Extrahepatic Biliary and Vascular Injuries Niqui Kiffin MD
Extrahepatic Biliary and Vascular Injuries Niqui Kiffin, MD 16 March 2010
Introduction l l Extrahepatic biliary and portal triad injuries make up 0. 07 -. 21% of all trauma admissions. Although rare, detection and management may be very difficult Injury to this area may carry a 50% mortality, with injury to the vascular structures being worse Most patients do not have an inury to one structure or another, but actually have a combination of injuries to multiple organs l l l Liver Porta Vena Cava Pancreas Surrounding viscera
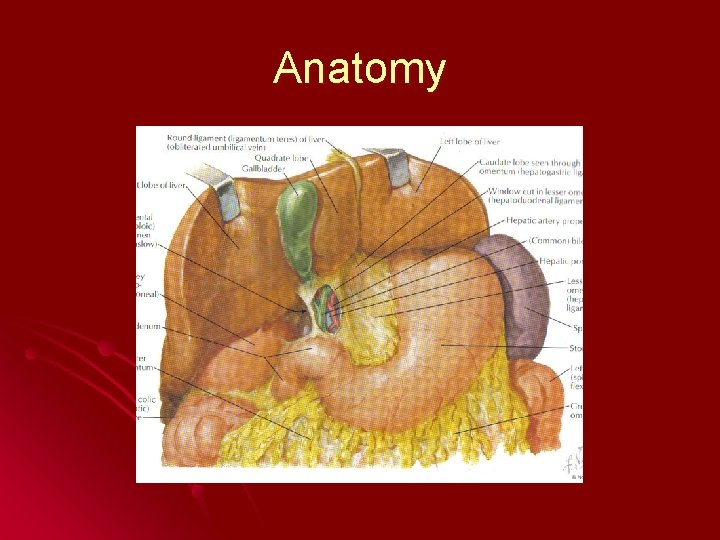
Anatomy

Discussion Gallbladder l Portal Vein l Hepatic Artery l Common Bile Duct l Pancreaticoduodenectomy l

Gallbladder Accounts for up to 66% of extrahepatic biliary tract injury l May be either blunt or penetrating l l Blunt l Avulsion l Contusion l Perforation l Penetrating l May duct involve anywhere from the body to the cystic
Diagnosis l Physical Exam l l Bile Peritonitis/RUQ Pain Late l l CT Scan l l Ill-defined contour of the GB wall Collapse of the lumen Intraluminal Hemorrhage Ultrasound l l Cholecystitis – blockage of the cystic duct with blood clots Has not been formally evaluated Laparotomy
Operative Management l Open Cholecystectomy l l l Laparoscopic Cholecystectomy l l Not recommended GB rarely injured alone Other injuries missed Non-operatively l l l Almost every case Must also be considered in patient’s where there is injury to cystic duct or R Hepatic Artery Minor GB contusions May lead to cholecystitis or rupture in the future Cholecystorraphy l Minor GB lacerations
