Everything you must know about shared decision making
Everything you must know about shared decision making Prof. dr. Ellen Smets Medical Psychology Academic Medical Centre/University of Amsterdam
Disclaimer Everything you must know about shared decision making ≠ everything ≠ must
AIM To provide you with balanced information, allowing you to make a well considered decision whether you deem SDM valuable for the care of cancer patients
Disclaimer Everything you must know about shared decision making ≠ everything ≠ must ≠ neutral
Program Background SDM Own research Training Practice
Shared Decision Making
Shared decison making Is not that the patient has to make the decision Take Home Is providing good care to prevent that patients receive a treatment they do not wish or which causes more harm than benefit for this individual patient.
Context Nowedays many treatment options to chose from Unwanted practice variation Patiënts increasingly autonomous Focus on self-management Physicians’ decisions are expected to incorporate patients’ values and needs

Definition Shared decision making is a conversation between physician and patient in which they mutally exchange information and considerations to reach a treatment decision that best fits this unique patient
When SDM? There is more than one reasonable approach available to manage the patient's situation Those approaches differ in ways that matter to patients Scientific uncertainty No evidence – no guideline No (continuation of) treatment is also an option
Profesional needs to be Role professional Up to date with available options and their (dis)advantages Provide understandable information Guide patients in reaching a decision
Shared decision making: When? / what might you gain? When not? / What might withold you? What would you need for SDM?
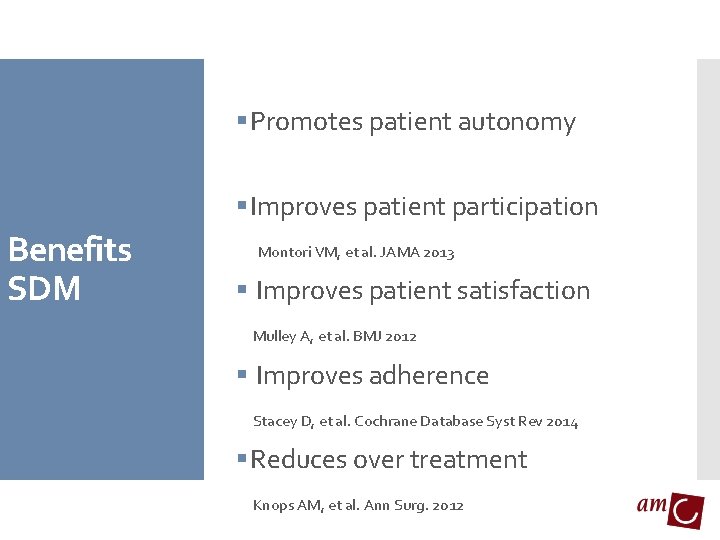
§ Promotes patient autonomy § Improves patient participation Benefits SDM Montori VM, et al. JAMA 2013 § Improves patient satisfaction Mulley A, et al. BMJ 2012 § Improves adherence Stacey D, et al. Cochrane Database Syst Rev 2014 § Reduces over treatment Knops AM, et al. Ann Surg. 2012
Do patients want and need to participate in decision making? Are they able to? Harm SDM Particularly in case of serious, life theatening conditions Vulnerable and insecure At odds with autonomy Fear of making the ‘wrong’ decison can be burdensome Consultations will last longer

Research
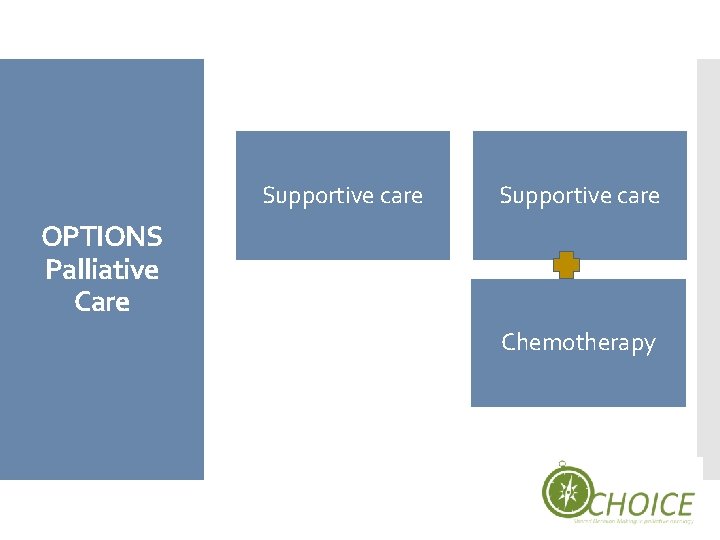
Supportive care OPTIONS Palliative Care Chemotherapy

Randomized Control Trial
Primary outcome: observed SDM Secondary outcomes: patient anxiety, hope, quality of life, satisfaction, trust, perceived efficacy, preferred role in decision making, attitude towards quantity/quality, oncologist satisfaction, observed communication on End of life, consultation duration, decision made.
