Evaluation of Heat Illness Physiology of Temperature Regulation

- Slides: 49
Evaluation of Heat Illness
Physiology of Temperature Regulation • Hypothalamus – Center for thermal regulation – integrates input from thermal receptors – Sends autonomic impulses to increase vasodilation / vasoconstriction to periphery and cause sweating / shivering
Body Temperature • Determined by balance between heat production (BMR, muscular activity) and heat loss • Environmental conditions can make 98. 6° difficult to maintain
Mechanisms to Promote Heat Loss • • Conduction Convection Evaporation Radiation S = M +/- R +/- K +/- Cv - E
Assumptions • Convection, and radiation are very effective when external temp is lower than 87° • If external temp is higher than body temp, heat transfer is reversed • Evaporation becomes primary method • The more humidity, the less effective evaporation becomes. (Big decrease when >60%).
Sweat Rates • Up to 2 liters per hour • 2% body weight impairs performance • Thirst not a good indicator of hydration status • 1 L of sweat = 1. 25 L ingested beverage • < 50% of fluid lost is typically replaced
Electrolyte Losses • Na+, Cl-, K+, Mg+ • Na – main one – muscle cramps • Typical American diet replaces most electrolytes
Heat Exposure Syndromes • Traditional – Heat Cramps – Heat Exhaustion – Heat Stroke • New Classifications – Heat Syncope – Exertional Hyponatremia
Heat Cramps • Water loss vs Electrolyte loss? • Athletes most at risk have a Hx • Extremities & abdominals
Rx for Heat Cramps • Fluid replacement w/ Na • Gentle Stretching and Massage • Lie Down to increase blood flow to the legs • Ice
Heat Syncope • AKA “Orthostatic Dizziness” • Caused by peripheral vasodilation, postural pooling of blood, decreased venous return and Q • 1 st 5 days before acclimatized
Heat Syncope Recognition • Brief episode of dizziness associated with tunnel vision, pale or sweaty skin, decreased pulse • Normal Temp (97 -104°)
Heat Exhaustion • AKA “Heat Prostration” • Caused by inadequate CV response – brain vs skin vs muscles – Dehydration decreases blood volume
Heat Syncope Rx • • Shade Monitor Vitals Elevate Legs Rehydrate