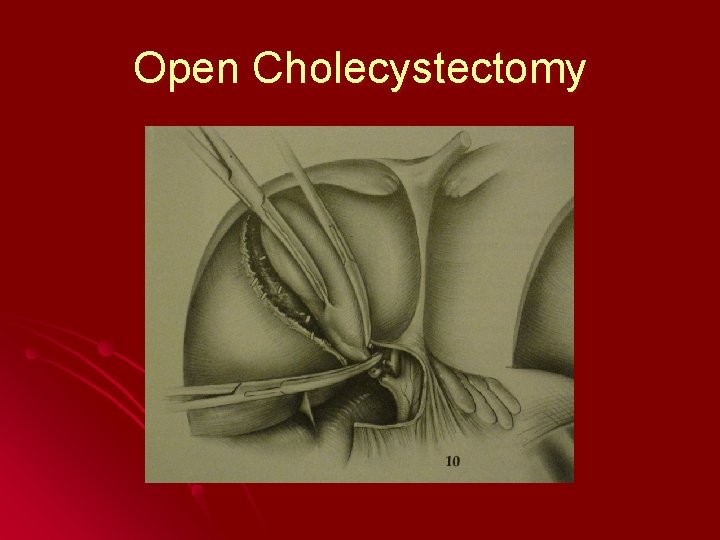
Open Cholecystectomy

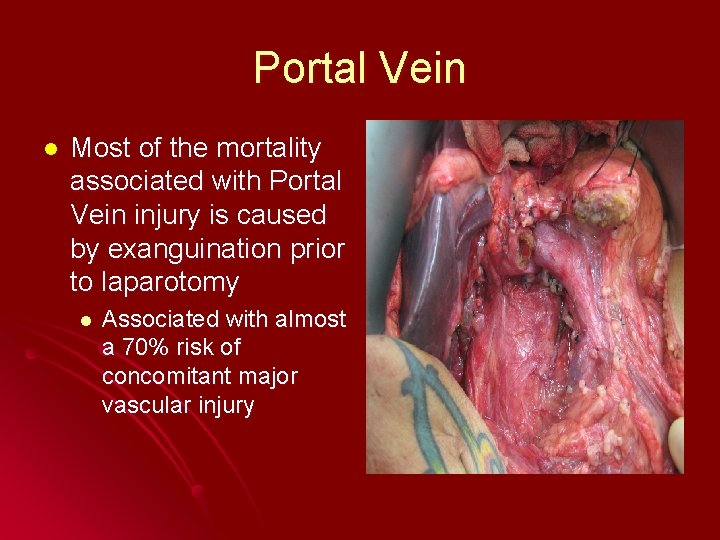
Portal Vein l Most of the mortality associated with Portal Vein injury is caused by exanguination prior to laparotomy l Associated with almost a 70% risk of concomitant major vascular injury

Location of Portal Vein Injury l The location of the injury is most likely within the hepatoduodenal ligament. l Look for hematoma or bleeding around/within the hepatoduodenal ligament during laparotomy
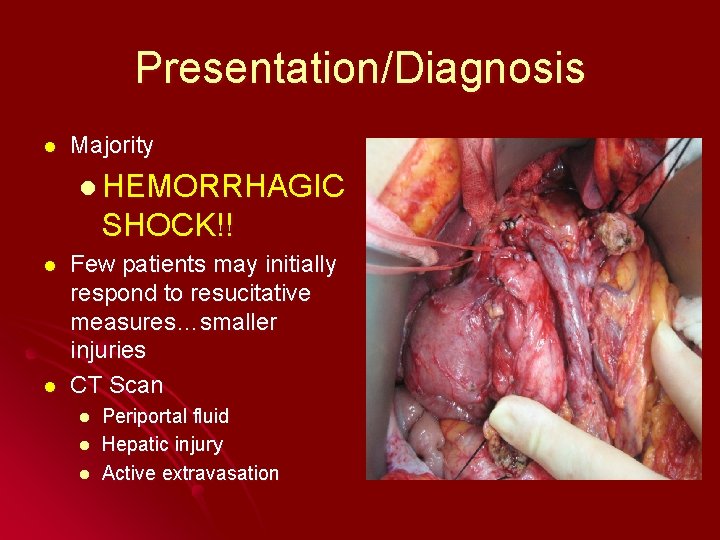
Presentation/Diagnosis l Majority l HEMORRHAGIC SHOCK!! l l Few patients may initially respond to resucitative measures…smaller injuries CT Scan l l l Periportal fluid Hepatic injury Active extravasation
Operative Management l Again, patients usually arrive in hemorrhagic shock…therefore treat with the same initial principles. l Midline Laparotomy l Evacuation of clots/hemoperitoneum l Urgent Packing l Allow for the Anesthesia team to catch up with blood products/fluid
Operative Management l Right-sided medial visceral rotation l Mobilize the ascending colon and hepatic flexure to expose the duodenum, head of the pancreas and IVC Initial control, may be obtained by a Pringle Manuever, manual compression or pressure packs l If possible obtain proximal and distal control l
