Falls Prevention during COVID Aida Wen MD Associate



- Slides: 28
Falls Prevention during COVID Aida Wen, MD Associate Professor Jan 2021
Patient Scenario • You get a call from Mr. Z’s wife that he just had a fall out in the garden today. Fortunately, he had no injuries, but was a bit shaken. This is his 2 nd fall since March 2020. He used to go out several times a week to visit friends. But he has stopped going out since the COVID pandemic started, and pretty much stays inside, except to do a little gardening with his wife in their small yard. He doesn’t want to go to the hospital or doctor’s office as it is too much trouble and due to COVID risk (12 steps down). He is 85 years old, and has a history of HTN, mild kidney disease, and a history of colon cancer 7 years ago. • How Can we do a Falls assessment, evaluation, and treatment? • How much of it can be done remotely?
Background Very Common: • 25% of older adults fall each year • 1/5 falls results in serious injury (Fractures, head trauma) • Every 20 min, an older adult dies from a fall • Leading cause of death from injury in persons >65 years old • Causes are Multifactorial

Relevance • Cost of falls is over $31 billion each year • Falls are associated with: • Increased use of medical services • Decline in functional status • Nursing home placement • Fear of Falling impacts well-being and psychosocial functioning. • PREVENTABLE!
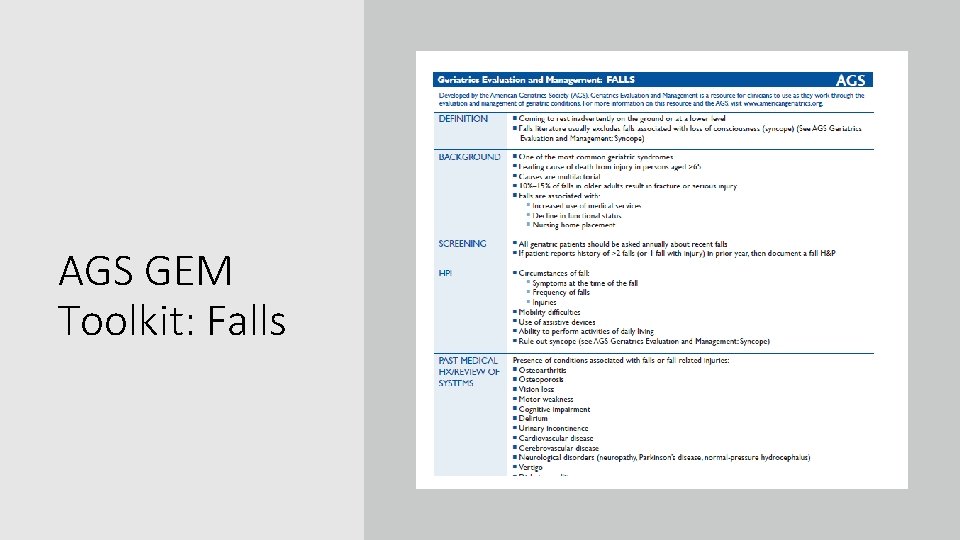
