Factors Associated with Immunization Information System IIS Participation



- Slides: 45
Factors Associated with Immunization Information System (IIS) Participation among Rural Practitioners, Oregon, 2005 -06: Successes with VFC, Challenges and More Opportunities James A. Gaudino, MD, MS, MPH*, ** Lyle (LJ) Fagnan, MD ** Andrew Sussman, Ph. D, MCRP ** Scott Shipman, MD, MPH ** Jennifer Holub, MA, MPH ** Jo Mahler, MS ** *Immunization Program, Office of Family Health, Public Health Division Department of Human Services, State of Oregon **Oregon Rural Practice-based Research Network (ORPRN), Oregon Health and Sciences University Thanks to: Heather Angier, BA **, Jim Wallace, BA ** , David De. Boer, MS**, Anne King **
Background l Little is known about practice barriers to immunization among US clinicians serving children in large rural, Western areas including Oregon
Background - Rural Oregon is predominantly a rural state: - In 2000, had only 3 cities with populations > 100, 000 - Nearly 200 towns have < 10, 000 inhabitants, including 145 with < 2, 500 l Thirty-six percent of Oregonians live in rural Oregon ~ 1. 3 million people* * Based on Oregon Office of Rural Health rural definition = living greater than 10 miles from a town of 30, 000 people or more
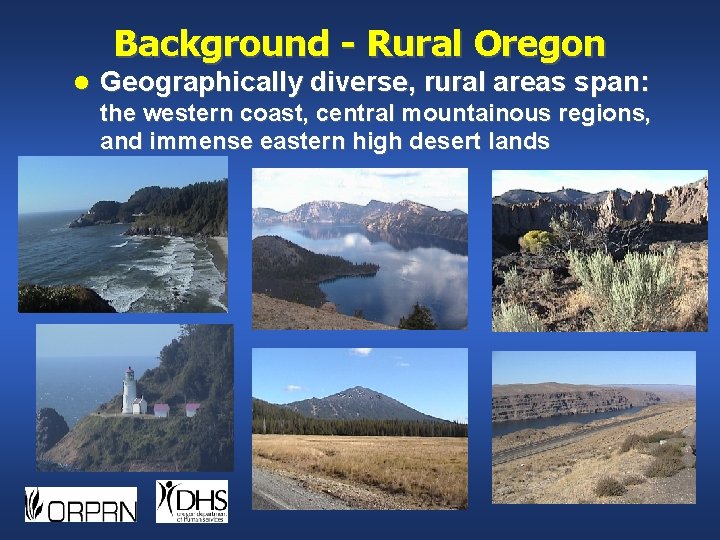
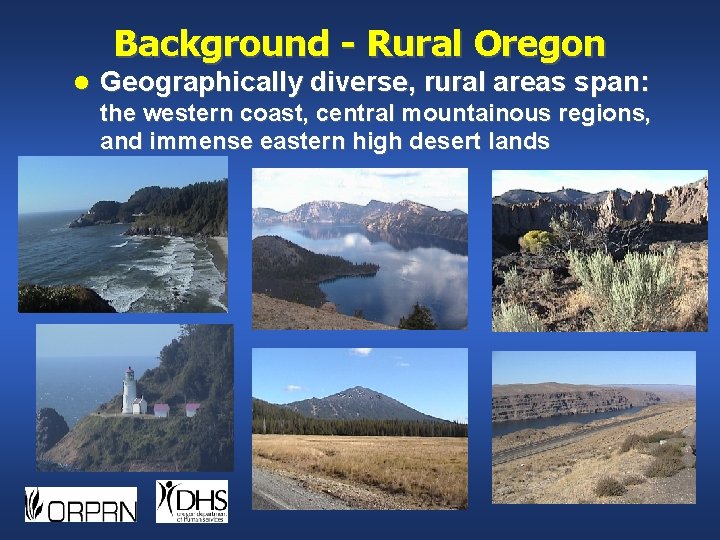
Background - Rural Oregon l Geographically diverse, rural areas span: the western coast, central mountainous regions, and immense eastern high desert lands
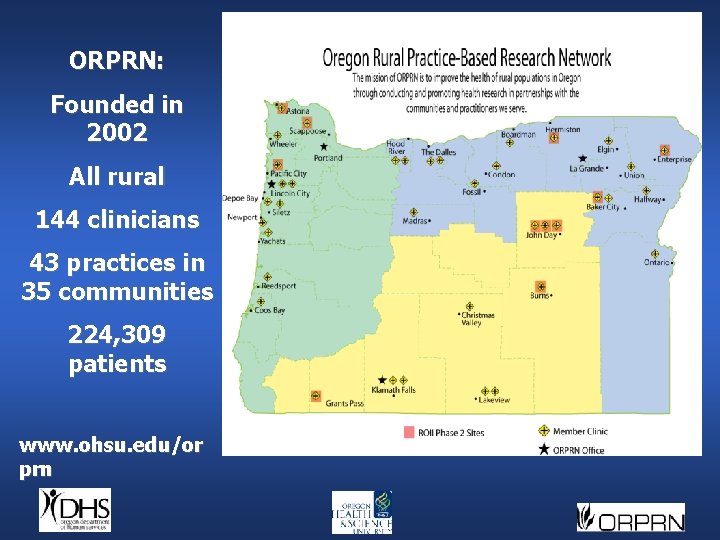
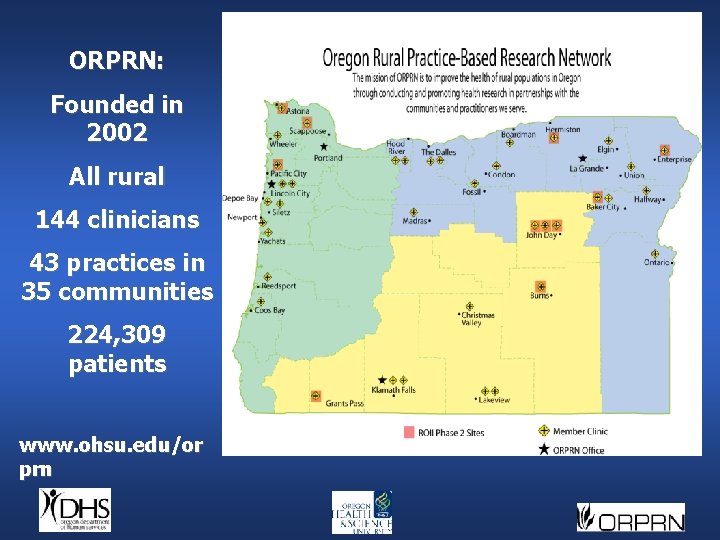
ORPRN: Founded in 2002 All rural 144 clinicians 43 practices in 35 communities 224, 309 patients www. ohsu. edu/or prn
Rural Oregon Immunization Initiative (ROII) Collaboration Oregon Rural Practice-Based Research Network (ORPRN) l Immunization Program, State of Oregon Department of Human Services (DHS) l CDC Health Services Research and Evaluation Branch (HSREB), National Center of Immunization and Respiratory Diseases (NCIRD) l AAFP Foundation PBRN Stimulation Grant State Immunization Program funding from CDC l CDC HSREB funding l ORPRN’s Federal AHQR* and other state funding l l * Agency for Healthcare Research and Quality (AHRQ)
Overview of ROII Methods Phase I –Quantitative statewide survey of primary care clinicians regarding current practices and barriers to immunization delivery l Phase 2 –Mixed-methods assessment of 11 practices including chart reviews, observations, and interviews with clinicians, clinic staff, parents, and county health department officers l Phase 3 –Obtain feedback about the phase 1 & 2 findings and, eventually, develop and implement practice-specific interventions using a participatory approach l
Purpose of this Study In late 2004 and early 2005, surveyed all licensed rural Oregon clinicians providing care for children, ages 0 to 3 l To assess rural Oregon clinicians’ participation with the statewide ALERT Immunization Information System (IIS). l To identify factors associated with non-participation in the ALERT IIS. l Expand understanding of ALERT use using qualitative phase 2 & 3 information.
