Feltys Syndrome Sham A Cader Eugeniusz J Kucharz

- Slides: 23
Felty’s Syndrome Sham A. Cader, Eugeniusz J. Kucharz Department Of Internal Medicine and Rheumatology Medical University Of Silesia Katowice - Poland
Felty’s syndrome represents one of many systemic complications of seropositive rheumatoid arthritis.
• In 1924 by A. R Felty described the triad of chronic arthritis, splenomegali and ganulocytopenia
Prevalence • The true prevalence of Felty’s syndrome is unknown, but it may be as high as 3 percent in seropositive rheumatoid arthritis patients. • In the US Felty’s syndrome affects approximately 1 -3% of all patients diagnosed with RA and RA occurs in about 1% of the general population.
Mortality and Morbidity • Although many patients are asymptomatic but others progress and develop life-threatening infections. • Pulmonary and skin infections are common. • One study from the southwest of England observed 32 patients with Felty’s syndrome; 5 died from bronchopneumonia during a mean follow-up period of 5. 2 years. ( Bath Institute for Rheumatic Diseases, UK)
Race • • Felty’s syndrome most often occurs in whites and infrequently occurs in blacks. The human leukocyte antigen DR 4 (HLA-DR 4) genotype, which is a marker for more aggressive RA and more frequent extraarticular manifestations in whites, is strongly associated with Felty’s syndrome. Also appear to be a DQ-linked susceptibility gene and a C 4 B-null allele that increase the risk of Felty’s syndrome. Incidence in women exceeds incidence in men by a ratio of 3: 1.