AGS GEM Toolkit: Falls

Get a Good Falls History • Circumstances • Symptoms, including syncope (fainting) • Frequency • Injuries • Mobility difficulties? • Use of assistive devices? • Include ADLs
Consider Medical Conditions that could be Fall Related • Vision Loss • Motor Weakness • Cognitive impairment • Urinary Incontinence • Stroke • Cardiac • Neurological disorders • Diabetes • Seizure disorders
Review Medications Thoroughly…including OTC • • • Beers Criteria STOPP/START Criteria Drug-Drug Interactions Antipsychotic meds Benzodiazepines Opioids Orthostatic Hypotension Hypoglycemia Proton Pump Inhibitors

• Alcohol • Social Support • Supervision Don’t Forget their Social History
Physical Exam with Special Focus: • Orthostatic Vitals (Drop in SBP> 20 mm. Hg) • Cognitive • Cardiac: HR, P • Gait: TUG • Balance: Berg • Strength evaluation • Neurological- reflexes, focal deficits, neuropathy, tremor, rigidity • Feet and footwear
Labs and Imaging • Basic Metabolic Profile (dehydration, hypoglycemia) • CBC (infection, anemia) • Vitamin D level • Vitamin B 12 level • BMD • Based on exam, consider: EKG, Neuroimaging, spine imaging
Additional Recommendations • Proper Footwear • Physical Therapy • PT with assistive device review for those who have fallen using an assistive device • Home safety evaluation for: • Potential environmental modifications: lighting, Bathmats, lower bed • Medical equipment: toilet riser, bedside commode, urinal, shower chair • Need for more assistance and supervision
