Female Genital CuttingMutilation What Clinicians Need to Know





- Slides: 38

Female Genital Cutting/Mutilation: What Clinicians Need to Know Gretchen Heinrichs MD, FACOG, DTMH Assistant Professor OBGYN Denver Health, UCDenver Director of Maternal Health Initiatives, Center for Global Health, Colorado School of Public Health Ranit Mishori, MD, MHS, FAAFP Georgetown University Katherine Stolarz, DO Med. Star Franklin Square Medical Center

Activity Disclaimer ACTIVITY DISCLAIMER It is the policy of the AAFP that all individuals in a position to control content disclose any relationships with commercial interests upon nomination/invitation of participation. Disclosure documents are reviewed for potential conflicts of interest (COI), and if identified, conflicts are resolved prior to confirmation of participation. Only those participants who had no conflict of interest or who agreed to an identified resolution process prior to their participation were involved in this CME activity. Gretchen Heinrichs, MD Ranit Mishori, MD, MHS, FAAFP Katherine Stolarz, DO have indicated they have no relevant financial relationships to disclose. Ranit Mishori, MD, MHS, FAAFP is a paid consultant for Physicians for Human Rights’ Sexual Violence in Conflict Zones program, and has received support from the Josiah Macy Foundation to create educational content for health profession students about refugee health topics. 2
Objectives: • • 3 Describe the prevalence of FGM around the world and in the US Understand the cultural background of the practice Describe the types according to WHO classification Describe acute and long-term effects of FGM Gain a basic understanding of the management of FGM in the pre-, peri- and post-natal period Understand the major controversies and techniques related to deinfibulation and reinfibulation Consider means of communicating about FGM in a gender- and culturesensitive way Gain a basic understanding of the ethical, rights-based and legal issues concerning FGM in the US and around the world
Case 1 • • G. W. underwent Female Genital Mutilation and remembers the event clearly. She states that she was taken by 3 women from her bed in the early morning, held her down and covered her mouth. Another woman came and performed the mutilation procedure, during which she remembers bleeding a lot and having severe pain. She recalls that the pain and bleeding were so severe she could not get out of bed for two weeks. She states that she began to have infections in her urine after the procedure which she experienced as difficulty urinating and pain with urination. She was unable to walk normally for weeks after the mutilation procedure. Currently, she has persistent pain with urination. Intercourse is also extremely painful and she has no desire or enjoyment from it. She lived in fear that because of the procedure she would have infertility and she suffered anxiety during the one year that it took to become pregnant after she began having sex with her husband. The lack of sexual desire, fear of intercourse, and pain have caused some relationship problems with her husband.
Case 2 • 38 yo woman presents 3 years after a vaginal delivery where she was defibulated at delivery and reinfibulated at her request. • She presents for GYN care requesting a more complete reinfibulation, as it was not done to her satisfaction at delivery and she notes an area of redundant vaginal tissue that did not heal properly after delivery and is bothering her, causing itching and rubbing.
Definition • “Female genital mutilation (FGM) comprises all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons. ” World Health Organization 2000, www. who. org
Why is this relevant? • 130 million women have undergone some form of genital mutilation (WHO, 2007) • 2 million procedures are performed every year (WHO, 2007) • 500, 000 women in the USA have undergone FGM or are at risk for the procedure (Population Reference Bureau/CDC survey, 2015) • 1 million African immigrants in the USA • 50, 000 first and second generation African immigrants in Denver area (Denver post 6/2014)
Female Genital Mutilation • Affects 100 -140 Million girls and women worldwide • Girls commonly 4 -15 yo, in some communities as infants; shortly before marriage • Cuts across religions Across socio-economic class • Trends since anti-FGM legislation introduced: – Medicalization of procedure – Younger age at time of En. wikipedia. org, WHO Female Genital Mutilation Fact Sheet, 2011 procedure – Fewer women choosing for daughters
Cultural Context Four main reasons for FGM: 1. Socio-cultural- female maturity(rite of passage), protect the infant at birth, ensures virginity, prerequisite for marriage, preserves cultural identity of a population group through tradition 2. Hygienic/aesthetic- external genitalia are “ugly” and “dirty”, makes a girl beautiful 3. Spiritual- spiritual cleansing, killing the “evil spirit” 4. Psycho-sexual- need to control women’s sexuality, maintain chastity and faithfulness during marriage, increases male pleasure
Procedure • Kidnapped or lured into the ceremony • Often performed by village midwife, “daya” • Use knives, pieces of glass, razors and rocks; no anesthetic • Use thorns, hemp sutures, earth, dung, medicinal salves for hemostasis • Tie the girls thighs together for several weeks to ensure healing
FGC Types I-III
Type IV • Type IV includes different practices of variable severity including pricking, piercing or incision of the clitoris and/or labia; stretching of the clitoris and/or labia; cauterization of the clitoris; and scraping or introduction of corrosive substances into the vagina.
