Extreme Makeover Simple Chart Review Transformed into PracticeBased
Extreme Makeover: Simple Chart Review Transformed into Practice-Based Learning Conference Melissa Jefferis, MD Miriam Chan, Pharm. D Riverside Methodist Hospital Family Medicine Residency Columbus, Ohio
Objectives • Review ACGME guidelines, PCMH criteria, and ABFM prerequisites • Identify the practice-based learning (PBL) curriculum needs • Develop a PBL conference • Incorporate patient population management techniques, METRICS, and medication safety management into a PBL curriculum
ACGME Competencies • Practice-based learning and Improvement – Residents must demonstrate the ability to investigate and evaluate their care of patients, to appraise and assimilate scientific evidence, and to continuously improve patient care based on constant self-evaluation and life-long learning.
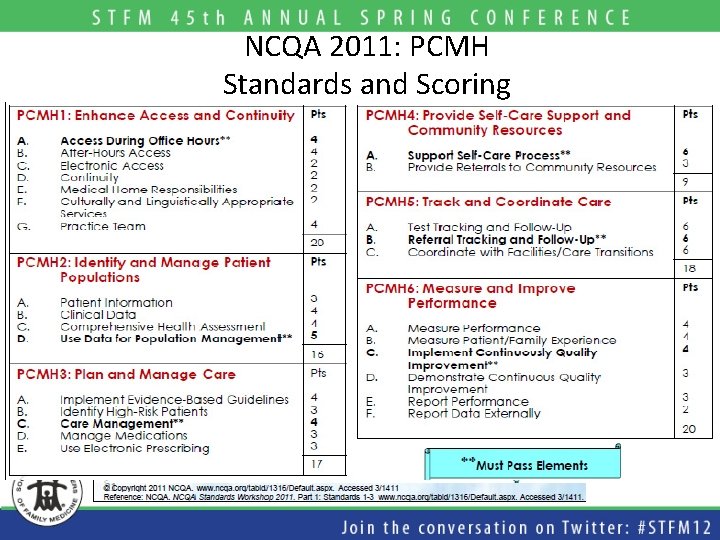
NCQA 2011: PCMH Standards and Scoring
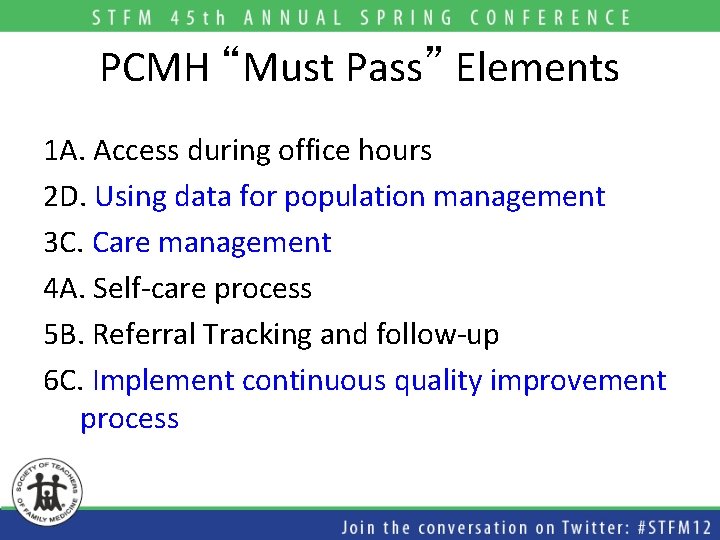
PCMH “Must Pass” Elements 1 A. Access during office hours 2 D. Using data for population management 3 C. Care management 4 A. Self-care process 5 B. Referral Tracking and follow-up 6 C. Implement continuous quality improvement process
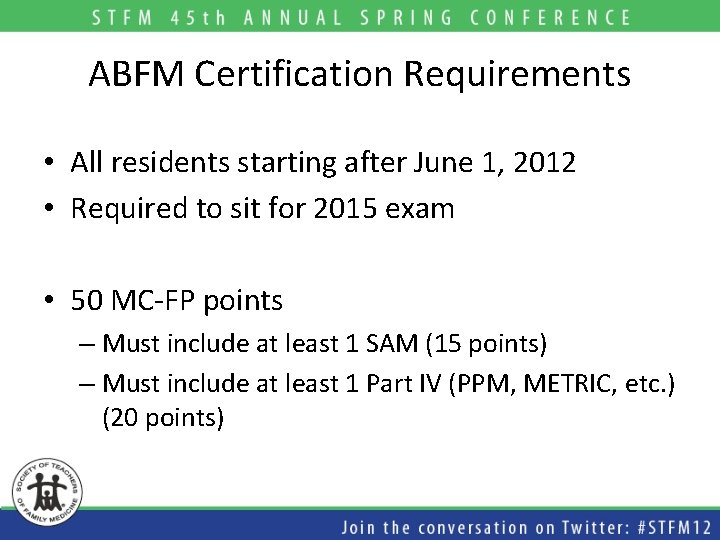
ABFM Certification Requirements • All residents starting after June 1, 2012 • Required to sit for 2015 exam • 50 MC-FP points – Must include at least 1 SAM (15 points) – Must include at least 1 Part IV (PPM, METRIC, etc. ) (20 points)
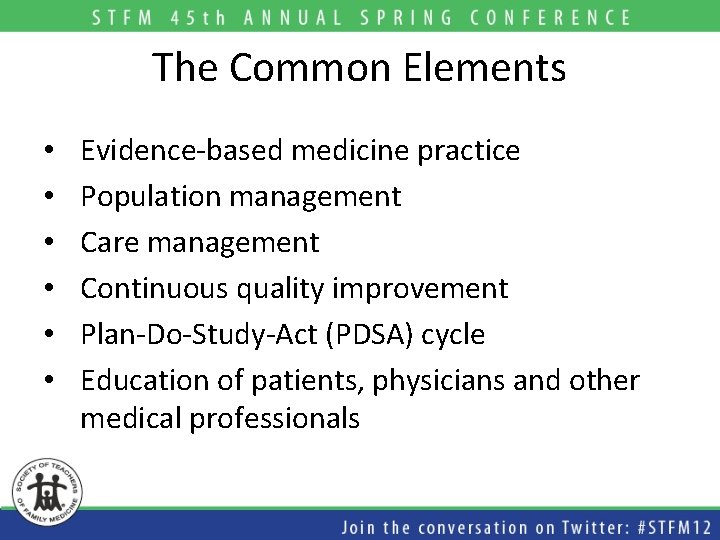
The Common Elements • • • Evidence-based medicine practice Population management Care management Continuous quality improvement Plan-Do-Study-Act (PDSA) cycle Education of patients, physicians and other medical professionals
