Evolving Technique PFA in Young Patients a Case


- Slides: 25

Evolving Technique: PFA in Young Patients – a Case Approach Phil Davidson, MD Davidson Orthopaedics Park City, Utah Ortho Summit, Las Vegas Dec 6, 2018
Disclosures none
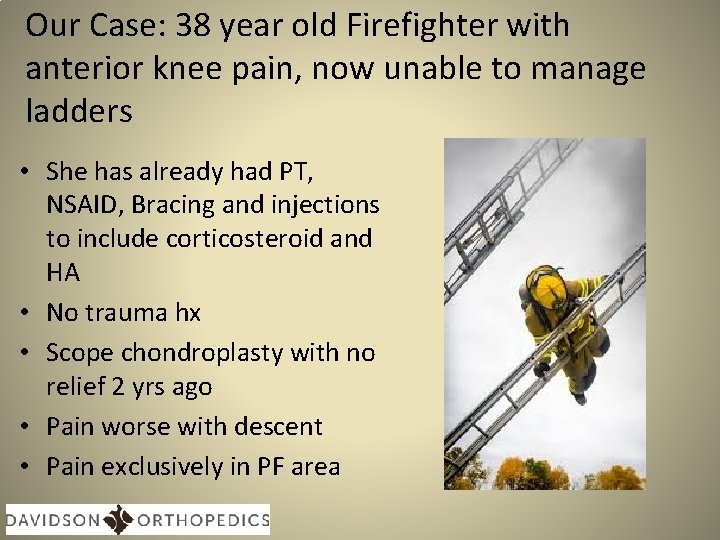
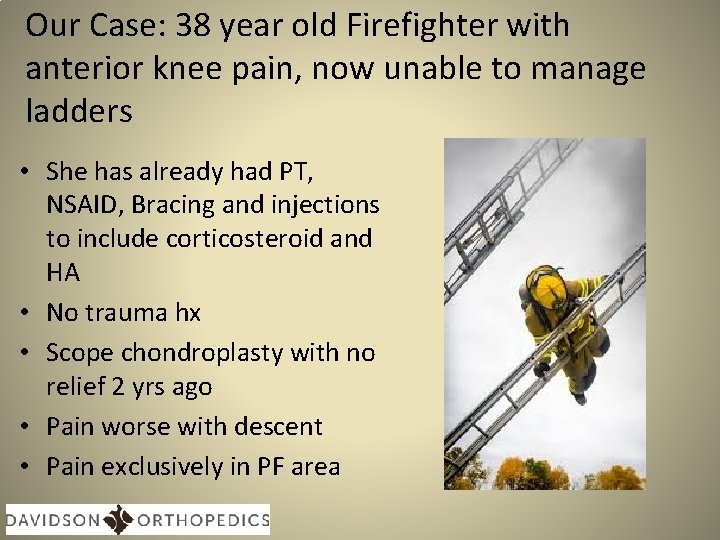
Our Case: 38 year old Firefighter with anterior knee pain, now unable to manage ladders • She has already had PT, NSAID, Bracing and injections to include corticosteroid and HA • No trauma hx • Scope chondroplasty with no relief 2 yrs ago • Pain worse with descent • Pain exclusively in PF area
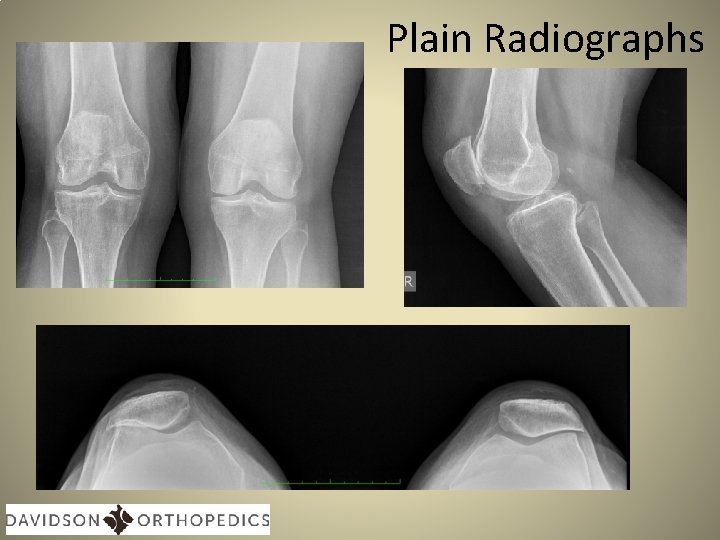
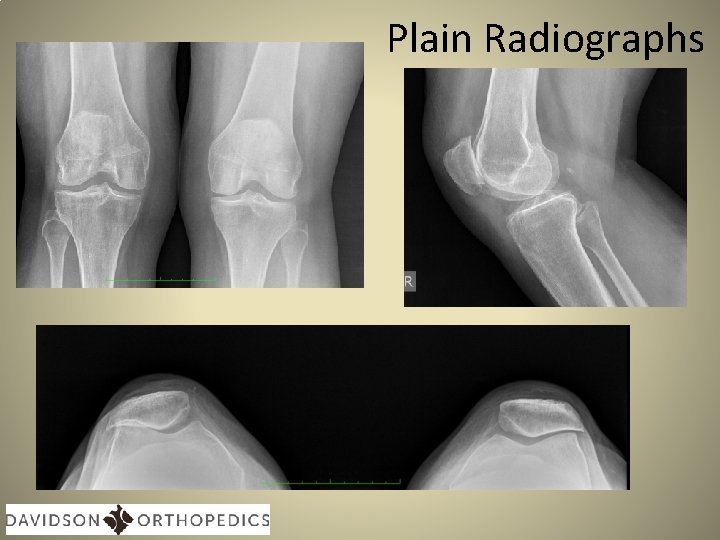
