EVALUATION OF CAPACITY TO MAKE HEALTHCARE DECISIONS GREGORY
- Slides: 48
EVALUATION OF CAPACITY TO MAKE HEALTHCARE DECISIONS GREGORY COWAN PH. D. UW WAUSAU FAMILY MEDICINE
I HAVE NO RELEVANT COMMERCIAL INTERESTS TO DISCLOSE
Outline o Guiding principles o Competency vs Capacity o Performing the evaluation
Ethical Principles �Autonomy (the right to participate in your own treatment) �Beneficence (doing good) �Nonmaleficence (do no harm) Patient autonomy is balanced against patient’s best interest
Competency and Capacity o Competency- a legal term-a determination made by a court o Capacity- a clinical term- basis of legal finding regarding competence o Abilities- specific behavioral aspects of capacities
Competency o “A legal term referring to individuals having sufficient ability…natural or legal qualifications to engage in a given endeavor” (Leo, 1999)
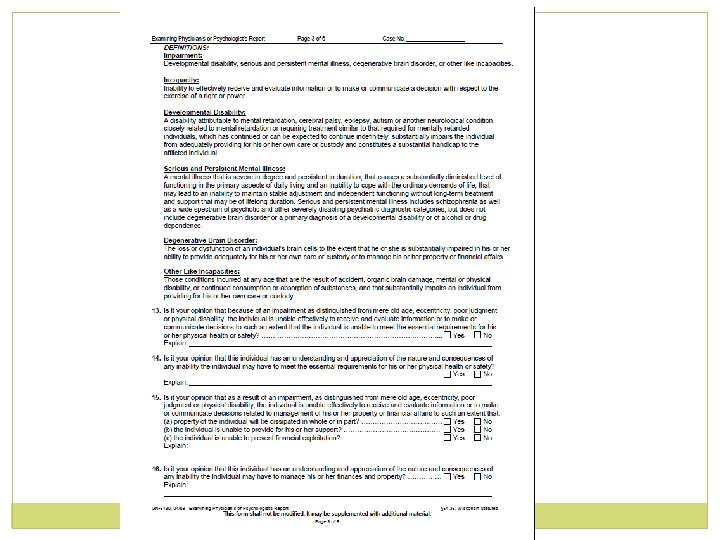
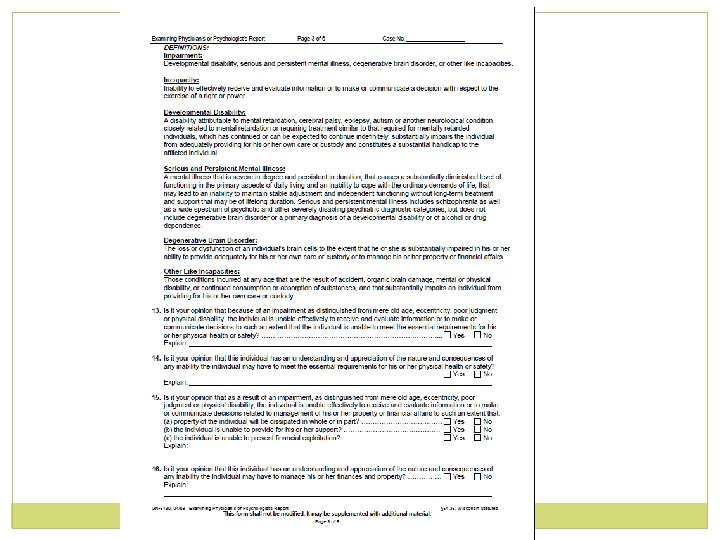
Capacity o “Incapacity: Inability to effectively receive and evaluate information or to make or communicate a decision with respect to the exercise of a right or power” (54. 36, Wisconsin statutes)
