Evaluating the Implementation of a Comprehensive Care Coordination
- Slides: 29
Evaluating the Implementation of a Comprehensive Care Coordination Program in New York City (NYC) 6 th International Conference on HIV Treatment and Prevention Adherence Eden Roc Renaissance® Miami Beach, Florida Tuesday May 24, 2011 International Association of Physicians in AIDS Care Abstract No: 69986 Authors: Yoran Grant Ph. D MPH*, Mary Irvine Dr. PH, Mc. Kaylee Robertson MPH , Stephanie Boarden MPH, Kevin Dugan MPH, Jenna Liut MPA, Jessica Auerbach MPH, Beau Mitts MPH, Graham Harriman MA, Daniel Weglein MD MPH, Fabienne Laraque MD MPH *Presenting Author
Agenda • Background • Demographics • Process Evaluation o o Goals and Methods Results § Focus Groups § Chart Reviews § Surveys • Discussion
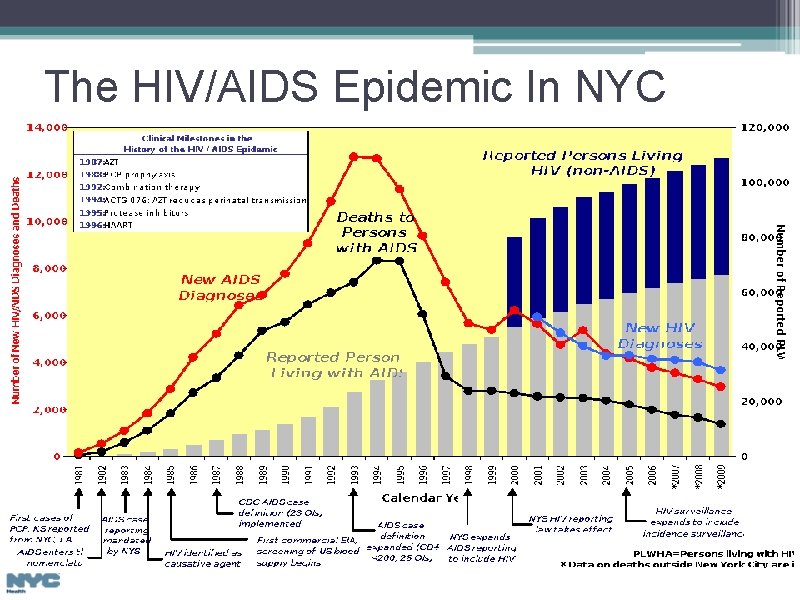
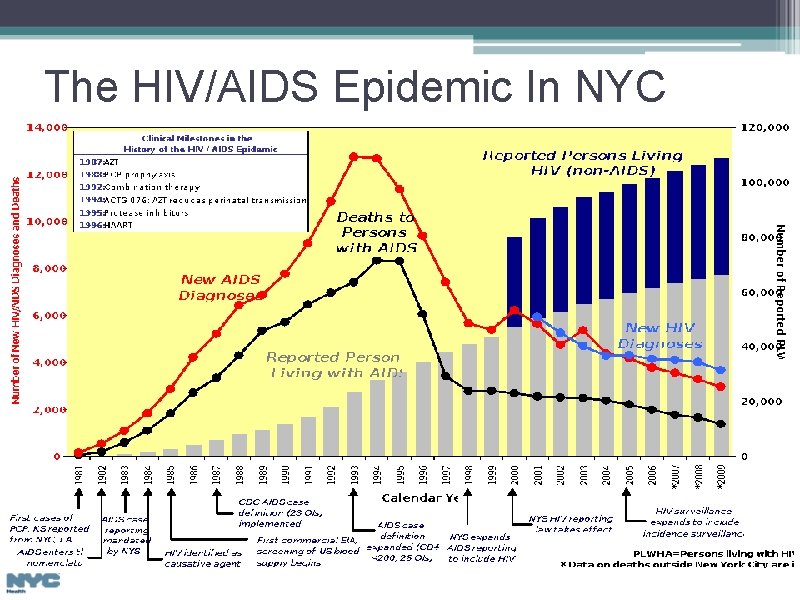
The HIV/AIDS Epidemic In NYC
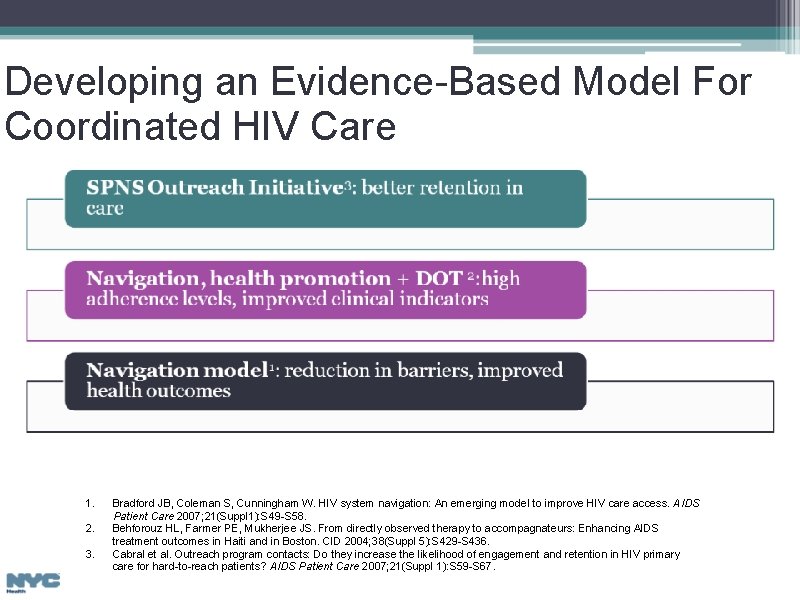
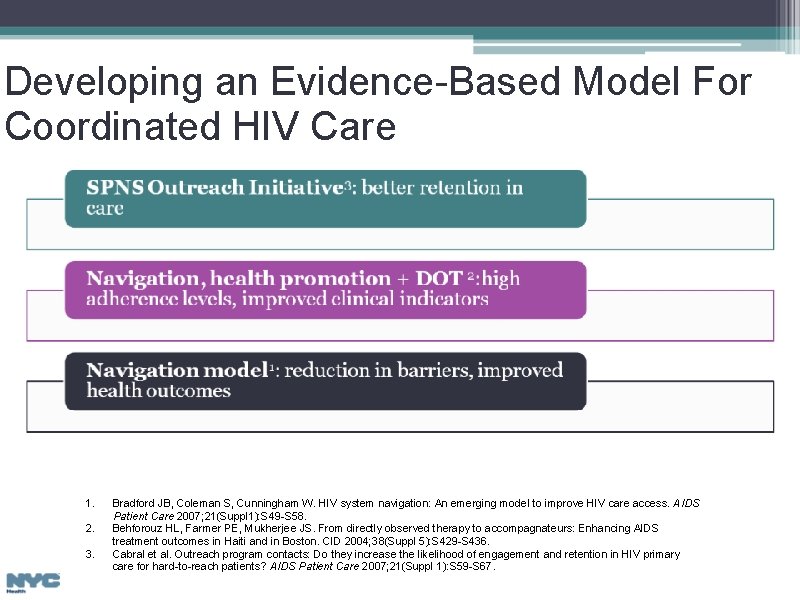
Developing an Evidence-Based Model For Coordinated HIV Care 1. 2. 3. Bradford JB, Coleman S, Cunningham W. HIV system navigation: An emerging model to improve HIV care access. AIDS Patient Care 2007; 21(Suppl 1): S 49 -S 58. Behforouz HL, Farmer PE, Mukherjee JS. From directly observed therapy to accompagnateurs: Enhancing AIDS treatment outcomes in Haiti and in Boston. CID 2004; 38(Suppl 5): S 429 -S 436. Cabral et al. Outreach program contacts: Do they increase the likelihood of engagement and retention in HIV primary care for hard-to-reach patients? AIDS Patient Care 2007; 21(Suppl 1): S 59 -S 67.
