Everything You Never Wanted to Know About Psychiatry
Everything You Never Wanted to Know About Psychiatry But Was on the Internal Medicine Board Examination Cynthia M. A. Geppert, MD Chief Consultation Psychiatry NMVAHCS Professor Department of Psychiatry UNMSOM Amanda Valone, DO UNM Psychiatry, PGY-4
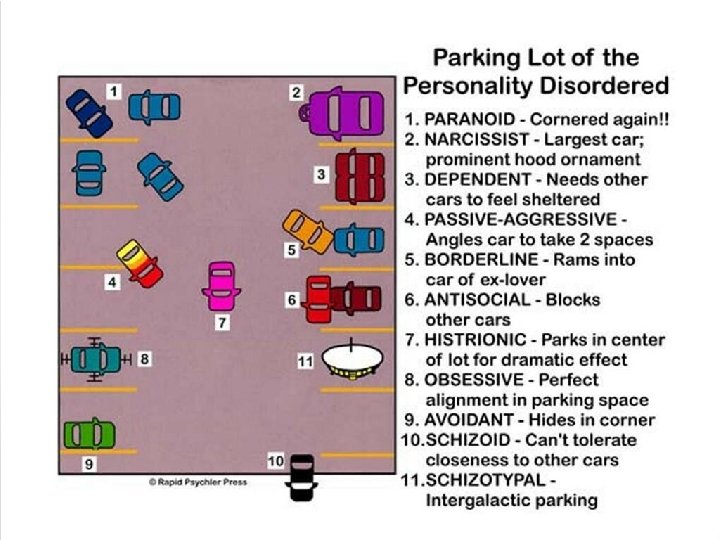
What do parking lots and Winnie the Pooh have to do with psychiatry? • Don’t fall asleep in this lecture and you’ll find out!
Objectives 1. At the end of this presentation the learner will be able to: 2. Identify the diagnostic criteria for mood, anxiety and psychotic disorders. 3. Give examples of the different personality, somatoform disorders and eating disorders. 4. Recommend appropriate psychiatric treatments for the major disorders.
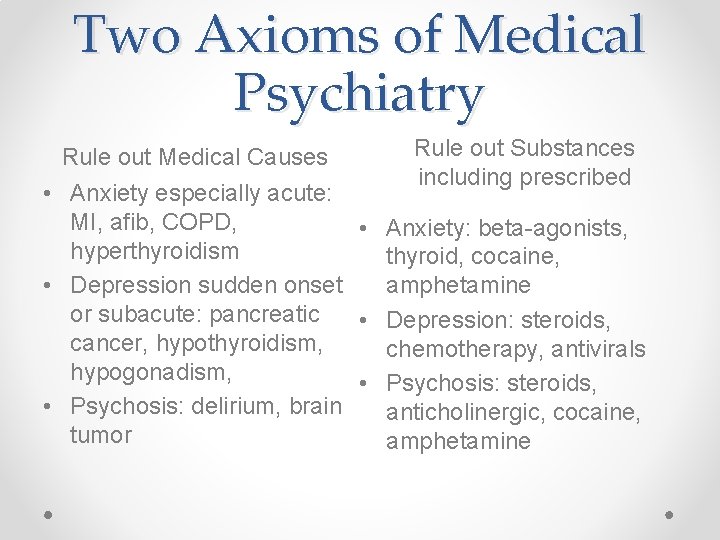
Two Axioms of Medical Psychiatry Rule out Medical Causes Rule out Substances including prescribed • Anxiety especially acute: MI, afib, COPD, • Anxiety: beta-agonists, hyperthyroidism thyroid, cocaine, amphetamine • Depression sudden onset or subacute: pancreatic • Depression: steroids, cancer, hypothyroidism, chemotherapy, antivirals hypogonadism, • Psychosis: steroids, • Psychosis: delirium, brain anticholinergic, cocaine, tumor amphetamine
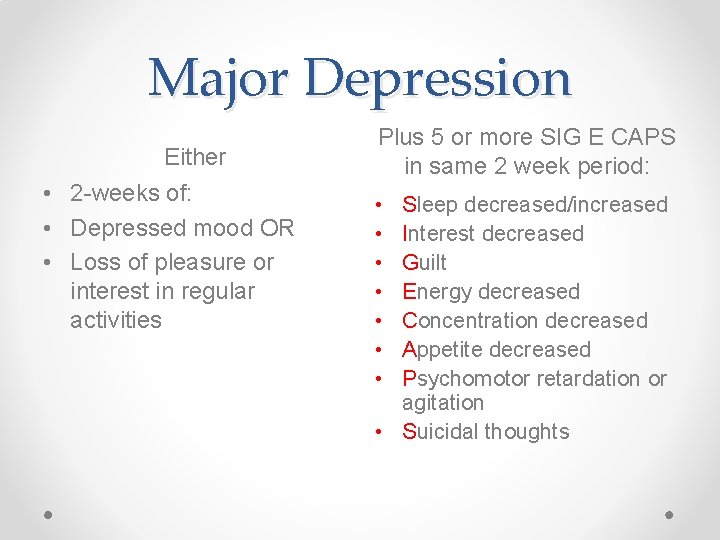
Major Depression Either • 2 -weeks of: • Depressed mood OR • Loss of pleasure or interest in regular activities Plus 5 or more SIG E CAPS in same 2 week period: • • Sleep decreased/increased Interest decreased Guilt Energy decreased Concentration decreased Appetite decreased Psychomotor retardation or agitation • Suicidal thoughts