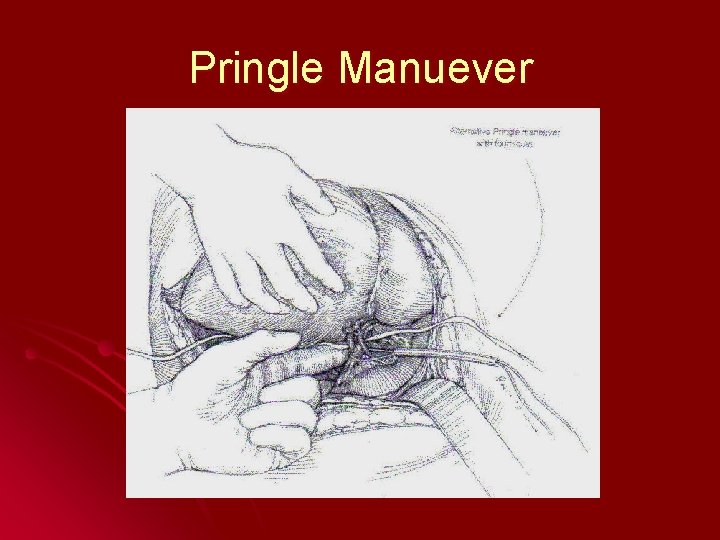
Pringle Manuever

Operative Management l l Lateral Venorrhaphy Saphenous Vein/Interposition Grafts End-to-End Primary Repair Portal Caval Shunt l l Directly above the injury Superior Mesenteric to Splenic Vein shunts
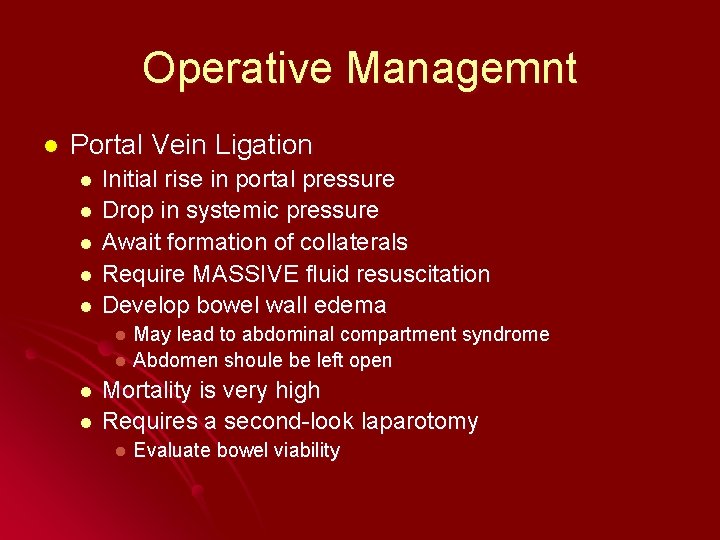
Operative Managemnt l Portal Vein Ligation l l l Initial rise in portal pressure Drop in systemic pressure Await formation of collaterals Require MASSIVE fluid resuscitation Develop bowel wall edema May lead to abdominal compartment syndrome l Abdomen shoule be left open l l l Mortality is very high Requires a second-look laparotomy l Evaluate bowel viability
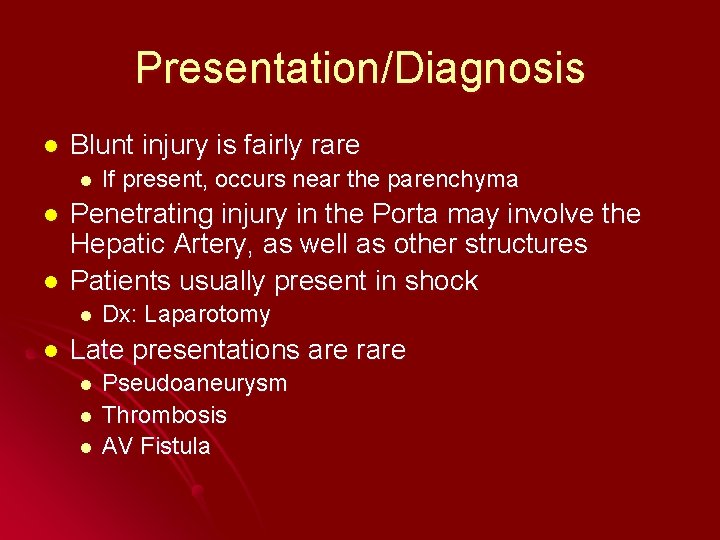
Presentation/Diagnosis l Blunt injury is fairly rare l l l Penetrating injury in the Porta may involve the Hepatic Artery, as well as other structures Patients usually present in shock l l If present, occurs near the parenchyma Dx: Laparotomy Late presentations are rare l l l Pseudoaneurysm Thrombosis AV Fistula
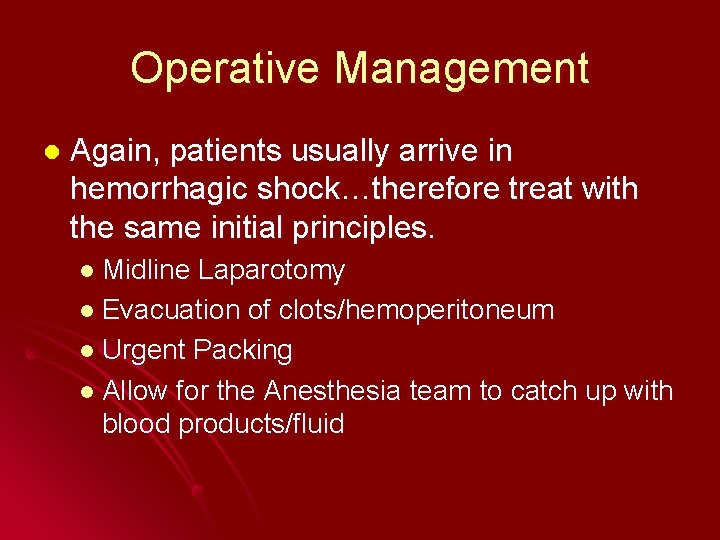
Operative Management l Again, patients usually arrive in hemorrhagic shock…therefore treat with the same initial principles. l Midline Laparotomy l Evacuation of clots/hemoperitoneum l Urgent Packing l Allow for the Anesthesia team to catch up with blood products/fluid
