Female reproductive hormones Gross anatomy of female reproductive
- Slides: 33
Female reproductive hormones
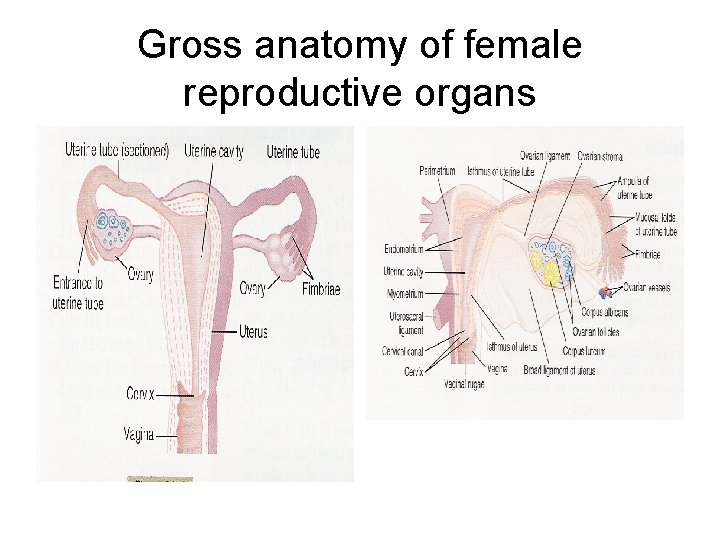
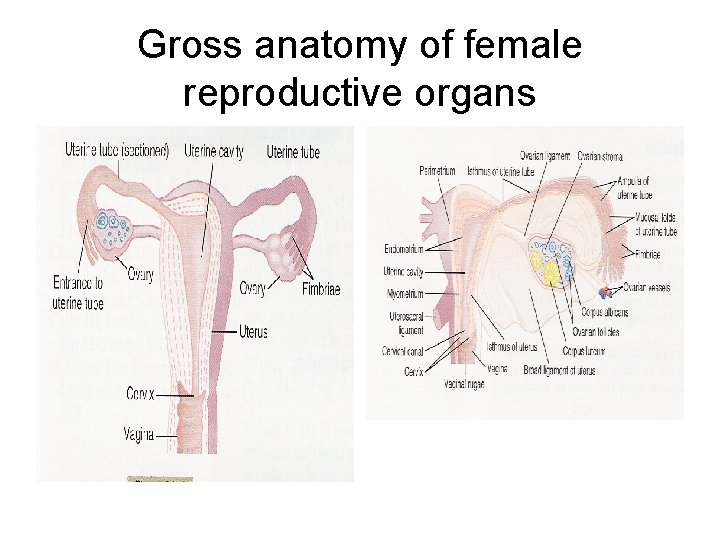
Gross anatomy of female reproductive organs
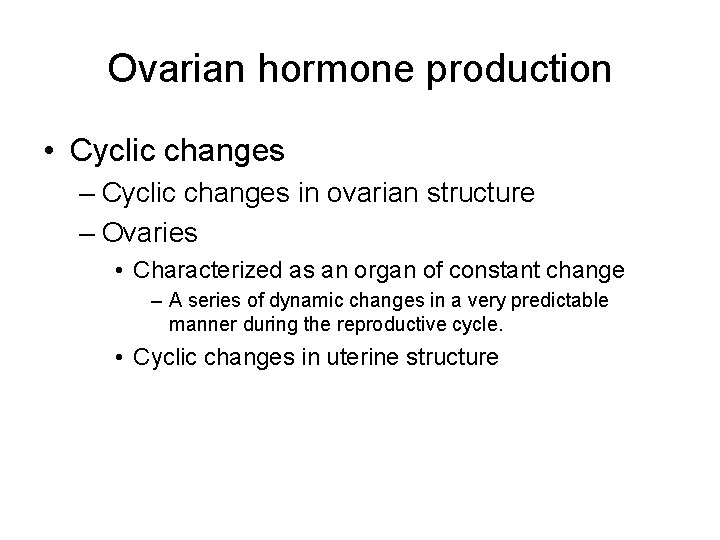
Ovarian hormone production • Cyclic changes – Cyclic changes in ovarian structure – Ovaries • Characterized as an organ of constant change – A series of dynamic changes in a very predictable manner during the reproductive cycle. • Cyclic changes in uterine structure
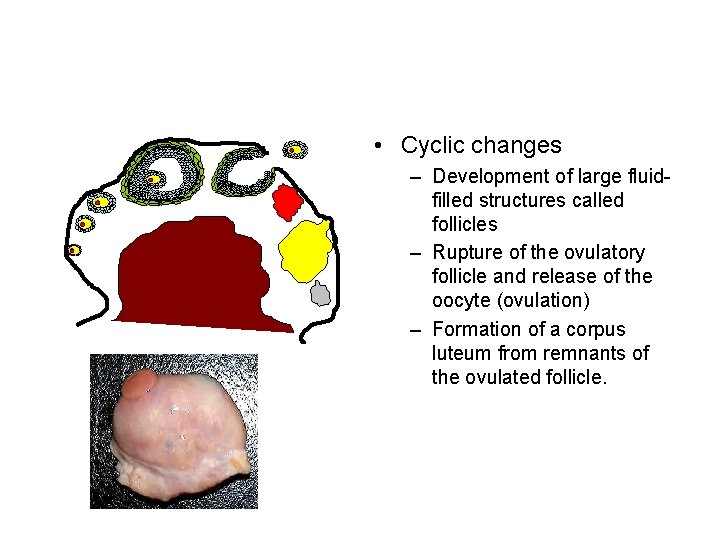
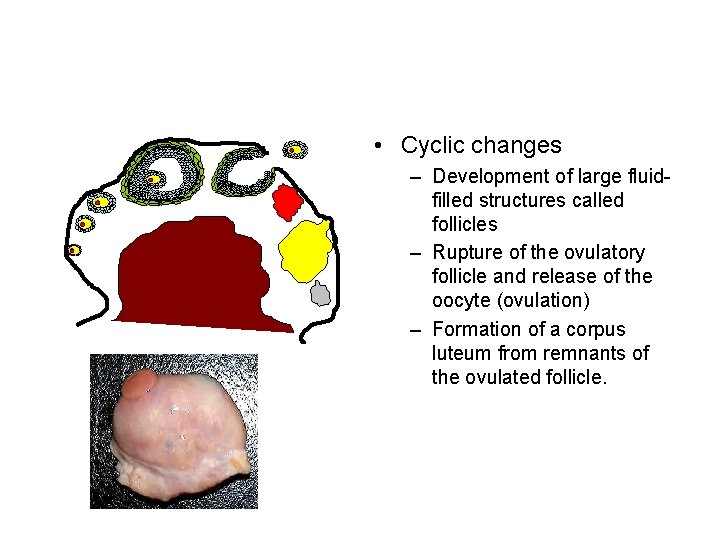
• Cyclic changes – Development of large fluidfilled structures called follicles – Rupture of the ovulatory follicle and release of the oocyte (ovulation) – Formation of a corpus luteum from remnants of the ovulated follicle.