Pathogenesis • Mechanism for the development of granulocytopenia include accelerated removal of granulocytes from the circulating pool and suppression of granulopoiesis. • Adherence of specific antibodies directed against granulocyte cell surface antigens, ingestion and surface-coating of immune complexes leads to impaired granucyte function and facilitates their removal by the reticularendothelial system.
• Sequestration and margination of granulocytes in the spleen and venules in the lungs and elsewhere results in a diminished circulating pool. • Impaired production is caused by humoral or T cell suppression of myelopoiesis or inhibition of granulocyte growth factor production by cytokines. • A study performed in „Medizinische Universitat zu Lubeck” Germany, patients with Felty’s syndrome have auto antibodies against granulocyte colony-stimulating factor (G-CSF).
Clinical Features • Classic triad Chronic arthritis Active rheumatoid arthritis is present in about 60% patients. ranges from mild involvement to severe deformity and erosion of the joints.
Splenomegaly Firm non tender spleen, ranges from nonpalpable (5 -10% of cases) to massive. There is no correlation between spleen size and the degree of leukopenia also mild hepatomegaly is common. Rare complications: splenic rupture, potal hypertension with esophageal verices.
Leukopenia • Recurrent serious infections in about 60% of patients; most common are skin infections (abscesses, cellulitis, furunculosis) • The degree of leukopenia does not correlate well with number and severity of infections • Granulocytopenia may develop in just weeks and spontaneous remmisions are uncommon
Extra-Articular Manifestations • • Rheumatoid nodules (76%) Weight loss (68%) Sjögren’s Syndrome (56%) Lymphoadenopathy (34%) Leg ulcers (25%) Pleuritis (19%) Skin pigmentation (17%) – pulpable pupura and brownish pigmentary changes of the lower extremities. • Peripheral neuropathy (17%) • Episcleritis (8%)
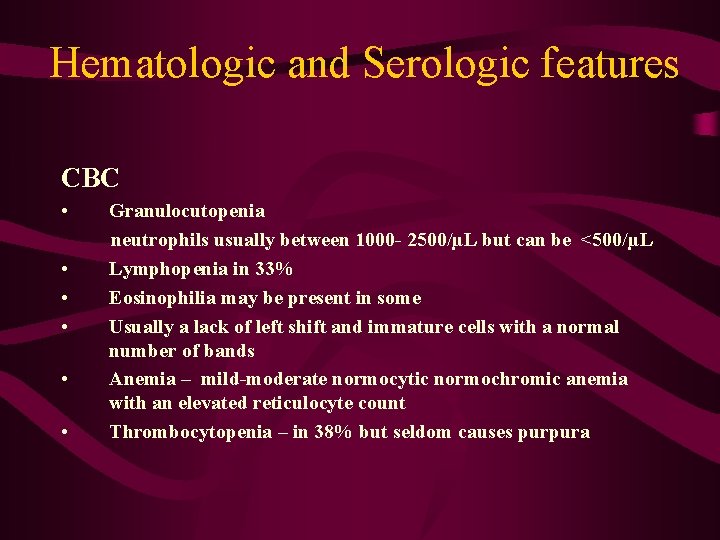
Hematologic and Serologic features CBC • • • Granulocutopenia neutrophils usually between 1000 - 2500/µL but can be <500/µL Lymphopenia in 33% Eosinophilia may be present in some Usually a lack of left shift and immature cells with a normal number of bands Anemia – mild-moderate normocytic normochromic anemia with an elevated reticulocyte count Thrombocytopenia – in 38% but seldom causes purpura
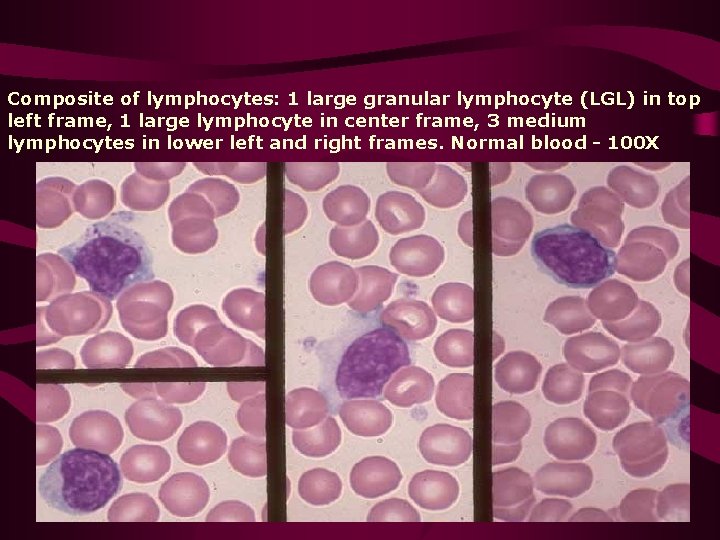
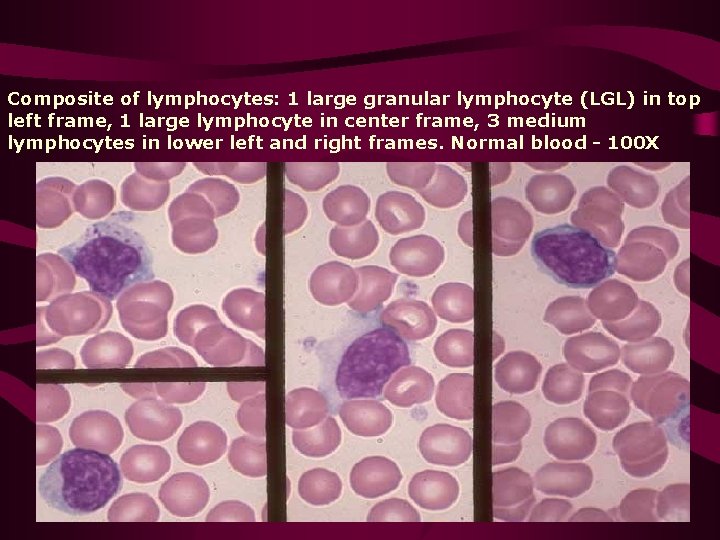