�“Incompetence is defined by one’s functional deficits, which are judged to be sufficiently great the person cannot meet the demands of a specific decision-making situation, weighed in light of its potential consequences” (Resnick, 2006)
Examples of Competence �Handle finances �Prepare a will �Stand trial �Make medical decisions
Parameters used in evaluating competence o 1. Person’s understanding of info presented o 2. Rational vs irrational manipulation of this information
o 3. Their understanding of how that info applies to them (do they understand risks and benefits, alternatives to proposed treatment) o 4. Ability to express a consistent choice
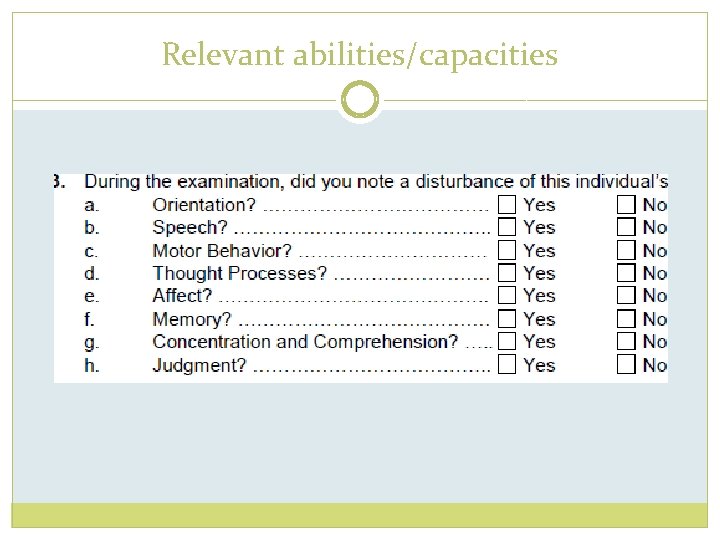
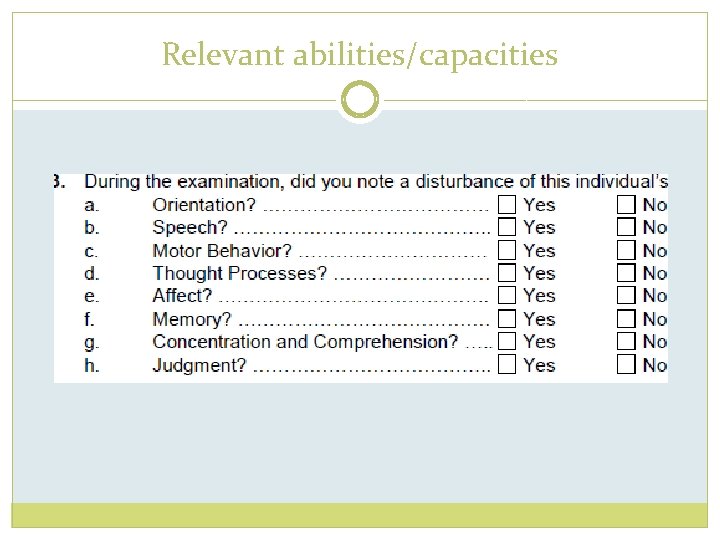
Relevant abilities/capacities
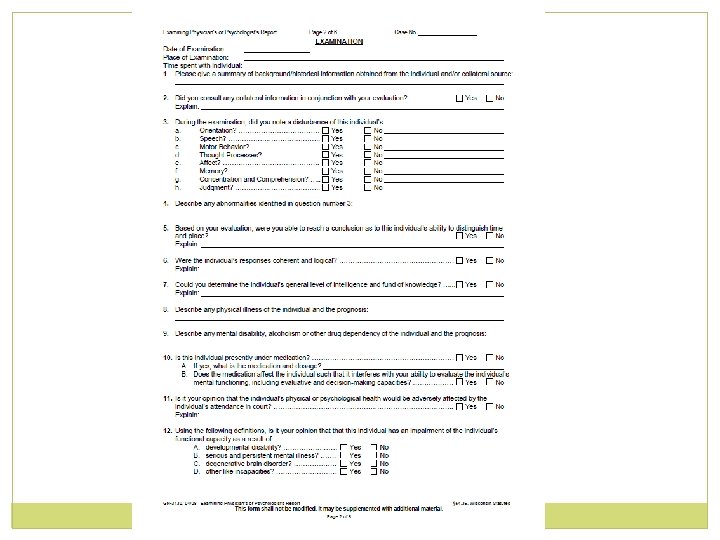
Orientation o Place (“What is the name of this place? ” “What kind of place is it? ”) o Time (“What year is it? . . . month? …day? ”) o Person (“What is your full name? ” “Who is the person in the chair? ”)
Speech �Rate, tone, productivity �Pressure of speech? �Speech content appropriate? �Tangential, circumstantial?
