Falls in Residential Care Dr Ludomyr Mykyta Consultant








- Slides: 24
Falls in Residential Care Dr Ludomyr Mykyta Consultant Geriatrician March 2018
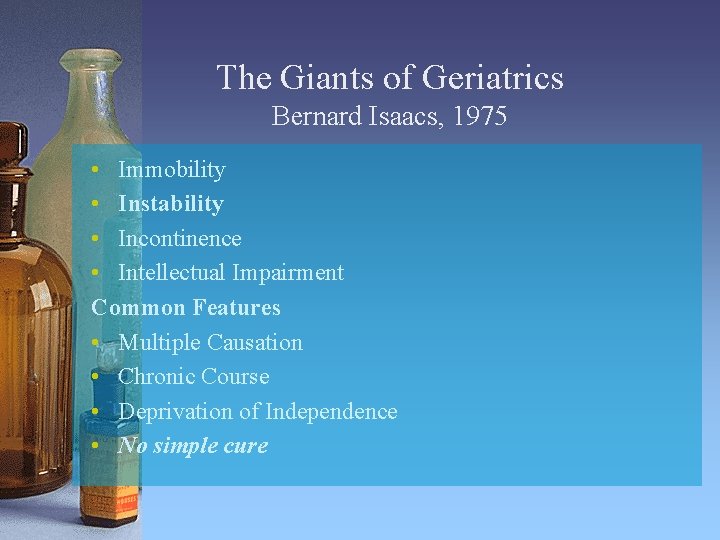
The Giants of Geriatrics Bernard Isaacs, 1975 • Immobility • Instability • Incontinence • Intellectual Impairment Common Features • Multiple Causation • Chronic Course • Deprivation of Independence • No simple cure
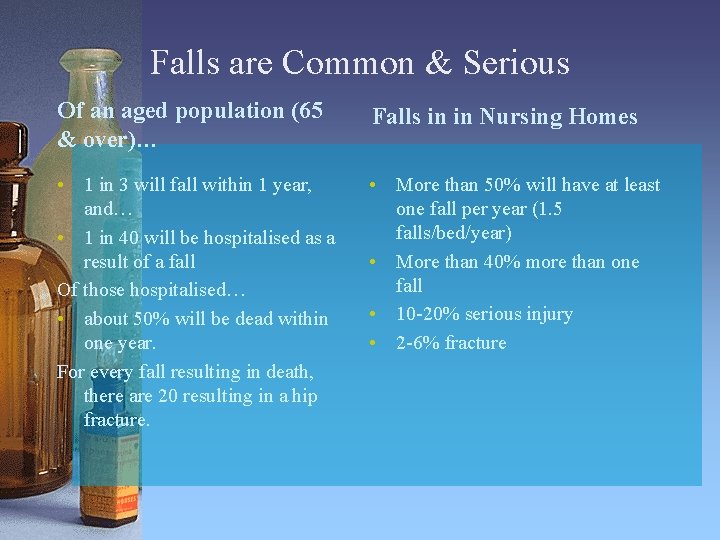
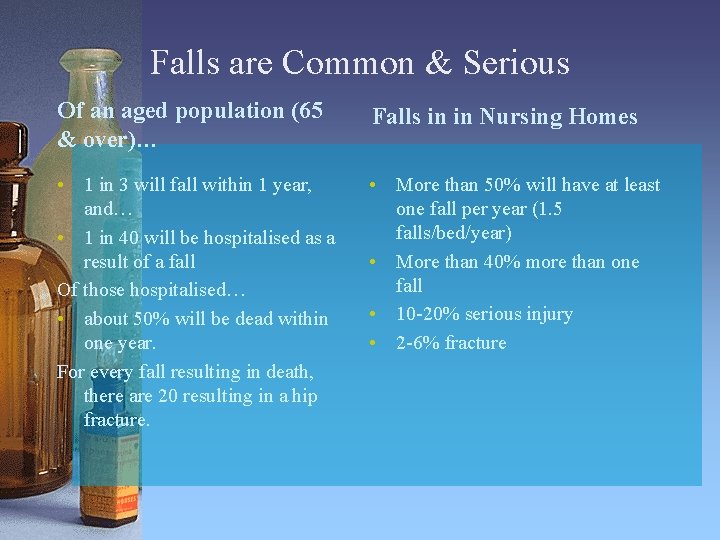
Falls are Common & Serious Of an aged population (65 & over)… Falls in in Nursing Homes • 1 in 3 will fall within 1 year, and… • 1 in 40 will be hospitalised as a result of a fall Of those hospitalised… • about 50% will be dead within one year. For every fall resulting in death, there are 20 resulting in a hip fracture. • More than 50% will have at least one fall per year (1. 5 falls/bed/year) • More than 40% more than one fall • 10 -20% serious injury • 2 -6% fracture

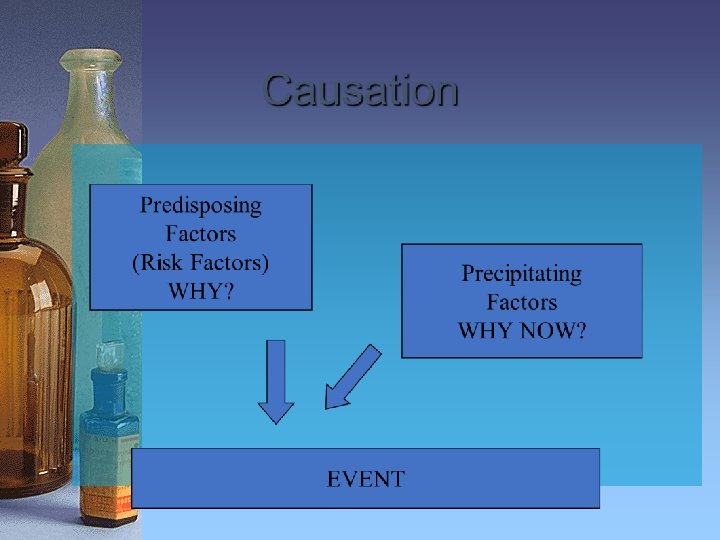
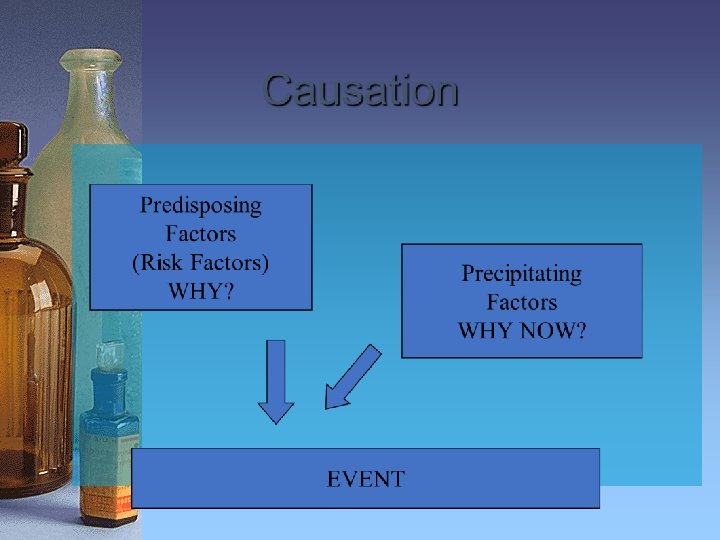
Causes of falls Known for many years • Intrinsic Risk Factors – Attributes of the person that predispose, increase