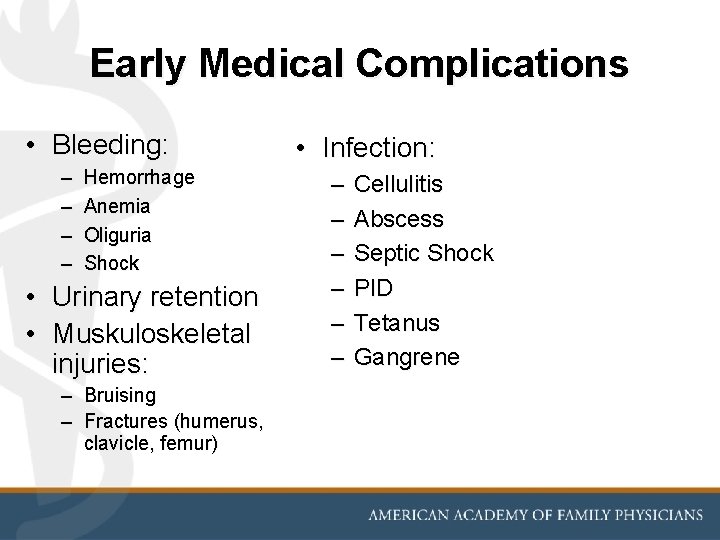
Early Medical Complications • Bleeding: – – Hemorrhage Anemia Oliguria Shock • Urinary retention • Muskuloskeletal injuries: – Bruising – Fractures (humerus, clavicle, femur) • Infection: – – – Cellulitis Abscess Septic Shock PID Tetanus Gangrene
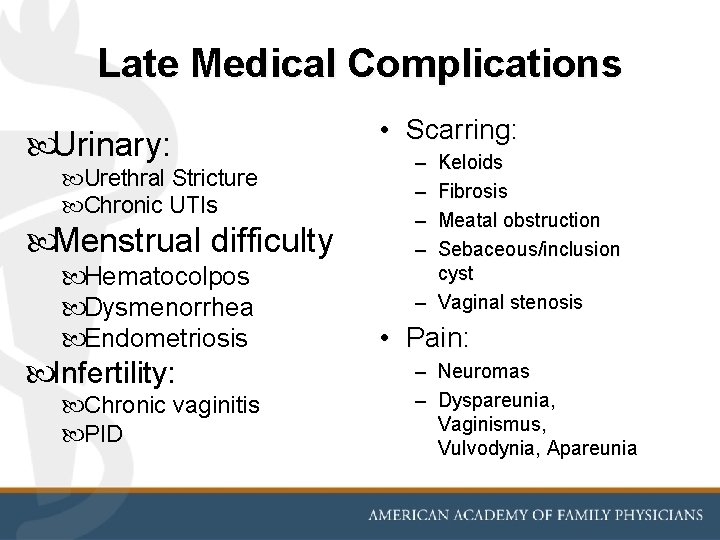
Late Medical Complications Urinary: Urethral Stricture Chronic UTIs Menstrual difficulty Hematocolpos Dysmenorrhea Endometriosis Infertility: Chronic vaginitis PID • Scarring: – – Keloids Fibrosis Meatal obstruction Sebaceous/inclusion cyst – Vaginal stenosis • Pain: – Neuromas – Dyspareunia, Vaginismus, Vulvodynia, Apareunia
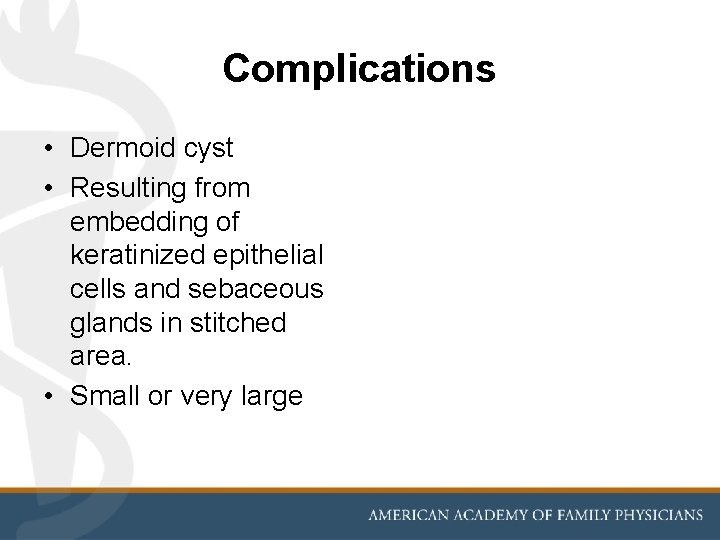
Complications • Dermoid cyst • Resulting from embedding of keratinized epithelial cells and sebaceous glands in stitched area. • Small or very large
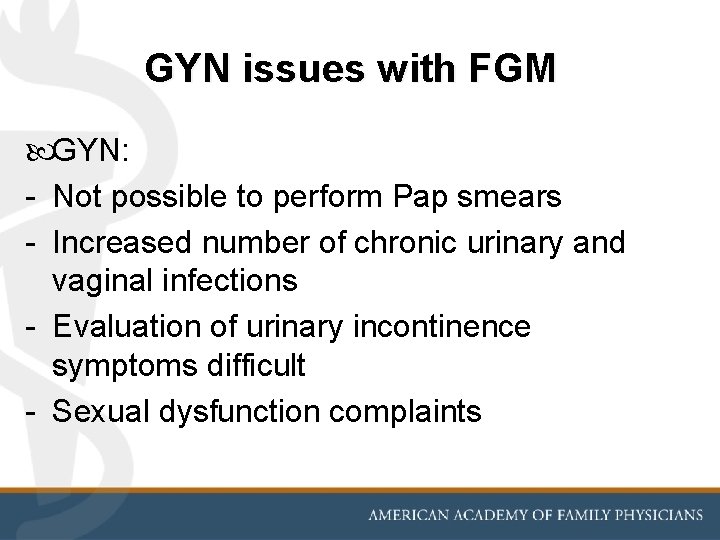
GYN issues with FGM GYN: - Not possible to perform Pap smears - Increased number of chronic urinary and vaginal infections - Evaluation of urinary incontinence symptoms difficult - Sexual dysfunction complaints
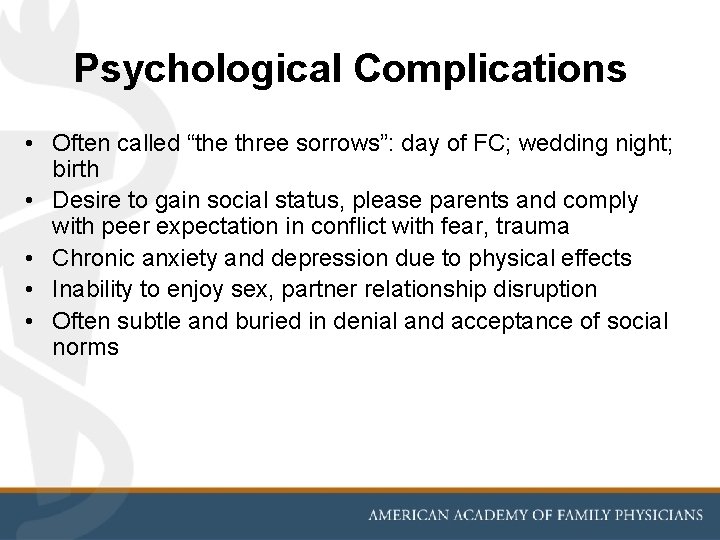
Psychological Complications • Often called “the three sorrows”: day of FC; wedding night; birth • Desire to gain social status, please parents and comply with peer expectation in conflict with fear, trauma • Chronic anxiety and depression due to physical effects • Inability to enjoy sex, partner relationship disruption • Often subtle and buried in denial and acceptance of social norms