Plain Radiographs
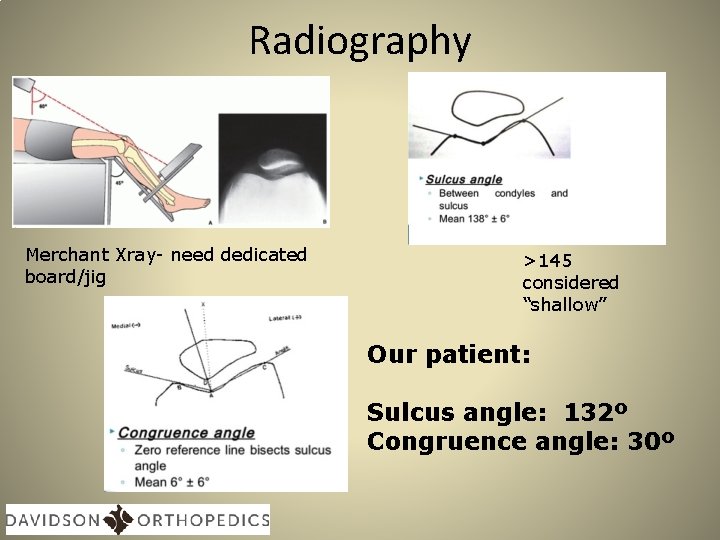
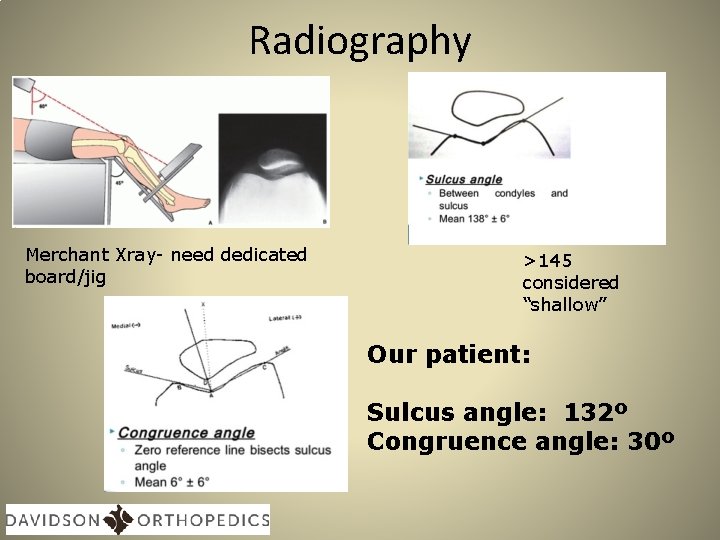
Radiography Merchant Xray- need dedicated board/jig >145 considered “shallow” Our patient: Sulcus angle: 132º Congruence angle: 30º
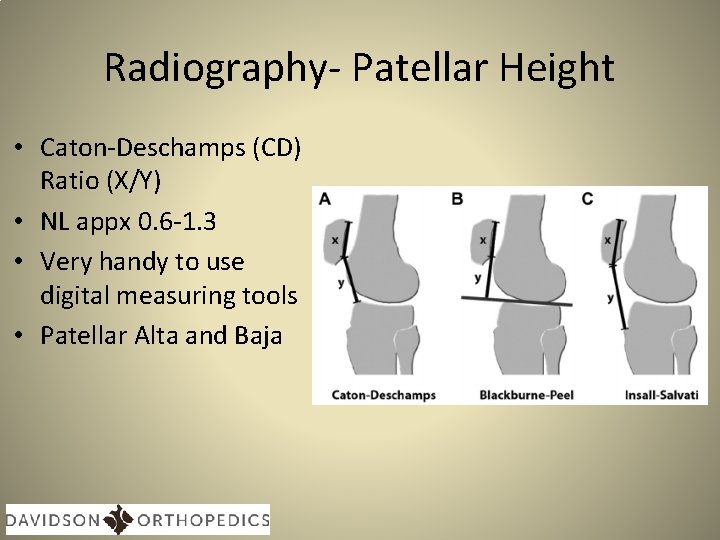
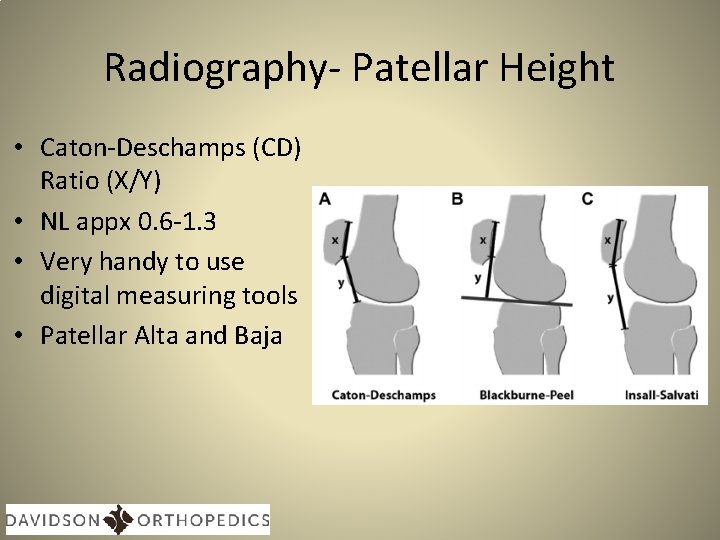
Radiography- Patellar Height • Caton-Deschamps (CD) Ratio (X/Y) • NL appx 0. 6 -1. 3 • Very handy to use digital measuring tools • Patellar Alta and Baja
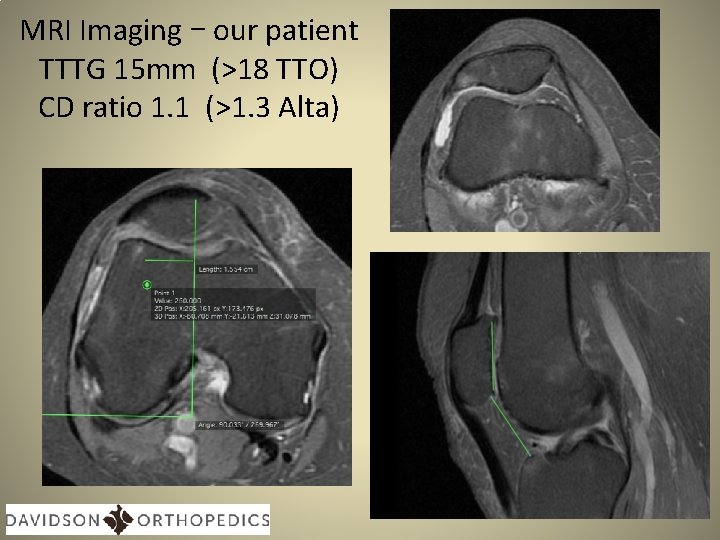
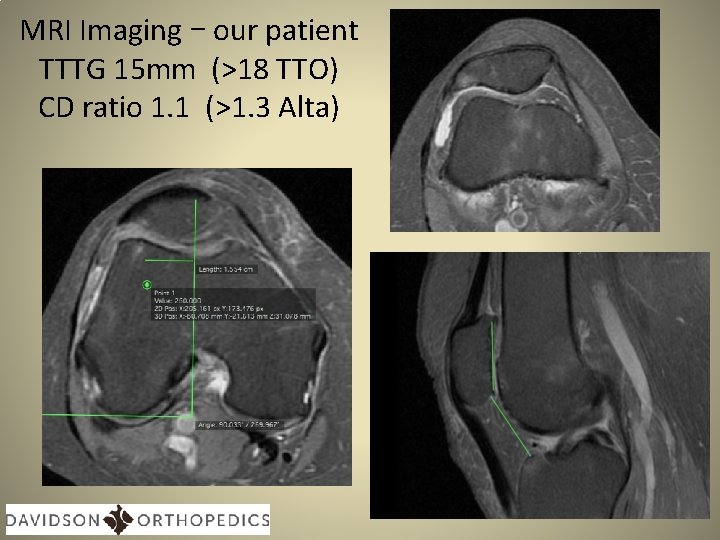
MRI Imaging – our patient TTTG 15 mm (>18 TTO) CD ratio 1. 1 (>1. 3 Alta)
