Fang Luo M D Associate Professor Department of
- Slides: 53
Fang Luo M. D. Associate Professor Department of Anesthesiology 2 nd clinical college Tongji Medical college luofang 0909@hotmail. com
Key points Introduction of Anesthesia Anesthetics General anesthesia Local anesthesia Special technique Deliberate hypotension Hypothermia Cardio-pulmonary Bypass
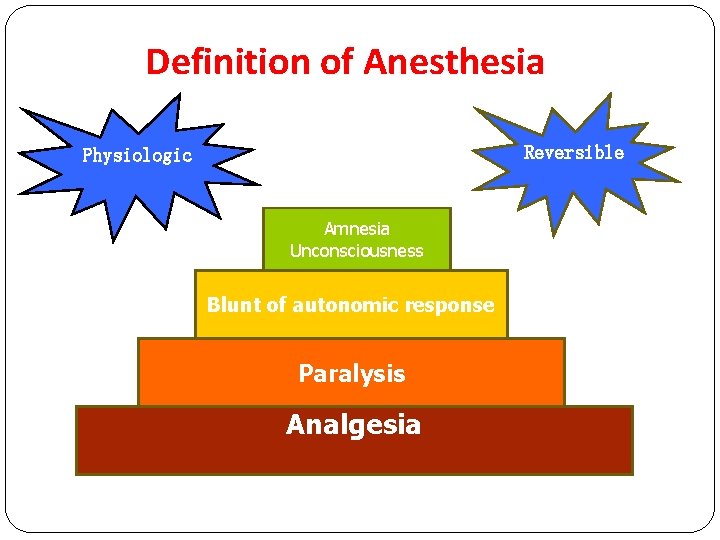
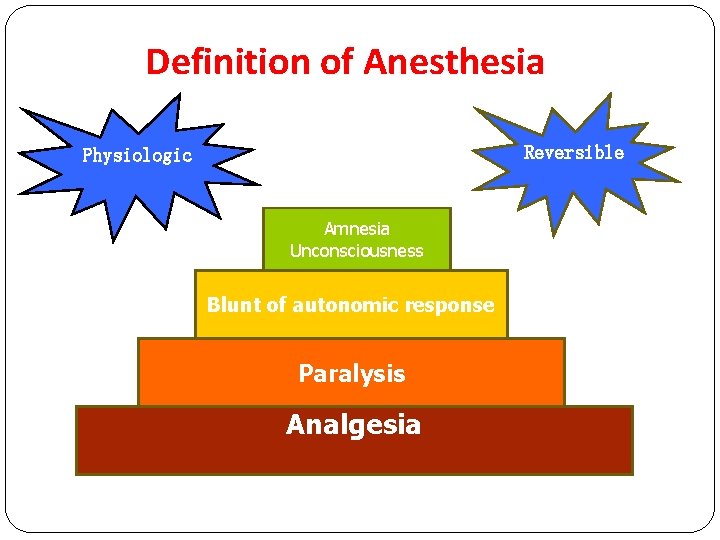
Definition of Anesthesia Reversible Physiologic Amnesia Unconsciousness Blunt of autonomic response Paralysis Analgesia
Anesthesiology p Clinical anesthesia p Pain clinic p Intensive Care p Resuscitation p Clinical and laboratory research
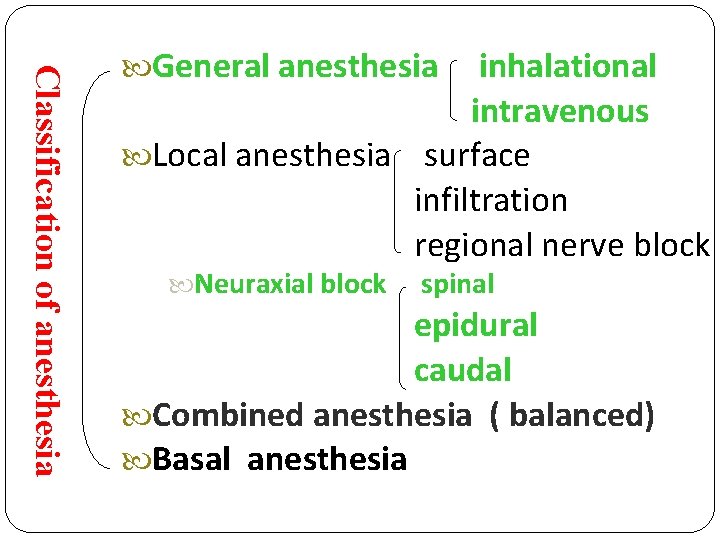
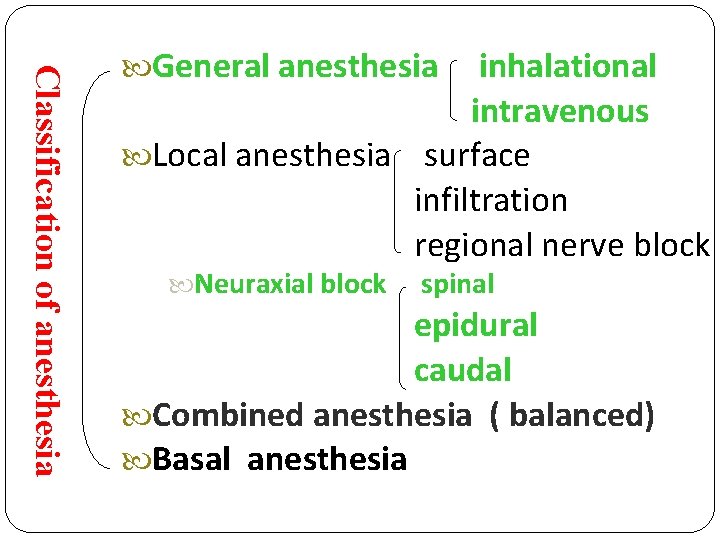
Classification of anesthesia General anesthesia inhalational intravenous Local anesthesia surface infiltration regional nerve block Neuraxial block spinal epidural caudal Combined anesthesia ( balanced) Basal anesthesia
preoperative evaluations
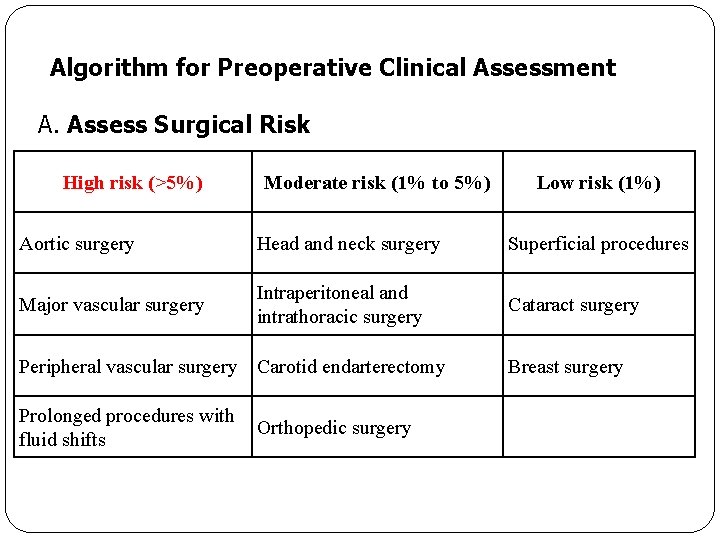
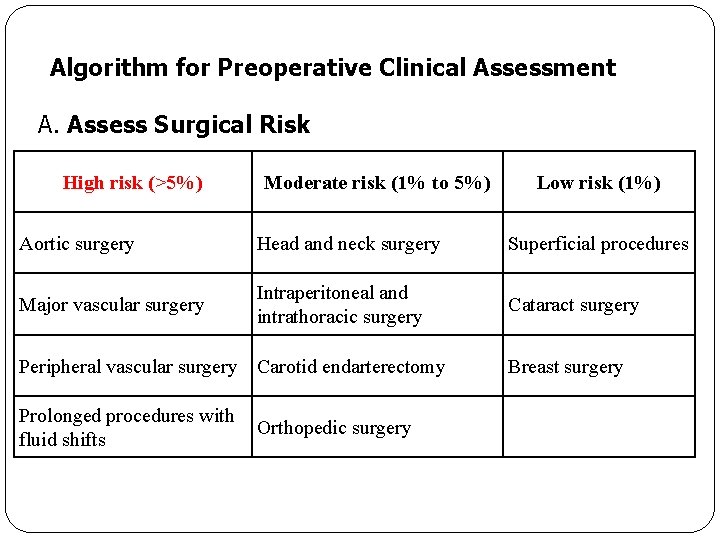
Algorithm for Preoperative Clinical Assessment A. Assess Surgical Risk High risk (>5%) Moderate risk (1% to 5%) Low risk (1%) Aortic surgery Head and neck surgery Superficial procedures Major vascular surgery Intraperitoneal and intrathoracic surgery Cataract surgery Peripheral vascular surgery Carotid endarterectomy Prolonged procedures with Orthopedic surgery fluid shifts Breast surgery
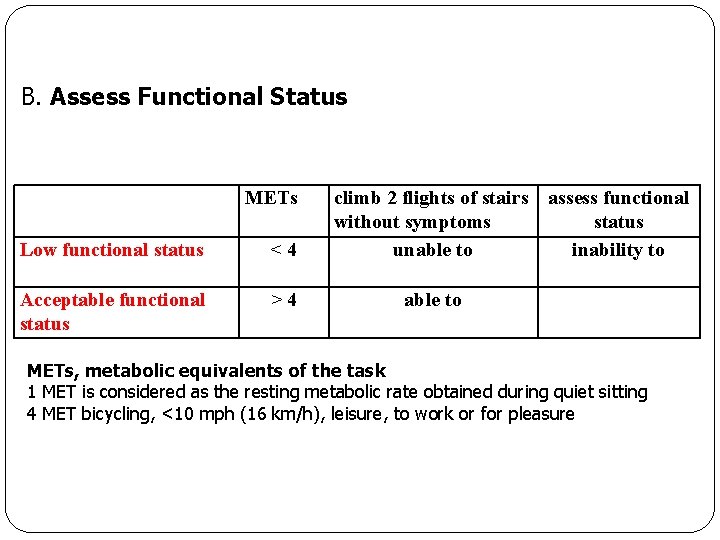
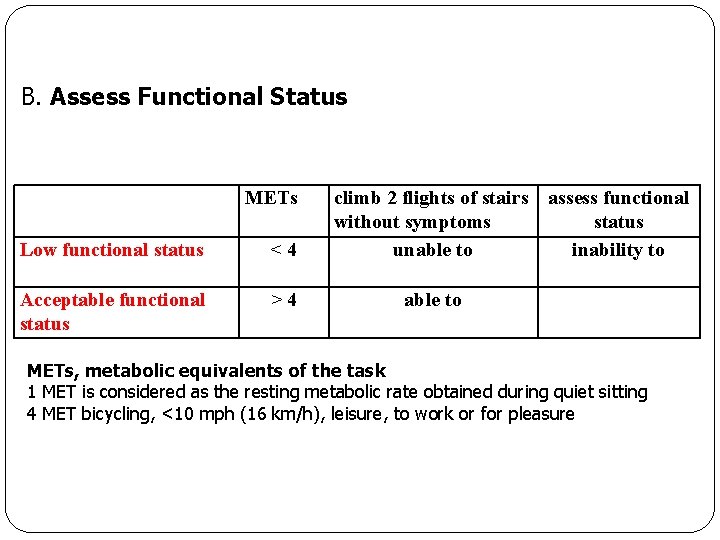
B. Assess Functional Status METs Low functional status <4 Acceptable functional status >4 climb 2 flights of stairs assess functional without symptoms status unable to inability to able to METs, metabolic equivalents of the task 1 MET is considered as the resting metabolic rate obtained during quiet sitting 4 MET bicycling, <10 mph (16 km/h), leisure, to work or for pleasure
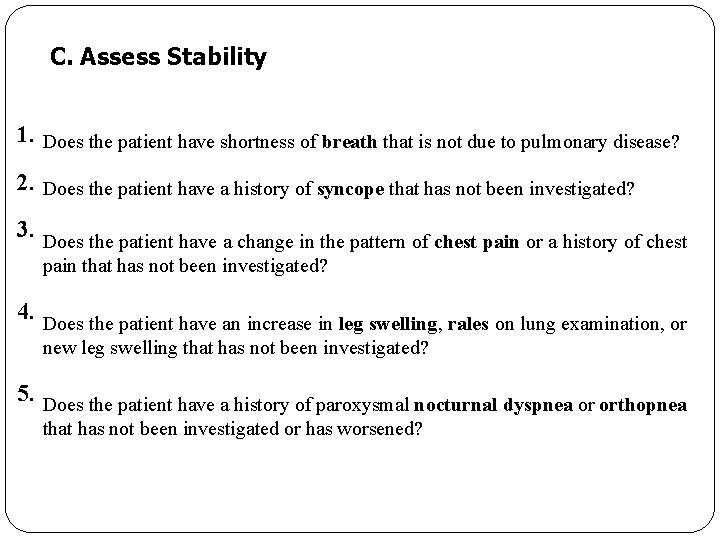
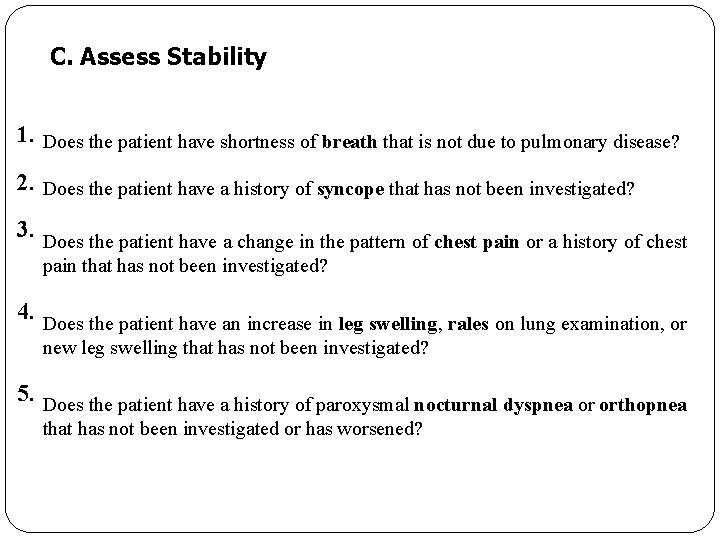
C. Assess Stability 1. Does the patient have shortness of breath that is not due to pulmonary disease? 2. Does the patient have a history of syncope that has not been investigated? 3. Does the patient have a change in the pattern of chest pain or a history of chest pain that has not been investigated? 4. Does the patient have an increase in leg swelling, rales on lung examination, or new leg swelling that has not been investigated? 5. Does the patient have a history of paroxysmal nocturnal dyspnea or orthopnea that has not been investigated or has worsened?
