Expanded and Marginal Donors in Liver Transplantation Need

- Slides: 44
Expanded and Marginal Donors in Liver Transplantation: Need, Use and Results Cosme Manzarbeitia, MD, FACS Director, Transplant and Hepatobiliary Surgery, Crozer Keystone Healthcare Network Associate Professor of Surgery, Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Definitions • 1 ideal donors • 2 extended donors • 3 marginal donors • Unacceptable donors? 1 2 3 ?
The Ideal Donor • Hemodynamically stable • Young (18 to 45) • Brain-dead • Disease-free • No cardiac arrest (? )
The Down Side of Waiting for the “Ideal” Donor • Death waiting • Tumors growing • Patients deteriorating • When does risk balance itself?
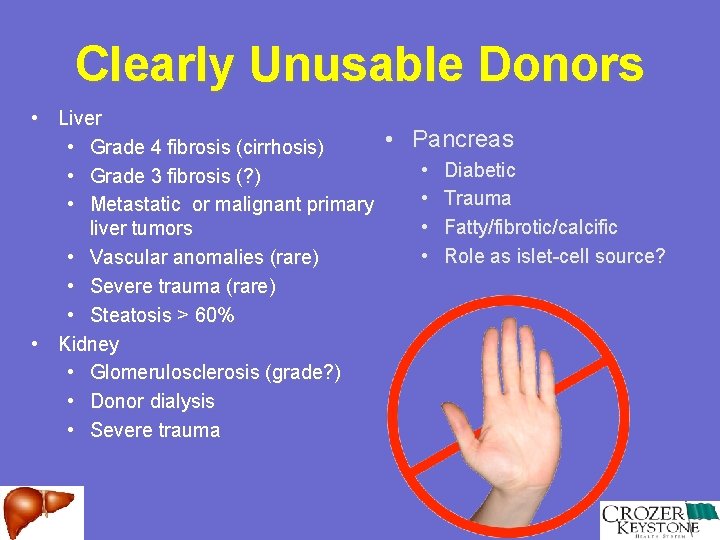
Clearly Unusable Donors • Liver • Pancreas • Grade 4 fibrosis (cirrhosis) • Diabetic • Grade 3 fibrosis (? ) • Trauma • Metastatic or malignant primary • Fatty/fibrotic/calcific liver tumors • Role as islet-cell source? • Vascular anomalies (rare) • Severe trauma (rare) • Steatosis > 60% • Kidney • Glomerulosclerosis (grade? ) • Donor dialysis • Severe trauma