Signs and Symptoms of Heat Exhaustion • • • Hypovolemic Shock Sx vary in severity and number Weakness, fatigue, dizziness, headache, loss of appetite, nausea, pallor, profuse sweating, vomiting, urge to defecate, syncope, thirsty, irritable Can be difficult to distinguish from Heat Stroke w/ out rectal temp Body Core Temp ranges from 97 -104° Assess cognitive skills to rule more serious conditions
Rx for Heat Exhaustion • Rest in Cool • Fluid Replacement – Ingesting – IV • Electrolyte Replacement • Supine Posture • Remove excessive clothing • Cold Buckets / Fans
Heat Stroke • Body’s cooling mechanisms have failed leading to hyperpyrexia (body temp > 104°) • Anhidrosis – body stops sweating • Causes damage to CNS and internal organs • May develop suddenly or progress from heat exhaustion • Medical Emergency
Signs and Symptoms of Heat Stroke • • • Hot, dry skin Decreasing BP Rapid, full pulse becomes rapid, weak • Vomiting, diarrhea, seizures, coma • Poor cognitive function • Multiple organ failure
Conditions Resulting from Heat Stroke • Lactic Acidosis • Hyperkalemia (excessive K+) • Renal Failure • Disseminated Intervascular Coagulaton
Rx for Heat Stroke • Cooling immediately – immerse in cold bath (35 -59 degrees) to reduce body temp to < 100° – Remove from pool when body temp reaches 101° • Use wet towels /ice bags and fanning in transport to hospital • Treat for shock
Exertional Hyponatremia • • • Rare? Low serum-Na level (< 130 mmol/L) Ingest too much water vs ingest too little Na? • Sx – disorientation, headache, vomiting, lethargy, swelling of extremities, pulmonary and cerebral edema, seizures • Results in death if not treated by rehydrating w/ fluids w/ Na
Reducing Risk of Heat Illness • Pre-participation Physical / Screening • Early Recognition of Sx • Conditioning • Acclimatization – 4– 7 days vs 10 -14 days vs months? – After 6 weeks able to produce 2. 5 x normal amount of sweat – Diminishes by day 6 of inactivity
Reducing Risk (con’t) • Educate players and coaches • Diet – extra Na+ • Rest and Digest • Monitor urine color and amount • Weigh in and out • Clothing / Equipment modifications