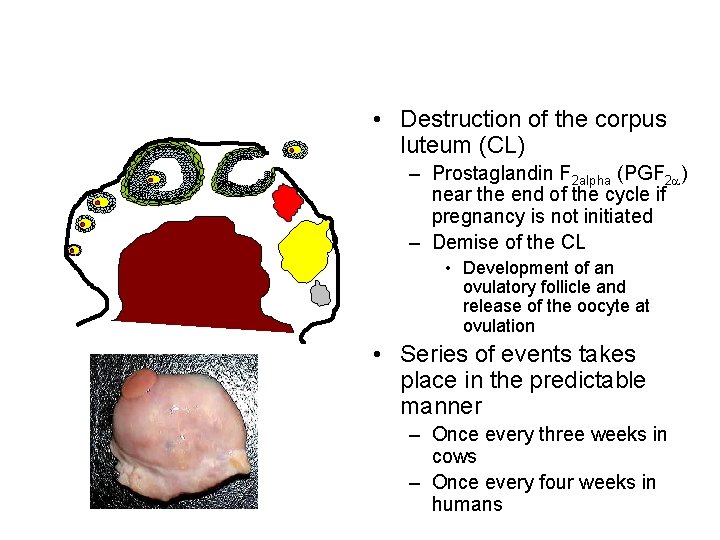
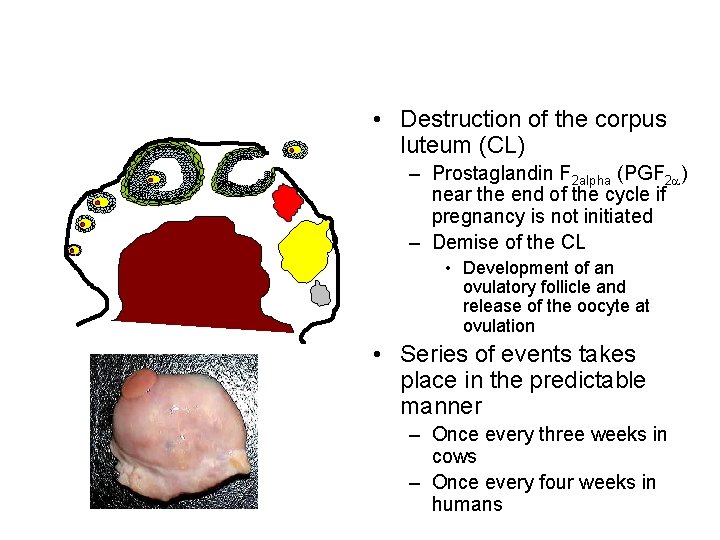
• Destruction of the corpus luteum (CL) – Prostaglandin F 2 alpha (PGF 2 a) near the end of the cycle if pregnancy is not initiated – Demise of the CL • Development of an ovulatory follicle and release of the oocyte at ovulation • Series of events takes place in the predictable manner – Once every three weeks in cows – Once every four weeks in humans
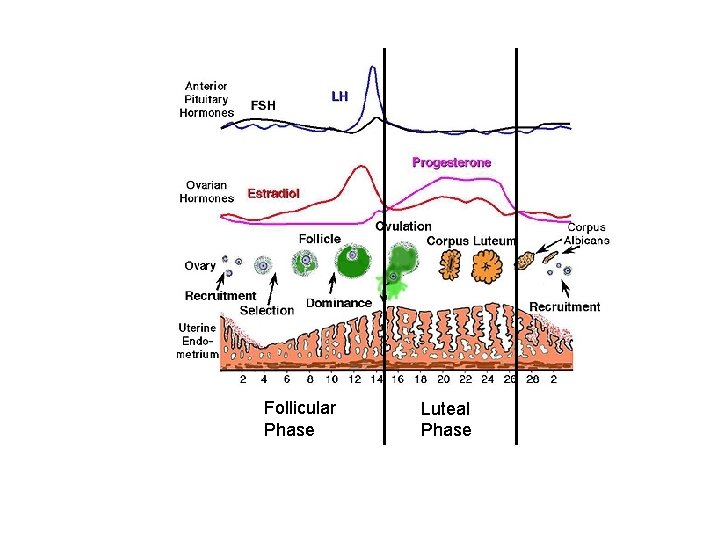
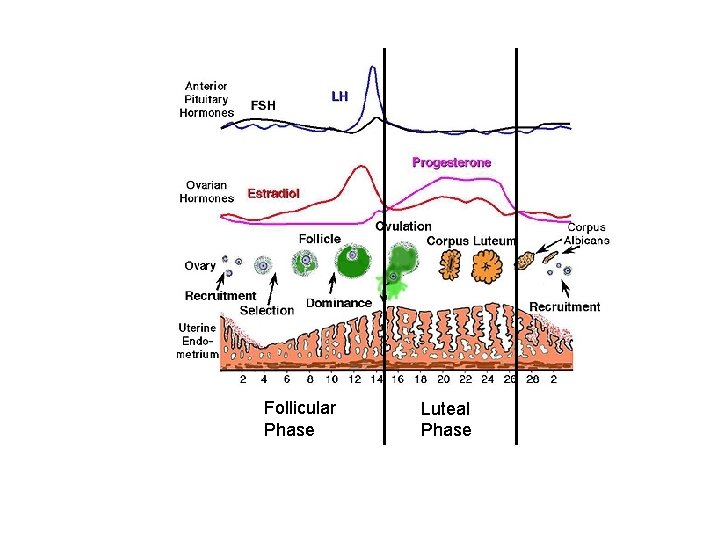
Follicular Phase Luteal Phase
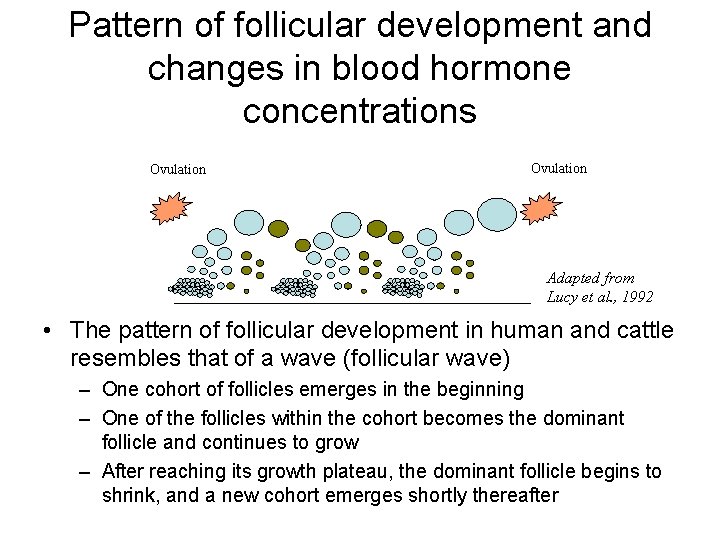
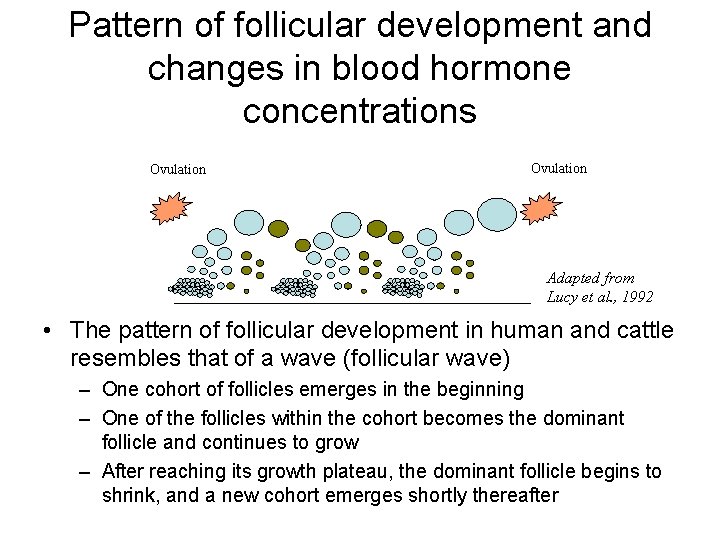
Pattern of follicular development and changes in blood hormone concentrations Ovulation CL CH Ovul ation Ovulation C Ovul ation Adapted from Lucy et al. , 1992 • The pattern of follicular development in human and cattle resembles that of a wave (follicular wave) – One cohort of follicles emerges in the beginning – One of the follicles within the cohort becomes the dominant follicle and continues to grow – After reaching its growth plateau, the dominant follicle begins to shrink, and a new cohort emerges shortly thereafter
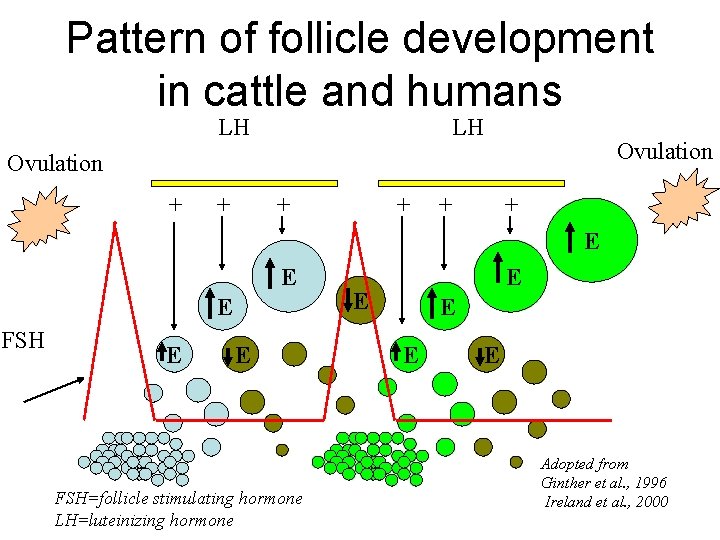
