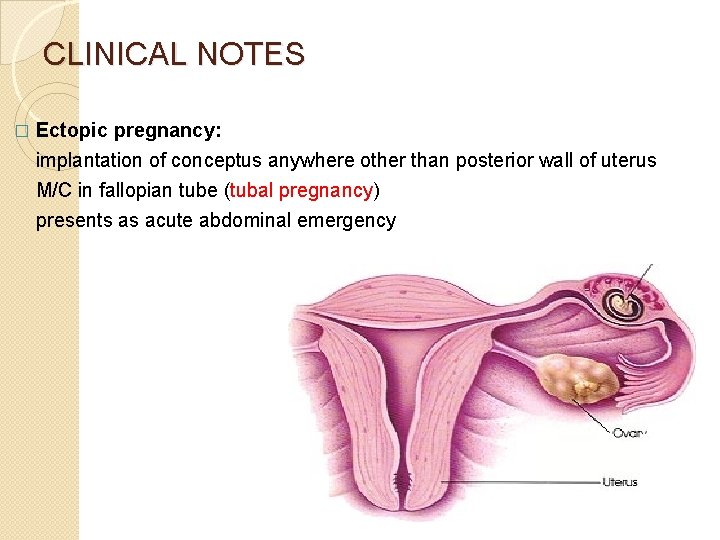
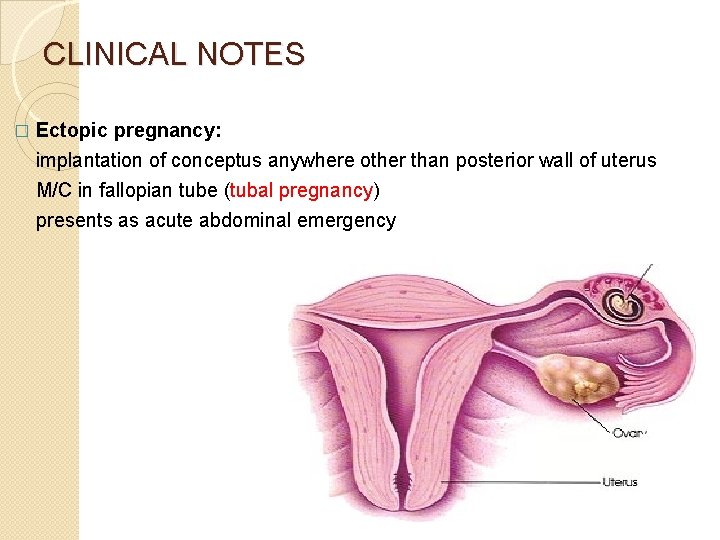
CLINICAL NOTES � Ectopic pregnancy: implantation of conceptus anywhere other than posterior wall of uterus M/C in fallopian tube (tubal pregnancy) presents as acute abdominal emergency
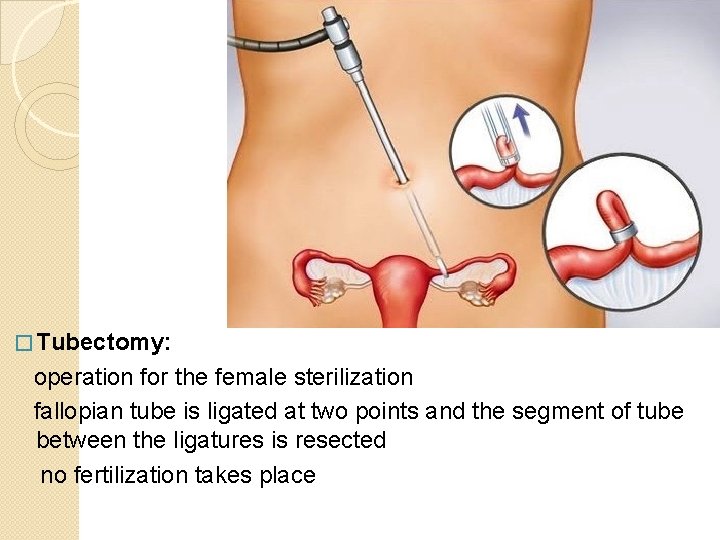
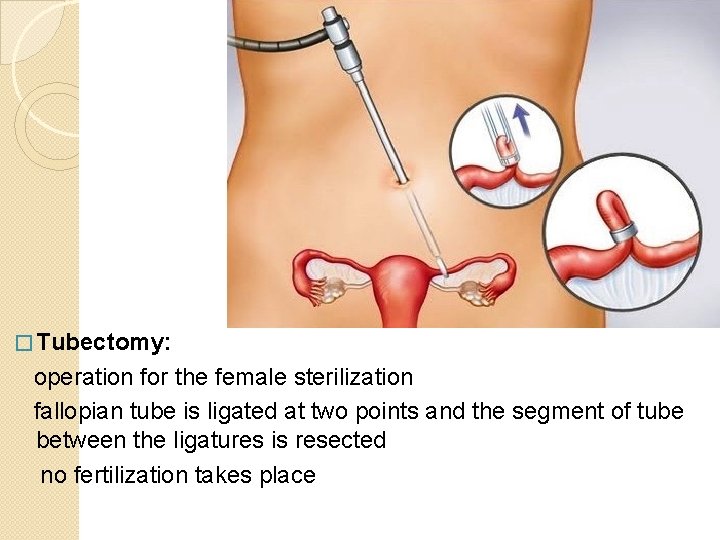
� Tubectomy: operation for the female sterilization fallopian tube is ligated at two