Family Community Medicine Faculty Compensation Incentive Plans Stephen
- Slides: 14
Family & Community Medicine Faculty Compensation & Incentive Plans Stephen J. Spann, M. D. , M. B. A. Atma Ram, M. S. , M. B. A ADFM Winter 2011 Conference February 24, 2011
Faculty Compensation & Incentive Plans Our Faculty Roster n 130 Faculty Members (106 FTEs) MDs n Ph. Ds n Majority are clinical (~94 FTEs) n Several involved in all three missions n n Education, Clinical, Research
Faculty Compensation & Incentive Plans Evolution 2004 to 2011 n Historical n n n Current n n n Multiple structures Within the Dept. , and across the College Standardized within the Department Some consistency across the College Going Forward n n Mission based CARTS methodology
Faculty Compensation & Incentive Plans Summary Feedback - 2007 n n n n n Underpaid, and severely underpaid Lack of recognition for years of service Multiple “base” salary levels CME $ award is not adequate Multiple approaches to Saturday/evening work Multiple hourly rates Provider retention issues – accelerating losses Leadership roles increasingly becoming challenging Only base salary was contributing to the retirement benefits
Faculty Compensation & Incentive Plans Our Approach n Structure n n n Base salary – fixed based on Rank and FTE Augmented for seniority, leadership role, additional duties Incentive compensation n Benchmarks n n n Clinical – based on above target production Research – based on salary coverage and total grant funding AAMC for base salary MGMA for clinical production in Work RVUs Other factors considered n n Academic practice and Community practice (public) Quality & Team work
Faculty Compensation & Incentive Plans Current Benchmarks n AAMC – Total compensation for Family Medicine (median) in $K n n n Assistant Professor Associate Professor Mid-levels MGMA – Production in Work RVUs (WRVU) n For clinical time only 75% tile for academic practice (private) n Median level for community practice (public) n
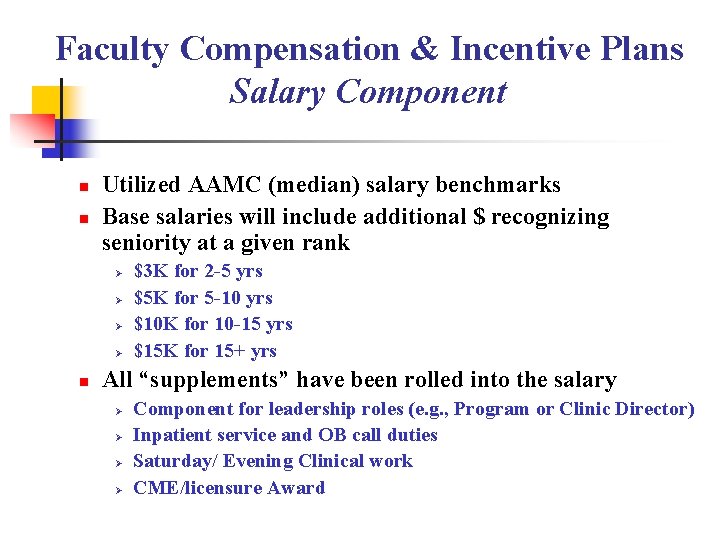
Faculty Compensation & Incentive Plans Salary Component n n Utilized AAMC (median) salary benchmarks Base salaries will include additional $ recognizing seniority at a given rank Ø Ø n $3 K for 2 -5 yrs $5 K for 5 -10 yrs $10 K for 10 -15 yrs $15 K for 15+ yrs All “supplements” have been rolled into the salary Ø Ø Component for leadership roles (e. g. , Program or Clinic Director) Inpatient service and OB call duties Saturday/ Evening Clinical work CME/licensure Award
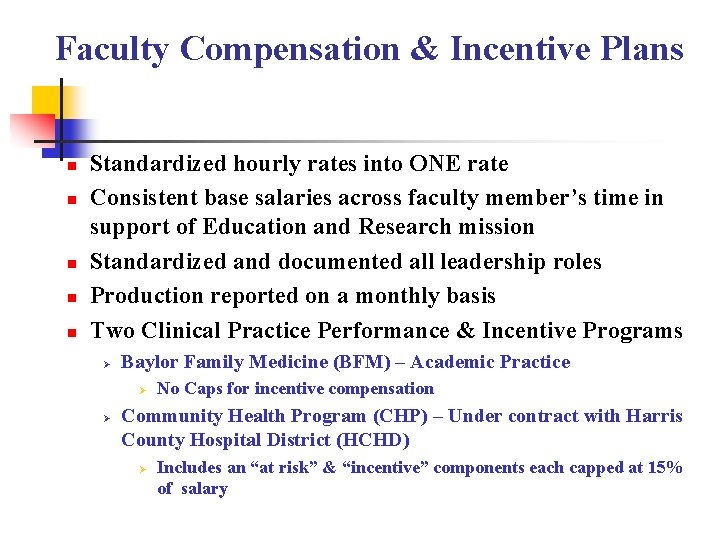