Care Coordination Definition 1 • The deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of health care services. • Organizing care involves the marshalling of personnel and other resources needed to carry out all required patient care activities, and is often managed by the exchange of information among participants responsible for different aspects of care. 1. Mc. Donald et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. AHRQ. June 2007. pg. 41.
Care Coordination Program Objectives • Ensure that HIV-infected persons are linked to care in a timely and coordinated manner and are retained in care • Teach and support treatment adherence and other health behaviors/skills to promote patient autonomy • Assist in obtaining social services and address mental health and drug use problems • Suppress viral load at the individual and at the population level • Routinely incorporate risk reduction activities as a part of health promotion
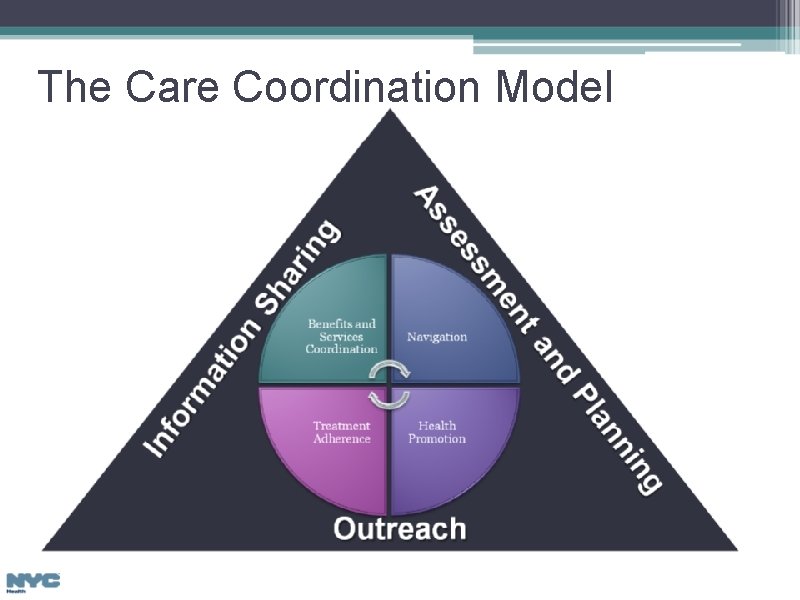
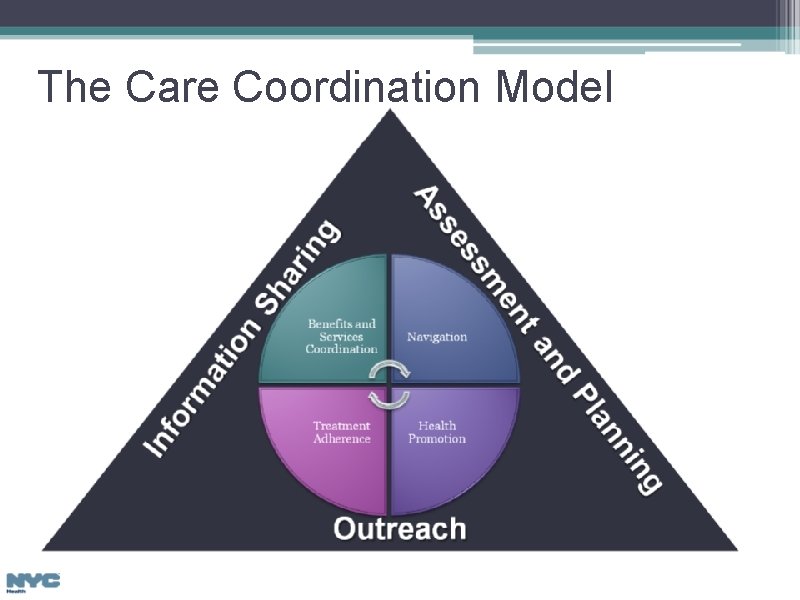
The Care Coordination Model
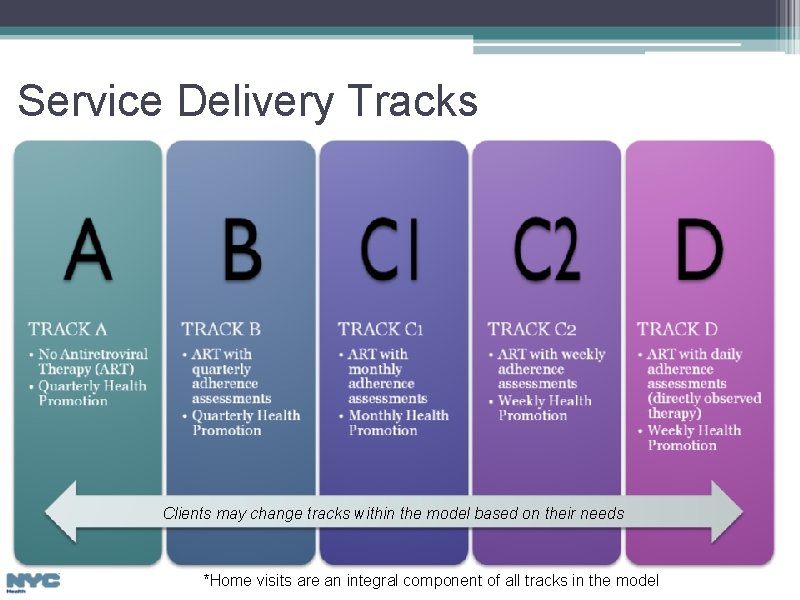
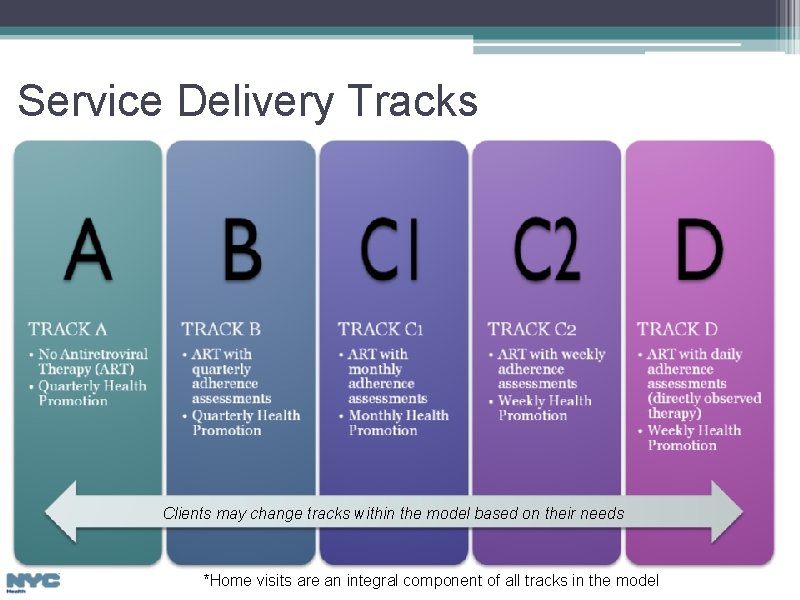
Service Delivery Tracks Clients may change tracks within the model based on their needs *Home visits are an integral component of all tracks in the model