Persistent Depressive Disorder (Dysthymia) • Depressed mood on most days for 2 years • AND Changes o Sleep o Appetite o Energy • • • Low self-esteem Poor concentration Hopelessness • Depressed mood most of the day on most days for 2 years. • Poor appetite or overeating • Insomnia/hypersomnia • Low energy & Selfesteem • Difficulty making decisions • Hopelessness
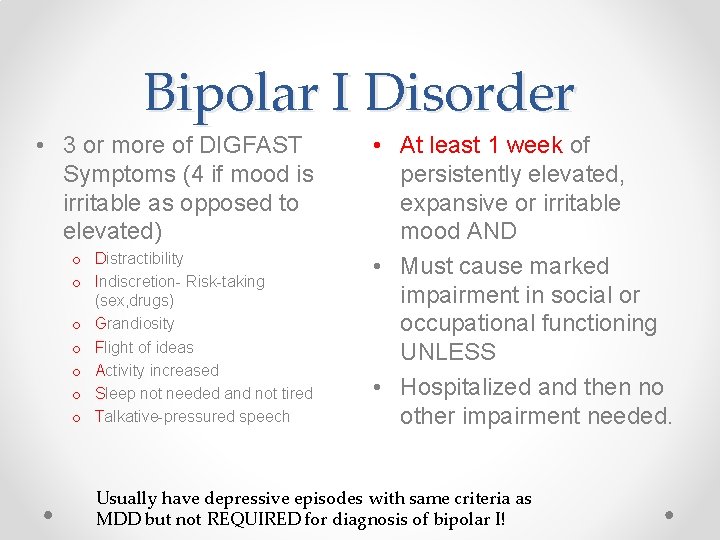
Bipolar I Disorder • 3 or more of DIGFAST Symptoms (4 if mood is irritable as opposed to elevated) o Distractibility o Indiscretion- Risk-taking (sex, drugs) o Grandiosity o Flight of ideas o Activity increased o Sleep not needed and not tired o Talkative-pressured speech • At least 1 week of persistently elevated, expansive or irritable mood AND • Must cause marked impairment in social or occupational functioning UNLESS • Hospitalized and then no other impairment needed. Usually have depressive episodes with same criteria as MDD but not REQUIRED for diagnosis of bipolar I!

Bipolar Disorder Bipolar II • Must have 1 episode of hypomania AND major depression. • Hypomania o 4 days of elevated, expansive or irritable mood plus o Symptoms of DIGFAST (again 3 if elevated mood, 4 if irritable mood). o Often remain functional Cyclothymic Disorder • 2 years of minor and shorter depressions alternating with hypomania. • Not meeting criteria for mania or MDD
Psychotic Disorders • • Schizophrenia Schizoaffective disorder Delusional disorder Brief psychotic disorder (psychotic symptoms 030 days) • Schizophreniform disorder (psychotic symptoms 1 -6 months)
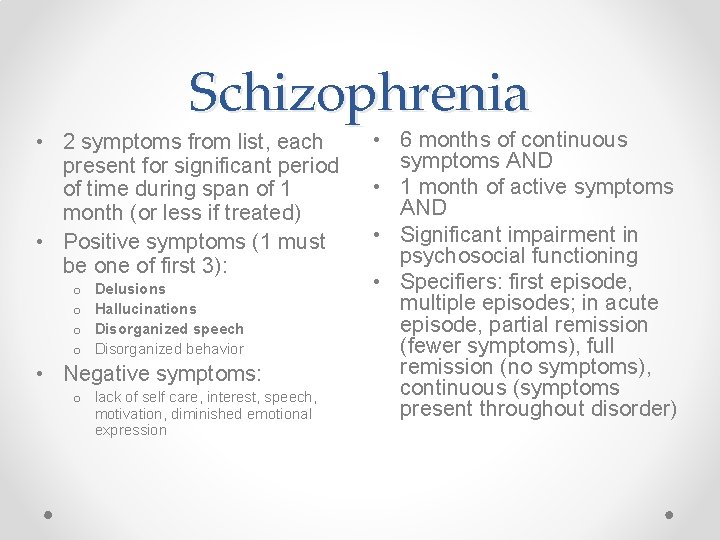
Schizophrenia • 2 symptoms from list, each present for significant period of time during span of 1 month (or less if treated) • Positive symptoms (1 must be one of first 3): o o Delusions Hallucinations Disorganized speech Disorganized behavior • Negative symptoms: o lack of self care, interest, speech, motivation, diminished emotional expression • 6 months of continuous symptoms AND • 1 month of active symptoms AND • Significant impairment in psychosocial functioning • Specifiers: first episode, multiple episodes; in acute episode, partial remission (fewer symptoms), full remission (no symptoms), continuous (symptoms present throughout disorder)
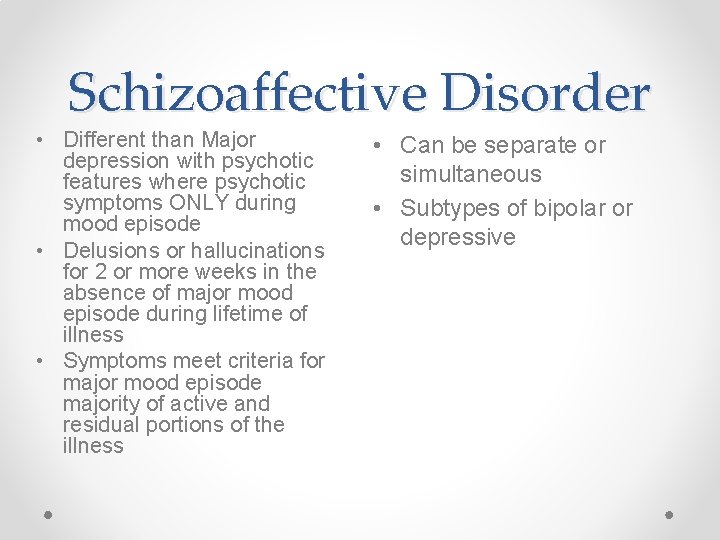
Schizoaffective Disorder • Different than Major depression with psychotic features where psychotic symptoms ONLY during mood episode • Delusions or hallucinations for 2 or more weeks in the absence of major mood episode during lifetime of illness • Symptoms meet criteria for major mood episode majority of active and residual portions of the illness • Can be separate or simultaneous • Subtypes of bipolar or depressive
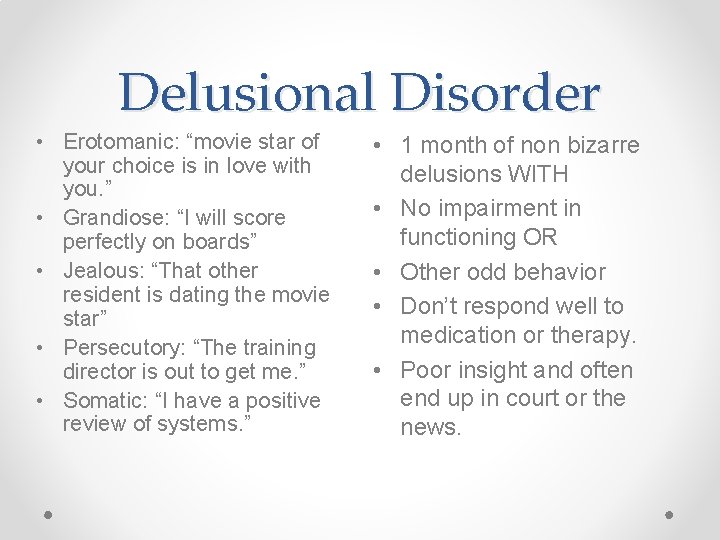
Delusional Disorder • Erotomanic: “movie star of your choice is in love with you. ” • Grandiose: “I will score perfectly on boards” • Jealous: “That other resident is dating the movie star” • Persecutory: “The training director is out to get me. ” • Somatic: “I have a positive review of systems. ” • 1 month of non bizarre delusions WITH • No impairment in functioning OR • Other odd behavior • Don’t respond well to medication or therapy. • Poor insight and often end up in court or the news.