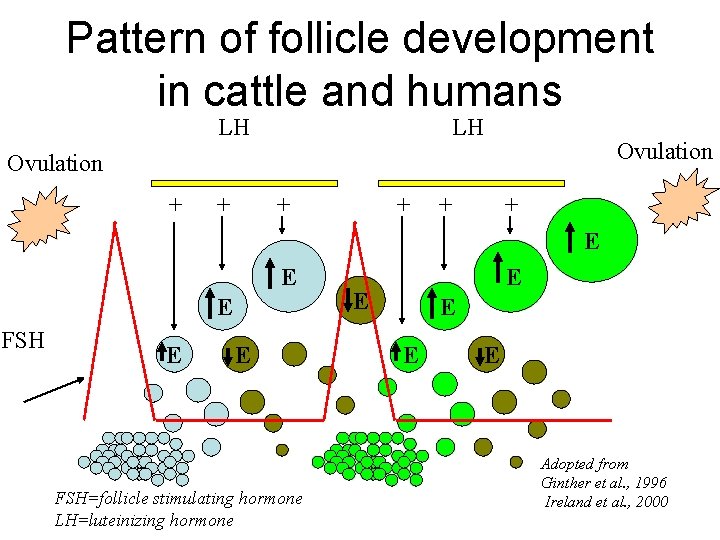
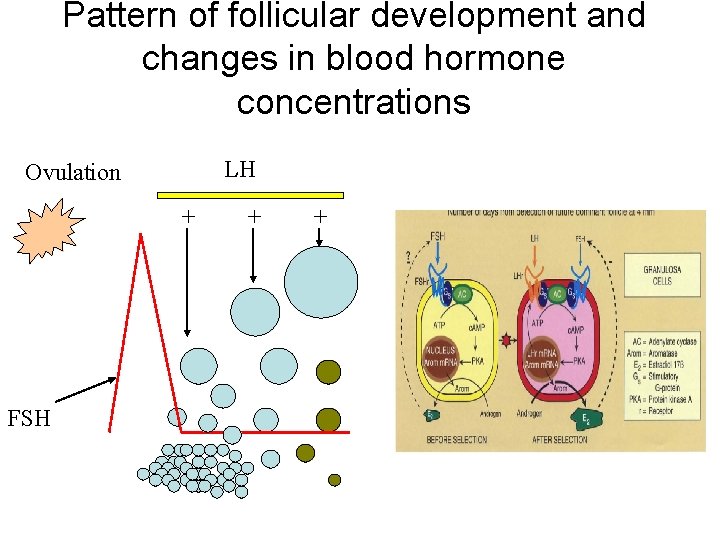
Pattern of follicle development in cattle and humans LH LH Ovulation + + + E E E FSH=follicle stimulating hormone LH=luteinizing hormone E E E Adopted from Ginther et al. , 1996 Ireland et al. , 2000
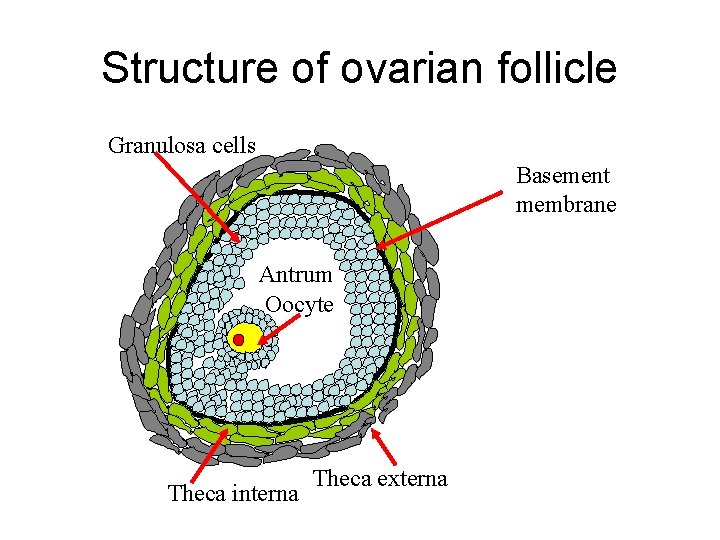
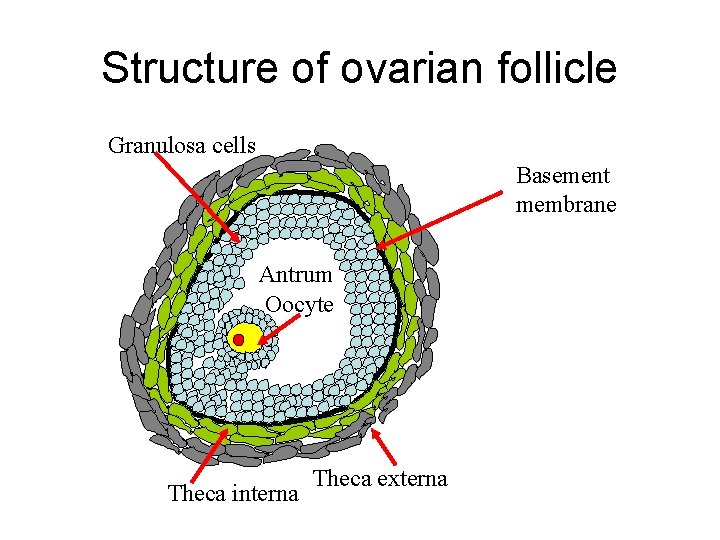
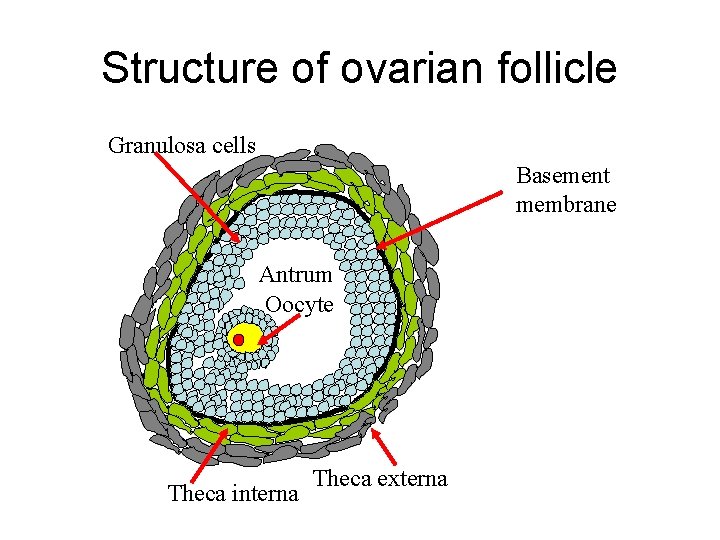
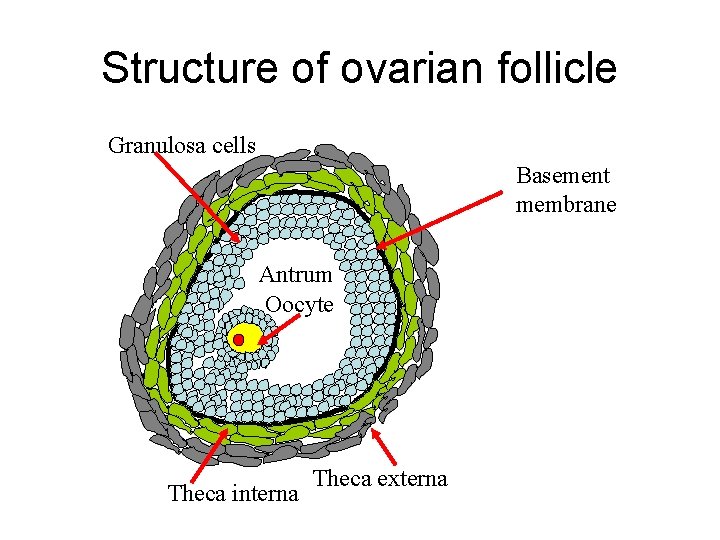
Structure of ovarian follicle Granulosa cells Basement membrane Antrum Oocyte Theca interna Theca externa
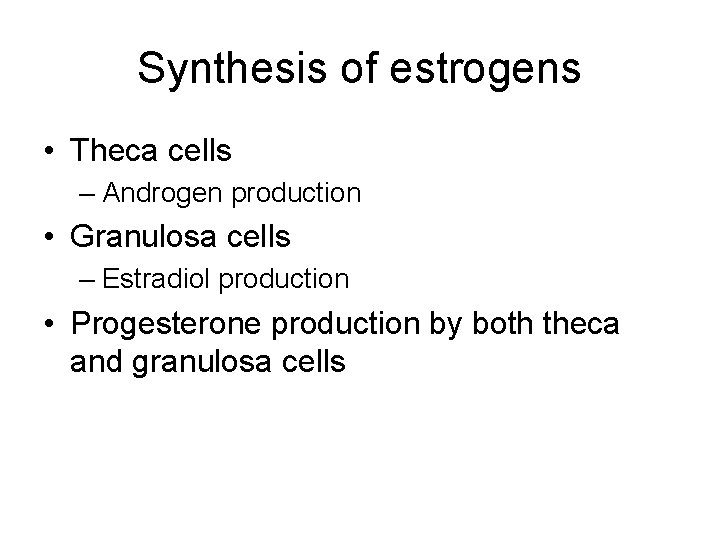
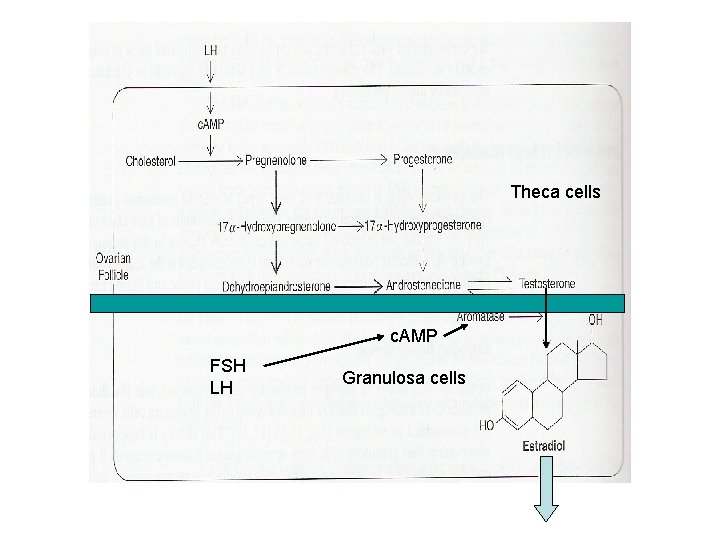
Synthesis of estrogens • Theca cells – Androgen production • Granulosa cells – Estradiol production • Progesterone production by both theca and granulosa cells
Structure of ovarian follicle Granulosa cells Basement membrane Antrum Oocyte Theca interna Theca externa
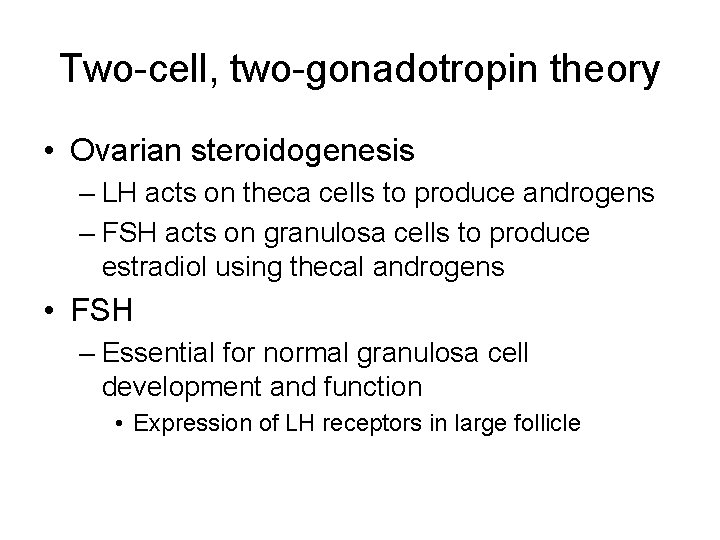
Two-cell, two-gonadotropin theory • Ovarian steroidogenesis – LH acts on theca cells to produce androgens – FSH acts on granulosa cells to produce estradiol using thecal androgens • FSH – Essential for normal granulosa cell development and function • Expression of LH receptors in large follicle