Reducing Risk (con’t) • Stay well hydrated (NATA Position Statement: Fluid Replacement ) – Pre: 17 -20 oz, 2 -3 hours before and 7 -10 oz. – 20 min before – During: 7 -10 oz every 20 min – Replace lost fluid
Reducing Risk (con’t) – Beverage Temp 50 -59° – Beverage Choice • Water • 6 -8% CHO solution if longer than 45 mins • No Caffeine, alcohol • . 3 -. 7 g/L Salt (esp 1 st 3 -5 days)
Reducing Risk (con’t) • • Fans Shade Cold buckets Cold Tub Thermometer BP Cuff Telephone
Predisposing Medical Conditions for Heat Illness • Sickle Cell Trait – carry less O 2 • Cystic Fibrosis Trait – increases salt loss in sweat • Arteriosclerotic Vascular Disease – thicker arterial walls decrease blood flow • Scleroderma – skin disorder that increases sweating
Predisposing Medical Conditions for Heat Illness • Drug / Supplement Use – Ephedra – Diuretics – Antidepressants decrease sweating – Beta blockers reduce skin blood flow – Antihistamines constrict blood vessels. (con’t)

Recommendations
National Weather Service Recommendations • Cease activity when Heat index is over 105° • Heat index only includes temperature and humidity
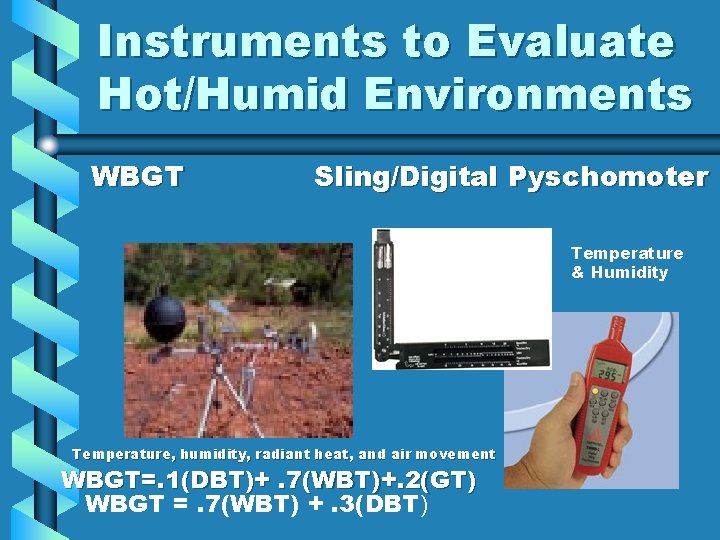
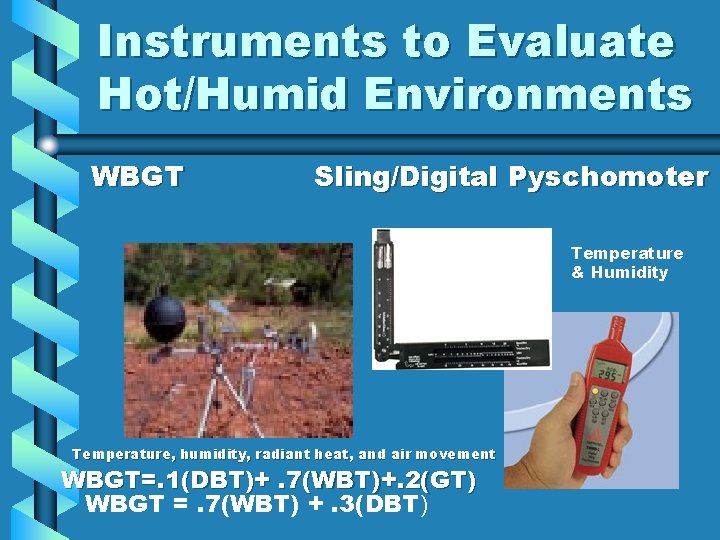
Instruments to Evaluate Hot/Humid Environments WBGT Sling/Digital Pyschomoter Temperature & Humidity Temperature, humidity, radiant heat, and air movement WBGT=. 1(DBT)+. 7(WBT)+. 2(GT) WBGT =. 7(WBT) +. 3(DBT)
Event and Practice Guidelines Arnheim & Prentice, 1993 – Watch the Obese • 80 -90 degrees & < 70% humidity – Take a 10 min rest every hour, change t-shirts when wet, watch all athletes • 80 -90 degrees and > 70% or 90 -100 degrees and < 70% – Suspend practice • > 100 degrees or > 90 degrees & humidity over 70% WBGT > 90 No training, skull sessions
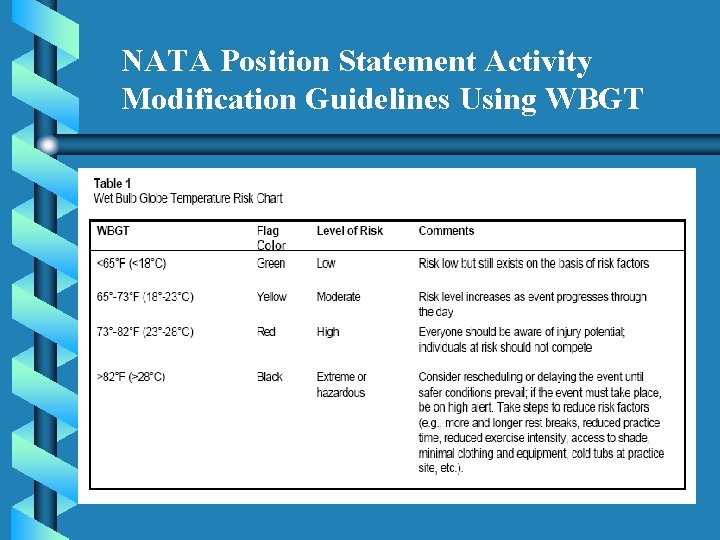
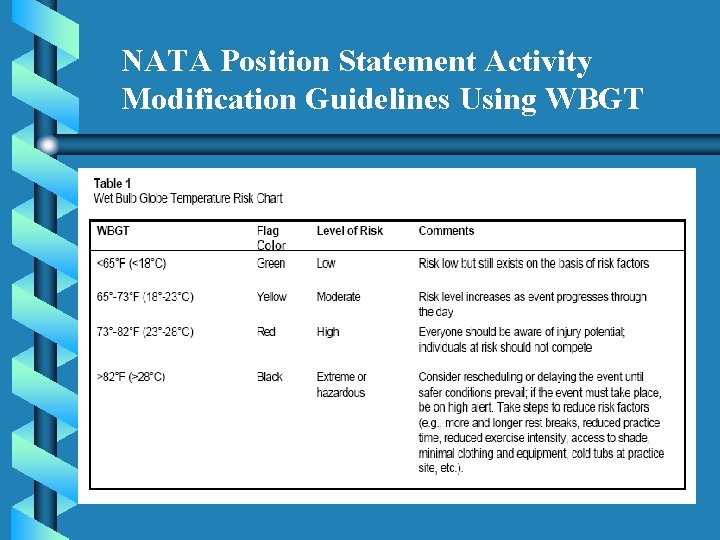
NATA Position Statement Activity Modification Guidelines Using WBGT
Event and Practice Guidelines (NATA Position Statement: Exertional Heat, 2002) • Wet Bulb Globe Temperature – WBGT > 82, reschedule, if possible Even in the South? We’d never practice!
