Female Incontinence Learning Objectives Define urinary incontinence Diagnosis
Female Incontinence

Learning Objectives • Define urinary incontinence • Diagnosis of stress, urge, and mixed incontinence • Evaluation of incontinence • Management – both conservative and surgical • Topics for another day • Interstitial cystitis • Neurogenic voiding dysfunction
Definitions • Urgency: the sudden, strong desire to pass urine that is difficult to defer • Incontinence: Involuntary loss of urine • Stress urinary incontinence: loss of urine secondary to an increase in abdominal pressure i. e. with coughing, sneezing, laughing • Urgency urinary incontinence: leakage associated with urgency • Mixed Urinary incontinence: incontinence associated with both stress and urgency • Overflow incontinence: incontinence secondary to a full bladder and inability to completely empty
Risk Factors • Age • Obesity • Parity • Mode of Delivery • Family History • Ethnicity/race
Diagnosis • Mandatory • History and Physical Exam • Urinalysis/Urine microscopy • Consider • Urine Culture • Renal function assessment • Voiding Diary • Very helpful in those with complaints of frequency, nocturia, and query IC • Renal US with PVR • Cystoscopy • Urodynamics
Overactive Bladder • Syndrome of urgency, with or without incontinence, which is often accompanied by nocturia and urinary frequency • Can be idiopathic or related to neurologic disorders • Beware the “hidden” Neurogenic Bladders • • Stroke Dementia Diabetes Degenerative disc disease
EPIC Study • Largest population based study on OAB • 19000 people • Overall prevalence of OAB 11. 8% (10. 8% men and 12. 8% women) • In patients 40 -59, 51% of men and 56% of women experience storage symptoms
Impact on Quality of Life • Urinary incontinence has major impact on quality of life • Direct correlation between UI and depression • Constant worry about reaching toilet in time • Impact on sexuality
Overactive Bladder or Interstitial Cystitis? • 2 key questions on history • Why do you void? • Patients with OAB void due to concern about leakage • Patients with IC void due to pain, which is relieved by voiding • Do you have night time symptoms? • Patients with OAB do not have significant nocturia – may void 1 -2 x/night • Patients with IC have equivalent frequency at nighttime as day time - typically voiding 5+ times per night