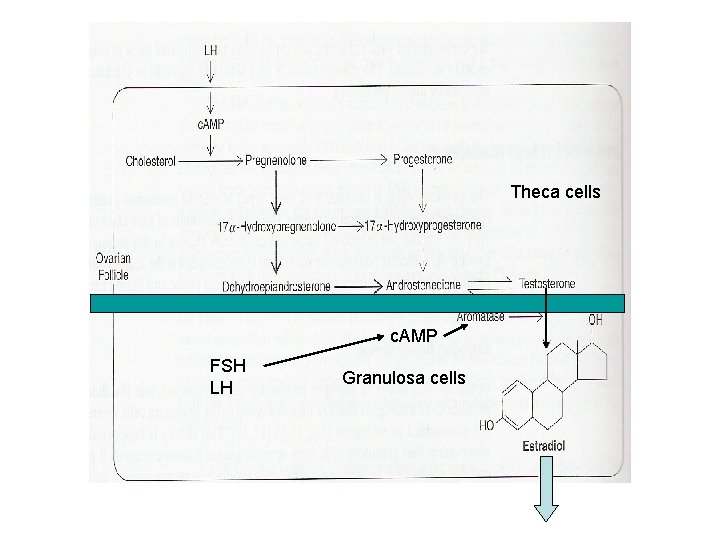
Theca cells c. AMP FSH LH Granulosa cells
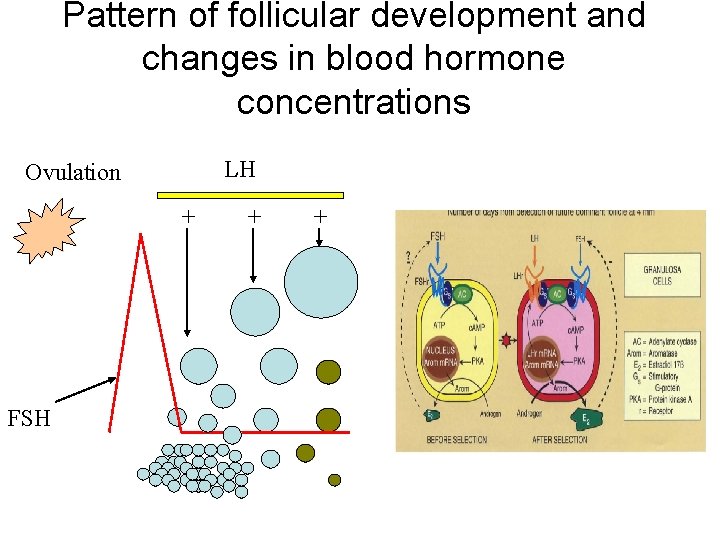
Pattern of follicular development and changes in blood hormone concentrations LH Ovulation + FSH + +
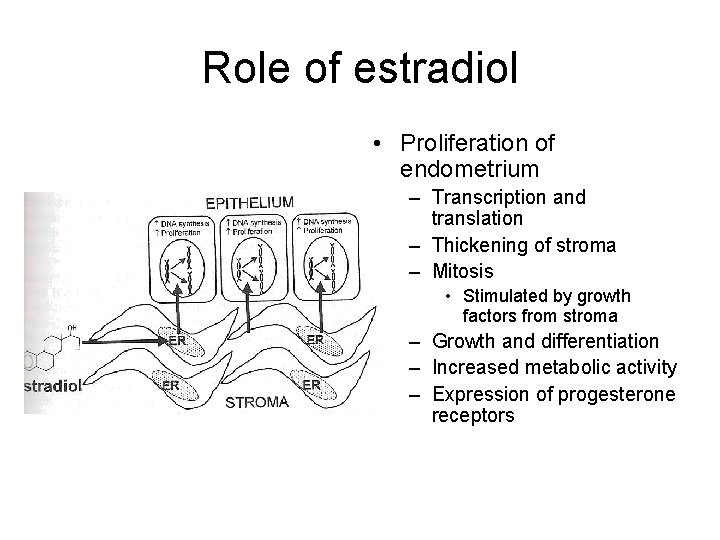
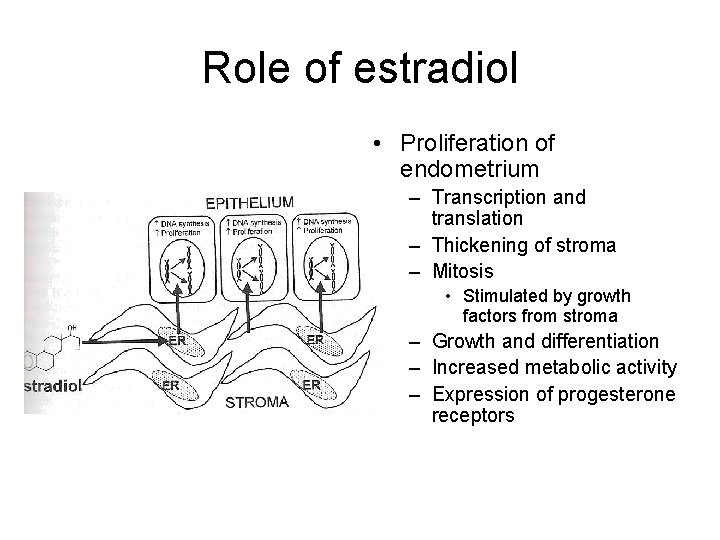
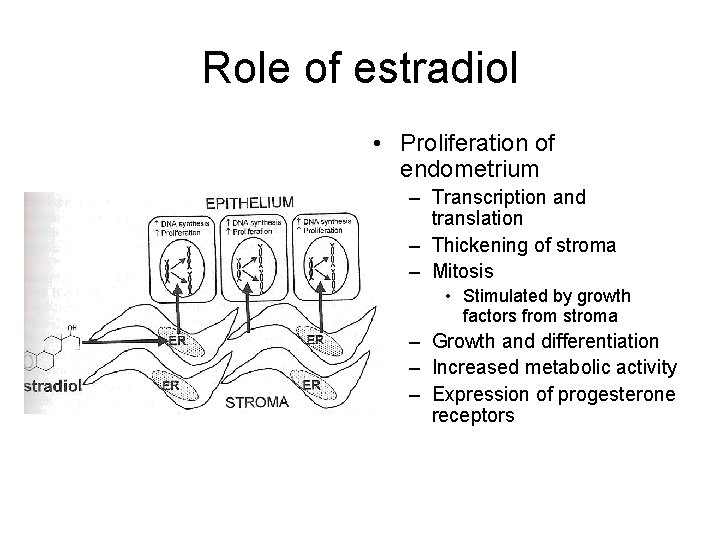
Role of estradiol • Proliferation of endometrium – Transcription and translation – Thickening of stroma – Mitosis • Stimulated by growth factors from stroma – Growth and differentiation – Increased metabolic activity – Expression of progesterone receptors
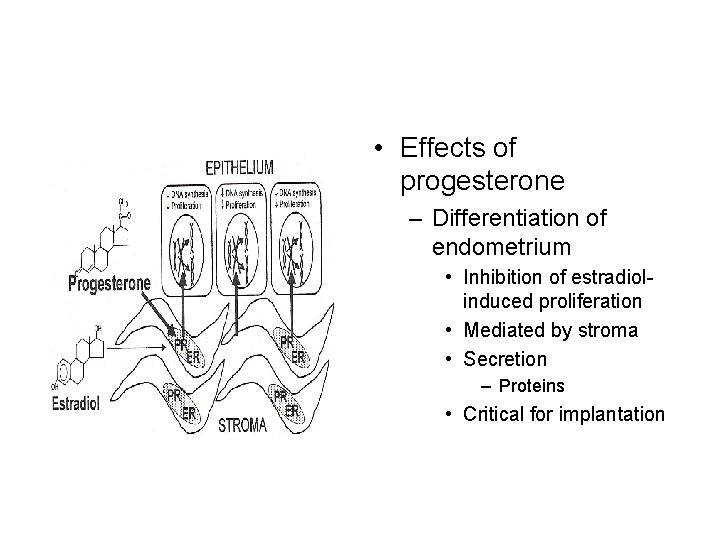
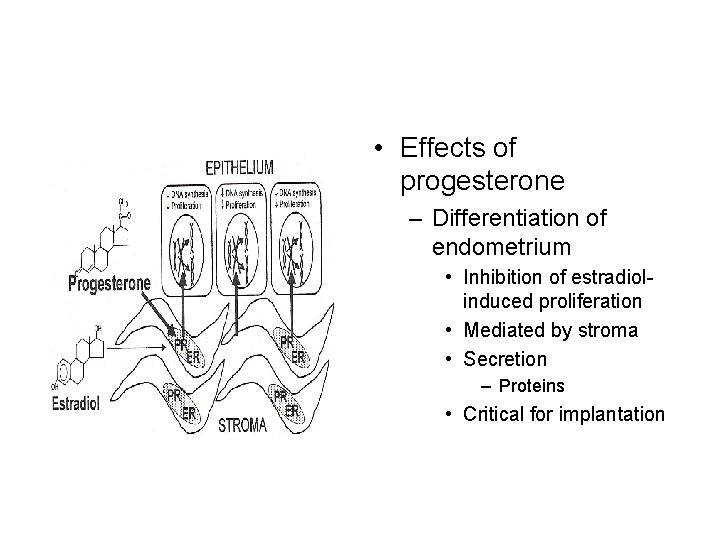
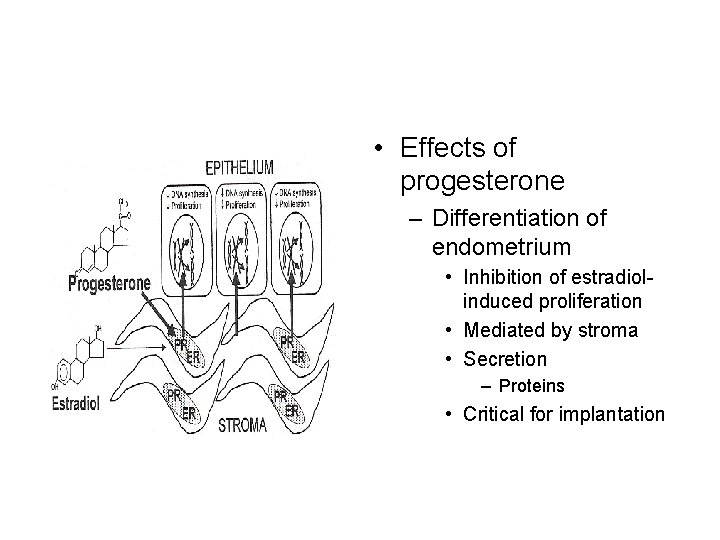
• Effects of progesterone – Differentiation of endometrium • Inhibition of estradiolinduced proliferation • Mediated by stroma • Secretion – Proteins • Critical for implantation
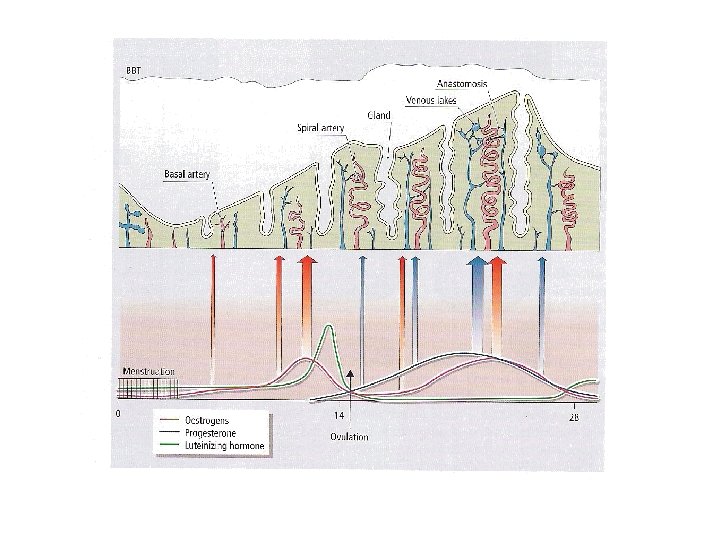
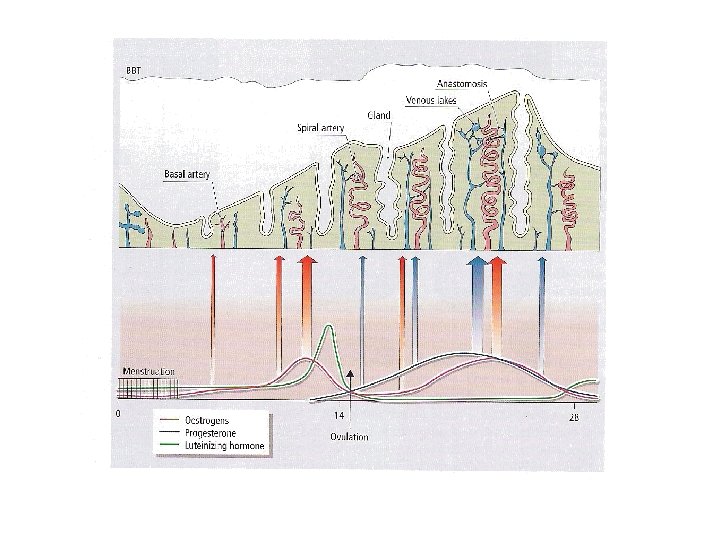