Survey Methods l Attempted to contact all 1158 licensed rural clinicians using Oregon’s Board of Medical Examiners mailing lists and the ORPRN database l Contact information was supplemented by phone directory information and other lists l Initially, sent the 46 -question survey electronically via e-mail or by mail l Followed by a reminder card to everyone and, then, US Priority mailings and telephone calls to non-respondents
Survey Methods l Phone follow-up mostly used to determine non-respondent eligibility l Eligible clinicians were those that: - Provide primary care. - Currently see child-patients from 0 -36 months of age. - Still practice in rural Oregon. E. g. , excluded Emergency Dept. clinicians from analyses
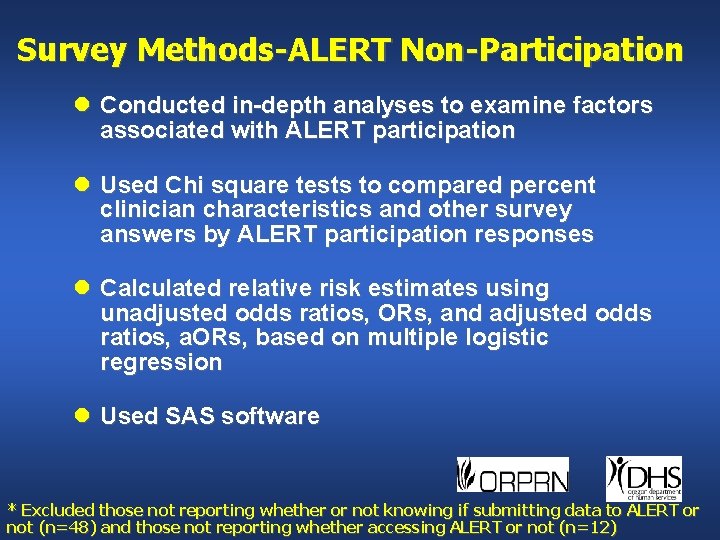
Survey Methods-ALERT Non-Participation l Conducted in-depth analyses to examine factors associated with ALERT participation l Used Chi square tests to compared percent clinician characteristics and other survey answers by ALERT participation responses l Calculated relative risk estimates using unadjusted odds ratios, ORs, and adjusted odds ratios, a. ORs, based on multiple logistic regression l Used SAS software * Excluded those not reporting whether or not knowing if submitting data to ALERT or not (n=48) and those not reporting whether accessing ALERT or not (n=12)
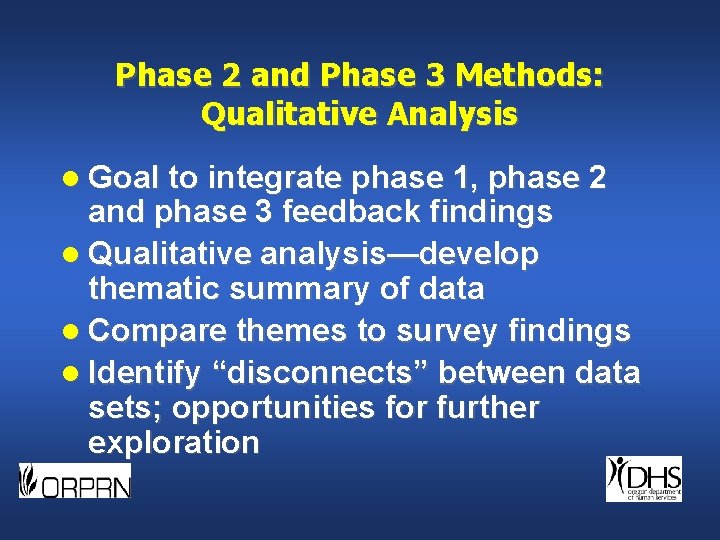
Phase 2 and Phase 3 Methods: Qualitative Analysis l Goal to integrate phase 1, phase 2 and phase 3 feedback findings l Qualitative analysis—develop thematic summary of data l Compare themes to survey findings l Identify “disconnects” between data sets; opportunities for further exploration
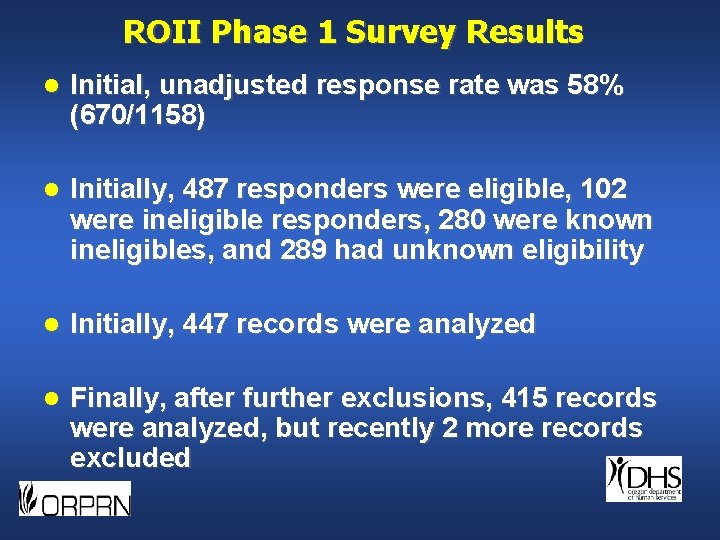
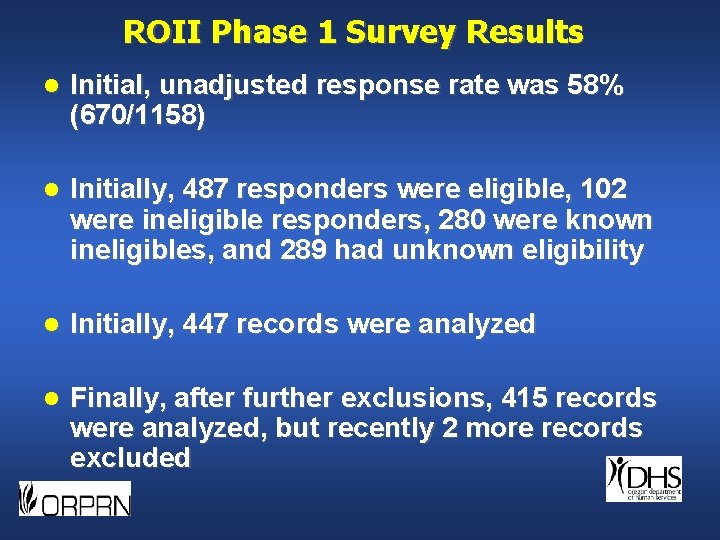
ROII Phase 1 Survey Results l Initial, unadjusted response rate was 58% (670/1158) l Initially, 487 responders were eligible, 102 were ineligible responders, 280 were known ineligibles, and 289 had unknown eligibility l Initially, 447 records were analyzed l Finally, after further exclusions, 415 records were analyzed, but recently 2 more records excluded
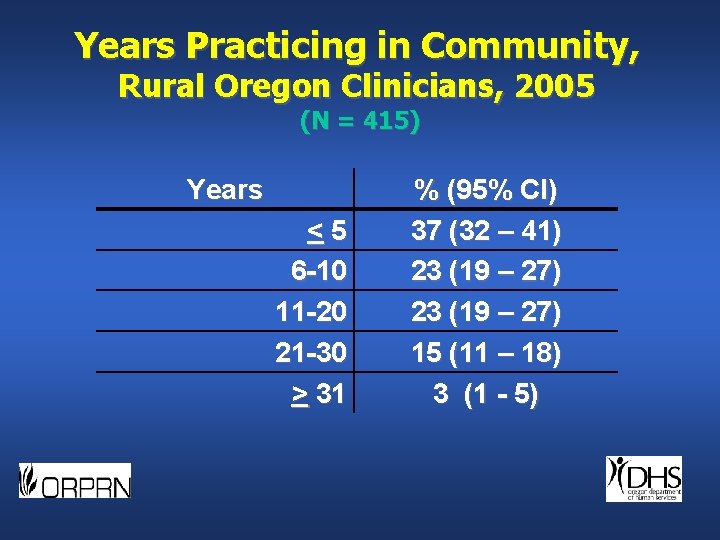
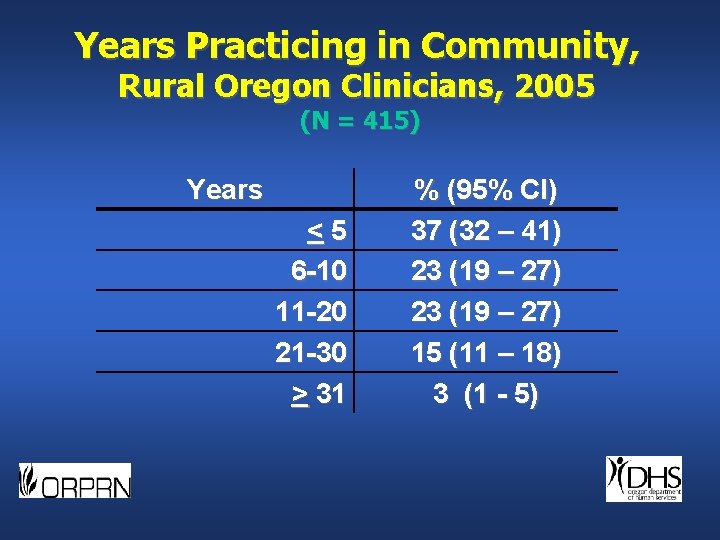
Years Practicing in Community, Rural Oregon Clinicians, 2005 (N = 415) Years <5 6 -10 11 -20 21 -30 > 31 % (95% CI) 37 (32 – 41) 23 (19 – 27) 15 (11 – 18) 3 (1 - 5)
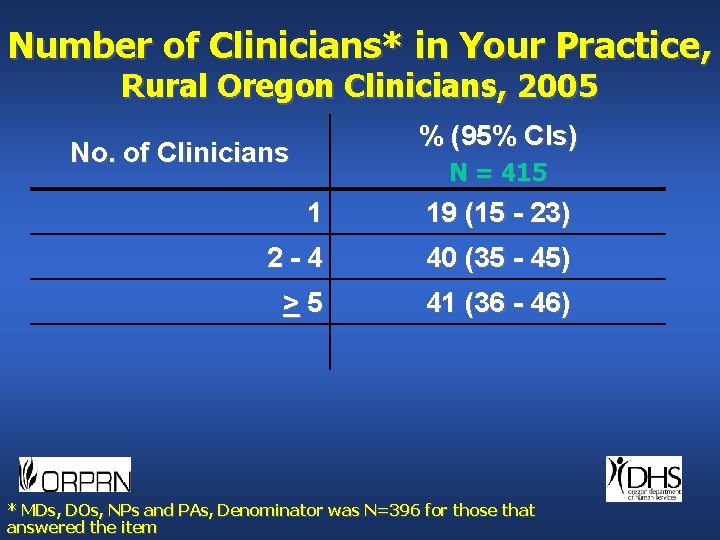
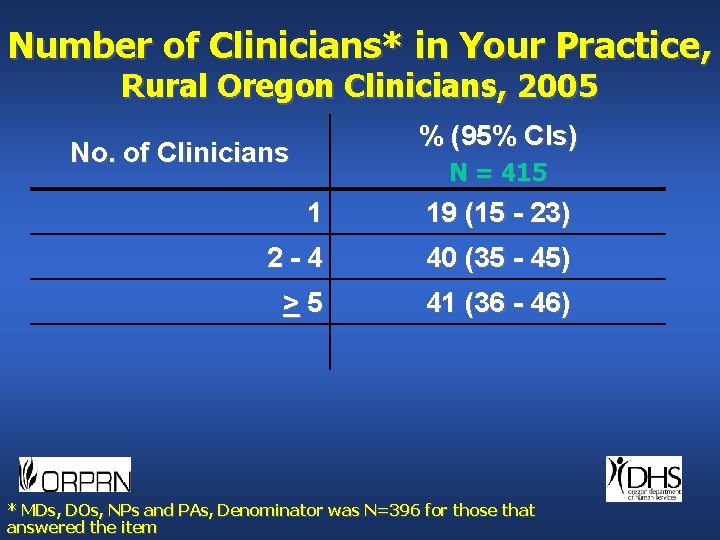
