EXTRACAPSULAR EXTENSION IN OROPHARYNGEAL CARCINOMA THE HPV ERA



- Slides: 51

EXTRACAPSULAR EXTENSION IN OROPHARYNGEAL CARCINOMA: THE HPV ERA THOMAS J. GAL, MD, MPH, FACS PROFESSOR, DIVISION OF HEAD AND NECK ONCOLOGY DEPARTMENT OF OTOLARYNGOLOGY UNIVERSITY OF KENTUCKY LEXINGTON, KY
THANK YOU • As a clinical researcher, I rely on your efforts • • • SEER NCDB Internal research • Kentucky Cancer Registry • Markey Cancer Center
WHY ME? • • Professor, Division of Head and Neck Oncology Masters of Public Health • • • Cancer Epidemiology Over 50 publication in Otolaryngology • • • University of Washington Skull base Maxillofacial trauma Head and Neck Oncology Microvascular reconstruction Most meaningful work comes from database analysis • Your work counts!
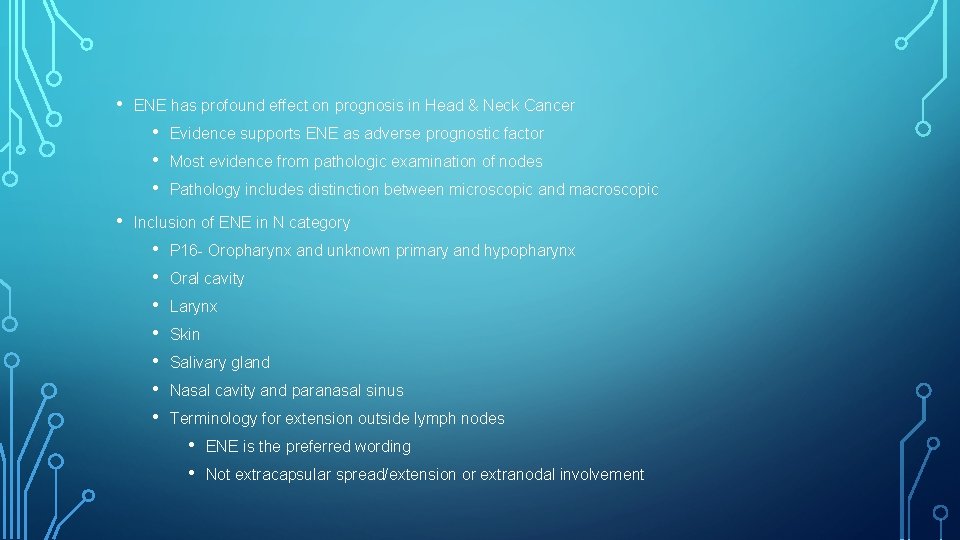
TOPIC TODAY • Oropharyngeal Carcinoma • Extracapsular Spread • • Extranodal Extension Extracapsular Extension • Extranodal Extension (ENE) considered best nomenclature
IMPACT OF EXTRANODAL EXTENSION • 1980’s • • • Decreased survival Increased risk of distant metastatic disease More aggressive pathology More aggressive therapy More aggressive chemotherapy
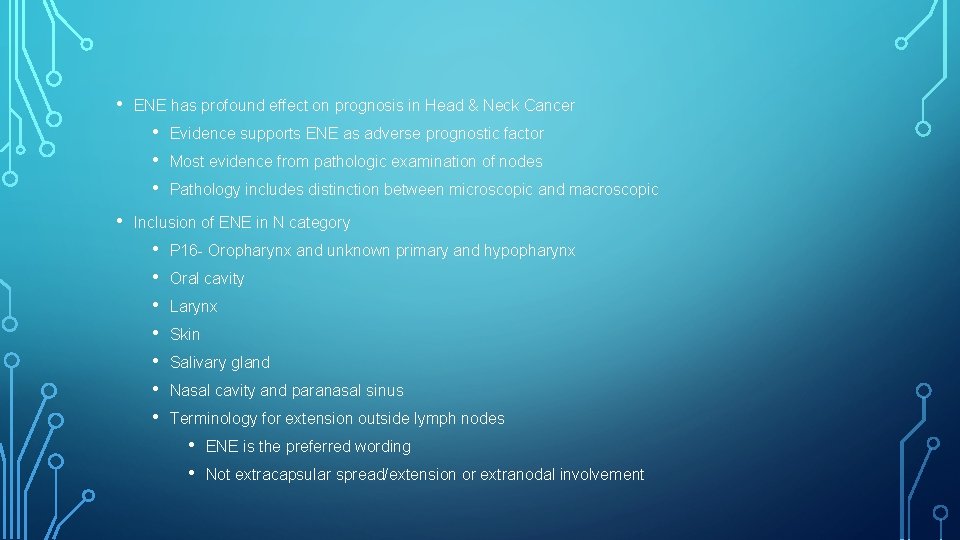