How Are You Meeting Practice-Based Learning Requirements?
Our Previous PBL Curriculum • Monthly Journal Club – EBM skills and practice • Scholarly activity – Quality and practice improvement projects • Weekly Chart Review – Random topic and patients – Obstetric, pediatric and diabetic patients – Checklist focusing on chart completion Our weakest link
Chart Review

PBL Conference AAFP METRIC Medication Safety Alerts Quality Benchmarks Enhanced OB Chart Review Population Outcomes Management Measurement
Resident Educational Objectives • Skills to investigate and evaluate the quality of patient care • Techniques to mine data from EMR • Experiences in engaging in Plan-Do-Study-Act cycles
PBL Conference • When? • 1 hour per week (Monday 1 pm) • Who? • Residents in the office that afternoon with rotating medical and pharmacy students • Where? • RFPC Conference Room
PBL Conference • PGY 1 – Unable to attend conference due to patient care time in late afternoon and/or Wednesday afternoon • PGY 2 – Attends conference 12 times per year • PGY 3 – Attends conference 16 -20 times per year
PBL Conference • Week 1 • Medication Safety • Week 2 • MGO Metric (screening-based) • Week 3 • AAFP Metric • Week 4 • Enhanced OB Chart Review
PBL Conference • Schedule of conference – 15 minutes: education from faculty regarding diagnosis, documentation, medication interactions, treatment guidelines and process for data abstraction – 45 minutes: residents complete data abstraction for assigned patients

Week 1 Managing Medication Safety Alerts in Riverside Family Practice Center