Number of Clinicians* in Your Practice, Rural Oregon Clinicians, 2005 % (95% CIs) No. of Clinicians N = 415 1 19 (15 - 23) 2 -4 40 (35 - 45) >5 41 (36 - 46) * MDs, DOs, NPs and PAs, Denominator was N=396 for those that answered the item
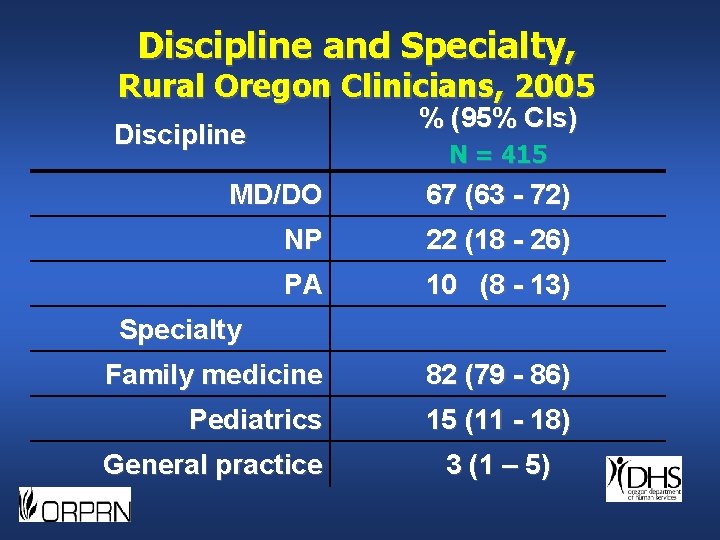
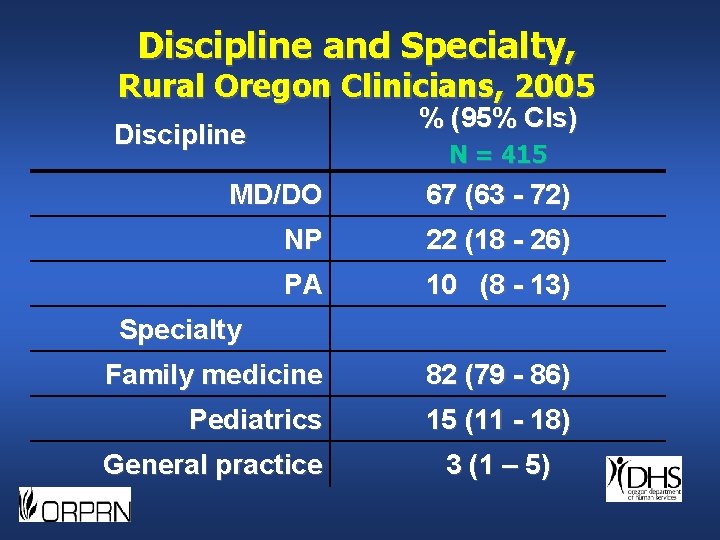
Discipline and Specialty, Rural Oregon Clinicians, 2005 % (95% CIs) Discipline N = 415 MD/DO 67 (63 - 72) NP 22 (18 - 26) PA 10 (8 - 13) Family medicine 82 (79 - 86) Pediatrics 15 (11 - 18) Specialty General practice 3 (1 – 5)
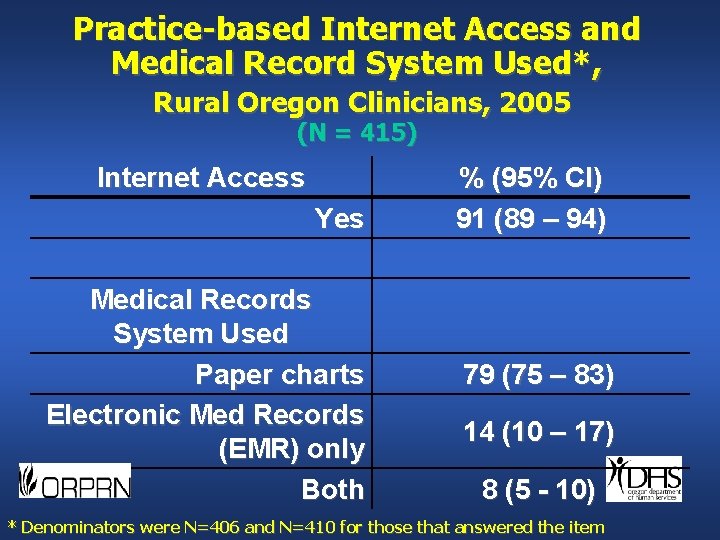
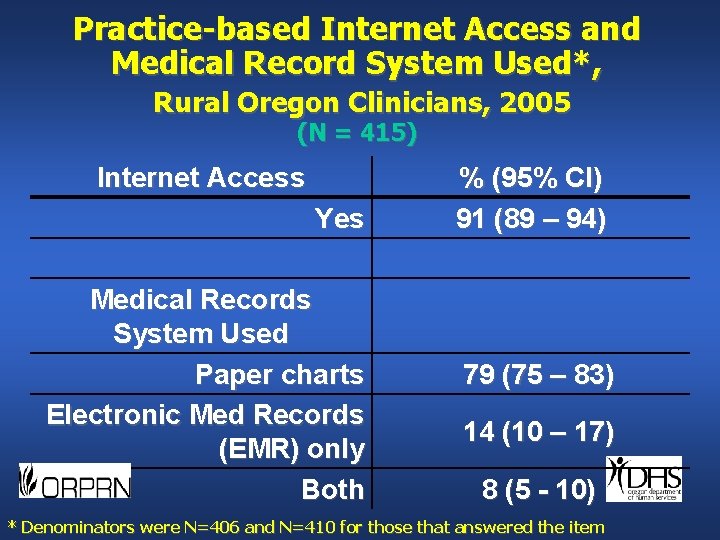
Practice-based Internet Access and Medical Record System Used*, Rural Oregon Clinicians, 2005 (N = 415) Internet Access Yes Medical Records System Used Paper charts Electronic Med Records (EMR) only Both % (95% CI) 91 (89 – 94) 79 (75 – 83) 14 (10 – 17) 8 (5 - 10) * Denominators were N=406 and N=410 for those that answered the item
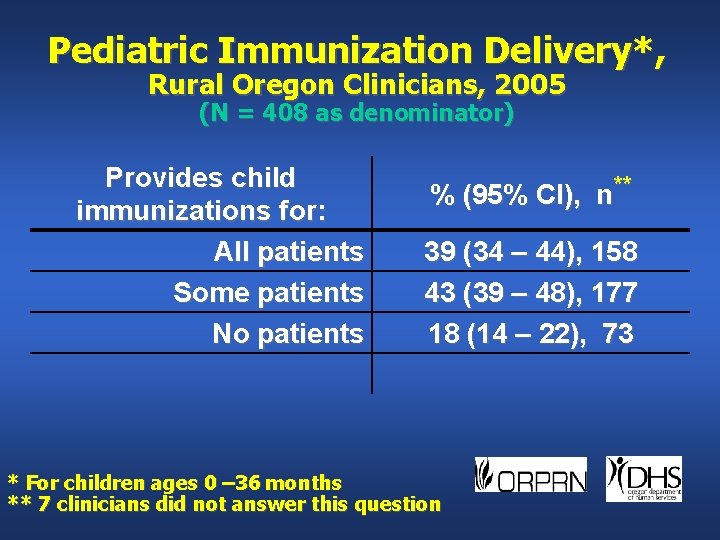
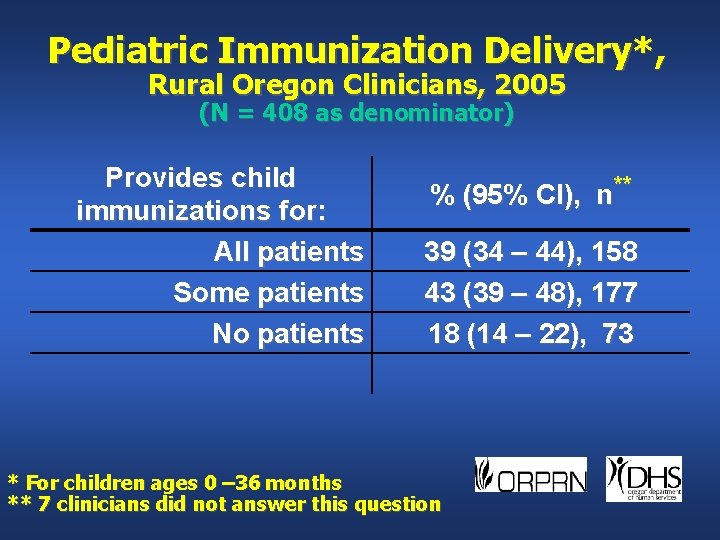
Pediatric Immunization Delivery*, Rural Oregon Clinicians, 2005 (N = 408 as denominator) Provides child immunizations for: All patients Some patients No patients % (95% CI), n** 39 (34 – 44), 158 43 (39 – 48), 177 18 (14 – 22), 73 * For children ages 0 – 36 months ** 7 clinicians did not answer this question
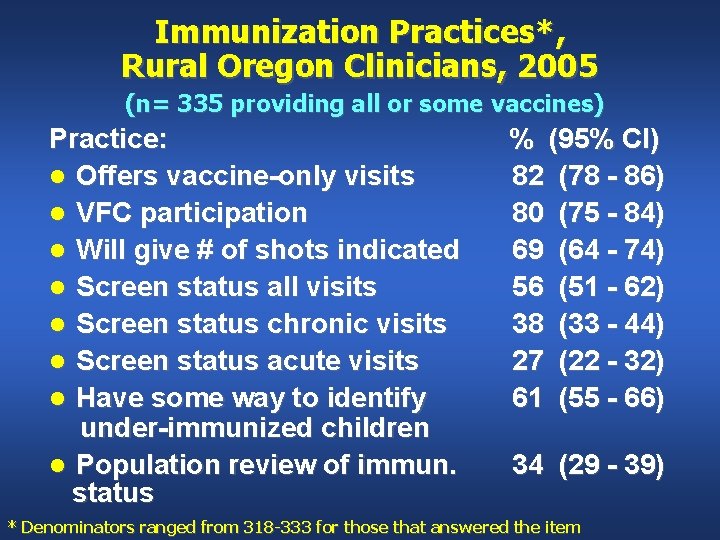
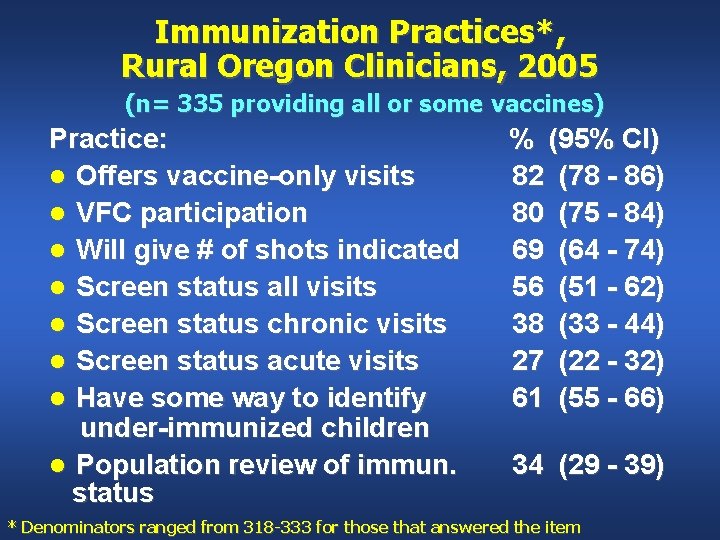
Immunization Practices*, Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Practice: l Offers vaccine-only visits l VFC participation l Will give # of shots indicated l Screen status all visits l Screen status chronic visits l Screen status acute visits l Have some way to identify under-immunized children l Population review of immun. status % (95% CI) 82 (78 - 86) 80 (75 - 84) 69 (64 - 74) 56 (51 - 62) 38 (33 - 44) 27 (22 - 32) 61 (55 - 66) 34 (29 - 39) * Denominators ranged from 318 -333 for those that answered the item
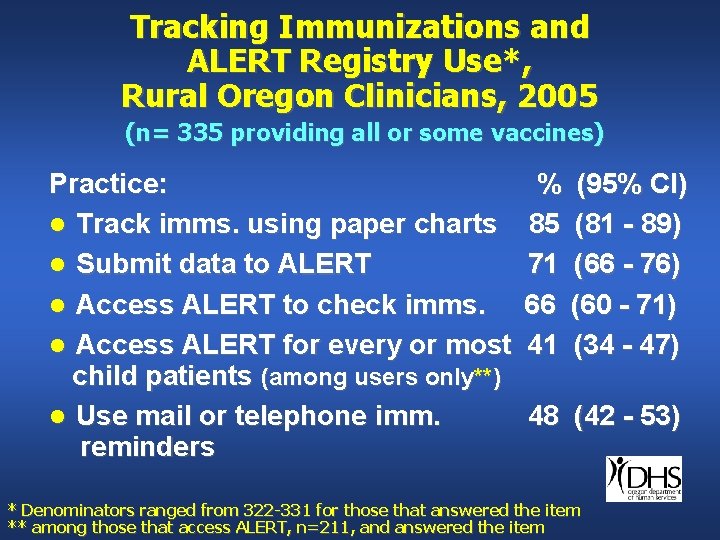
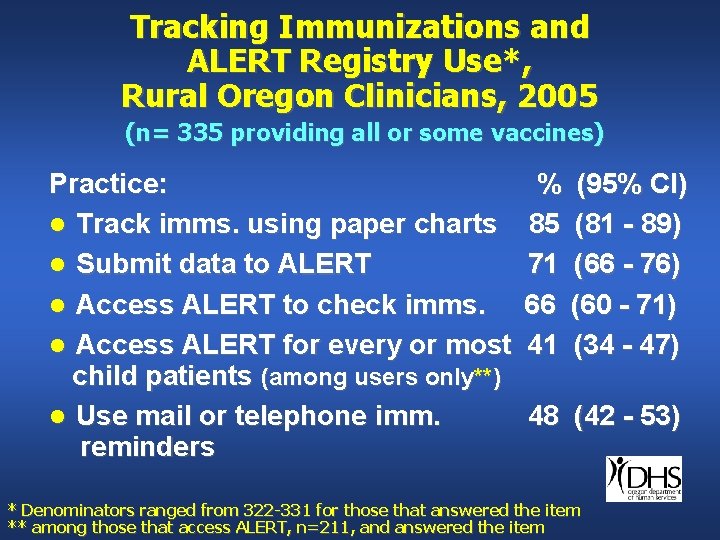
Tracking Immunizations and ALERT Registry Use*, Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Practice: l Track imms. using paper charts l Submit data to ALERT l Access ALERT to check imms. l Access ALERT for every or most child patients (among users only**) l Use mail or telephone imm. reminders % (95% CI) 85 (81 - 89) 71 (66 - 76) 66 (60 - 71) 41 (34 - 47) 48 (42 - 53) * Denominators ranged from 322 -331 for those that answered the item ** among those that access ALERT, n=211, and answered the item
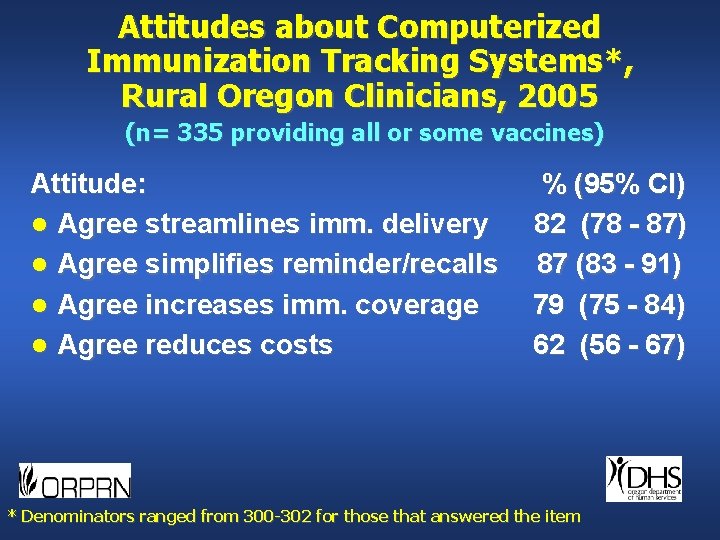