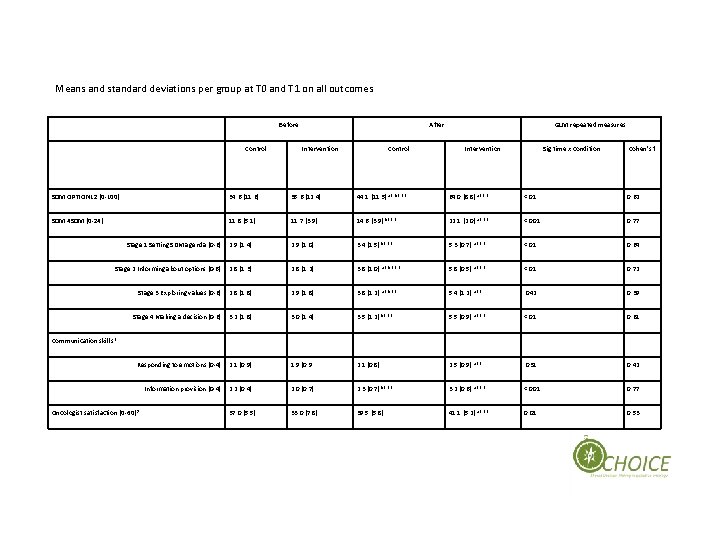
Means and standard deviations per group at T 0 and T 1 on all outcomes Before Control After Intervention Control GLM repeated measures Intervention Sig time x condition Cohen’s f SDM OPTION 12 (0 -100) 34. 6 (11. 6) 35. 6 (12. 4) 44. 1 (11. 5) a* b*** 64. 0 (8. 8) a*** <. 01 0. 62 SDM 4 SDM (0 -24) 11. 8 (5. 1) 11. 7 (3. 9) 14. 6 (3. 9) b*** 22. 1 (2. 0) a*** <. 001 0. 77 2. 9 (1. 4) 2. 9 (1. 0) 3. 4 (1. 5) b*** 5. 3 (0. 7) a*** <. 01 0. 64 Stage 2 Informing about options (0 -6) 2. 8 (1. 3) 2. 8 (1. 2) 3. 8 (1. 0) a* b*** 5. 8 (0. 5) a*** <. 01 0. 72 Stage 3 Exploring values (0 -6) 2. 8 (1. 8) 2. 9 (1. 8) 3. 8 (1. 2) a* b** 5. 4 (1. 2) a** . 042 0. 39 Stage 4 Making a decision (0 -6) 3. 2 (1. 8) 3. 0 (1. 4) 3. 5 (1. 2) b*** 5. 5 (0. 9) a*** <. 01 0. 61 Responding to emotions (0 -4) 2. 1 (0. 9) 1. 9 (0. 9 2. 1 (0. 8) 2. 5 (0. 9) a** . 031 0. 42 Information provision (0 -4) 2. 2 (0. 4) 2. 0 (0. 7) 2. 3 (0. 7) b*** 3. 2 (0. 6) a*** <. 001 0. 77 37. 0 (5. 5) 33. 0 (7. 8) 39. 5 (5. 8) 41. 1 (5. 2) a*** 0. 01 0. 53 Stage 1 Setting SDM agenda (0 -6) First results Communication skills 1 Oncologist satisfaction (0 -60) 2
The independent and combined effect of 2 interventions on Shared Decision Making is tested in a multi center Randomized Control Trial (RCT): - A Patient Communication Aid (PCA), including a Question Prompt Sheet (QPS) and Value Clarification Exercise (VCE) for patients - A communication training for oncologists on SDM in palliative oncology, consisting of a reader, theory, role playing games with simulated patients, personal feedback and a movie designed for the purpose of the training.