Disclaimer • “Certified athletic trainers work in a variety of professional and geographic settings…. . obviously the ATC in Florida will adapt the recommendations to his or her environment, while the ATC in Maine will make different adjustments. ” - Casa • “Athletic trainers should recognize that temperature ranges might vary widely based upon geographic regions. Athletic trainers may practice in regions, such as the southeastern United States, where the WBGT is routinely in the high or extreme or hazardous level of risk throughout a significant part of the year. In these regions, while it may not be practical to reschedule or delay events, the athletic trainer must recognize that the level of risk is high and take appropriate steps to reduce risk. ” – NATA
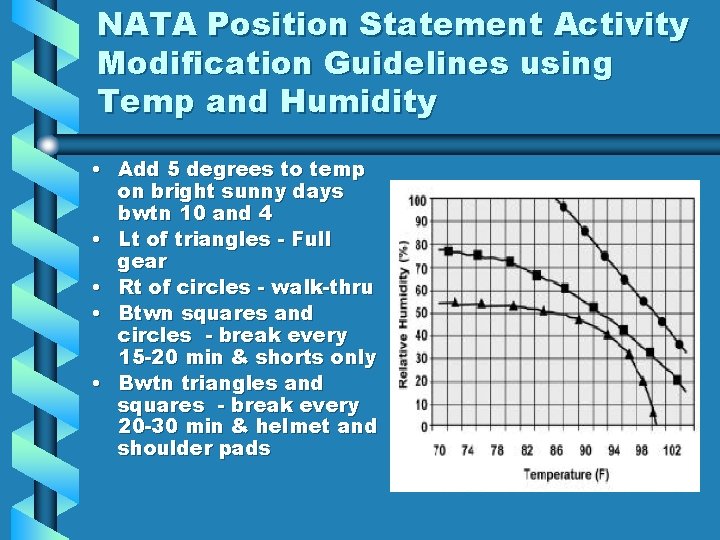
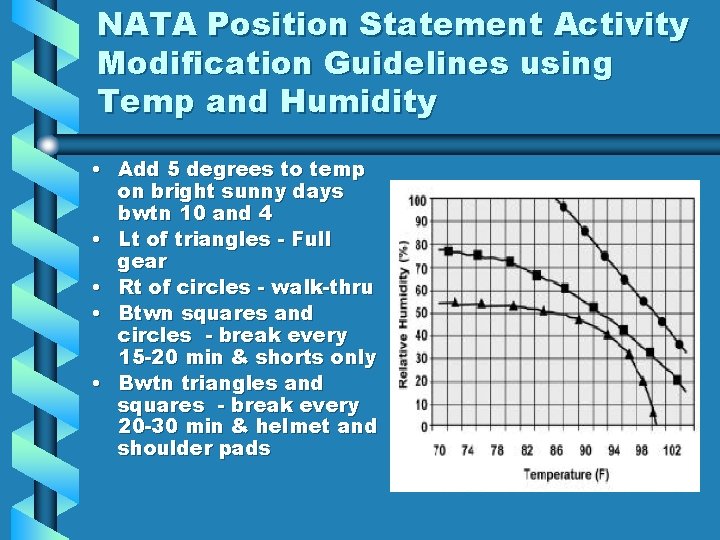
NATA Position Statement Activity Modification Guidelines using Temp and Humidity • Add 5 degrees to temp on bright sunny days bwtn 10 and 4 • Lt of triangles - Full gear • Rt of circles - walk-thru • Btwn squares and circles - break every 15 -20 min & shorts only • Bwtn triangles and squares - break every 20 -30 min & helmet and shoulder pads