Implementing Care Coordination • 12/1/2009 – Program Launch o Development and distribution of a formal protocol to inform service delivery o 27 agencies charged with staffing and client enrollment § 1 agency lost due to closure § 2 additional agencies added in August 2010 to improve coverage citywide • 9/30/2010 o Agencies were at 75% staff o 2, 400 clients were enrolled and active in the program • 10/1/2010 o NYC DOHMH commences a process evaluation after first 10 months of implementation
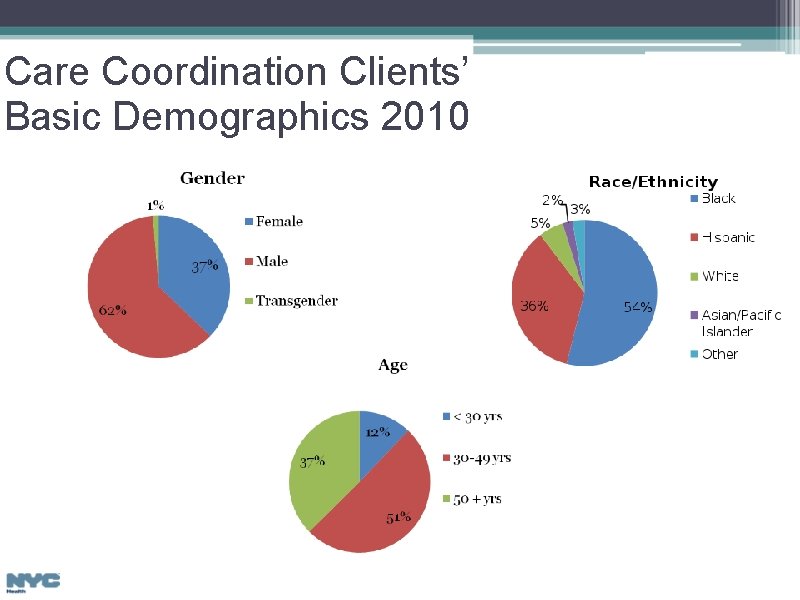
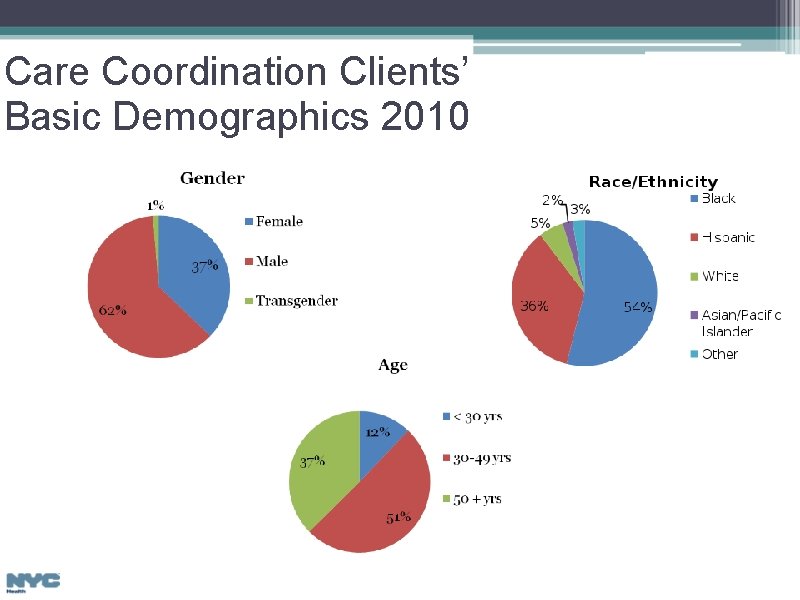
Care Coordination Clients’ Basic Demographics 2010
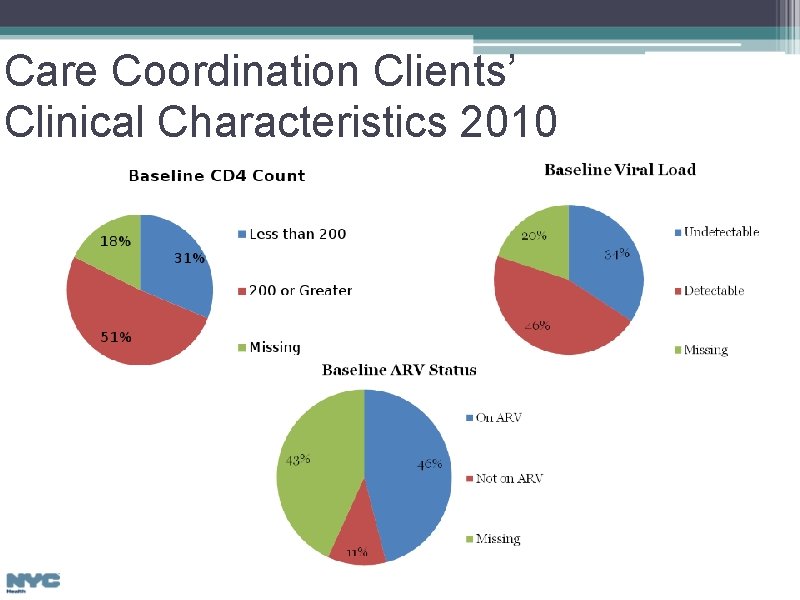
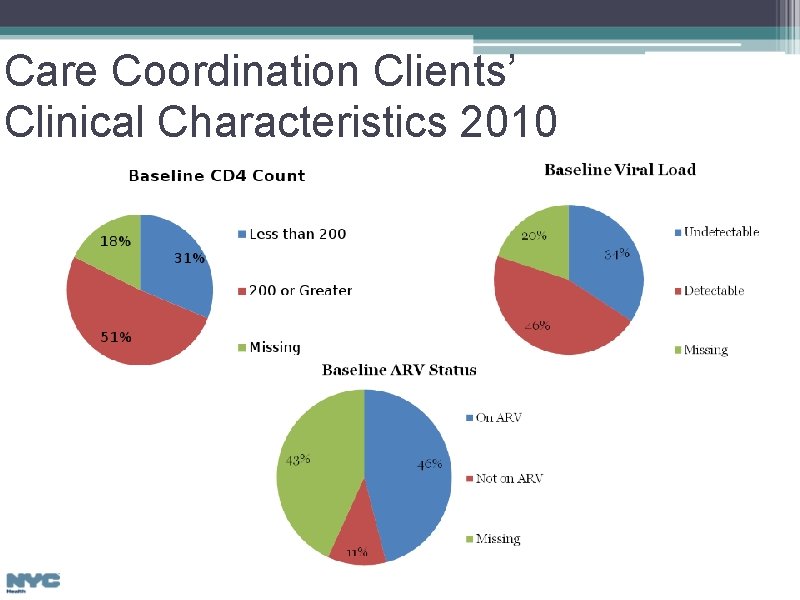
Care Coordination Clients’ Clinical Characteristics 2010