• Uterine endometrium – Mucosal lining of the uterus • Inner-most lining • Well-developed in human compared to other species – Placentation • Menstruation (shedding of endomertial tissue) – Spiral arteries – Hemorrhage (changes in blood flow) – Renewal of endometrium during each reproductive cycle
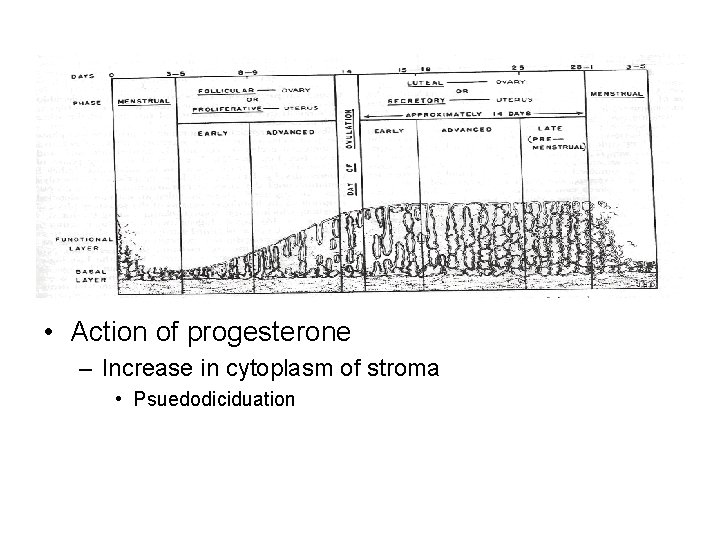
• Hormone-induced changes in endometrium – Cyclic in nature • Re-epithelialization – Menstrual-postmenstrual transition • Endometrial proliferation – Estradiol • Epithelial secretion – Estradiol and progesterone • Premestrual ischemia – Loss of blood supply to epithelia • Menstruation
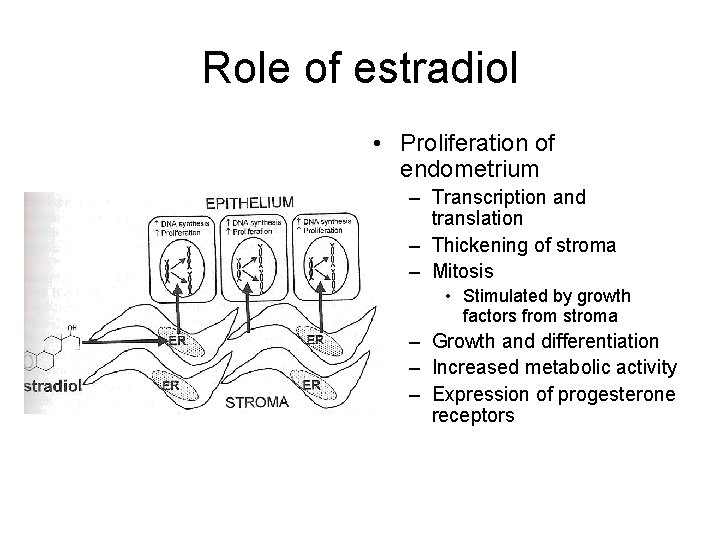
Role of estradiol • Proliferation of endometrium – Transcription and translation – Thickening of stroma – Mitosis • Stimulated by growth factors from stroma – Growth and differentiation – Increased metabolic activity – Expression of progesterone receptors
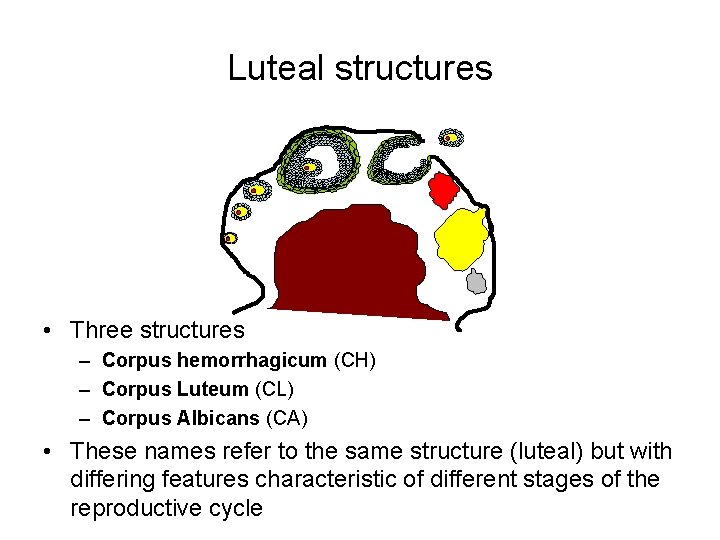
Luteal structures • After ovulation – The oocyte is released from the preovulatory follicle – Theca and granulosa cells remaining in the follicular wall undergo dramatic changes • Formation of a corpus luteum. – A shift from producing estradiol (granulosa) androgen (theca) to producing large amounts of progesterone
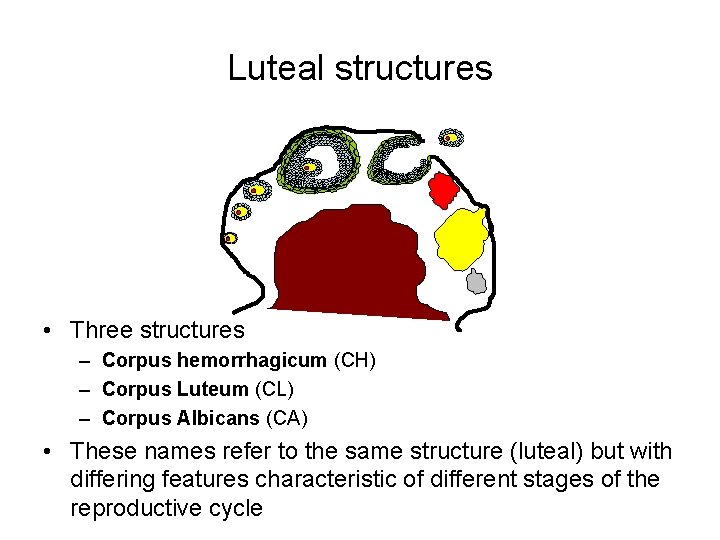