Screening and Evaluation Amrik Sidhu, PT, DPT Genesis Rehab Services
Screening vs Evaluation • Screening • • • ‘Hands-off’ approach Questionnaire History (Medical Hx, Fall Hx) Information from family, nursing, etc Answer the Question: “Is an Evaluation Indicated? ” • Evaluation • • Use of Tests & Measures Thorough Examination/ Assessment Development of Treatment Plan (Plan of Care) Goals/ Outcomes
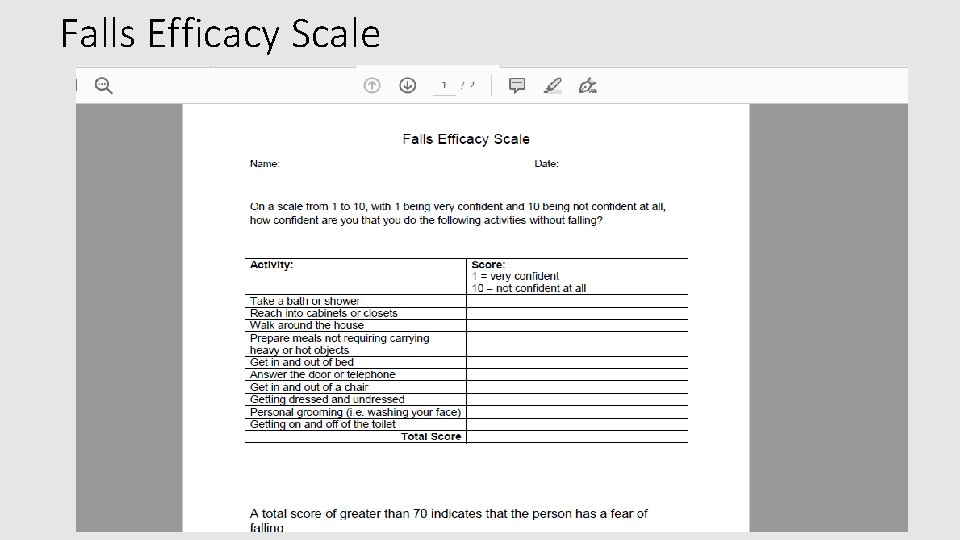
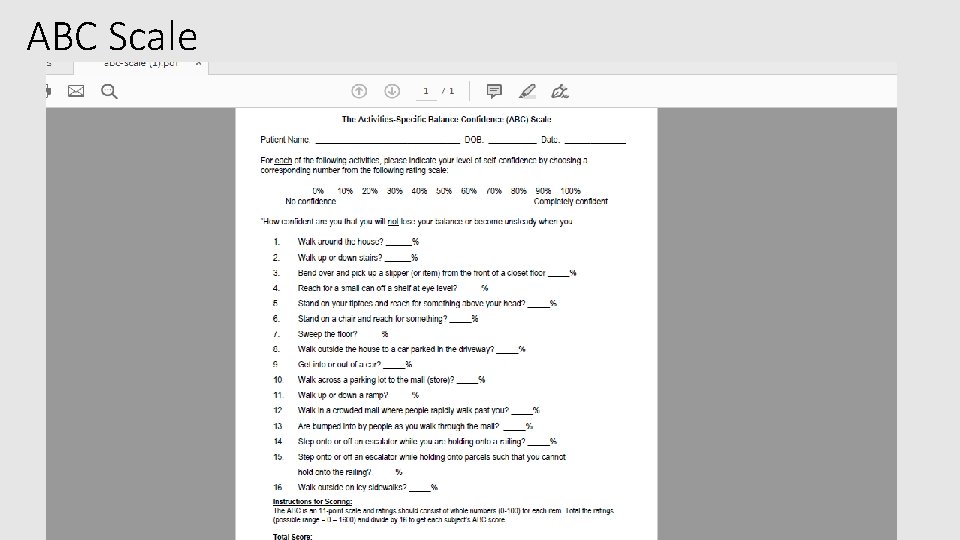
Screening Tools • Risk Factors • Fall History – Even 1 fall is predictive of Fall Risk • Cognitive/ Physical Impairments • Unsteady or Fear of Falling • 4 or more Medications • Fall Risk Questionnaires • Falls Efficacy Scale • ABC Scale (Activities-Specific Balance Confidence)
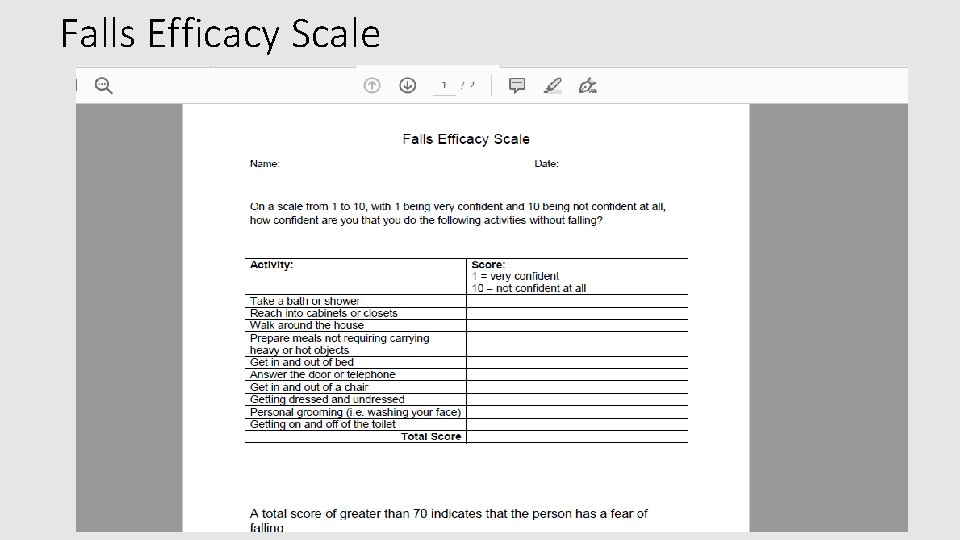
Falls Efficacy Scale
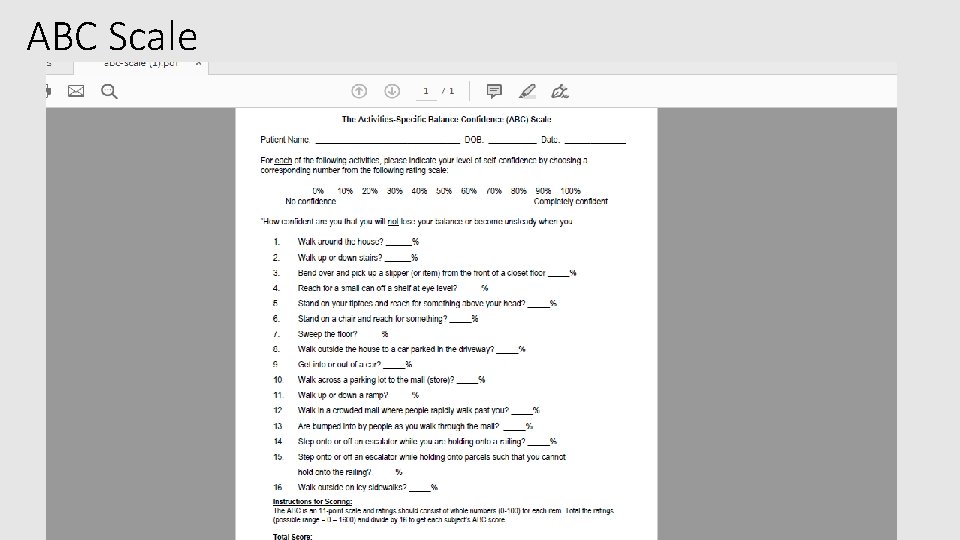
ABC Scale
Evaluation Tools • Questionnaires • Physical Assessments • Sit to Stand in 30 sec – STRENGTH ASSESSMENT • TUG (Timed up & go) – ADL ASSESSMENT • BERG – BALANCE ASSESSMENT • Other Balance Assessments: • Single Leg Stance • Functional Reach
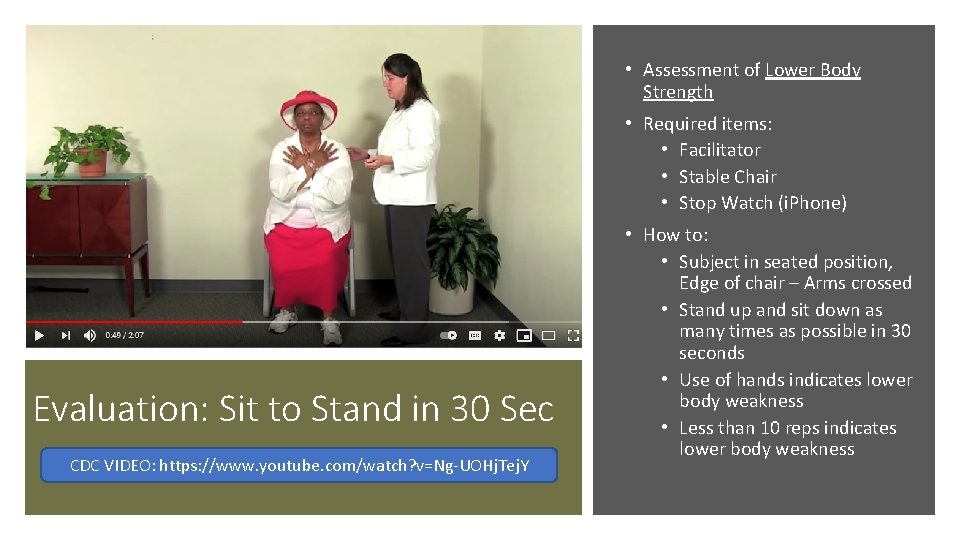
• Assessment of Lower Body Strength • Required items: • Facilitator • Stable Chair • Stop Watch (i. Phone) Evaluation: Sit to Stand in 30 Sec CDC VIDEO: https: //www. youtube. com/watch? v=Ng-UOHj. Tej. Y • How to: • Subject in seated position, Edge of chair – Arms crossed • Stand up and sit down as many times as possible in 30 seconds • Use of hands indicates lower body weakness • Less than 10 reps indicates lower body weakness