Motor Behavior Restless? activity? Agitated? Lethargic? unusual motor level of consciousness- stuporous, alert, drowsy, distracted, variable Sleep, appetite
Thought Processes o “Why are you in the hospital/clinic? ” o “What kind of medical problem do you have? ” o “What kind of treatment do you think you need? ” o “What will happen to you if you do/don’t receive treatment? ”
Thought Processes o Do they comprehend speech? o Hallucinating, delusional, or Hx of such
o Poverty of thought? Difficulty finding words? o Flight of ideas? Loose associations?
o Abstract thinking o o Proverb interpretation (“grass always greener”, “can’t judge a book”, etc. ) Similarities (How are red and green/dog and lion/north and west… alike? ”) o Fund of information
Mood and Affect o Euthymic- normal o Depressed, anxious o Expansive- lack of restraint in expressing feelings
o Elevated- euphoria o Irritable o Suicidal/homicidal thoughts/intent/plan
o Restricted/blunted/constricted- limited range or intensity of emotional expression o Flat- near absence of emotional expression
o Labile- rapidly changing expression of emotion o Inappropriate (inconsistent with speech or thought)
Memory o Recent memoryo “How long have you been here? ” “How did you get here? ” o “Have you eaten anything today? ” “What did you have for dinner last night? ”
o Immediate memory- 3 words, ask to repeat, then ask to name them 5 minutes later o Remote memory- What year did you get married/graduate from high school
Concentration/Attention o Digit span o Serial sevens, threes o Simple arithmetic o Ability to track conversation