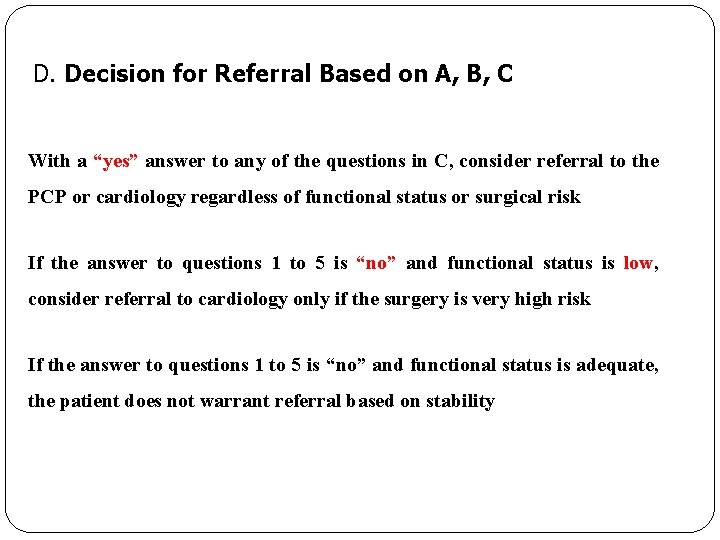
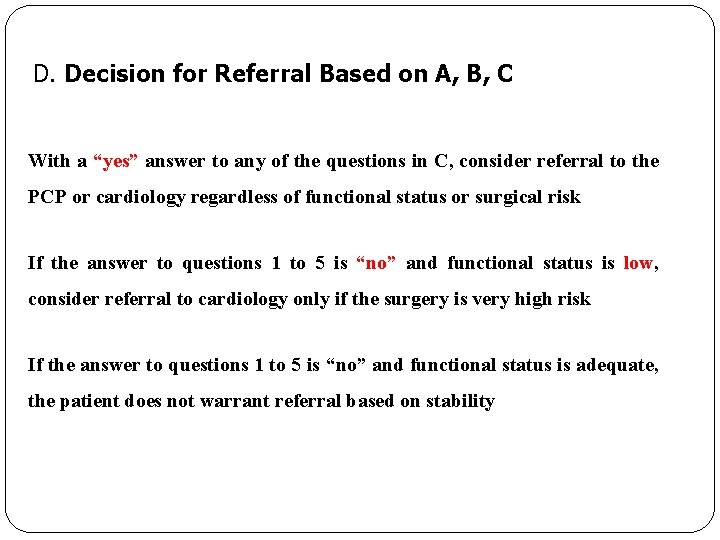
D. Decision for Referral Based on A, B, C With a “yes” answer to any of the questions in C, consider referral to the PCP or cardiology regardless of functional status or surgical risk If the answer to questions 1 to 5 is “no” and functional status is low, consider referral to cardiology only if the surgery is very high risk If the answer to questions 1 to 5 is “no” and functional status is adequate, the patient does not warrant referral based on stability
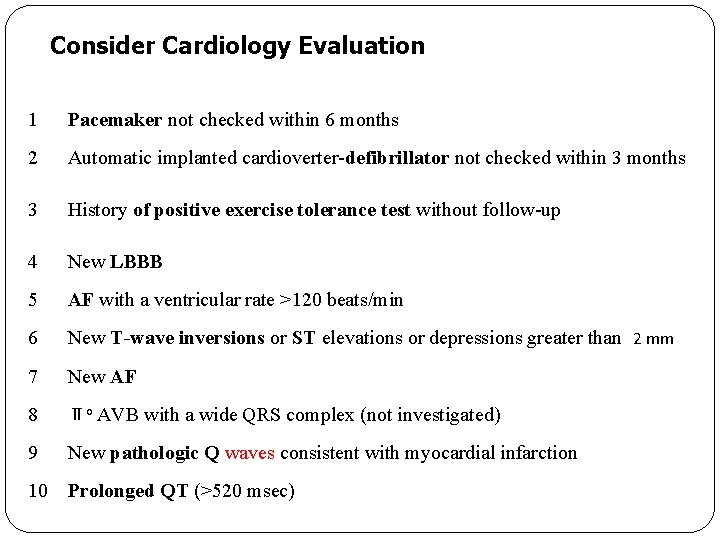
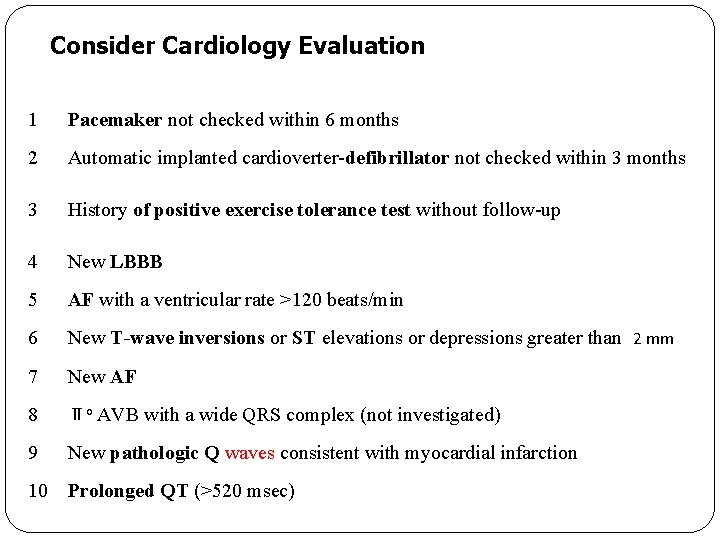
Consider Cardiology Evaluation 1 Pacemaker not checked within 6 months 2 Automatic implanted cardioverter-defibrillator not checked within 3 months 3 History of positive exercise tolerance test without follow-up 4 New LBBB 5 AF with a ventricular rate >120 beats/min 6 New T-wave inversions or ST elevations or depressions greater than 2 mm 7 New AF 8 Ⅱo AVB with a wide QRS complex (not investigated) 9 New pathologic Q waves consistent with myocardial infarction 10 Prolonged QT (>520 msec)
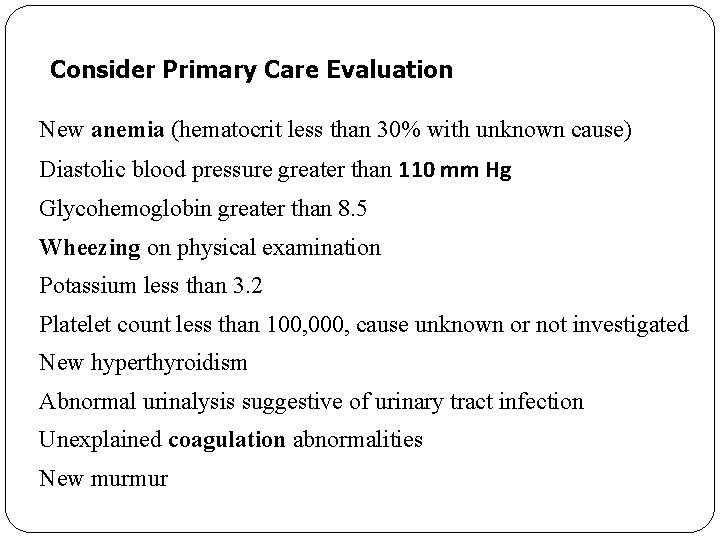
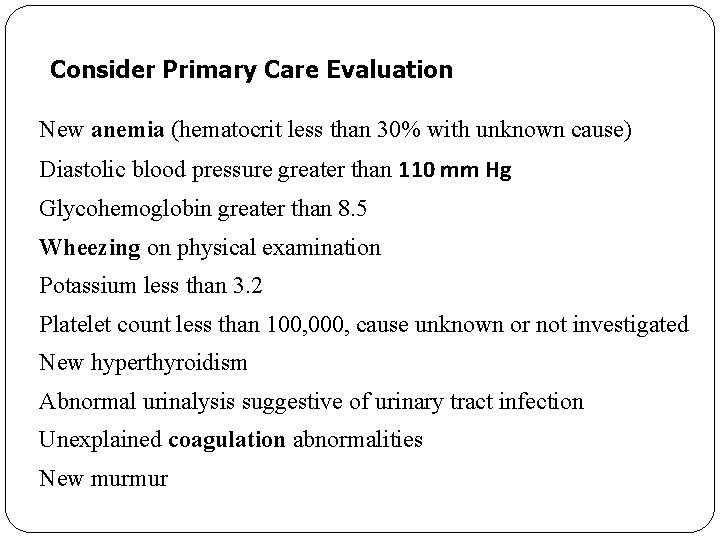
Consider Primary Care Evaluation New anemia (hematocrit less than 30% with unknown cause) Diastolic blood pressure greater than 110 mm Hg Glycohemoglobin greater than 8. 5 Wheezing on physical examination Potassium less than 3. 2 Platelet count less than 100, 000, cause unknown or not investigated New hyperthyroidism Abnormal urinalysis suggestive of urinary tract infection Unexplained coagulation abnormalities New murmur
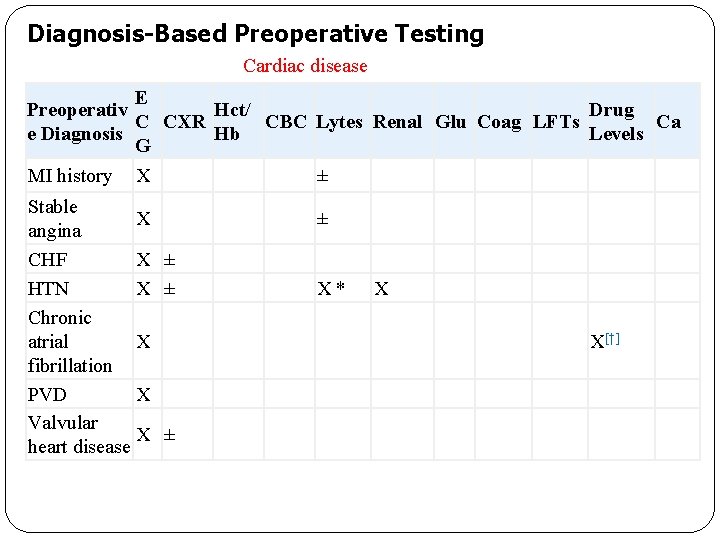
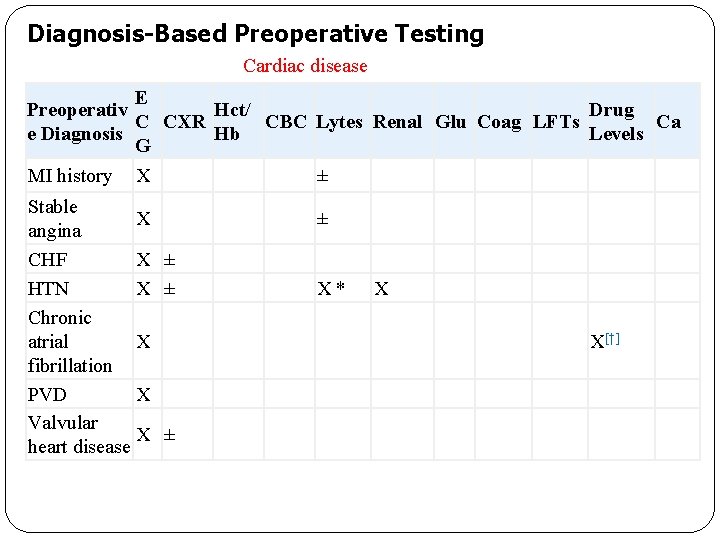
Diagnosis-Based Preoperative Testing Cardiac disease E Preoperativ Hct/ Drug CBC Lytes Renal Glu Coag LFTs Ca C CXR e Diagnosis Hb Levels G MI history X Stable X angina CHF X ± HTN X ± Chronic X atrial fibrillation PVD X Valvular X ± heart disease ± ± X * X X[†]
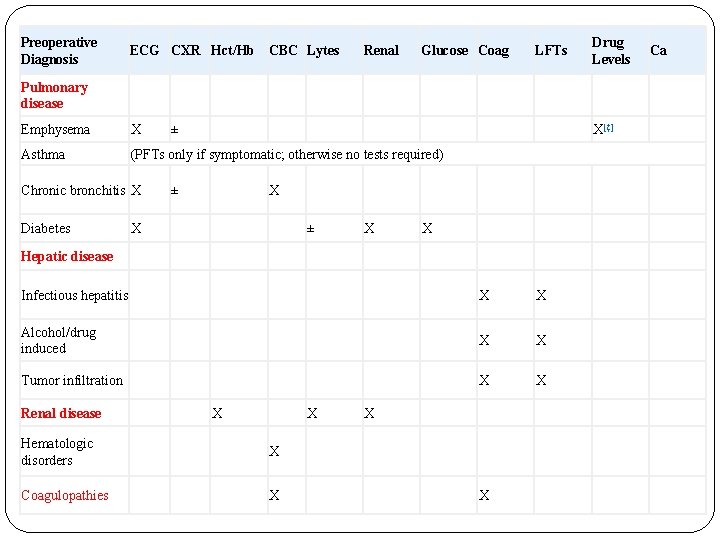
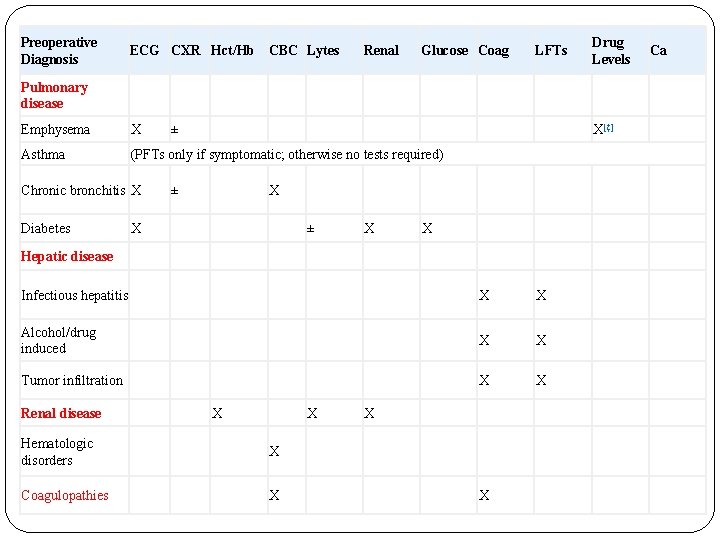
Preoperative Diagnosis ECG CXR Hct/Hb CBC Lytes Renal Glucose Coag LFTs Drug Levels Pulmonary disease Emphysema X Asthma (PFTs only if symptomatic; otherwise no tests required) Chronic bronchitis X Diabetes ± X[‡] ± X X Hepatic disease Infectious hepatitis X X Alcohol/drug induced X X Tumor infiltration X X Renal disease X X Hematologic disorders X Coagulopathies X X X Ca