Process Evaluation Goals • Assess the implementation of the Care Coordination program • Identify program-wide areas for technical assistance • Identify agency-specific areas for technical assistance
Methodology • Step 1: Chart reviews o o Conducted from 10/13 – 11/30/2010 25 agencies • Step 2: Focus groups o o Representative sampling of sites Role Specific • Step 3: Provider Surveys o Distributed in April 2011 to all Care Coordination staff at all provider agencies
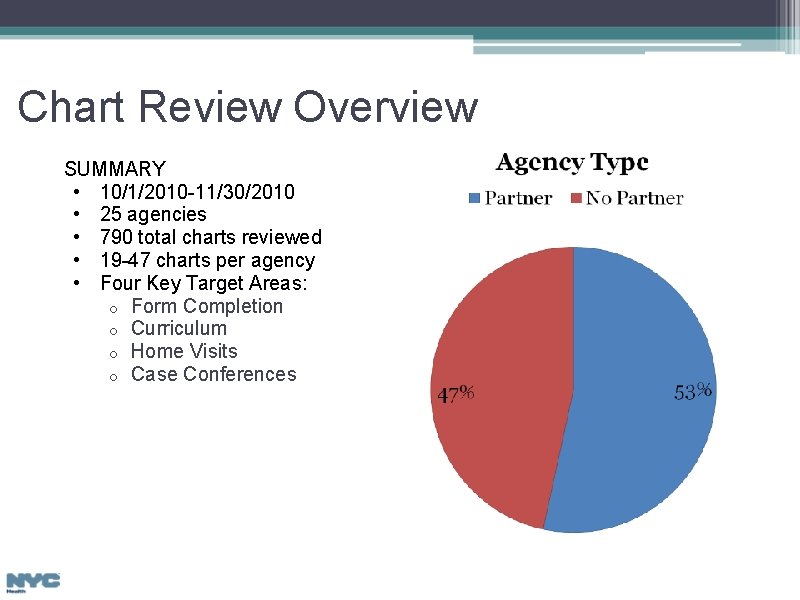
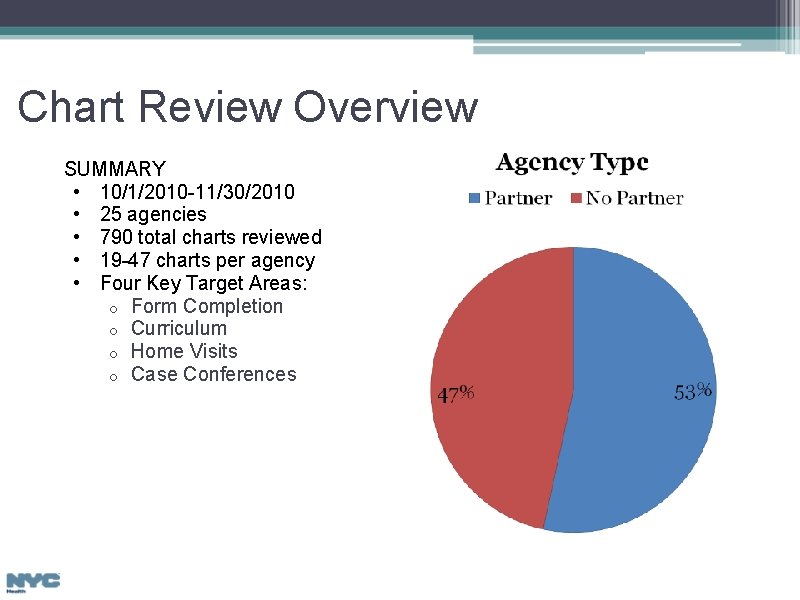
Chart Review Overview SUMMARY • 10/1/2010 -11/30/2010 • 25 agencies • 790 total charts reviewed • 19 -47 charts per agency • Four Key Target Areas: o Form Completion o Curriculum o Home Visits o Case Conferences