Luteal structures • Three structures – Corpus hemorrhagicum (CH) – Corpus Luteum (CL) – Corpus Albicans (CA) • These names refer to the same structure (luteal) but with differing features characteristic of different stages of the reproductive cycle
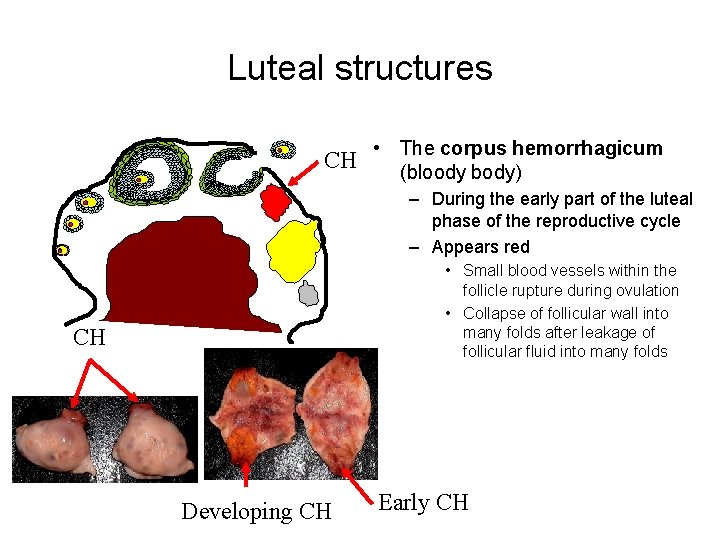
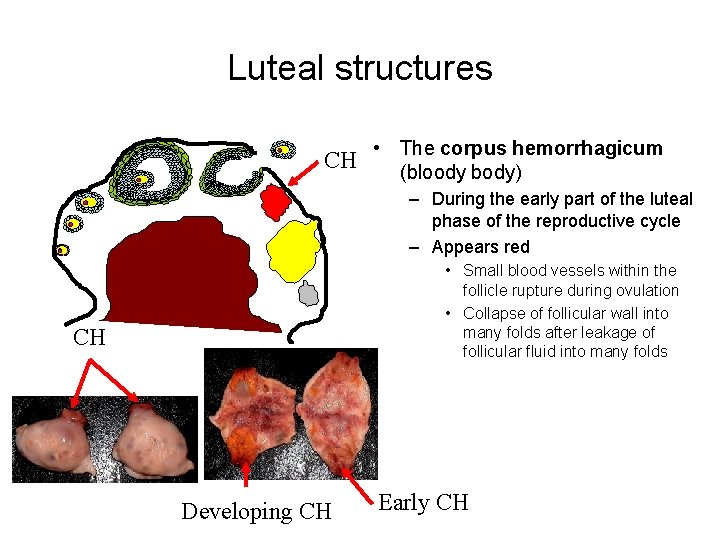
Luteal structures • The corpus hemorrhagicum CH (bloody body) – During the early part of the luteal phase of the reproductive cycle – Appears red • Small blood vessels within the follicle rupture during ovulation • Collapse of follicular wall into many folds after leakage of follicular fluid into many folds CH Developing CH Early CH
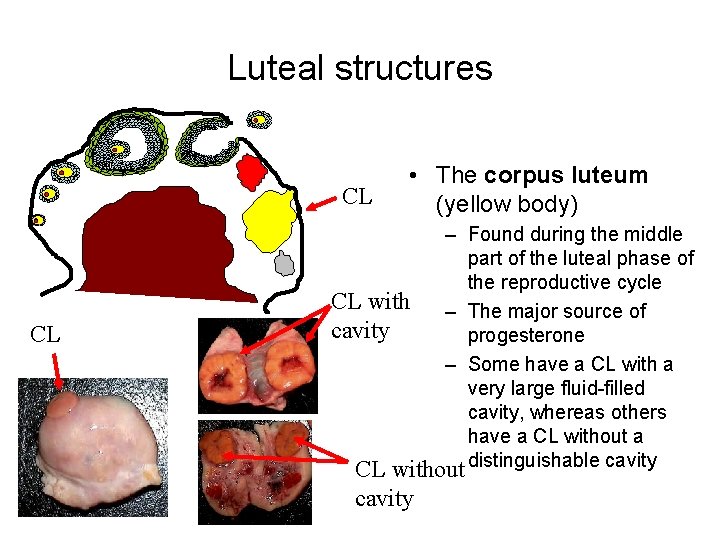
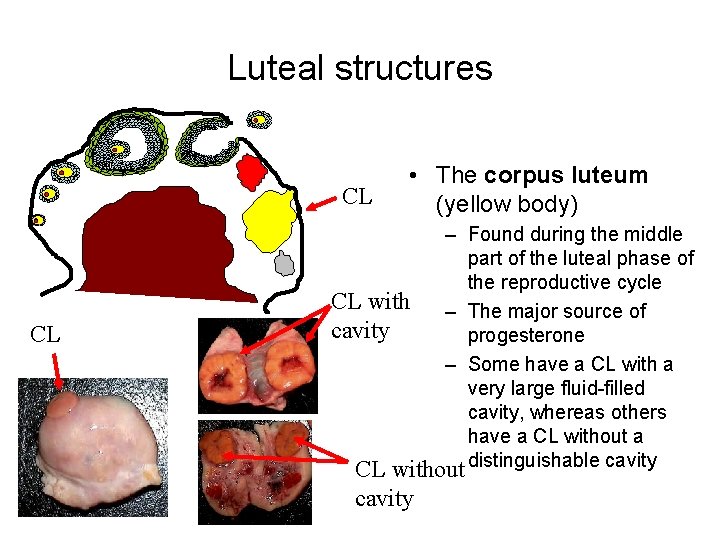
Luteal structures CL CL • The corpus luteum (yellow body) – Found during the middle part of the luteal phase of the reproductive cycle CL with – The major source of cavity progesterone – Some have a CL with a very large fluid-filled cavity, whereas others have a CL without distinguishable cavity
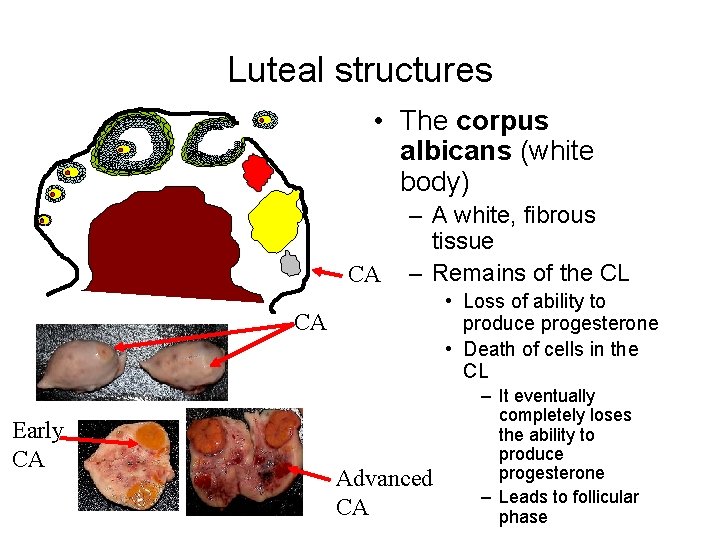
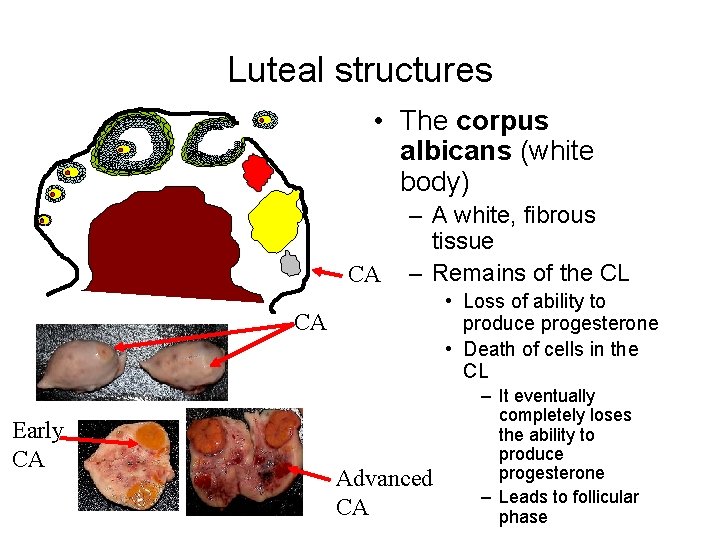