Anxiety Disorders • Panic disorder • Generalized anxiety disorder • Obsessive compulsive disorder • Posttraumatic stress disorder
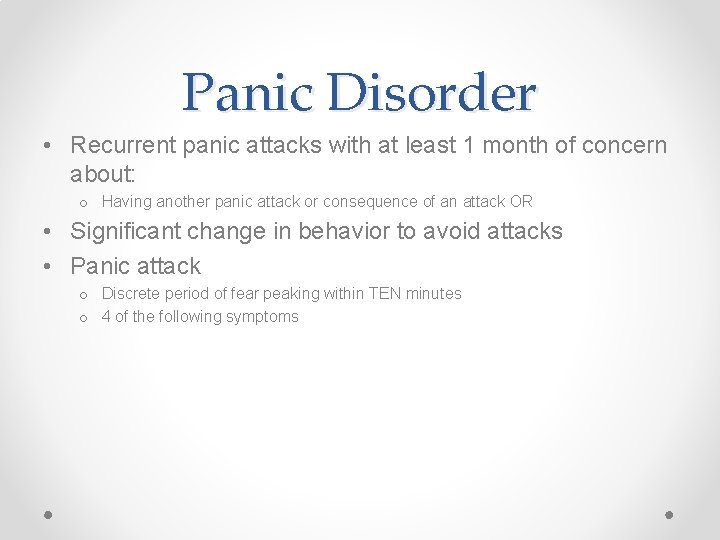
Panic Disorder • Recurrent panic attacks with at least 1 month of concern about: o Having another panic attack or consequence of an attack OR • Significant change in behavior to avoid attacks • Panic attack o Discrete period of fear peaking within TEN minutes o 4 of the following symptoms

Panic Disorder Symptoms • • Hot flushes Sense of choking Diaphoresis Fear of losing control or dying • Parathesias/numbness • Can be with or without agoraphobia • • • Dizziness Palpitations Chest pain Nausea Depersonalization or derealization • Dyspnea • Chills
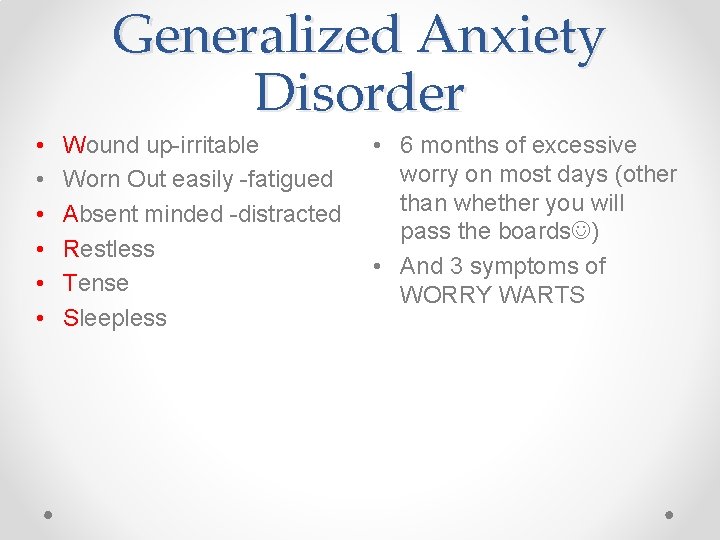
Generalized Anxiety Disorder • • • Wound up-irritable Worn Out easily -fatigued Absent minded -distracted Restless Tense Sleepless • 6 months of excessive worry on most days (other than whether you will pass the boards ) • And 3 symptoms of WORRY WARTS

Obsessive Compulsive Disorder (OCD=MD) • Obsessions: o Recurrent, persistent, intrusive o Inappropriate thoughts that cause distress (sex & violence) • Compulsions o Repetitive behaviors performed in response to obsessions or rules. o Washing (most common), checking, counting, praying, hoarding. • Obsessions and/or compulsions o Patient and others see as excessive o Ego-dystonic o Cause marked distress o Interfere with function o Different from psychotic symptoms as patient has insight


Posttraumatic Stress disorder • Experience, witness or confront an event that involved: • Death or serious injury or the threat of same • Response to threat or event involve overwhelming fear/horror or helplessness • >1 month of symptoms in the following clusters • Symptoms lasting less than 1 month is Acute Stress Disorder.
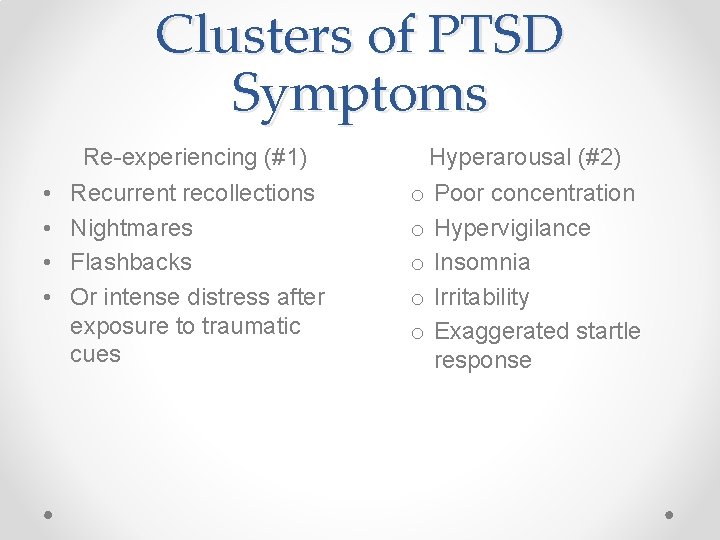
Clusters of PTSD Symptoms Re-experiencing (#1) • • Recurrent recollections Nightmares Flashbacks Or intense distress after exposure to traumatic cues Hyperarousal (#2) o o o Poor concentration Hypervigilance Insomnia Irritability Exaggerated startle response