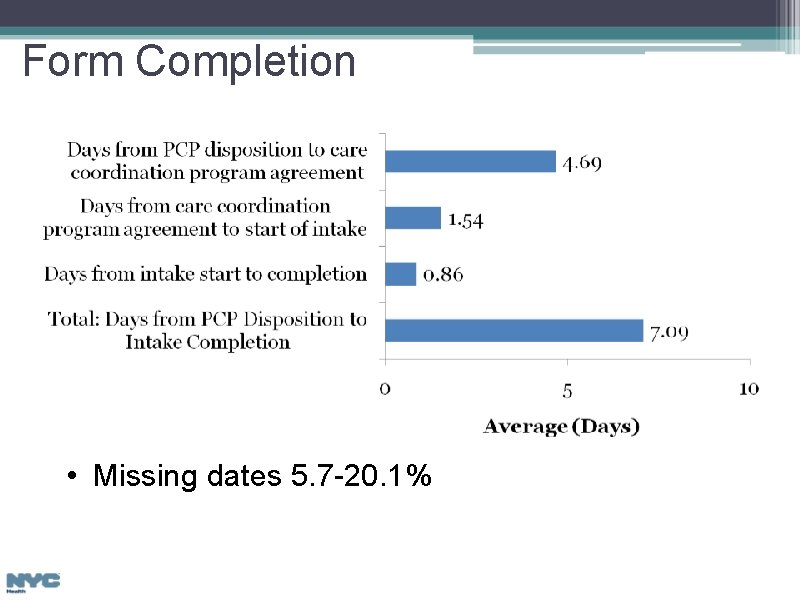
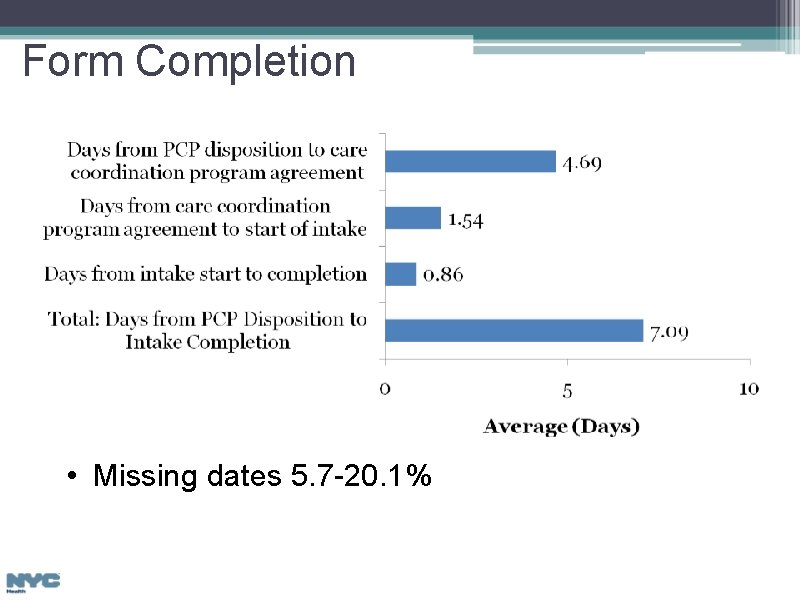
Form Completion • Missing dates 5. 7 -20. 1%
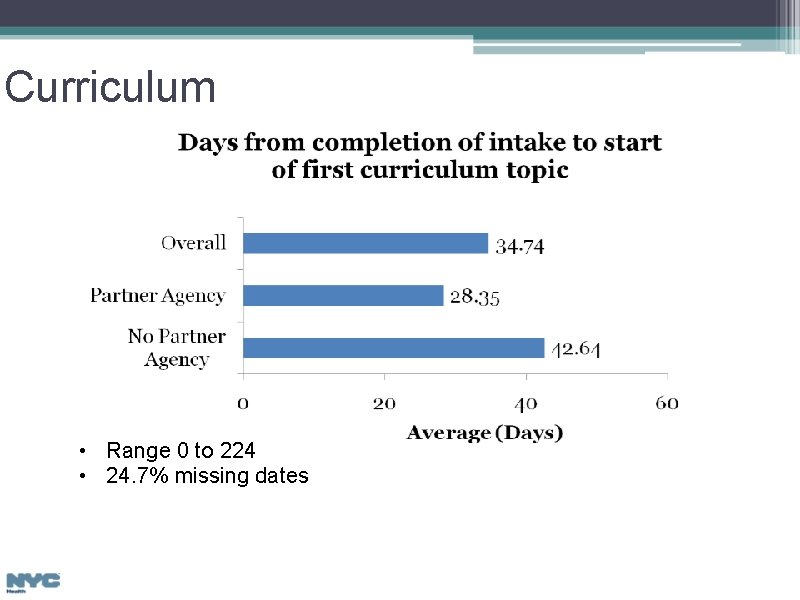
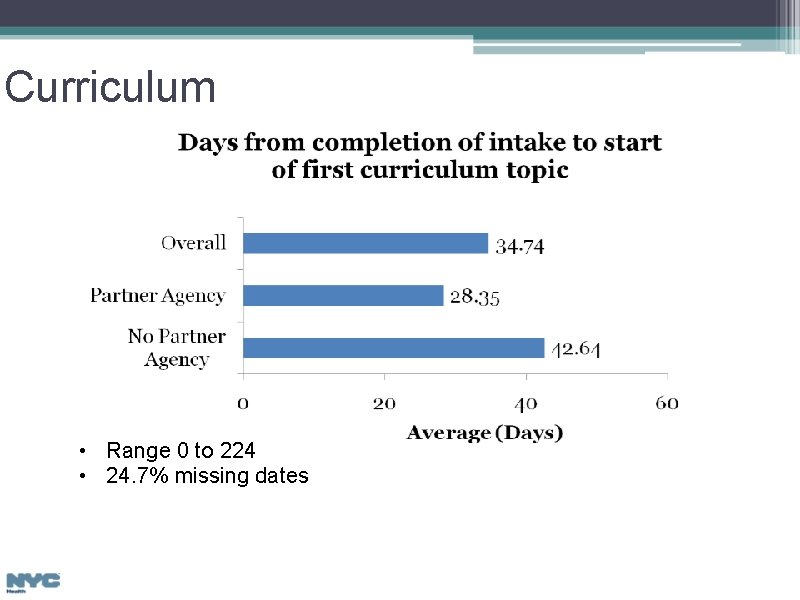
Curriculum • Range 0 to 224 • 24. 7% missing dates
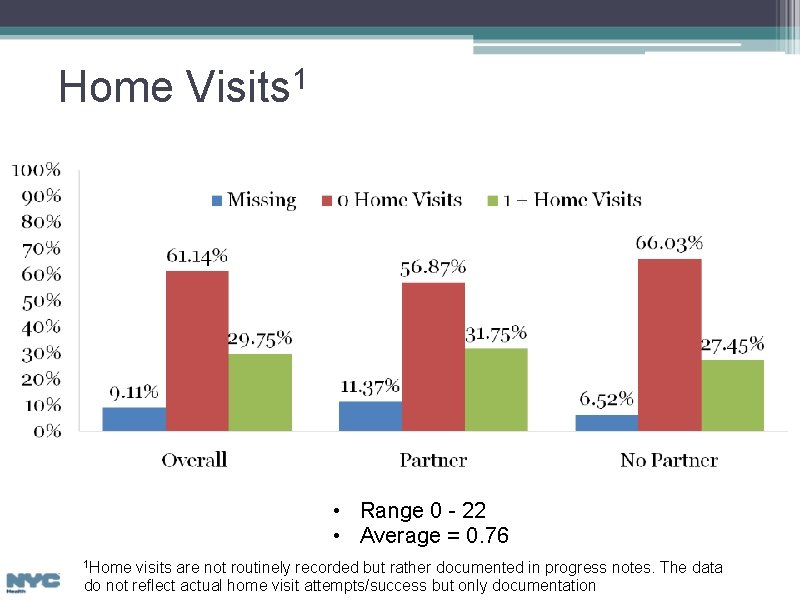
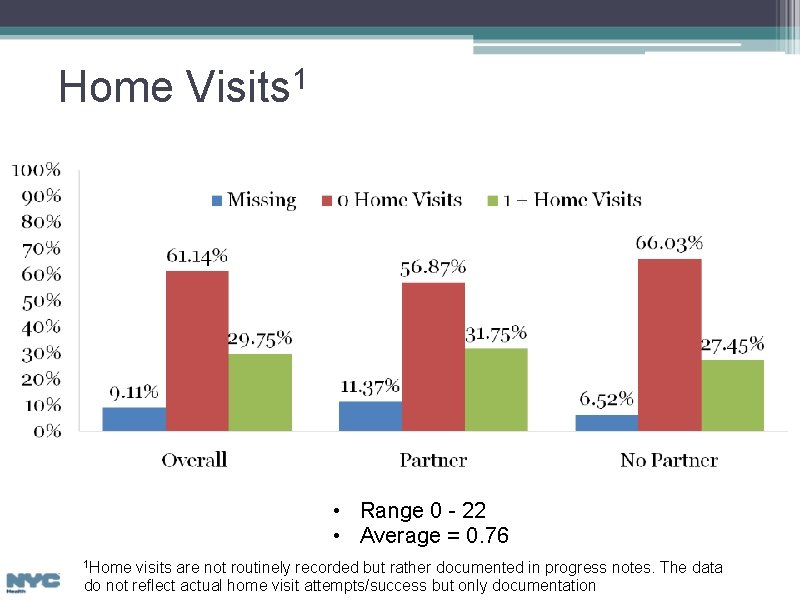
Home Visits 1 • Range 0 - 22 • Average = 0. 76 1 Home visits are not routinely recorded but rather documented in progress notes. The data do not reflect actual home visit attempts/success but only documentation
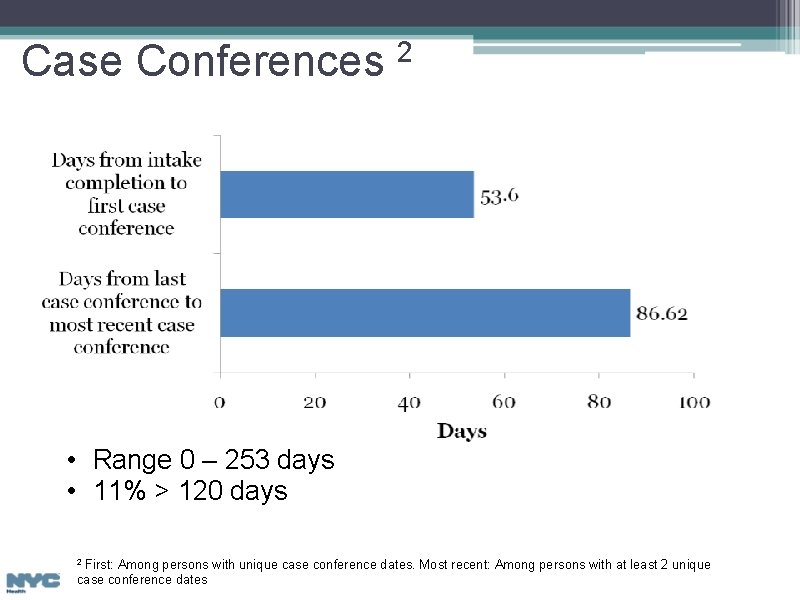