Audience Participation 1. Activity modification, bracing, more non surgical RX 2. TKA 3. Biological Resurfacing 4. TTO alone 5. PFA with prox realignment 6. PFA with TTO
How should we approach options here? • Etiology • Anatomy • Biologic vs Prosthetic
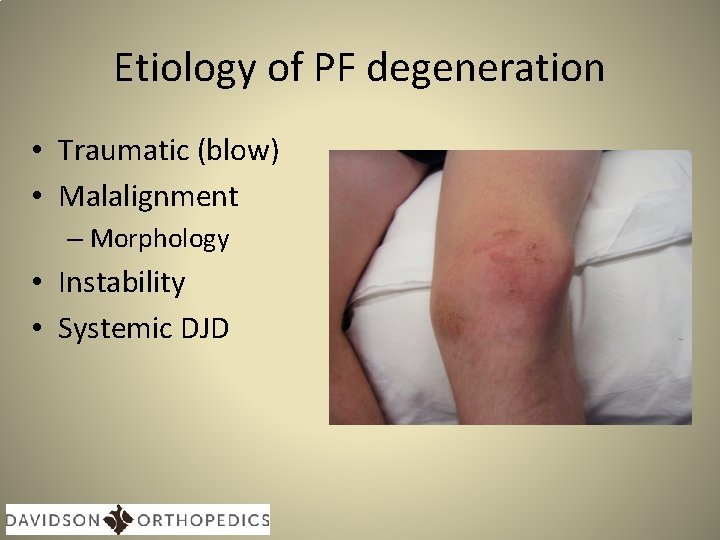
Etiology of PF degeneration • Traumatic (blow) • Malalignment – Morphology • Instability • Systemic DJD
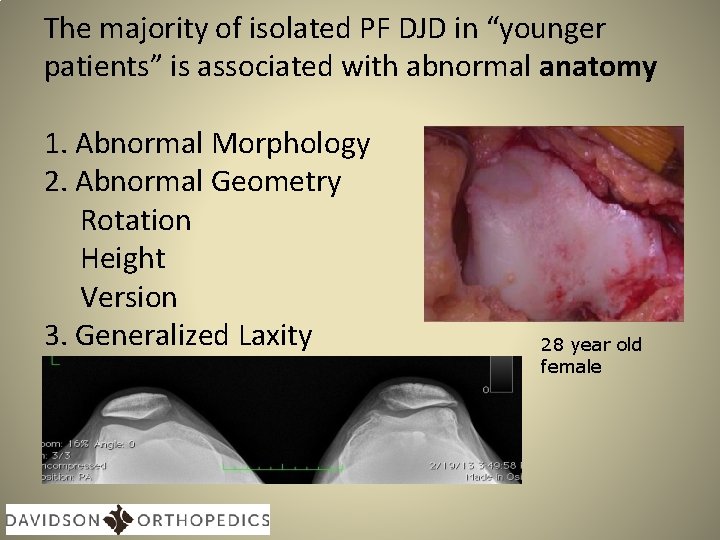
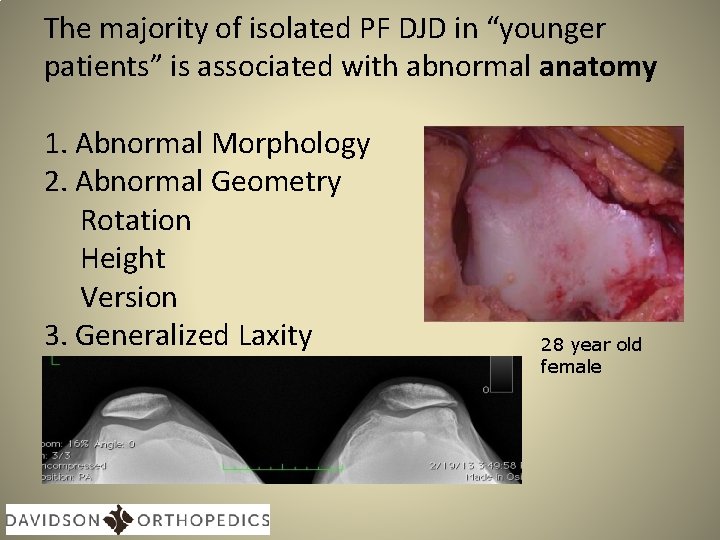
The majority of isolated PF DJD in “younger patients” is associated with abnormal anatomy 1. Abnormal Morphology 2. Abnormal Geometry Rotation Height Version 3. Generalized Laxity 28 year old female
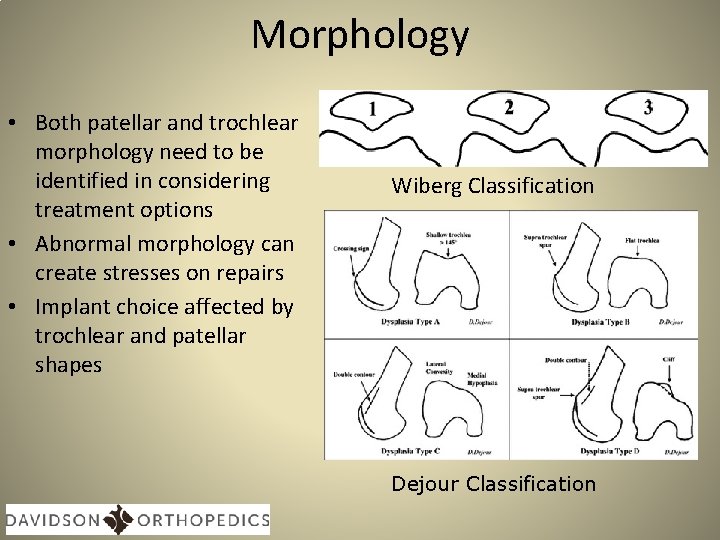