PTSD Clusters Avoidance (#3) • Avoidance of thoughts, feelings, sensations or conversations, people, places, activities associated with the traumatic event • Difficulty remembering aspects of the event Numbing (#4) • Loss of interest in usual activities • Detachment or estrangement • Sense of foreshortened future • Restricted affect
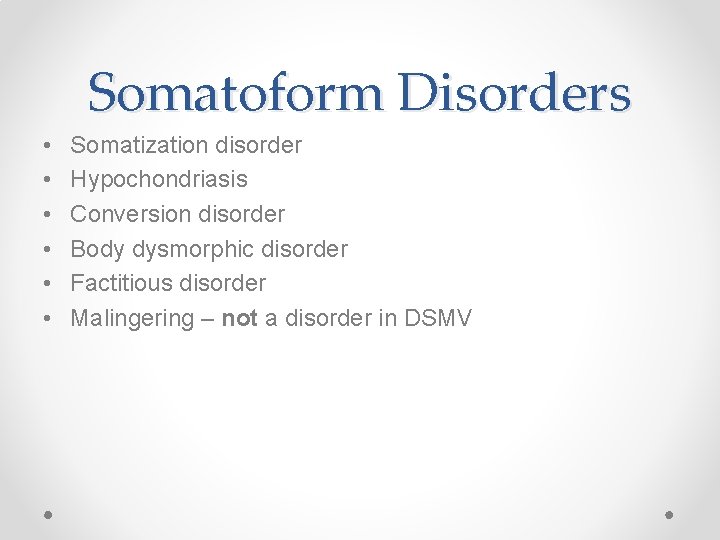
Somatoform Disorders • • • Somatization disorder Hypochondriasis Conversion disorder Body dysmorphic disorder Factitious disorder Malingering – not a disorder in DSMV

Somatic Symptom Disorder • 1 or more somatic symptoms that are distressing or result in significant disruption of life • Excessive thoughts, feelings or behaviors related to somatic symptoms • May not be one specific symptom but symptomatic for more than 6 months • Multiple physical complaints • Onset before age of 30 • Treatment is sought for the complaints • Disorder impairs functioning • More common in women, less educated, lower SE

Body Dysmorphic Disorder • Intense preoccupation with a minor or even imagined physical defect not evident to others. • Can reach delusional proportions. • Often develop repetitive behaviors. • Desperate attempts to correct e. g. , plastic surgery.

Other Somatoform Disorders • Hypochondriasis (Now called Illness Anxiety Disorder) o Preoccupation of strong belief (NOT a delusion) that a serious illness, e. g. , cancer or ulcer, is present in response to benign perturbations in physiologic function like dyspepsia or fatigue o Requires extensive reassurance • Conversion disorder o 1 symptom affecting sensory or motor function, e. g. , blindness, paralysis. o Psychological factors are considered important in onset and perpetuation of symptoms

Differential Diagnosis Disorder Motivation Awareness Factitious Disorder: intentional feigning of signs and symptoms of illness. *Munchausen and by proxy most infamous. Primary gain is to obtain the attention and succor of the sick role. Tertiary gain in factitious disorder by proxy. Conscious of causing the symptoms but often not of the motivation. Somatic Symptom Disorder Goal is to have medical problem treated and symptoms relieved. May develop primary and secondary gain from disorder. Conscious of pain and distress but not usually that is psyche more than soma causing.
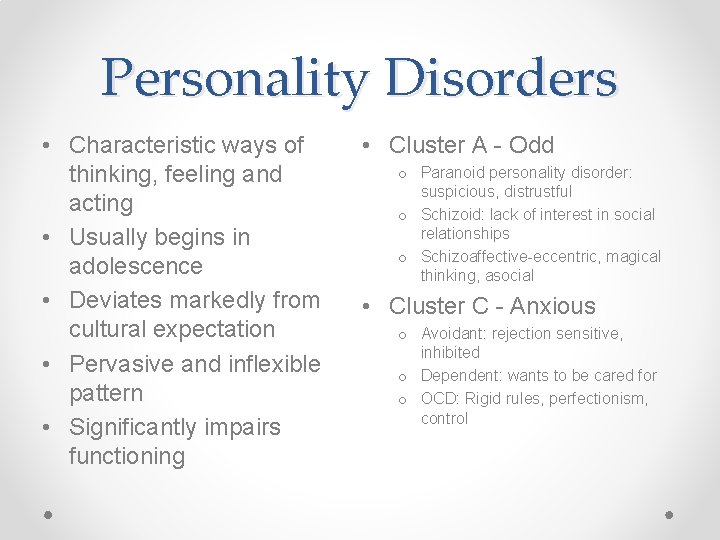
Personality Disorders • Characteristic ways of thinking, feeling and acting • Usually begins in adolescence • Deviates markedly from cultural expectation • Pervasive and inflexible pattern • Significantly impairs functioning • Cluster A - Odd o Paranoid personality disorder: suspicious, distrustful o Schizoid: lack of interest in social relationships o Schizoaffective-eccentric, magical thinking, asocial • Cluster C - Anxious o Avoidant: rejection sensitive, inhibited o Dependent: wants to be cared for o OCD: Rigid rules, perfectionism, control

Cluster B Personality Disorder – Erratic and Dramatic Borderline Personality Disorder • History of intense conflicted relationships • Often unstable or traumatic childhood • Emotional liability • Suicidal behavior • Intense fear of abandonment Narcissistic Personality Disorder • Believes in own specialness • Needs attention • Arrogant • Entitled • Exploitive • Seeks power • Lack of empathy

Cluster B Histrionic • Pervasive pattern of excess emotion since adolescence. • Must be center of attention • Sexually provocative/seductive • Shallow rapid mood shifts • Highly suggestive • Overly familiar • Drama queen Antisocial • Pervasive pattern violation of the rights of others starting at least by age 15. • Lying and conning • Illegal & criminal conduct • Lack of remorse and responsibility • Poor impulse control • Angry and aggressive


Eating Disorders Anorexia Nervosa • Refusal to maintain normal body weight (LOW BMI is key! mild: BMI >17, moderate: 16 -16. 99, severe: 15 -15. 99, extreme: <15) • Intense fear of becoming fat or gaining weight • Distortion of body image: emaciated thinks fat. o Restricting type: fasts and exercises, no purging o Binge-purge: overuse of laxatives, self induced vomiting Bulimia Nervosa • Recurrent binge eating o Eating within a 2 -hr period much more food than normal. o Lack of control over eating o Mild: 1 -3/wk, moderate: 4 -7/wk, severe: 8 -13/wk, extreme: >14/wk • Overemphasis on body • Recurrent purging to prevent weight gain o o Fasting Self-induced vomiting Laxatives Excessive exercise Often normal or increased BMI.