Key Diagnoses to Rule Out • Bladder cancer • Ensure UA is bland • Urinary retention • Check a post void residual • Neurologic Disorders
Management • Lifestyle Modification and healthy bladder habits • • Weight loss Avoiding bladder irritants Management of constipation Smoking cessation • Furtherapy should be very patient driven • Long term adherence to medical therapy for OAB is poor
Management • Overactive Bladder • Pharmacotherapy • Anticholinergic medication • Beta 3 agonist • Intradetrusor Botox • Surgical management • Family physicians should feel comfortable with medical therapy for OAB • One study demonstrated that less than 25% of patients referred to urology for urgency and UUI had been trialed on a medication prior to referral
Anticholinergic Medication • • • Allow the bladder to hold more Decrease urgency Decrease incontinence episodes Improve frequency Side effects • • Dry mouth Dry eyes Constipation Contraindications • Uncontrolled tachyarrythmias, myasthenia gravis, gastric retention, narrow angle-closure glaucoma • Please avoid oxybutynin • Major cognitive side effects, particularly in elderly
Anticholinergic Medication • Vesicare or Solifenacin • • Most M 3 or ”bladder selective” 5 mg PO daily Can increase to 10 mg PO daily or 5 mg PO BID Give at least 1 month trial • Other anticholinergics • Tolterodine, fesoterodine, darifenacin, trospium • If medication is not efficacious, consider a change in dose, change in medication, or change to Beta agonist
Beta 3 Agonist • Sympathetic agonist • Similar effects as anticholinergic medication • Myrbetriq or Mirabegron • 25 mg PO daily or 50 mg PO daily • Side effects • Slight increase of systolic BP by 2 -3 points • Should not be given to patients with uncontrolled hypertension • Takes 8 weeks to reach maximum benefit
Maximal Medical Therapy for OAB • Combination of Vesicare and Myrbetriq in studies • Can combine any anticholinergic with Myrbetriq • Intradetrusor botox is the next step if this fails
Medication Pathway • Start with Vesicare 5 mg PO daily x 3 months • If side effects/minimal efficacy, trial myrbetriq 25 mg PO daily x 7 days then increase to 50 mg PO daily x 3 months • Will then combine Vesicare + myrbetriq x 3 months • Then botox
