Family Caregiving and Transitional Care A Critical Review







- Slides: 20
Family Caregiving and Transitional Care: A Critical Review Mary Jo Gibson, Kathleen Kelly, Alan Kaplan October 2012 Presentation of Findings: 2013 Annual Meeting American Society on Aging
Why We Did This Study • Transitions across health care settings, such as hospital to home, are fraught with risks for older adults and adults with disabilities • Family caregivers usually implement the care plans after release from the hospital but rarely are actively engaged in discharge planning • Transitions from hospital to home are receiving policy attention especially with current focus on reducing readmissions soon after hospitalization
How We Did This Study • Conducted a methodical review of the literature from 2000 to 2012 on “family (or informal) caregivers” and “care transistions”, “transitional care”, “discharge planning” on Pub. Med, MEDLINE, the Cochrane Database of Systematic Reveiws & the Journals of the GSA • Internet searches of publications by governmental, provider, health policy and consumer organizations to ensure currency

How We Did the Study, part 2 • Focused on seven transitional care programs identified as evidence-based transition interventions by CMS and ACL” • Five “Hospital to Home” care transitions programs: – – – Care Transitions Intervention (Coleman) Transitional Care Model (Naylor) BRIDGE Project RED Project BOOST • Two physician practice-based coordination programs: – Guided Care – GRACE
What We Found: Family Caregivers Receive Inadequate Support • Relatively sparse evidence on how caregivers perceive their own roles and needs • What is available indicates they do not receive adequate recognition or support during the discharge process from health care professionals
“Even when a caregiver was present, hospital staff frequently directed teaching exclusively toward the patient. For example, a nurse and patient sat sideby-side to review instructions; the highly motivated caregiver, seated across the room due to lack of space, was unable to see the written material. The integral role of caregivers in helping patients at home contrasted with their often peripheral role in in-hospital transition processes”. Carol H. Cain, 2012
What We Found: Family Caregiver Involvement Can Improve Patient Outcomes and Continuity of Care • The evidence base on how family caregiver involvement affects the quality of health care is expanding. • Their involvement has improved outcomes for persons with physical, mental and cognitive disorders, contributes to greater patient satisfaction, and improved continuity of care. • Evidence suggests that family caregivers should not be expected to provide complex medical care in the home, especially without training on in-home support from professionals

What We Found: Health Professionals are Increasingly Recognizing the Need to Work with Family Caregivers • Little research has been conducted on health care professionals perceptions of family caregivers roles and needs or on their communication with them. • However, leading physician, nursing, social work organizations have affirmed family caregivers’ contributions and the need to work in partnership with them

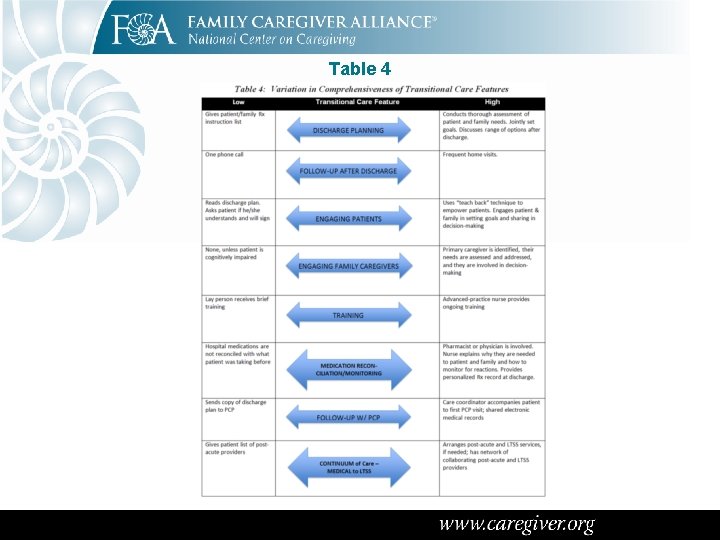
What We Found: Transitional Care Programs Vary in Key Features • Hospital to home programs all share some common characteristics: – Interaction with a designated staff person prior to and following discharge (phone, in-person) – Enhanced discharged planning – Medication reconciliation – Coordination with the PCP so that follow up visit is arranged – Improved provider to provider communication – Patient and caregiver education – Referrals to community resources
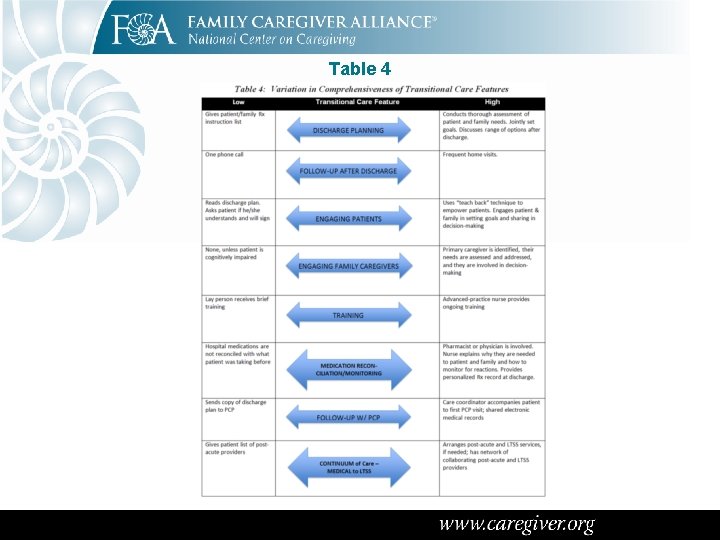
Table 4
What We Found: A Greater Focus on LTSS is Needed • Only a few of these programs place substantial emphasis on coordinating care with LTSS after release from the hospital • This part of the care continuum is essential for most of the “high risk” older adults on which the programs focus, and it is the part in which families play starring roles