Medical Complications of Eating Disorders • • Symptoms Dizziness Cold intolerance Fatigue Dyspepsia Headache Constipation/Bloating Loss of sex drive Menstrual problems (more commonly with anorexia) Signs • • • Bradycardia Erosion of dental enamel Hypotension Pitting edema Swollen parotid glands Muscle weakness/wasting Russell’s sign Lanugo Electrolyte abnormalities (HYPO – sodium, potassium, magnesium, phosphate, creatinine; although may be normal in restricting type) Acid base – chloride responsive metabolic alkalosis
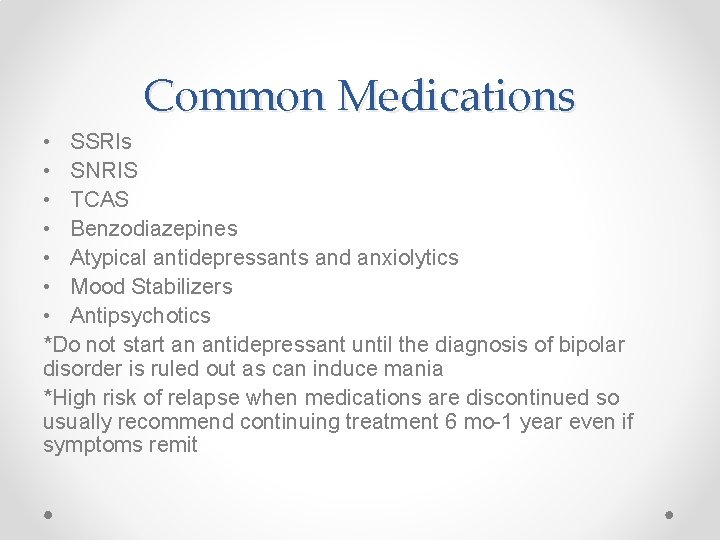
Common Medications • SSRIs • SNRIS • TCAS • Benzodiazepines • Atypical antidepressants and anxiolytics • Mood Stabilizers • Antipsychotics *Do not start an antidepressant until the diagnosis of bipolar disorder is ruled out as can induce mania *High risk of relapse when medications are discontinued so usually recommend continuing treatment 6 mo-1 year even if symptoms remit

SSRIs • Fluoxetine: very long half life, many metabolites, drug interactions, anxiogenic: good for young, not for old • Citalopram: not above 40 mg, 20 mg if 60 years or older, QTc prolongation, don’t use with other risks. • Escitalopram: fewest drug interactions • Sertraline: preferred in renal failure • Paroxetine: most sedating, anticholinergic, withdrawal syndrome • Fluvoxamine: mostly OCD, many drug interactions

SSRI Basics • • Takes 3 -6 weeks to respond Safe in overdose No one agent superior to any other Early side effects mainly headache, GI, anxiety, sexual dysfunction longer lasting. • Can affect bleeding time, increase GI bleeding.

Serotonin-Norepinephrine Reuptake Inhibitors • Venlafaxine’s main side effect (and most tested) is hypertension • Serotonergic below 150 mg; only effect norepinephrine above these dosages • Duloxetine: better for pain, not as good for depression • Caution in liver and kidney disease • Better tolerated TCAs • May work faster and better • IR formulation especially has severe withdrawal syndrome • May work better in men. SSRIs in women.

TCA Basics Serious • Anticholinergic • Antihistaminergic • Need EKG if over 50 or any cardiac history • In overdose block fast sodium channel, death by arrhythmias or seizures requiring IV sodium bicarbonate. Common • • • Orthostatic hypotension Urinary retention Constipation Sedation Dry mouth

TCAs Secondary amines • Despiramine: well tolerated, cardiac side effects especially younger • Nortriptyline: fewer side effects, less anticholinergic Tertiary amines • Doxepin very potent H 2 blocker used in dermatology. • Amitriptyline: good for migraine, neuropathic pain • Clomipramine only used in OCD
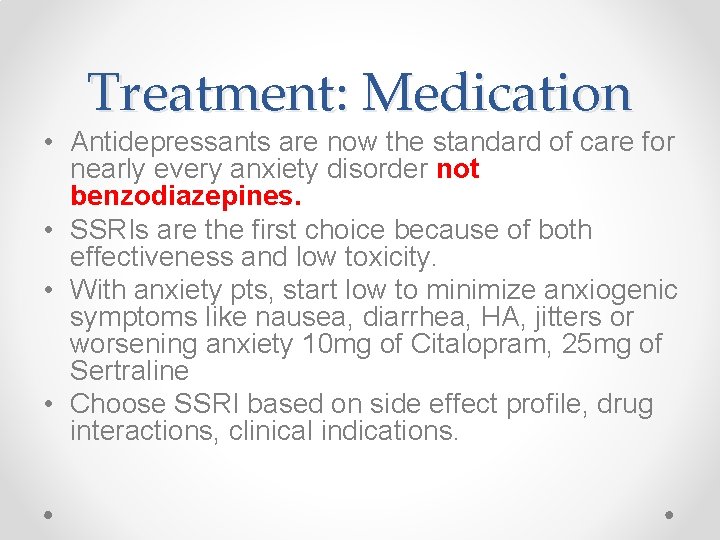
Treatment: Medication • Antidepressants are now the standard of care for nearly every anxiety disorder not benzodiazepines. • SSRIs are the first choice because of both effectiveness and low toxicity. • With anxiety pts, start low to minimize anxiogenic symptoms like nausea, diarrhea, HA, jitters or worsening anxiety 10 mg of Citalopram, 25 mg of Sertraline • Choose SSRI based on side effect profile, drug interactions, clinical indications.
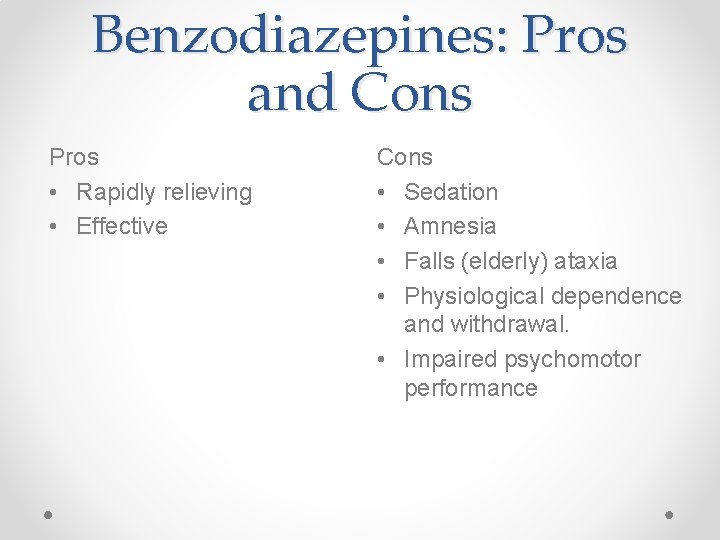
Benzodiazepines: Pros and Cons Pros • Rapidly relieving • Effective Cons • Sedation • Amnesia • Falls (elderly) ataxia • Physiological dependence and withdrawal. • Impaired psychomotor performance
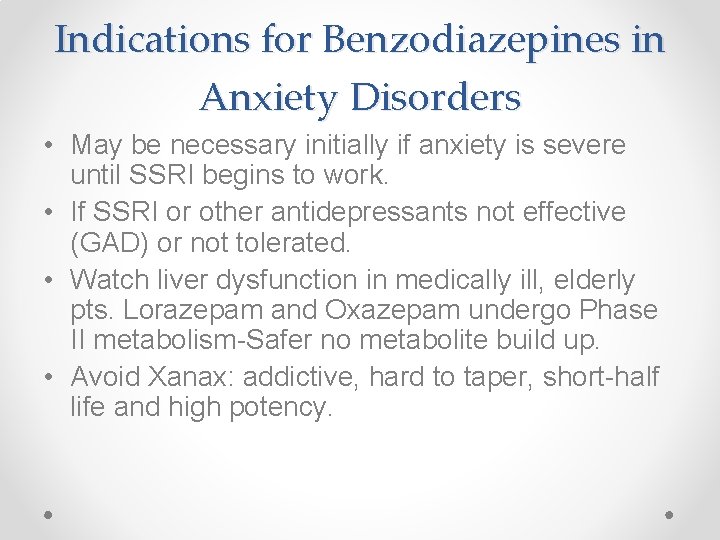
Indications for Benzodiazepines in Anxiety Disorders • May be necessary initially if anxiety is severe until SSRI begins to work. • If SSRI or other antidepressants not effective (GAD) or not tolerated. • Watch liver dysfunction in medically ill, elderly pts. Lorazepam and Oxazepam undergo Phase II metabolism-Safer no metabolite build up. • Avoid Xanax: addictive, hard to taper, short-half life and high potency.

