Factors Associated with Necrotizing Enterocolitis in Very Low
- Slides: 1
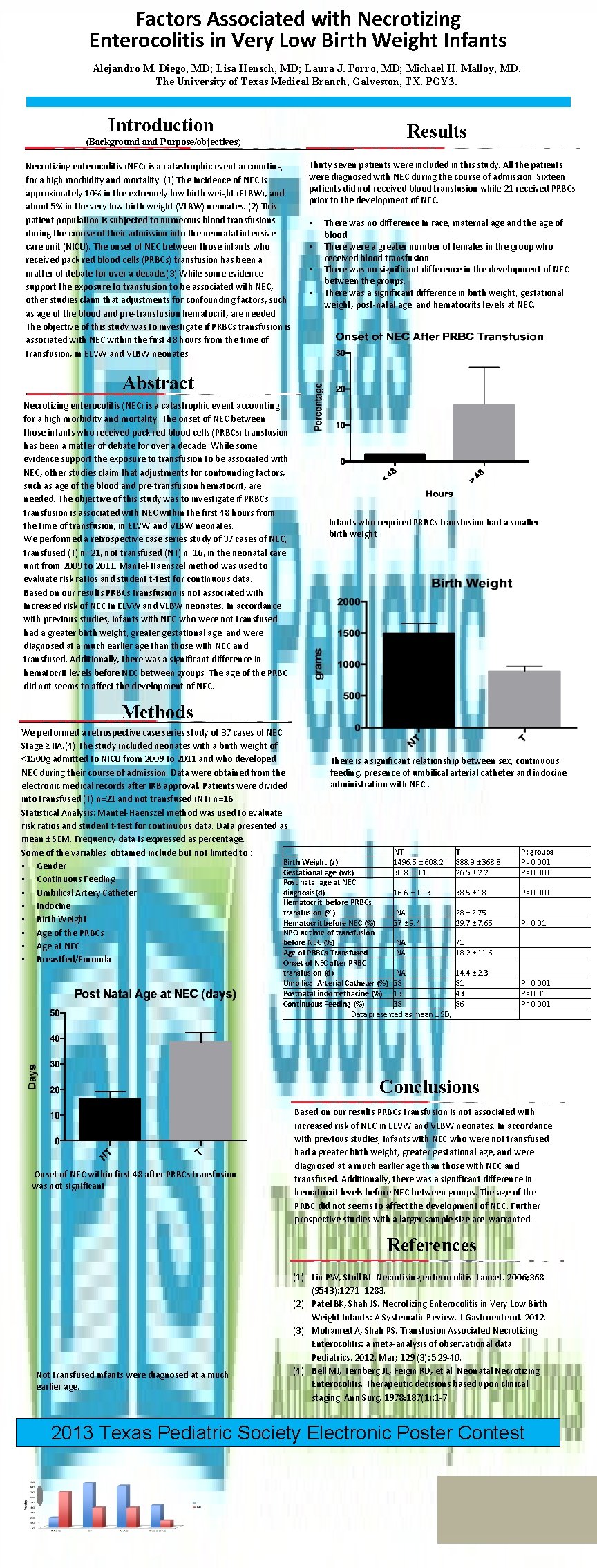
Factors Associated with Necrotizing Enterocolitis in Very Low Birth Weight Infants Alejandro M. Diego, MD; Lisa Hensch, MD; Laura J. Porro, MD; Michael H. Malloy, MD. The University of Texas Medical Branch, Galveston, TX. PGY 3. Introduction Results (Background and Purpose/objectives) Necrotizing enterocolitis (NEC) is a catastrophic event accounting for a high morbidity and mortality. (1) The incidence of NEC is approximately 10% in the extremely low birth weight (ELBW), and about 5% in the very low birth weight (VLBW) neonates. (2) This patient population is subjected to numerous blood transfusions during the course of their admission into the neonatal intensive care unit (NICU). The onset of NEC between those infants who received pack red blood cells (PRBCs) transfusion has been a matter of debate for over a decade. (3) While some evidence support the exposure to transfusion to be associated with NEC, other studies claim that adjustments for confounding factors, such as age of the blood and pre-transfusion hematocrit, are needed. The objective of this study was to investigate if PRBCs transfusion is associated with NEC within the first 48 hours from the time of transfusion, in ELVW and VLBW neonates. Thirty seven patients were included in this study. All the patients were diagnosed with NEC during the course of admission. Sixteen patients did not received blood transfusion while 21 received PRBCs prior to the development of NEC. • • There was no difference in race, maternal age and the age of blood. There were a greater number of females in the group who received blood transfusion. There was no significant difference in the development of NEC between the groups. There was a significant difference in birth weight, gestational weight, post-natal age and hematocrits levels at NEC. Abstract Necrotizing enterocolitis (NEC) is a catastrophic event accounting for a high morbidity and mortality. The onset of NEC between those infants who received pack red blood cells (PRBCs) transfusion has been a matter of debate for over a decade. While some evidence support the exposure to transfusion to be associated with NEC, other studies claim that adjustments for confounding factors, such as age of the blood and pre-transfusion hematocrit, are needed. The objective of this study was to investigate if PRBCs transfusion is associated with NEC within the first 48 hours from the time of transfusion, in ELVW and VLBW neonates. We performed a retrospective case series study of 37 cases of NEC, transfused (T) n=21, not transfused (NT) n=16, in the neonatal care unit from 2009 to 2011. Mantel-Haenszel method was used to evaluate risk ratios and student t-test for continuous data. Based on our results PRBCs transfusion is not associated with increased risk of NEC in ELVW and VLBW neonates. In accordance with previous studies, infants with NEC who were not transfused had a greater birth weight, greater gestational age, and were diagnosed at a