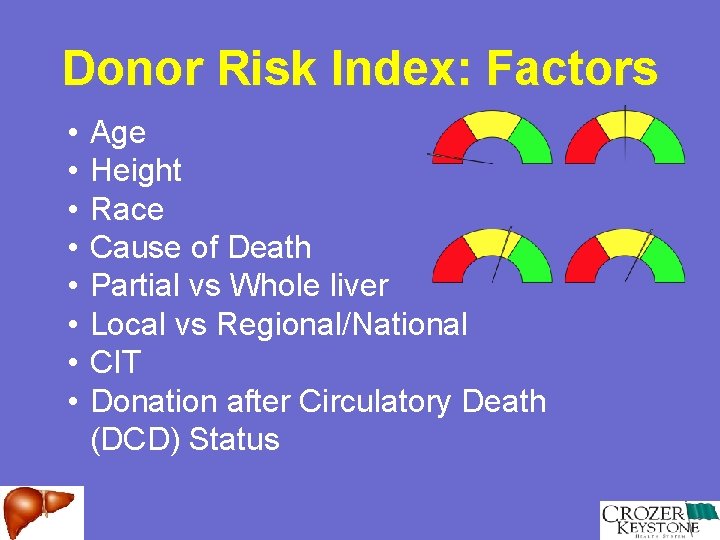
Donor Risk Index: Factors • • Age Height Race Cause of Death Partial vs Whole liver Local vs Regional/National CIT Donation after Circulatory Death (DCD) Status
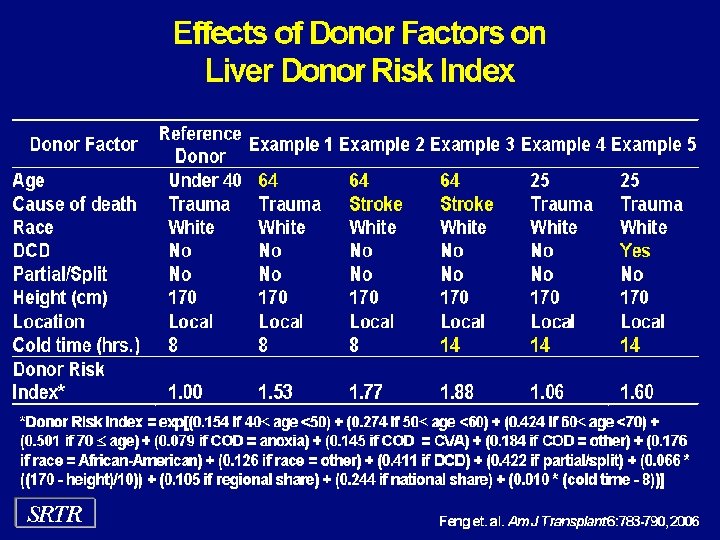
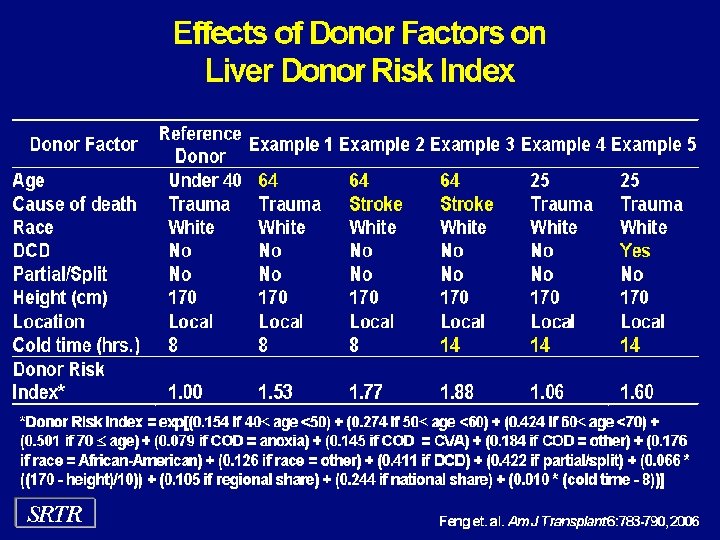
Effects of Donor Factors on Liver Donor Risk Index
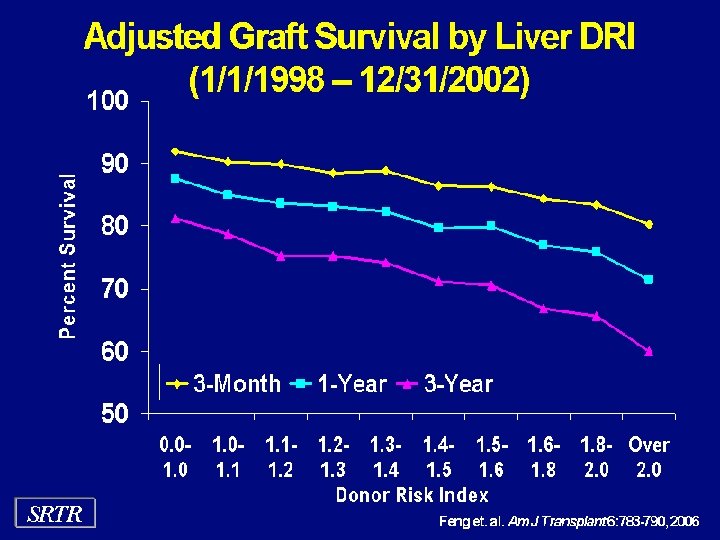
Graft Survival by Donor Risk Index
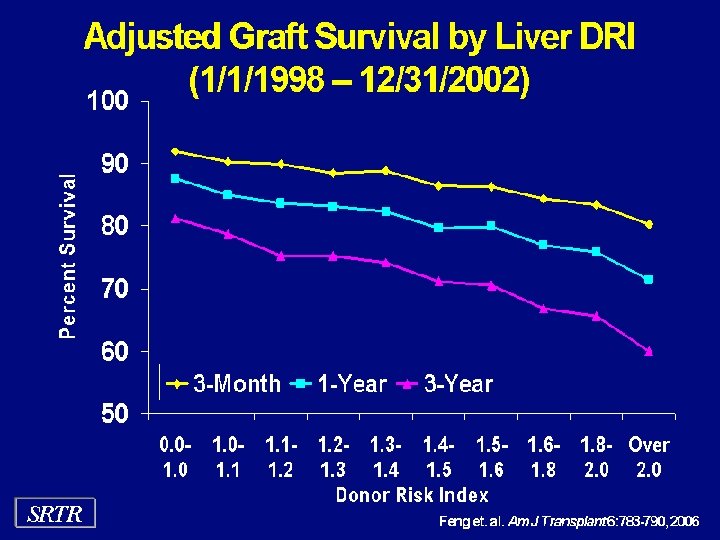
Adjusted Graft Survival by Liver DRI (1/1/1998 – 12/31/2002)
Obese Donors
Obese Donors and Liver Transplantation • Increased incidence of fatty changes in patients with BMI > 25 1 • BMI 25 -28: 33% • BMI > 28: 78% • • • Unclear size estimation Difficult dissection Up to 50% of obese and morbidly obese donors provide livers amenable to transplantation 2 • Vascular issues (also apply to kidney, pancreas)
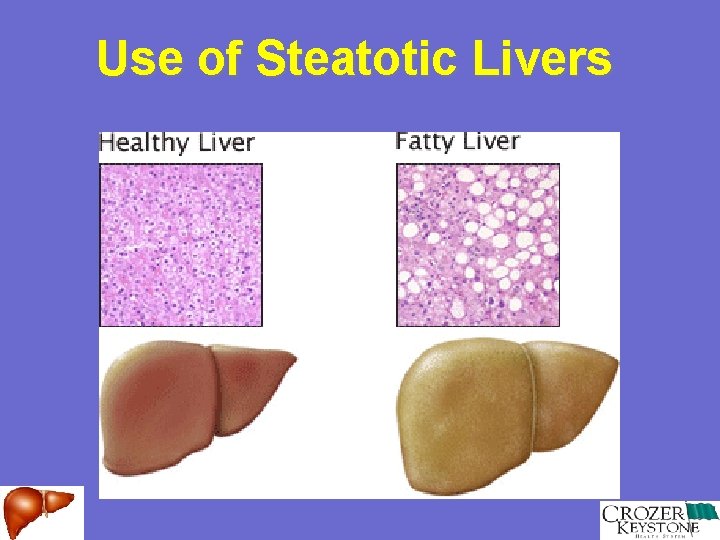
Steatosis in Liver Donors • Increased risk of PNF 1 • Acceptable limits • Macrovesicular • Up to 30% • Microvesicular • Up to 100% • Optimizing preservation time • Liberalization of biopsy at time of procurement 2