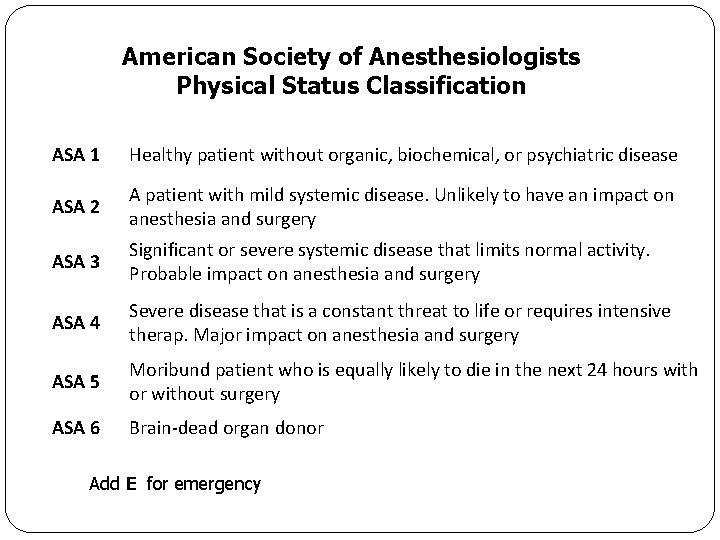
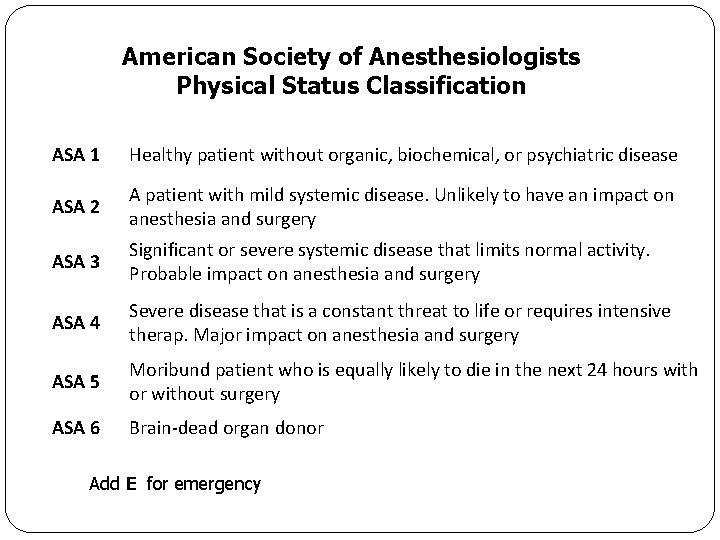
American Society of Anesthesiologists Physical Status Classification ASA 1 Healthy patient without organic, biochemical, or psychiatric disease ASA 2 A patient with mild systemic disease. Unlikely to have an impact on anesthesia and surgery ASA 3 Significant or severe systemic disease that limits normal activity. Probable impact on anesthesia and surgery ASA 4 Severe disease that is a constant threat to life or requires intensive therap. Major impact on anesthesia and surgery ASA 5 Moribund patient who is equally likely to die in the next 24 hours with or without surgery ASA 6 Brain-dead organ donor Add E for emergency
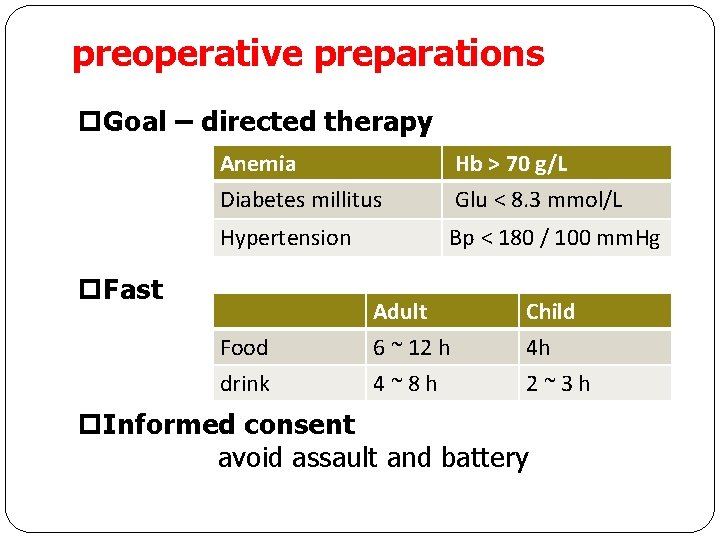
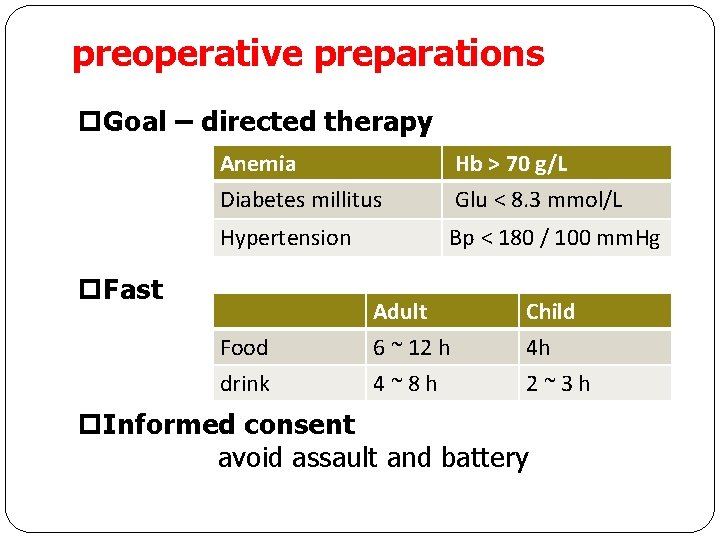
preoperative preparations p. Goal – directed therapy Anemia Diabetes millitus Hb > 70 g/L Glu < 8. 3 mmol/L Hypertension Bp < 180 / 100 mm. Hg p. Fast Food drink Adult 6 ~ 12 h 4~8 h Child 4 h 2~3 h p. Informed consent avoid assault and battery
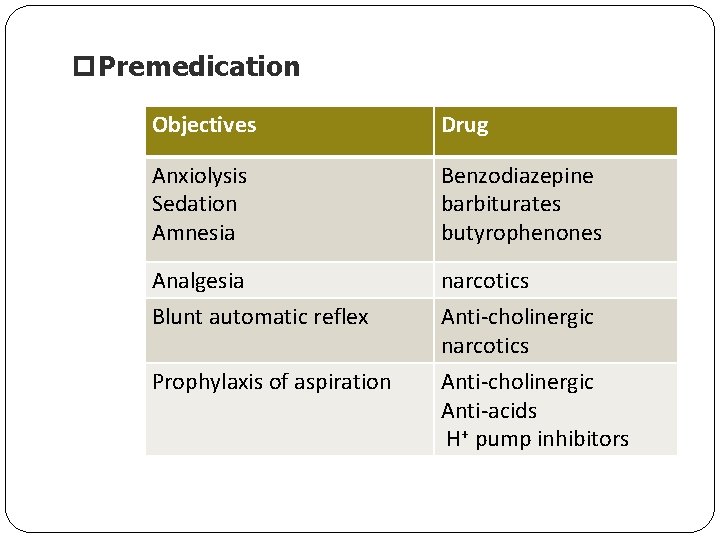
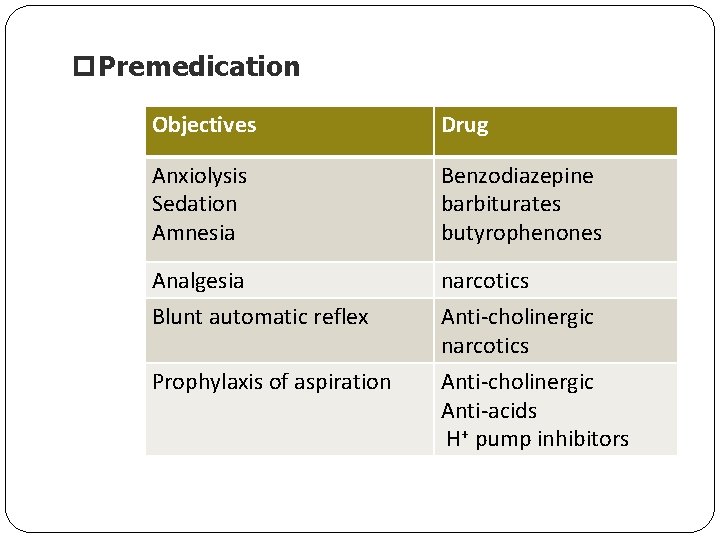
p. Premedication Objectives Drug Anxiolysis Sedation Amnesia Benzodiazepine barbiturates butyrophenones Analgesia Blunt automatic reflex narcotics Anti-cholinergic Anti-acids H+ pump inhibitors Prophylaxis of aspiration
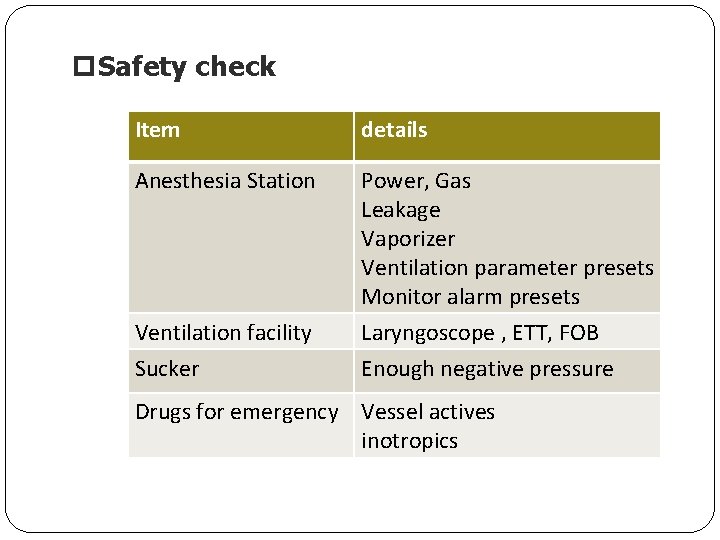
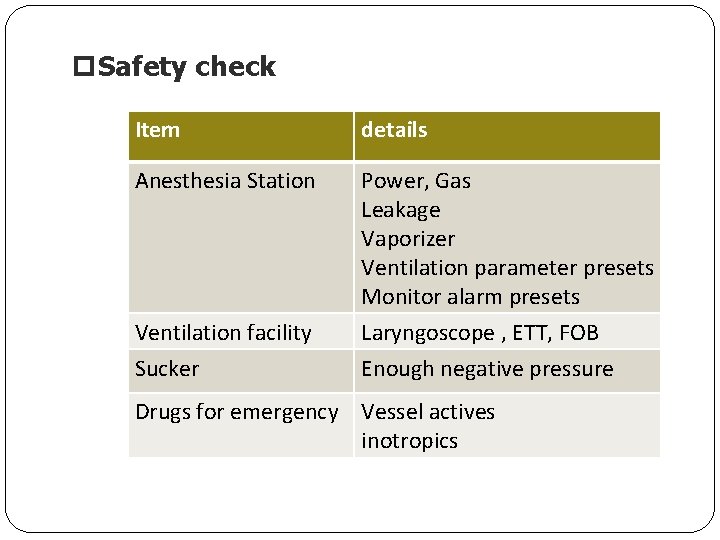
p. Safety check Item details Anesthesia Station Power, Gas Leakage Vaporizer Ventilation parameter presets Monitor alarm presets Laryngoscope , ETT, FOB Enough negative pressure Ventilation facility Sucker Drugs for emergency Vessel actives inotropics
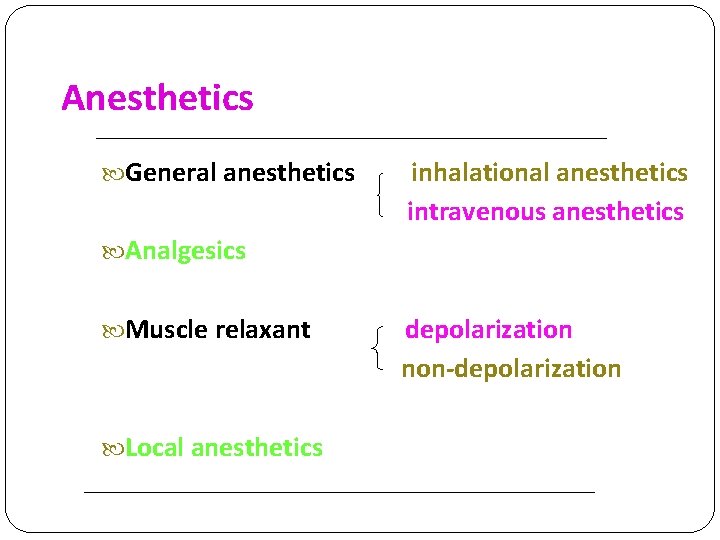
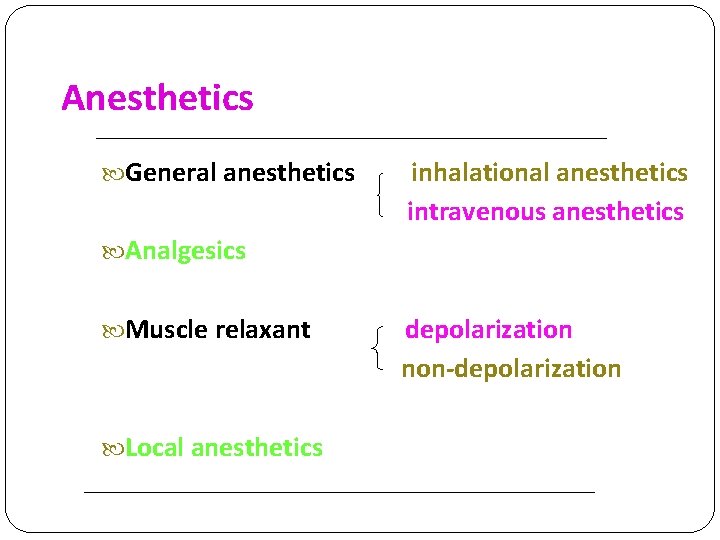
Anesthetics General anesthetics inhalational anesthetics Analgesics intravenous anesthetics Muscle relaxant depolarization non-depolarization Local anesthetics
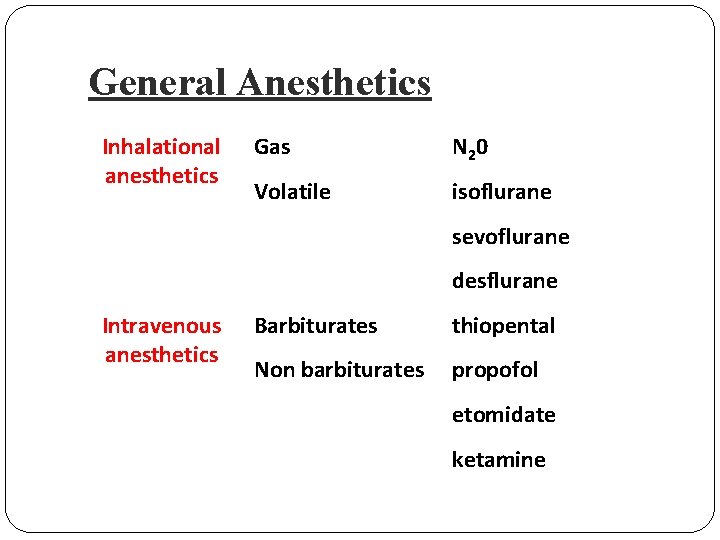
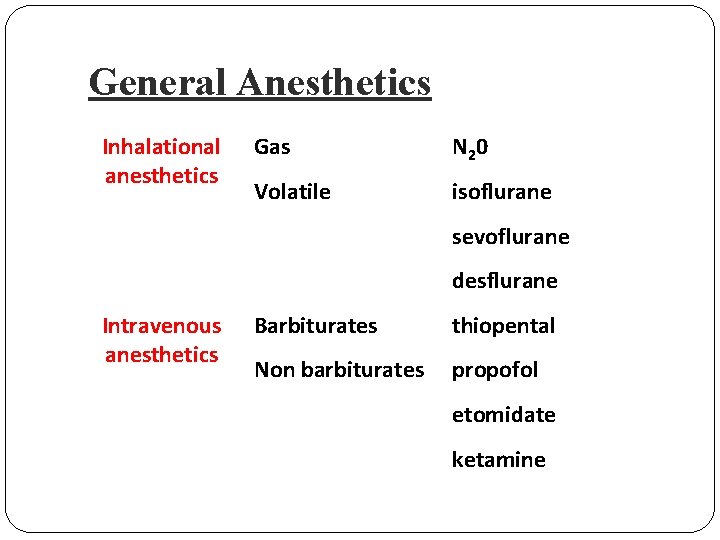
General Anesthetics Inhalational anesthetics Gas N 20 Volatile isoflurane sevoflurane desflurane Intravenous anesthetics Barbiturates thiopental Non barbiturates propofol etomidate ketamine