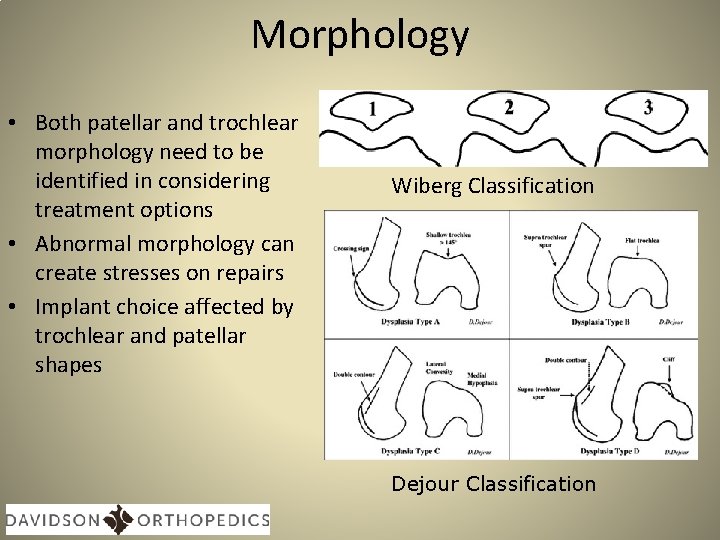
Morphology • Both patellar and trochlear morphology need to be identified in considering treatment options • Abnormal morphology can create stresses on repairs • Implant choice affected by trochlear and patellar shapes Wiberg Classification Dejour Classification
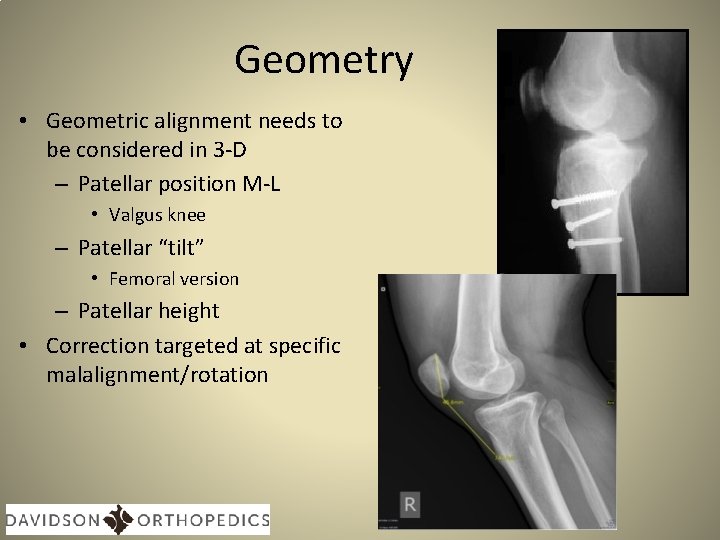
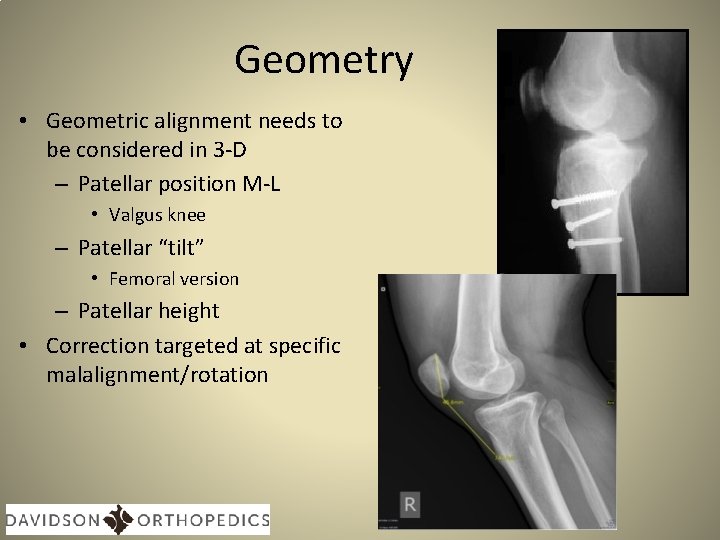
Geometry • Geometric alignment needs to be considered in 3 -D – Patellar position M-L • Valgus knee – Patellar “tilt” • Femoral version – Patellar height • Correction targeted at specific malalignment/rotation
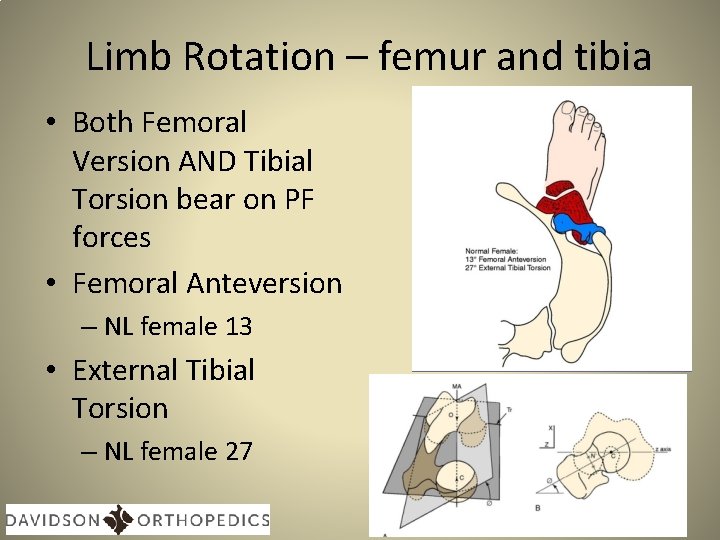
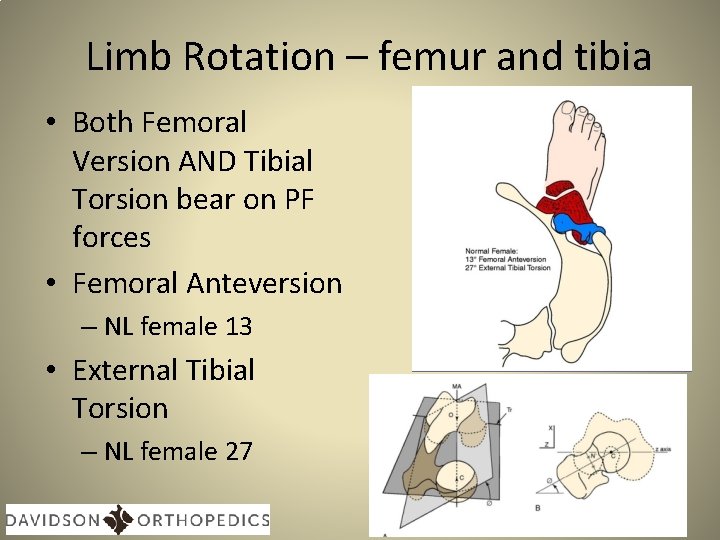