Faculty Compensation & Incentive Plans n n n Standardized hourly rates into ONE rate Consistent base salaries across faculty member’s time in support of Education and Research mission Standardized and documented all leadership roles Production reported on a monthly basis Two Clinical Practice Performance & Incentive Programs Ø Baylor Family Medicine (BFM) – Academic Practice Ø Ø No Caps for incentive compensation Community Health Program (CHP) – Under contract with Harris County Hospital District (HCHD) Ø Includes an “at risk” & “incentive” components each capped at 15% of salary
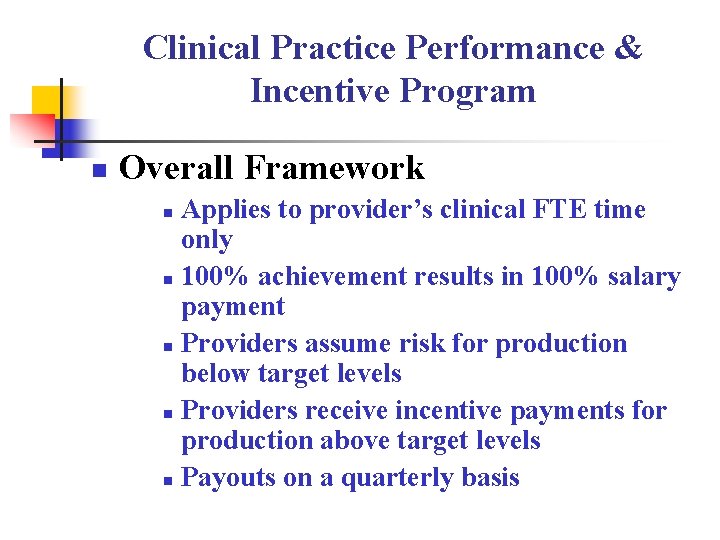
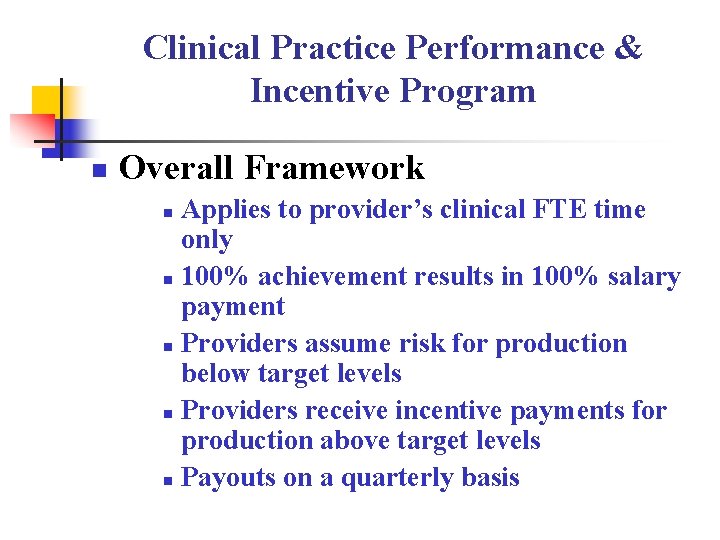
Clinical Practice Performance & Incentive Program n Overall Framework Applies to provider’s clinical FTE time only n 100% achievement results in 100% salary payment n Providers assume risk for production below target levels n Providers receive incentive payments for production above target levels n Payouts on a quarterly basis n
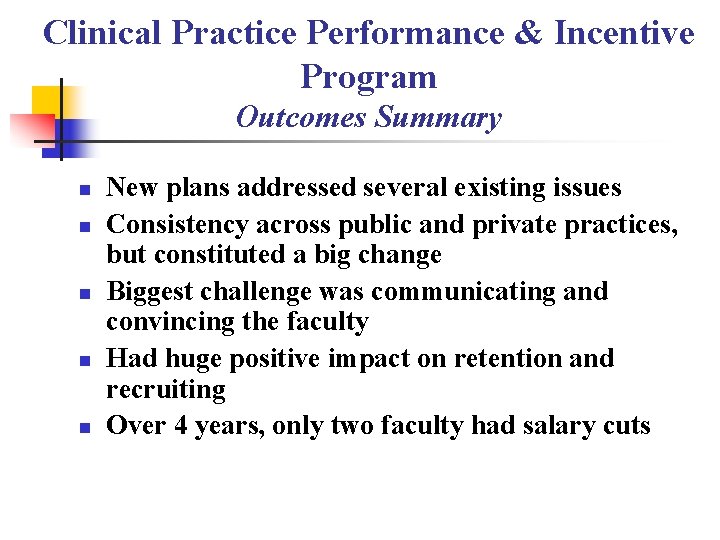
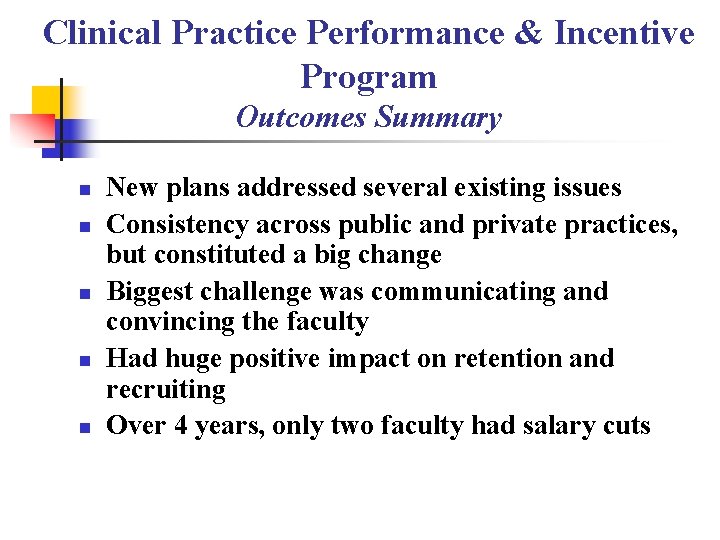
Clinical Practice Performance & Incentive Program Outcomes Summary n n n New plans addressed several existing issues Consistency across public and private practices, but constituted a big change Biggest challenge was communicating and convincing the faculty Had huge positive impact on retention and recruiting Over 4 years, only two faculty had salary cuts