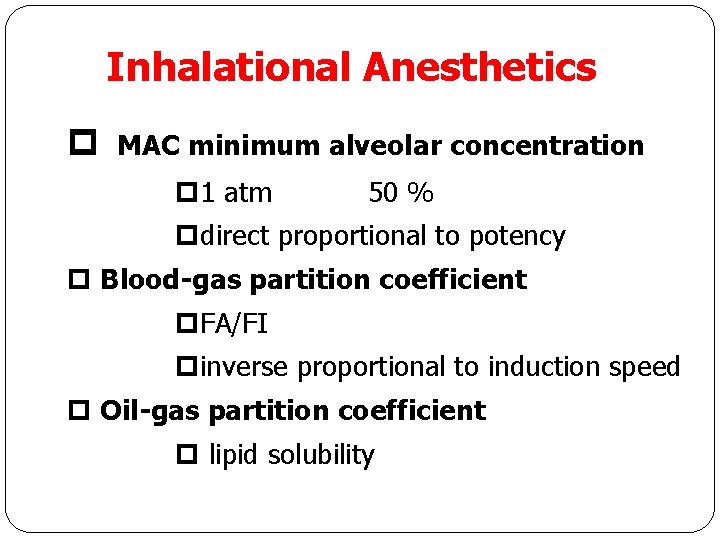
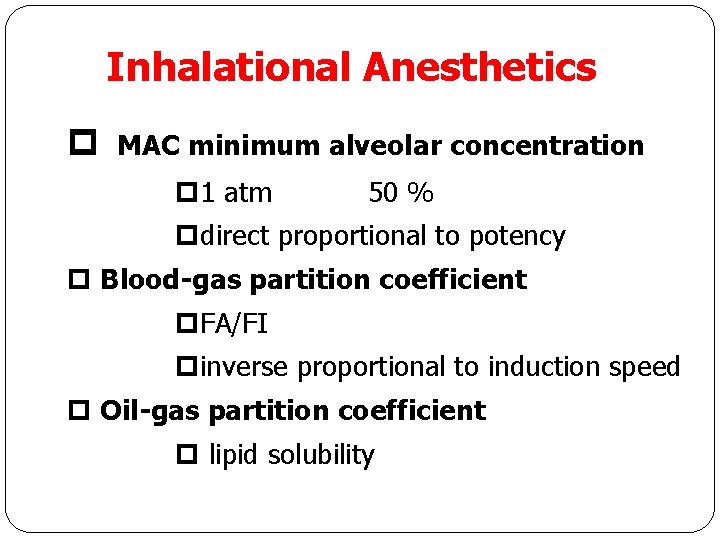
Inhalational Anesthetics p MAC minimum alveolar concentration p 1 atm 50 % pdirect proportional to potency p Blood-gas partition coefficient p. FA/FI pinverse proportional to induction speed p Oil-gas partition coefficient p lipid solubility
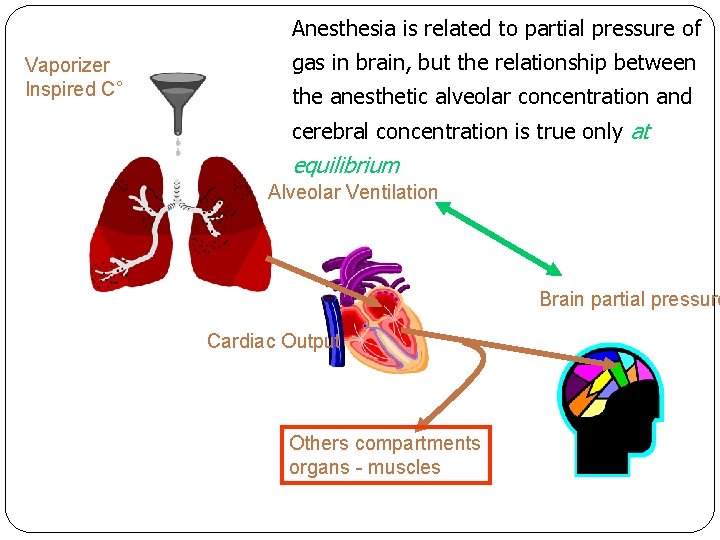
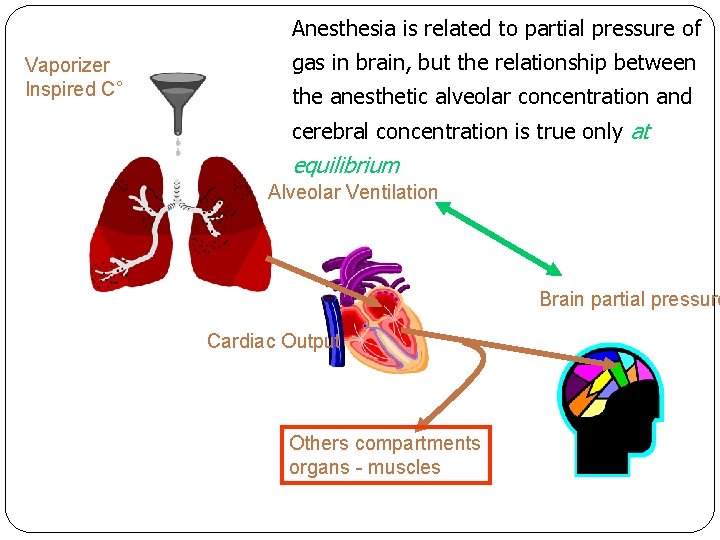
Anesthesia is related to partial pressure of Vaporizer Inspired C° gas in brain, but the relationship between the anesthetic alveolar concentration and cerebral concentration is true only at equilibrium Alveolar Ventilation Brain partial pressure Cardiac Output Others compartments organs - muscles
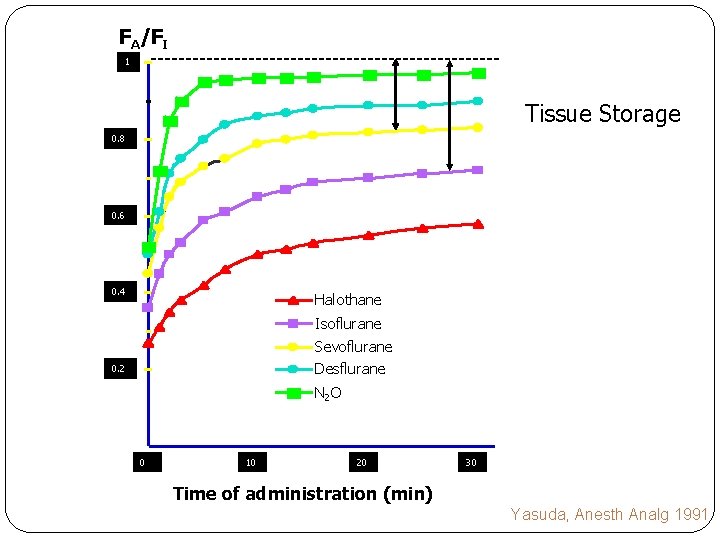
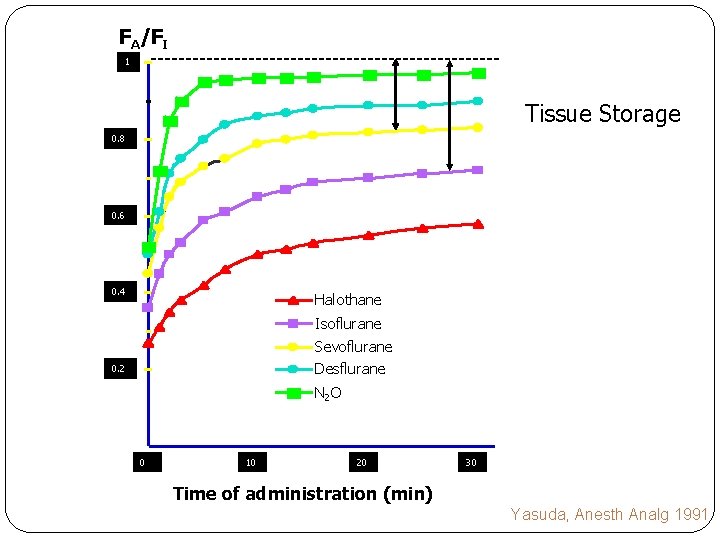
FA/FI 1 Tissue Storage 0. 8 0. 6 0. 4 Halothane Isoflurane Sevoflurane Desflurane 0. 2 N 2 O 0 10 20 Time of administration (min) 30 Time of administration (min) Yasuda, Anesth Analg 1991
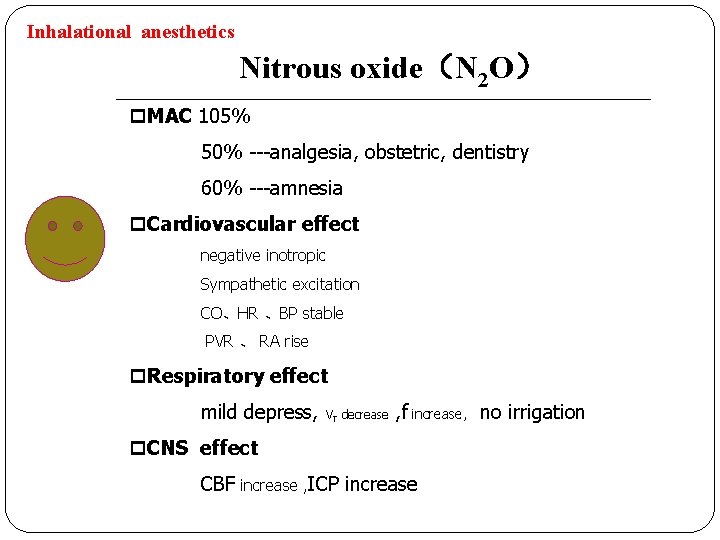
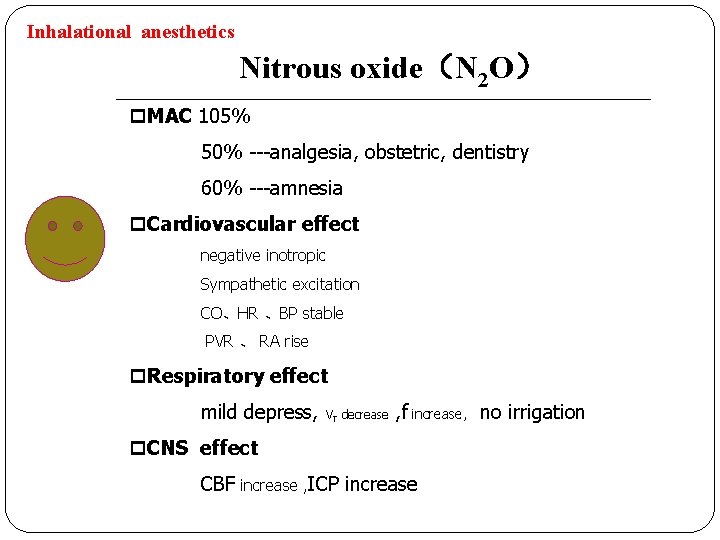
Inhalational anesthetics Nitrous oxide(N 2 O) p. MAC 105% 50% ---analgesia, obstetric, dentistry 60% ---amnesia p. Cardiovascular effect negative inotropic Sympathetic excitation CO、HR 、BP stable PVR 、 RA rise p. Respiratory effect mild depress, VT decrease , f increase, no irrigation p. CNS effect CBF increase , ICP increase
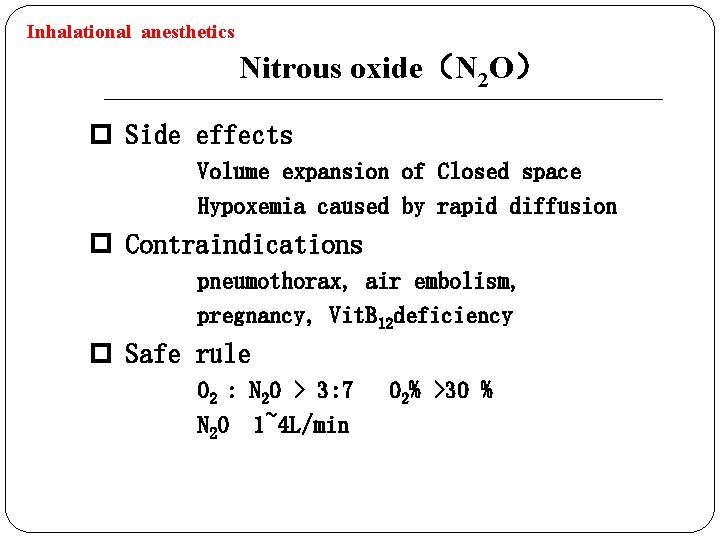
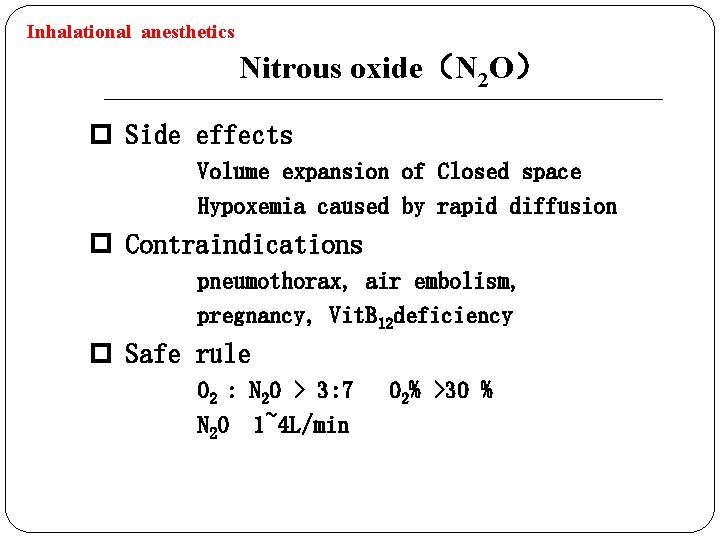
Inhalational anesthetics Nitrous oxide(N 2 O) p Side effects Volume expansion of Closed space Hypoxemia caused by rapid diffusion p Contraindications pneumothorax, air embolism, pregnancy, Vit. B 12 deficiency p Safe rule O 2 : N 2 O > 3: 7 N 2 O 1~4 L/min O 2% >30 %
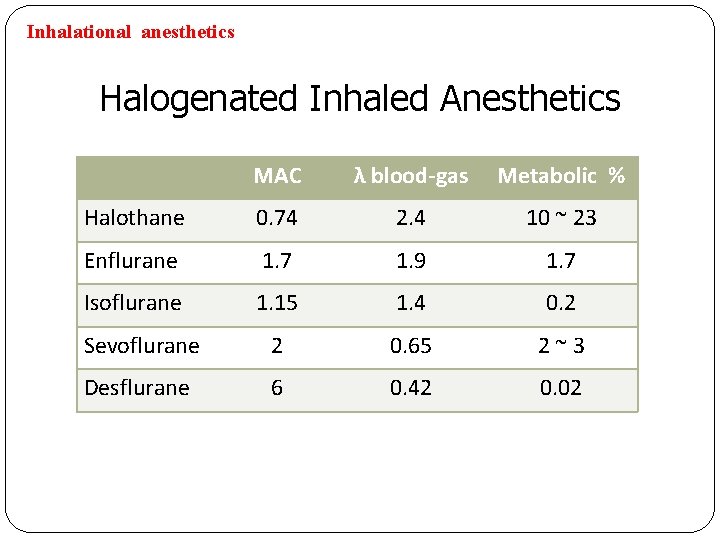
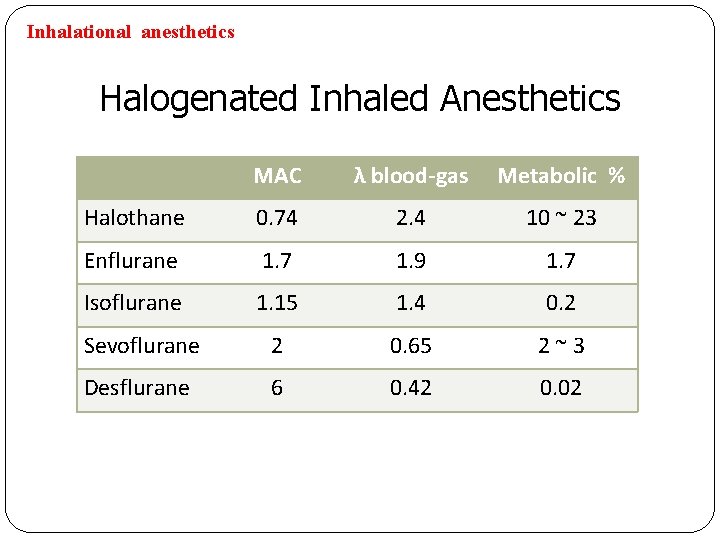
Inhalational anesthetics Halogenated Inhaled Anesthetics MAC λ blood-gas Metabolic % Halothane 0. 74 2. 4 10 ~ 23 Enflurane 1. 7 1. 9 1. 7 Isoflurane 1. 15 1. 4 0. 2 Sevoflurane 2 0. 65 2~3 Desflurane 6 0. 42 0. 02
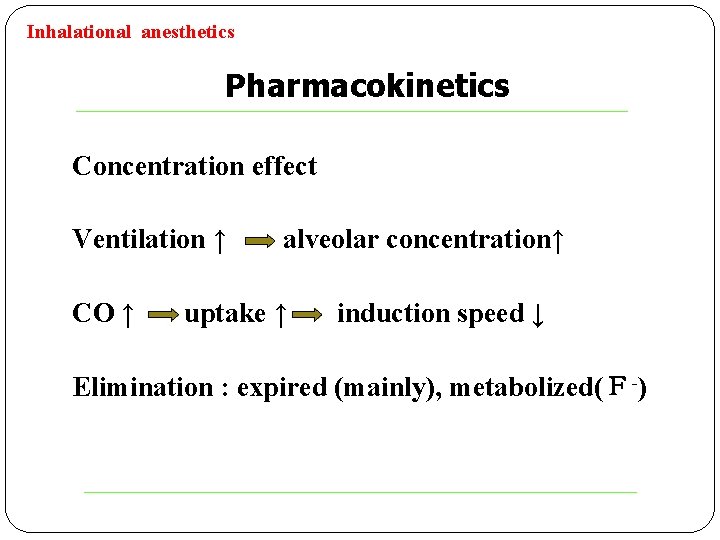
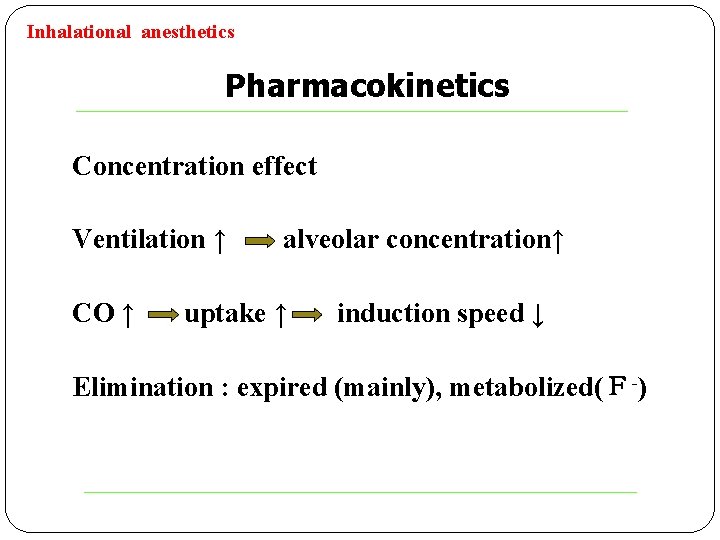