Operative Management l l l Again, mobilize the ascending colon and hepatic flexure for adequate exposure and visualization. Manual compression/Pringle Manuever Primary Repair Interposition Grafts Hepatic Artery Ligation l l l Approximately 75% of blood flow via the portal system Even so, ligation of the Hepatic Artery should only be done in extreme circumstances because there have been reports of hepatic ischemia and necrosis Also, remember to also perform a cholecystectomy
Hepatic Artery – Primary Repair

Common Bile Duct l Occurs most commonly with penetrating injury l Usually l partial transection If injured via blunt mechanism, it usually occurs where the bile duct is fixed to nearby structures (pancreaticoduodenal junction) l Usually complete transection
Diagnosis l Early l During laparotomy, pt in shock with multiple injuries l l l Liver Pancreas Duodenum Vascular Late l 24 hr – 6 wks l l l Jaundice Abdominal distension/Pain Intolerence to TF Sepsis Bilious Ascites
Evaluation l CT Scan l Usually nonspecific l l l Pancreatic head fullness Duodenal thickening Portal edema DPL l Lack of specificity l l l Injuries to other structures may also produce bile Bile may be obscured by the presence of blood Laparotomy (may require a cholangiogram) l l Cannot differentiate blood from bile Bile staining Late Presenters l May require CT Scan, U/S, or ERCP
Operative Management l l Address CBD only after hemorrhage is controlled. Damage Control – Drainage l l l Jackson-Pratt T-Tube “Stable” Patients l 4 Types of Injuries Avulsion of cystic duct/small laceration l Transection without tissue loss l Extensive defect in the wall l Segmental loss of ductal tissue l