points and the segment of tube between the ligatures is resected no fertilization takes place
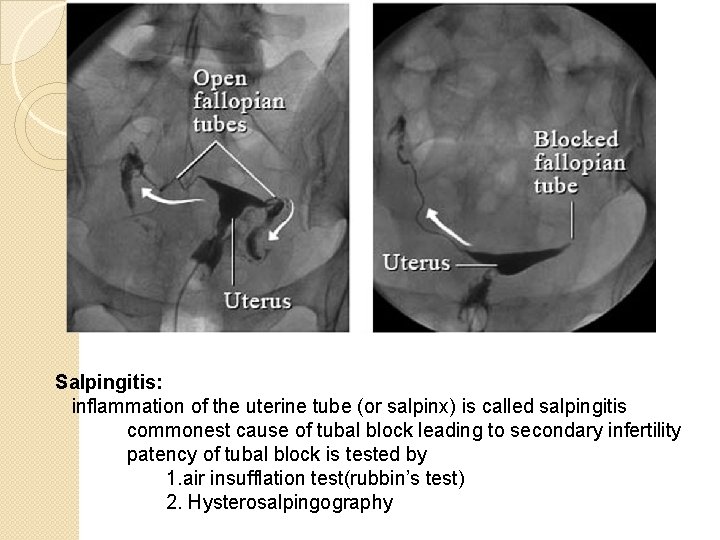
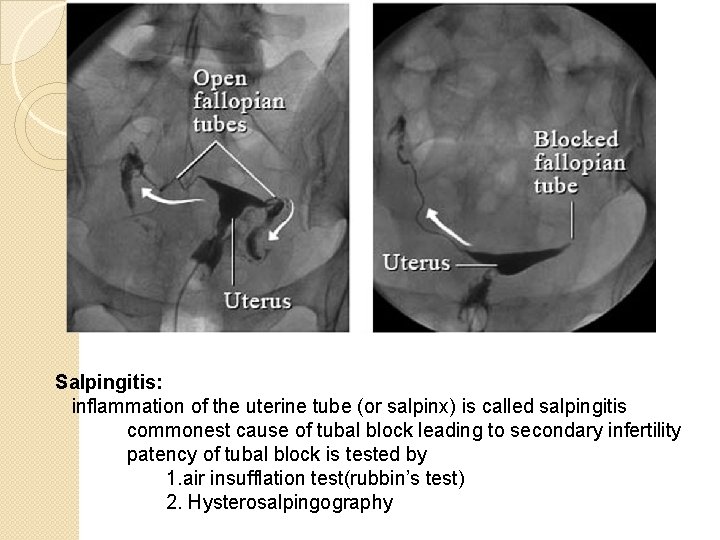
Salpingitis: inflammation of the uterine tube (or salpinx) is called salpingitis commonest cause of tubal block leading to secondary infertility patency of tubal block is tested by 1. air insufflation test(rubbin’s test) 2. Hysterosalpingography
THANK YOU