Inhalational anesthetics Pharmacokinetics Concentration effect Ventilation ↑ CO ↑ alveolar concentration↑ uptake ↑ induction speed ↓ Elimination : expired (mainly), metabolized(F-)
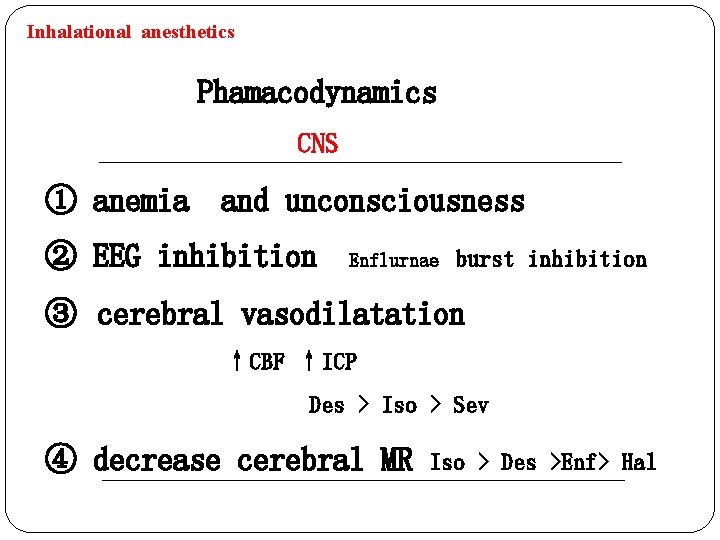
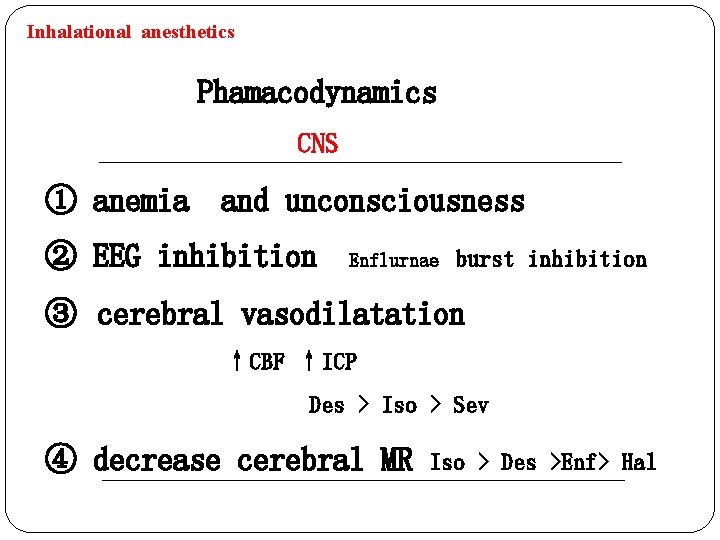
Inhalational anesthetics Phamacodynamics ① anemia CNS and unconsciousness ② EEG inhibition Enflurnae burst inhibition ③ cerebral vasodilatation ↑CBF ↑ICP Des > Iso > Sev ④ decrease cerebral MR Iso > Des >Enf> Hal
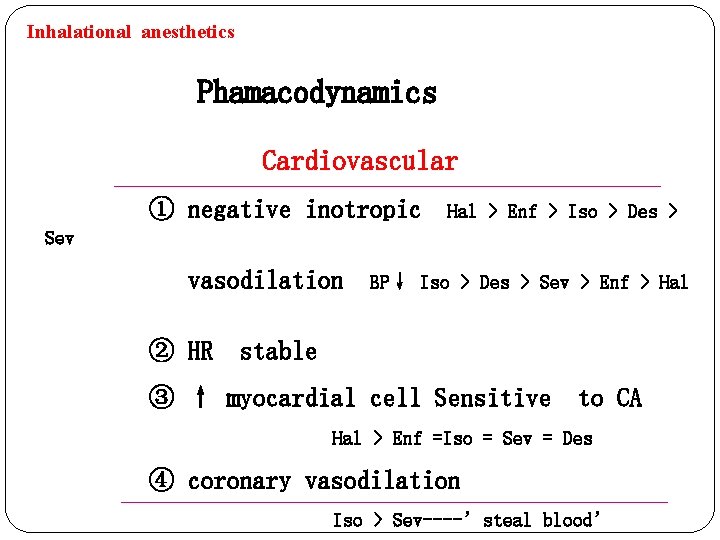
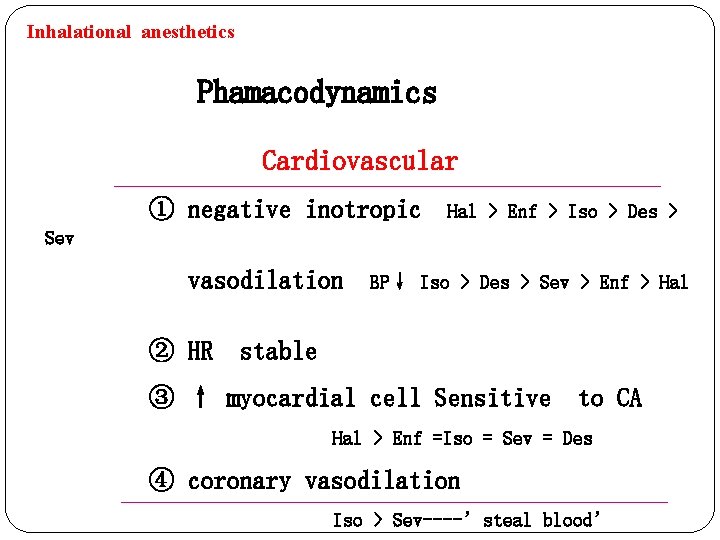
Inhalational anesthetics Phamacodynamics Cardiovascular ① negative inotropic Hal > Enf > Iso > Des > Sev vasodilation BP↓ Iso > Des > Sev > Enf > Hal ② HR stable ③ ↑ myocardial cell Sensitive to CA Hal > Enf =Iso = Sev = Des ④ coronary vasodilation Iso > Sev----’steal blood’
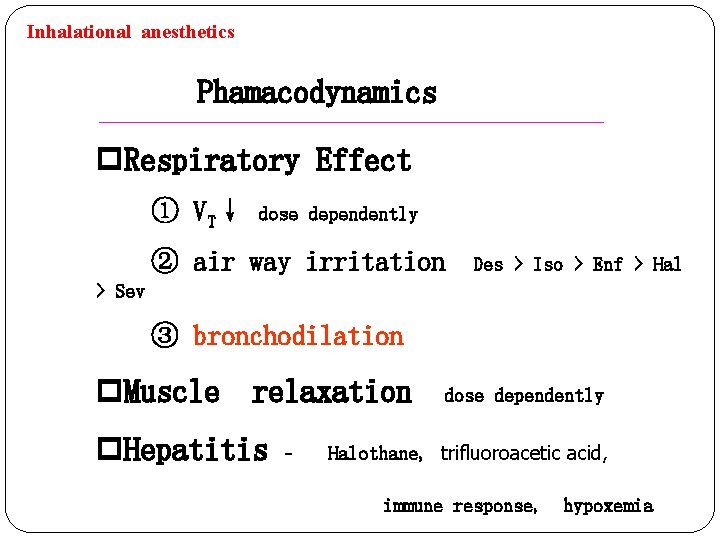
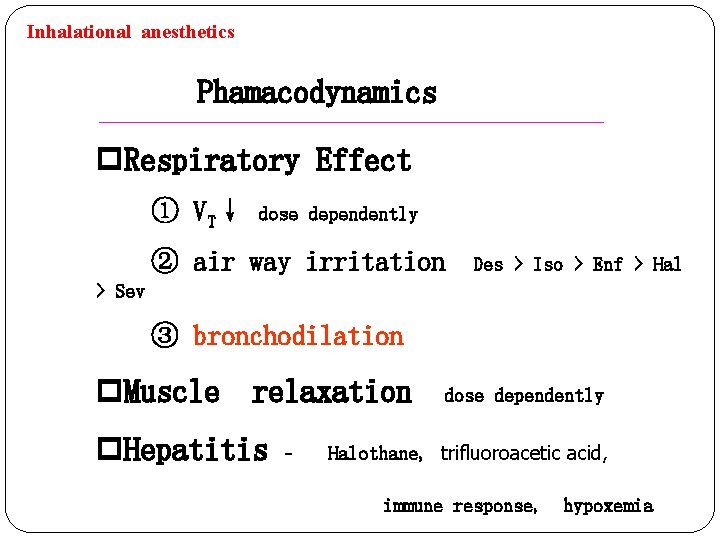
Inhalational anesthetics Phamacodynamics p. Respiratory Effect ① VT↓ dose dependently ② air way irritation Des > Iso > Enf > Hal > Sev ③ bronchodilation p. Muscle relaxation dose dependently p. Hepatitis - Halothane, trifluoroacetic acid, immune response, hypoxemia
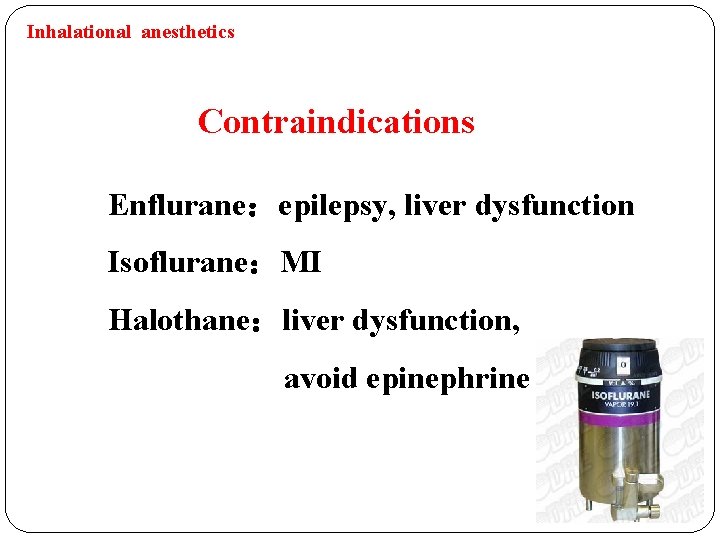
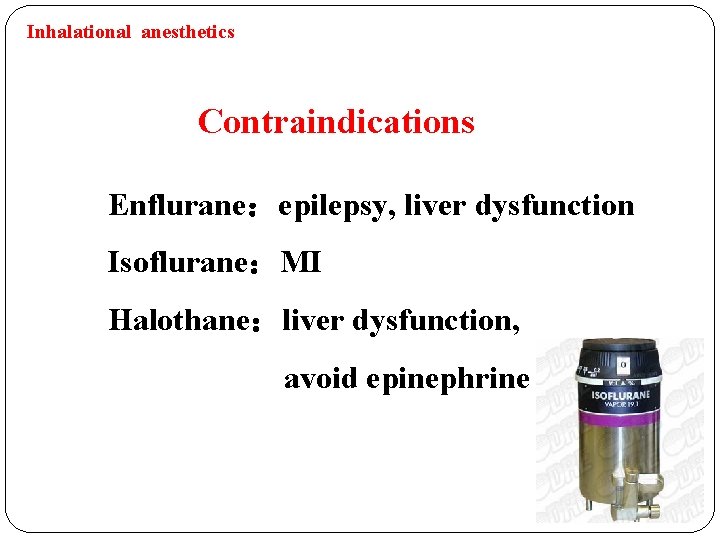
Inhalational anesthetics Contraindications Enflurane:epilepsy, liver dysfunction Isoflurane:MI Halothane:liver dysfunction, avoid epinephrine
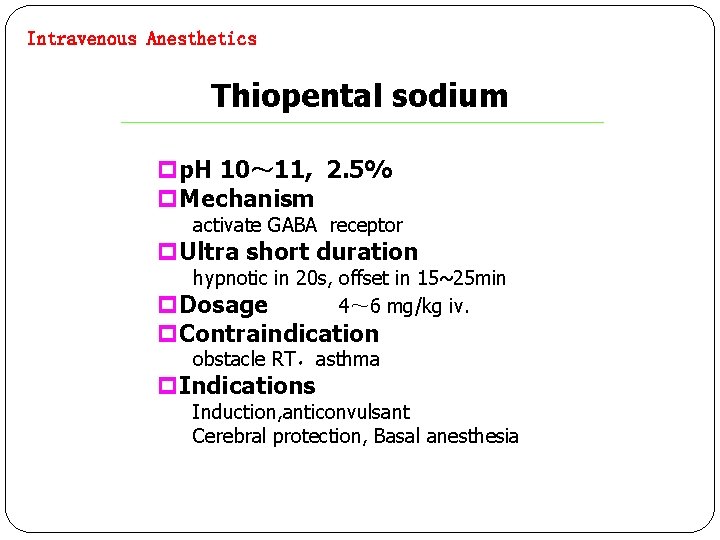
Intravenous Anesthetics Thiopental sodium pp. H 10~ 11, 2. 5% p. Mechanism activate GABA receptor p. Ultra short duration hypnotic in 20 s, offset in 15~25 min p. Dosage 4~ 6 mg/kg iv. p. Contraindication obstacle RT,asthma p. Indications Induction, anticonvulsant Cerebral protection, Basal anesthesia
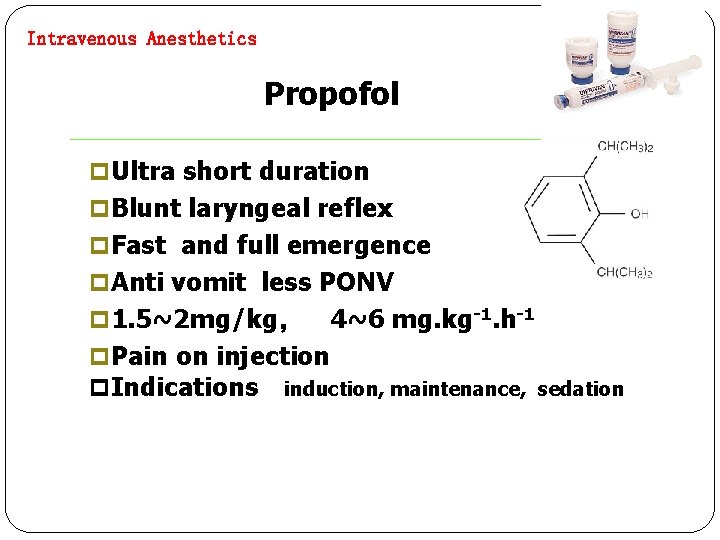
Intravenous Anesthetics Propofol p Ultra short duration p Blunt laryngeal reflex p Fast and full emergence p Anti vomit less PONV p 1. 5~2 mg/kg, 4~6 mg. kg-1. h-1 p Pain on injection p Indications induction, maintenance, sedation
Intravenous Anesthetics Etomidate Advantages minimal effect on cardiovascular and respiratory system Coronary vasodilation, decrease ICP Disadvantages Pain on injection, thrombophlebitis Myoclonus PONV 40 % inhibition of adrenocortical synthesis Indication Induction 0. 2 ~ 0. 3 mg/kg iv.