Avulsion of Cystic Duct l Primary repair l 6 -0 Prolene l Be careful not to narrow duct l Consider using a piece of the cystic duct or gallbladder wall l May require a T-Tube l Be aware that some techniques used to place Ttube may actually damage the duct l ERCP with Stent Placement
Transection (No tissue loss) l End-to-End Anastomosis l Minimal l Devascularization will lead to stricture at a later date which may require an enteric conversion l No l dissection tension Devascularization will lead to stricture at a later date which may require an enteric conversion
Extensive Defects (Tissue Loss) l Biliary Enteric Anastomosis l Roux-en-Y hepaticojejunostomy l May even be sutured at the bifurcation or even the hilar plate l Roux-en-Y l choledochojejunostomy Vascularity is crucial… l Cholecystojejunostomy l Patent cystic duct is necessary l Viable solution in patients with small caliber ducts or unstable patients
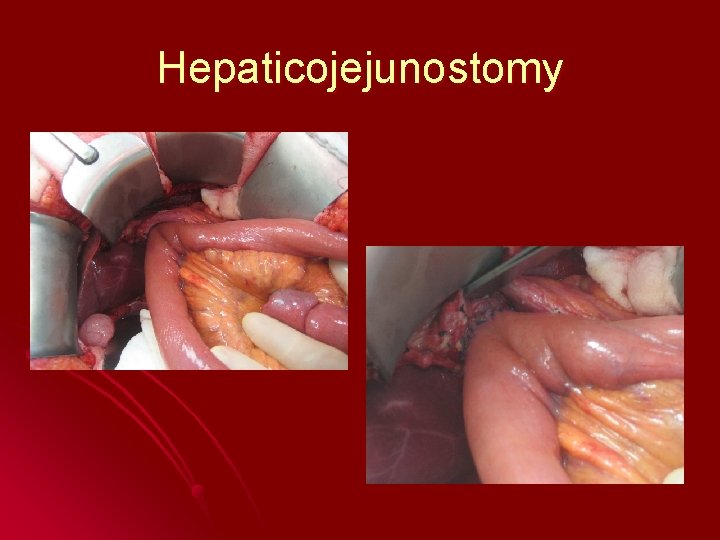
Hepaticojejunostomy
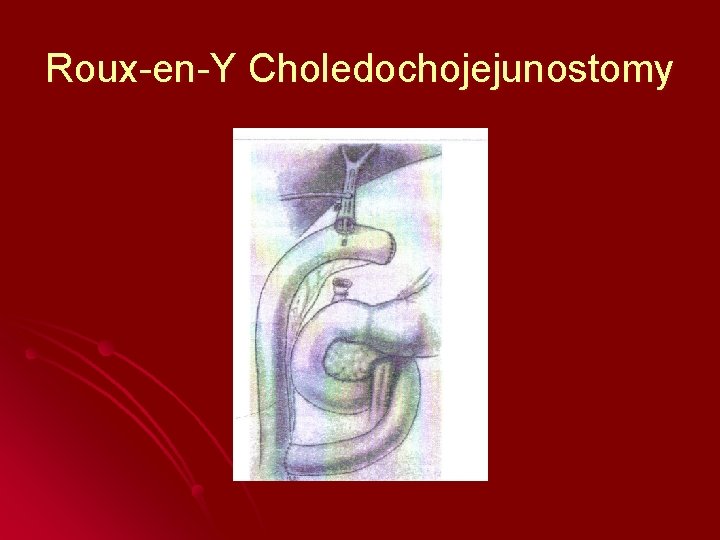
Roux-en-Y Choledochojejunostomy
Extensive Defects (Tissue Loss) l Ligation of Hepatic Duct (Right or Left) l Usually leads to atrophy of the affected side, not biliary cirrhosis
