Fatigue weakness and spasticity in MS a selfmanagement





- Slides: 24
Fatigue, weakness and spasticity in MS… a self-management challenge! Thomas R. Holtackers, PT 1
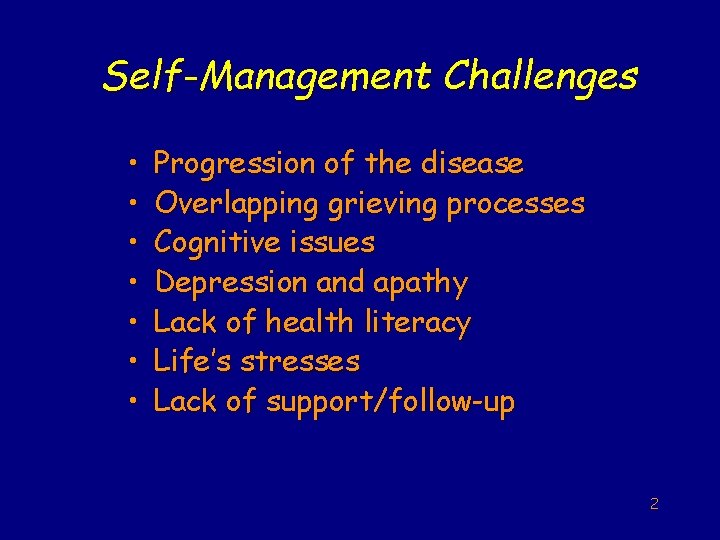
Self-Management Challenges • • Progression of the disease Overlapping grieving processes Cognitive issues Depression and apathy Lack of health literacy Life’s stresses Lack of support/follow-up 2
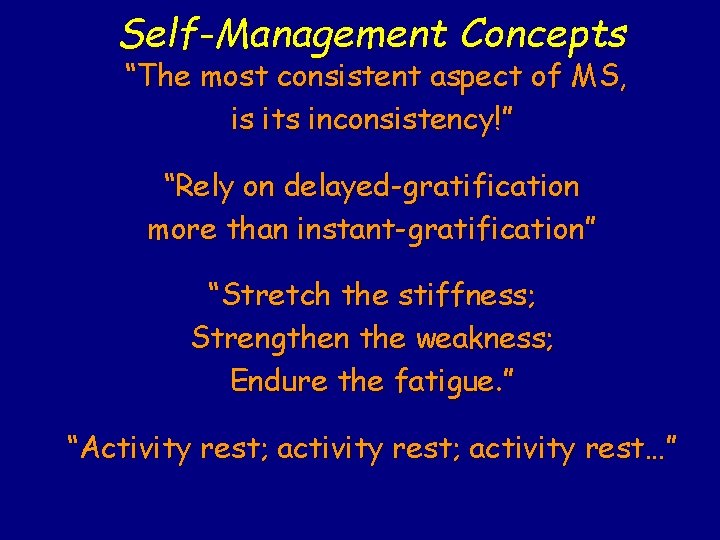
Self-Management Concepts “The most consistent aspect of MS, is its inconsistency!” “Rely on delayed-gratification more than instant-gratification” “Stretch the stiffness; Strengthen the weakness; Endure the fatigue. ” “Activity rest; activity rest…”
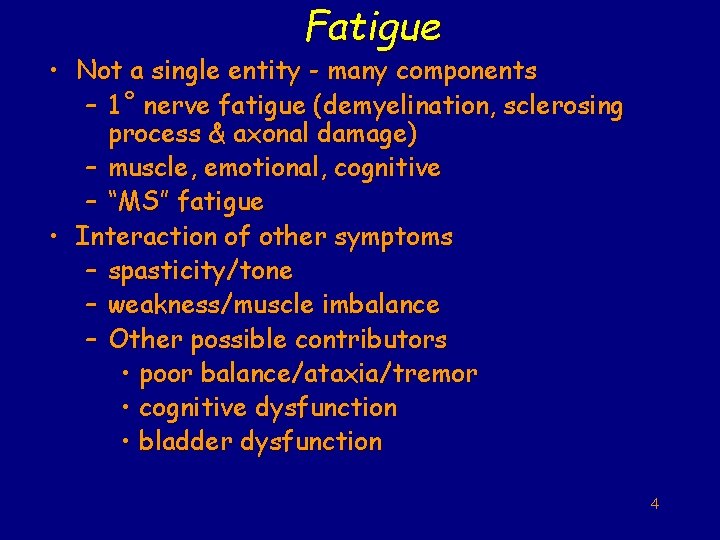
Fatigue • Not a single entity - many components – 1 ˚ nerve fatigue (demyelination, sclerosing process & axonal damage) – muscle, emotional, cognitive – “MS” fatigue • Interaction of other symptoms – spasticity/tone – weakness/muscle imbalance – Other possible contributors • poor balance/ataxia/tremor • cognitive dysfunction • bladder dysfunction 4
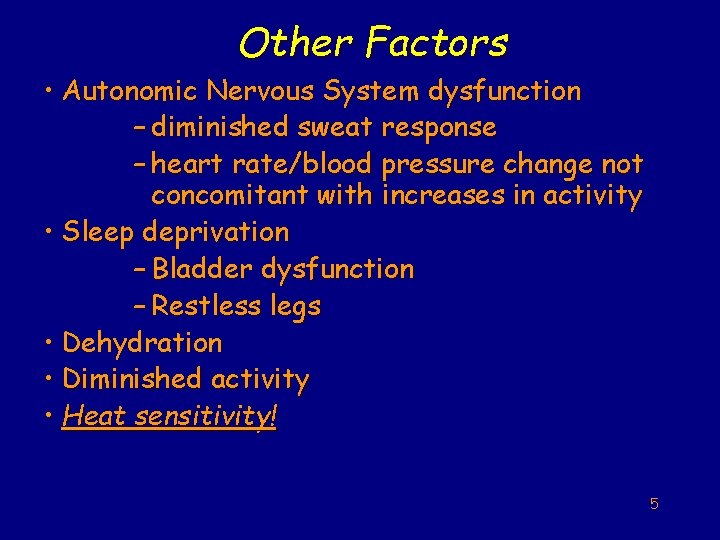
Other Factors • Autonomic Nervous System dysfunction – diminished sweat response – heart rate/blood pressure change not concomitant with increases in activity • Sleep deprivation – Bladder dysfunction – Restless legs • Dehydration • Diminished activity • Heat sensitivity! 5
Variables of Increased Core Body Temperature • • Activity/exercise Ambient temperature/humidity Poor sweat response “Diurnal” temperature change Temperature of food/drink Radiant energy/direct sunlight Heavy/warm clothing Thermogenesis of digestion 6
Fatigue Management • • • Managing other symptoms Practice heat sensitivity management skills Sleep management Practicing good nutritional habits Use of adaptive equipment Prioritizing energy expenditure – Pacing activities – Finding a balance between exercise, activity and inactivity – Adopting the concept of… activity, rest; etc 7