• ENE has profound effect on prognosis in Head & Neck Cancer • • Evidence supports ENE as adverse prognostic factor Most evidence from pathologic examination of nodes Pathology includes distinction between microscopic and macroscopic Inclusion of ENE in N category • • P 16 - Oropharynx and unknown primary and hypopharynx Oral cavity Larynx Skin Salivary gland Nasal cavity and paranasal sinus Terminology for extension outside lymph nodes • • ENE is the preferred wording Not extracapsular spread/extension or extranodal involvement
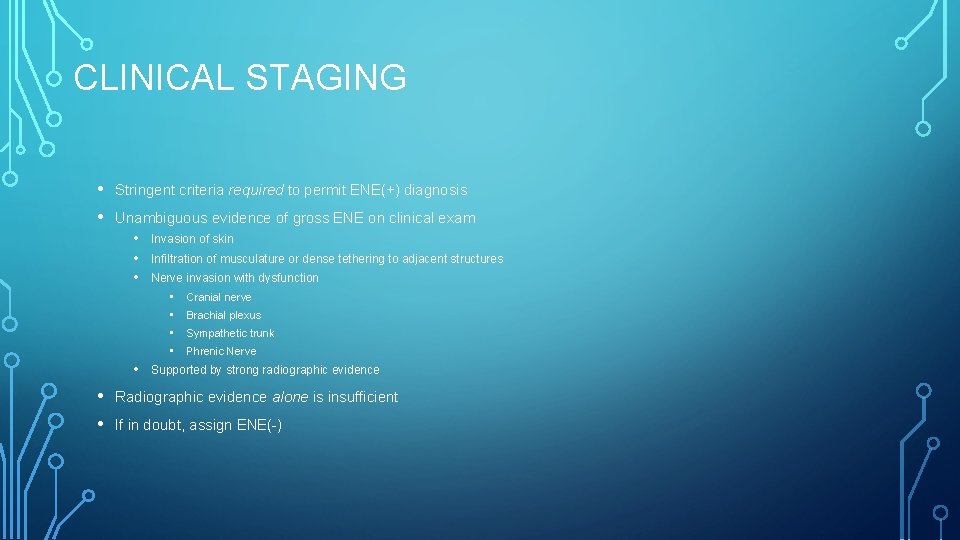
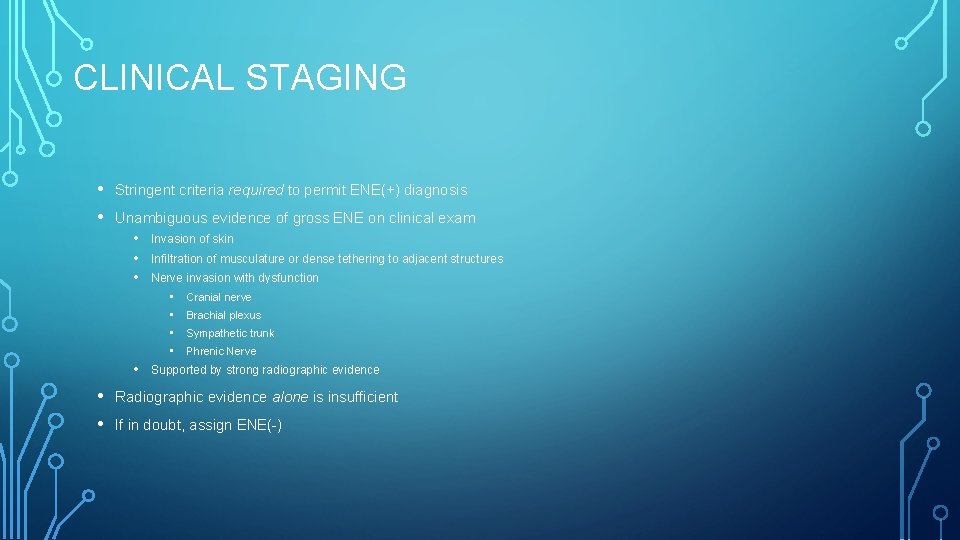
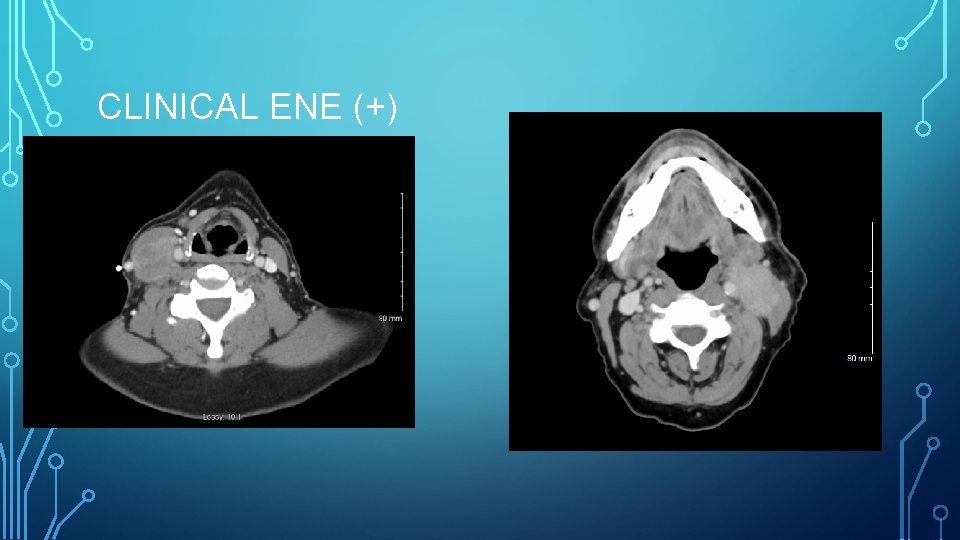
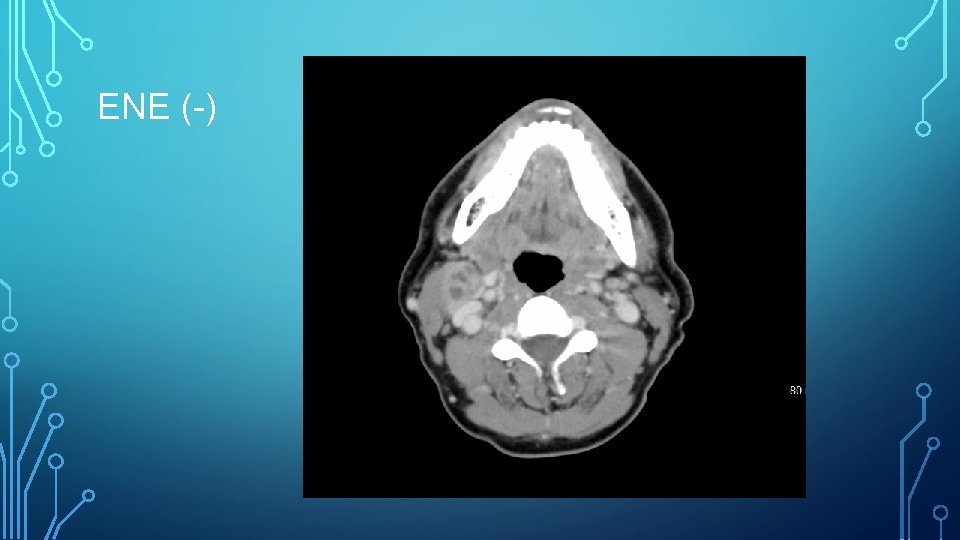
CLINICAL STAGING • • Stringent criteria required to permit ENE(+) diagnosis Unambiguous evidence of gross ENE on clinical exam • Invasion of skin • Infiltration of musculature or dense tethering to adjacent structures • Nerve invasion with dysfunction • • Cranial nerve Brachial plexus Sympathetic trunk Phrenic Nerve Supported by strong radiographic evidence Radiographic evidence alone is insufficient If in doubt, assign ENE(-)
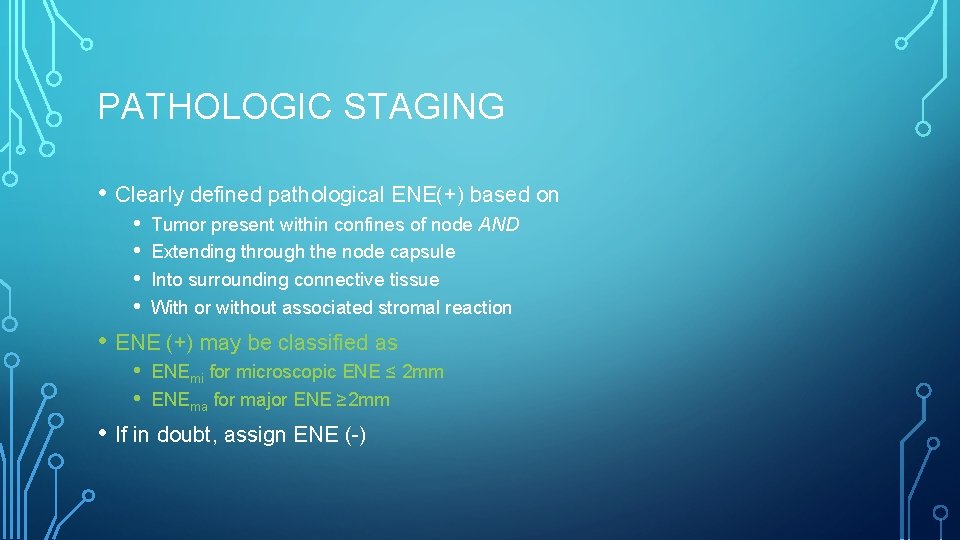