Limb Rotation – femur and tibia • Both Femoral Version AND Tibial Torsion bear on PF forces • Femoral Anteversion – NL female 13 • External Tibial Torsion – NL female 27
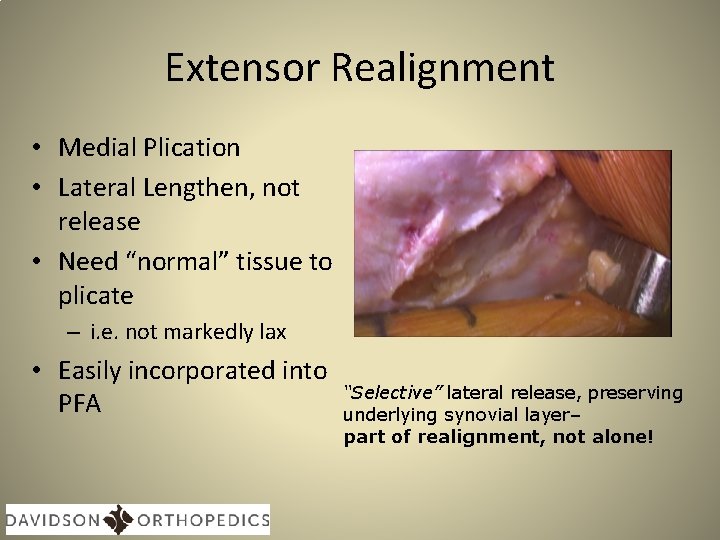
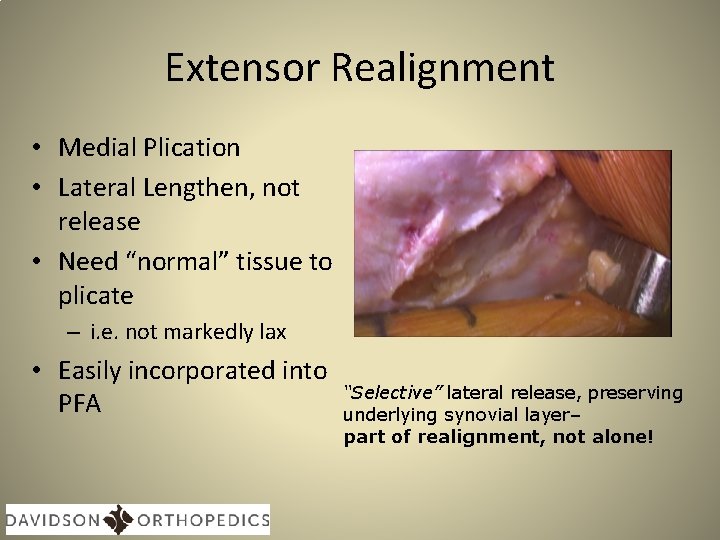
Extensor Realignment • Medial Plication • Lateral Lengthen, not release • Need “normal” tissue to plicate – i. e. not markedly lax • Easily incorporated into PFA “Selective” lateral release, preserving underlying synovial layer– part of realignment, not alone!
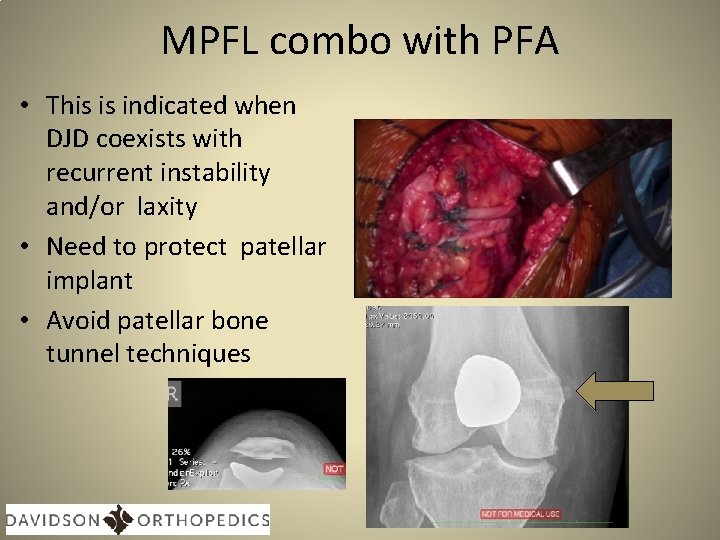
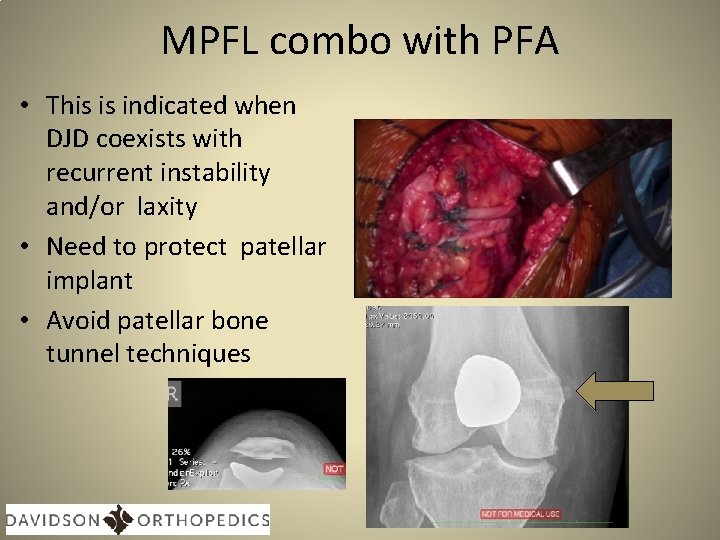
MPFL combo with PFA • This is indicated when DJD coexists with recurrent instability and/or laxity • Need to protect patellar implant • Avoid patellar bone tunnel techniques