Use of Benzodiazepines • Clonazepam 0. 5 -1. 0 mg works well for first weeks of SSRI therapy. Taper once pt adjusts and SSRI starts working. • Clonazepam, Ativan, Valium useful in panic and GAD but give scheduled and not PRN which reinforces symptoms. • Try to discontinue after 6 -9 months, based on symptoms. • Discontinuation: Relapse versus Rebound. Titrate down gradually to minimize.

Other anxiolytic agents Buspar • non-benzodiazepine, non-sedative, • Some anti-depressant effect. May be useful in Alcoholic and Sexual dysfunction pts. • Good for COPD improves respiratory function (Pa. CO 2) • SE profile like SSRIs. Nausea, HA, dizziness. (2 -4 weeks for effect) • 10 -30 mg tid, (use 15 mg tabs easier dosing)

Atypical Agents Mirtazapine • Antagonist at the 2 A inhibitory serotonin receptors resulting in release of SE/NE • Potent H 2 blocker, good for GI patients. • Increase sleep and weight gain are positives in elders • • • Bupropion Acts to increase dopamine/NE Least sexual dysfunction Contraindicated in patients with seizure disorder (why bulimia) Smoking cessation Treat SSRI induced sexual dysfunction

Lithium • First medication to be found effective in the treatment of BPAD. (acute and maintenance) • Not metabolized by the liver but excreted unchanged by kidney. • Lithium acts post-synaptically to inhibit secondary messengers (phosphatidylinositol phosphate (PIP). • Mildly pro-serotonergic and acts on G proteins. • Reduces mortality from Suicide. • May be neuroprotective.

COMMON Side Effects • • • Sedation Cognitive difficulties Tremor Decreased creativity Weight gain Polydipsia/polyuria Nausea Diarrhea Psoriasis/acne

LESS COMMON but More Serious • Cardiac: sick sinus syndrome. • Mild leukocytosis. • Ebstein’s anomaly if used in 1 st trimester of pregnancy. • Thyroid abnormalities: 5% of patients hypothyroid. • Li reduces thyroid’s sensitivity to TSH. • Effect on Kidney is longer term - reduces GFR slightly over 10 -20 years.

Toxicity • Generally non-toxic • Borderline toxicity: GI, tremor, ataxia, polyuria • Mild to moderate: dizzy, vomiting, confusion • Moderate to severe; delirium, EEG abnormal, cardiac, renal risk of coma • Severe : renal failure, seizures and death. • Therapeutic level is 0. 61. 2 • 1. 2 -1. 5 - mild • 1. 5 -2. 0 - moderate • 2. 0 -2. 5 - severe • Above 2. 5 HEMODIALYSIS

