Fall Prevention Remote Video Monitoring UT TYLER NURS




- Slides: 16

Fall Prevention: Remote Video Monitoring UT TYLER NURS 5382. 060
Summary of Project Patient safety is a top priority Falls in the acute care setting are a challenge 1: 1 sitter is costly for healthcare organizations Technology has introduced Remote Video Monitoring 1: 12 Video Monitor Technician (VMT) ratio
Rationale for Project To reduce the occurrence of falls Evidence‐Based Practice interventions have been implemented Falls are continually occurring Patient outcomes after a fall
To implement Remote Video Monitoring in the following capacities: • Safely • Cost effective • Staff efficient
Literature Synthesis Reduction in falls through video monitoring: Vortuba, L. et al. (2016) – 35% reduction in falls with video monitoring Sand‐Jecklin, K. R. , Johnson, J. , & Tylka, S. (2016) – Pre video monitoring: 74 falls on 4 units Post video monitoring: 15 falls on 4 units Cournan, M. , Fusco‐Gessick, B. , & Wright, L. (2018)– Falls decreased from 97 to 65 Cook, N. , Komansky, B. , Urton, M. (2020) – 27% decrease in falls Burtson, P. , & Vento, L. (2015) – 57 falls prevented during first three months with video monitoring
Chief Nursing Officer Nursing Administration Financial Information Technology Risk Management and Patient Privacy Officer Security Falls Committee Clinical Nurse Managers and Leads Bedside Nurses Clinical Education
Implementation Plan 311‐bed acute care facility Engagement of stakeholders Creating of workflows Determination of equipment ordering Identifying possible barriers Resources necessary for implementation
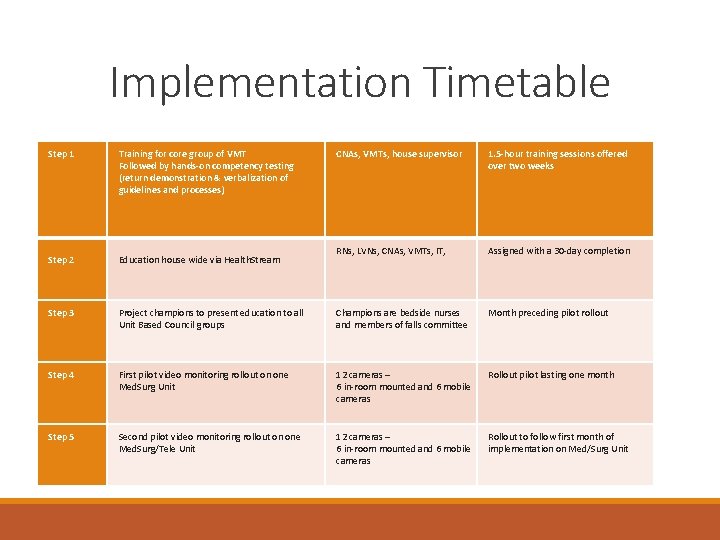
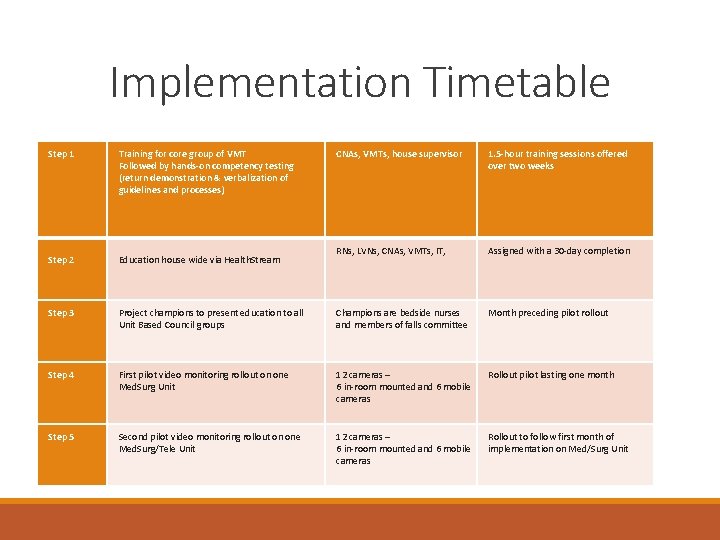
