Fall Prevention in a Neurosurgery Clinic DNP Student
- Slides: 1
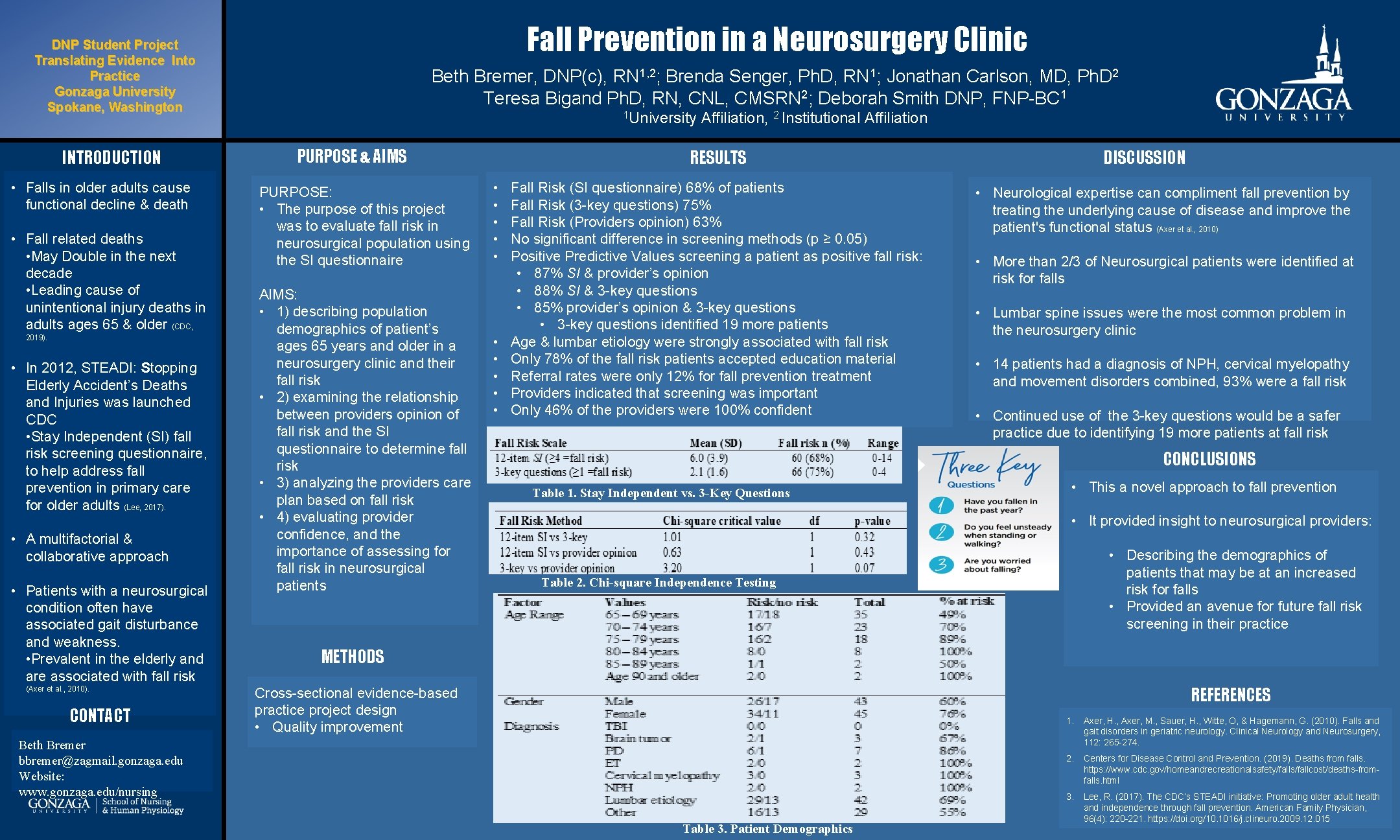
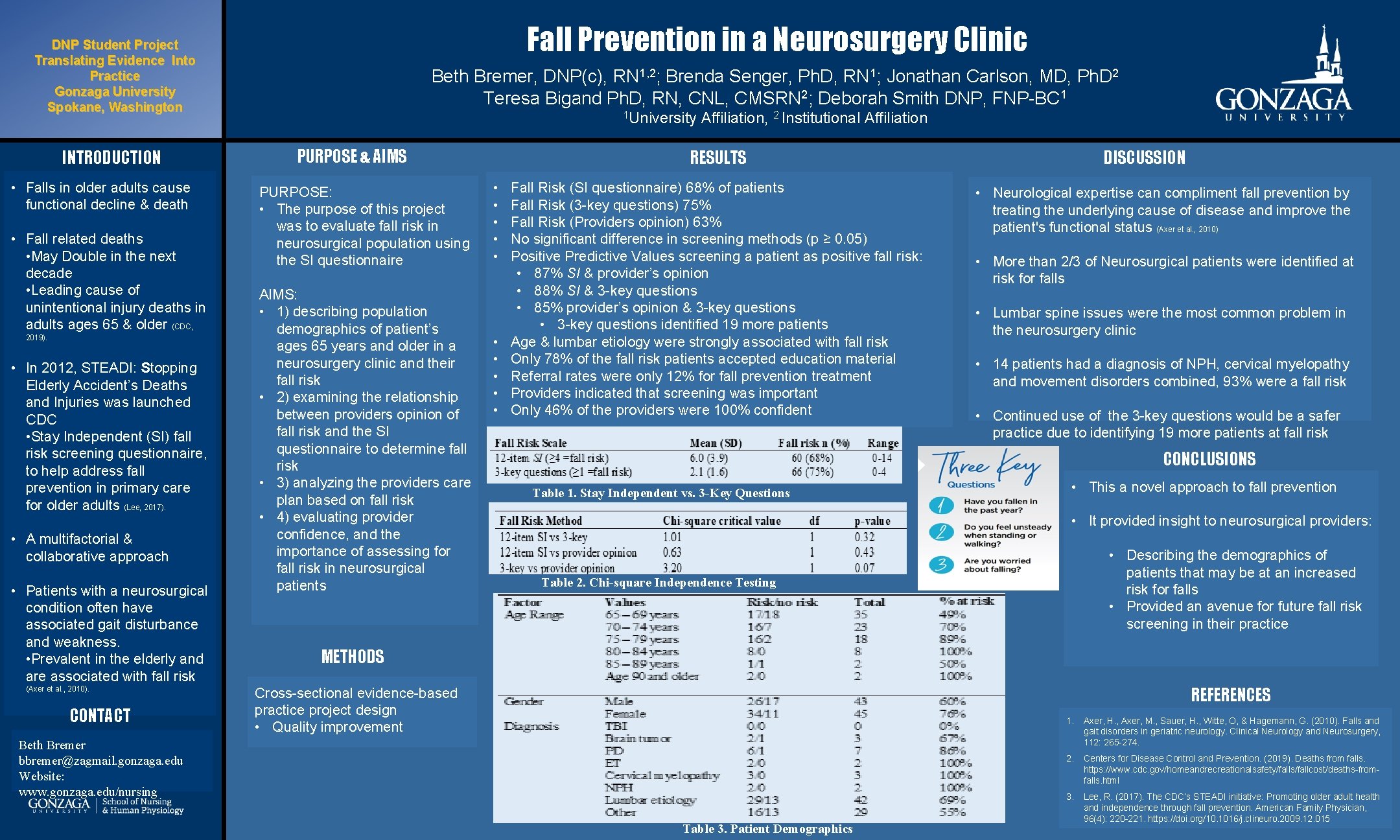
Fall Prevention in a Neurosurgery Clinic DNP Student Project Translating Evidence Into Practice Gonzaga University Spokane, Washington INTRODUCTION • Falls in older adults cause functional decline & death • Fall related deaths • May Double in the next decade • Leading cause of unintentional injury deaths in adults ages 65 & older (CDC, 2019). • In 2012, STEADI: Stopping Elderly Accident’s Deaths and Injuries was launched CDC • Stay Independent (SI) fall risk screening questionnaire, to help address fall prevention in primary care for older adults (Lee, 2017). • A multifactorial & collaborative approach • Patients with a neurosurgical condition often have associated gait disturbance and weakness. • Prevalent in the elderly and are associated with fall risk (Axer et al. , 2010). CONTACT Beth Bremer, DNP(c), RN 1, 2; Brenda Senger, Ph. D, RN 1; Jonathan Carlson, MD, Ph. D 2 Teresa Bigand Ph. D, RN, CNL, CMSRN 2; Deborah Smith DNP, FNP-BC 1 1 University PURPOSE & AIMS PURPOSE: • The purpose of this project was to evaluate fall risk in neurosurgical population using the SI questionnaire AIMS: • 1) describing population demographics of patient’s ages 65 years and older in a neurosurgery clinic and their fall risk • 2) examining the relationship between providers opinion of fall risk and the SI questionnaire to determine fall risk • 3) analyzing the providers care plan based on fall risk • 4) evaluating provider confidence, and the importance of assessing for fall risk in neurosurgical patients Affiliation, 2 Institutional Affiliation RESULTS • • • Fall Risk (SI questionnaire) 68% of patients Fall Risk (3 -key questions) 75% Fall Risk (Providers opinion) 63% No significant difference in screening methods (p ≥ 0. 