much earlier age than those with NEC and transfused. Additionally, there was a significant difference in hematocrit levels before NEC between groups. The age of the PRBC did not seems to affect the development of NEC. Infants who required PRBCs transfusion had a smaller birth weight Methods We performed a retrospective case series study of 37 cases of NEC Stage ≥ IIA. (4) The study included neonates with a birth weight of <1500 g admitted to NICU from 2009 to 2011 and who developed There is a significant relationship between sex, continuous NEC during their course of admission. Data were obtained from the feeding, presence of umbilical arterial catheter and indocine administration with NEC. electronic medical records after IRB approval. Patients were divided into transfused (T) n=21 and not transfused (NT) n=16. Statistical Analysis: Mantel-Haenszel method was used to evaluate risk ratios and student t-test for continuous data. Data presented as mean ± SEM. Frequency data is expressed as percentage. NT T P; groups Some of the variables obtained include but not limited to : Birth Weight (g) 1496. 5 ± 608. 2 888. 9 ± 368. 8 P< 0. 001 • Gender Gestational age (wk) 30. 8 ± 3. 1 26. 5 ± 2. 2 P< 0. 001 • Continuous Feeding Post natal age at NEC diagnosis(d) 16. 6 ± 10. 3 38. 5 ± 18 P< 0. 001 • Umbilical Artery Catheter Hematocrit before PRBCs • Indocine transfusion (%) NA 28 ± 2. 75 • Birth Weight Hematocrit before NEC (%) 37 ± 9. 4 29. 7 ± 7. 65 P< 0. 01 NPO at time of transfusion • Age of the PRBCs before NEC (%) NA 71 • Age at NEC Age of PRBCs Transfused NA 18. 2 ± 11. 6 • Breastfed/Formula Onset of NEC after PRBC transfusion (d) NA Umbilical Arterial Catheter (%) 38 Postnatal indomethacine (%) 13 Continuous Feeding (%) 38 Data presented as mean ± SD, 14. 4 ± 2. 3 81 43 86 P< 0. 001 Conclusions Onset of NEC within first 48 after PRBCs transfusion was not significant Based on our results PRBCs transfusion is not associated with increased risk of NEC in ELVW and VLBW neonates. In accordance with previous studies, infants with NEC who were not transfused had a greater birth weight, greater gestational age, and were diagnosed at a much earlier age than those with NEC and transfused. Additionally, there was a significant difference in hematocrit levels before NEC between groups. The age of the PRBC did not seems to affect the development of NEC. Further prospective studies with a larger sample size are warranted. References Not transfused infants were diagnosed at a much earlier age. (1) Lin PW, Stoll BJ. Necrotising enterocolitis. Lancet. 2006; 368 (9543): 1271– 1283. (2) Patel BK, Shah JS. Necrotizing Enterocolitis in Very Low Birth Weight Infants: A Systematic Review. J Gastroenterol. 2012. (3) Mohamed A, Shah PS. Transfusion Associated Necrotizing Enterocolitis: a meta-analysis of observational data. Pediatrics. 2012. Mar; 129 (3): 529 -40. (4) Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal Necrotizing Enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978; 187(1): 1 -7 2013 Texas Pediatric Society Electronic Poster Contest