Management • Mixed Urinary Incontinence • Have to treat the urgency FIRST • Surgery for SUI can either improve or worsen urgency • Patients with predominant SUI and concomitant urge are still candidates for surgery, as long as they are aware of the risk of worsening urgency
Intradetrusor Botox • Onabotulinum Toxin A • Prevents muscle contraction by inhibiting acetylcholine release at the neuromuscular junction • Initially only approved for Neurogenic detrusor overactivity • Now commonly used in idiopathic OAB • To be covered in BC, patients must have failed 2 previous oral therapies • Significant improvement in daily UUI episodes compared to placebo • Instillation q 6 -9 months cystoscopically • Local anesthetic instillation into bladder prior to procedure • Most patients can tolerate without sedation
Management • Stress Urinary Incontinence • Pelvic Floor Muscle Training • Physio referral • Incontinence pessary • Medication – duloxetine • Surgery • • Urethral bulking agents Midurethral slings – most common Pubovaginal sling Colposuspension
Pelvic Floor Muscle Training • Strengthen pelvic floor musculature • Give the urethra a “backbone” for closure • Reflexively inhibit bladder contractions • Supervised modalities most effective – pelvic floor physiotherapy • Other options • Vaginal weighted cones • Biofeedback – patients can buy apps for their phones!
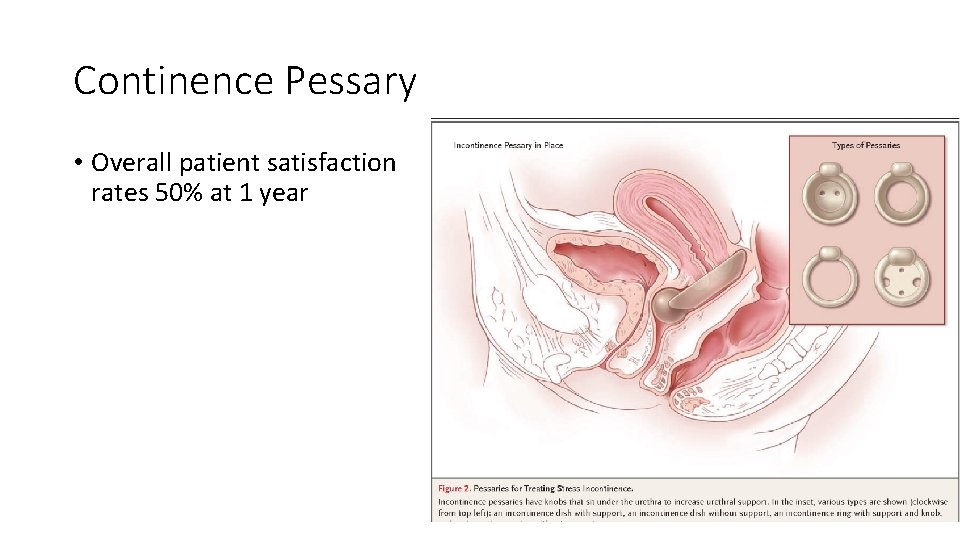
Continence Pessary • Overall patient satisfaction rates 50% at 1 year
Surgical Management of SUI • Urethral bulking agents • Midurethral sling • Fascial Sling • Colposuspension
Surgery • Meta-analysis of 21, 000 women from 175 trials reported SUI cure rates • • 89. 4% fascial sling 89. 1% retropubic MUS 76. 6% open colposuspension 64. 1% transobturator MUS • Several studies report subjective cure rates of 77 -85% at 7, 11, and 17 years with retropubic MUS
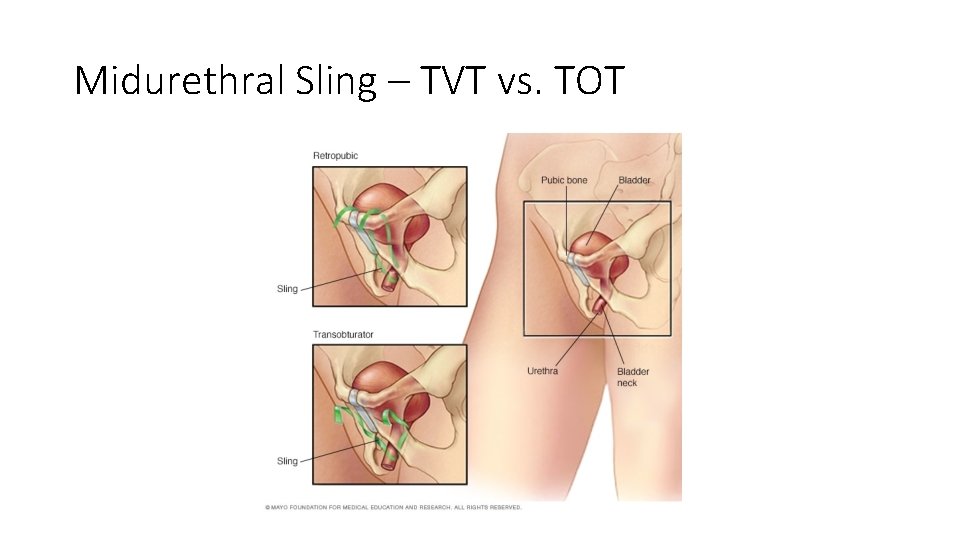
Midurethral Sling – TVT vs. TOT
Male Urinary Incontinence
Learning Objectives • Define male incontinence, and how it differs from female incontinence • Evaluation of male incontinence • Determining the etiology of incontinence • Treatment of BPH and BOO • Treatment of OAB • Management of post void dribble and other male urologic concerns