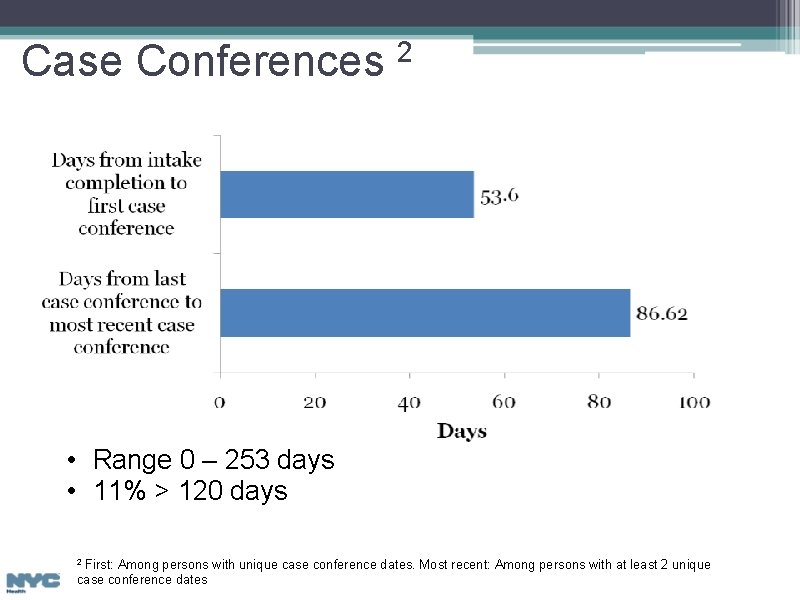
Case Conferences 2 • Range 0 – 253 days • 11% > 120 days First: Among persons with unique case conference dates. Most recent: Among persons with at least 2 unique case conference dates 2
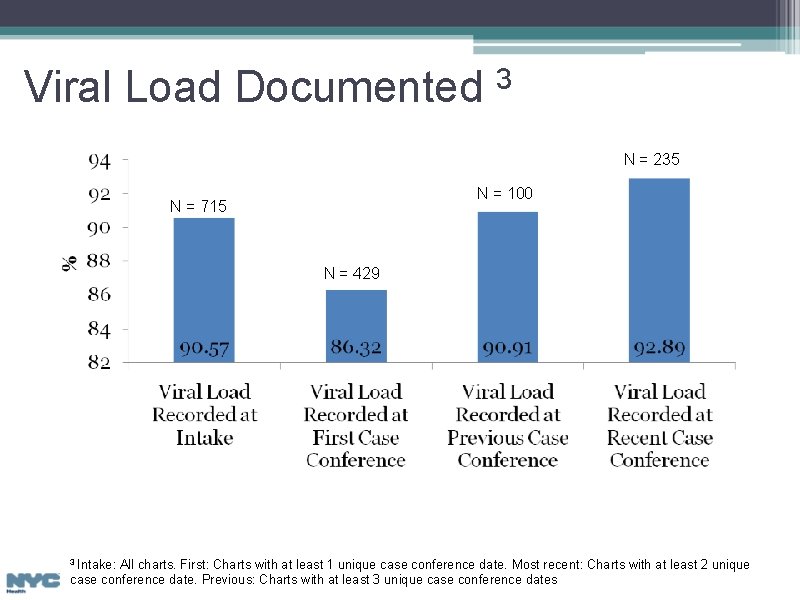
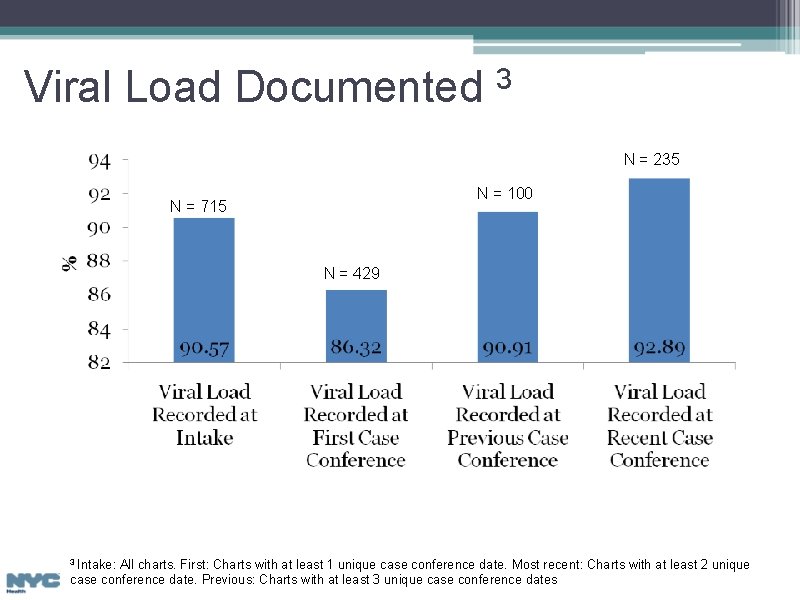
Viral Load Documented 3 N = 235 N = 100 N = 715 N = 429 3 Intake: All charts. First: Charts with at least 1 unique case conference date. Most recent: Charts with at least 2 unique case conference date. Previous: Charts with at least 3 unique case conference dates
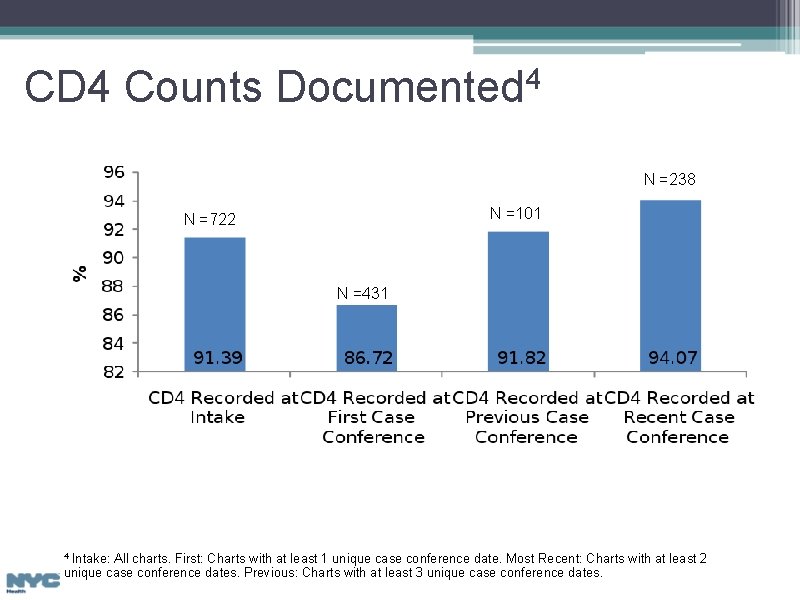
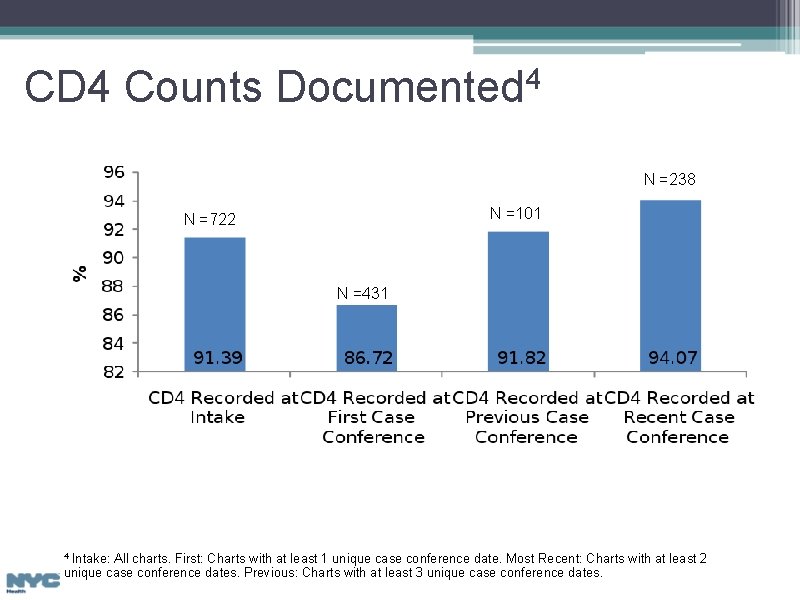