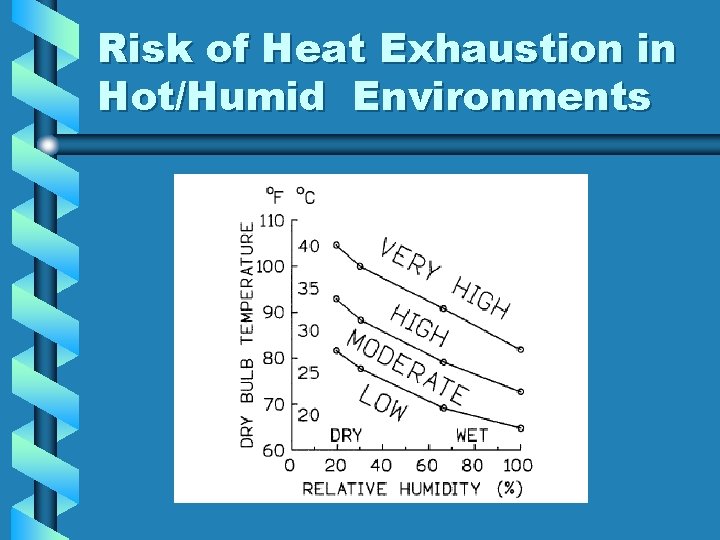
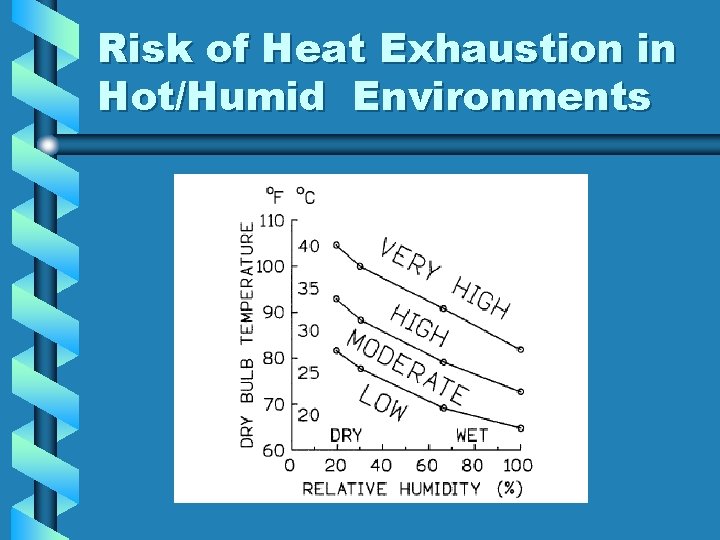
Risk of Heat Exhaustion in Hot/Humid Environments
Take a look at the Inter. Association Task Force Heat Illness Consensus Statement
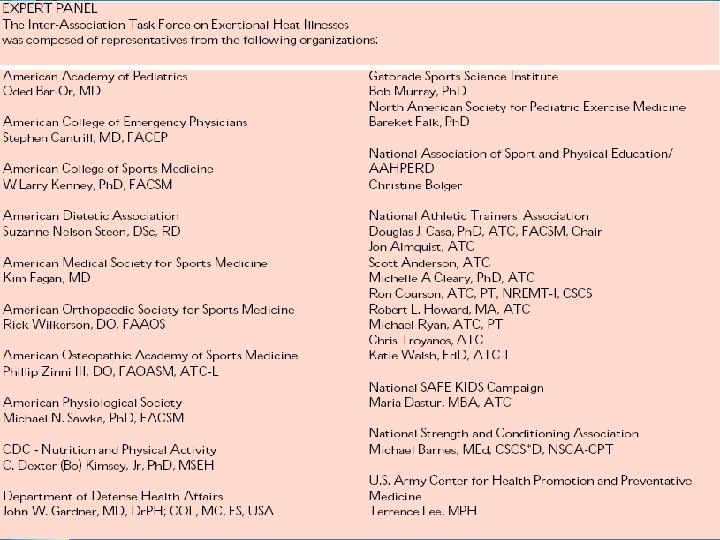
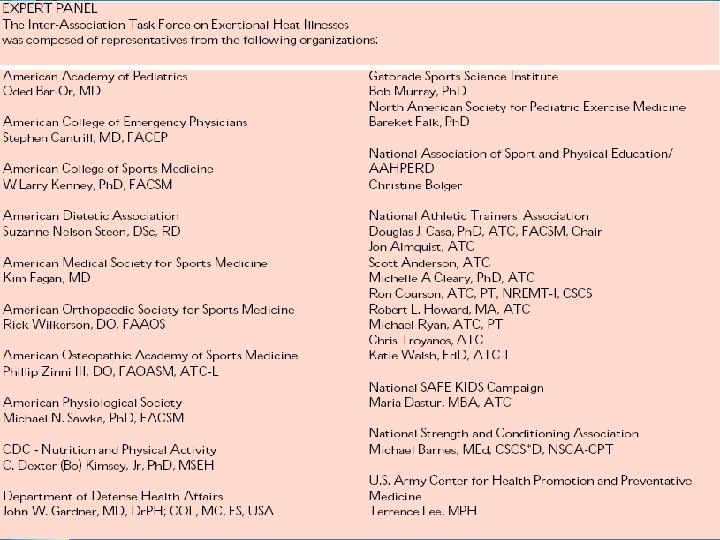
Inter-Association Task Force on Exertional Heat Illnesses Consensus Statement (June 2004) These guidelines were established to increase safety and performance for individuals engaged in physical activity, especially in warm and hot environments. The risks associated with exercise in the heat are well documented, but policies and procedures often do not reflect current state-of-the-art knowledge. Many cases of exertional heat illness are preventable and can be successfully treated if onsite personnel identify the condition and implement appropriate care in a timely manner. Strategies to optimize proper care of dehydration, exertional heat stroke (EHS), heat exhaustion, heat cramps and exertional hyponatremia