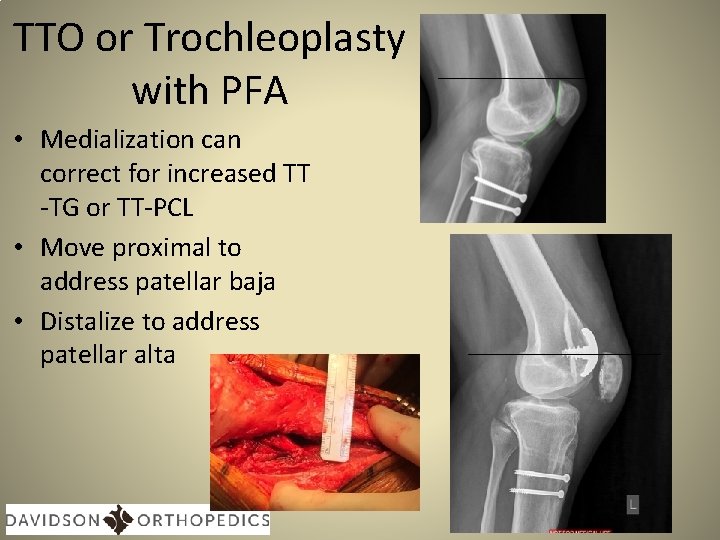
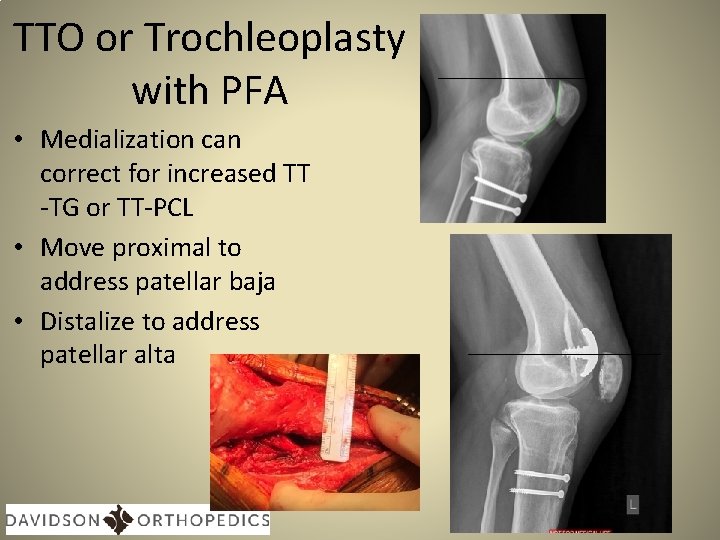
TTO or Trochleoplasty with PFA • Medialization can correct for increased TT -TG or TT-PCL • Move proximal to address patellar baja • Distalize to address patellar alta
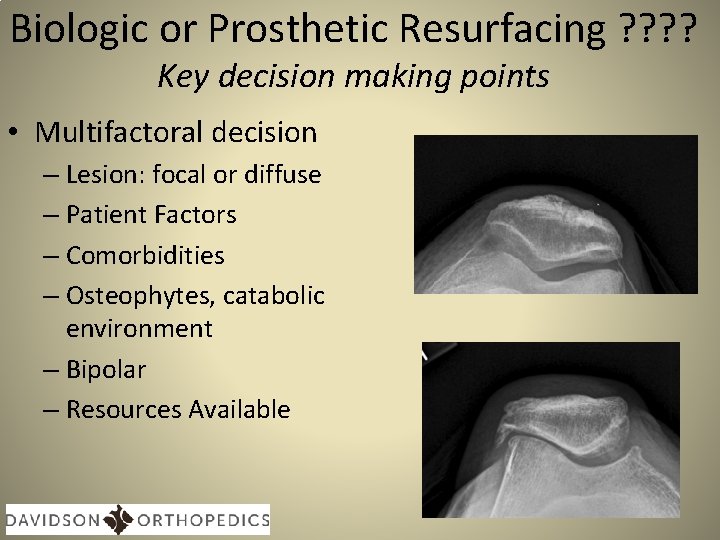
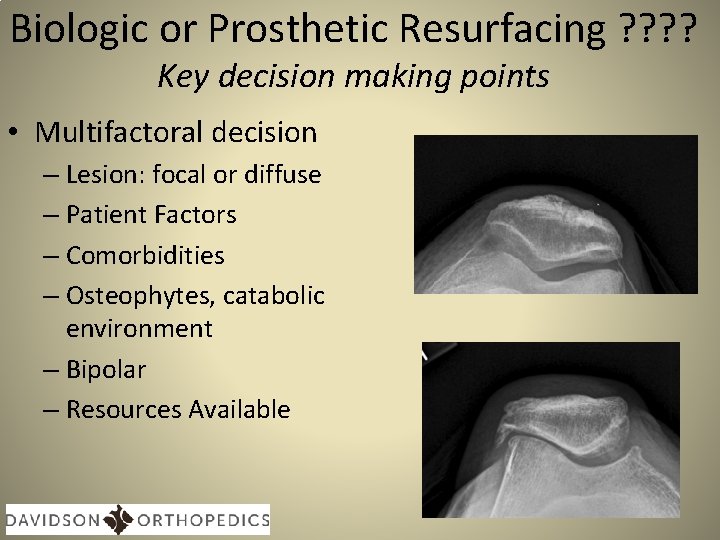
Biologic or Prosthetic Resurfacing ? ? Key decision making points • Multifactoral decision – Lesion: focal or diffuse – Patient Factors – Comorbidities – Osteophytes, catabolic environment – Bipolar – Resources Available
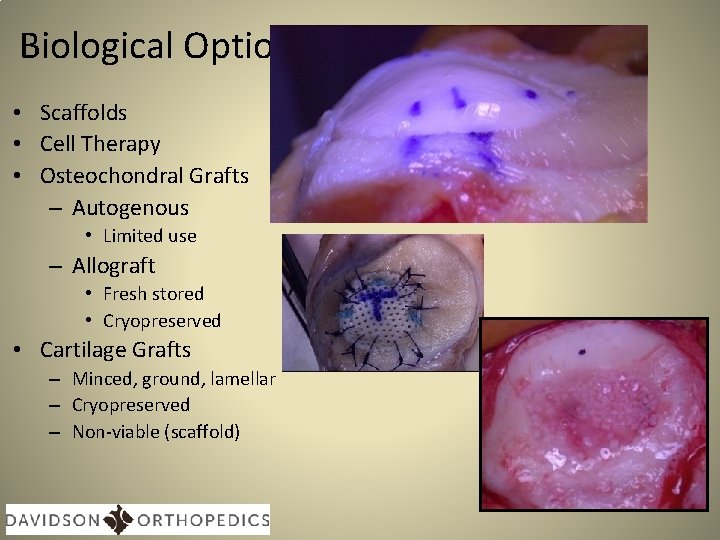