To Stent or Not To Stent? l Stent l Allows for decompression l Allows access for cholangiography l T-tubes must exit outside the repair area or stricture will result l No Stent l Foreign body in an already small duct promotes stricture or obstruction l Use at your discretion…
Ampulla/Intrapancreatic Injury Consider pancreaticoduodenectomy if duodenum and pancreas are also injured. l If not, consider transduodenal sphinteroplasty or ampullary reimplantation l l Consider more specialized consultation
Pancreaticoduodenectomy l l Whipple Procedure aka Pancreaticoduodenectomy may be required for severe duodenal injuries that involve the main pancreatic duct and the CBD or ampulla Indications include: l l l Massive, uncontrollable bleeding from the HOP or adjacent vascular structures Massive and unreconstructable injury to the main pancreatic duct in the head Combined unreconstructable injuries of: l l Duodenum and HOP Duodenum, HOP, and CBD Almost never performed during the 1 st operation Approximately 30 -40% mortality rate with patients that require trauma Whipple
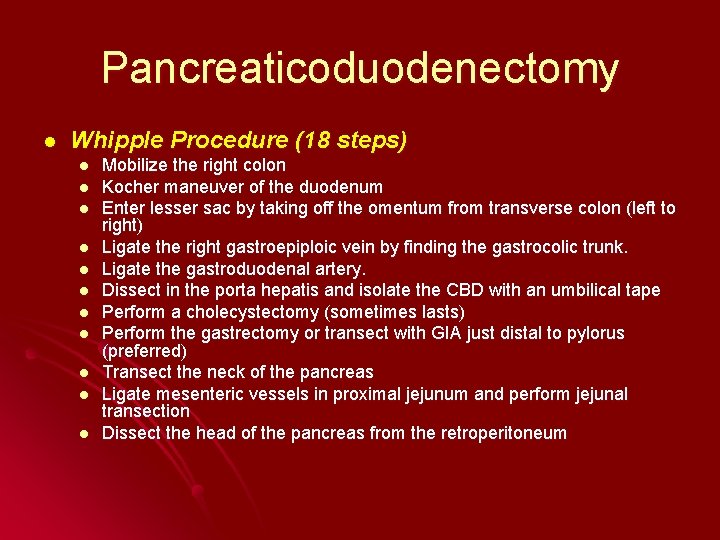
Pancreaticoduodenectomy l Whipple Procedure (18 steps) l l l Mobilize the right colon Kocher maneuver of the duodenum Enter lesser sac by taking off the omentum from transverse colon (left to right) Ligate the right gastroepiploic vein by finding the gastrocolic trunk. Ligate the gastroduodenal artery. Dissect in the porta hepatis and isolate the CBD with an umbilical tape Perform a cholecystectomy (sometimes lasts) Perform