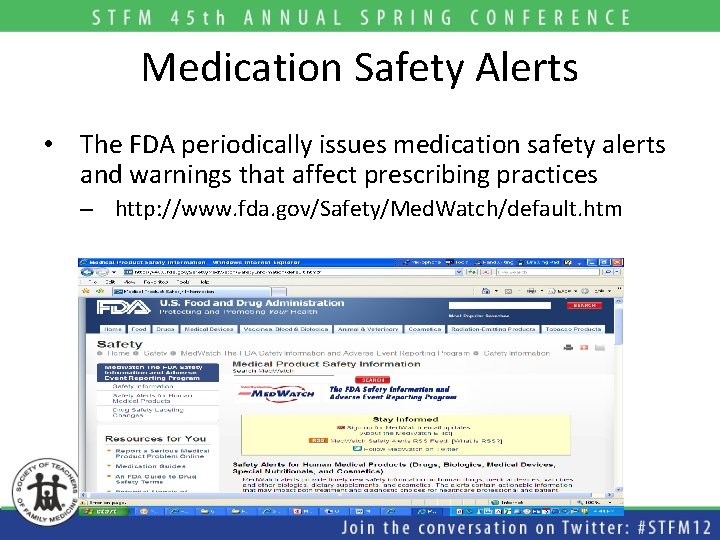
Medication Safety Alerts • The FDA periodically issues medication safety alerts and warnings that affect prescribing practices – http: //www. fda. gov/Safety/Med. Watch/default. htm
Recent Examples • Citalopram related to a potential risk of arrhythmia with doses>40 mg/day • Drug interactions, contraindications, dose limitations for lovastatin • New restrictions, contraindications, dose limitations for simvastatin • Plavix and PPIs potential interactions
Medication Safety in Our PBL Curriculum • Goal: – Teach residents how to manage medication safety alerts • Objectives: – Locate, appraise and assimilate the new evidence-based medication interactions, guidelines, and warnings – Perform population-based approaches to medication safety in the outpatient setting
A 3 -Step Process Education and planning Intervention Monitor outcomes
Step 1: Education and Planning • Review FDA alert and recommendations • Assess risk to patients and implications for the practice • Identify patients who are taking the affected medication • Design a coordinated response and patient letter
Step 2: Intervention • Review chart of affected patients • Alert PCPs of their affected patients in the EMR • Provide PCPs with relevant information and standard patient letter • PCPs take appropriate medication safety measures
Step 3: Monitor Outcomes • Re-run medication list query to identify patients continuing to have the affected medication • Review charts of these patients • Assess impact of intervention – Review process and identify practice/ communication gaps
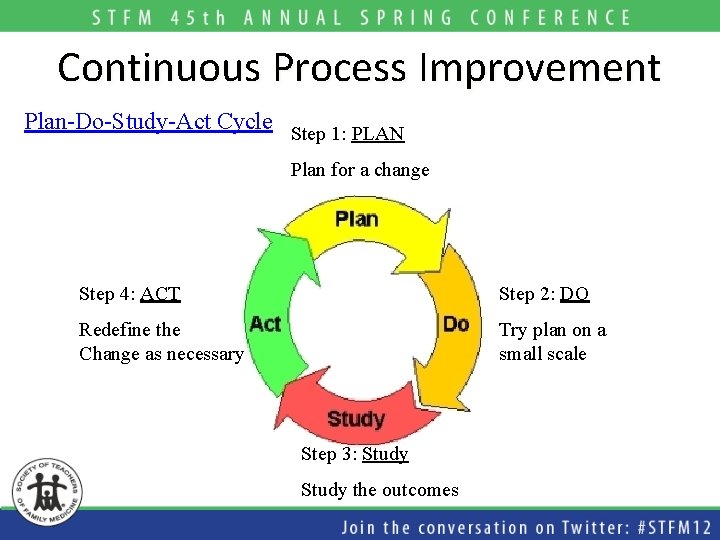