Clinical Management - Prenatal • Ask at first prenatal appointment • Use terminology which is culturally respectful and non-judgemental • Document findings and assess clinical needs • Anticipate problems during delivery and discuss plan with patient • Adjust process of Pelvic exam (may be difficult, painful or impossible)
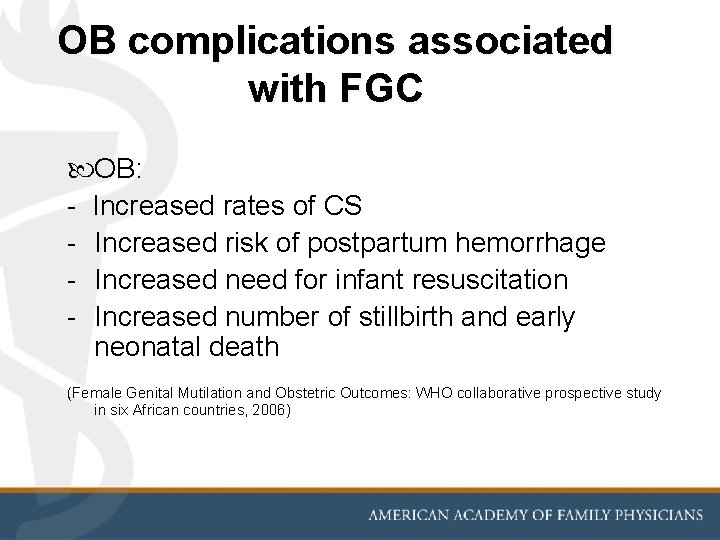
OB complications associated with FGC OB: - Increased rates of CS - Increased risk of postpartum hemorrhage - Increased need for infant resuscitation - Increased number of stillbirth and early neonatal death (Female Genital Mutilation and Obstetric Outcomes: WHO collaborative prospective study in six African countries, 2006)
Defibulation • • Elective procedure May be performed when non-pregnant May be performed after 20 weeks May be performed as part of birth process
Defibulation 21

Defibulation -- Minor Surgical Procedure -- Apply local anesthesia at midline area along original scar line •
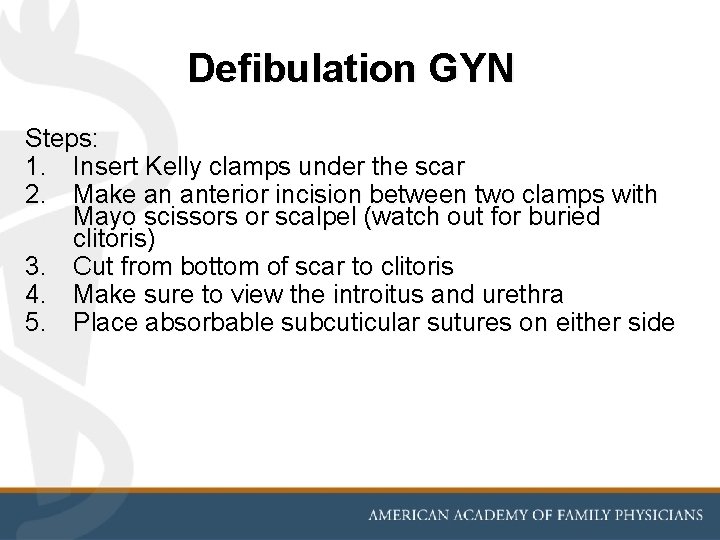
Defibulation GYN Steps: 1. Insert Kelly clamps under the scar 2. Make an anterior incision between two clamps with Mayo scissors or scalpel (watch out for buried clitoris) 3. Cut from bottom of scar to clitoris 4. Make sure to view the introitus and urethra 5. Place absorbable subcuticular sutures on either side
Defibulation procedure OB • Insert 1 or 2 fingers under anterior scar tissue to protect baby’s head and avoid damage to underlying tissue • Use fingers to feel how far up to cut • Aim for anterior episiotomy to extend just above urethral meatus to allow for unobstructed voiding • Mediolateral episiotomy if needed for crowning. 24