• Assessment of ability to perform ADL (Activities of Daily Living) • Required Items: • Facilitator • Stable Chair • Stop Watch • Measure 3 meters (9. 8 feet) • Use of Assistive Device (walker, cane) OK, but should be noted Evaluation: Timed Up and Go (TUG) CDC VIDEO: https: //www. youtube. com/watch? v=BA 7 Y_o. LEl. GY • How to: • From seated position, stand walk 3 meters, turn and sit (timed) • Less than 10 seconds indicates impairment
Evaluation: BERG Balance Test VIDEO: https: //www. youtube. com/watch? v=99 I 5009 HFk. I • Assessment of Balance • Required Items: • Two Standard Chairs • Yard Stick • Foot stool or Step • Stop Watch • How to: • 14 tasks (Transfer, Single leg stance, turns, etc) • Score 0 -4 on each item, Total of 56 • Score less than 45 indicates high risk for falls
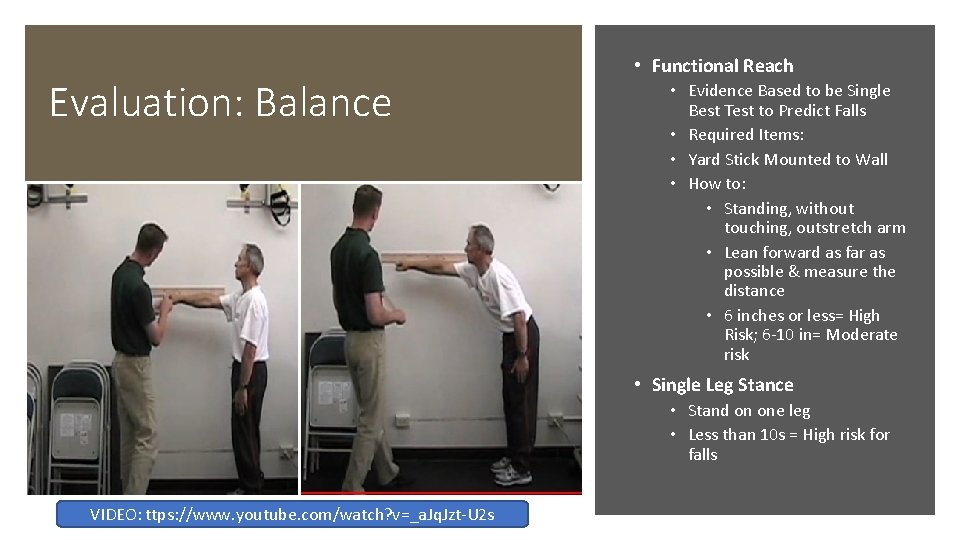
Evaluation: Balance • Functional Reach • Evidence Based to be Single Best Test to Predict Falls • Required Items: • Yard Stick Mounted to Wall • How to: • Standing, without touching, outstretch arm • Lean forward as far as possible & measure the distance • 6 inches or less= High Risk; 6 -10 in= Moderate risk • Single Leg Stance • Stand on one leg • Less than 10 s = High risk for falls VIDEO: ttps: //www. youtube. com/watch? v=_a. Jq. Jzt-U 2 s