05) Positive Predictive Values screening a patient as positive fall risk: • 87% SI & provider’s opinion • 88% SI & 3 -key questions • 85% provider’s opinion & 3 -key questions • 3 -key questions identified 19 more patients Age & lumbar etiology were strongly associated with fall risk Only 78% of the fall risk patients accepted education material Referral rates were only 12% for fall prevention treatment Providers indicated that screening was important Only 46% of the providers were 100% confident DISCUSSION • Neurological expertise can compliment fall prevention by treating the underlying cause of disease and improve the patient's functional status (Axer et al. , 2010) • More than 2/3 of Neurosurgical patients were identified at risk for falls • Lumbar spine issues were the most common problem in the neurosurgery clinic • 14 patients had a diagnosis of NPH, cervical myelopathy and movement disorders combined, 93% were a fall risk • Continued use of the 3 -key questions would be a safer practice due to identifying 19 more patients at fall risk CONCLUSIONS Table 1. Stay Independent vs. 3 -Key Questions • This a novel approach to fall prevention • It provided insight to neurosurgical providers: • Describing the demographics of patients that may be at an increased risk for falls • Provided an avenue for future fall risk screening in their practice Table 2. Chi-square Independence Testing METHODS REFERENCES Cross-sectional evidence-based practice project design • Quality improvement Beth Bremer bbremer@zagmail. gonzaga. edu Website: www. gonzaga. edu/nursing Table 3. Patient Demographics 1. Axer, H. , Axer, M. , Sauer, H. , Witte, O, & Hagemann, G. (2010). Falls and gait disorders in geriatric neurology. Clinical Neurology and Neurosurgery, 112: 265 -274. 2. Centers for Disease Control and Prevention. (2019). Deaths from falls. https: //www. cdc. gov/homeandrecreationalsafety/falls/fallcost/deaths-fromfalls. html 3. Lee, R. (2017). The CDC’s STEADI initiative: Promoting older adult health and independence through fall prevention. American Family Physician, 96(4): 220 -221. https: //doi. org/10. 1016/j. clineuro. 2009. 12. 015