vulnerability – Affecting the capacity to maintain a stable upright position both standing & moving • Extrinsic – Environmental factors that increase the risk of falling and the resultant injury • Mixed

HLC Residents A very special group The sickest & most • Very old disabled people in our • Multiple cocommunity morbidities • Multiple disabilities • Dementia
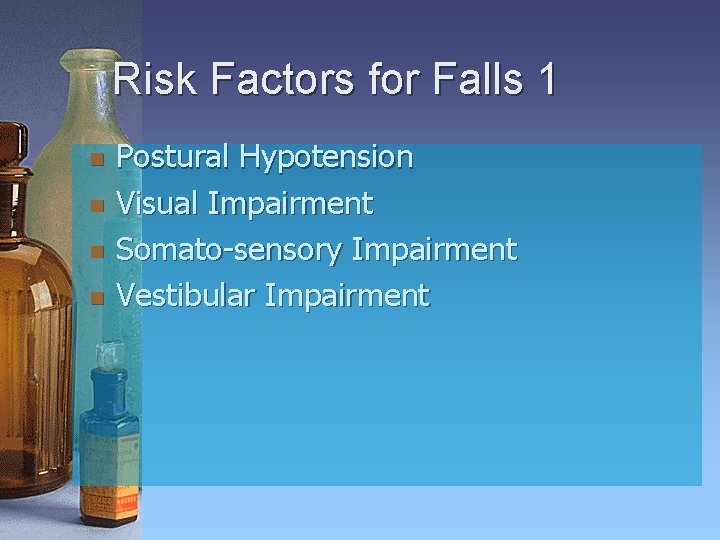
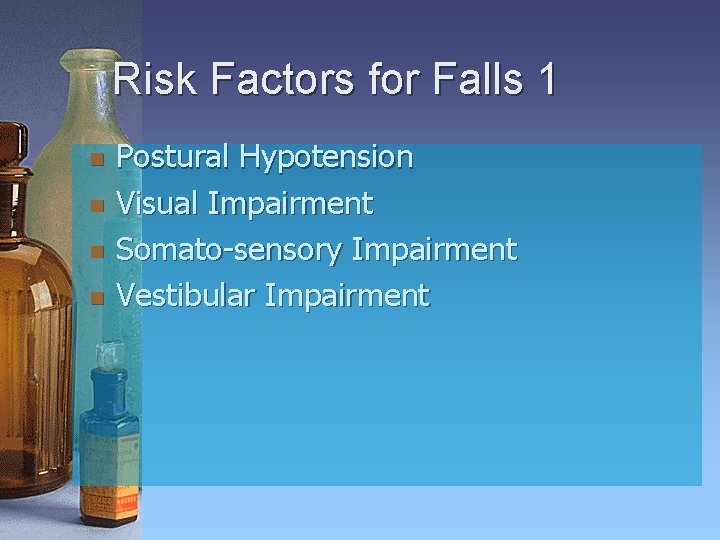
Risk Factors for Falls 1 n n Postural Hypotension Visual Impairment Somato-sensory Impairment Vestibular Impairment