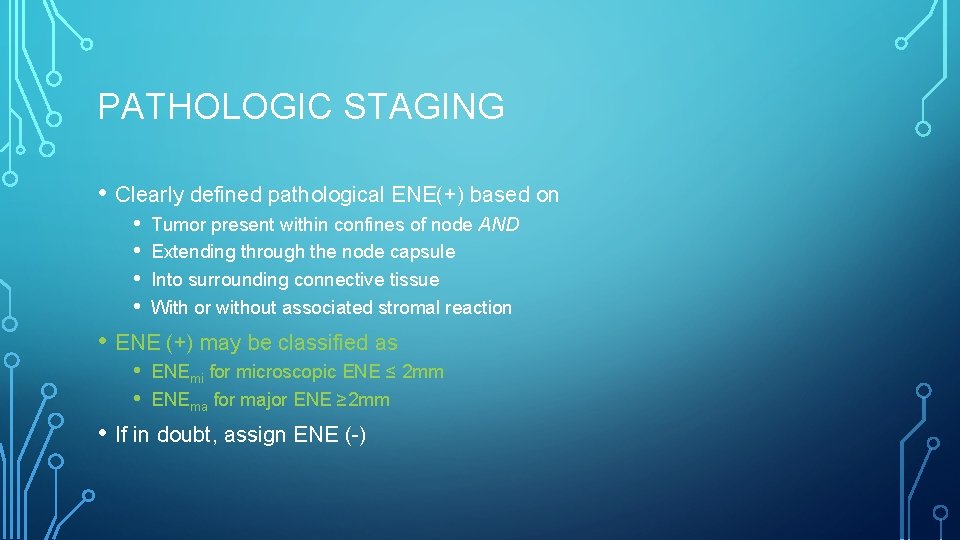
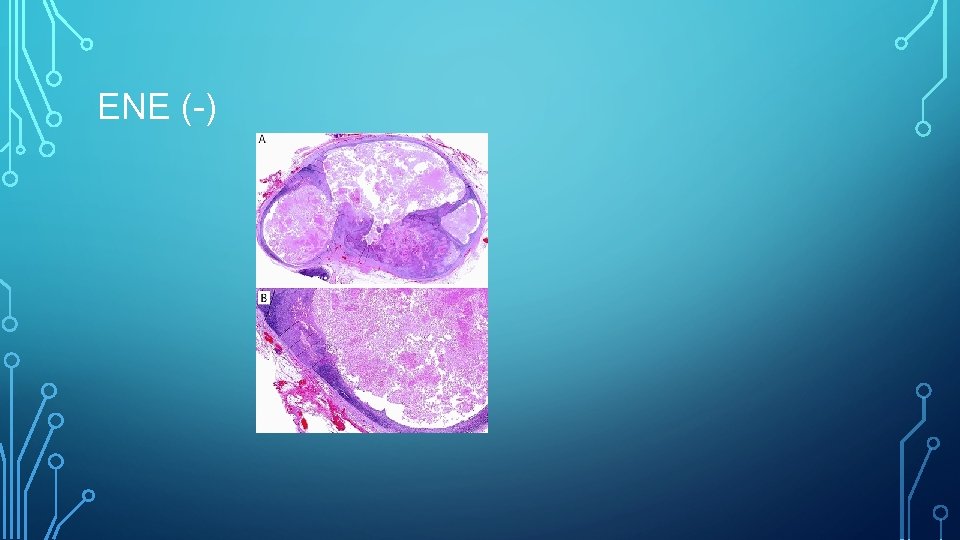
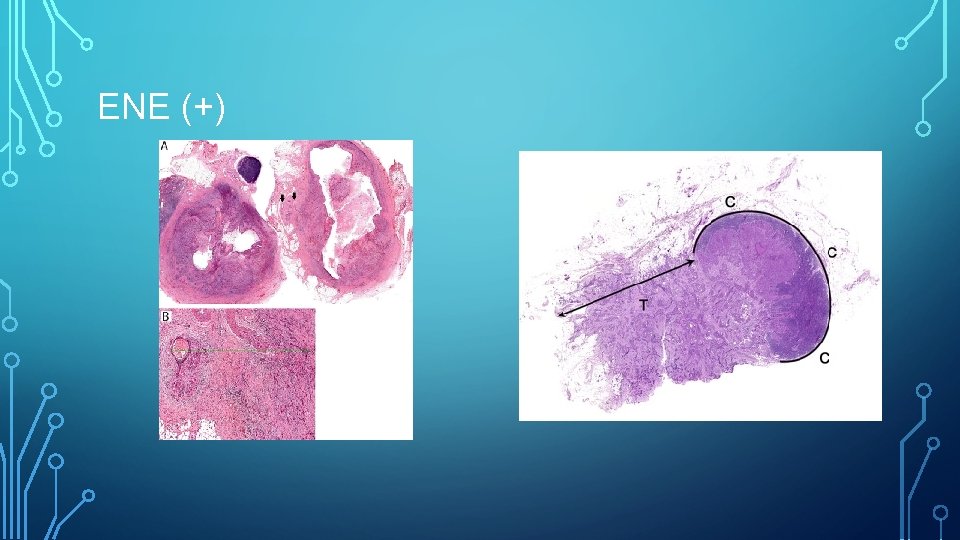
PATHOLOGIC STAGING • Clearly defined pathological ENE(+) based on • • Tumor present within confines of node AND Extending through the node capsule Into surrounding connective tissue With or without associated stromal reaction • ENE (+) may be classified as • • ENEmi for microscopic ENE ≤ 2 mm ENEma for major ENE ≥ 2 mm • If in doubt, assign ENE (-)
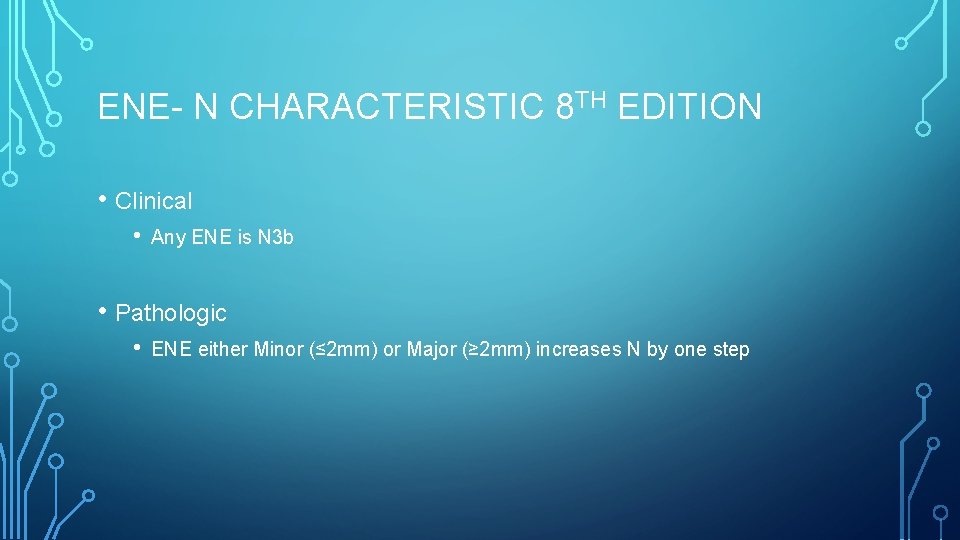
ENE- N CHARACTERISTIC 8 TH EDITION • Clinical • Any ENE is N 3 b • Pathologic • ENE either Minor (≤ 2 mm) or Major (≥ 2 mm) increases N by one step
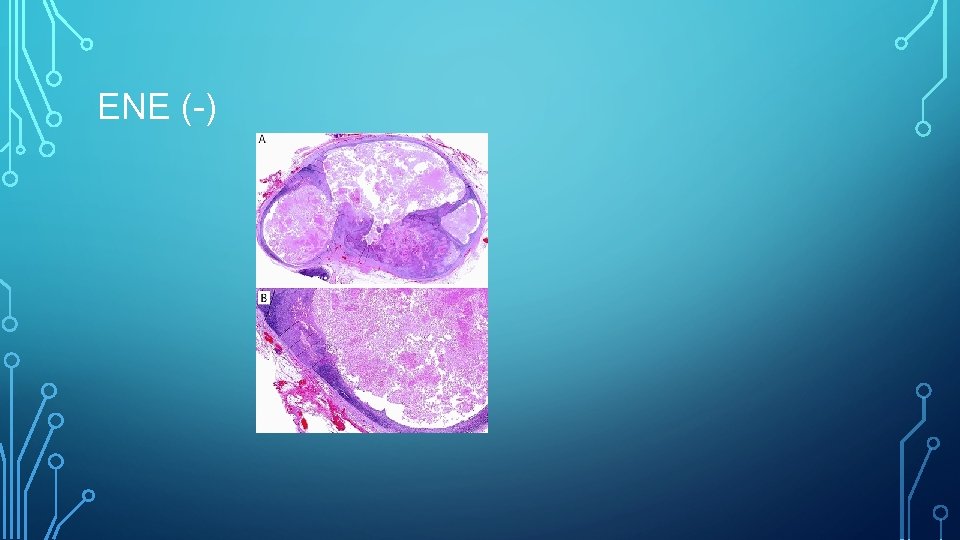
ENE (-)
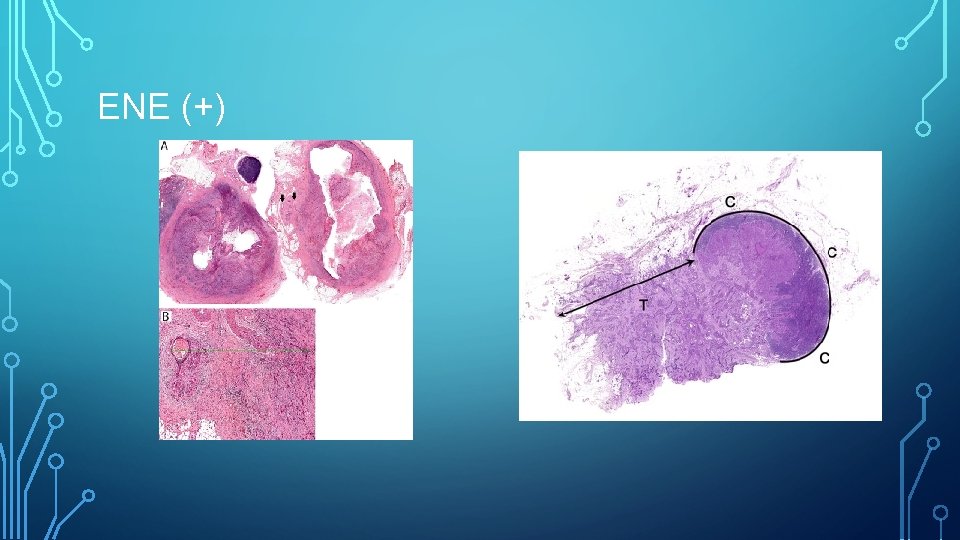
ENE (+)
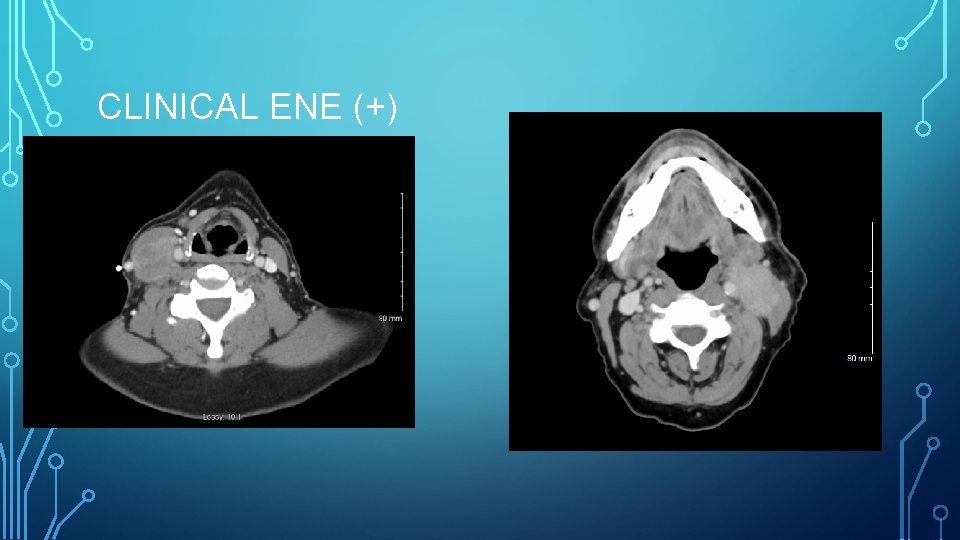
CLINICAL ENE (+)
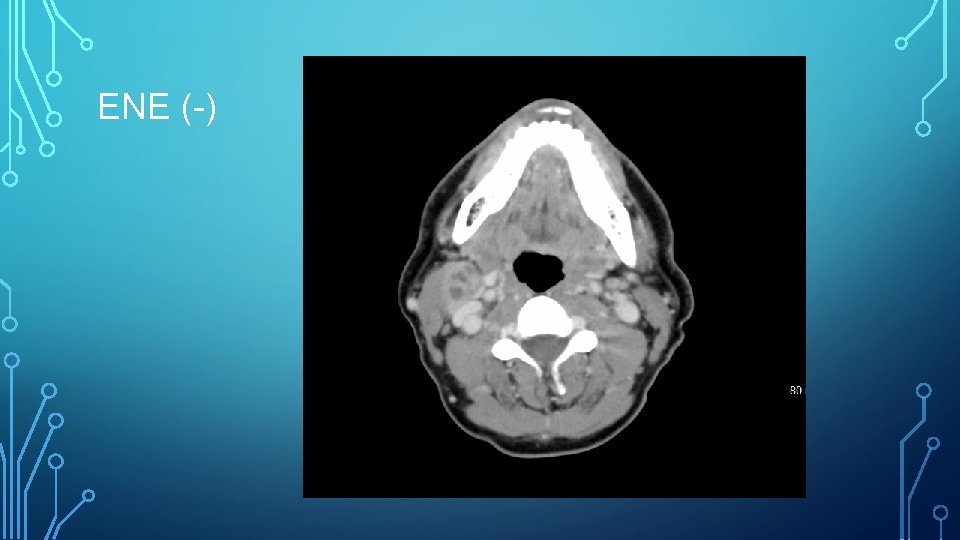
ENE (-)
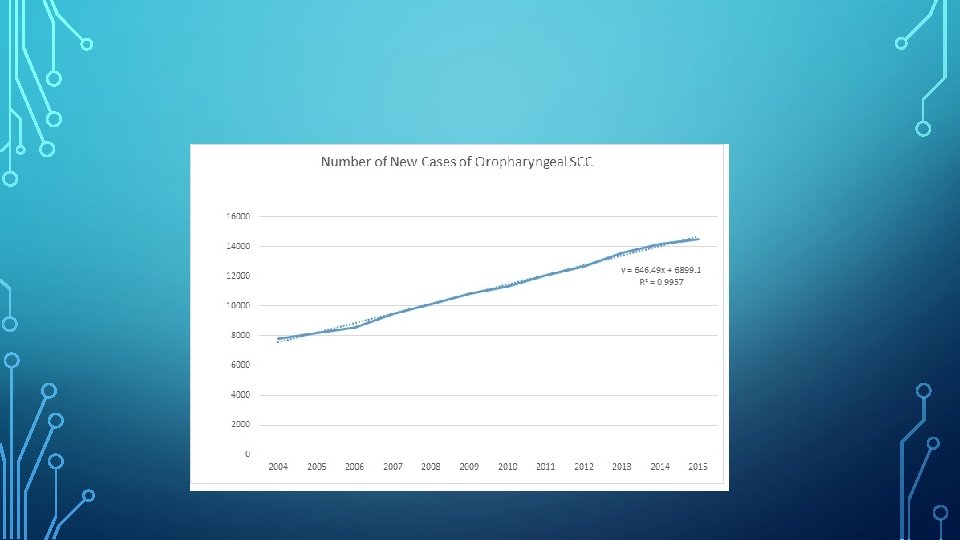
EXTRANODAL EXTENSION: WHY HAS THIS CHANGED? • • Human Papillomavirus (HPV) Distinct pathologic entity • • • Non-smokers Younger Viral Favorable treatment profile Treatment De-escalation? No significant change in risk for smoking-related “garden variety” head and neck cancer • But what about this?