Treatment: Function Based • Strength • Assessment to determine the Impairment (Drive Treatment Focus) • 60 -80% of 1 Rep Max, Roughly 12 Repetitions • Balance • Components: Visual, Somatosensory, Vestibular • Fall prevention strategies: Ankle, Hip, Stepping • Endurance • Determine what tasks need to be completed (Get to BR, Laundry, etc) • Gait/ Ambulation • Not effective treatment for balance, but is functional • Compensatory Strategies • Use of Assistive Devices: Walker, Cane, W/C, Bathroom DME, etc
Treatment Referral • Physical Therapy (PT) • Focus on Balance, Ambulation, Strengthening • Occupational Therapy (OT) • Focus on ADLs, Compensatory Strategies • Speech Language Pathologist (SLP) AKA “ST” • Cognitive Impairments, Expressive/ Receptive, Dysphagia • Home Health Referral • Must meet “Home-bound” Requirements • Outpatient Referral • Access to gym-based equipment
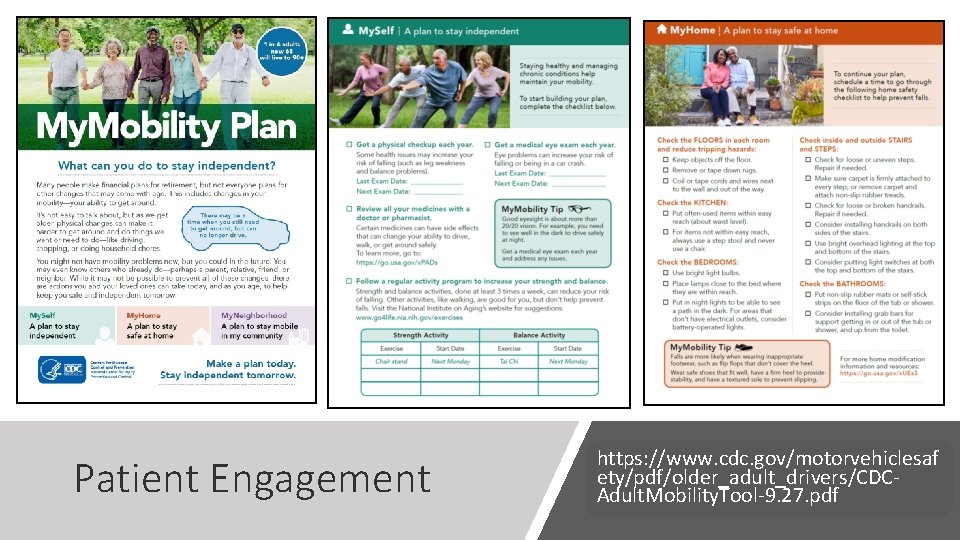
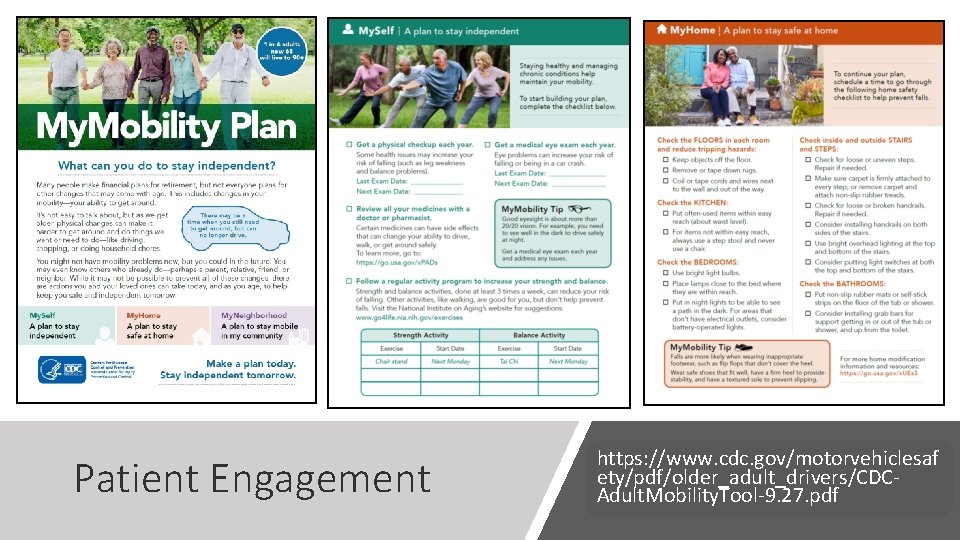
Patient Engagement https: //www. cdc. gov/motorvehiclesaf ety/pdf/older_adult_drivers/CDCAdult. Mobility. Tool-9. 27. pdf
Patient Scenario- revisited • You get a call from Mr. Z’s wife that he just had a fall out in the garden today. Fortunately, he had no injuries, but was a bit shaken. This is his 2 nd fall since March 2020. He used to go out several times a week to visit friends. But he has stopped going out since the COVID pandemic