Intravenous Anesthetics Ketamine p. Mechanism NMDA receptor antagonist p. Dissociative anesthesia lsympathomimetic activity l. HR,BP↑ l. CBF ↑, CMR↑, ICP↑ p. Advantage • Keep normal breath • bronchodilation • Analgesia p Disadvantage Larynx reflex,troublesome salivation, mental disorder
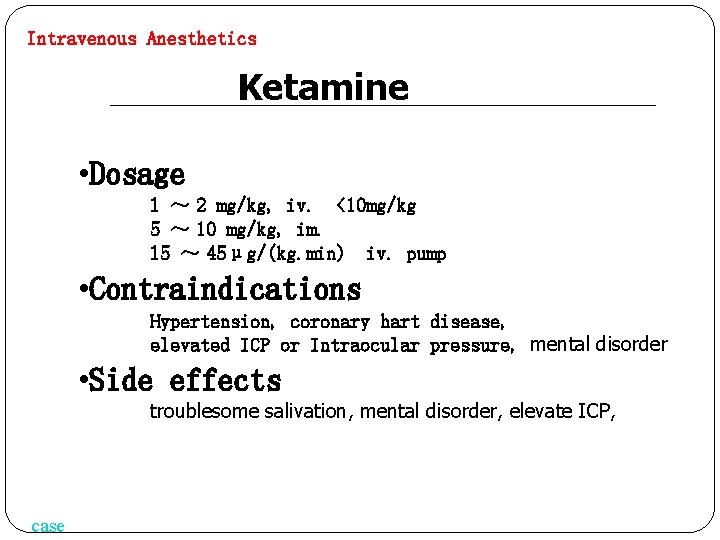
Intravenous Anesthetics Ketamine • Dosage 1 ~ 2 mg/kg, iv. <10 mg/kg 5 ~ 10 mg/kg, im. 15 ~ 45μg/(kg. min) iv. pump • Contraindications Hypertension, coronary hart disease, elevated ICP or Intraocular pressure, mental disorder • Side effects troublesome salivation, mental disorder, elevate ICP, case
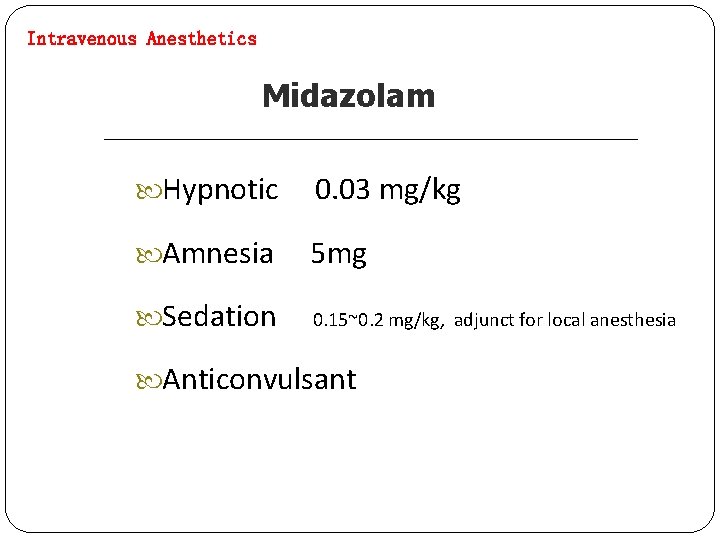
Intravenous Anesthetics Midazolam Hypnotic 0. 03 mg/kg Amnesia 5 mg Sedation 0. 15~0. 2 mg/kg, adjunct for local anesthesia Anticonvulsant
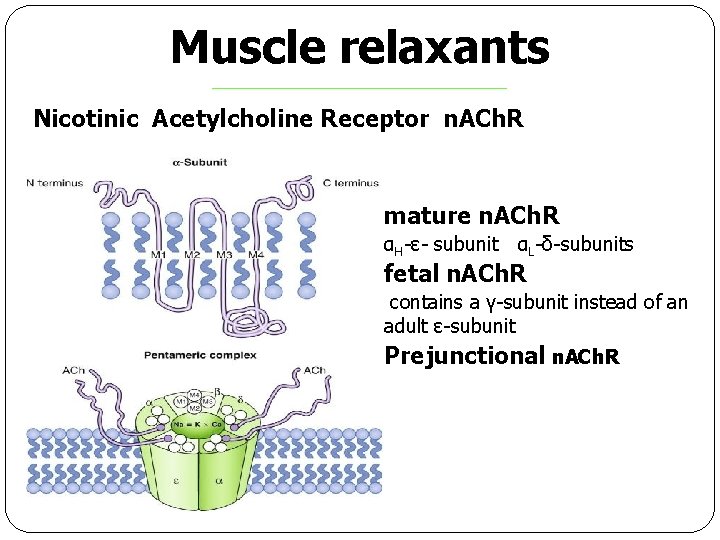
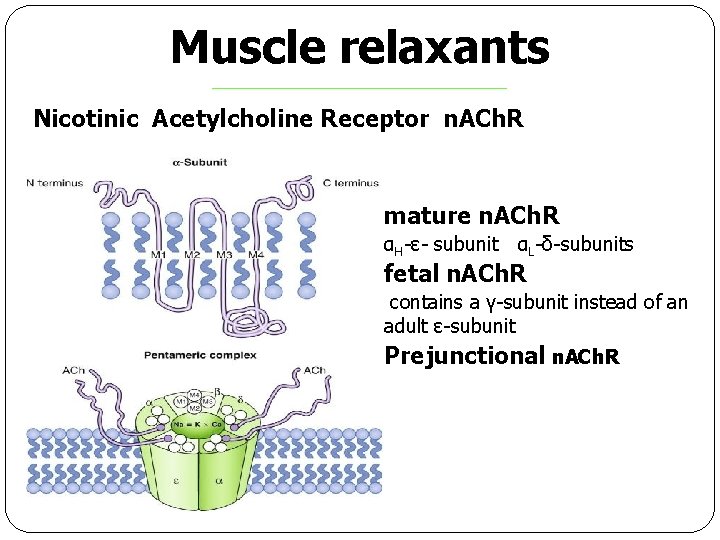
Muscle relaxants Nicotinic Acetylcholine Receptor n. ACh. R mature n. ACh. R αH-ε- subunit αL-δ-subunits fetal n. ACh. R contains a γ-subunit instead of an adult ε-subunit Prejunctional n. ACh. R
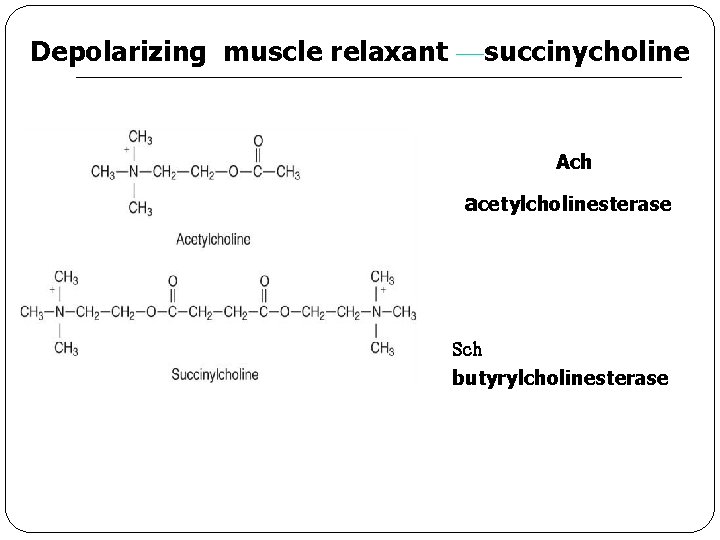
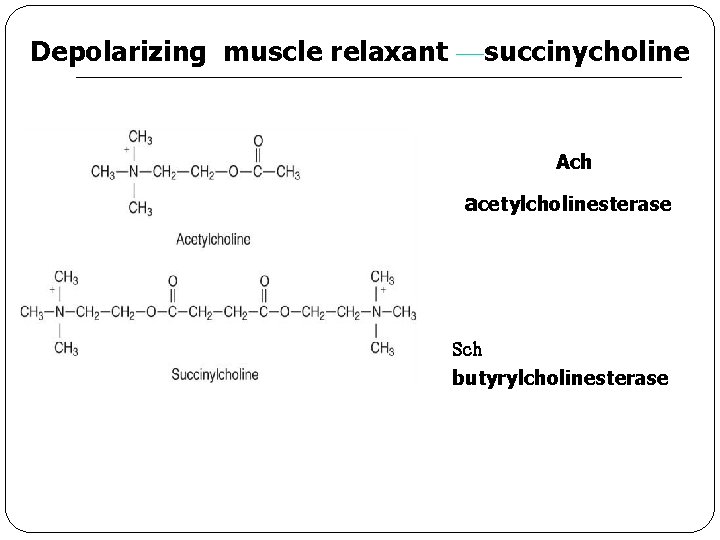
Depolarizing muscle relaxant —succinycholine Ach acetylcholinesterase Sch butyrylcholinesterase
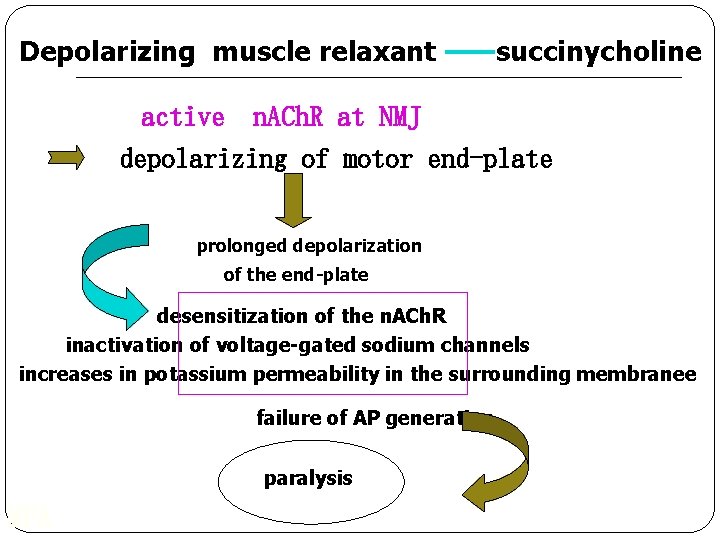
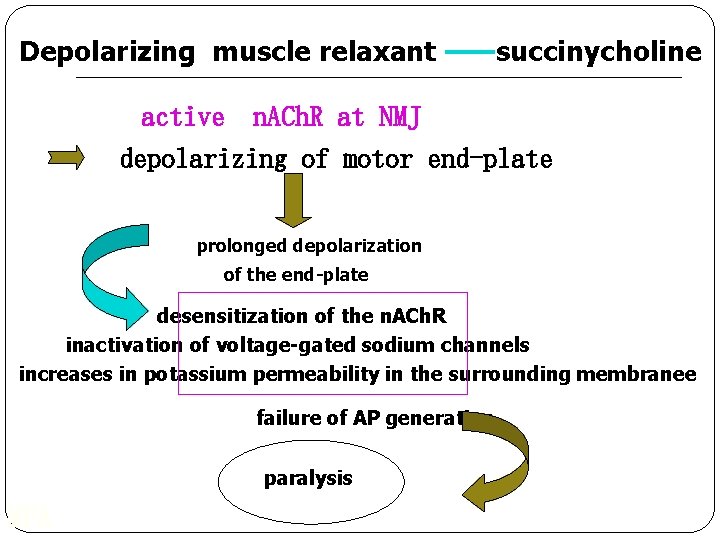
Depolarizing muscle relaxant ——succinycholine active n. ACh. R at NMJ depolarizing of motor end-plate prolonged depolarization of the end-plate desensitization of the n. ACh. R inactivation of voltage-gated sodium channels increases in potassium permeability in the surrounding membranee failure of AP generation paralysis MPA
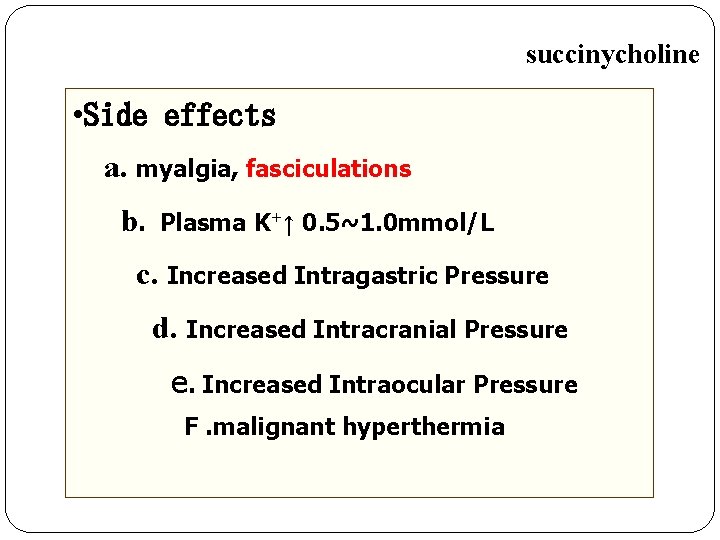
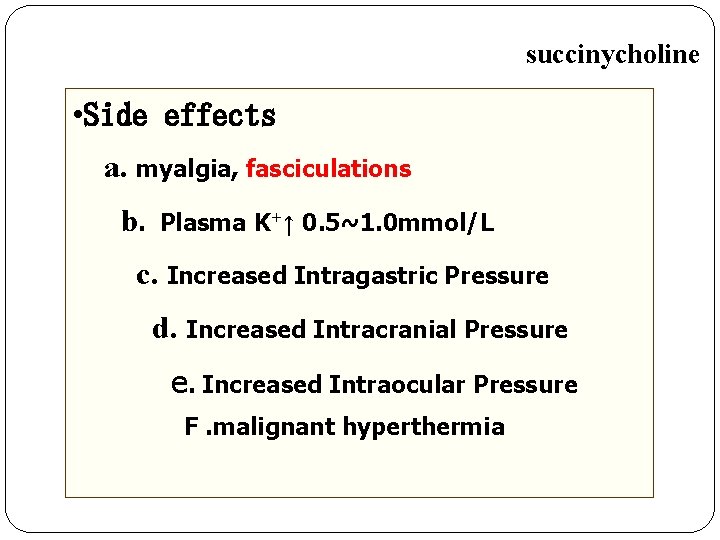
succinycholine • Side effects a. myalgia, fasciculations b. Plasma K+↑ 0. 5~1. 0 mmol/L c. Increased Intragastric Pressure d. Increased Intracranial Pressure e. Increased Intraocular Pressure F. malignant hyperthermia
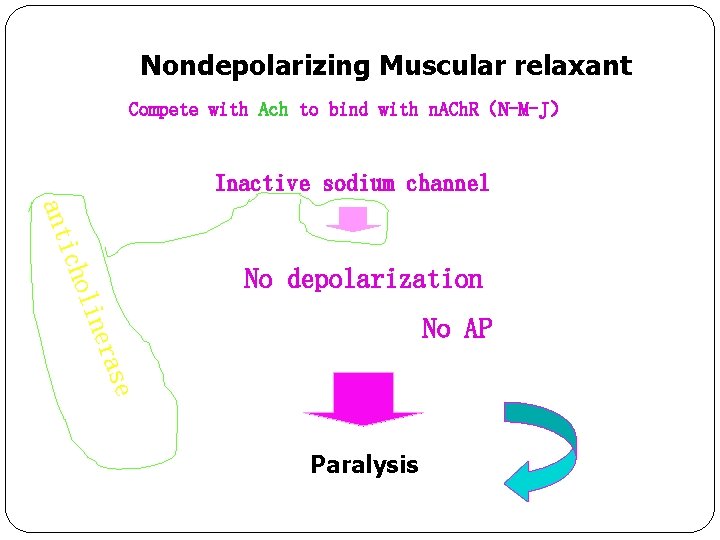
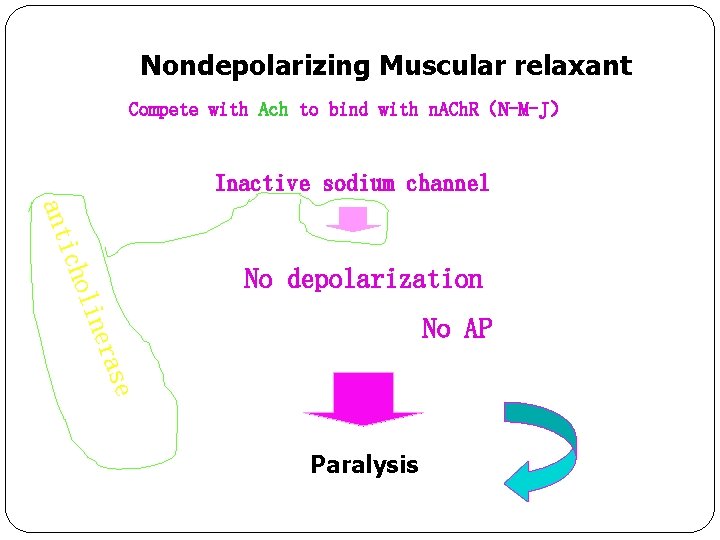
Nondepolarizing Muscular relaxant Compete with Ach to bind with n. ACh. R(N-M-J) Inactive sodium channel No depolarization lin o ich ant se era No AP Paralysis
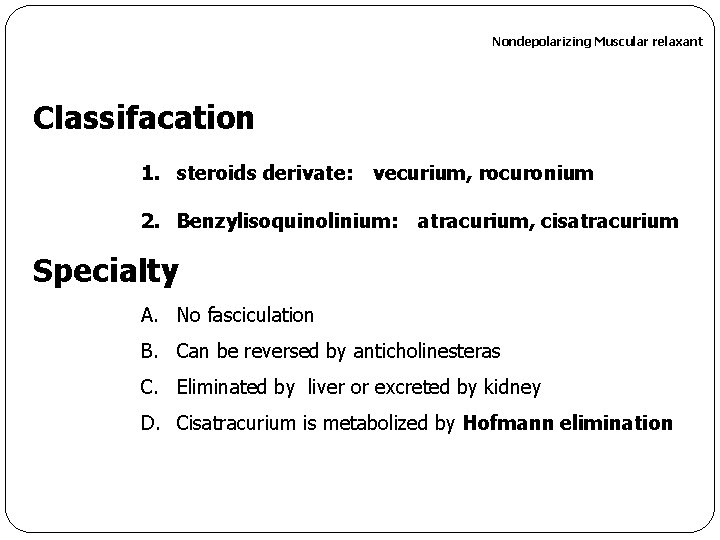