are presented here. This consensus statement was developed by medical / scientific experts experienced in the prevention, recognition and treatment of exertional heat illnesses.
Return to Play Criteria for Dehydration • A nauseated or vomiting athlete should seek medical attention to replace fluids via an intravenous line. • Return-to-Play Considerations – If the degree of dehydration is minor and the athlete is symptom free, continued participation is acceptable. The athlete must maintain hydration status and should receive periodic checks from onsite medical personnel.
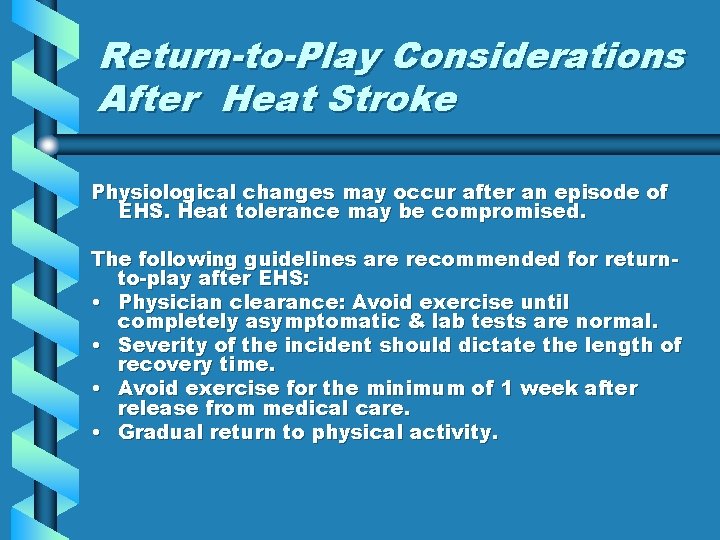
Return-to-Play Considerations After Heat Stroke Physiological changes may occur after an episode of EHS. Heat tolerance may be compromised. The following guidelines are recommended for returnto-play after EHS: • Physician clearance: Avoid exercise until completely asymptomatic & lab tests are normal. • Severity of the incident should dictate the length of recovery time. • Avoid exercise for the minimum of 1 week after release from medical care. • Gradual return to physical activity.