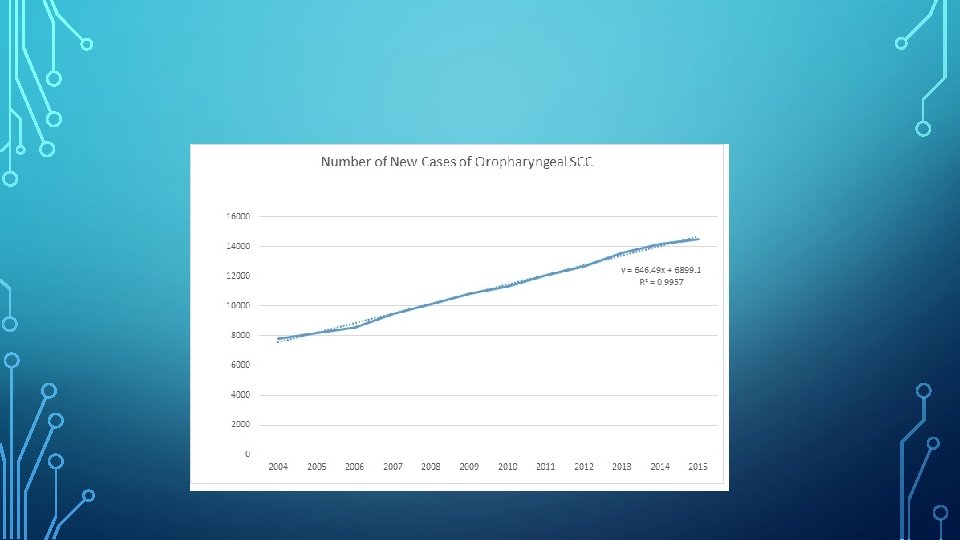
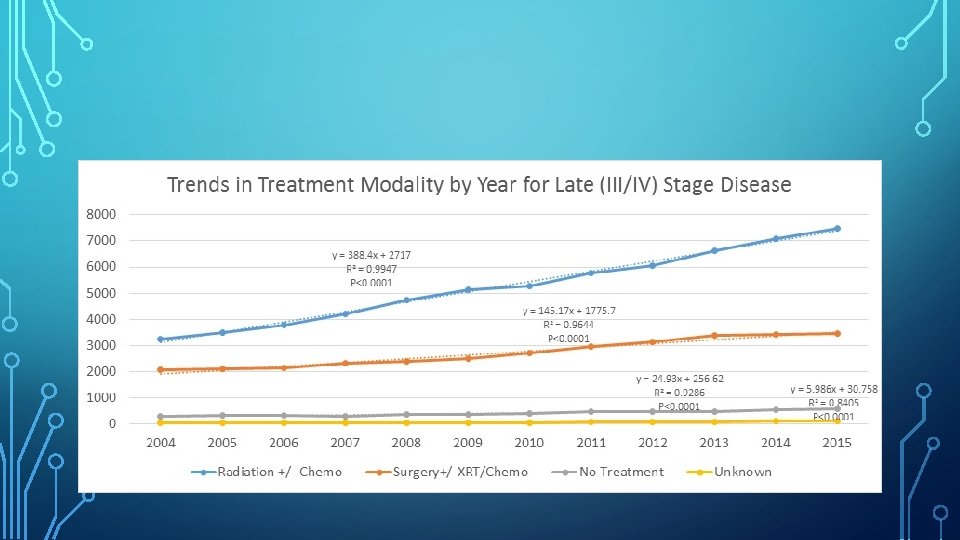
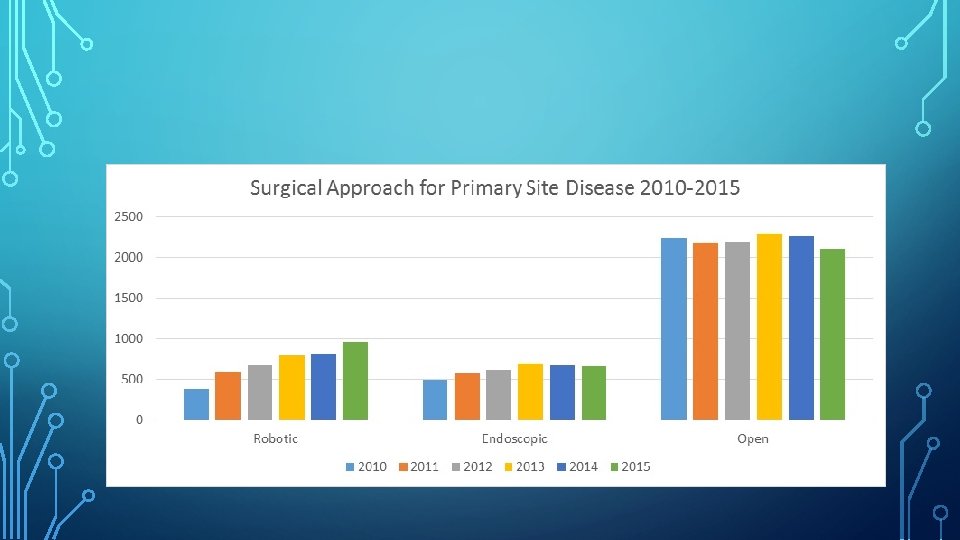
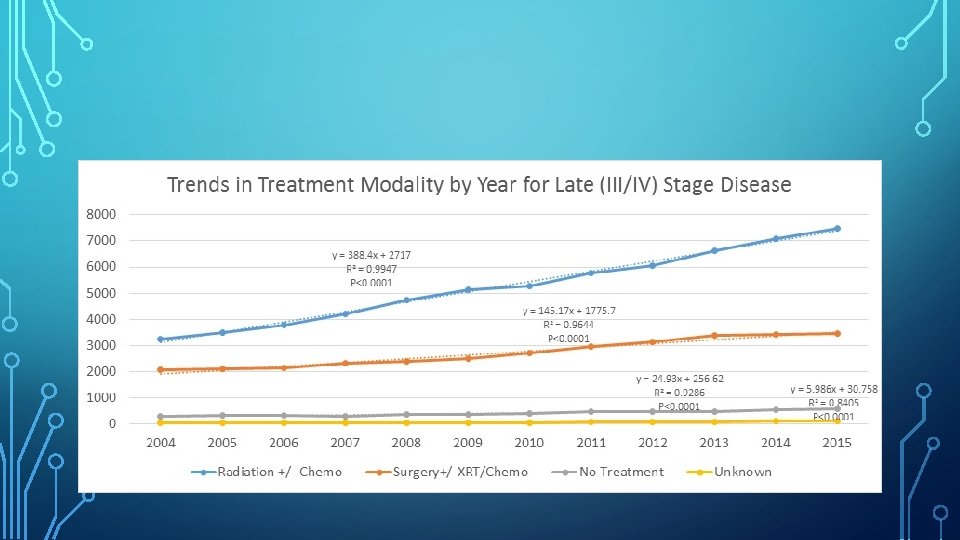
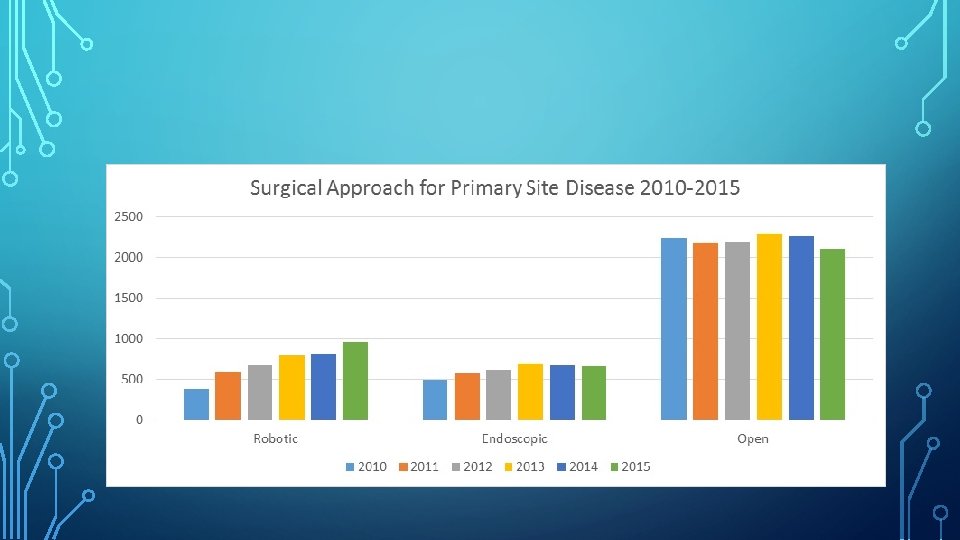
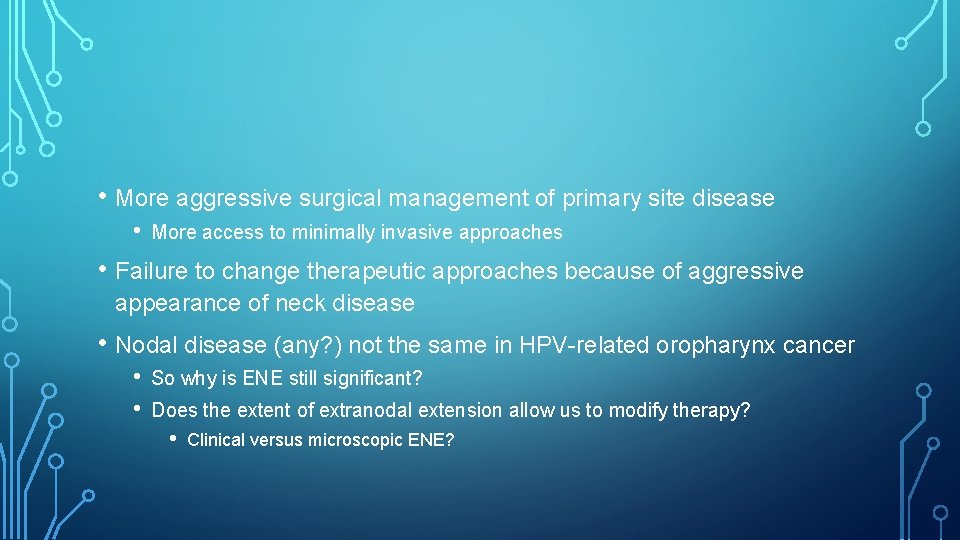
• More aggressive surgical management of primary site disease • More access to minimally invasive approaches • Failure to change therapeutic approaches because of aggressive appearance of neck disease • Nodal disease (any? ) not the same in HPV-related oropharynx cancer • • So why is ENE still significant? Does the extent of extranodal extension allow us to modify therapy? • Clinical versus microscopic ENE?
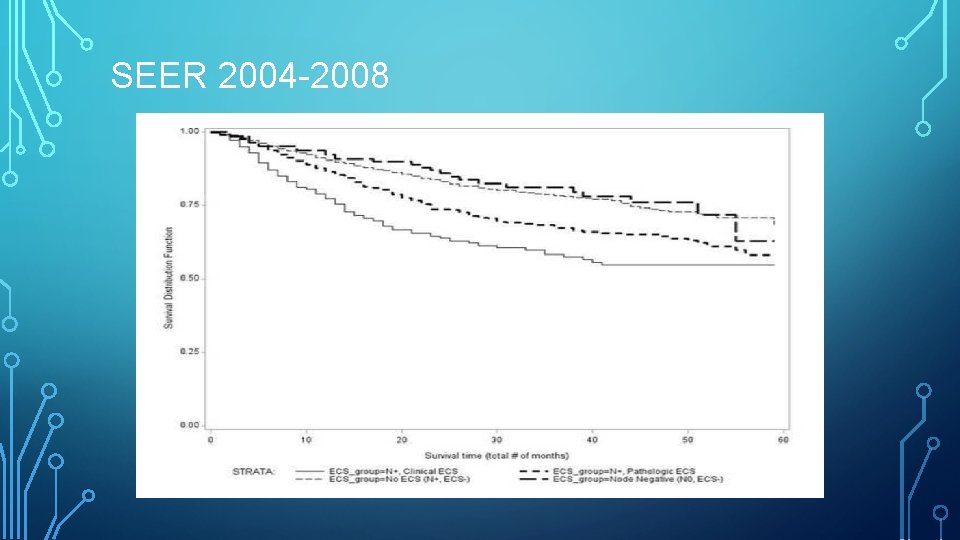
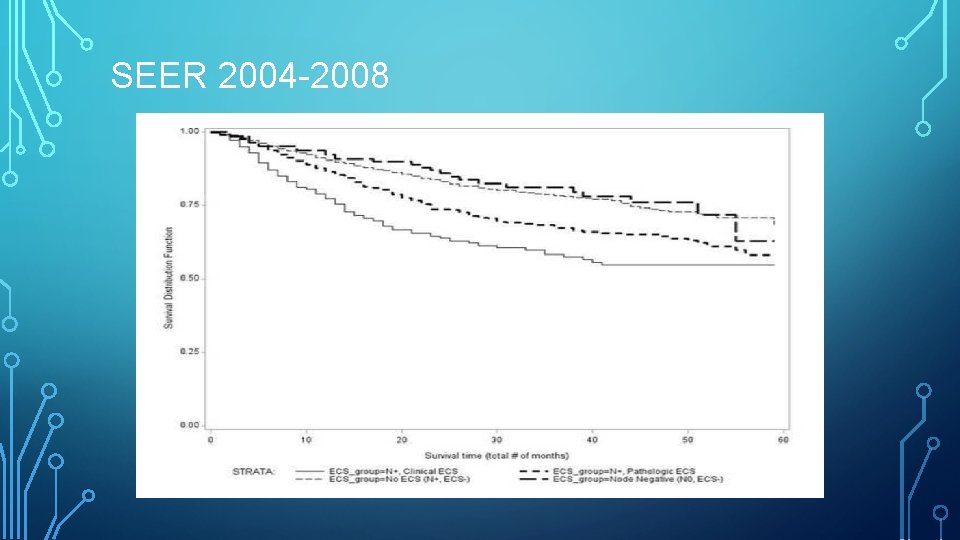
SEER 2004 -2008
SEER DATA 2008 • • We thought we were on to something THEY BASHED THE MANUSCRIPT! • SEER doesn’t have chemo data • No delineation of HPV disease • Completely counter to current knowledge at the time • FLAT EARTH? • Predates actual awareness of HPV epidemic • Testing • Predates attempts to change therapy based on disease
MARKEY CANCER CENTER • NCI designation • Access to NCDB • Chemo data • HPV from 2010

CURRENT DATA • NCDB • 2010 -2015 • Includes HPV • All treatment data • Chemotherapy
NCDB • Nationwide clinical surveillance data set that includes approximately 70% of all newly diagnosed malignancies. • It includes all cancer cases treated at American College of Surgeons Commissions on Cancer (Co. C) accredited hospitals in the US • Access requires NCI status
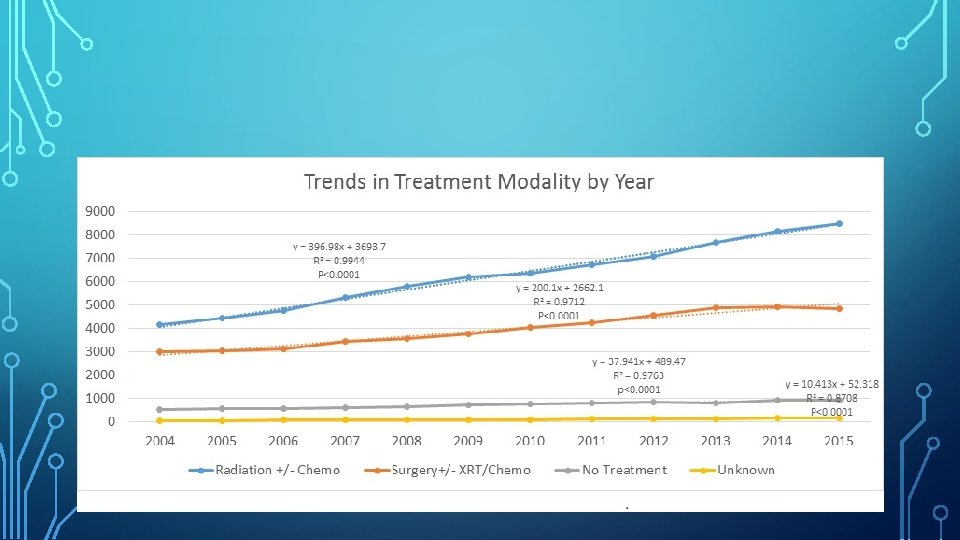
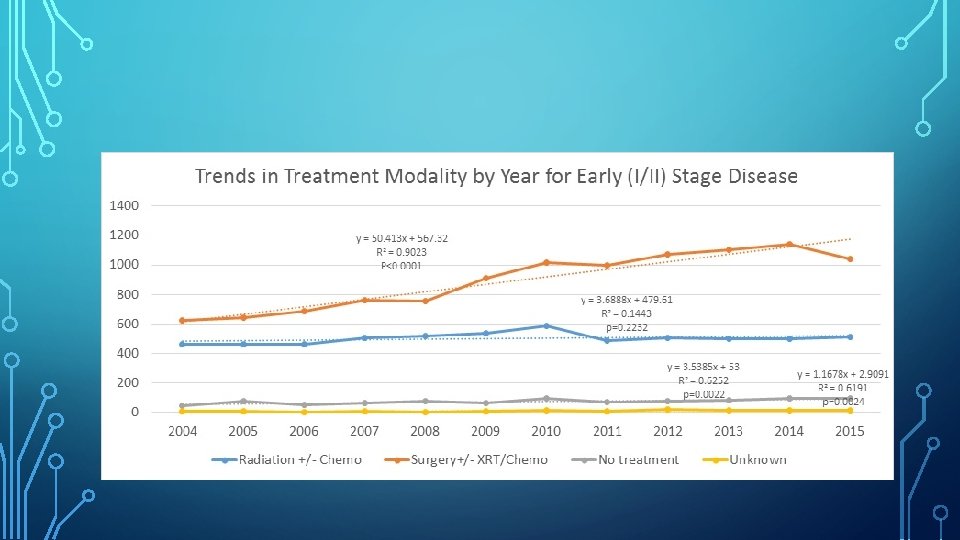
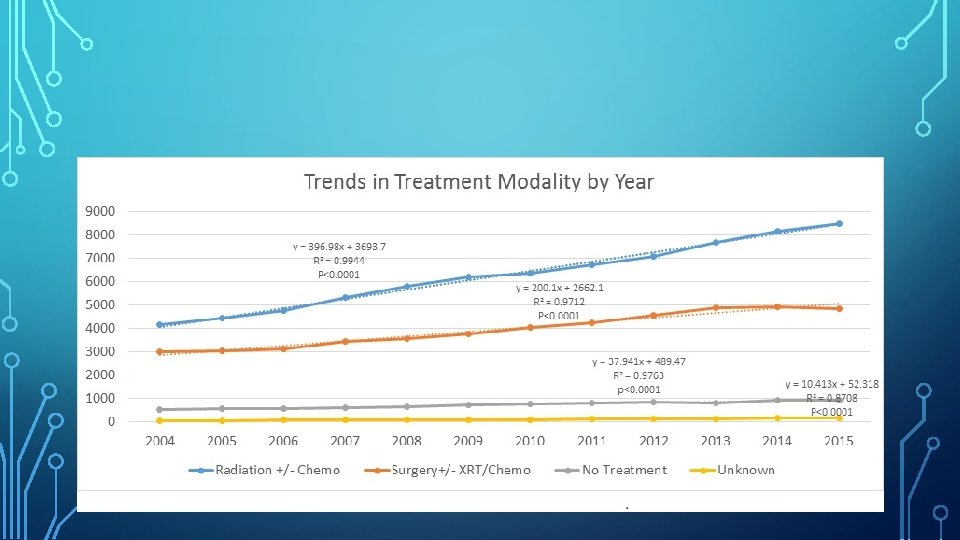
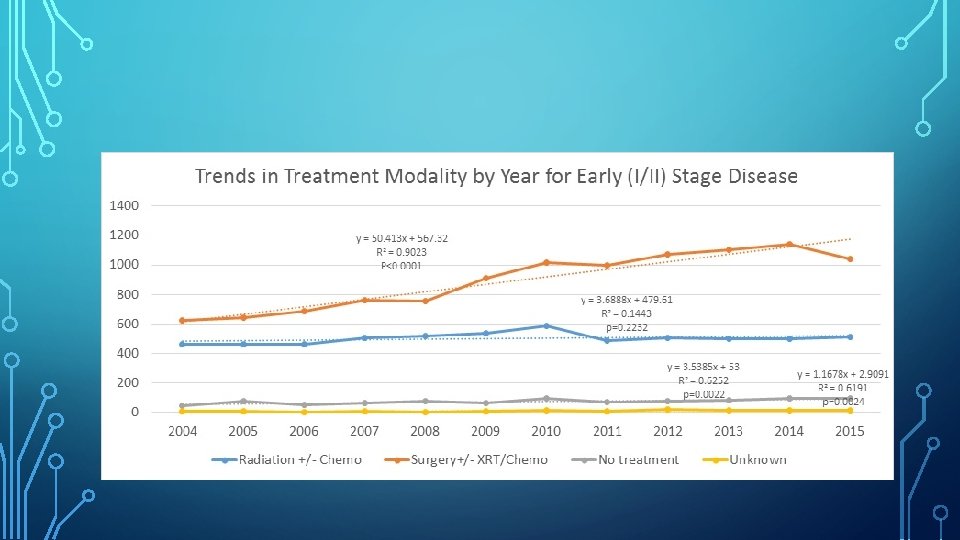