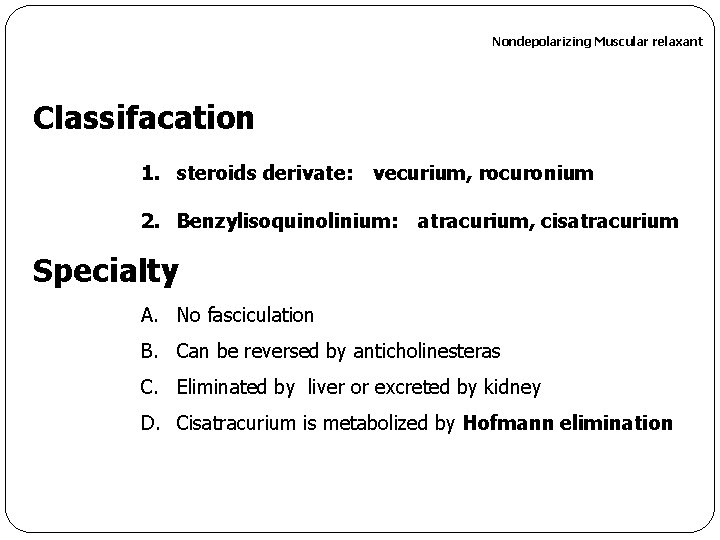
Nondepolarizing Muscular relaxant Classifacation 1. steroids derivate: vecurium, rocuronium 2. Benzylisoquinolinium: atracurium, cisatracurium Specialty A. No fasciculation B. Can be reversed by anticholinesteras C. Eliminated by liver or excreted by kidney D. Cisatracurium is metabolized by Hofmann elimination
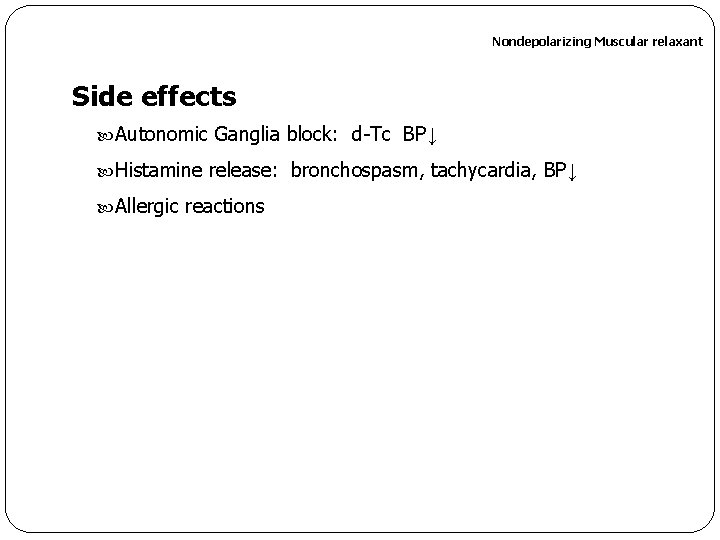
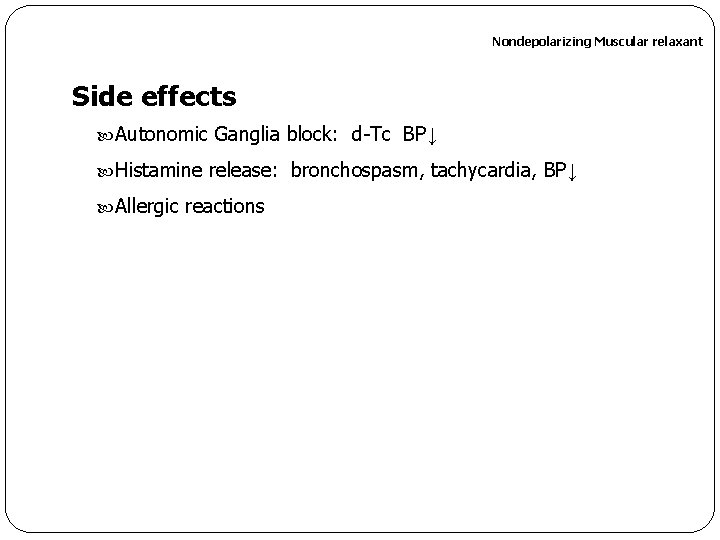
Nondepolarizing Muscular relaxant Side effects Autonomic Ganglia block: d-Tc BP↓ Histamine release: bronchospasm, tachycardia, BP↓ Allergic reactions
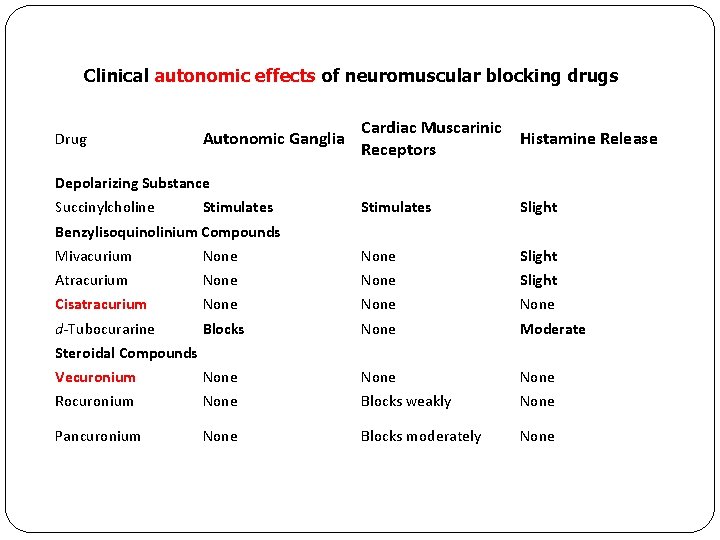
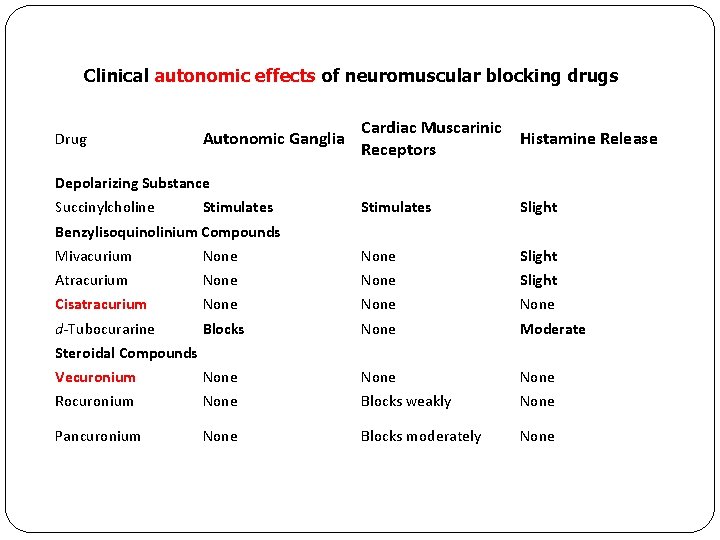
Clinical autonomic effects of neuromuscular blocking drugs Drug Autonomic Ganglia Cardiac Muscarinic Receptors Histamine Release Stimulates Slight Depolarizing Substance Succinylcholine Stimulates Benzylisoquinolinium Compounds Mivacurium None Slight Atracurium None Slight Cisatracurium None d-Tubocurarine Blocks None Moderate Vecuronium None Rocuronium None Blocks weakly None Pancuronium None Blocks moderately None Steroidal Compounds
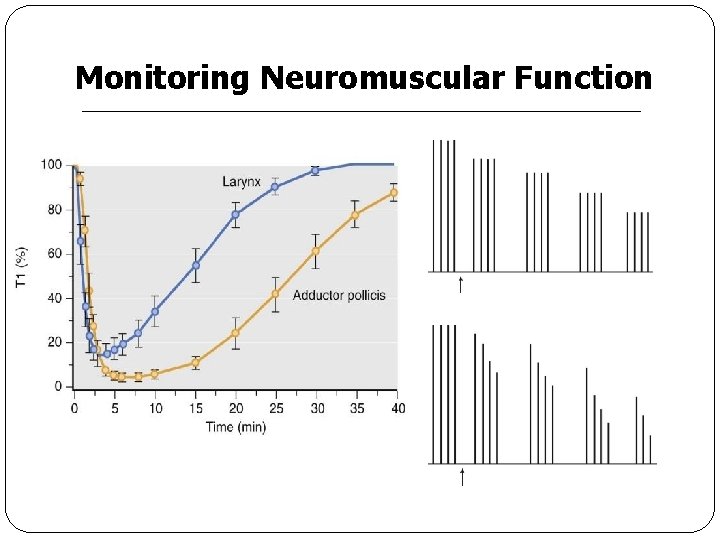
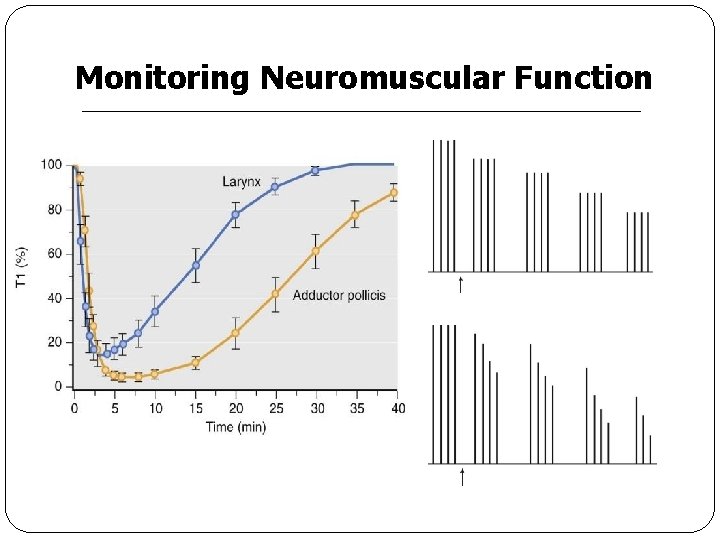
Monitoring Neuromuscular Function
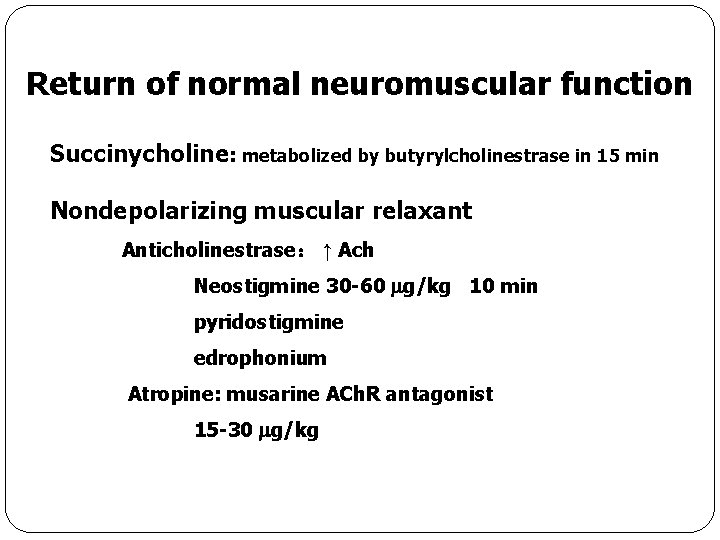
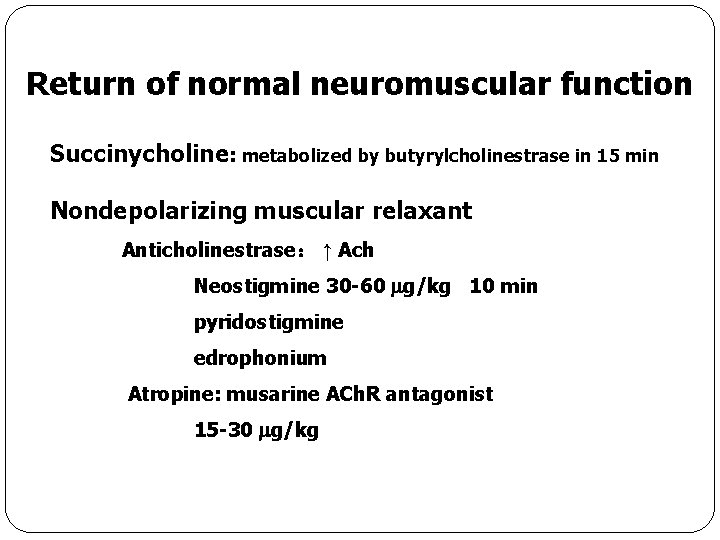
Return of normal neuromuscular function Succinycholine: metabolized by butyrylcholinestrase in 15 min Nondepolarizing muscular relaxant Anticholinestrase: ↑ Ach Neostigmine 30 -60 g/kg 10 min pyridostigmine edrophonium Atropine: musarine ACh. R antagonist 15 -30 g/kg
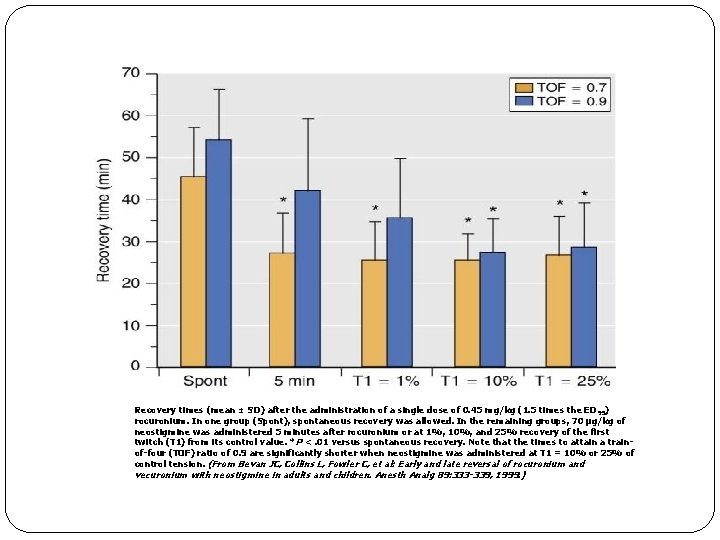
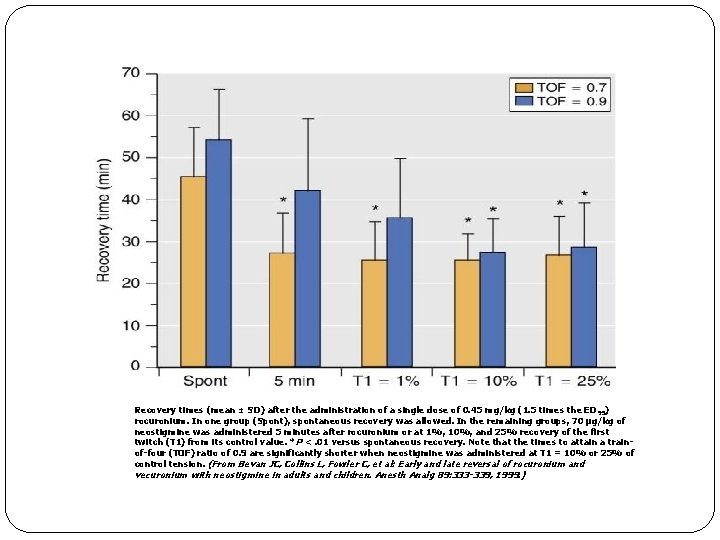
Recovery times (mean ± SD) after the administration of a single dose of 0. 45 mg/kg (1. 5 times the ED 95) rocuronium. In one group (Spont), spontaneous recovery was allowed. In the remaining groups, 70 µg/kg of neostigmine was administered 5 minutes after rocuronium or at 1%, 10%, and 25% recovery of the first twitch (T 1) from its control value. *P <. 01 versus spontaneous recovery. Note that the times to attain a trainof-four (TOF) ratio of 0. 9 are significantly shorter when neostigmine was administered at T 1 = 10% or 25% of control tension. (From Bevan JC, Collins L, Fowler C, et al: Early and late reversal of rocuronium and vecuronium with neostigmine in adults and children. Anesth Analg 89: 333 -339, 1999. )