the gastrectomy or transect with GIA just distal to pylorus (preferred) Transect the neck of the pancreas Ligate mesenteric vessels in proximal jejunum and perform jejunal transection Dissect the head of the pancreas from the retroperitoneum
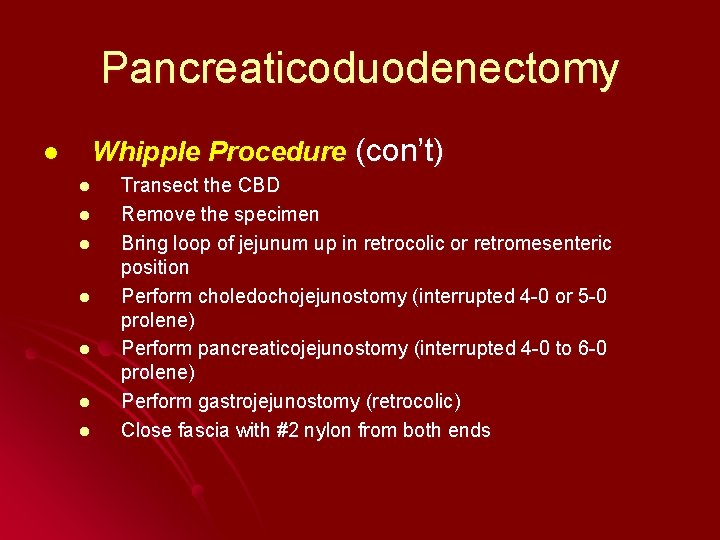
Pancreaticoduodenectomy l Whipple Procedure (con’t) l l l l Transect the CBD Remove the specimen Bring loop of jejunum up in retrocolic or retromesenteric position Perform choledochojejunostomy (interrupted 4 -0 or 5 -0 prolene) Perform pancreaticojejunostomy (interrupted 4 -0 to 6 -0 prolene) Perform gastrojejunostomy (retrocolic) Close fascia with #2 nylon from both ends

Whipple (No Reconstruction)
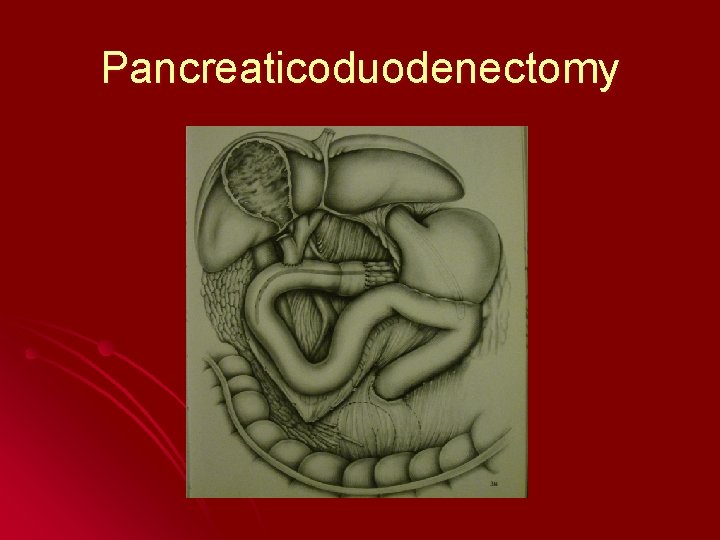
Pancreaticoduodenectomy
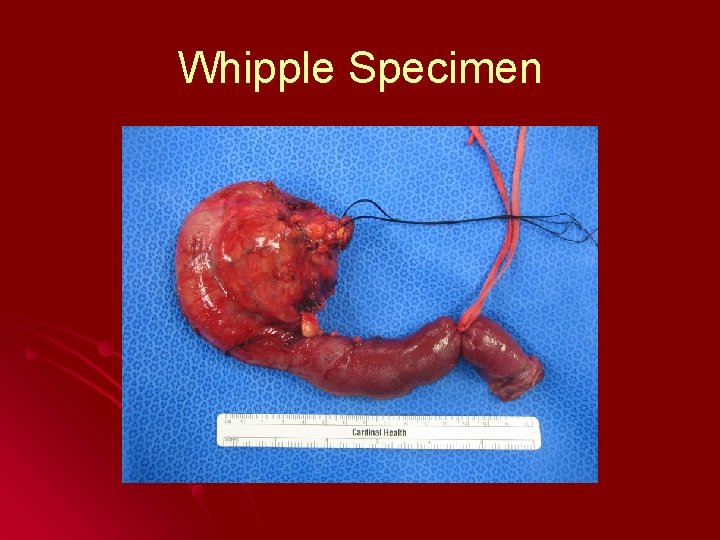
Whipple Specimen
Conclusion l l l Injuries to the extrahepatic biliary and vascular stuctures are very rare. They are closely located to multiple major organs (liver, duodenum, pancreas), therefore their injury may be masked by greater destruction. As a Trauma surgeon, one must be aware of multiple techniques on how to quickly access these structures and make rapid decisions about repair verses damage control manuevers.
References… Feliciano DV, Mattox KL, Moore EE: Trauma 6 th Ed: CH 32 Liver and Biliary Tract; 2008 l van Heerden JA, Farley DR: Operative Techniques in General Surgery Vol 2, No 3; Complex Hepatc Injuries 206 -20; 2000 l
- Slides: 44