Continuous Process Improvement Plan-Do-Study-Act Cycle Step 1: PLAN Plan for a change Step 4: ACT Step 2: DO Redefine the Change as necessary Try plan on a small scale Step 3: Study the outcomes
For Example • Simvastatin Label Change (6/8/11)
Educate About The Alert • FDA alert – Use of simvastatin when taken at high doses or in combination with several interacting medications • FDA recommendations – New contraindications – Dose limitations for simvastatin when taken with certain other medications • Risk to patients – Simvastatin (80 mg) is associated with increased risk of myopathy
Develop an Action Plan
Evaluate The Alert • Impact to practice – Simvastatin is a common prescribed medication for hyperlipidemia • Generate a listing of patients taking simvastatin 80 mg as well as patients taking simvastatin in combination with other contraindicated medications
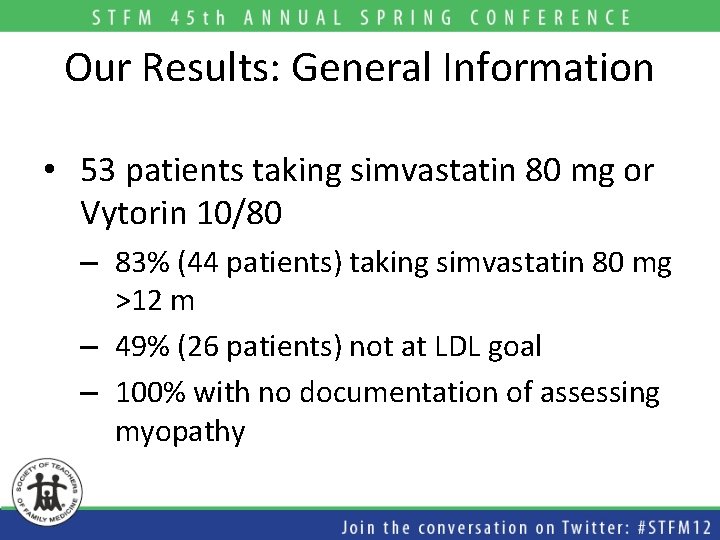
Our Results: General Information • 53 patients taking simvastatin 80 mg or Vytorin 10/80 – 83% (44 patients) taking simvastatin 80 mg >12 m – 49% (26 patients) not at LDL goal – 100% with no documentation of assessing myopathy
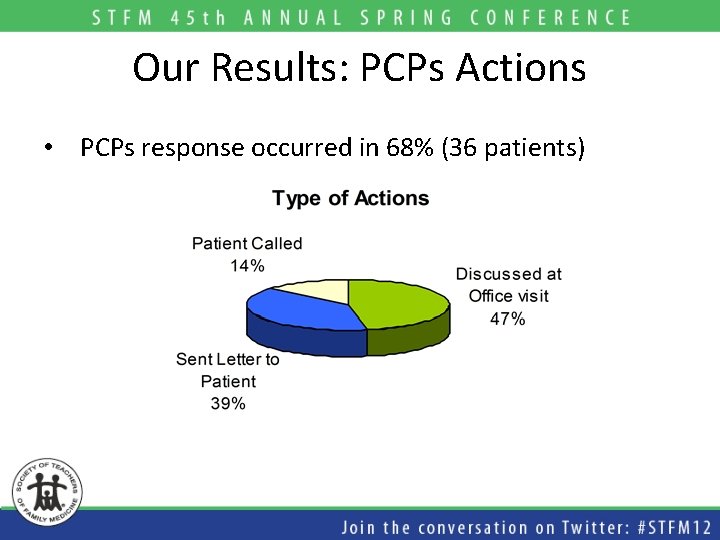
Our Results: PCPs Actions • PCPs response occurred in 68% (36 patients)
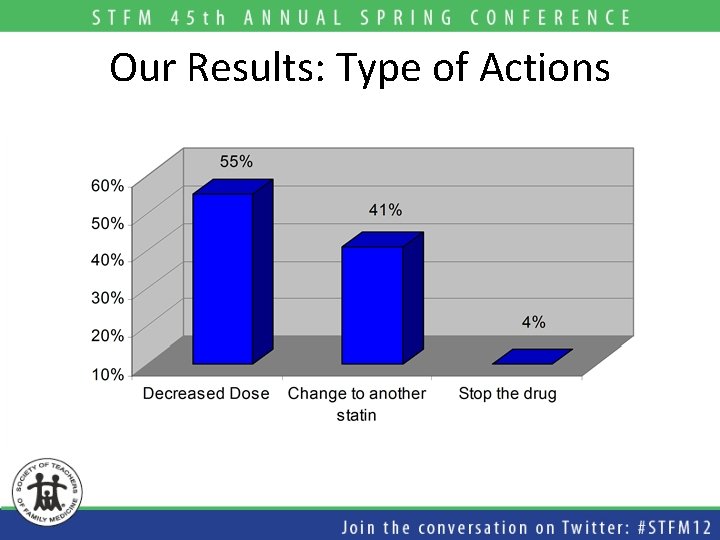
Our Results: Type of Actions
How To Improve PCP Response? 32% (17 patients) did not have any action taken • “Take cover now” VS • “unsurvivable” • “mass devastation” • “catastrophic”
Weeks 2 and 3 Implementing AAFP and MGO METRICs
METRIC Measuring, Evaluating and Translating Research Into Care
Available AAFP METRICs • • • Asthma Chronic Obstructive Pulmonary Disease Coronary Artery Disease Depression Diabetes Geriatrics Hypertension Immunizations for Adolescents Immunizations for High-Risk Adults