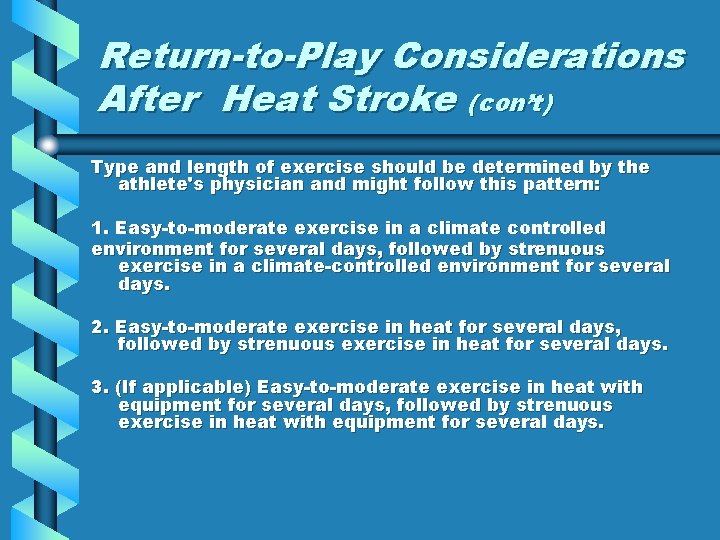
Return-to-Play Considerations After Heat Stroke (con’t) Type and length of exercise should be determined by the athlete's physician and might follow this pattern: 1. Easy-to-moderate exercise in a climate controlled environment for several days, followed by strenuous exercise in a climate-controlled environment for several days. 2. Easy-to-moderate exercise in heat for several days, followed by strenuous exercise in heat for several days. 3. (If applicable) Easy-to-moderate exercise in heat with equipment for several days, followed by strenuous exercise in heat with equipment for several days.
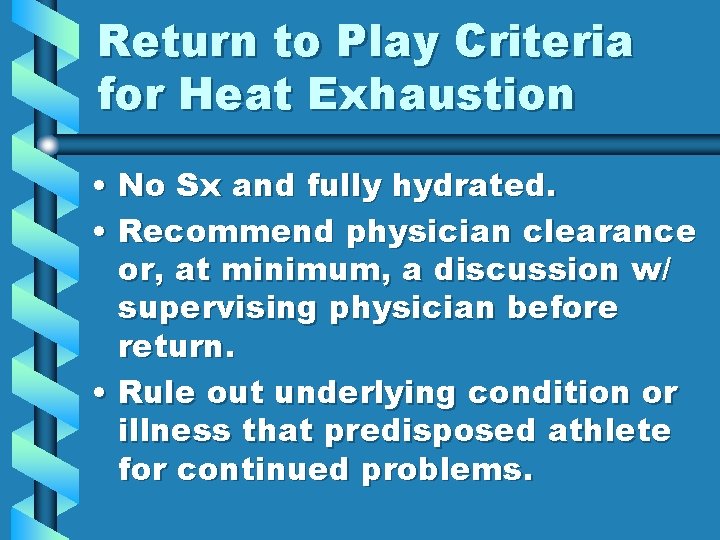
Return to Play Criteria for Heat Exhaustion • No Sx and fully hydrated. • Recommend physician clearance or, at minimum, a discussion w/ supervising physician before return. • Rule out underlying condition or illness that predisposed athlete for continued problems.
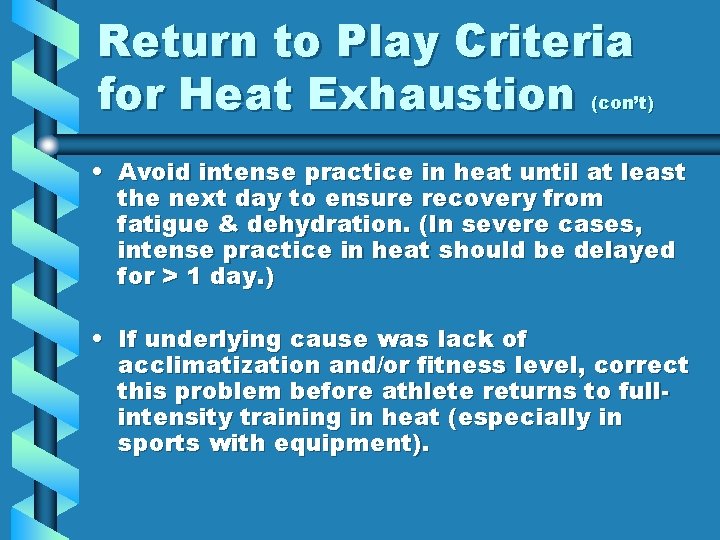
Return to Play Criteria for Heat Exhaustion (con’t) • Avoid intense practice in heat until at least the next day to ensure recovery from fatigue & dehydration. (In severe cases, intense practice in heat should be delayed for > 1 day. ) • If underlying cause was lack of acclimatization and/or fitness level, correct this problem before athlete returns to fullintensity training in heat (especially in sports with equipment).