Implementation Timetable Step 1 Training for core group of VMT Followed by hands-on competency testing (return demonstration & verbalization of guidelines and processes) CNAs, VMTs, house supervisor 1. 5 -hour training sessions offered over two weeks Step 2 Education house wide via Health. Stream RNs, LVNs, CNAs, VMTs, IT, Assigned with a 30‐day completion Step 3 Project champions to present education to all Unit Based Council groups Champions are bedside nurses and members of falls committee Month preceding pilot rollout Step 4 First pilot video monitoring rollout on one Med. Surg Unit 12 cameras – 6 in‐room mounted and 6 mobile cameras Rollout pilot lasting one month Step 5 Second pilot video monitoring rollout on one Med. Surg/Tele Unit 12 cameras – 6 in‐room mounted and 6 mobile cameras Rollout to follow first month of implementation on Med/Surg Unit
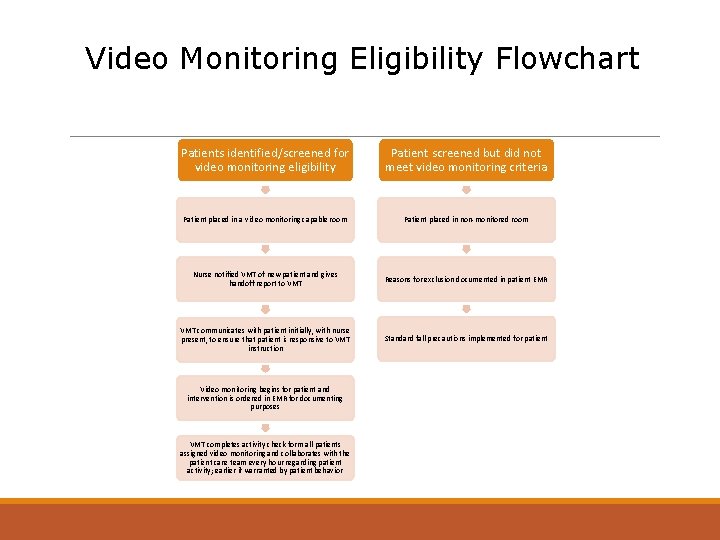
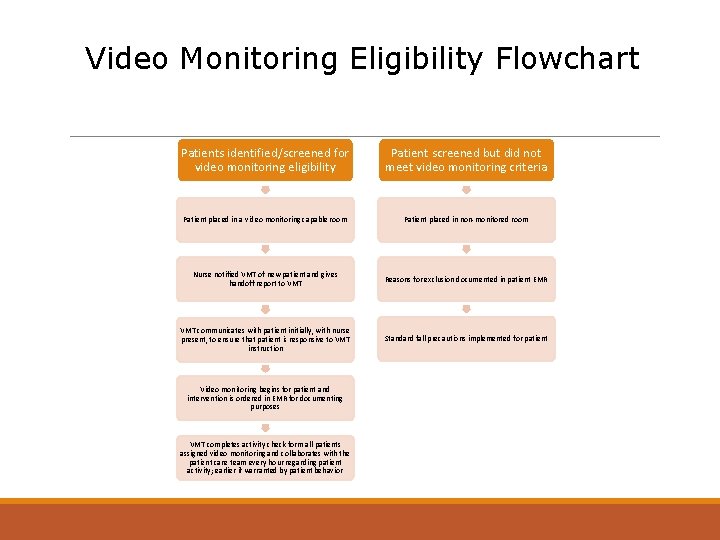
Video Monitoring Eligibility Flowchart Patients identified/screened for video monitoring eligibility Patient screened but did not meet video monitoring criteria Patient placed in a video monitoring capable room Patient placed in non‐monitored room Nurse notified VMT of new patient and gives handoff report to VMT Reasons for exclusion documented in patient EMR VMT communicates with patient initially, with nurse present, to ensure that patient is responsive to VMT instruction Standard fall precautions implemented for patient Video monitoring begins for patient and intervention is ordered in EMR for documenting purposes VMT completes activity check form all patients assigned video monitoring and collaborates with the patient care team every hour regarding patient activity; earlier if warranted by patient behavior