Luteal structures • The corpus albicans (white body) CA – A white, fibrous tissue – Remains of the CL • Loss of ability to produce progesterone • Death of cells in the CL CA Early CA Advanced CA – It eventually completely loses the ability to produce progesterone – Leads to follicular phase
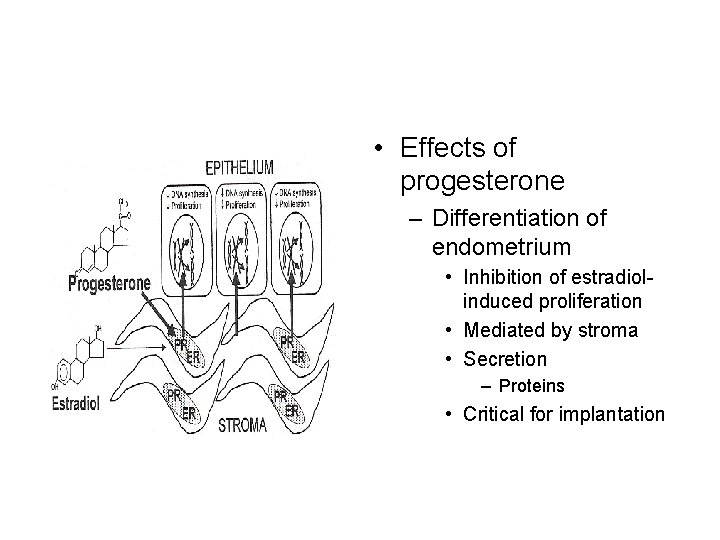
• Effects of progesterone – Differentiation of endometrium • Inhibition of estradiolinduced proliferation • Mediated by stroma • Secretion – Proteins • Critical for implantation
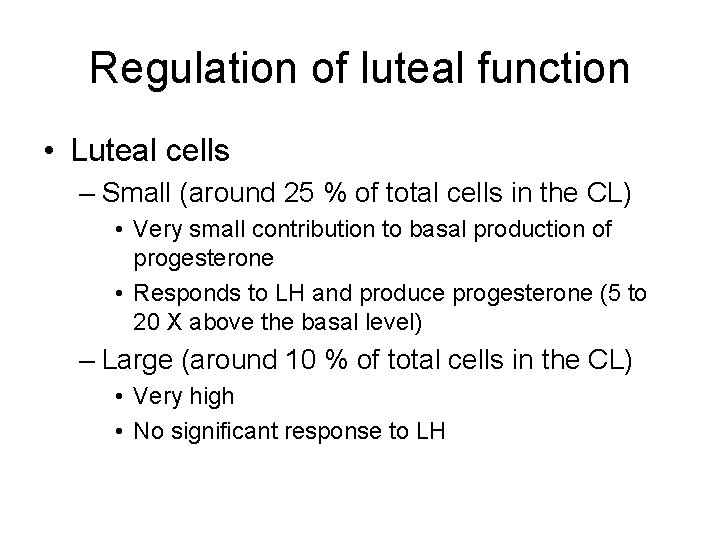
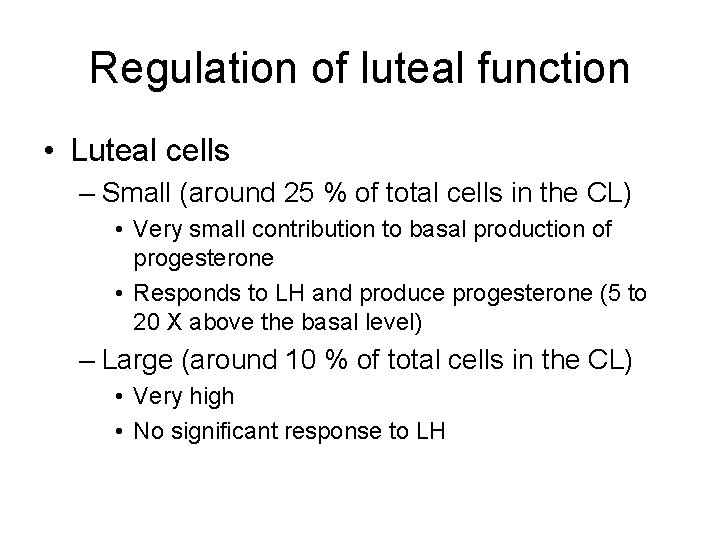
Regulation of luteal function • Luteal cells – Small (around 25 % of total cells in the CL) • Very small contribution to basal production of progesterone • Responds to LH and produce progesterone (5 to 20 X above the basal level) – Large (around 10 % of total cells in the CL) • Very high • No significant response to LH
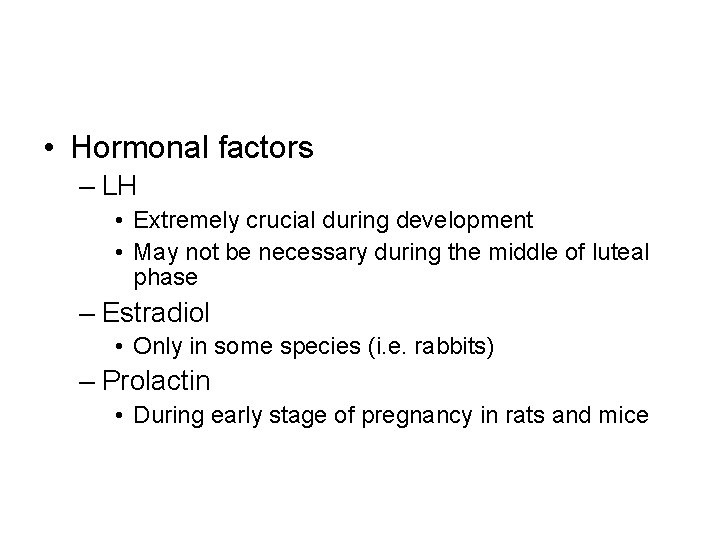
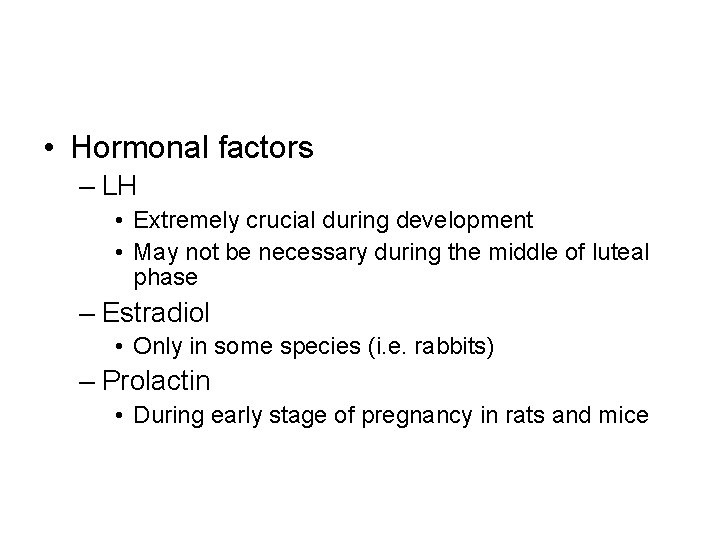
• Hormonal factors – LH • Extremely crucial during development • May not be necessary during the middle of luteal phase – Estradiol • Only in some species (i. e. rabbits) – Prolactin • During early stage of pregnancy in rats and mice