METHODS • Squamous Cell Carcinoma of the Oropharynx • • Specifically tonsil, base of tongue Demographics AJCC 7 th Edition Staging Treatment categorized • • Surgery alone Surgery with adjuvant radiotherapy±chemotherapy No treatment Unknown
METHODS • Patients treated with surgery as the initial treatment modality • • • Primary Site Neck Salvage surgery excluded • Excluded patients with surgery only for primary site or only for neck • Evidence of primary site surgery • • Margins, PNI, LVI, etc. AND lymph nodes examined
METHODS • • • Node negative Node (+), ENE (-) Node (+), ENE (+) • • • Clinical Microscopic/Pathologic To review, ENE (+) may be classified as • • ENEmi for microscopic ENE ≤ 2 mm ENEma for major ENE ≥ 2 mm
METHODS • Descriptive Analysis • Survival Analysis • Cox proportional hazards models
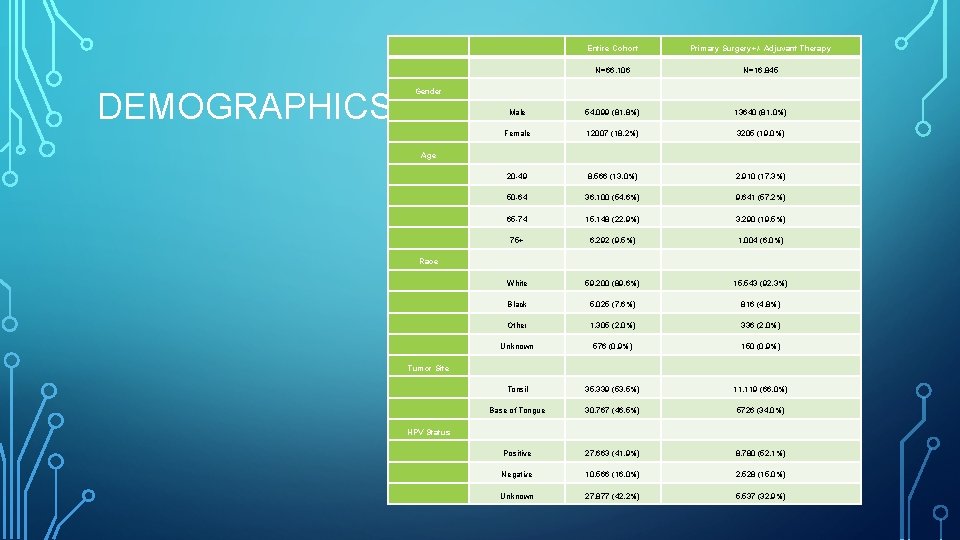
RESULTS • 2010 -2015 • 66, 106 patients • • White Male Age 50 -64 41. 9% (27, 663) HPV+ • 42. 2% HPV unknown
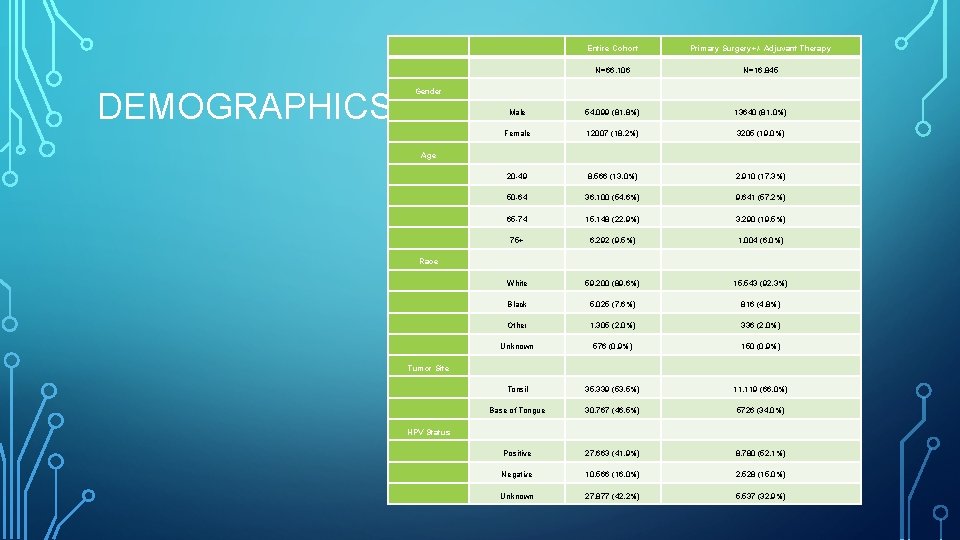
DEMOGRAPHICS Entire Cohort Primary Surgery+/- Adjuvant Therapy N=66, 106 N=16, 845 Gender Male 54, 099 (81. 8%) 13640 (81. 0%) Female 12007 (18. 2%) 3205 (19. 0%) Age 20 -49 8, 566 (13. 0%) 2, 910 (17. 3%) 50 -64 36, 100 (54. 6%) 9, 641 (57. 2%) 65 -74 15, 148 (22. 9%) 3, 290 (19. 5%) 75+ 6, 292 (9. 5%) 1, 004 (6. 0%) Race White 59, 200 (89. 6%) 15, 543 (92. 3%) Black 5, 025 (7. 6%) 816 (4. 8%) Other 1, 305 (2. 0%) 336 (2. 0%) Unknown 576 (0. 9%) 150 (0. 9%) Tumor Site Tonsil 35, 339 (53. 5%) 11, 119 (66. 0%) Base of Tongue 30, 767 (46. 5%) 5726 (34. 0%) HPV Status Positive 27, 663 (41. 9%) 8, 780 (52. 1%) Negative 10, 566 (16. 0%) 2, 528 (15. 0%) Unknown 27, 877 (42. 2%) 5, 537 (32. 9%)
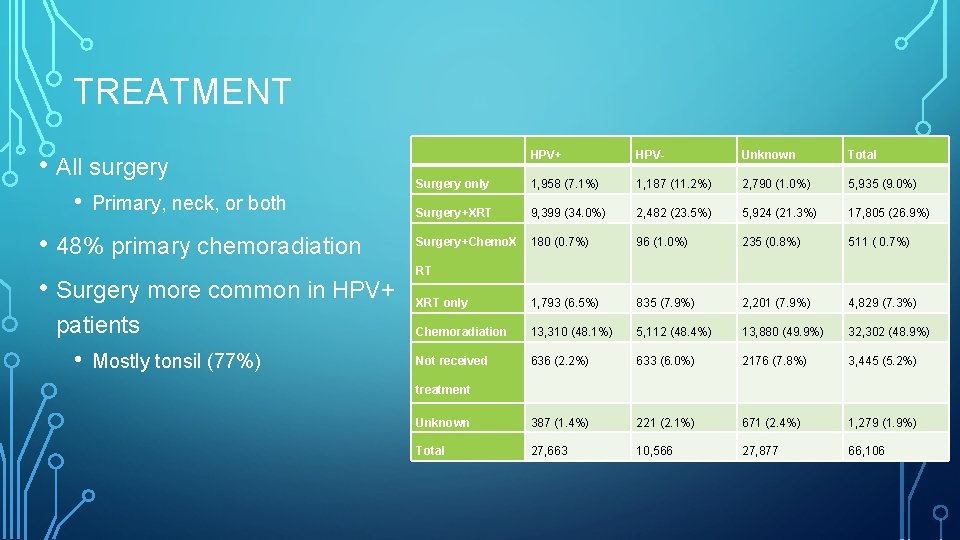