Fatty Liver
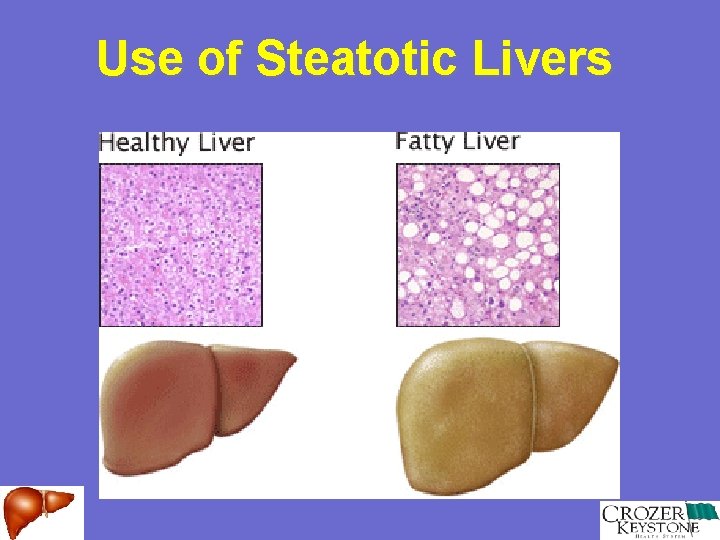
Use of Steatotic Livers
Donation after Cardiac Death (DCD)
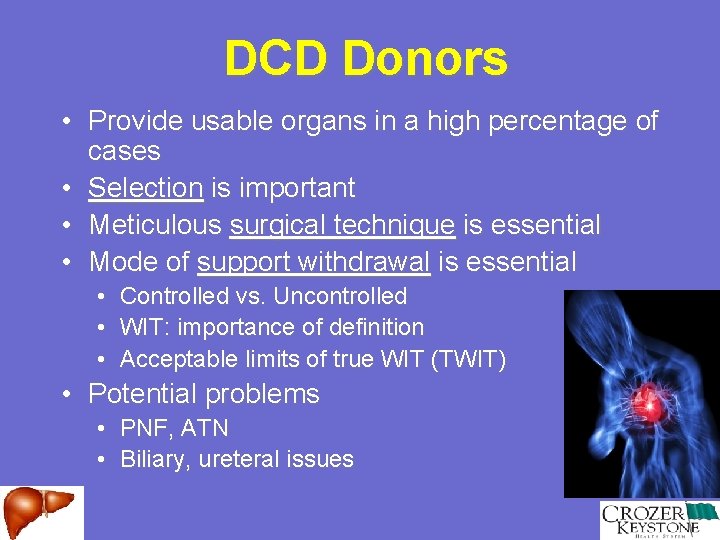
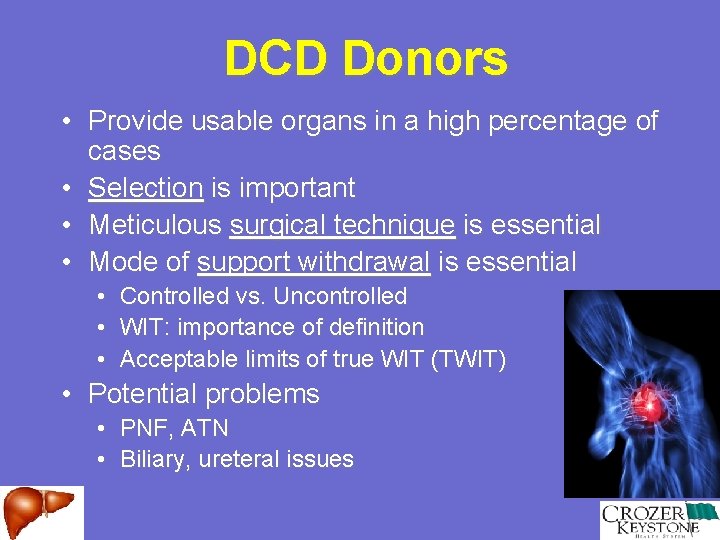
DCD Donors • Provide usable organs in a high percentage of cases • Selection is important • Meticulous surgical technique is essential • Mode of support withdrawal is essential • • • Controlled vs. Uncontrolled WIT: importance of definition Acceptable limits of true WIT (TWIT) • Potential problems • • PNF, ATN Biliary, ureteral issues
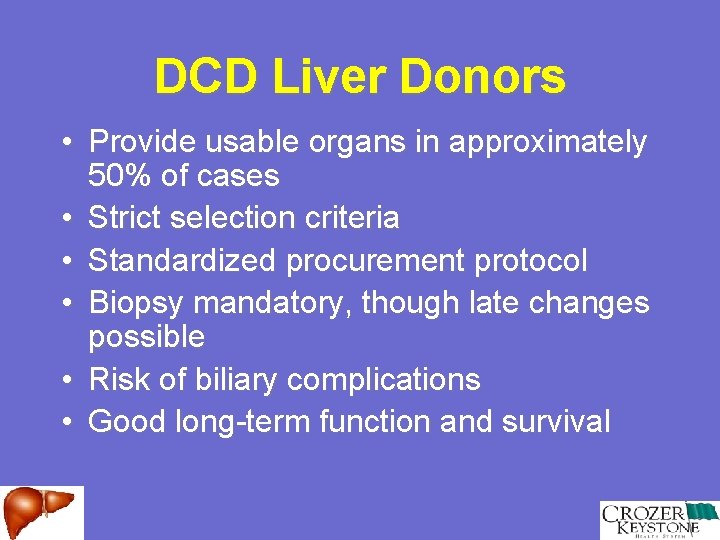
DCD Liver Donors • Provide usable organs in approximately 50% of cases • Strict selection criteria • Standardized procurement protocol • Biopsy mandatory, though late changes possible • Risk of biliary complications • Good long-term function and survival
Hepatitis C Positive Donors