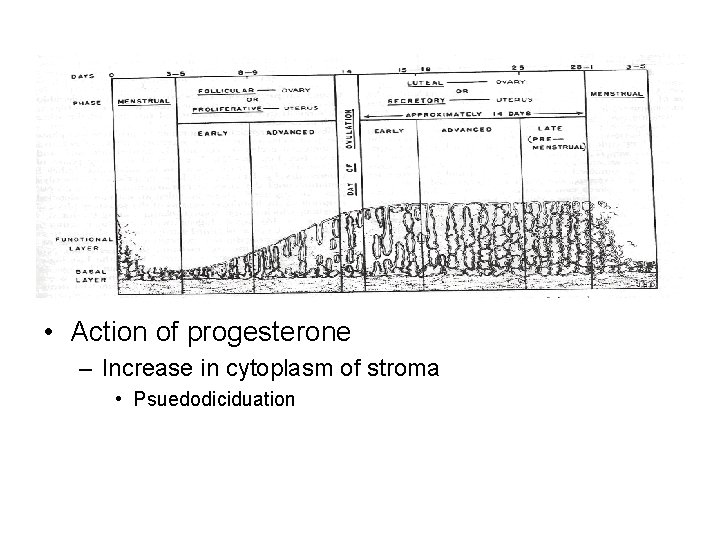
• Action of progesterone – Increase in cytoplasm of stroma • Psuedodiciduation
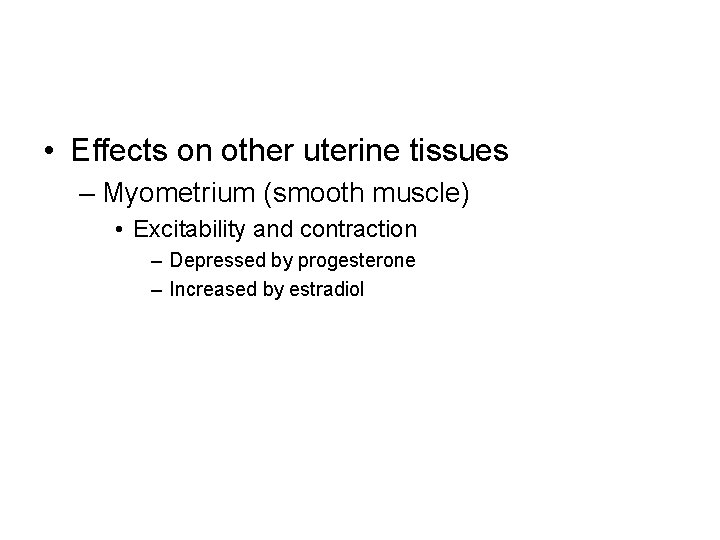
• Effects on other uterine tissues – Myometrium (smooth muscle) • Excitability and contraction – Depressed by progesterone – Increased by estradiol
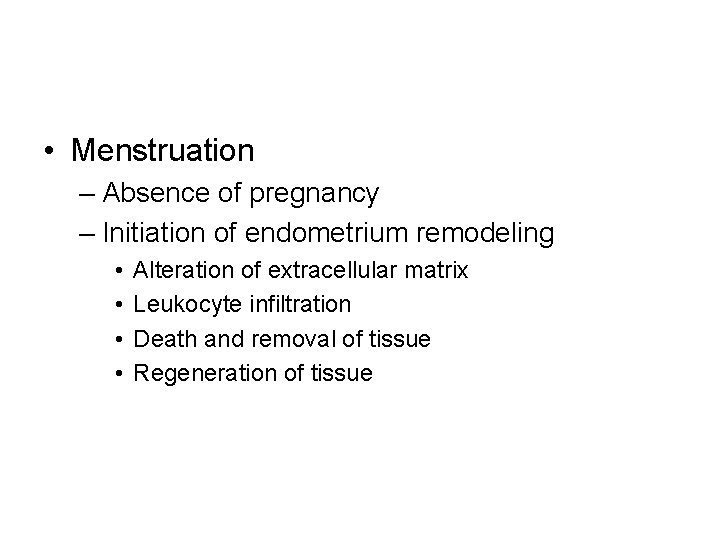
• Menstruation – Absence of pregnancy – Initiation of endometrium remodeling • • Alteration of extracellular matrix Leukocyte infiltration Death and removal of tissue Regeneration of tissue
• Menstruation – Withdraw of steroid hormones • Constriction of arterioles and coiled arteries – Ischemia – Precedes bleeding • Bleeding – Relaxation of arteries – Induction of hypoxia-reperfusion injury (formation of hematoma) – Detachment of tissue fragments
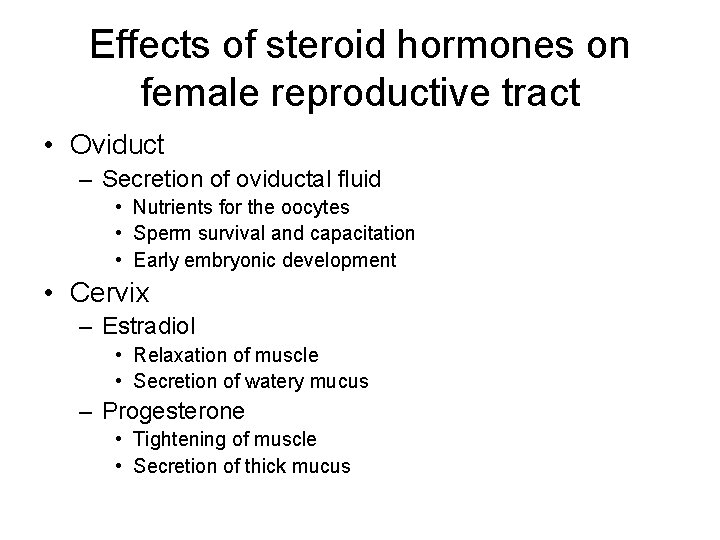
Effects of steroid hormones on female reproductive tract • Oviduct – Secretion of oviductal fluid • Nutrients for the oocytes • Sperm survival and capacitation • Early embryonic development • Cervix – Estradiol • Relaxation of muscle • Secretion of watery mucus – Progesterone • Tightening of muscle • Secretion of thick mucus