TRAINING
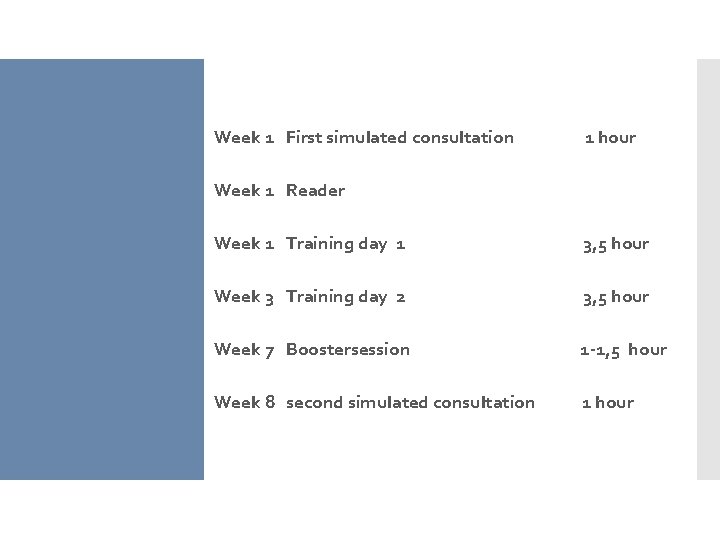
Week 1 First simulated consultation 1 hour Week 1 Reader Week 1 Training day 1 3, 5 hour Week 3 Training day 2 3, 5 hour Week 7 Boostersession 1 -1, 5 hour Week 8 second simulated consultation 1 hour
A women of xx with metastased inoperable cancer visits you the day after the diagnosis. The median Case survival time without treatment is 1 year. She is eligible for chemotherapy treatment which might relieve her tumor related complaints and which offers a median survival of xx months. The to be expected side-effects of the chemotherapy are xx.
Steps 1) The professional informs the patient that a decision is to be made and that the patient’s opinion is important; 2) The professional explains the options and the pros and cons of each option 3) The professional and patient discuss the patients’ preferences; the professional supports deliberation. 4) The professional and patient discuss patients’ decisional role preference, make or defer the decision and discuss possible follow-up. Stiggelbout et al. PEC 2015
Creating choice awareness Step 1 § a decison needs to be made, there are two options § There is no best option, your considerations and preferences are decisive
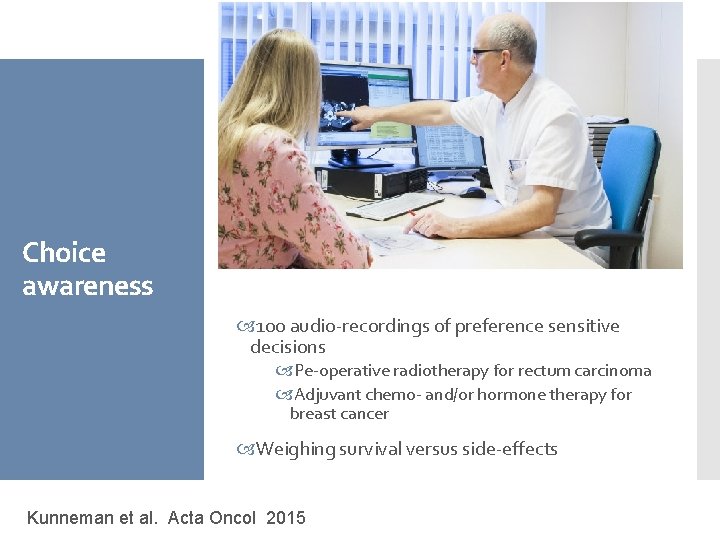
Choice awareness 100 audio-recordings of preference sensitive decisions Pe-operative radiotherapy for rectum carcinoma Adjuvant chemo- and/or hormone therapy for breast cancer Weighing survival versus side-effects Kunneman et al. Acta Oncol 2015
In only 3 of the 100 consultations a decision was explicitly mentioned Kunneman et al. Acta Oncol 2015
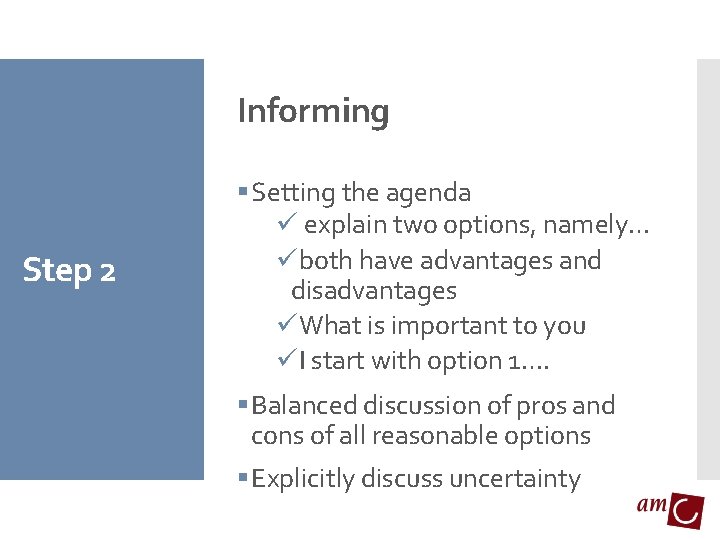