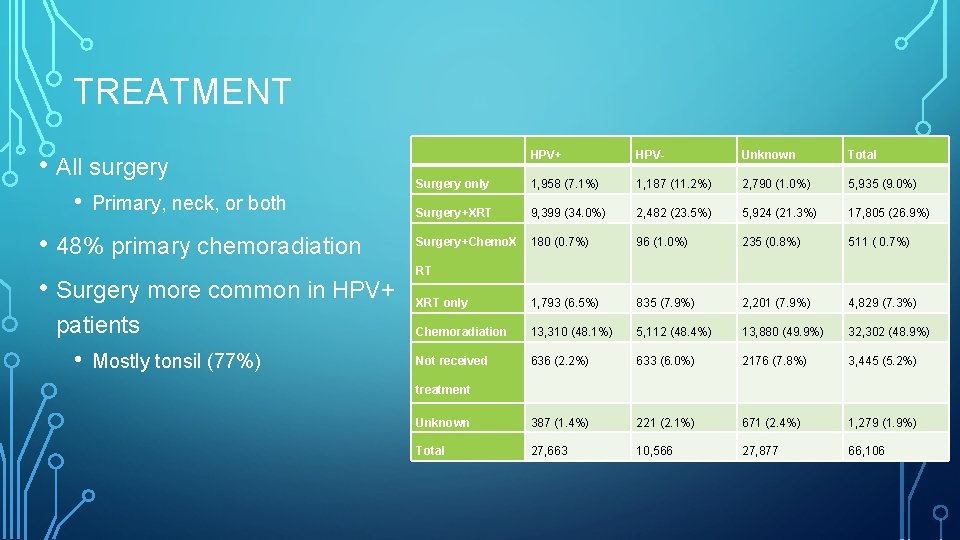
TREATMENT • All surgery • Primary, neck, or both • 48% primary chemoradiation • Surgery more common in HPV+ patients • Mostly tonsil (77%) HPV+ HPV- Unknown Total Surgery only 1, 958 (7. 1%) 1, 187 (11. 2%) 2, 790 (1. 0%) 5, 935 (9. 0%) Surgery+XRT 9, 399 (34. 0%) 2, 482 (23. 5%) 5, 924 (21. 3%) 17, 805 (26. 9%) Surgery+Chemo. X 180 (0. 7%) 96 (1. 0%) 235 (0. 8%) 511 ( 0. 7%) XRT only 1, 793 (6. 5%) 835 (7. 9%) 2, 201 (7. 9%) 4, 829 (7. 3%) Chemoradiation 13, 310 (48. 1%) 5, 112 (48. 4%) 13, 880 (49. 9%) 32, 302 (48. 9%) Not received 636 (2. 2%) 633 (6. 0%) 2176 (7. 8%) 3, 445 (5. 2%) Unknown 387 (1. 4%) 221 (2. 1%) 671 (2. 4%) 1, 279 (1. 9%) Total 27, 663 10, 566 27, 877 66, 106 RT treatment
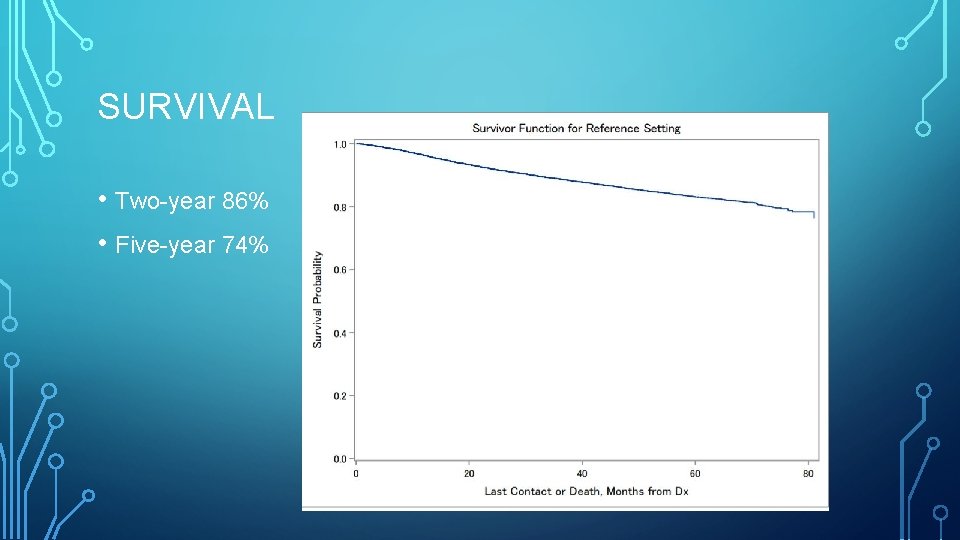
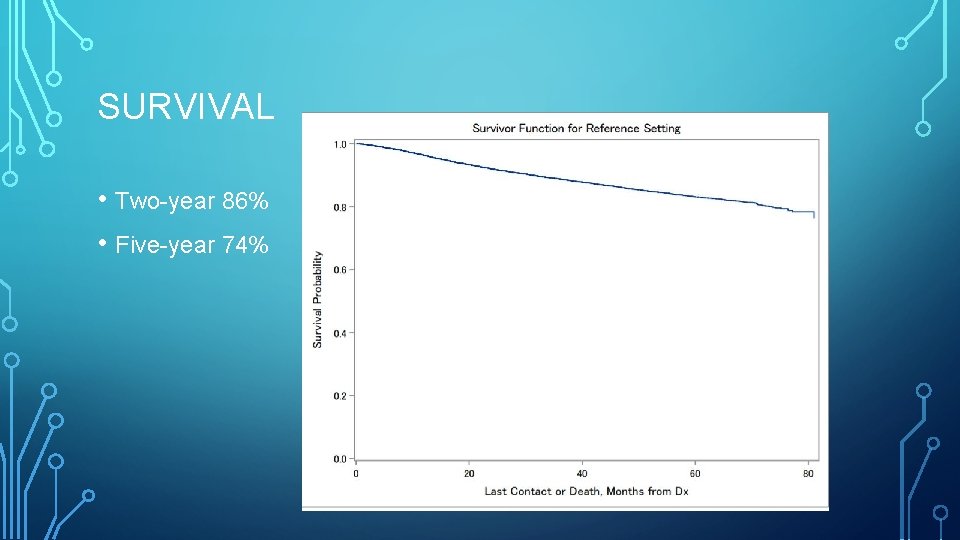
SURVIVAL • Two-year 86% • Five-year 74%
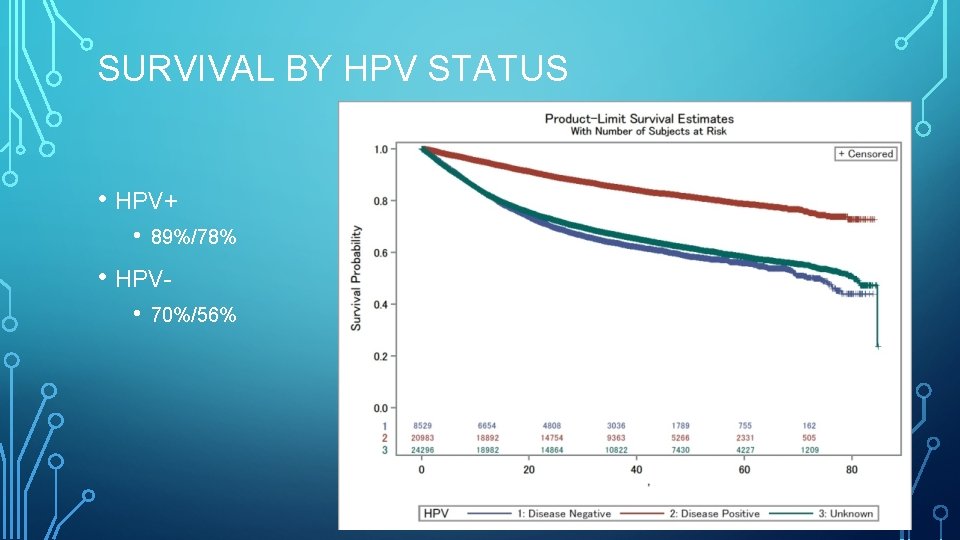
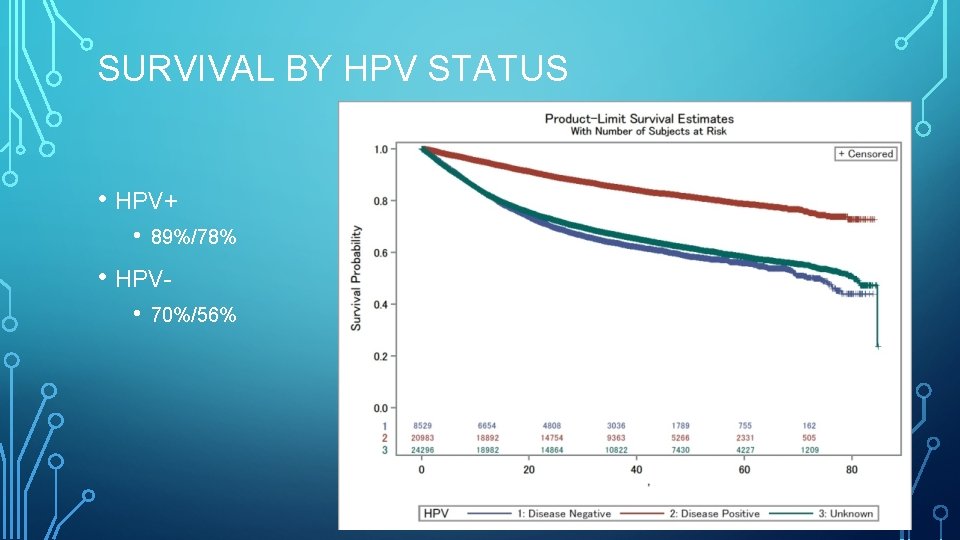
SURVIVAL BY HPV STATUS • HPV+ • 89%/78% • HPV • 70%/56%
RESULTS: SURGERY • 16, 845 patients with primary surgery± adjuvant therapy • 8, 780 HPV+ • 11, 119 tonsil (66%) • 5, 726 BOT (34%) • 12, 256 received adjuvant XRT • 6, 302 received adjuvant chemotherapy
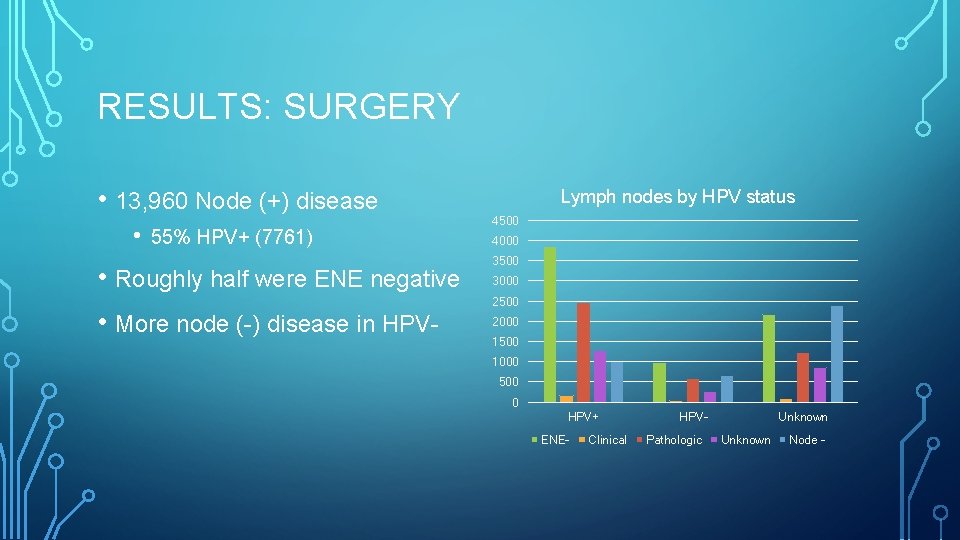
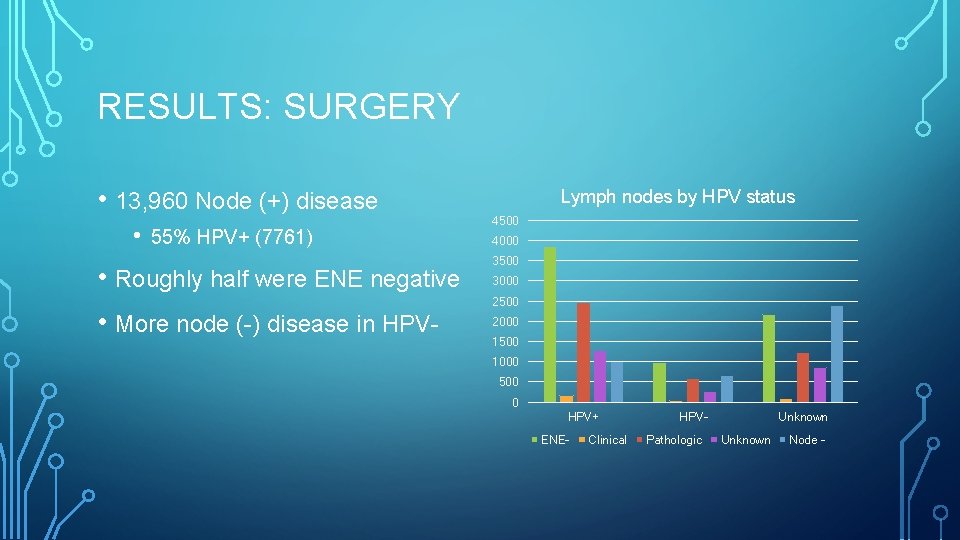
RESULTS: SURGERY • 13, 960 Node (+) disease • 55% HPV+ (7761) • Roughly half were ENE negative • More node (-) disease in HPV- Lymph nodes by HPV status 4500 4000 3500 3000 2500 2000 1500 1000 500 0 HPV+ ENE- Clinical HPVPathologic Unknown Node -
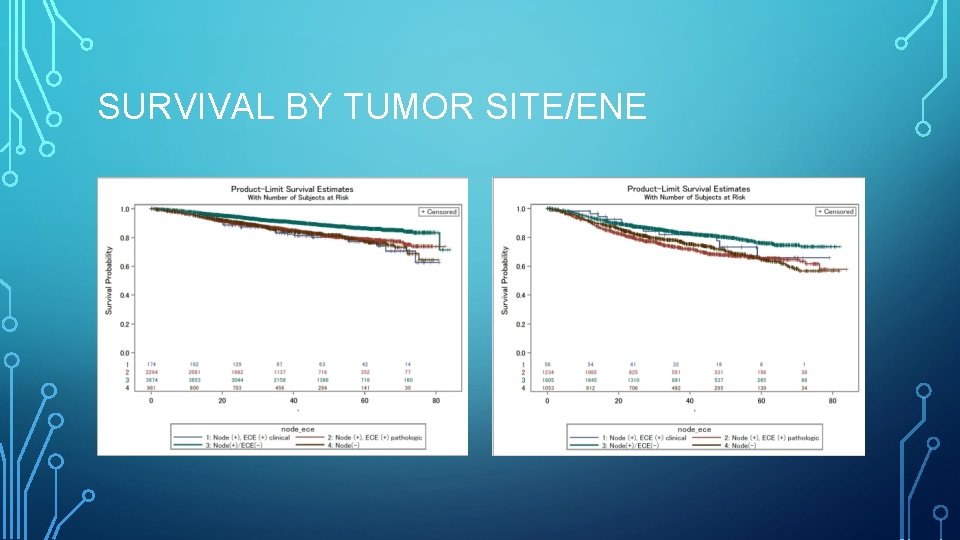
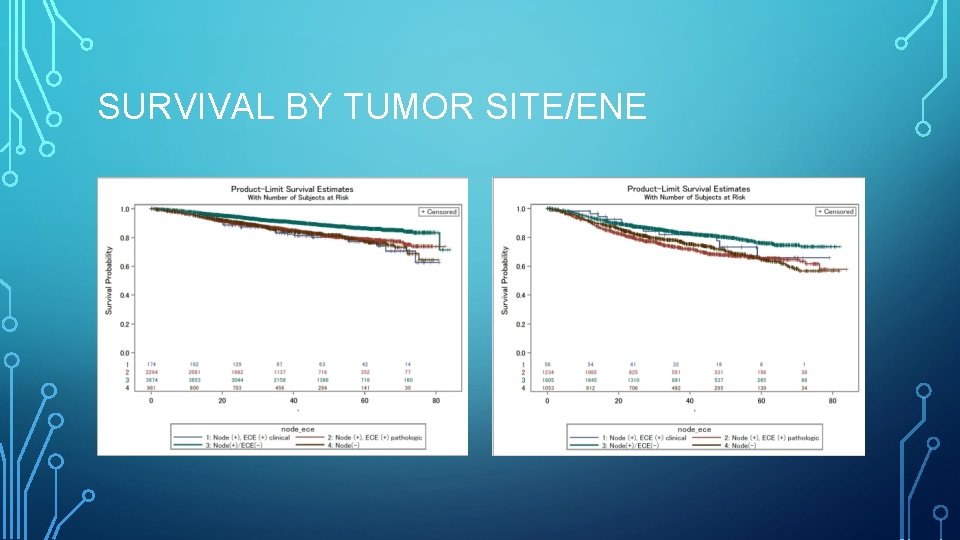
SURVIVAL BY TUMOR SITE/ENE
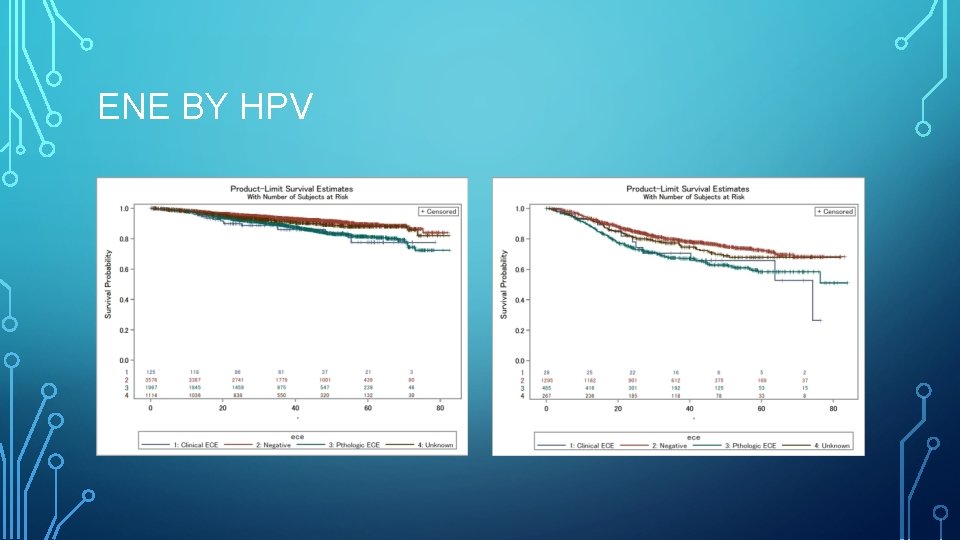
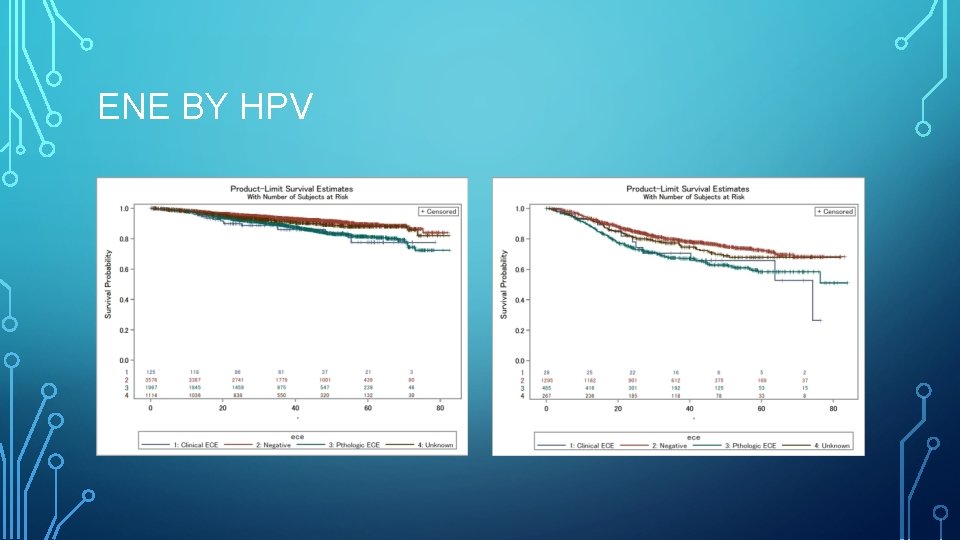