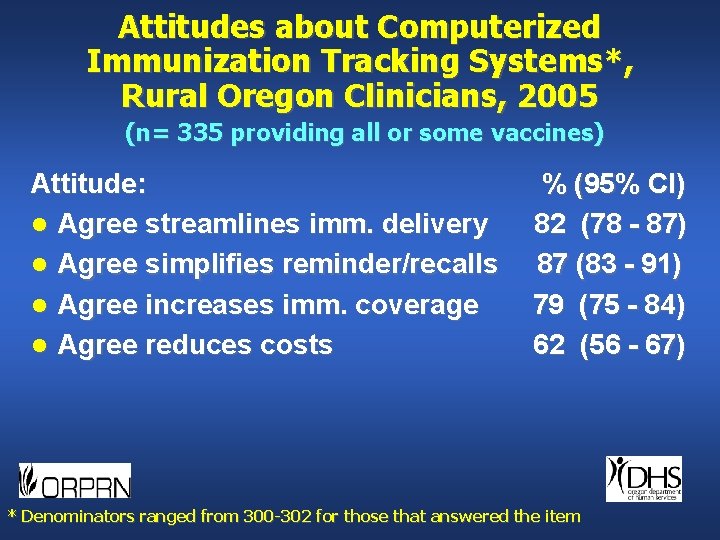
Attitudes about Computerized Immunization Tracking Systems*, Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Attitude: l Agree streamlines imm. delivery l Agree simplifies reminder/recalls l Agree increases imm. coverage l Agree reduces costs % (95% CI) 82 (78 - 87) 87 (83 - 91) 79 (75 - 84) 62 (56 - 67) * Denominators ranged from 300 -302 for those that answered the item
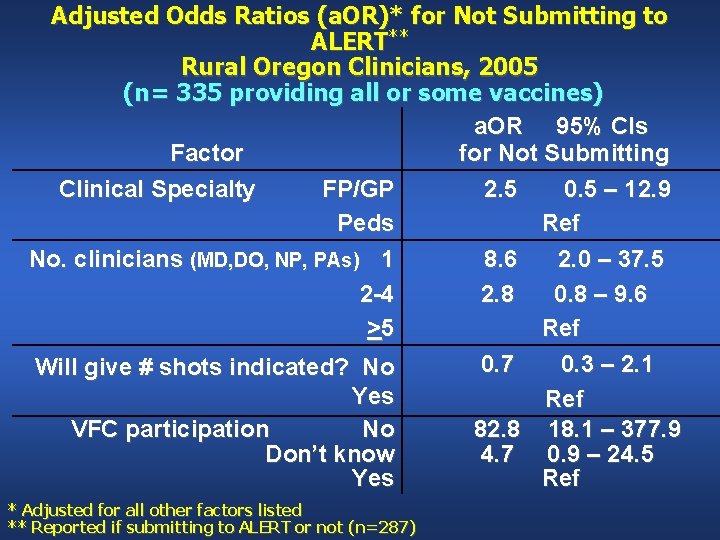
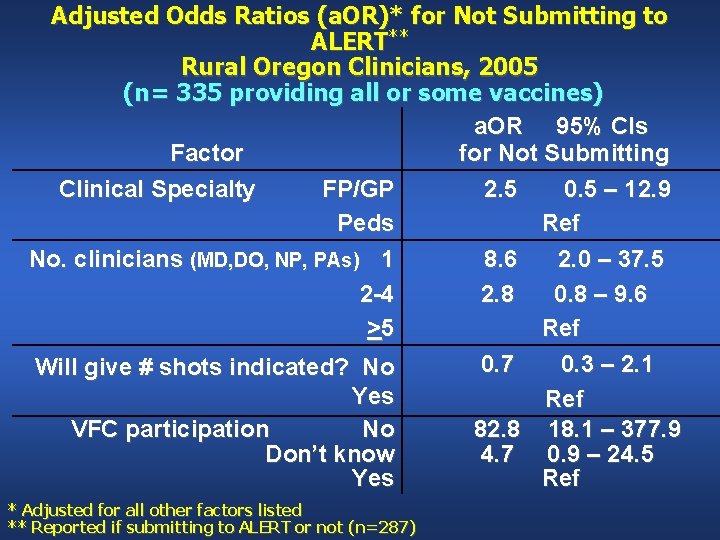
Adjusted Odds Ratios (a. OR)* for Not Submitting to ALERT** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) a. OR 95% CIs Factor for Not Submitting Clinical Specialty FP/GP 2. 5 0. 5 – 12. 9 Peds Ref No. clinicians (MD, DO, NP, PAs) 1 8. 6 2. 0 – 37. 5 2 -4 2. 8 0. 8 – 9. 6 >5 Ref 0. 7 0. 3 – 2. 1 Will give # shots indicated? No Yes Ref VFC participation No 82. 8 18. 1 – 377. 9 Don’t know 4. 7 0. 9 – 24. 5 Yes Ref * Adjusted for all other factors listed ** Reported if submitting to ALERT or not (n=287)
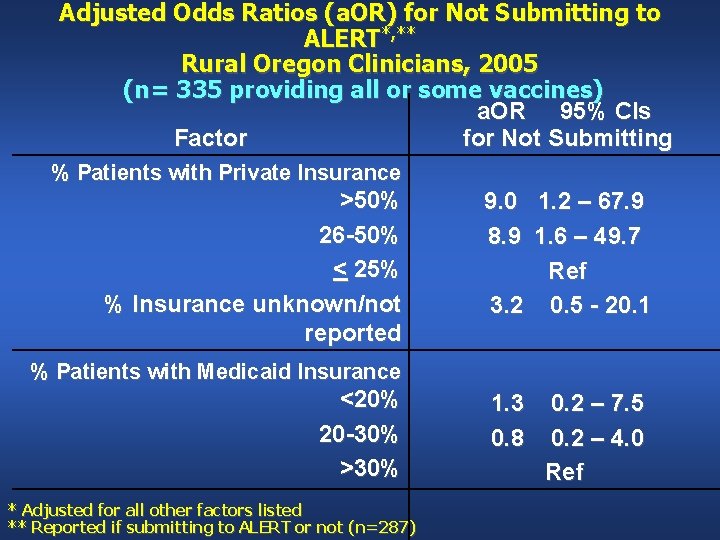
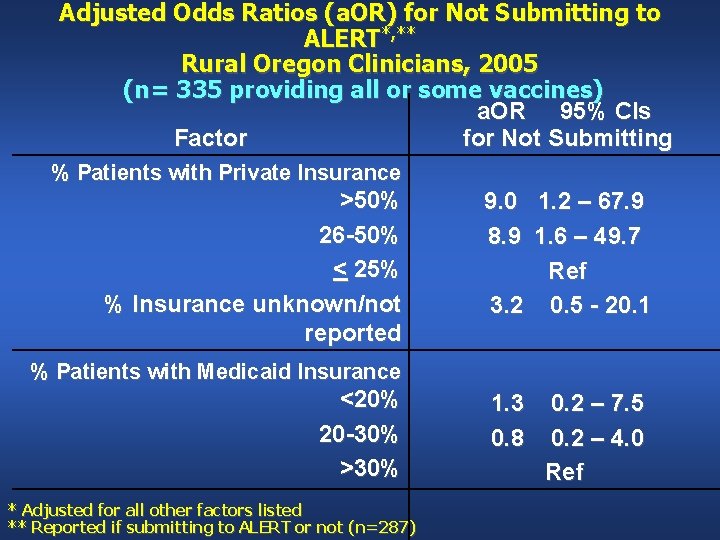
Adjusted Odds Ratios (a. OR) for Not Submitting to ALERT*, ** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) a. OR 95% CIs Factor for Not Submitting % Patients with Private Insurance >50% 26 -50% < 25% % Insurance unknown/not reported 9. 0 1. 2 – 67. 9 8. 9 1. 6 – 49. 7 Ref 3. 2 0. 5 - 20. 1 % Patients with Medicaid Insurance <20% 20 -30% >30% * Adjusted for all other factors listed ** Reported if submitting to ALERT or not (n=287) 1. 3 0. 8 0. 2 – 7. 5 0. 2 – 4. 0 Ref
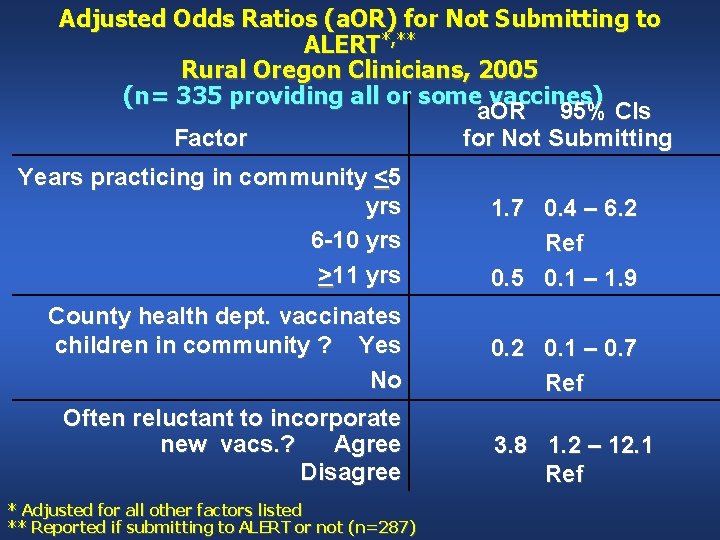
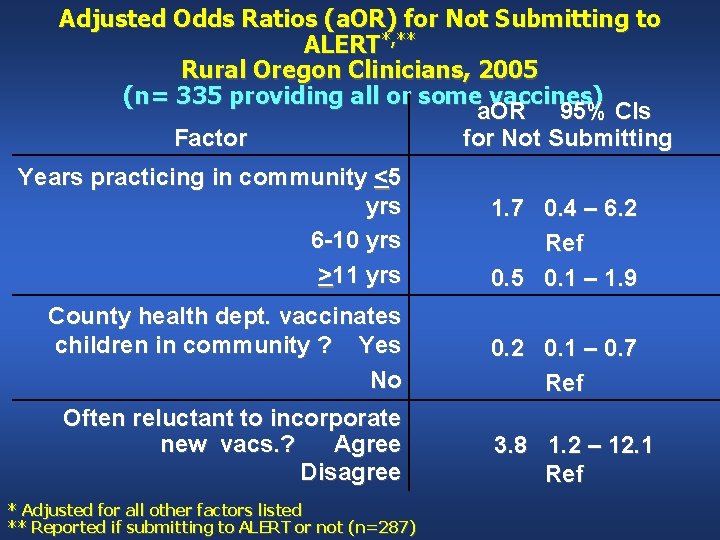
Adjusted Odds Ratios (a. OR) for Not Submitting to ALERT*, ** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) a. OR 95% CIs Factor for Not Submitting Years practicing in community <5 yrs 6 -10 yrs >11 yrs 1. 7 0. 4 – 6. 2 Ref 0. 5 0. 1 – 1. 9 County health dept. vaccinates children in community ? Yes No 0. 2 0. 1 – 0. 7 Ref Often reluctant to incorporate new vacs. ? Agree Disagree * Adjusted for all other factors listed ** Reported if submitting to ALERT or not (n=287) 3. 8 1. 2 – 12. 1 Ref
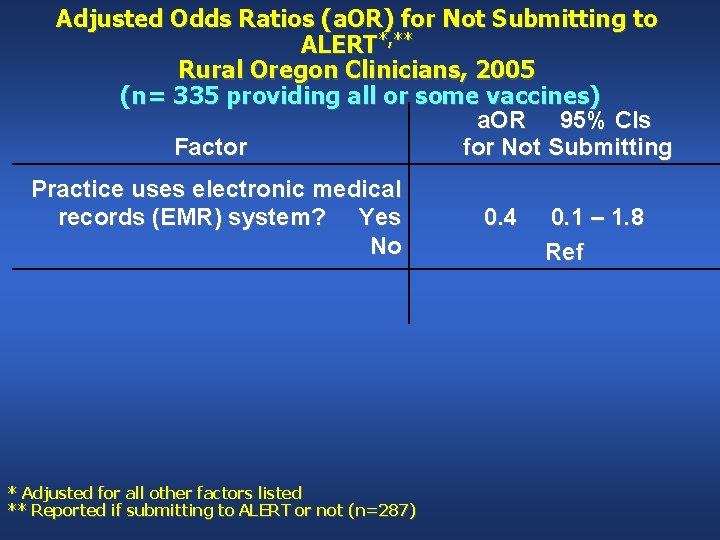
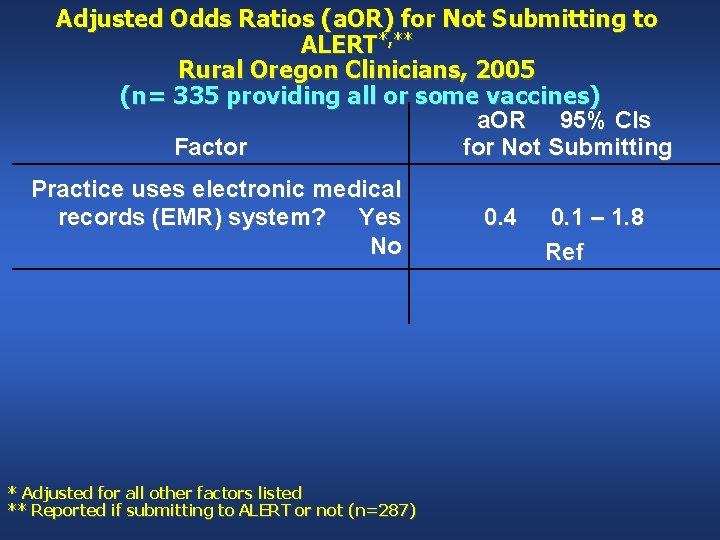
Adjusted Odds Ratios (a. OR) for Not Submitting to ALERT*, ** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) a. OR 95% CIs Factor for Not Submitting Practice uses electronic medical records (EMR) system? Yes No * Adjusted for all other factors listed ** Reported if submitting to ALERT or not (n=287) 0. 4 0. 1 – 1. 8 Ref