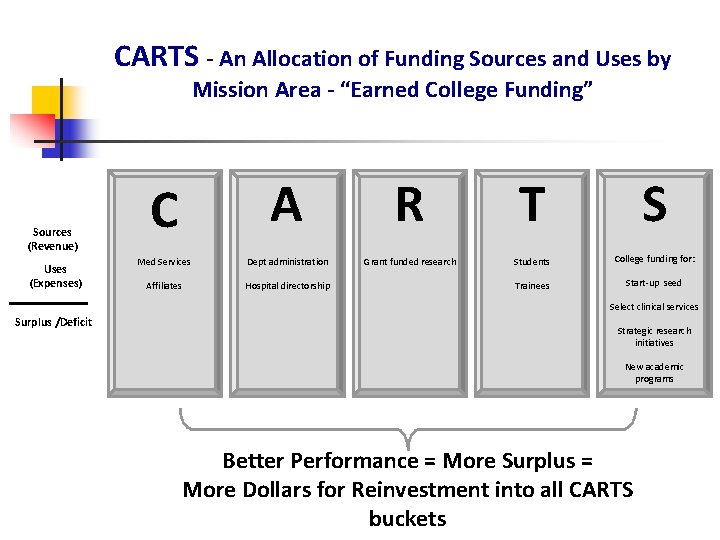
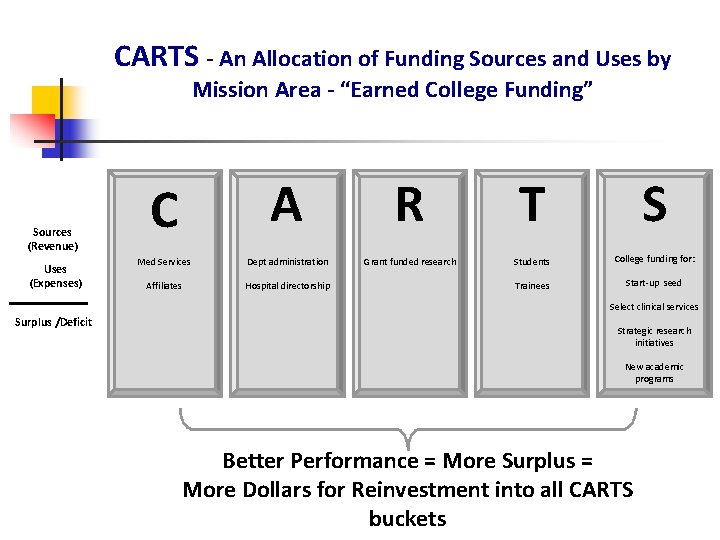
CARTS - An Allocation of Funding Sources and Uses by Mission Area - “Earned College Funding” Sources (Revenue) Uses (Expenses) A R T S Med Services Dept administration Grant funded research Students College funding for: Affiliates Hospital directorship Trainees Start-up seed C Select clinical services Surplus /Deficit Strategic research initiatives New academic programs Better Performance = More Surplus = More Dollars for Reinvestment into all CARTS buckets
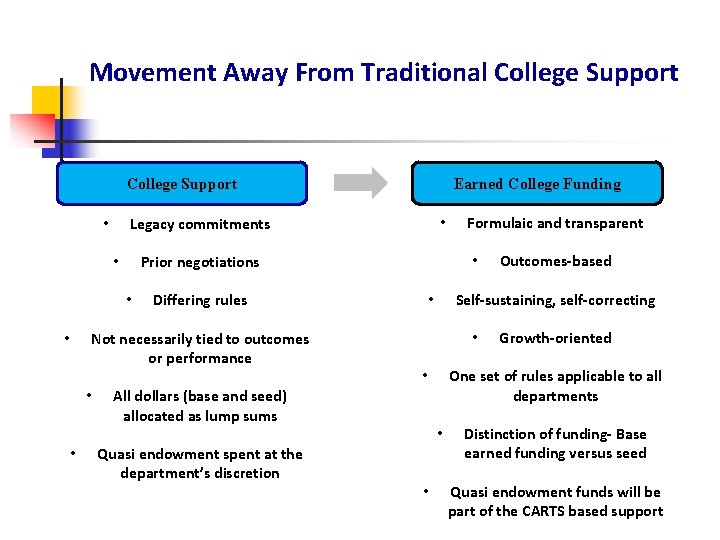
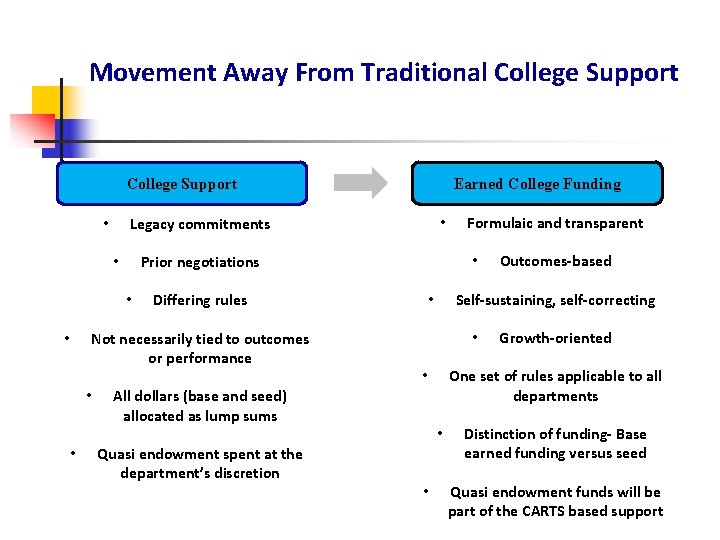
Movement Away From Traditional College Support • • • Quasi endowment spent at the department’s discretion • • Growth-oriented One set of rules applicable to all departments • All dollars (base and seed) allocated as lump sums Outcomes-based Self-sustaining, self-correcting • Differing rules Not necessarily tied to outcomes or performance Formulaic and transparent • Prior negotiations • • • Legacy commitments • • Earned College Funding Distinction of funding- Base earned funding versus seed Quasi endowment funds will be part of the CARTS based support