AAFP METRICs • Goal: • Teach residents performance improvement • Objectives: • Residents will be able to: • • Use EMR to create patient registry Assess current practice patterns Develop performance improvement plan Study effectiveness of performance improvement plan
A 3 -Step Process Learning from current practice Application of PI plan Evaluation of PI effort
Step 1: Learning from current practice • Use EMR to develop patient registry for each physician participating • Chart review to determine baseline performance data
Step 2: Application of PI Plan • Review baseline data to find poor performance areas • Determine performance improvement plan • Education to physicians and staff regarding plan • Implement the plan
Step 3: Evaluation of PI Effort • Create updated patient registries for participating physicians • Repeat chart review to determine performance • Compare post-intervention to pre-intervention performance
AAFP METRIC Depression
Develop an Action Plan
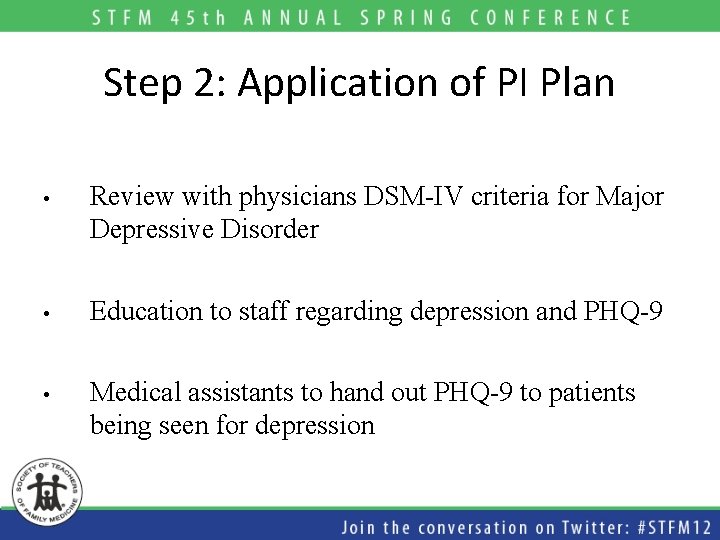
Step 2: Application of PI Plan • Review with physicians DSM-IV criteria for Major Depressive Disorder • Education to staff regarding depression and PHQ-9 • Medical assistants to hand out PHQ-9 to patients being seen for depression
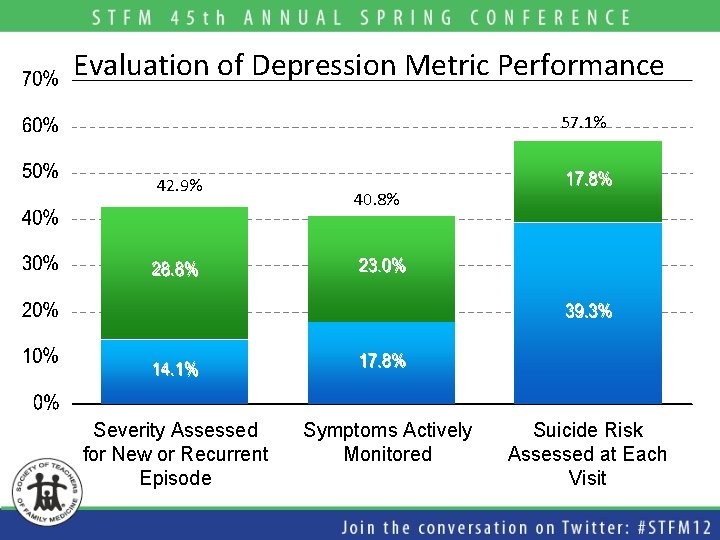
Evaluation of Depression Metric Performance 57. 1% 42. 9% Severity Assessed for New or Recurrent Episode 40. 8% Symptoms Actively Monitored Suicide Risk Assessed at Each Visit
RFPC Data • Interns do not have the patient numbers required for participation • Staff participation varied with handing out PHQ-9