Informing Step 2 § Setting the agenda ü explain two options, namely… üboth have advantages and disadvantages üWhat is important to you üI start with option 1…. § Balanced discussion of pros and cons of all reasonable options § Explicitly discuss uncertainty
Advantages Voor- en nadelen Disadvantages
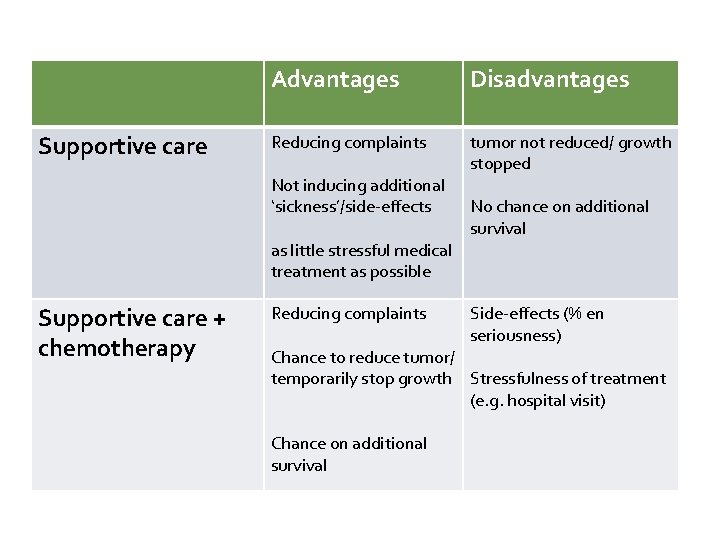
Supportive care Advantages Disadvantages Reducing complaints tumor not reduced/ growth stopped Not inducing additional ‘sickness’/side-effects Voor- en nadelen Supportive care + chemotherapy as little stressful medical treatment as possible Reducing complaints No chance on additional survival Side-effects (% en seriousness) Chance to reduce tumor/ temporarily stop growth Stressfulness of treatment (e. g. hospital visit) Chance on additional survival
Deliberation § Actively asking questions to stimulate patients’ deliberation Step 3. § Pitfall: waiting passively what patient will decide after having provided information

Listen Summarise Ask for clarification Use reflections
Deciding Step 4 Find out treatment preference ‘What is your incliniation at this point? ’ Find out decisional preference ‘Are we going to decide now and are you willing to make the decision? ’ A decision can be reconsidered If desired, you may advise taking considerations of patient into account If desired, decision can de deferred
Deciding Step 4 Find out treatment preference ‘What is your incliniation at this point? ’ Find out decisional preference ‘Are we going to decide now and are you willing to make the decision? ’ • Closure: summary ‘So we decide to x, because you expressed that {considerations patient}’

Let’s practice
- Slides: 37