Clinical Pearls • Male incontinence is the prostate’s fault until proven otherwise • Men are half as likely as women to seek care for their symptoms • Incidence of incontinence is 21% in men >65 • Incidence of overactive bladder is equivalent in men and women
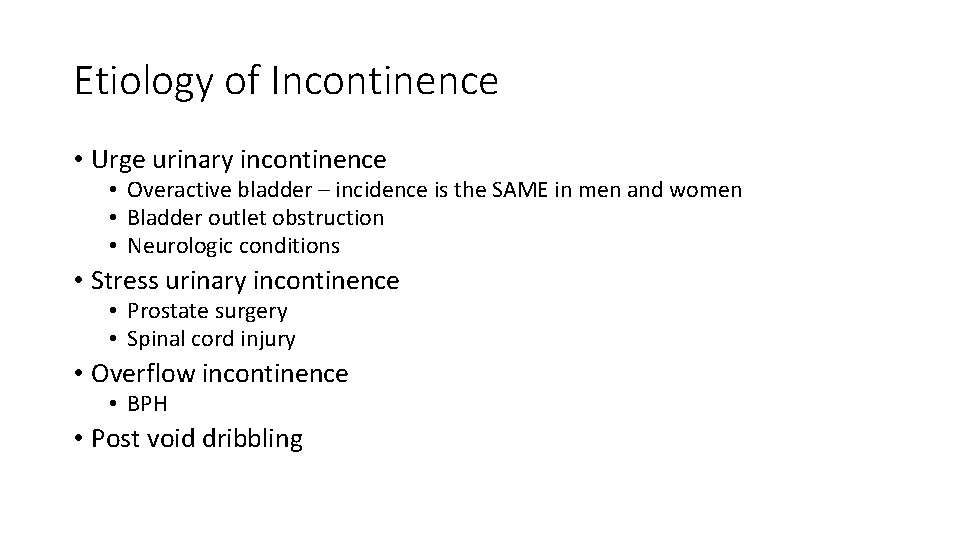
Etiology of Incontinence • Urge urinary incontinence • Overactive bladder – incidence is the SAME in men and women • Bladder outlet obstruction • Neurologic conditions • Stress urinary incontinence • Prostate surgery • Spinal cord injury • Overflow incontinence • BPH • Post void dribbling
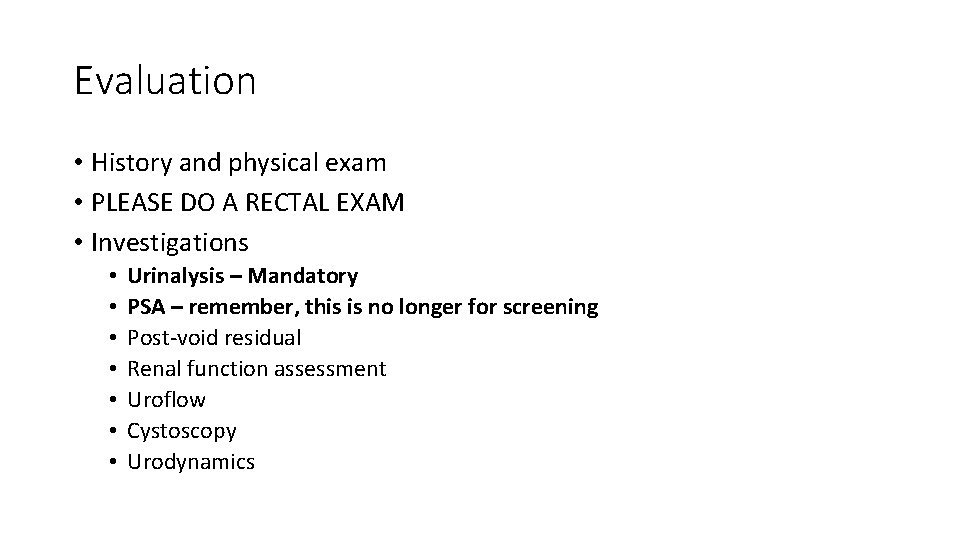
Evaluation • History and physical exam • PLEASE DO A RECTAL EXAM • Investigations • • Urinalysis – Mandatory PSA – remember, this is no longer for screening Post-void residual Renal function assessment Uroflow Cystoscopy Urodynamics
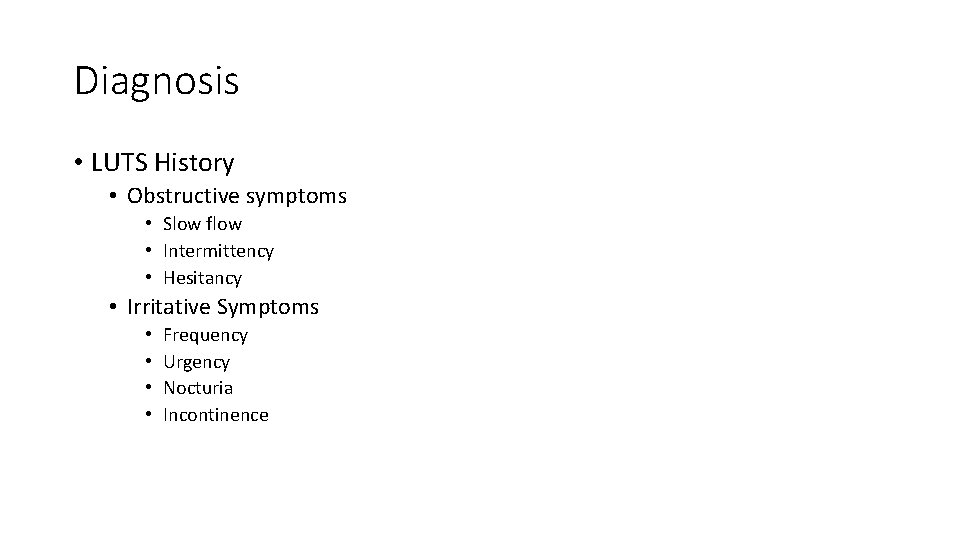
Diagnosis • LUTS History • Obstructive symptoms • Slow flow • Intermittency • Hesitancy • Irritative Symptoms • • Frequency Urgency Nocturia Incontinence
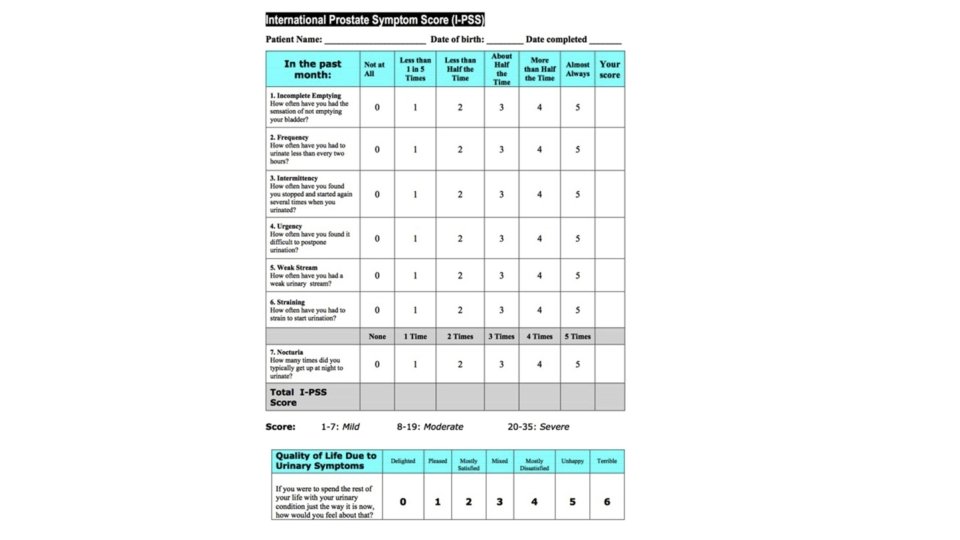
FUNWISE • Frequency • Urgency • Nocturia • Weak stream • Intermittency • Straining • Emptying (incomplete)
1 st Step in Male Incontinence: Define the Problem • Is this a Bladder problem or a prostate problem? • Clues it’s a bladder problem: • • • Young patient Predominantly irritative symptoms Low PSA Small prostate on exam Negligible PVR • Clues it’s a prostate problem: • • • Older patient Many obstructive symptoms as well as irritative symptoms Higher PSA Large prostate on exam Elevated PVR
Benign Prostatic Hypertrophy • Presumptive diagnosis: presence of storage and voiding symptoms in conjunction with an enlarged, nontender, smooth prostate on physical exam • BUT: • Size of the prostate DOES NOT correlate well with symptoms • Other disease presentations can mimic BPH
Beware of BPH Imitators • Men under 40 do not have BPH • Consider other etiologies of LUTS in all men • • Urethral stricture Dysfunctional voiding Bladder neck contracture Prostate cancer UTI Neurogenic bladder Bladder pain syndrome, chronic pelvic pain
If the prostate is the problem… • Treat the prostate • The likely etiology of their incontinence and OAB symptoms is BPH and BOO • Medical therapy is the first step, followed by consideration of surgical management