Week 4 Enhanced OB Chart Review

OB Chart Review • Previously – Monthly chart review of OB patients at 36 weeks gestation. – Used a paper form to review a paper chart for completeness. • Currently – Monthly chart review using a paper form to review an EMR chart for completeness.
NCQA PCPI Guidelines • Prenatal Measures – Establishment of Gestational Age – Prenatal Care Screening – Behavioral Health Risk Assessment – BMI Assessment and recommended weight gain • Doing very well at #1 and #2. Need to revise forms to gather more applicable data for the rest
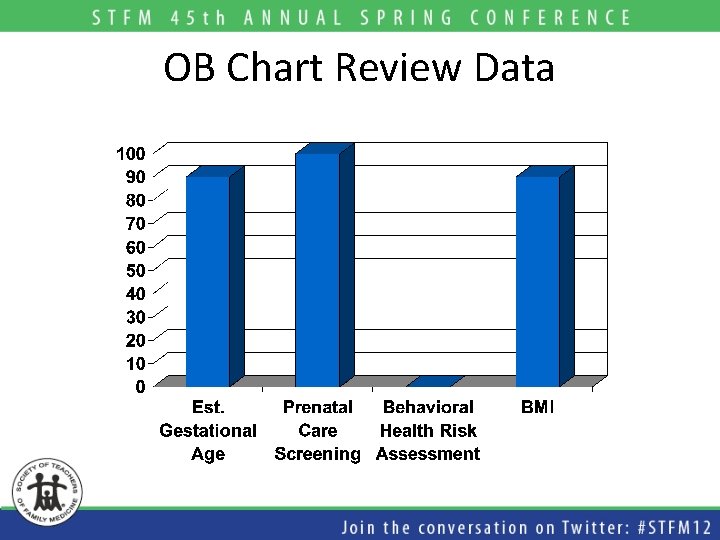
OB Chart Review Data

Future Projects: Medication Safety • Citalopram (Celexa) Dosing Considerations in Geriatric Patients • Aliskiren (Tekturna) Containing Medications in Chronic Renal Disease and Diabetic Patients • New FDA Medication Alerts
Future Projects: Performance Improvement • Preventative Care Measures (MGO) – Colorectal Cancer Screening – Partnership with Ohio Academy of Family Physicians • AAFP Metrics – Hypertension – Core disease state for PCMH Application – Workgroup across Ohio. Health addressing documentation issues
Future Projects: OB • Labor and Delivery Measures – – – Elective Delivery Before 39 Weeks Cesarean Delivery for Low-Risk Nulliparous Episiotomy Spontaneous Labor and Birth Care Coordination: prenatal record present at delivery • Postpartum Measures – Breastfeeding rate – Postpartum Follow-up Rate
Conclusions • We hope that our experience has helped you: – Evaluate your current practice-based learning curriculum – Find your educational need – Create your own customized PBL curriculum
Questions?
- Slides: 56