HCV Positive Donors • 100% transmissibility of disease • More worrisome in liver donors • Accept up to grade 2 -3, stage 2 with good initial function • Above that, high risk of PEGF, early cirrhosis and liver failure • Use in tumors, in-extremis cases
HCV infected donors: The Past • • • University of Pittsburgh HCV+ donors for 45 recipients HCV- donors for 515 recipients 1, 3, 5 year graft survival 78, 72, 69% (HCV+) 1, 3, 5 year graft survival 73, 67, 59%(HCV-) Patient and graft survival not statistically significantly different
HCV Positive Donors • 2 -5% of potential organ donors infected • May be used in the presence of the newer DAA therapies (? )
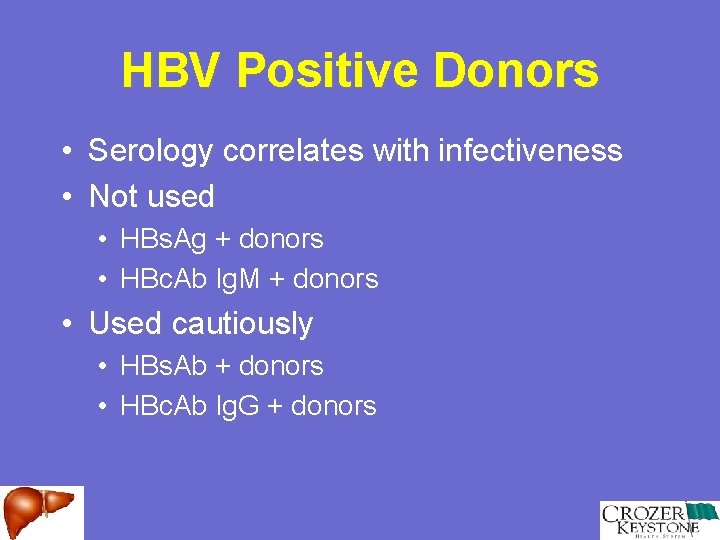
Hepatitis B Positive Donors
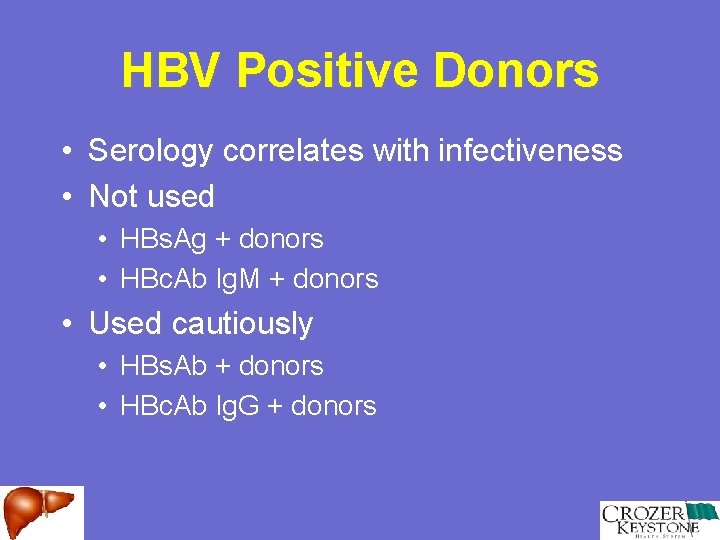
HBV Positive Donors • Serology correlates with infectiveness • Not used • HBs. Ag + donors • HBc. Ab Ig. M + donors • Used cautiously • HBs. Ab + donors • HBc. Ab Ig. G + donors
Older Donors
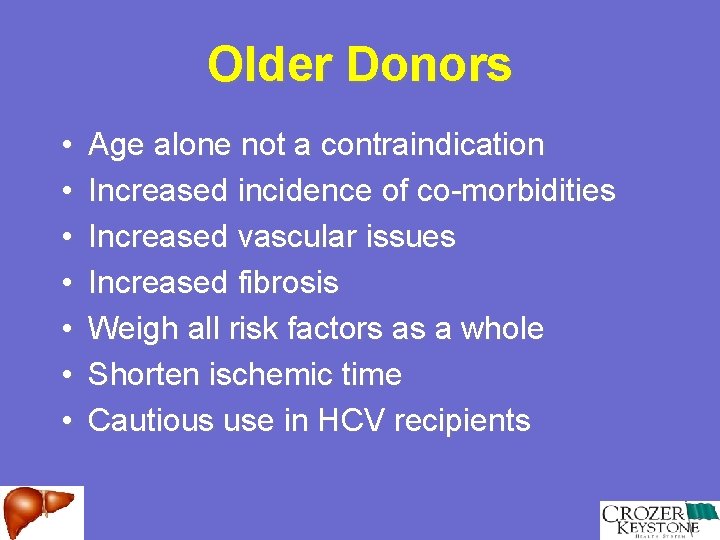
Older Donors • • Age alone not a contraindication Increased incidence of co-morbidities Increased vascular issues Increased fibrosis Weigh all risk factors as a whole Shorten ischemic time Cautious use in HCV recipients