started, and pretty much stays inside, except to do a little gardening with his wife in their small yard. He doesn’t want to go to the hospital or doctor’s office as it is too much trouble (12 steps down) and due to COVID risk. He is 85 years old, and has a history of HTN, mild kidney disease, and a history of colon cancer 7 years ago. Your input?
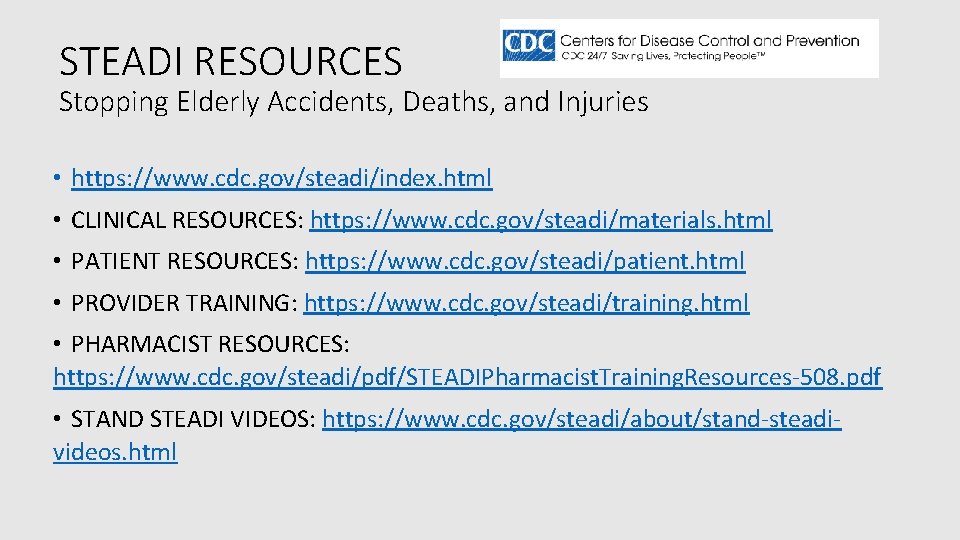
STEADI RESOURCES Stopping Elderly Accidents, Deaths, and Injuries • https: //www. cdc. gov/steadi/index. html • CLINICAL RESOURCES: https: //www. cdc. gov/steadi/materials. html • PATIENT RESOURCES: https: //www. cdc. gov/steadi/patient. html • PROVIDER TRAINING: https: //www. cdc. gov/steadi/training. html • PHARMACIST RESOURCES: https: //www. cdc. gov/steadi/pdf/STEADIPharmacist. Training. Resources-508. pdf • STAND STEADI VIDEOS: https: //www. cdc. gov/steadi/about/stand-steadivideos. html
OTHER RESOURCES Falls Efficacy Scale: https: //www. sralab. org/rehabilitation-measures/tinetti-falls-efficacyscale ABC Scale: https: //www. sralab. org/rehabilitation-measures/activities-specific-balanceconfidence-scale Sit to Stand 30 sec: https: //www. sralab. org/rehabilitation-measures/30 -second-sit-stand-test Timed up and Go (TUG): https: //www. sralab. org/rehabilitation-measures/timed-and-go BERG Balance: https: //www. sralab. org/rehabilitation-measures/berg-balance-scale Functional Reach: http: //www. hhvna. com/Functional_Reach_Test. pdf