Composite of lymphocytes: 1 large granular lymphocyte (LGL) in top left frame, 1 large lymphocyte in center frame, 3 medium lymphocytes in lower left and right frames. Normal blood - 100 X
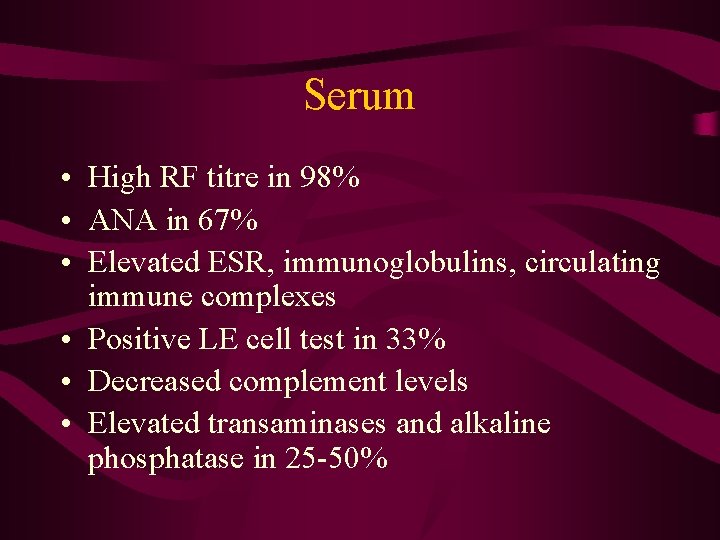
Serum • High RF titre in 98% • ANA in 67% • Elevated ESR, immunoglobulins, circulating immune complexes • Positive LE cell test in 33% • Decreased complement levels • Elevated transaminases and alkaline phosphatase in 25 -50%
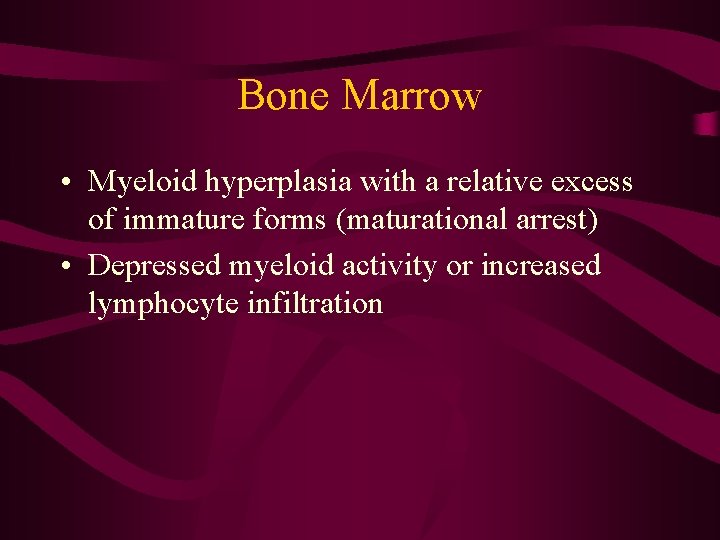
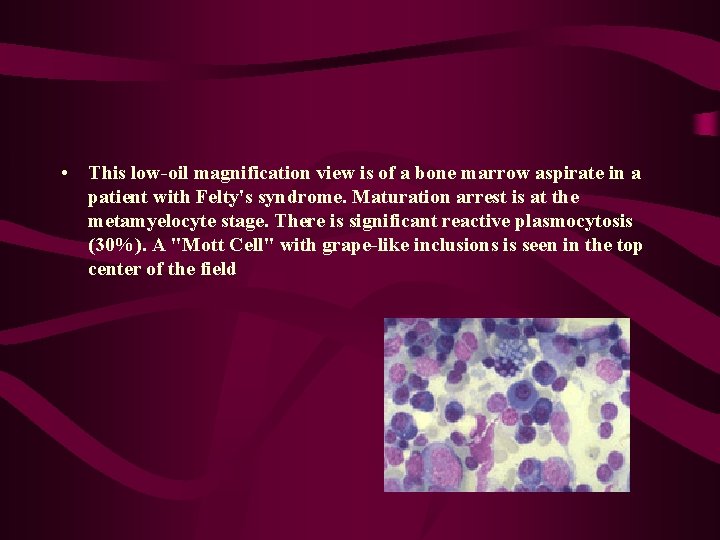
Bone Marrow • Myeloid hyperplasia with a relative excess of immature forms (maturational arrest) • Depressed myeloid activity or increased lymphocyte infiltration
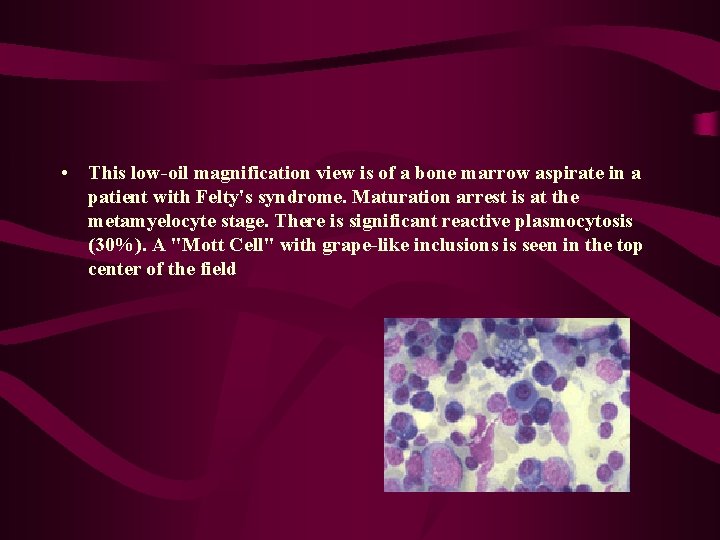
• This low-oil magnification view is of a bone marrow aspirate in a patient with Felty's syndrome. Maturation arrest is at the metamyelocyte stage. There is significant reactive plasmocytosis (30%). A "Mott Cell" with grape-like inclusions is seen in the top center of the field
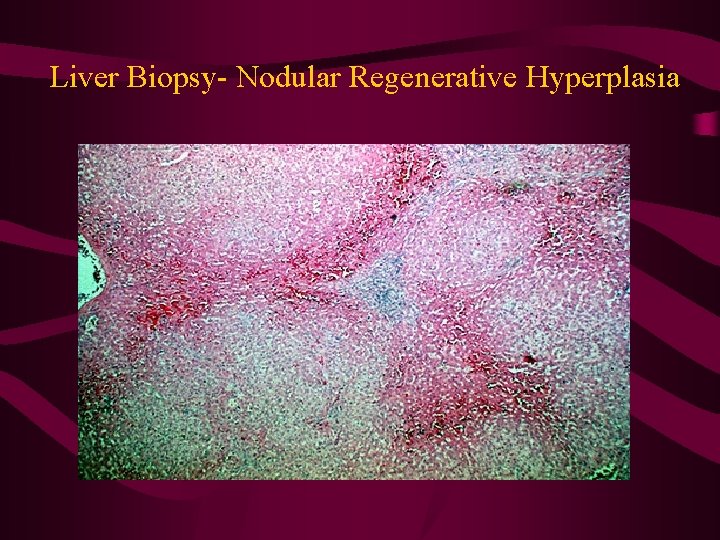
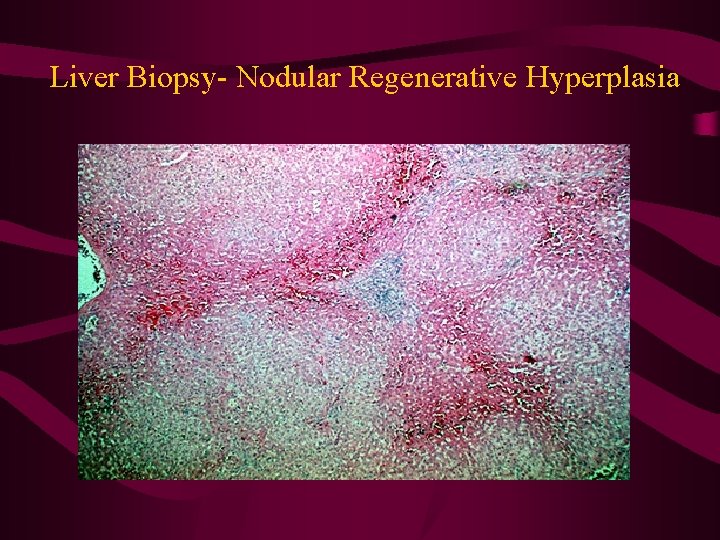
Liver Biopsy- Nodular Regenerative Hyperplasia
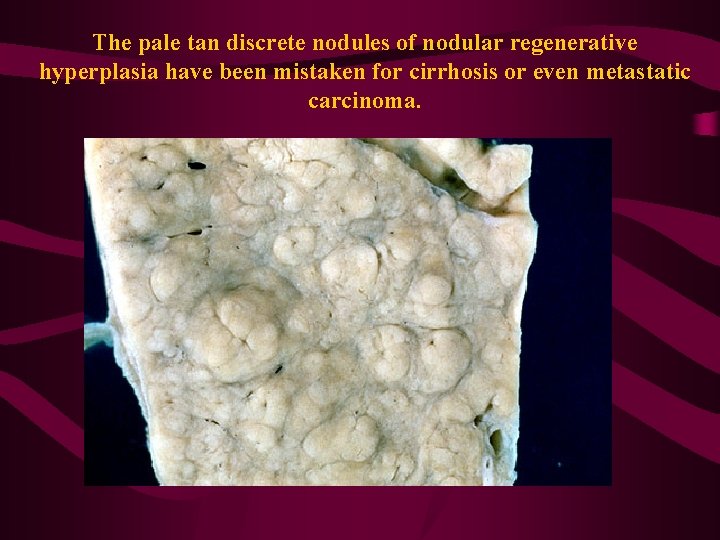
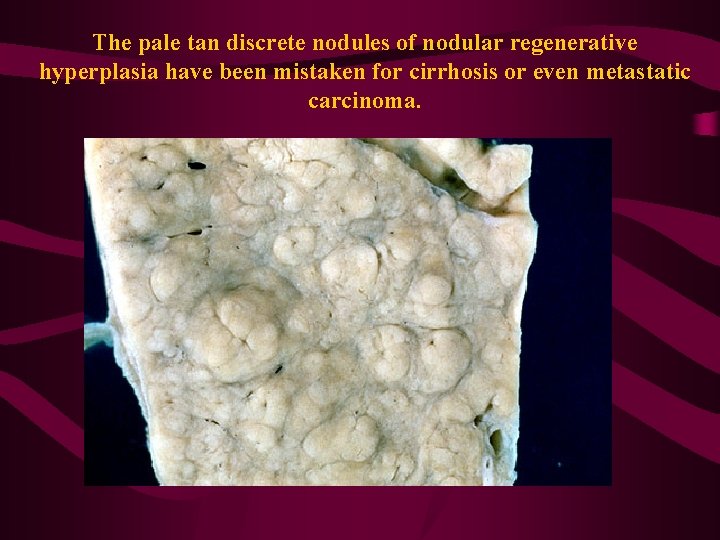
The pale tan discrete nodules of nodular regenerative hyperplasia have been mistaken for cirrhosis or even metastatic carcinoma.