Judgment o Information from record review and family are very important here- recent or repeated lapses of judgment? Financial, safety risks? o “What should you do if a pan of grease catches fire on the stove? ” … “if your neighbor’s house catches fire? ”
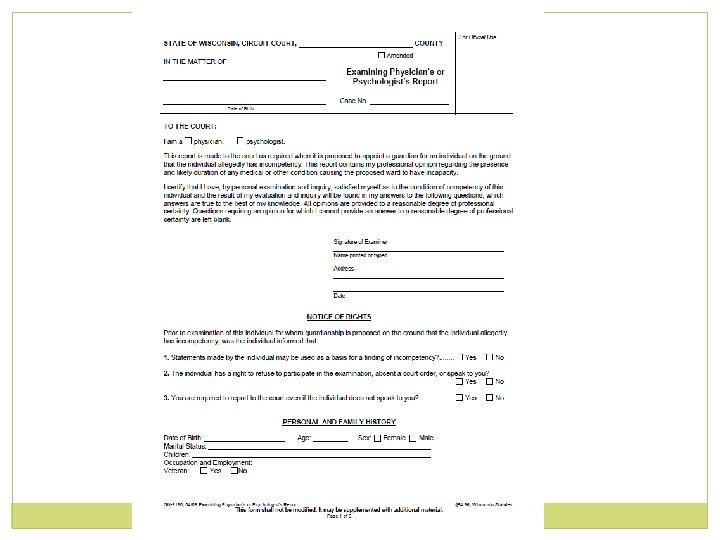
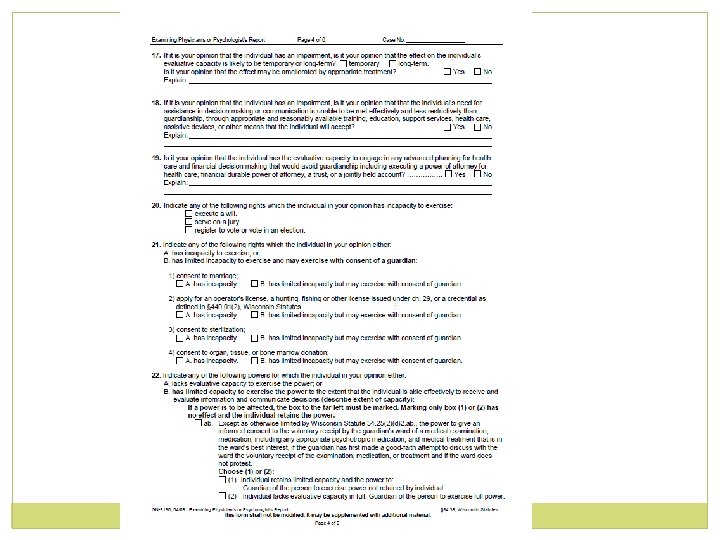
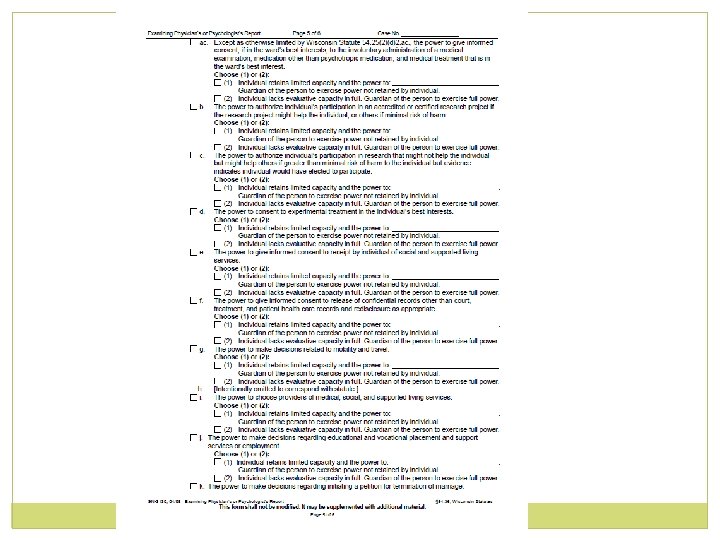
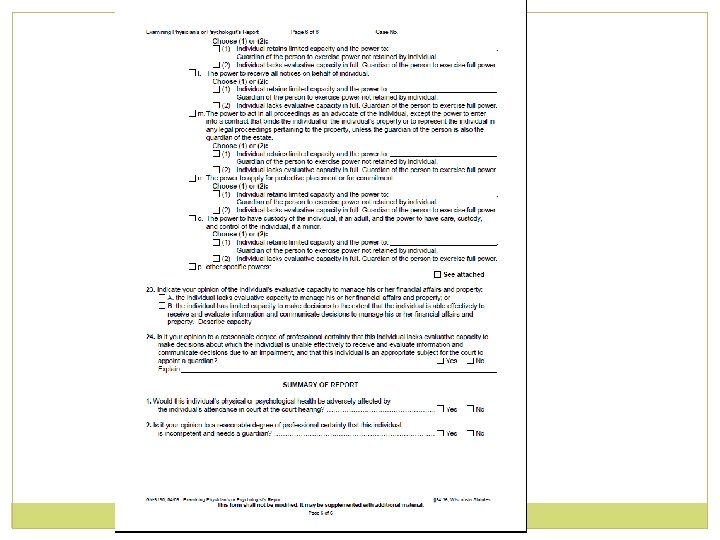
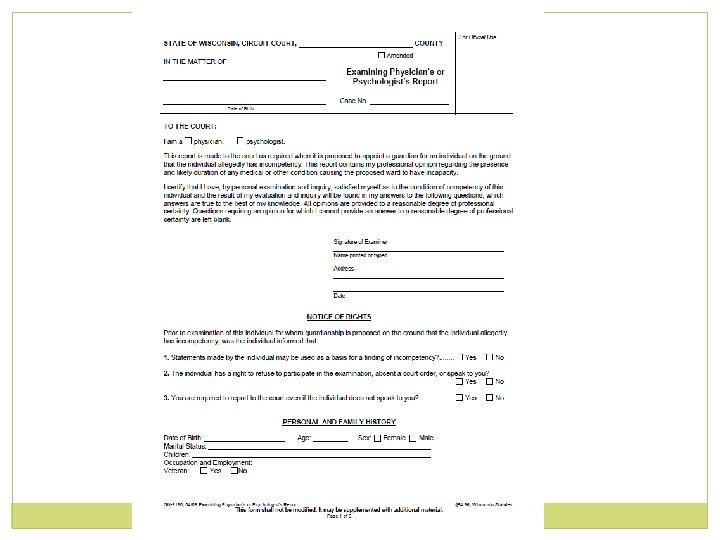
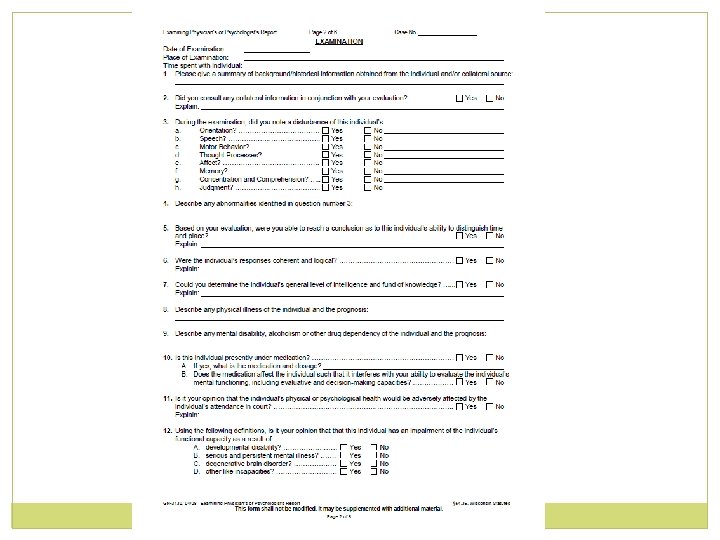
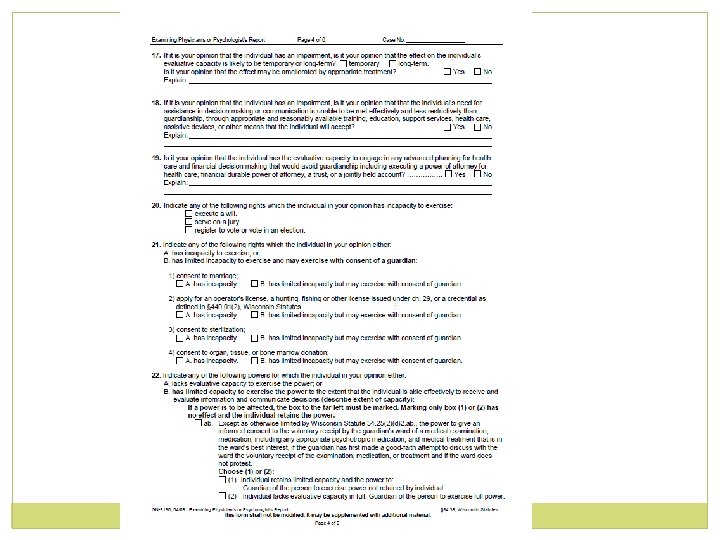
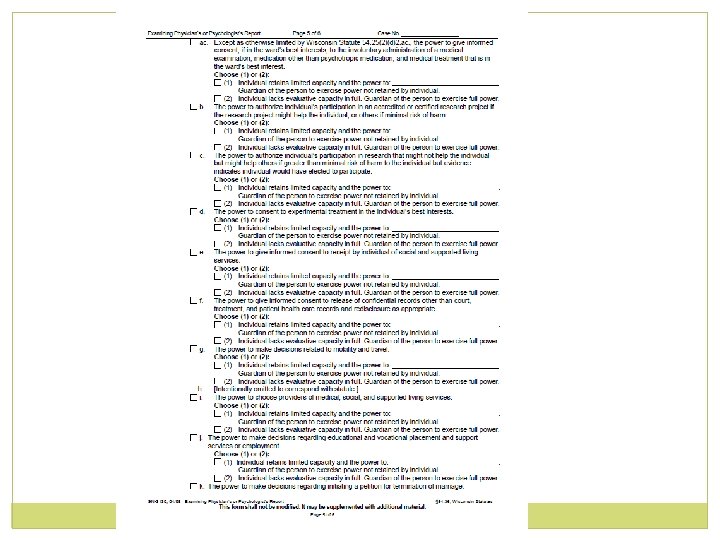
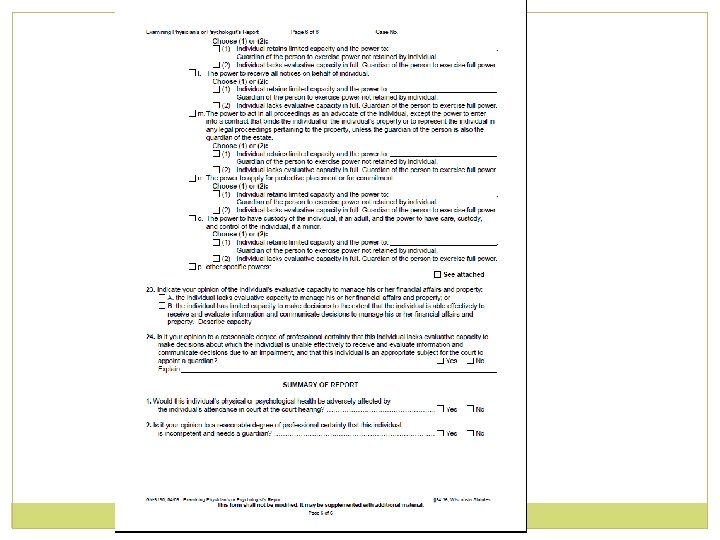
State Form GN-3130, Examining Physician’s or Psychologist’s Report
Recognized Impairing Conditions o Developmental Disability o Serious and persistent mental illness o Degenerative brain disorder o Other like capacities
Caveats o Presence of any of these diagnoses/conditions in and of itself is not considered a basis for a finding of incompetency o It is the resulting deficit in capacity that serves as this basis
�A person’s failure to make or communicate a decision must be a product of that condition in order for incapacity/incompetence to be inferred �Thus, a person who refuses surgery and is depressed may not be refusing because of pessimism, hopelessness or other product of depression; a person who refuses Tx as a way to manipulate family may not be incompetent
More caveats o Mere refusal of treatment, alone, does not constitute incompetency o Nor does “eccentricity” or “poor judgment”