Post-Partum • Explain Physiological changes • Voiding - pattern may be faster, stronger stream, noisier • Menstruation – blood loss may appear heavier and more intense, clots • Intercourse – may be less painful, feeling of looseness due to wider introitus • Appearance of genitalia may be altered • Vaginal mucous may appear more copious
Re-infibulation? • • Some women may request it Feel “naked” if area is left open Traditionally performed: raw edges are sewn back together Medically harmful and ethically problematic; possibly illegal in US, UK • Study in the Sudan: 60% of 100 women found to have had “tightening” operations following childbirth. 35% of the women who had not undergone sutured FGM before delivery underwent such surgery in the postnatal period. (African Journal of Midwifery and Women’s Health. 1 (1), pp. 42 -45)
Re-infibulation • RCOG: “Any repair carried out after birth, whether following spontaneous laceration or deliberate defibulation, should be sufficient to appose raw edges and control bleeding, but must not result in a vaginal opening that makes intercourse difficult or impossible. ” 27
Re-infibulation • ACOG: no current guidelines • AAFP: no current guidelines “…the AAFP strongly cautions its members against performing reinfibulation”. http: //www. aafp. org/about/policies/all/genitalmutilation. html 28 • SOGC: no current guidelines [J Obstet Gynaecol Can 2013; 35(11) http: //sogc. org/wpcontent/uploads/2013/10/gui 299 CPG 1311 E. pdf] • FIGO (2010): Reinfibulation is legal at delivery. Published letters condemn practice and asking health community to stop
FGC is a Human Rights Violation • Danger to women’s health. • Since the 1980 s, the practice has increasingly been considered a Human Rights Violation.