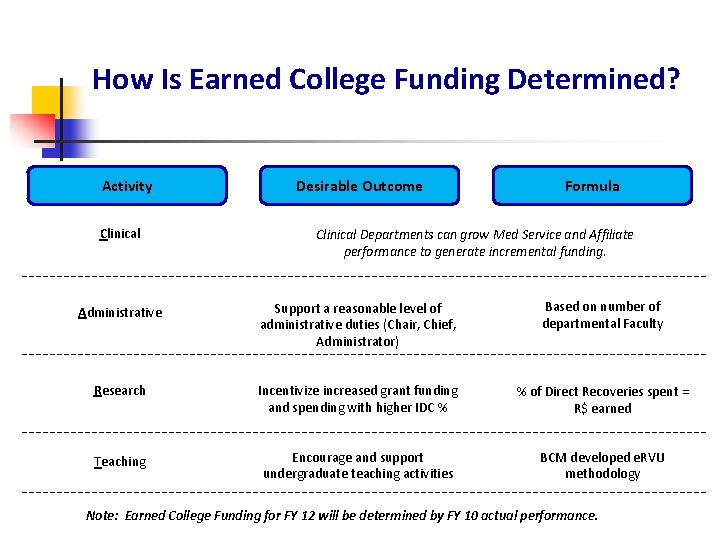
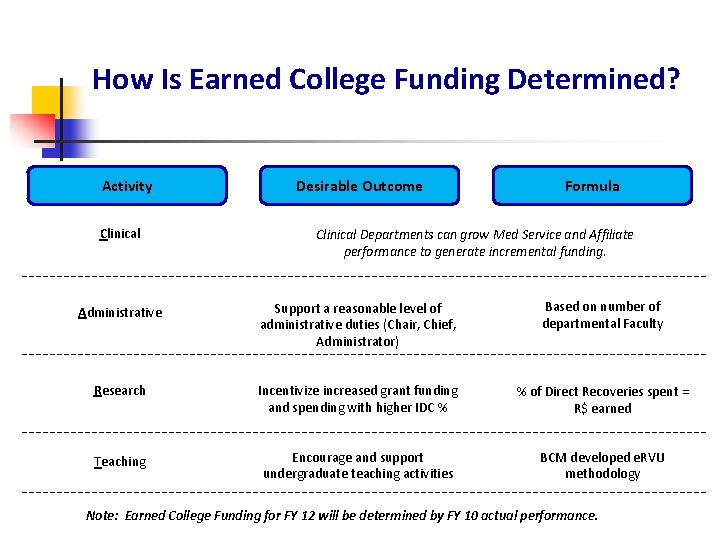
How Is Earned College Funding Determined? Activity Clinical Desirable Outcome Formula Clinical Departments can grow Med Service and Affiliate performance to generate incremental funding. Administrative Support a reasonable level of administrative duties (Chair, Chief, Administrator) Based on number of departmental Faculty Research Incentivize increased grant funding and spending with higher IDC % % of Direct Recoveries spent = R$ earned Teaching Encourage and support undergraduate teaching activities BCM developed e. RVU methodology Note: Earned College Funding for FY 12 will be determined by FY 10 actual performance.
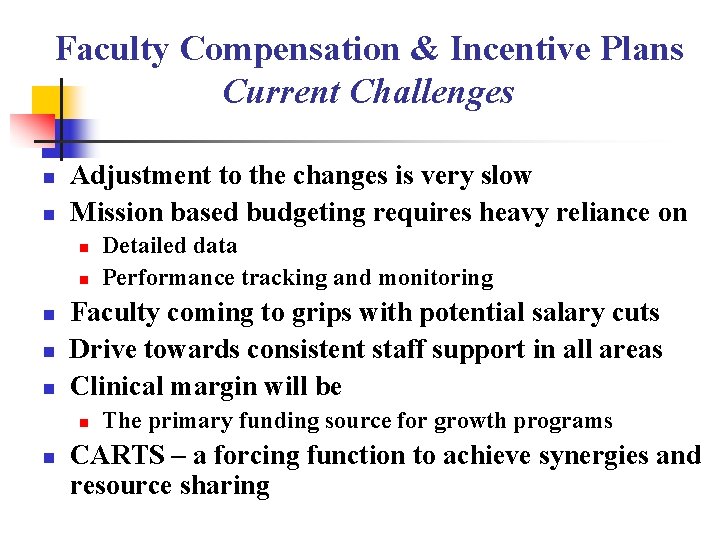
Faculty Compensation & Incentive Plans Current Challenges n n Adjustment to the changes is very slow Mission based budgeting requires heavy reliance on n n Faculty coming to grips with potential salary cuts Drive towards consistent staff support in all areas Clinical margin will be n n Detailed data Performance tracking and monitoring The primary funding source for growth programs CARTS – a forcing function to achieve synergies and resource sharing