Age and HCV Recurrence • Advancing donor liver age and rapid fibrosis progression following transplantation for hepatitis C. • Donor younger than 40 progress to cirrhosis at 10 years • Donor older than 50 progress to cirrhosis at 2. 2 years
Age and HCV Recurrence • Moreno et al, Madrid • Mean donor age was higher in patients diagnosed with severe recurrent hepatitis • Berenguer et al, (Hepatology 2002) • Reasons for the recent worse outcome in HCV+ recipients include increased donor age and immunosuppression.
Age and HCV Recurrence • UNOS database from 1994 -2002 • Older donor age is associated with lower short-term graft survival in recipients with HCV. • Older donor age does not effect recipients with cholestatic or alcoholic liver disease
Donors With a History of Malignancy
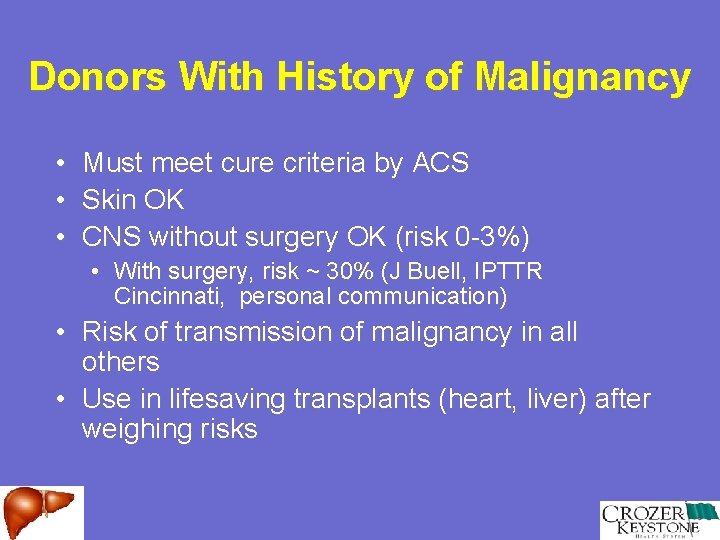
Donors With History of Malignancy • Must meet cure criteria by ACS • Skin OK • CNS without surgery OK (risk 0 -3%) • With surgery, risk ~ 30% (J Buell, IPTTR Cincinnati, personal communication) • Risk of transmission of malignancy in all others • Use in lifesaving transplants (heart, liver) after weighing risks
