EXTERNAL EYE DISEASE IN CHILDREN BY HANY ELDEFRAWY
EXTERNAL EYE DISEASE IN CHILDREN BY HANY ELDEFRAWY LOCUM CONSULTANT OPHTHALMOLOGY , UNIVERSITY HOSPITALS OF BIRMINGHAM
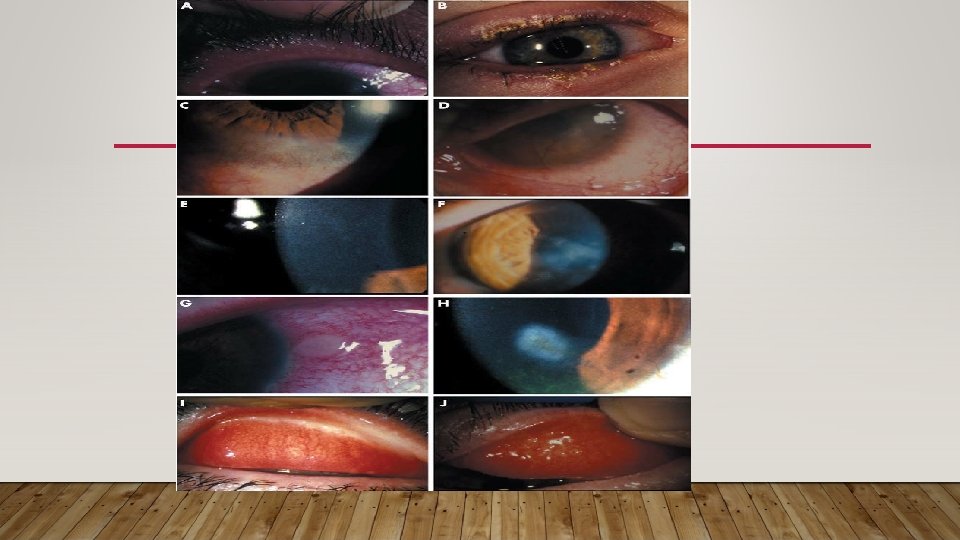
BLEPHAROKERATOCONJUNCTIVITIS (BKC) • Is common in all age groups • Lid disease can involve anterior lid margin (lash follicles) or posterior lid margin (Meibomian glands) • Conjunctivitis • Styes and Meibomian cysts • Keratitis • Dermatologic disease
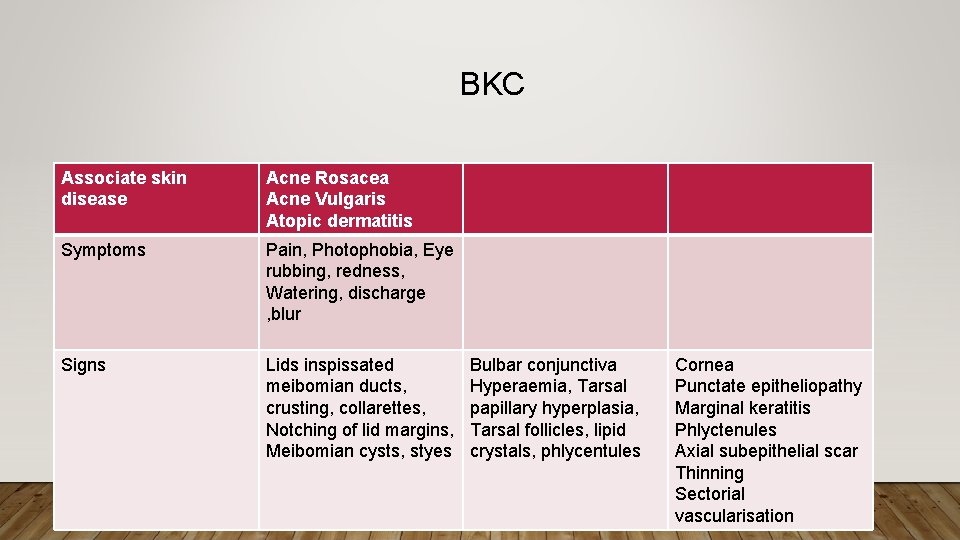
BKC Associate skin disease Acne Rosacea Acne Vulgaris Atopic dermatitis Symptoms Pain, Photophobia, Eye rubbing, redness, Watering, discharge , blur Signs Lids inspissated meibomian ducts, crusting, collarettes, Notching of lid margins, Meibomian cysts, styes Bulbar conjunctiva Hyperaemia, Tarsal papillary hyperplasia, Tarsal follicles, lipid crystals, phlycentules Cornea Punctate epitheliopathy Marginal keratitis Phlyctenules Axial subepithelial scar Thinning Sectorial vascularisation

PATHOGENSIS • Delayed hypersensitivity response to Bacterial antigens released into the tear film • Inflammation • Posterior lid margin is not the result of infection. Clinically there is keratinisation of the ductules of meibomian glands and meibomian gland drop-out
PRESENTATION • Asymmetric or unilateral • Photophobia • Eye rubbing or crusting in the morning • Present late with reduced vision due to corneal scarring • Vision loss may be severe and insidious • Reversible if it is the result of epitheliopathy, Permanent if it is result of central extension of peripheral corneal disease or diffuse central stromal scar
TREATMENT • Warm compresses with short course topical antibiotic • Meibomian cysts may resolve spontaneously • Incision of meibomian cyst if persistent more than 3 months or if they affect vision by altering lid position • Oral antibiotic (Doxocycline) for recurrent cysts
VERNAL KERATOCONJUNCTIVITIS (VKC) • Atopic disease in which allergic response is mounted to common environmental allergens , dust or pollens • Seasonal or perennial • Early onset • Atopic VKC develop older patients with severe atopic dermatitis (Eczema) and is unremitting.
CLINICAL FEATURES • 1 st decade (82% by age 10 years) • 95% remission by late teens • In the middle East is considered a substantial public health problem (3% of eye clinic patients and 10% of outpatient attendances) • Prevalence in Western Europe is less than 0. 03% • More common in Males • 45 -75% have history of asthma or Eczema
• Limbal VKC is common in patients of African or Asian descent