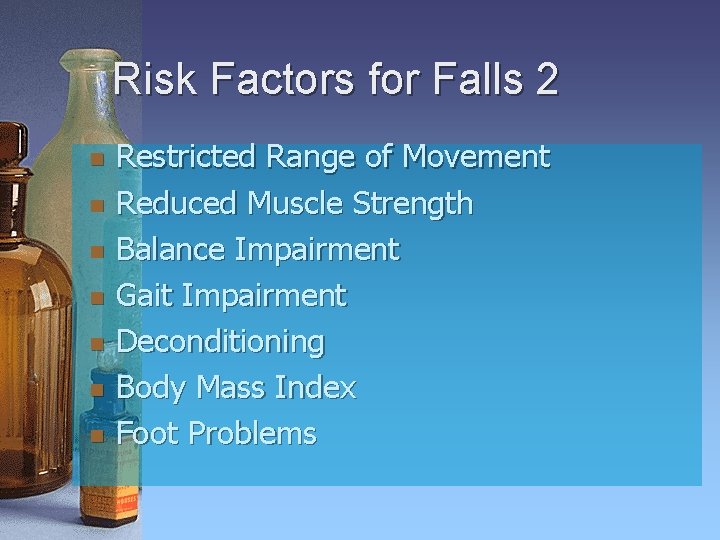
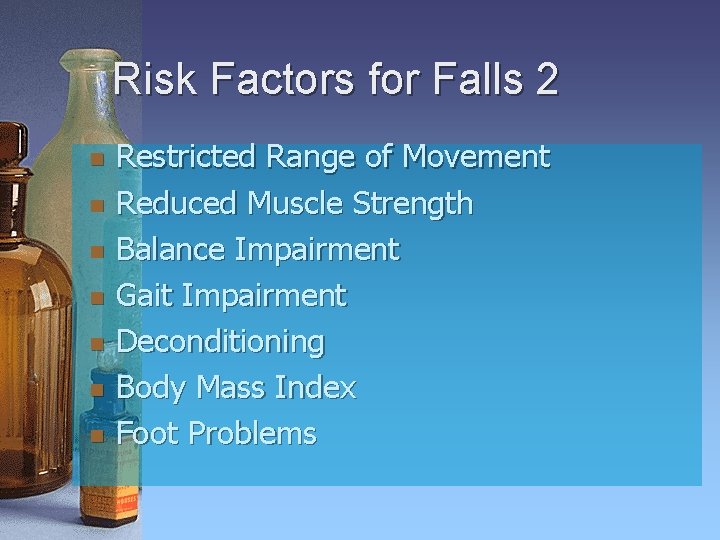
Risk Factors for Falls 2 n n n n Restricted Range of Movement Reduced Muscle Strength Balance Impairment Gait Impairment Deconditioning Body Mass Index Foot Problems
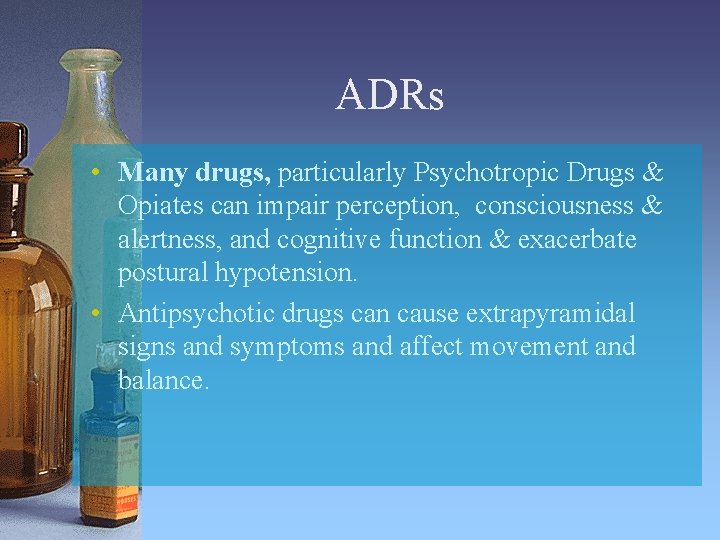
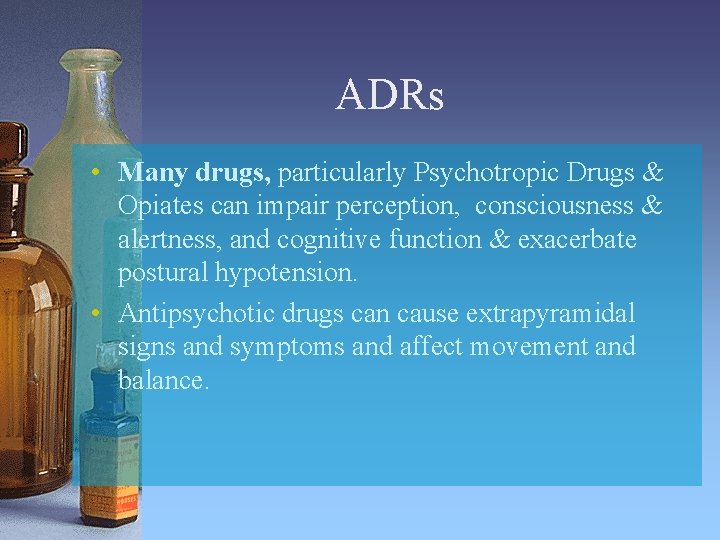
ADRs • Many drugs, particularly Psychotropic Drugs & Opiates can impair perception, consciousness & alertness, and cognitive function & exacerbate postural hypotension. • Antipsychotic drugs can cause extrapyramidal signs and symptoms and affect movement and balance.