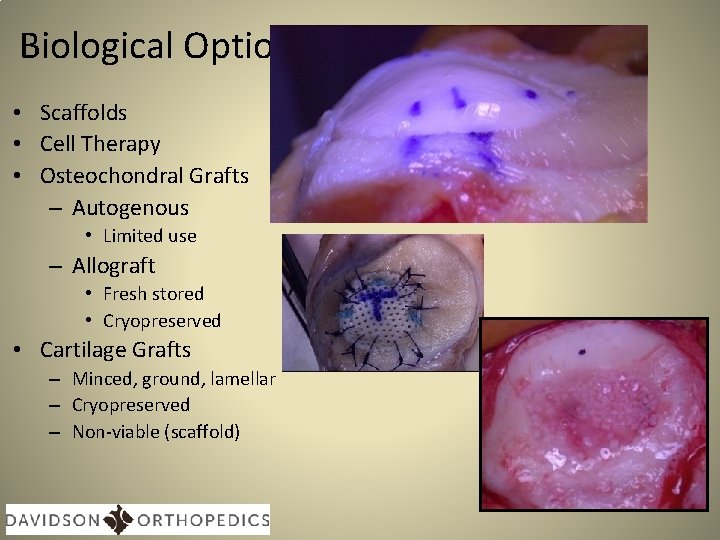
Biological Options • Scaffolds • Cell Therapy • Osteochondral Grafts – Autogenous • Limited use – Allograft • Fresh stored • Cryopreserved • Cartilage Grafts – Minced, ground, lamellar – Cryopreserved – Non-viable (scaffold)
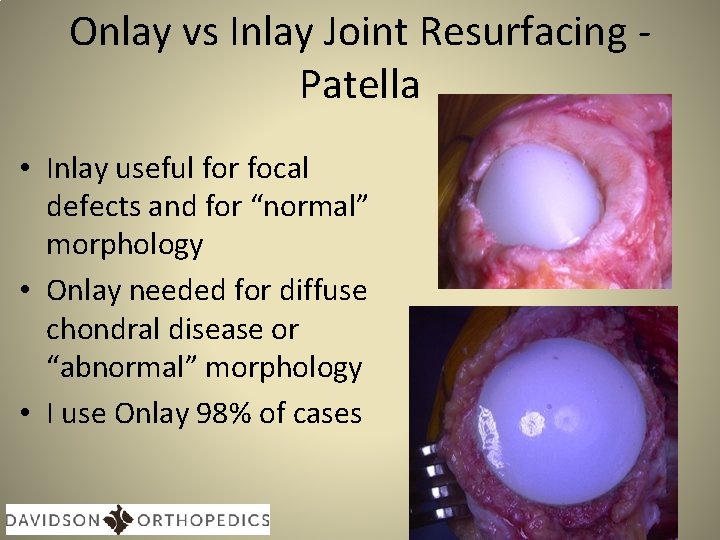
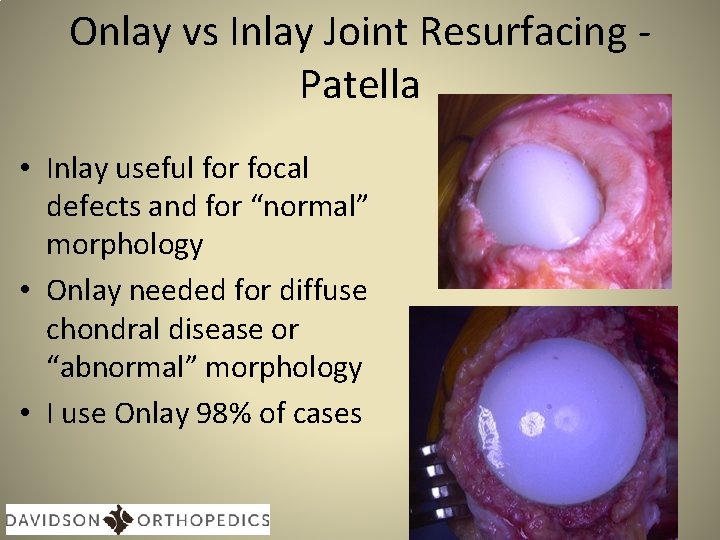
Onlay vs Inlay Joint Resurfacing Patella • Inlay useful for focal defects and for “normal” morphology • Onlay needed for diffuse chondral disease or “abnormal” morphology • I use Onlay 98% of cases
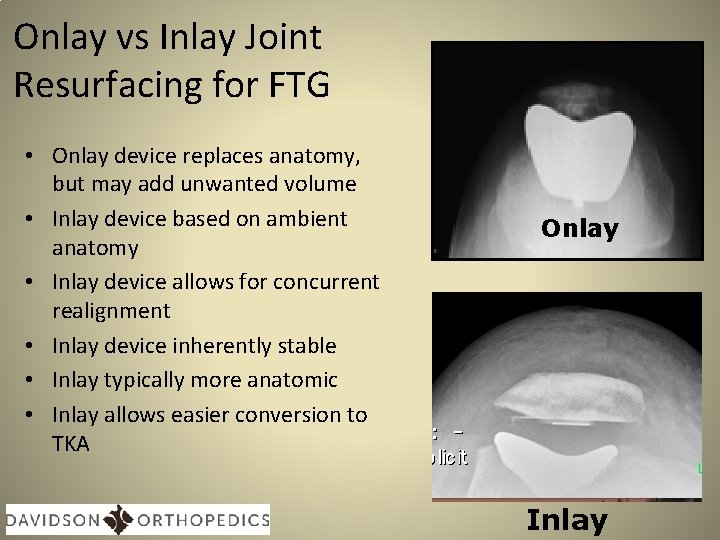
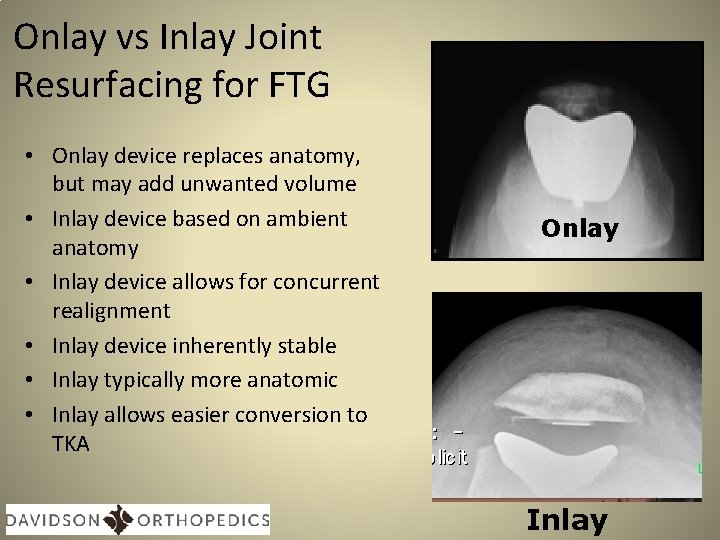