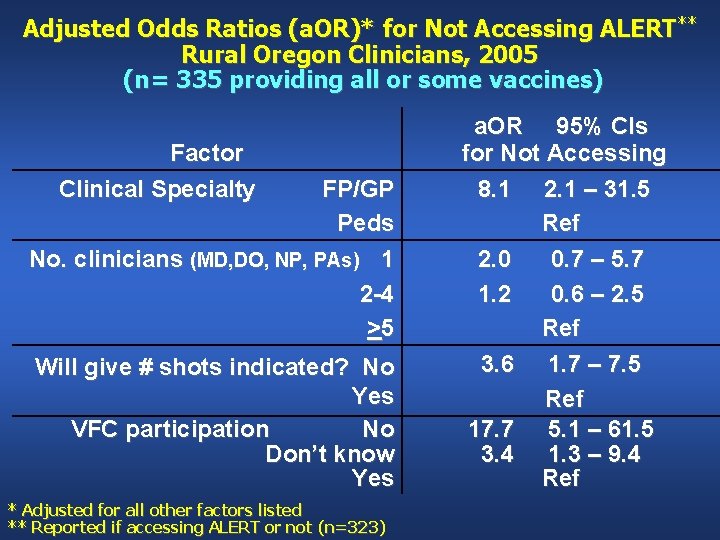
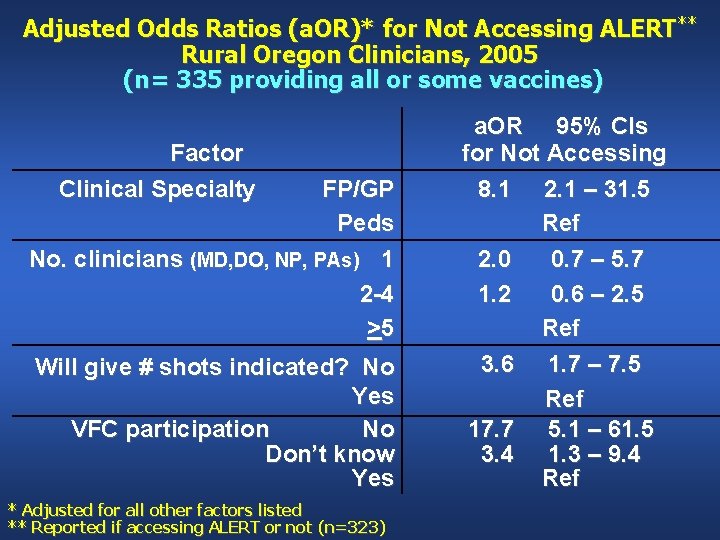
Adjusted Odds Ratios (a. OR)* for Not Accessing ALERT** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Factor Clinical Specialty FP/GP Peds No. clinicians (MD, DO, NP, PAs) 1 2 -4 >5 Will give # shots indicated? No Yes VFC participation No Don’t know Yes * Adjusted for all other factors listed ** Reported if accessing ALERT or not (n=323) a. OR 95% CIs for Not Accessing 8. 1 2. 1 – 31. 5 Ref 2. 0 0. 7 – 5. 7 1. 2 0. 6 – 2. 5 Ref 3. 6 1. 7 – 7. 5 Ref 17. 7 5. 1 – 61. 5 3. 4 1. 3 – 9. 4 Ref
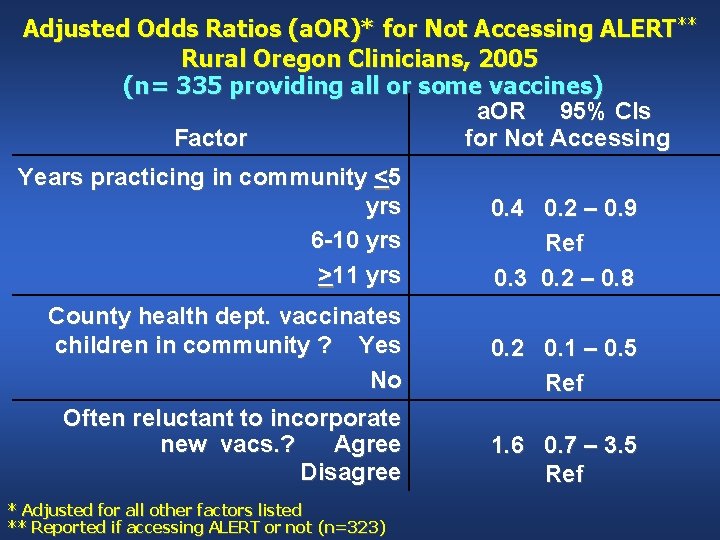
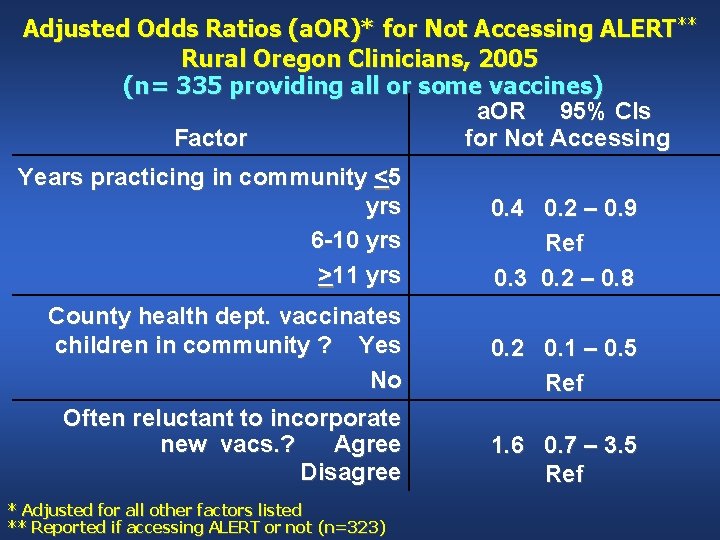
Adjusted Odds Ratios (a. OR)* for Not Accessing ALERT** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) a. OR 95% CIs Factor for Not Accessing Years practicing in community <5 yrs 6 -10 yrs >11 yrs 0. 4 0. 2 – 0. 9 Ref 0. 3 0. 2 – 0. 8 County health dept. vaccinates children in community ? Yes No 0. 2 0. 1 – 0. 5 Ref Often reluctant to incorporate new vacs. ? Agree Disagree 1. 6 0. 7 – 3. 5 Ref * Adjusted for all other factors listed ** Reported if accessing ALERT or not (n=323)
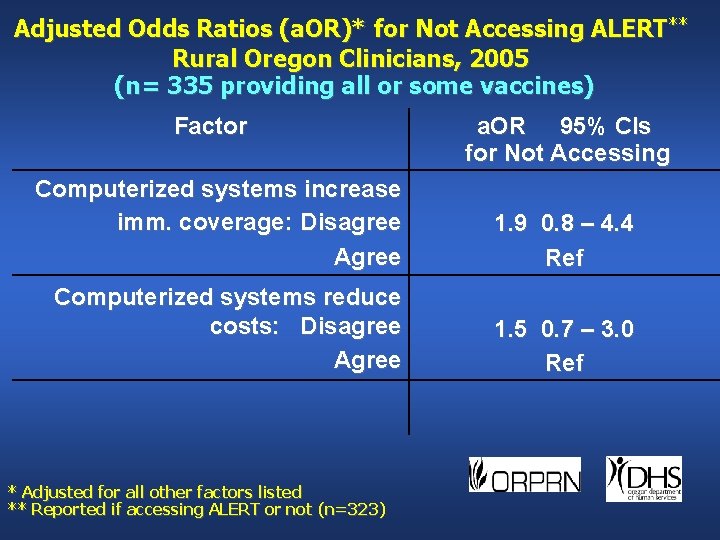
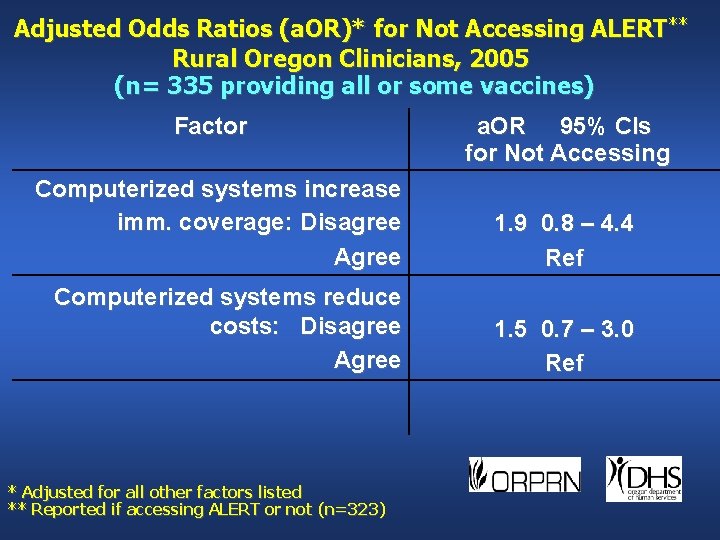
Adjusted Odds Ratios (a. OR)* for Not Accessing ALERT** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Factor a. OR 95% CIs for Not Accessing Computerized systems increase imm. coverage: Disagree Agree 1. 9 0. 8 – 4. 4 Ref Computerized systems reduce costs: Disagree Agree 1. 5 0. 7 – 3. 0 Ref * Adjusted for all other factors listed ** Reported if accessing ALERT or not (n=323)
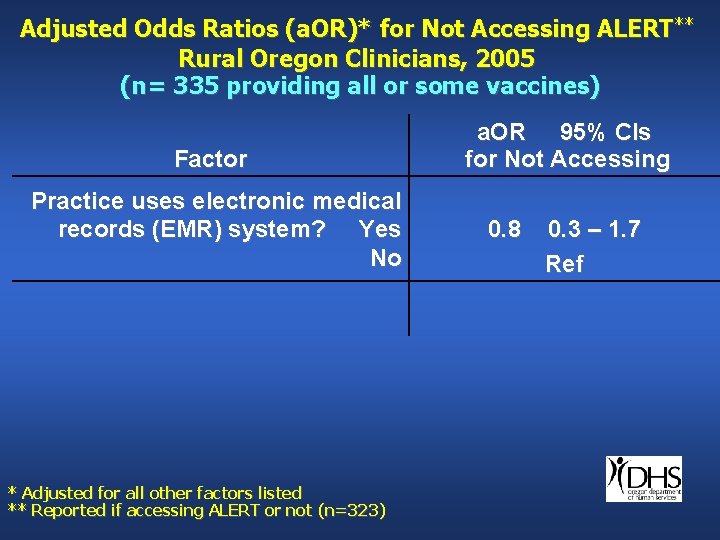
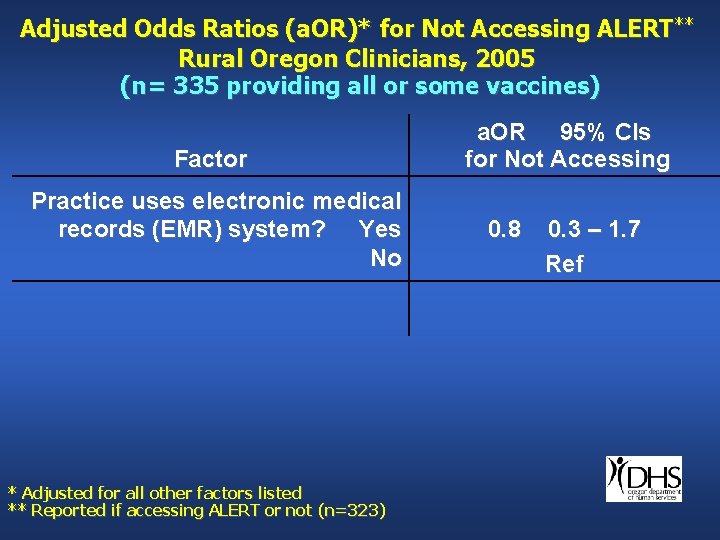
Adjusted Odds Ratios (a. OR)* for Not Accessing ALERT** Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Factor Practice uses electronic medical records (EMR) system? Yes No * Adjusted for all other factors listed ** Reported if accessing ALERT or not (n=323) a. OR 95% CIs for Not Accessing 0. 8 0. 3 – 1. 7 Ref
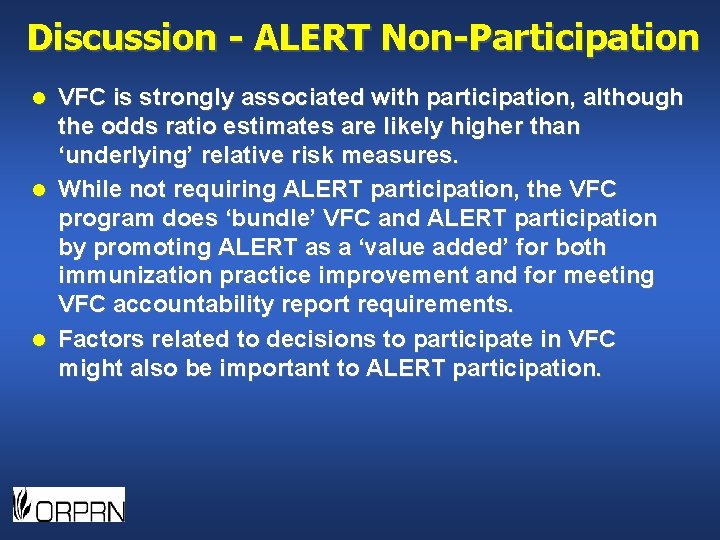
Discussion - ALERT Non-Participation VFC is strongly associated with participation, although the odds ratio estimates are likely higher than ‘underlying’ relative risk measures. l While not requiring ALERT participation, the VFC program does ‘bundle’ VFC and ALERT participation by promoting ALERT as a ‘value added’ for both immunization practice improvement and for meeting VFC accountability report requirements. l Factors related to decisions to participate in VFC might also be important to ALERT participation. l