Dementia The most disabling condition • Loss &/or impairment of Procedural Memory • Executive Dysfunction • Changes in Personality & Behaviour
Intellectual & Dysexecutive Changes • Loss of insight & Perception – Results from inability to make new memories – Inability to recognise that there is a problem – Misperceptions: Delusions & Hallucinations • Inability to reason • Impaired judgement & Inability to take probable consequences of an action into account • Inability to plan, sequence, and follow through a course of action, and/or Failure to complete assignments • Impaired problem solving skills • Inability to learn from errors
Changes in Personality and Behaviour • • • Loss of concentration & attention Lack of inhibition, Impulsivity, loss of impulse control, risk-taking Irascibility, verbal aggression Loss of empathy Apathy, lack of initiative and spontaneity
Risk Factors for Falls External/Extrinsic Hazards n n n n Access Barriers, Clutter Surfaces Pets Furniture Domestic work setting Illumination Safety Equipment

Home-like environment A HLC Facility is primarily a place of care. The architecture should facilitate delivery of care in a safe & effective manner, & the highest achievable level of independent function. “Home is where the heart is” a place shared with people we love & who love us. It is not a fairy-tale cottage. Relationships are more important than places.

People with dementia need surveillance & supervision • Adequate staffing levels in all categories • Technology • The architecture should enable rapid responses for those at highest risk • Privacy vs Safety

High risk fallers Common Problems • Deconditioning • Muscle weakness • Poor balance • Gait • Medication Responses • Increase fitness, strength and balance • Modify all risk factors present • Modify behaviour • Correct use of aids to mobility & ADL
Learning, Prevention, & Rehabilitation in Dementia • The brain runs on information, which is held in the memory stores. Memories are lost & decay & must be continually up-dated to be relevant. • The ability to learn, to make new memories is severely impaired in advanced dementia. • Procedural memories (doing complex things) are the most robust. They form “routines” that are accessed subconsciously. These routines are acquired through constant reinforcement. • All activities, individual & group, should be deliberately designed as part of the responses listed previously. • Physiotherapists & physical trainers are experts in these activities.

RGH(Daw Park) Rehabilitation Unit In the 1970 s every patient was provided with a “geriatric chair” adjusted to the individual, a personal walking aid, and had to wear correct footwear when up and about. All were taught how to rise from the chair, use the walking aid, & move off; & how to approach the chair and sit down. Every member of the staff who had contact with patients (including orderlies & cleaners: that is what team care is all about) was taught the same techniques, and deputised to make the patient repeat the actions if they were not done correctly at any time, day or night. Our outcomes & length of stay was commended by a formal rehabilitation unit review.
Caring in Residential Facilities • No matter who you are in the hierarchy, to be effective you must become a trusted friend of the resident, dedicated to the resident’s well-being. • You must be able to engage in all situations. • You may become the one that the resident looks to for advice and reassurance, & the conduit for communication with other elements of the team, which is always headed by the resident’s partner or relative.
Use of medication in dementia Alter the course of the dementia: stop or slow progression Treat and prevent the psychiatric disorders: Psychosis, Anxiety & PTSD, Depression. Promote engagement & Manage behavioural problems in conjunction with non-pharmacological methods
Prescribing Rules – A Reminder • Diagnosis • Clear Indications/Treatment Goals – Do a “risk-benefit” analysis • Pharmacology – Understand the pharmacology and ADR profile – Anticipate ADRs – Don’t panic, the S/E may be transient • Dose – “Start low, go slow”, but get to a therapeutic level! • Regimen – The simpler, the better – Minimise PRN (Pro Re Nata – as needed)
What and when is Palliative Care? The Context “Palliative care is the active total care of patients whose disease is not responsive to curative treatment…the goal of palliative care is the achievement of the best possible quality of life for patients and their families”. WHO Palliative does not mean nihilistic: “For those near the end of life, physicians have a moral & ethical obligation to provide comfort and dignity”.