Spasticity/Tone • Spasticity is velocity related • Postural tone • Mild to severe • Often co-exists with weakness • More apparent in the lower extremities

• • Spasticity/Tone Negative Consequences • May interfere with: Pain/discomfort - ADL’s Contractures - hygiene energy-cost -bowel/bladder sheer forces - sexual activity skin breakdown - gait/transfers safety - general mobility work for caregiver - posture - sleep - breathing 9
Spasticity/Tone Positive Consequences • Possible advantages of spasticity – Good vs. bad spasticity – Maintains muscle tone/bulk – Helps support circulatory function – May prevent formation of deep vein thrombosis – May assist with postural control – May assist in activities of daily living, i. e. transfers, dressing, gait 10

Spasticity/Tone Management • Stretching (primary) - intensity} moderate - duration} short - repetition} many - frequency} often 11
• • Positioning/change in position Activity (“motion is lotion”) Strengthen antagonist muscle groups Other considerations: – rotatory trunk movements – reciprocal movements – vibration – topical heat vs cold – reciprocating electrical stimulation 12

Spasticity/Tone Medical Management • Medical intervention – Baclofen – Zanaflex/valium/catapres – Baclofen pump – Botox injections – Nerve blocks • Surgical intervention – Neurotomy – Tendinotomy 13
Weakness • Primary (organic) – – Due to MS plaques in the CNS results in physiological muscle fatigue, paresis, or paralysis • Secondary – 2º disuse, deconditioning, compensatory movements, pain, contractures, proprioceptive loss, tendonitis, etc. – 2º spasticity & fatigue 14
Weakness Management • Primary weakness - Strengthening exercise to maintain - Be aware of overuse - May require compensatory intervention (mobility aids, electrical stimulation, bracing, etc. ) 15
• Secondary weakness - Often overlooked - May be minimized with early intervention - emphasize posture/stability - correct compensatory gait - reduce lifestyle risk factors - incorporate energy management strategies 16
Weakness Management • Strengthening exercises - Positioning to reduce effects of tone & spasticity - Isometric vs Isotonic - Functional antigravity muscle groups - “Core” groups - Quality of repetitions - Relaxation between reps - Number of repetitions - Speed of contractions 17
Treatment Considerations Lower Extremity FWS Functional considerations • Gait/standing/transfers • Wheelchair/sitting posture to help reduce extensor/flexor/adductor tone • Bed positioning to help reduce same • Driving: gassing/braking 18
• Ankle/Foot Weak dorsiflexion vs. strong, spastic plantar flexion vs. extensor tone • Stretch ankle into dorsiflexion • Strengthen anterior tib with knee flexed • Strengthen anterior tib with knee in extension • If a walker, consider rocker bottom shoe; use the toe test • Consider extensor tone during gait on ankle/knee/hip synergy • AFO to help prevent foot drop; consider weight increase/influence on hip flexion; disuse atrophy • FES of anterior tib; consider over stimulation/fatigue/spasticity; disuse atrophy 19
Knee • Quadriceps/hamstring strength/spasticity inequities vs. extensor/flexor tone • Stretch and strengthen both • Consider stretch of antagonist prior to strengthening agonist • Position to reduce tone • When strengthening use a circuit of alternating between knee extension and knee flexion 20
Hip • Hip flexor/extensor imbalance – Stretch and strengthen – Positioning/posture considerations • Hip abductor/adductor imbalance – Stretch and strengthen – Positioning/posture considerations • Trunk instability/“core” weakness – Get “on the ball” – Pilates concepts 21
Other Considerations • Asymmetry of weakness/spasticity • Increased work of mobility with gait aids; cane, crutches, walkers • Wheelchair use • Other MS symptoms - pain, tremor, sensory dysfunction, central ataxia, cognitive dysfunction, emotional dysfunction • Other diseases: Cardiopulmonary/vascular, arthritis, etc 22
Conclusions • Fatigue, weakness and spasticity (FWS) are common symptoms of MS • FWS are manageable through physical and medical interventions • Self-management of FWS is challenging and requires effort, consistency and support 23

MS Society Resources • For professionals 1 -866 -MS-TREAT • www. nationalmssociety. org/PRC. asp • Healthprof_info@nmss. org (bulletin) • For clients 1 -800 FIGHTMS 24