§ Vigi. Lanz § Fall data collected for a fiscal year § Cost of services § Cost of litigation

Annual sitter cost = $490, 374 Total project cost = $556, 435 First Year loss = $66, 061 Annual cost of program = $113, 250

Discussion/Recommendations The creation of additional care capacities Patient Safety through: • Fall prevention with video monitoring • Reduction of in room sitters • Return on investment
References Burtson, P. L. , & Vento, L. (2015). Sitter reduction through mobile video monitoring: A nurse‐driven sitter protocol and administrative oversight. JONA: The Journal of Nursing Administration, 45(7/8), 363 ‐ 369. Bernocchi, P. , Giordano, A. , Pintavalle, G. , Galli, T. , Ballini Spoglia, E. , Baratti, D. , & Scalvini, S. (2019). Feasibility and Clinical Efficacy of a Multidisciplinary Home‐Telehealth Program to Prevent Falls in Older Adults: A Randomized Controlled Trial. Journal of the American Medical Directors Association, 20(3), 340– 346. https: //doi‐org. ezproxy. uttyler. edu/10. 1016/j. jamda. 2018. 09. 003 Cook, N. , Komansky, B. , & Urton, M. (2020). Do no harm: A multifactorial approach to preventing emergency department falls‐‐a quality improvement project. Journal of Emergency Nursing. 46(5). 666‐ 674. https: //doi. org/10. 1016/j. jen. 2020. 03. 007 Cournan, M. , Fusco‐Gessick, B. , & Wright, L. (2018). Improving patient safety through video monitoring. Rehabilitation Nursing, 43(2), 111.
References Davis, J. , Kutash, M. , Whyte, J. (2016). A comparative study of patient sitters with video monitoring versus in‐room sitters. The Journal of Nursing Education and Practice, 7(3), 137‐ 142. doi: 10. 5430/jnep. v 7 n 3 p 137 Gringauz, I. , Shemesh, Y. , Dagan, A. , Israelov, I. , Feldman, D. , Pelz‐Sinvani, N. , Justo, D. , & Segal, G. (2017). Risk of falling among hospitalized patients with high modified Morse scores could be further Stratified. BMC Health Services Research, 17, 1– 7. https: //doi‐org. ezproxy. uttyler. edu/10. 1186/s 12913 ‐ 017‐ 2685‐ 2 Lerdal, A. , Sigurdsen, L. W. , Hammerstad, H. , Granheim, T. I. , Risk Study Research Group, & Gay, C. L. (2018). Associations between patient symptoms and falls in an acute care hospital: A cross‐sectional study. Journal of Clinical Nursing (John Wiley & Sons, Inc. ), 27(9– 10), 1826– 1835. https: //doi‐ org. ezproxy. uttyler. edu/10. 1111/jocn. 14364
References Lucero, R. J. , Lindberg, D. S. , Fehlberg, E. A. , Bjarnadottir, R. I. , Li, Y. , Cimiotti, J. P. , Crane, M. , & Prosperi, M. (2019). A data‐driven and practice‐based approach to identify risk factors associated with hospital‐acquired falls: Applying manual and semi‐ and fully‐automated methods. International Journal of Medical Informatics, 122, 63– 69. https: //doi‐ org. ezproxy. uttyler. edu/10. 1016/j. ijmedinf. 2018. 11. 006 Melnyk, B. M. , & Fineout‐Overholt, E. (2015). Models to guide implementation and sustainability of evidence‐based practice. In D. Dang, B. M. Melnyk, E. Fineout‐Overholt, D. Ciliska, A. Di. Censo, L. Cullen, M. Cvach, J. Larrabee, J. Rycroft‐Malone, A. Schultz, C. Stetler, & K. Stevens (Eds. ), Evidencebased practice in nursing & healthcare: A guide to best practice. (p. 289‐ 294). Philadelphia, PA: Wolters Kluwer. Melnyk, B. M. , & Fineout‐Overholt, E. (2015). Implementing evidence in clinical settings. In M. Hockenberry, T. Brown, & C. Rodgers (Eds. ), Evidence-based practice in nursing & healthcare: A guide to best practice. (p. 289‐ 294). Philadelphia, PA: Wolters Kluwer. Rheaume, J. , Fruh, S. (2015). Retrospective case reviews of adult inpatient falls in the acute care setting. MEDSURG Nursing, 24(5), 318– 324.
References Sand‐Jecklin, K. , Johnson, J. , Tringhese, A. , Daniels, C. , & White, F. (2018). Video Monitoring for Fall Prevention and Patient Safety: Process Evaluation and Improvement. Journal of Nursing Care Quality, 34(2), 145‐ 150. Sand‐Jecklin, K. R. , Johnson, J. , & Tylka, S. (2016). Protecting Patient Safety: Can Video Monitoring Prevent Falls in High‐Risk Patient Populations? Journal of Nursing Care Quality, 31(2), 131‐ 138. Tzeng, H. ‐M. , & Yin, C. ‐Y. (2017). A multihospital survey on effective interventions to prevent hospital falls in adults. Nursing Economic$, 35(6), 304– 313 Votruba, L. , Graham, B. , Wisinski, J. , & Syed, A. (2016). Video monitoring to reduce falls and patient companion costs for adult inpatients. Nursing Economic$, 34(4), 185– 189.