ENE BY HPV
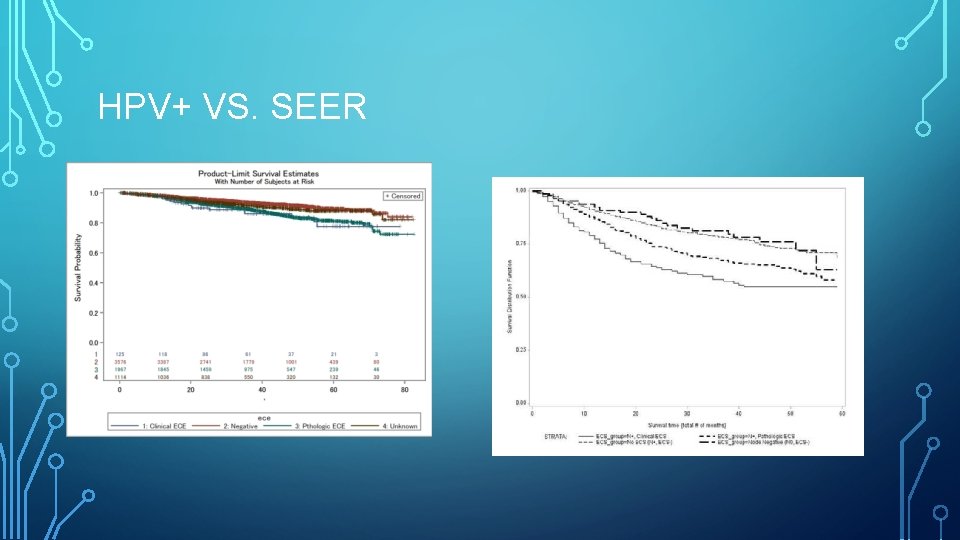
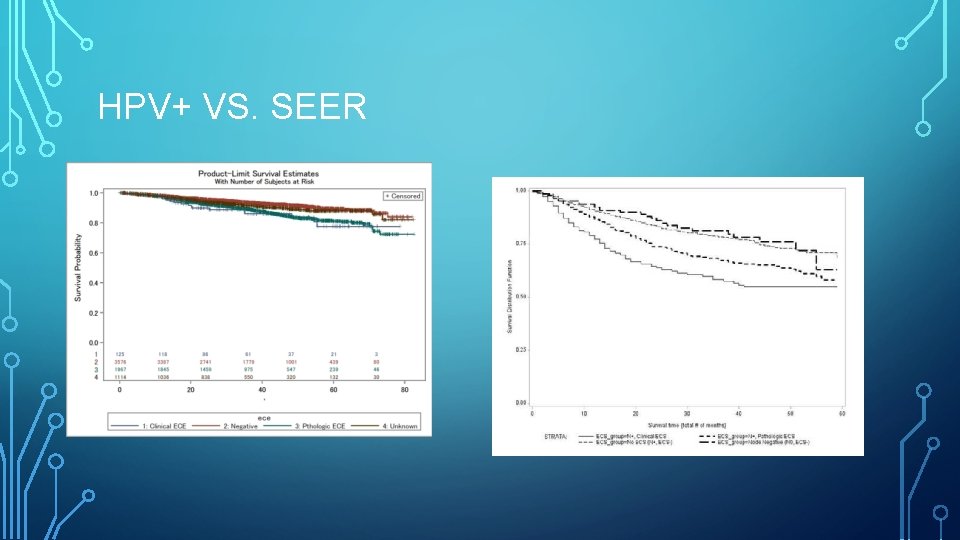
HPV+ VS. SEER
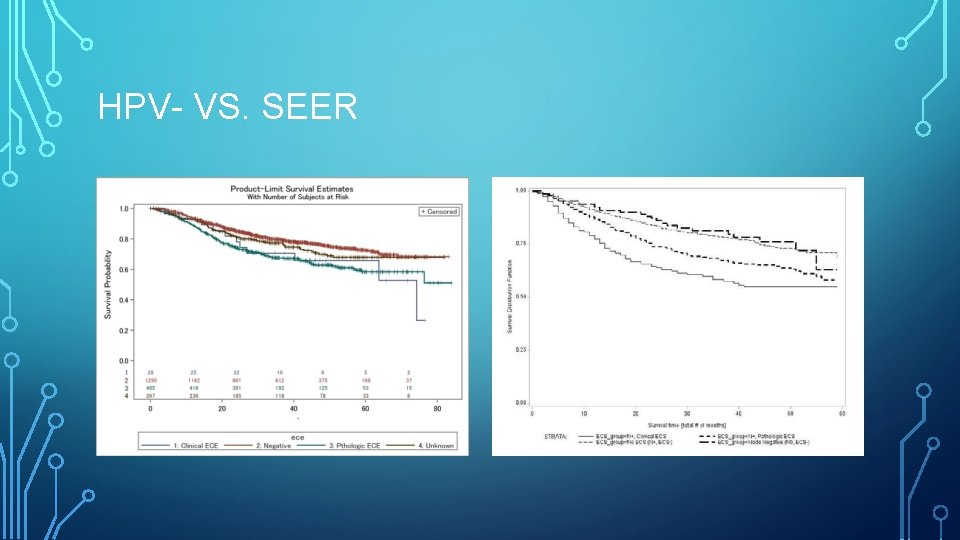
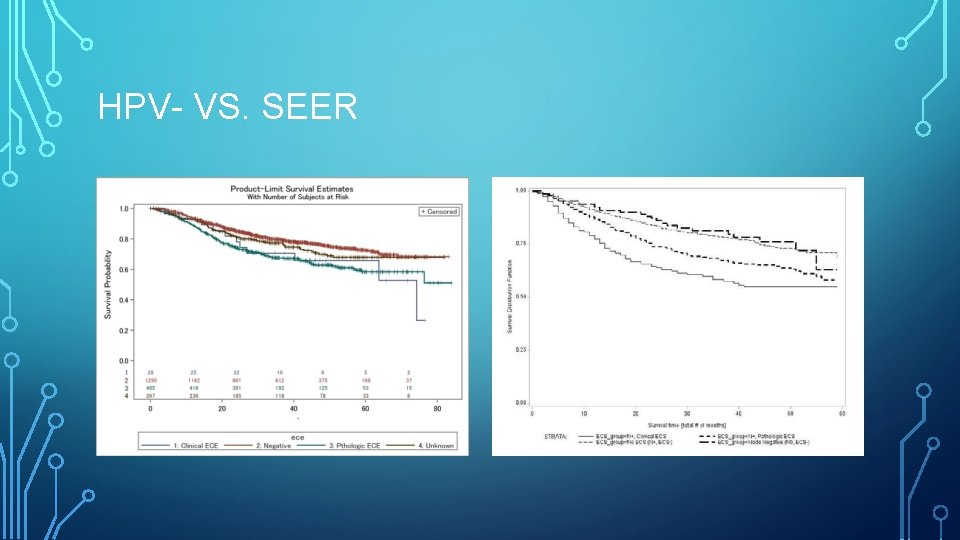
HPV- VS. SEER
COX PROPORTIONAL HAZARDS • Age • Gender • Race • Tumor site • HPV status • Radiotherapy • CHemotherapy
COX PROPORTIONAL HAZARDS • No significant differences between clinical and pathologic ENE • Compared to ENE (-), both had increased risk of mortality (HR 1. 83, p<0. 001) • HPV- patients had 2. 5 x risk of mortality • XRT 33% improved survival • Chemotherapy 10% reduction in mortality
DISCUSSION • Observational study of the impact of ENE in oropharyngeal cancer • Goal was to determine if the longstanding tenets regarding ENE still held true given the different epidemiology of this disease • Seems to
DISCUSSION • It is known that ENE is a significant prognostic indicator in oropharyngeal carcinoma • • Increased incidence of regional and distant metastatic disease Survival rates of 29 -45%, improving to 58% with systemic chemotherapy • Some evidence to suggest that chemotherapy is of little benefit in HPV+ disease • Association with advanced T stage
DISCUSSION • An, et al • • • NCDB data through 2012 ENE associated with poorer survival Chemotherapy (vs. XRT alone) was not associated with improved survival • Stage I or II disease treated with XRT alone did more poorly than chemoradiation or surgery with adjuvant therapy • Stage III disease: trimodality therapy improved survival compared with chemoradiation • Best options for eliminating chemotherapy appear to involve incorporation of surgery into the treatment algorithm