If the bladder is the problem… • Similar therapies for OAB can be utilized in men • May want to consider these in conjunction with tamsulosin in older gentlemen • Low risk of urinary retention with either anticholinergic or beta 3 agonists, even in men with mild BPH
Management of BPH • Alpha-1 -adrenergic antagonists • Most common therapy for BPH • Typically start with this class as monotherapy and reassess efficacy • 5 -alpha-reductase inhibitors • Consider adding to Alpha blockers in men with a prostate volume > 30 cc, or PSA >1. 5 • More efficacious in men with larger prostates • Phosphodiesterase-5 inhibitions • Daily Cialis 5 mg may be efficacious in patients who can not tolerate one of the above medications • Anticholinergics/B 3 agonists • Risk of urinary retention is highest in elderly men and those with significant BOO (PVR>250 -300 cc)
When to Refer to a Urologist • Men <45 years old • Abnormal DRE • Abnormal PSA • Hematuria • Severe symptoms, or failure of medical therapy • Previous surgical management of urethra or prostate • Urinary retention • Renal dysfunction secondary to BOO
Indications for Surgical Management • Absolute • Urinary retention • Renal dysfunction • Relative • • • Recurrent hematuria secondary to BPH Bladder calculi Recurrent UTIs Symptoms despite medical therapy Patient wishes
Odd Urologic Complaints
Post Void Dribble • History in a male: “After I void, I get a small amount of urine in my underwear" • Typically due to pooling of urine in the bulbar urethra • Trial of pressing on perineum post void • May also be a sign of OAB • If the perineal pressure is not efficacious, may trial medical therapy for OAB
Nocturia (in isolation) • Isolated nocturia (i. e. without daytime symptoms) is typically a medical issue! • Nocturia: a void that is preceded and followed by sleep • Consider nocturnal polyuria (>25 -30% urine volume made at night) • Assessment: voiding diary • Etiologies • Hyperglycemia • Renal dysfunction • Obstructive sleep apnea
The Tip of my Penis Hurts • Bladder fullness/overactivity is referred to the glans penis • Urethral/penile pain is a common symptom of overactive bladder in men
Where’s My Ejaculate? • Retrograde ejaculation is very common with Flomax or other alpha blockers • Occurs 100% of the time after TURP • Reassurance
Questions?
- Slides: 48