CLINICAL PICTURE • Itching, photophobia, discomfort, blepharospasm, blurred vision, mucous discharge • Asymmetric • Eczematous with excoriation at the canthi and reactive ptosis • Papillary hypertrophy and cellular infilteration over the upper tarsal plate obscuring the pattern of underlying vessels • Giant papillae >1 mm with cobble stone appearance • Papillae can form at the limbus appearing as gelatinous or vascular mounds with white Horner. Tranta dots (aggregates of degenerated eosinophils) • VKC may be palpebral , limbal or combined disease

CORNEAL CHANGES IN VKC • Punctate epithelial erosions in the superior and central cornea • Mucus filaments • Superficial corneal vascularisation • Severe palpebral disease may lead to macroerosion • Vernal ulcer (Shield ulcer) may develop in neglected cases of macroerosion due to deposition of mucus and calcium in Bowman’s layer preventing reepithelialisation. • 2 ry infection and crystalline keratopathy.
ASSOCIATED DISEASE • Herpes Simplex keratitis • Keratoconus in 26% • Anterior capsular cataract in 8% of cases • 20% complication due to unsupervised steroid treatment
PATHOGENSIS • In Atopy a subpopulation of T lymphocytes (Th 2) is abnormally expanded • Ig. E mediated immediate hypersentivity response • Th 2 cells generate cytokines and interleukins (IL-3, IL-4 & IL-13) • Synthesis of Ig. E by B cells • Allergen-Mast cell coated Ig. E contact will lead to degranulation and release of Histamines and other cytokines • Papillae central vascular core of mononuclear cells surrounded by edematous connective infiltrated by plasma cells, mast cells, activated eosinophils and lymphocytes
LAB TEST • Total serum Ig E and tear Ig E are usually elevated (Non-specific) • Measurement of local Ig E production by RAST • Cytology specimen • Allergy testing is not indicated in the majority of patients

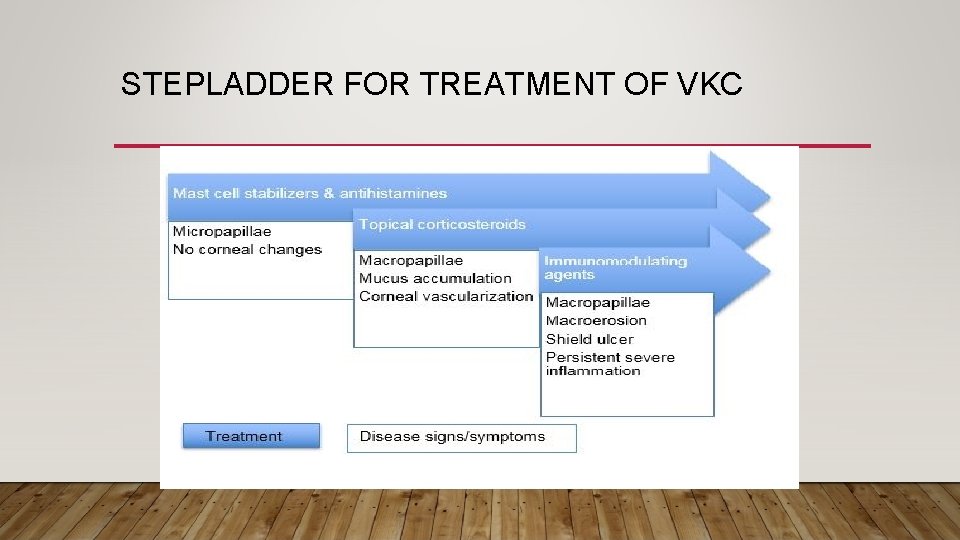
STEPLADDER FOR TREATMENT OF VKC
• Allergen avoidance (Carpets, Pets, feather pillows) • Oral antihistamine can help sleep and reduce eye rubbing • Topical histamine antagonist (H 1) Antagonists (Levocobastine 0. 05%, emedastine 0. 05% ) • Topical cromones (sodium cromoglycate 2 -4%, Nedocromil sodium 2%, other mast cell stablizers Lodoxamide 0. 1% • Dual action agent active against H 1 receptors and mast cell degranulation (Olopatadine 0. 1%) • Topical acetylcysteine 5 -10% reduces mucus • Topical corticosteroids is very effective but patients should be carefully monitored for side effects