Nodular sinusoidal lymphocytes in Felty’s syndrome • Image donated by: Professor Ian Lauder Donor organization: Leicester University, Department of Pathology
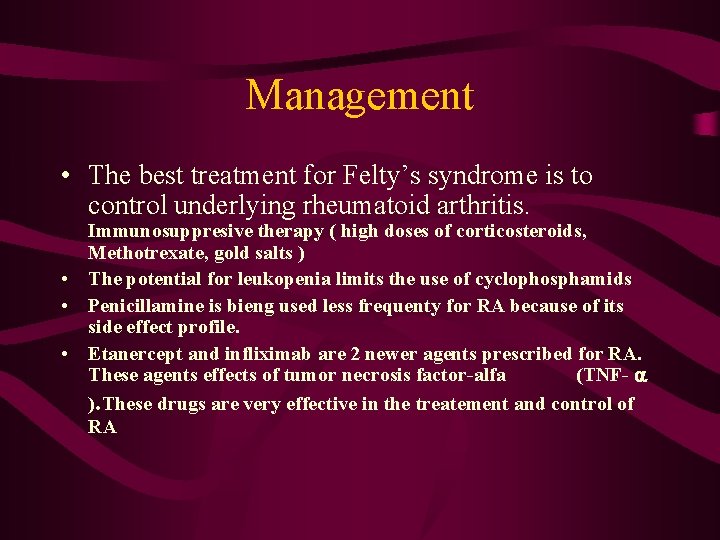
Management • The best treatment for Felty’s syndrome is to control underlying rheumatoid arthritis. Immunosuppresive therapy ( high doses of corticosteroids, Methotrexate, gold salts ) • The potential for leukopenia limits the use of cyclophosphamids • Penicillamine is bieng used less frequenty for RA because of its side effect profile. • Etanercept and infliximab are 2 newer agents prescribed for RA. These agents effects of tumor necrosis factor-alfa (TNF- ). These drugs are very effective in the treatement and control of RA
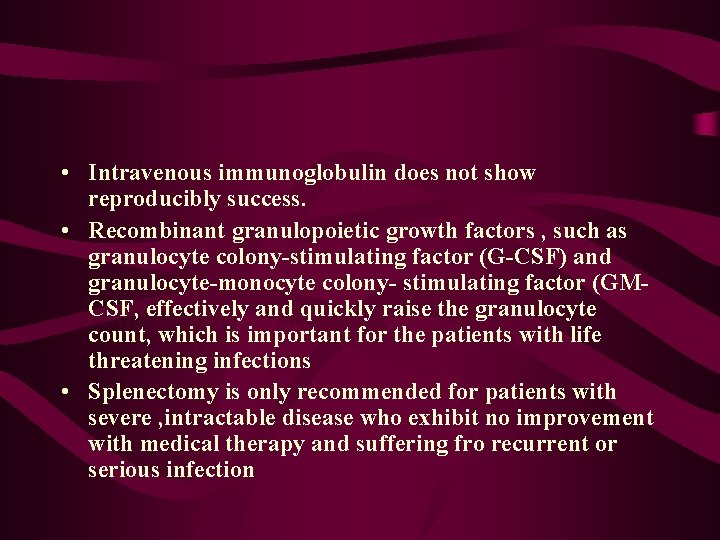
• Intravenous immunoglobulin does not show reproducibly success. • Recombinant granulopoietic growth factors , such as granulocyte colony-stimulating factor (G-CSF) and granulocyte-monocyte colony- stimulating factor (GMCSF, effectively and quickly raise the granulocyte count, which is important for the patients with life threatening infections • Splenectomy is only recommended for patients with severe , intractable disease who exhibit no improvement with medical therapy and suffering fro recurrent or serious infection
• Though Felty’s syndrome appears to be rare in rheumatoid arthritis patients, a proper complete diagnosis should be done in all RA patients and proper control of the RA.