Onlay vs Inlay Joint Resurfacing for FTG • Onlay device replaces anatomy, but may add unwanted volume • Inlay device based on ambient anatomy • Inlay device allows for concurrent realignment • Inlay device inherently stable • Inlay typically more anatomic • Inlay allows easier conversion to TKA Onlay Inlay
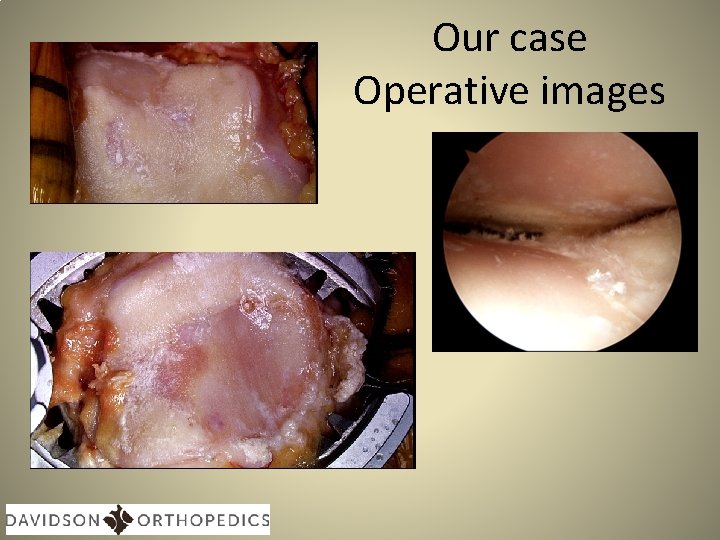
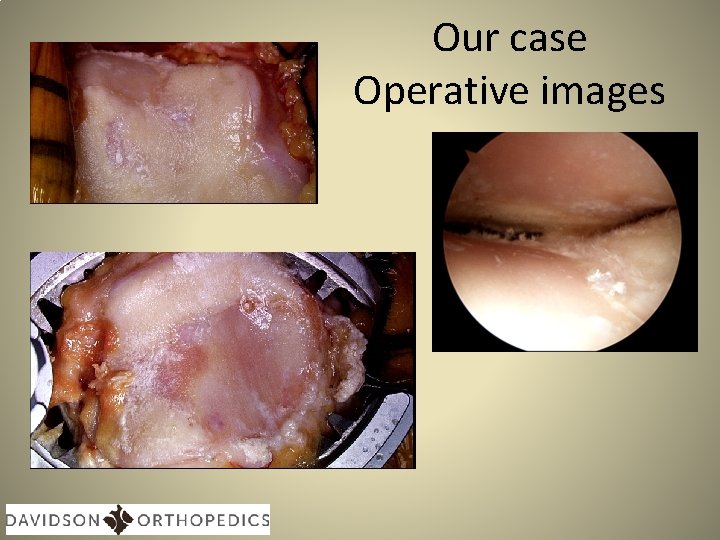
Our case Operative images
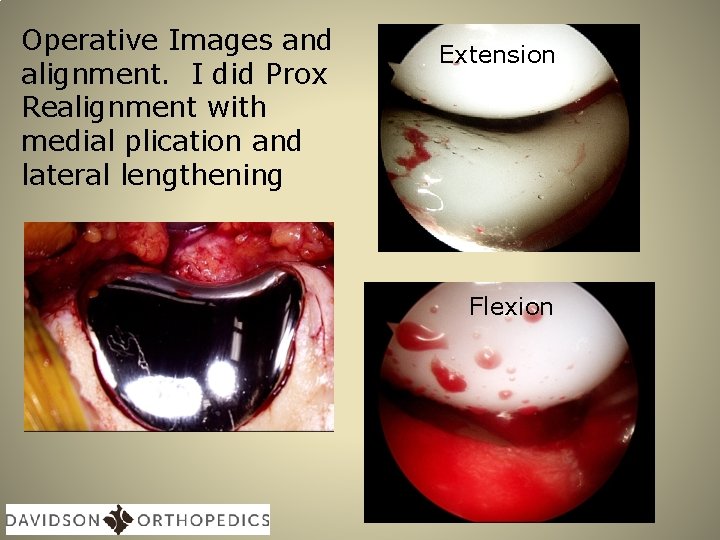
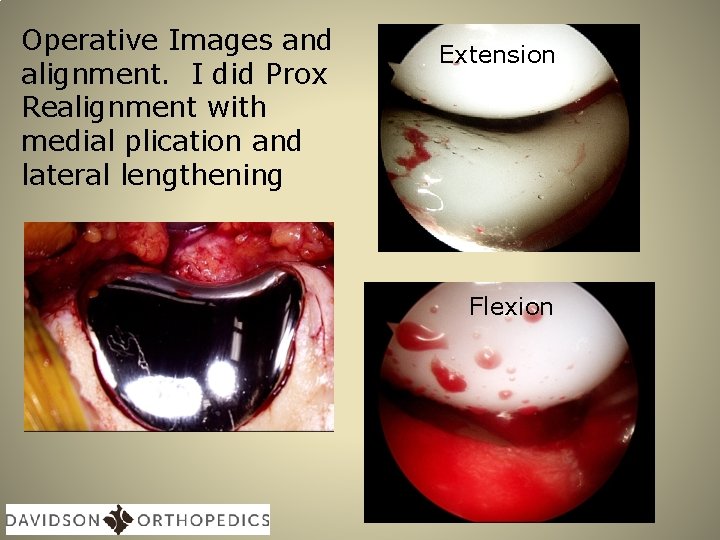
Operative Images and alignment. I did Prox Realignment with medial plication and lateral lengthening Extension Flexion
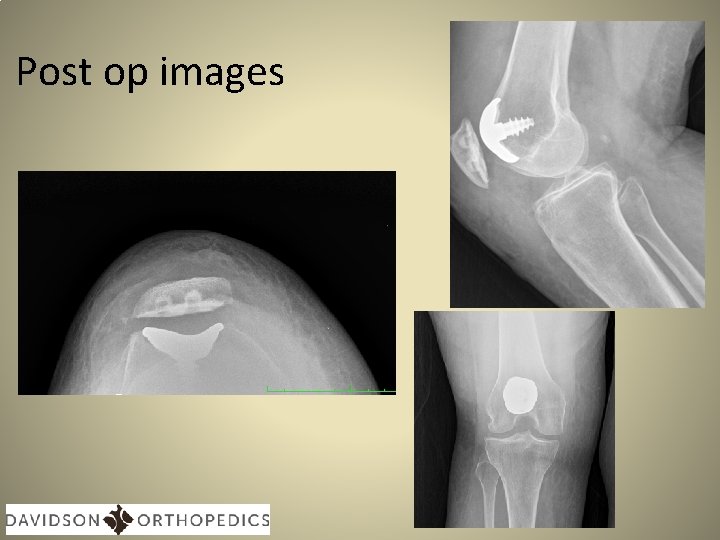
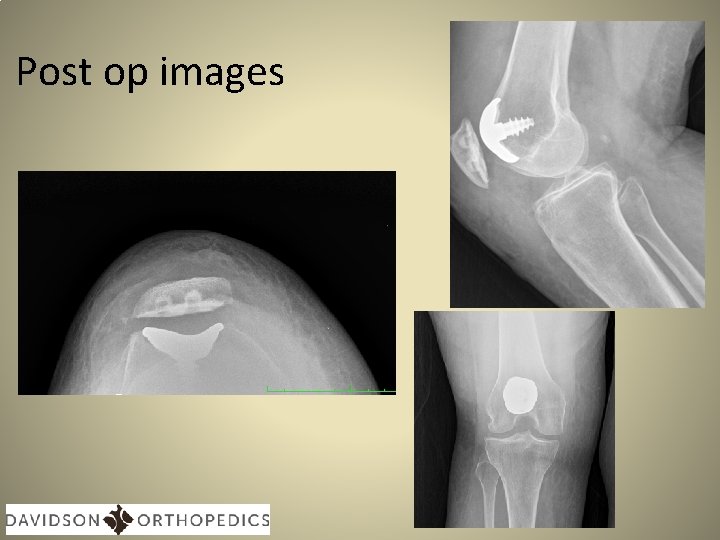
Post op images

Thank You phildavidsonmd@gmail. com