�An alcoholic who continues to drink is not necessarily incompetent, even if safety of self/others is threatened while intoxicated
Relevant diagnostic issues o Is the condition reversible? Temporary? o Dementia vs delirium o Dementia vs depressive pseudodementia o Dementia vs effects of medication, medical conditions
o This is a legal document that serves as a recommendation o The individual is entitled to a court hearing o The final decision rests with the court
Case �J. A. is a 79 y. 0. female, admitted with pulse 150, a fib, shortness of breath �Was living alone, at times would not allow visiting nurse into her home �Daughter has noticed gradual decline in functioning. MMSE score 22 �Refuses cardioversion, cannot say why
Case �B. H. is a 79 y. o. female admitted with herniated disc, degenerative joint disease, COPD; numerous medications, intense pain/narcotic pain meds �MMSE on day of assessment was 22, only partially oriented �Mild loss of short term memory over last few years. A week earlier her functioning was fair to good-still driving, able to prepare meals �Her attention, orientation, and comprehension have fluctuated from good to poor day by day during admission
Case �T. S. is a 60 y. o. male with a history of depression. Admitted with pneumonia, end stage kidney disease, diabetic retinopathy, left foot amputation �Mental status exam- depressive symptoms have improved with treatment-no indication of thought disorder-no clear suicidal ideation… �But refuses to consider dialysis