What We Have Learned: Transitional Care Programs Vary in How Actively They Engage Family Caregivers • While 4 of the 7 transitional care programs reviewed offer specfic steps to actively engage family caregivers as partners, in the other three programs they are viewed more passively • In the latter, mention of family caregivers focuses on how they can help patients adhere to discharge instructions or medication regimens, not on how their expertise can be tapped to improve transitional care or how their needs as individuals should be assessed and addressed as part of effective discharge planning • Outcomes for family caregivers, such as reduction in stress, have been reported for only two of the programs

Table 6
What We Have Learned: New Teaching Guides and Programs Are Available but Often Not Accessible • Good methods of and tools for engaging family caregivers in transitional care exist but are not yet being used widely • A growing body of teaching programs, guides and checklists is becoming available to assist both patients and family caregivers during transitions • It is a challenge to make these materials easily usuable and available when needed, especially at the point of care – new digital technologies hold promise in this area
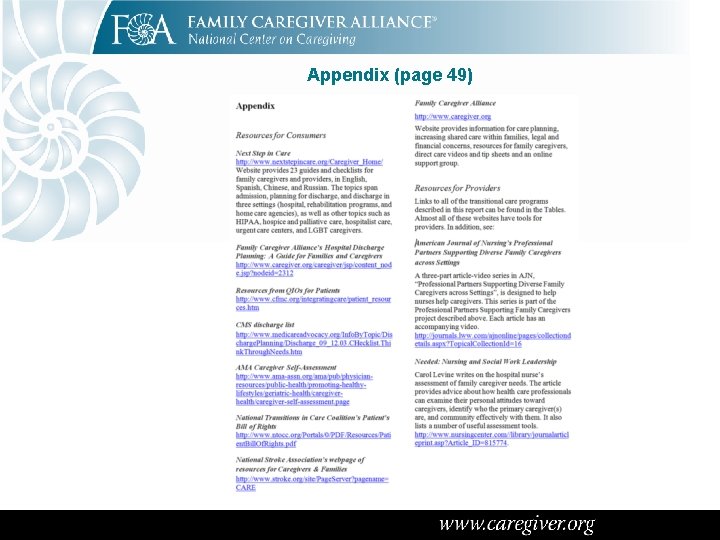
Appendix (page 49)

What We Have Learned: Barriers to Greater Engagement with Family Caregivers Should be Recognized • Financial pressures on hospitals to reduce length of stay mean patients are more complex at the point of discharge • Insufficient attention to arranging and integrating LTSS in health care delivery • Patient education materials written at a level that most patients and caregivers cannot understand • Reluctance of patients and families to ask questions for fear of being labeled “difficult” • Lack of awareness of discharge-related rights during transitions (such as “safe discharge”)
Recommendations 1. 2. 3. 4. 5. Adopt a patient and family-centered framework for transitional care Focus more attention on the needs of patients and family caregivers of diverse cultures, ethnicities and races. Fund the development of quality measures focused on family caregivers in transitional care. Enroll family caregivers in studies on transitional care that include measures of their needs and the outcomes they experience. Conduct more research on attitudes of healthcare professionals toward family caregivers and barriers they encounter while trying to improve transitional care processes and engage family caregivers.

Recommendations 6. Require primary care practices to demonstrate active engagement of patients and families in transitional care and quality improvement activities in order to qualify as a medical home. 7. Include information about family caregivers in the electronic medical record that transfers across settings. 8. Seeking meaningful responses by hospitals to the Medicare Conditions of Participation. 9. Change payment to support the engagement of patients and families. 10. Expand family caregiver engagement in new programs in the Affordable Care Act.
End Note Almost all of are or will be family caregivers who provide medical care and long-term services and supports, including implementing hospital discharge care plans. Family caregivers are a critical part of the solution.
Contact Information: National Center on Caregiving 785 Market Street Ste 750 San Francisco CA 94104 415. 434. 3388 Authors: Mary Jo Gibson mjgibson 100@gmail. com Kathleen Kelly kkelly@caregiver. org Alan Kaplan akkaplan@verizon. net A copy of the full report can be found on the FCA website: http: //www. caregiver. org/caregiver/jsp/content/pdfs/Fam. CGing_Trans. Care_Crit. Rvw_FINAL 10. 31. 2012. pdf
 Compassion fatigue vs burnout
Compassion fatigue vs burnout American association of caregiving youth
American association of caregiving youth Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Spaulding classification
Spaulding classification Torrance memorial transitional care unit
Torrance memorial transitional care unit Levels of health care primary secondary tertiary
Levels of health care primary secondary tertiary Slidetodoc.com
Slidetodoc.com Epithelial cells in urine images
Epithelial cells in urine images Transition and topic sentence
Transition and topic sentence Transitional words
Transitional words Transitional fossils
Transitional fossils Modes of glandular secretion
Modes of glandular secretion Thor approved rehab ga
Thor approved rehab ga Transitional signals
Transitional signals Dynamic postural assessment
Dynamic postural assessment Kinetic chain checkpoints
Kinetic chain checkpoints Stratified columnar
Stratified columnar Positioned between horizontal and vertical lines
Positioned between horizontal and vertical lines Simple cuboidal epithelium
Simple cuboidal epithelium Transitional medical assistance ohio
Transitional medical assistance ohio Evolution fact or fiction
Evolution fact or fiction