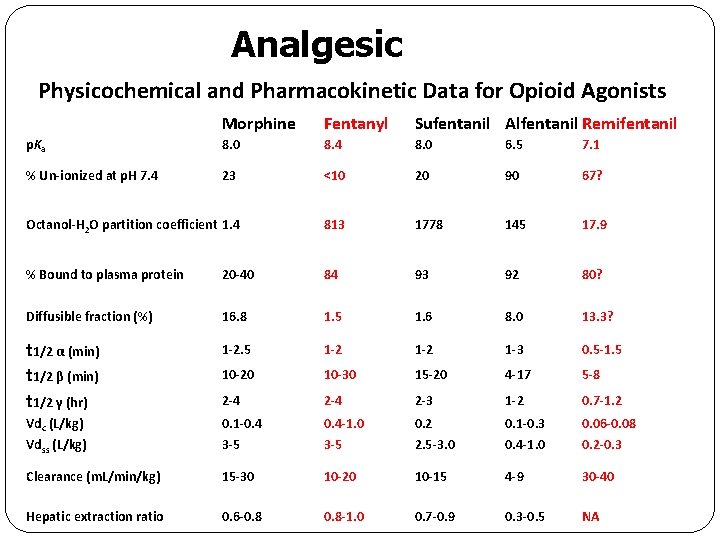
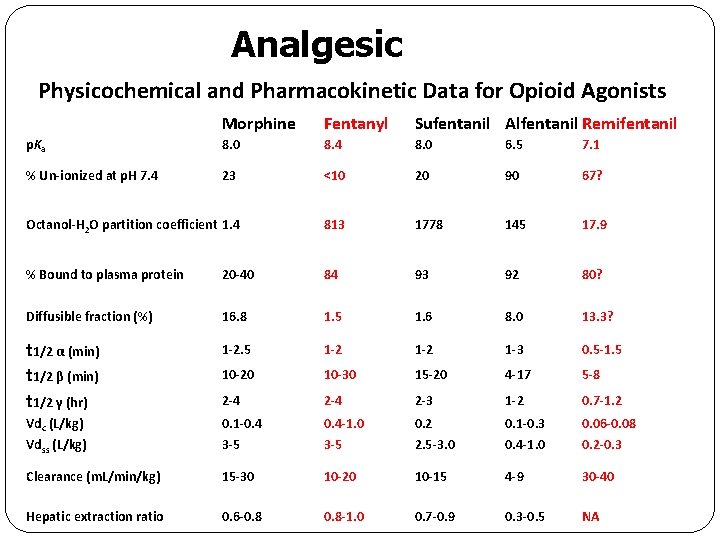
Analgesic Physicochemical and Pharmacokinetic Data for Opioid Agonists Morphine Fentanyl Sufentanil Alfentanil Remifentanil p. Ka 8. 0 8. 4 8. 0 6. 5 7. 1 % Un-ionized at p. H 7. 4 23 <10 20 90 67? Octanol-H 2 O partition coefficient 1. 4 813 1778 145 17. 9 % Bound to plasma protein 20 -40 84 93 92 80? Diffusible fraction (%) 16. 8 1. 5 1. 6 8. 0 13. 3? t 1/2 α (min) t 1/2 β (min) t 1/2 γ (hr) 1 -2. 5 1 -2 1 -3 0. 5 -1. 5 10 -20 10 -30 15 -20 4 -17 5 -8 2 -4 2 -3 1 -2 0. 7 -1. 2 Vdc (L/kg) 0. 1 -0. 4 -1. 0 0. 2 0. 1 -0. 3 0. 06 -0. 08 Vdss (L/kg) 3 -5 2. 5 -3. 0 0. 4 -1. 0 0. 2 -0. 3 Clearance (m. L/min/kg) 15 -30 10 -20 10 -15 4 -9 30 -40 Hepatic extraction ratio 0. 6 -0. 8 -1. 0 0. 7 -0. 9 0. 3 -0. 5 NA
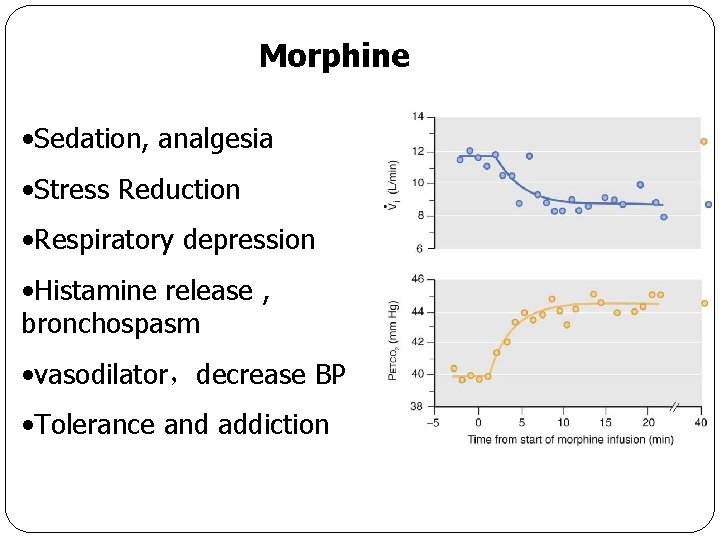
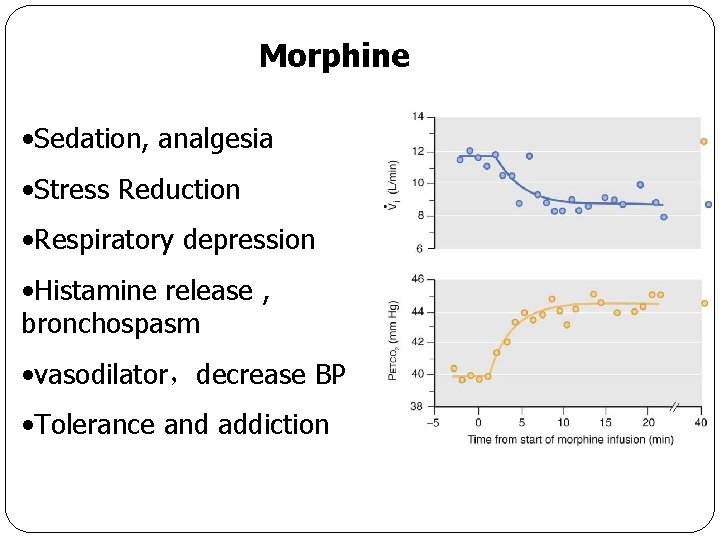
Morphine • Sedation, analgesia • Stress Reduction • Respiratory depression • Histamine release , bronchospasm • vasodilator,decrease BP • Tolerance and addiction
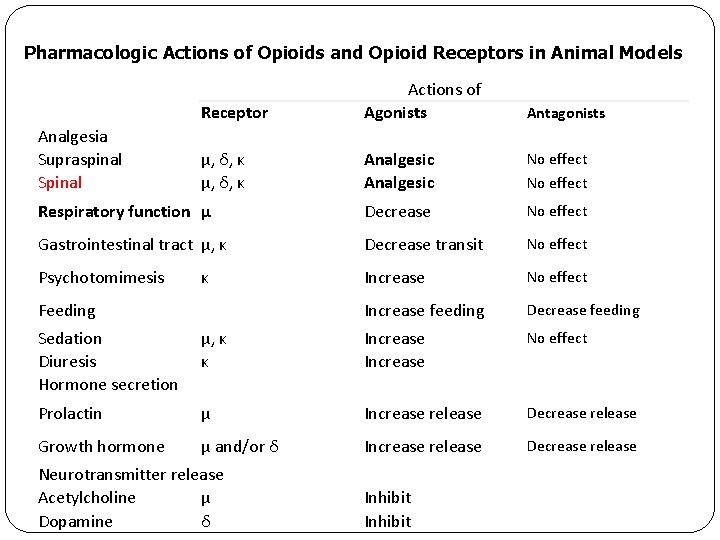
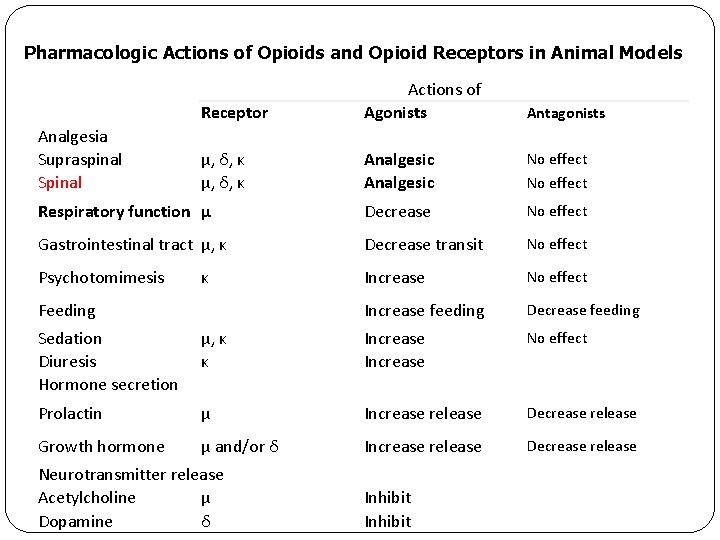
Pharmacologic Actions of Opioids and Opioid Receptors in Animal Models Receptor Actions of Agonists Antagonists μ, δ, κ Analgesic No effect Respiratory function μ Decrease No effect Gastrointestinal tract μ, κ Decrease transit No effect Psychotomimesis Increase No effect Increase feeding Decrease feeding Analgesia Supraspinal Spinal κ Feeding Sedation Diuresis Hormone secretion μ, κ κ Increase No effect Prolactin μ Increase release Decrease release Growth hormone μ and/or δ Increase release Decrease release Neurotransmitter release Acetylcholine μ Dopamine δ Inhibit
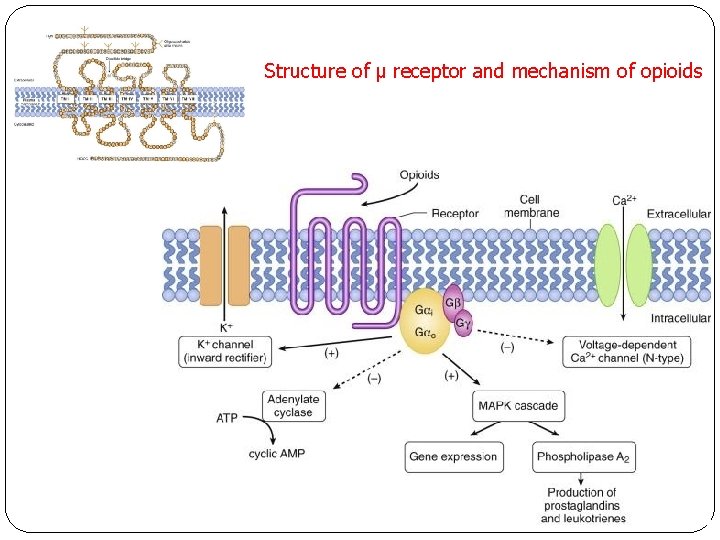
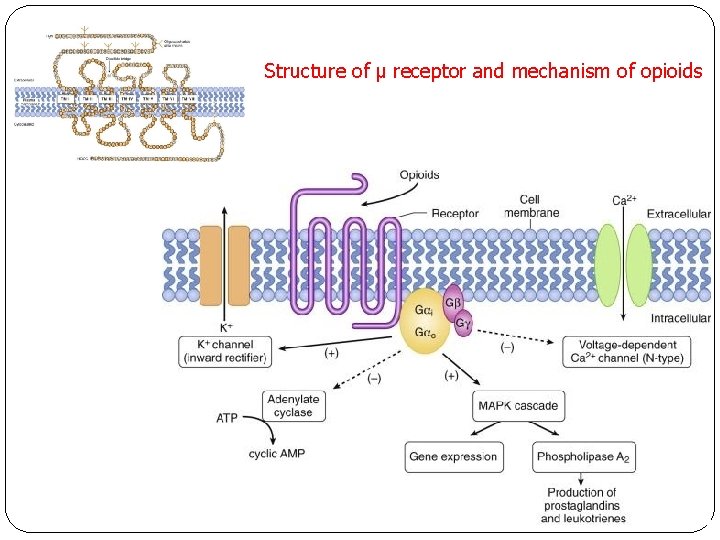
Structure of μ receptor and mechanism of opioids
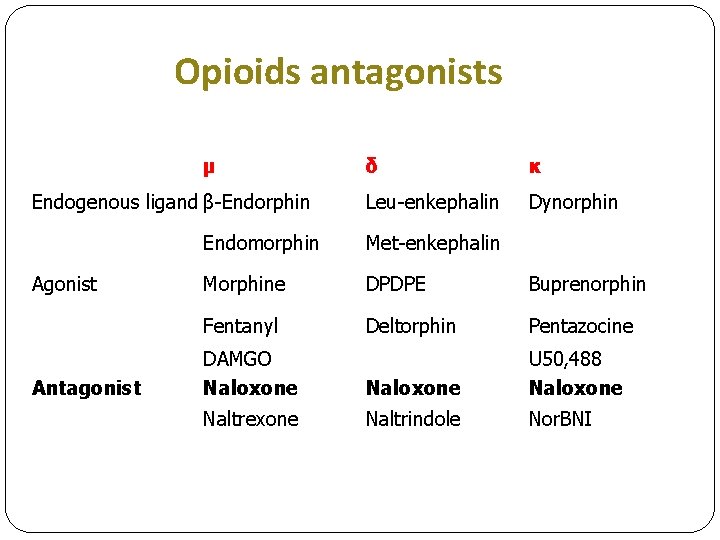
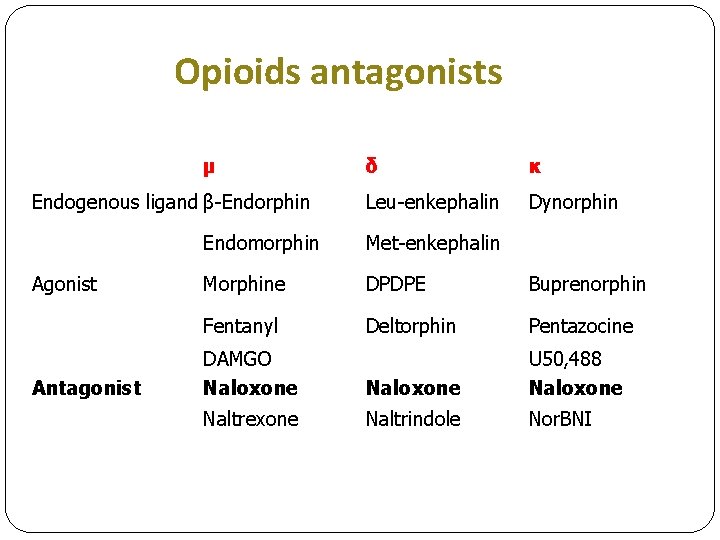
Opioids antagonists μ Endogenous ligand β-Endorphin Agonist Antagonist δ κ Leu-enkephalin Dynorphin Endomorphin Met-enkephalin Morphine DPDPE Buprenorphin Fentanyl Deltorphin Pentazocine DAMGO Naloxone U 50, 488 Naloxone Naltrexone Naltrindole Nor. BNI