Framing as Human Rights Violation • Places responsibility for the practice with governments: have duty to ensure the enjoyment of human rights in their jurisdictions. • Subjecting girls and women to FGM violates a number of rights: right to be free from all forms of gender discrimination, the rights to life and to physical integrity, the right to health, and children’s right to special protections.
Legal Issues • Practice condemned by most Western governments, NGOs, UN agencies – human rights violation • Considered child abuse by UNICEF, most US States • Great social pressure to continue practice even when living outside of native country “vacation cutting”. • Cases reported of daughters sent to home country to get FC; underground practitioners in US • Need to address issue of preventing circumcision of patient’s daughter

Domestic Legal Issues • Federal Prohibition of Female Genital Mutilation Act of 1995: illegal to practice FGM on persons under the age of 18. May result in imprisonment and/or large fines. • 2013 FGM travel provision, ‘Transport for Female Genital Mutilation’: illegal to knowingly transport a girl out of the U. S. for FGM. • Department of Health and Human Services required to compile data on FGM and to educate people on its harmful effects • INS required to pass out information on the effects of and the laws surrounding FGM to any immigrants applying for US visas
Counter Argument • Some have argued that the right to enjoy one’s own culture and to choose one’s own religion should not be subject to government intervention, and that government action to prevent FGM is an intolerable intrusion. • This view is not supported by international Human Rights Laws
Prevention Approaches • Health Risk and Harm • Combine social and economic development with women’s empowerment • Women’s empowerment through educational projects • Alternative Rites of passage ceremonies • “Positive deviant” approach • Social marketing to community leaders (males) • Education of circumcisers
Does not include? : Labiaplasty/Vaginoplasty Gender reassignment surgery Genital modification

Advocacy • UN: International Day of Zero Tolerance for FGM. February 6 th. • Equality Now. http: //www. equalitynow. org/fgm • 28 Too Many. http: //28 toomany. org/ • Tostan 36 http: //www. tostan. org/
Sources World Health Organization, www. who. org United States Health and Human Services Department, www. hhs. gov Dirie, MA, Lindmark, G. The risk of medical complications after female circumcision. East Afr Med J 1992; 69: 479. Skaine, Rosemarie. Female Genital Mutilation- the Legal, Cultural and Medical Issues. Mc. Farland, 2005 • Johsdotter S, Essén, B. Genitals and ethnicity: the politics of gender modifications. Reproductive Health Matters. 2010; 18(35): 29 -37. • World Health Organization. Eliminating female genital mutilation: an interagency statement. Geneva: WHO Department of Reproductive Health and Research. 2008. Nour NM, Michels KB, Bryant AE. Defibulation to Treat Female Genital Cutting: Effect on Symptoms and Sexual Function. Obstetrics and Gynecology. 2006. 108: 55 -60. http: //www. unfpa. org/resources/female-genital-mutilation-fgmfrequently-asked-questions
Sources: • Rosenberg LB, Gibson K, Shulman JF. When Cultures Collide: Female Genital Cutting and U. S. Obstetric Practice. Obstetrics and Gynecology. VOL. 113, NO. 4, APRIL 2009. 931 -4. • Nour, N. Female Genital Cutting: a Persisting Practice. Reviews in Obstetrics and Gynecology. VOL. 1 NO. 3 2008. 135 -9. 38