Goals of Palliative Care • Attending to suffering and distress in all domains: � Biological and Physical � Psychological and Emotional � Social and Interpersonal � Spiritual and Religious � Intellectual and Professional � Safety & Security � The best Quality of Life attainable in the circumstances � When all else is gone the most precious thing we have is relationships
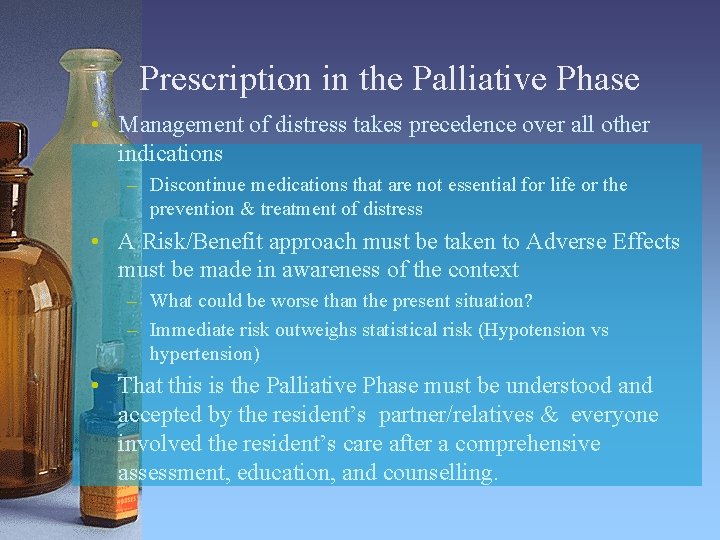
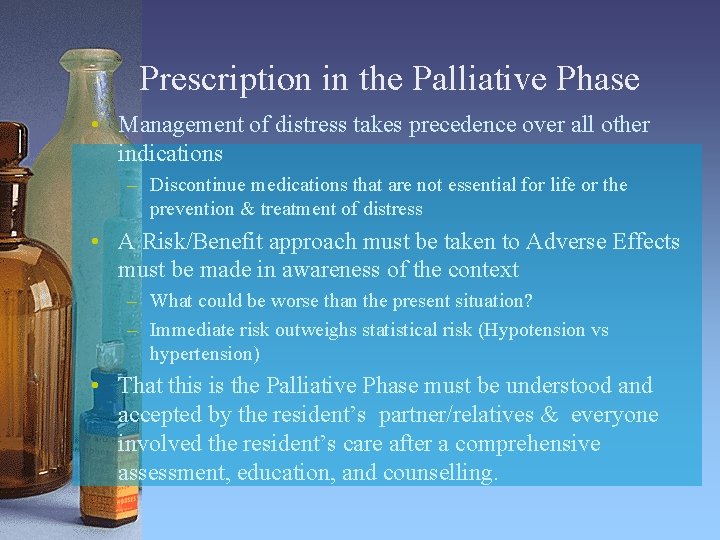
Prescription in the Palliative Phase • Management of distress takes precedence over all other indications – Discontinue medications that are not essential for life or the prevention & treatment of distress • A Risk/Benefit approach must be taken to Adverse Effects must be made in awareness of the context – What could be worse than the present situation? – Immediate risk outweighs statistical risk (Hypotension vs hypertension) • That this is the Palliative Phase must be understood and accepted by the resident’s partner/relatives & everyone involved the resident’s care after a comprehensive assessment, education, and counselling.
 Haccp flow chart complex food preparation
Haccp flow chart complex food preparation Theories about group living
Theories about group living Primary secondary and tertiary health care
Primary secondary and tertiary health care Green world management
Green world management Verizon ip centrex
Verizon ip centrex Court security consultant
Court security consultant Scan based trading consultant
Scan based trading consultant Consultant mediu
Consultant mediu Philips talent acquisition
Philips talent acquisition Wireless communication consultant
Wireless communication consultant Consultant contract 2003
Consultant contract 2003 Classroom management consultant
Classroom management consultant Ovtopodump
Ovtopodump Microsoft flow consultant
Microsoft flow consultant Internet consultant job description
Internet consultant job description Rcem consultant sign off
Rcem consultant sign off Drive.google
Drive.google Epicor configurator demo
Epicor configurator demo New consultant in casualty
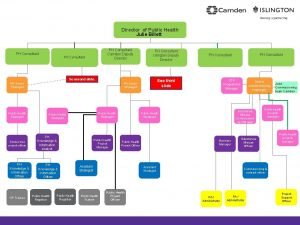
New consultant in casualty Julie billett public health
Julie billett public health Mrs rajlaxmi is working
Mrs rajlaxmi is working United states lactation consultant association
United states lactation consultant association Partner technical consultant
Partner technical consultant A department store decides to use secret shoppers
A department store decides to use secret shoppers New consultant training
New consultant training