Discussion - ALERT Non-Participation l l l Opportunities may exist to work with private insurance payers to increase incentives to track immunizations with ALERT by leveraging ALERT use for QI, e. g. , Oregon AFIX work with Medicaid plans. Clinicians in smaller clinics may have less capacity to use ALERT and may need help to participate. Newer clinicians in communities may be more technically apt or interested in using ALERT. Longer serving clinicians may be in more established clinics more able to use ALERT. EMRs may facilitate participation once the value of using ALERT is recognized.
ALERT in Practice* Selected Practices in Rural Oregon, 2006 Generally perceived as low to moderate burden l ALERT part of immunization safety net toolkit l Knowledge and usage of ALERT widely varies l Communication issues may remain — usage of ALERT, here is one example. l * Based on key informant and focus group interviews with clinicians and staff at 11 rural practices and county health department officials where practices located.
ALERT in Practice*—Communication Disconnect l County Health Officer: “You know, we used to. Every time one of their patients came in and got an immunization, we would make a printed copy and give it to them. And we’ve kind of backed away from that now, because they have access to ALERT, and any time they want to know where their child is, they can look it up and it’s right at their fingertips. So we really don’t do that much anymore. It seems to be effective. And sometimes they still do call and say, ‘So-and-So’s here. What have they had? ’ and we’re gracious enough to give ’em the information, instead of saying, ‘Well, did you check ALERT? ” * Based on key informant and focus group interviews with clinicians and staff at 11 rural practices and county health department officials where practices located.
ALERT in Practice*—Communication Disconnect l Clinician: “Nope, the only time there’s communication is when they show up in our office, and we call over there and ask them to send those records, or we look up on the ALERT website. There’s no communication between the health department telling us that our kids are over there getting immunized. They don’t do anything like that. And that would help. I mean, if they were seeing kids and asked the families to say, you know, ‘Who’s your primary provider? ’ and send records just automatically, that would be hugely helpful, but that doesn’t happen, no. ” * Based on key informant and focus group interviews with clinicians and staff at 11 rural practices and county health department officials where practices located.