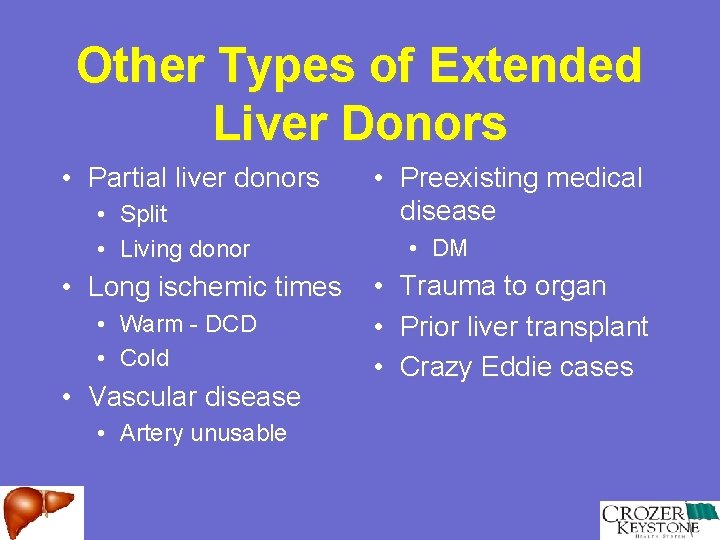
Other Types of Extended Liver Donors • Partial liver donors • Split • Living donor • Long ischemic times • Warm - DCD • Cold • Vascular disease • Artery unusable • Preexisting medical disease • DM • • • Trauma to organ Prior liver transplant Crazy Eddie cases
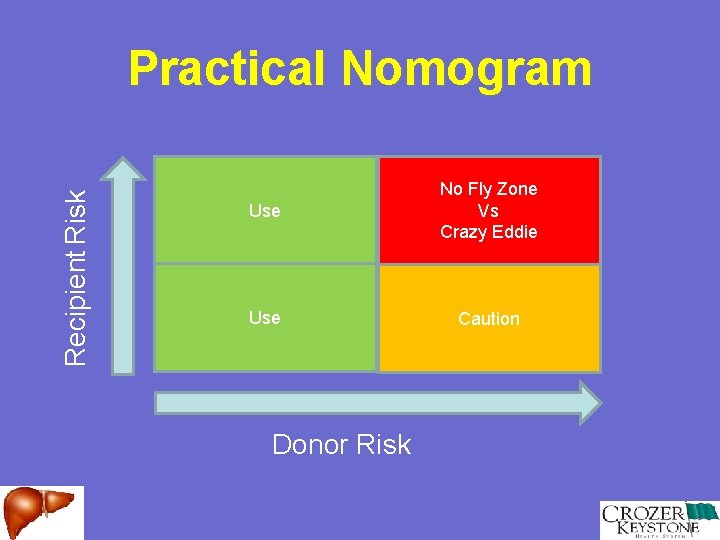
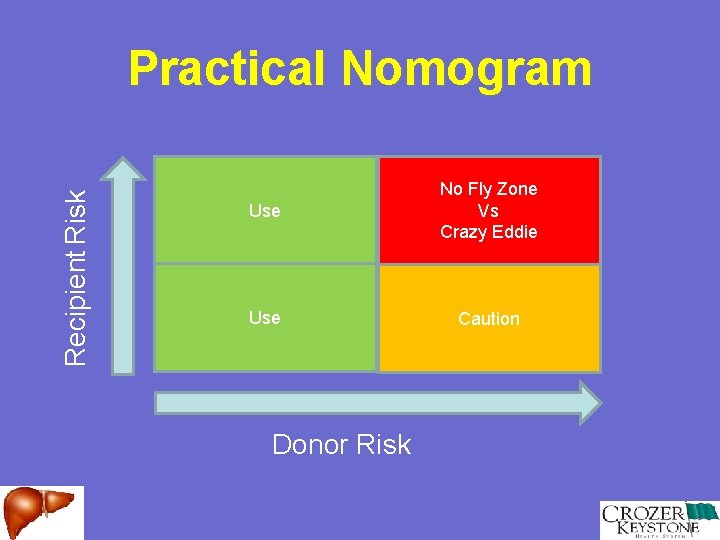
Recipient Risk Practical Nomogram Use No Fly Zone Vs Crazy Eddie Use Caution Donor Risk
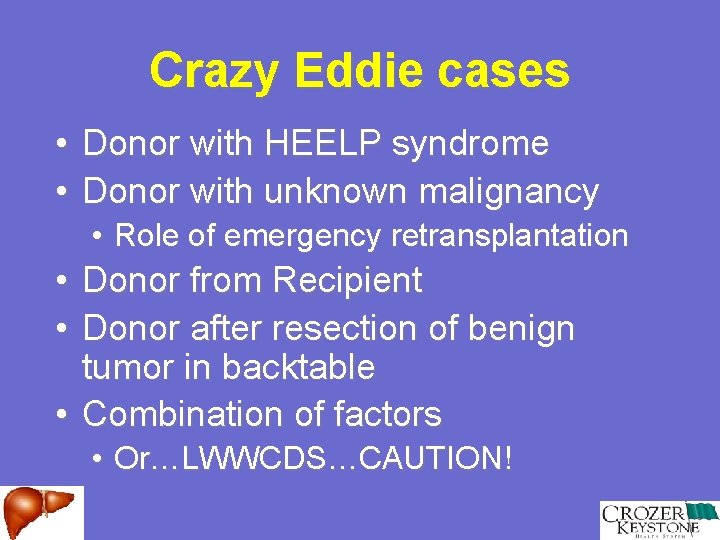
Crazy Eddie cases • • Donor with HEELP syndrome Donor with unknown malignancy • Role of emergency retransplantation • Donor from Recipient • Donor after resection of benign tumor in backtable • Combination of factors • Or…LWWCDS…CAUTION!
Donor Risk Assessment and Management
Donor Factors Influencing Moderate to Severe Preservation Injury • • Macrovesicular Steatosis >30% ICU stay > 4 days High inotropes (DA>15 mic/kg) CIT / per hour Donor age / per year Multiple factors increase risk of severe PI Severe Preservation Injury associated with PNF/DGF