Case �D. B. is an 86 y. o. male with history of transient ischemic attacks �Memory has declined significantly over past few years. Resides in assisted living facility. �Hx colon CA, now worked up for likely throat CA �Possible decisions looming-surgery, treatment, hospice, life-sustaining measures �He is well oriented, rational, but unable to recall having previous conversations about these issues, even day before �In each discussion he has expressed clear desire for full code, any treatments or measures to sustain his life
Whatever houses I may visit, I will come for the benefit of the sick, remaining free of all intentional injustice, of all mischief and in particular of sexual relations with both female and male persons, be they free or slaves. . . I will keep them from harm and injustice
I swear by Apollo the Physician and Asclepius and Hygieia and Panaceia and all the gods, and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant: To hold him who has taught me this art as equal to my parents and to live my life in partnership with him, and if he is in need of money to give him a share of mine…
Resources �Baker R, Lichtenberg P, Moye J. A practice guideline for assessment of competency and capacity of the older adult. Prof Psychology: Research and Practice 1998; 29(2): 149 -154. �Buchanan A. Mental capacity, legal competence and consent to treatment. J of the Royal Society of Medicine 2004; 97: 415 -420. �Leo R. Competency and the capacity to make treatment decisions. Primary Care Companion J Clin Psychiatry 1999; 1(5): 131 -141.