DISCUSSION • In this study, ENE was associated with an 83% decreased survival • Extent of ENE not significant • Impact of ENE does not seem to be offset by the use of chemotherapy • Appears to behave similarly to HPV- counterparts
DISCUSSION • Chemotherapy • • • 6302 patients 4553 observed to have ENE of any type 1749 received chemotherapy without ENE • • • High volume nodal disease Positive margins Other unfavorable features 10% reduction in mortality Unclear if this is a function of the beneficial effects of chemotherapy given an otherwise high-risk profile
SHORTCOMINGS • Low number of surgically treated patients (275) with clinical ENE • Surgical selection of more favorable disease • Select out patients with more aggressive ENE • ENE, when present AND surgically resectable, is neither a contraindication for surgery nor does it carry a less favorable profile than more indolent disease • Thus conclusion is there is no difference between pathologic ENE and surgically resectable clinical ENE
SHORTCOMINGS • Hard to make true treatment recommendations on retrospective data • Difficult to determine if similarities in survival profiles are due to the behavior of the disease or simply a manifestation of appropriately treated disease. • Prospective trials • Evidence for treatment de-escalation applies to adjuvant therapy in the postoperative setting • No evidence for de-escalation in the non-surgical setting
CONCLUSION • ENE remains a significant prognostic indicator in oropharyngeal carcinoma • Clinical and pathologic ENE are both associated with decreased survival • • No significant difference between the two Surgically resectable clinical ENE • Clinical impact of these observations in HPV+ and HPV- disease requires further study

THANK YOU