• Synthetic steroids (fluoromethalone, loteprednol, rimexolone) may reduce the risk of glaucoma and cataract. Steroid ointment, such as betamethasone, may be useful at night to reduce treatment frequency. • Steroid injected into the supratarsal space after lid eversion (0. 5– 1. 0 ml of either dexamethasone (4 mg/ml) or triamcinolone (40 mg/ml)) is reserved for severe disease not responding to topical treatment, or given following surgery for a vernal plaque. • Cyclosporin A (0. 05% to 2%) is safe in children. It is an alternative to topical corticosteroid, but probably less well tolerated, less effective, and more expensive
• Systemic immunosuppression with corticosteroids, cyclosporin A, tacrolimus, or azathioprine is reserved for severe unremitting disease with corneal complications. • Treatment of vernal plaque is by superficial keratectomy after the local allergic disease has been medically controlled. The epithelium should be reflected to show the full extent of the plaque and the plaque debrided or “peeled” from the surface. A minimum depth of tissue should be removed. There is no advantage in using laser phototherapeutic keratectomy. An amniotic membrane graft may rarely be required for a large persistent epithelial defect. A bandage contact lens is not an alternative to effective medical management. It increases the risk of secondary infection
• For chronic disease, a daily warm compress followed by lid cleaning with a cotton bud moistened in boiled water followed by topical antibiotic ointment. This can take 4– 6 weeks to work. • Topical corticosteroid is the basis of treatment for most cases of BKC with conjunctival phlyctenules or significant corneal disease. For example, fluoromethalone 0. 1% four times a day, reducing to once daily after 4 weeks. Long-term treatment (i. e. for years) with low-dose steroid may be required.
• Treat visually significant keratitis with long-term (8– 12 weeks) low-dose oral antibiotic • Corneal phlyctenules can rarely lead to perforation of the cornea and loss of vision due to scarring. They should be treated with intensive topical corticosteroids and topical antibiotics if there is an epithelial defect. • Systemic antibiotics reduce the frequency and severity of relapses of phlyctenular disease
• Dietary supplement with oral flaxseed oil has been recommended. • Rarely, for inexorable corneal opacification, systemic immunosuppression (e. g. with mycophenolate) is required. • Secondary microbial keratitis can occur; it should be treated immediately. • An axial corneal opacity or irregular astigmatism may cause amblyopia. Visual correction may be possible in older children using a rigid contact lens
- Slides: 25