ALERT in Practice*—Verification l ALERT especially important given complexity of vaccine schedule and challenges of parent recall “. . . so we double check, because we do find discrepancies. And then sometimes the patient will bring their immunization record in and it is completely different, so it is like eeny, miny, moe. . . you know, so I mean we have to double check. * Based on key informant and focus group interviews with clinicians and staff at 11 rural practices and county health department officials where practices located.
ALERT in Practice*—Verification “We access ALERT if we do not have a shot record and we know the kid is from the State or if there is a question on any of the shot records, any of the documentation, we access ALERT just to check and see what the State has because some of our kids like to go back and forth to the Health Department. I use it a lot. It does have errors. I do not believe in it 100%, but it is helpful. * Based on key informant and focus group interviews with clinicians and staff at 11 rural practices and county health department officials where practices located.
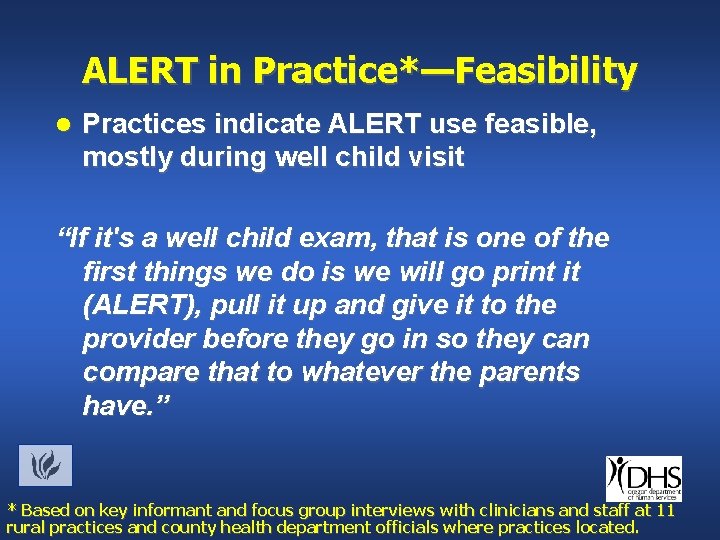
ALERT in Practice*—Feasibility l Practices indicate ALERT use feasible, mostly during well child visit “If it's a well child exam, that is one of the first things we do is we will go print it (ALERT), pull it up and give it to the provider before they go in so they can compare that to whatever the parents have. ” * Based on key informant and focus group interviews with clinicians and staff at 11 rural practices and county health department officials where practices located.
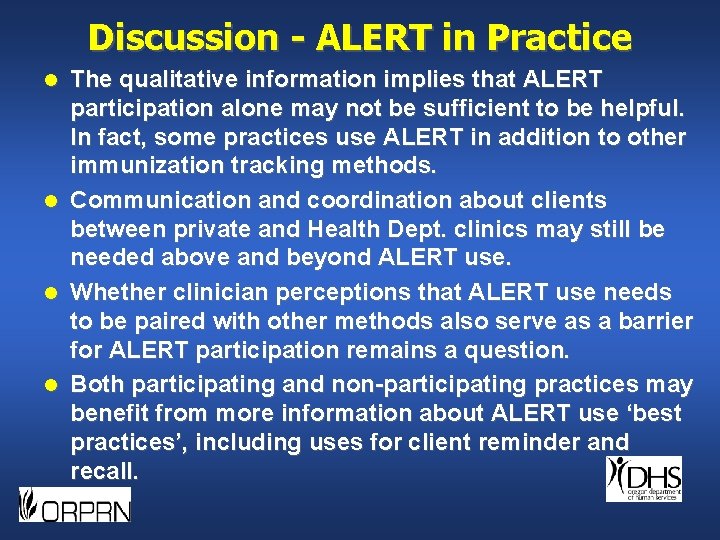
Discussion - ALERT in Practice l l The qualitative information implies that ALERT participation alone may not be sufficient to be helpful. In fact, some practices use ALERT in addition to other immunization tracking methods. Communication and coordination about clients between private and Health Dept. clinics may still be needed above and beyond ALERT use. Whether clinician perceptions that ALERT use needs to be paired with other methods also serve as a barrier for ALERT participation remains a question. Both participating and non-participating practices may benefit from more information about ALERT use ‘best practices’, including uses for client reminder and recall.