Valproate • Anticonvulsant used for petit and grand mal seizures. • Acts by increasing CNS GABA. • More effective than Li for rapid cycling, mixed episodes and substance abuse. • Therapeutic level of 50 -100 ug/ml • Highly protein bound. • 8 hr half life leads to bid/tid dosing. • For mania may use Depakote ER once daily • Can be used for acute agitation as well (more in delirium lecture)
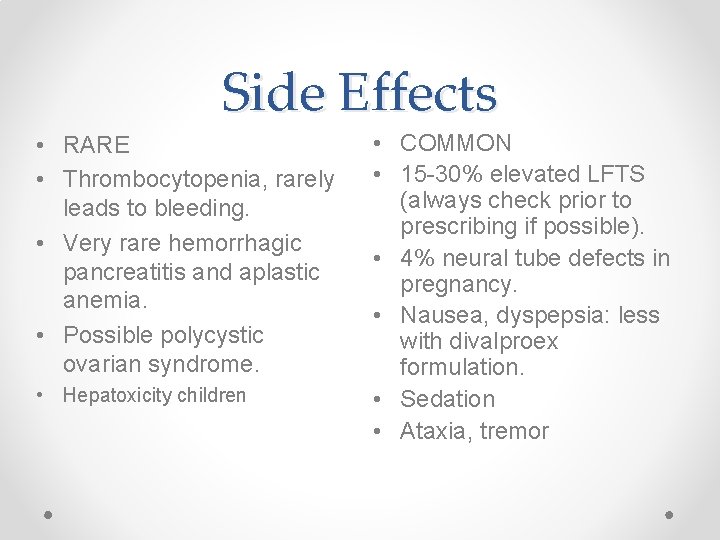
Side Effects • RARE • Thrombocytopenia, rarely leads to bleeding. • Very rare hemorrhagic pancreatitis and aplastic anemia. • Possible polycystic ovarian syndrome. • Hepatoxicity children • COMMON • 15 -30% elevated LFTS (always check prior to prescribing if possible). • 4% neural tube defects in pregnancy. • Nausea, dyspepsia: less with divalproex formulation. • Sedation • Ataxia, tremor
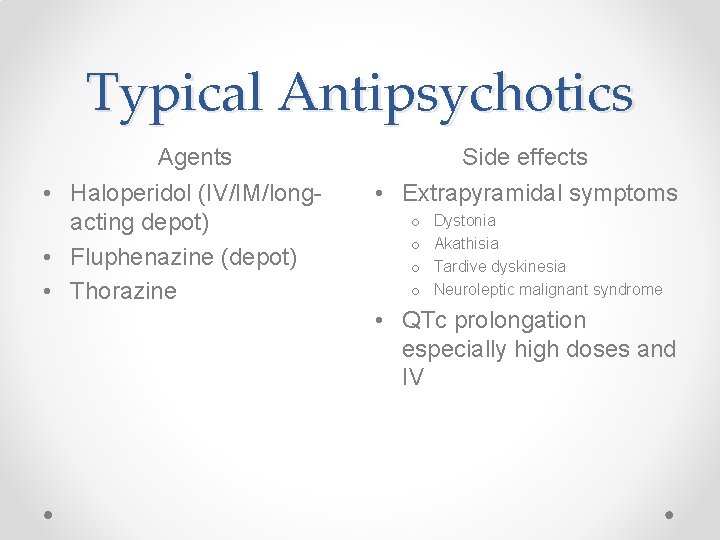
Typical Antipsychotics Agents • Haloperidol (IV/IM/longacting depot) • Fluphenazine (depot) • Thorazine Side effects • Extrapyramidal symptoms o o Dystonia Akathisia Tardive dyskinesia Neuroleptic malignant syndrome • QTc prolongation especially high doses and IV
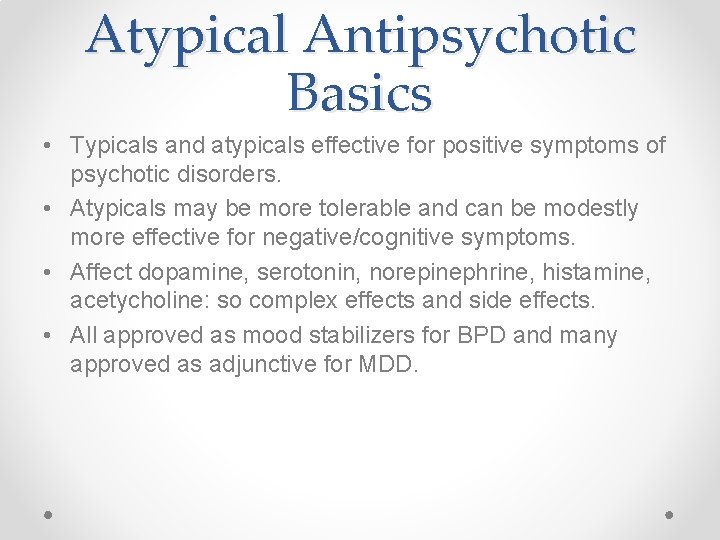
Atypical Antipsychotic Basics • Typicals and atypicals effective for positive symptoms of psychotic disorders. • Atypicals may be more tolerable and can be modestly more effective for negative/cognitive symptoms. • Affect dopamine, serotonin, norepinephrine, histamine, acetycholine: so complex effects and side effects. • All approved as mood stabilizers for BPD and many approved as adjunctive for MDD.
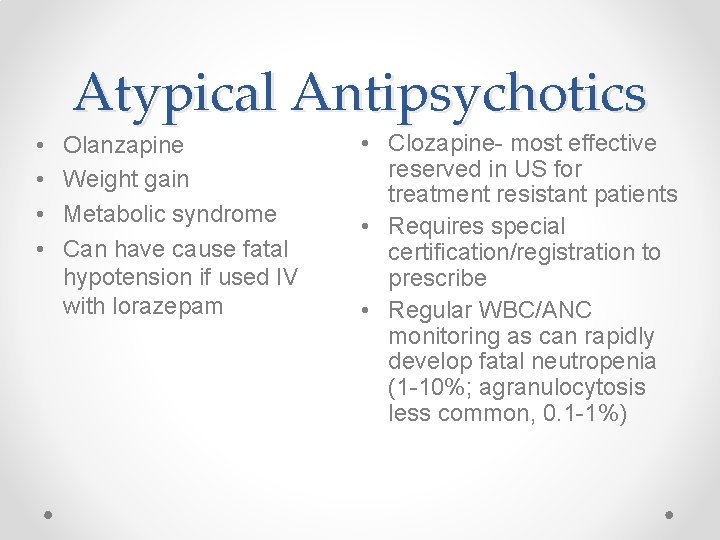
Atypical Antipsychotics • • Olanzapine Weight gain Metabolic syndrome Can have cause fatal hypotension if used IV with lorazepam • Clozapine- most effective reserved in US for treatment resistant patients • Requires special certification/registration to prescribe • Regular WBC/ANC monitoring as can rapidly develop fatal neutropenia (1 -10%; agranulocytosis less common, 0. 1 -1%)