Return to Play Guidelines for Heat Cramps • Perform at the level needed for successful participation? • Review – – – Diet Rehydration practices Electrolyte consumption Fitness status Level of acclimatization Use of dietary supplements
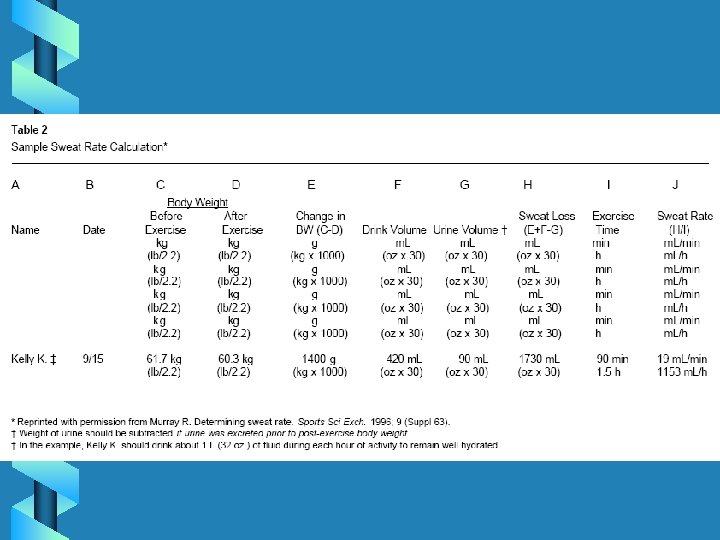
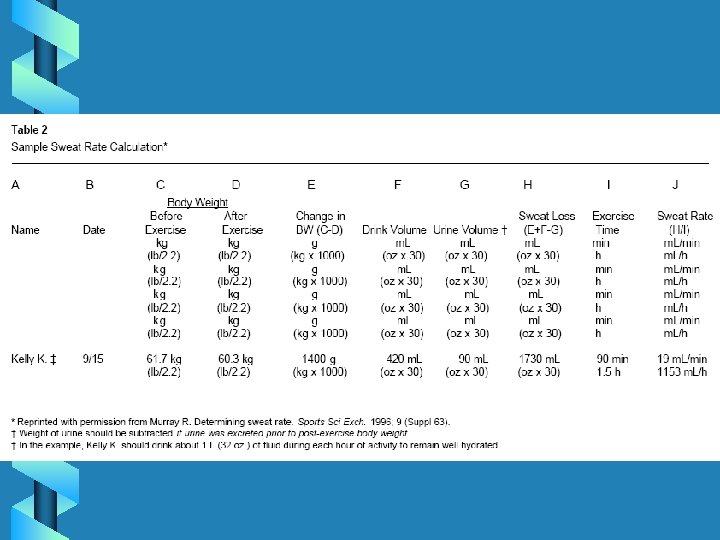
Return to Play Criteria for Exertional Hyponatriema • Physician clearance • Mild cases, activity can resume a few days after completing an educational session on establishing an individualspecific hydration protocol – ensures proper amount and type of beverages and meals are consumed before, during and after physical activity (see Table 2).
References • Arnheim D. D. & Prentice W. E. (1993). Principles of Athletic Training. (8 th ed. ) St. Louis: Mosby-Year Book. • American Academy of Orthopaedic Surgeons. (1999). Athletic Training and Sports Medicine. (3 rd ed. ) • Binkley HM, Beckett, Casa DJ, Kleiner DM, Plummer PE. (2002). National Athletic Trainers’ Association Position Statement: exertional heat illness. Journal of Athletic Training, 37(3): 329343. • Casa DJ, Armstrong LE, Hillman SK, Montain SJ, Reiff RV, Rich BS, Roberts WO, Stone JA. (2000). National Athletic Trainers’ Association Position Statement: fluid replacement for athletes. Journal of Athletic Training, 35(2): 212 -224. • Inter-Association Task Force on Exertional Heat Illness Consensus Statement (2004). www. nata. org