Marginal Markers • Not necessarily constitute unusable organs • High pressor use, DM, HTN, medical disease • Prolonged hospital/ICU stay • Elevated organ function labs • Trends • Consider recipient status

Financial Impact
Financial Impact of Using Extended Donors in Abdominal Organ Transplantation • Items to weigh • Cost of death waiting • Cost of management of complications (kidney, liver, pancreas) • Cost of dialysis (kidneys) • Is using extended donors more costly than regular donors? • Complication rates • Graft survival • Patient survival
Recipient Factors That Increase Cost in Liver Transplantation • Incidence of acute rejection • Tacrolimus more cost-effective than Cy. A 1 • Disease severity 2, 3 • Renal failure 3 • Blood transfusion requirements 3 • Infections • CMV 3 • Bacteremia 3 • Retransplantation 3
Donor Factors Associated With Decreased Graft Function After LT • Univariate • Multivariate • Donor • ICU LOS • Hemodynamic instability • Recipient • Anhepatic period • Blood transfusions • CIT • • Creatinine ICU LOS BMI NOT age! • Recipient • • • Anhepatic period Blood transfusions CIT
Cost of Procuring Extended Donors • Costs average > 20%/organ as compared with regular donors • More time on site, spent allocating organs • Less organs recovered • Significant decrease in survival rates • Kidney - graft (p=0. 02) • Liver – patient (p=0. 05) and graft (p=0. 01) • • Organs were used in sicker patients (liver) Use of extended organs is justified
Conclusions • Broadening the criteria for acceptable abdominal organs for transplant appears to slightly lessen graft survival rates • Use of this organs must be weighed in against the potential to offer lifesaving organ transplantation to an ever-increasing and aging waiting list
Conclusions 2 • Better research and strategies are needed to evaluate these expanded donors and determine which ones are truly marginal or unusable • More detailed follow-up data is needed in recipient of expanded and marginal organs
Thank You