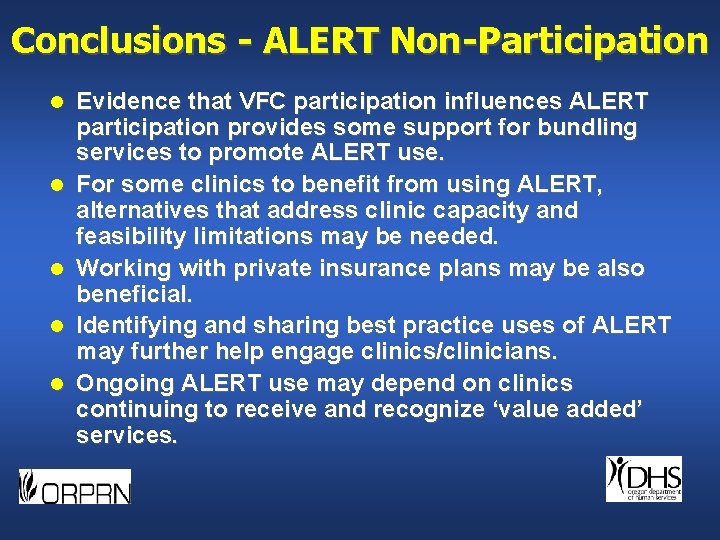
Conclusions - ALERT Non-Participation l l l Evidence that VFC participation influences ALERT participation provides some support for bundling services to promote ALERT use. For some clinics to benefit from using ALERT, alternatives that address clinic capacity and feasibility limitations may be needed. Working with private insurance plans may be also beneficial. Identifying and sharing best practice uses of ALERT may further help engage clinics/clinicians. Ongoing ALERT use may depend on clinics continuing to receive and recognize ‘value added’ services.

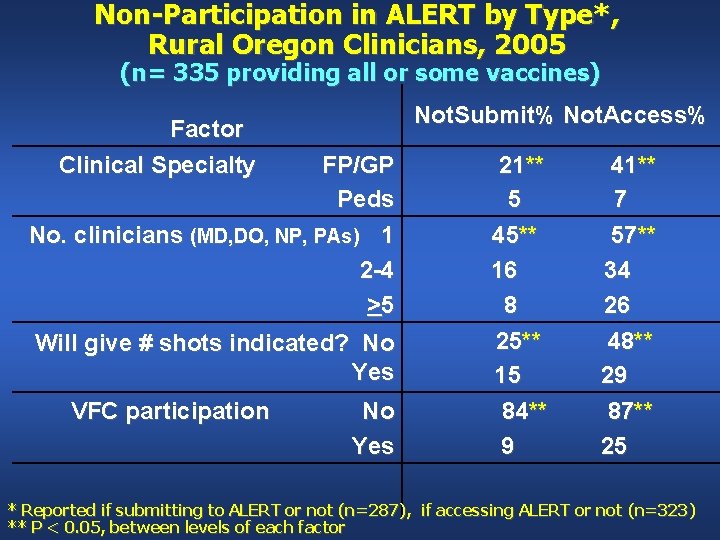
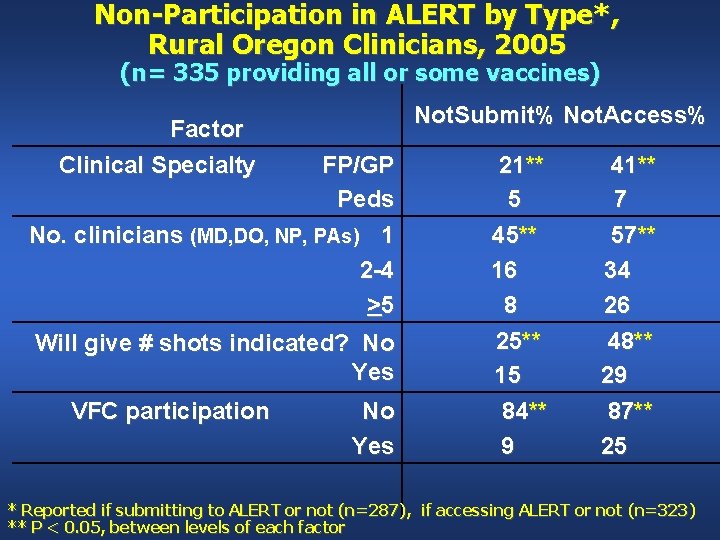
Non-Participation in ALERT by Type*, Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Not. Submit% Not. Access% Factor Clinical Specialty FP/GP Peds No. clinicians (MD, DO, NP, PAs) 1 2 -4 >5 Will give # shots indicated? No Yes VFC participation No Yes 21** 5 45** 16 8 25** 15 84** 9 41** 7 57** 34 26 48** 29 87** 25 * Reported if submitting to ALERT or not (n=287), if accessing ALERT or not (n=323) ** P < 0. 05, between levels of each factor
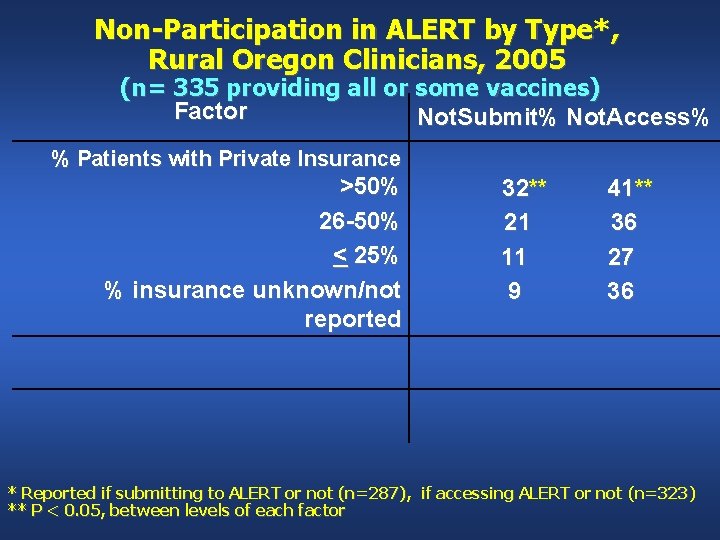
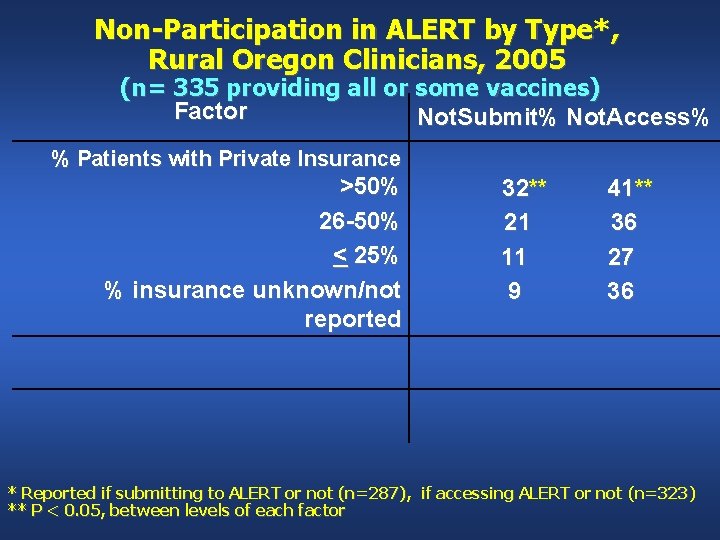
Non-Participation in ALERT by Type*, Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Factor Not. Submit% Not. Access% % Patients with Private Insurance >50% 26 -50% < 25% % insurance unknown/not reported 32** 21 11 9 41** 36 27 36 * Reported if submitting to ALERT or not (n=287), if accessing ALERT or not (n=323) ** P < 0. 05, between levels of each factor
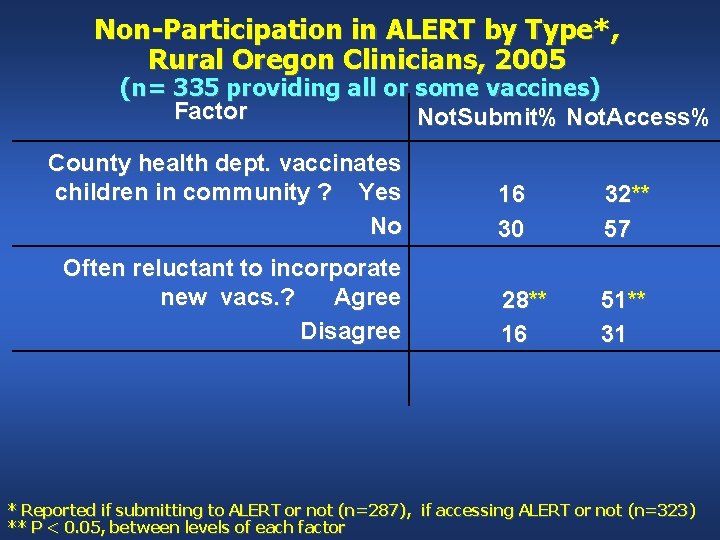
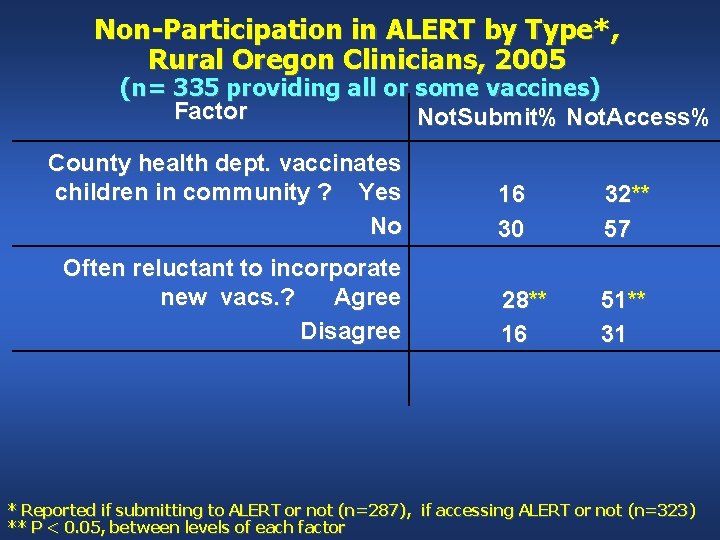
Non-Participation in ALERT by Type*, Rural Oregon Clinicians, 2005 (n= 335 providing all or some vaccines) Factor Not. Submit% Not. Access% County health dept. vaccinates children in community ? Yes No Often reluctant to incorporate new vacs. ? Agree Disagree 16 30 32** 57 28** 16 51** 31 * Reported if submitting to ALERT or not (n=287), if accessing ALERT or not (n=323) ** P < 0. 05, between levels of each factor