Atypicals Continued Quetiapine: po Risperidone: po-IM-depot • Black box warning for Torsades: monitor QTc and other QTc prolonging drugs. • Good for depressionanxiety • Drug of choice in Parkinson’s-least EPS • At high doses same EPS risks as haldol • Can increase prolactin and cause sexual dysfunction • Medium weight and QTc side effects
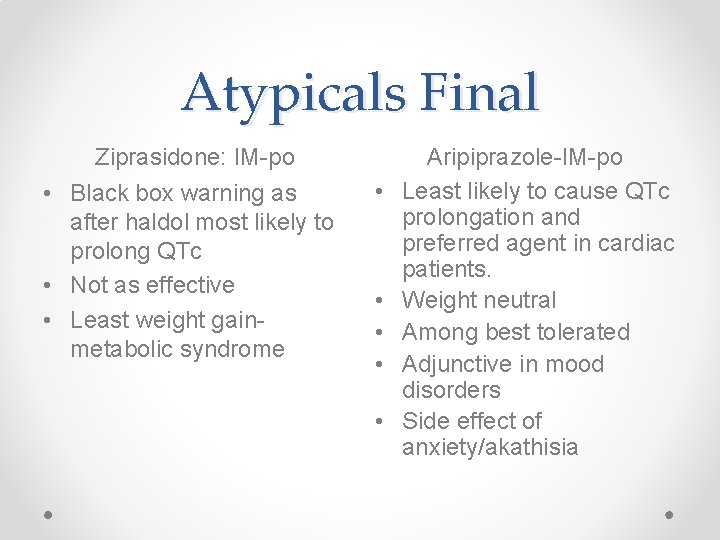
Atypicals Final Ziprasidone: IM-po • Black box warning as after haldol most likely to prolong QTc • Not as effective • Least weight gainmetabolic syndrome • • • Aripiprazole-IM-po Least likely to cause QTc prolongation and preferred agent in cardiac patients. Weight neutral Among best tolerated Adjunctive in mood disorders Side effect of anxiety/akathisia
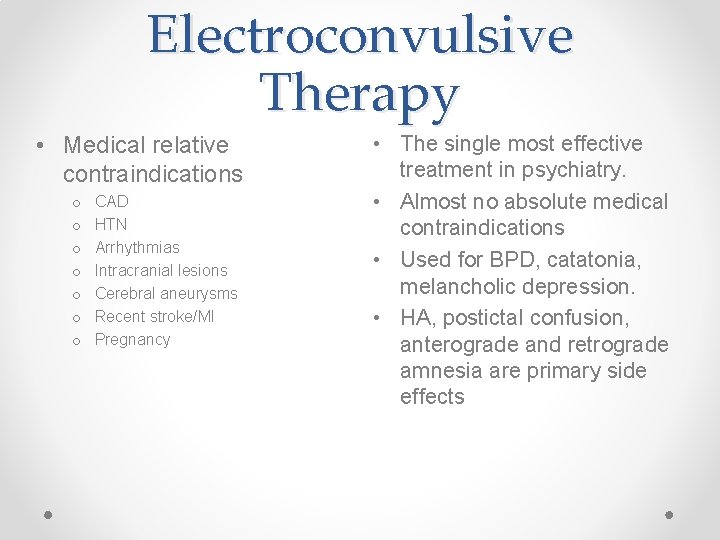
Electroconvulsive Therapy • Medical relative contraindications o o o o CAD HTN Arrhythmias Intracranial lesions Cerebral aneurysms Recent stroke/MI Pregnancy • The single most effective treatment in psychiatry. • Almost no absolute medical contraindications • Used for BPD, catatonia, melancholic depression. • HA, postictal confusion, anterograde and retrograde amnesia are primary side effects

5 -Minute Psychotherapy Primer Cognitive-Behavioral Therapy-CBT Feelings come from thoughts, change feelings Uses homework, challenging dysfunctional to changes thoughts Treatment of choice for OCD, anxiety, mild to moderate depression Dialectical Behavior Therapy-DBT Focused on mindfullness, emotional regulation, radical acceptance Specialized for borderline PD Motivational Interviewing technique to facilitate change Stages of changeprecontemplation, action, maintenance, relapse First used in addiction now used for a variety of health behaviors

Question/Case 1 • You have been treating a 22 -year old woman in your clinic for a first episode of major depression after her father died. She received bereavement counseling at her church. You started her on 20 mg of fluoxetine 4 months ago and increased the dose to 40 mg 2 months ago. The PHQ-9 shows her depression is nearly remitted. The patient does not like taking medications and requests to stop the antidepressant. Which of the following is the best advice to give her? a. Fluoxetine has a long half-life so she can safely stop the medication without tapering. Fluoxetine should be tapered down to 20 mg for 1 week and then stopped. Fluoxetine should be continued for at least 6 more months and then if the patient is still in remission, discontinued. * b. c. d. e. Because the patient had a diagnosis of major depression, fluoxetine should be continued for at least 2 years. Fluoxetine can be stopped as long as the patient continues in counseling.

• a. b. c. d. e. Question/Case 2 A 32 -year-old teacher presents to your outpatient clinic with symptoms of anhedonia, depressed mood of a month’s duration, weight loss and insomnia. She denies a prior history of depression. Family history is positive for substance use and mood disorders. Her sister has an anxiety disorder and has done well on escitalopram. Which of the following is the most important next step before prescribing the escitalopram? Refer the patient for psychotherapy Check thyroid function Screen for substance use disorders See what is on the formulary Ask about a history of hypomanic or manic symptoms*
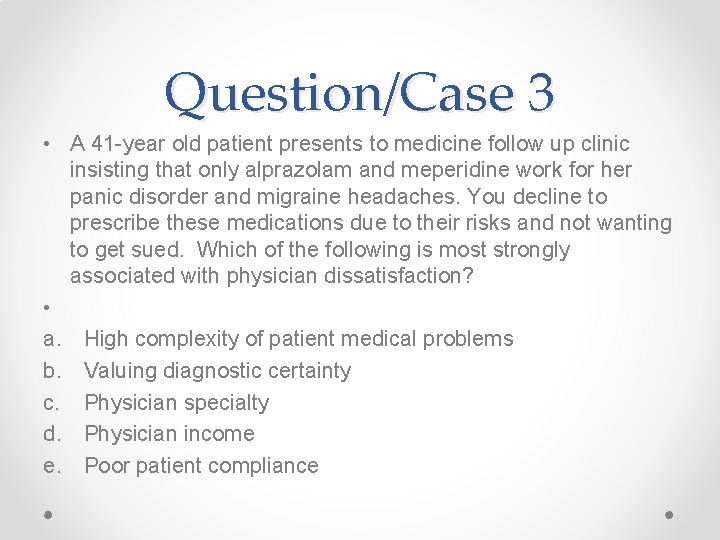
Question/Case 3 • A 41 -year old patient presents to medicine follow up clinic insisting that only alprazolam and meperidine work for her panic disorder and migraine headaches. You decline to prescribe these medications due to their risks and not wanting to get sued. Which of the following is most strongly associated with physician dissatisfaction? • a. High complexity of patient medical problems b. Valuing diagnostic certainty c. Physician specialty d. Physician income e. Poor patient compliance
- Slides: 61