CD 4 Counts Documented 4 N =238 N =101 N =722 N =431 Intake: All charts. First: Charts with at least 1 unique case conference date. Most Recent: Charts with at least 2 unique case conference dates. Previous: Charts with at least 3 unique case conference dates. 4
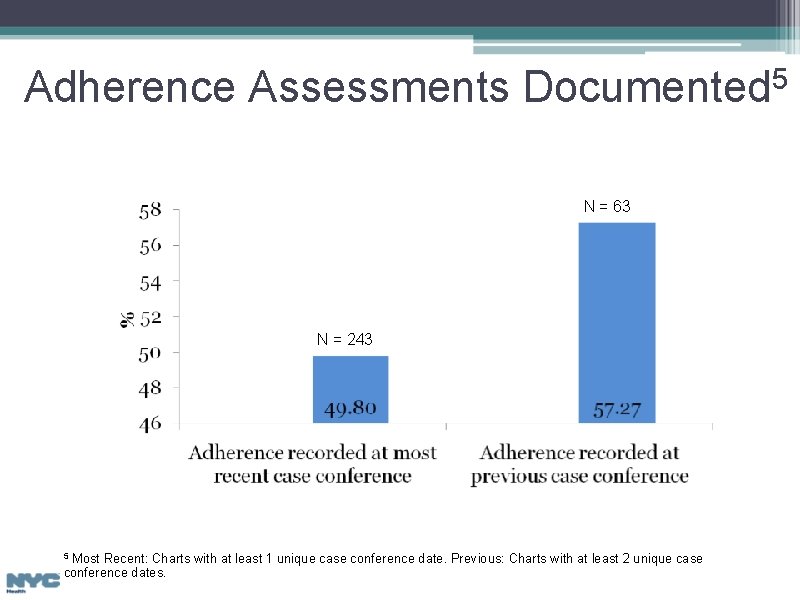
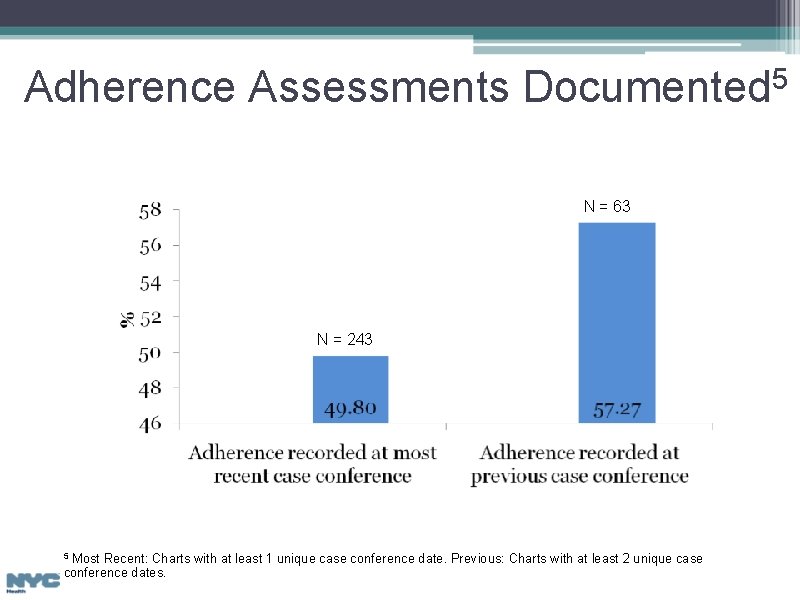
Adherence Assessments Documented 5 N = 63 N = 243 Most Recent: Charts with at least 1 unique case conference date. Previous: Charts with at least 2 unique case conference dates. 5
GROUP DISCUSSION: Overarching Themes • • • Workbooks* Home Visits Protocol Flexibility Communication Training Staffing *Guide for health promotion and other work with the client
Role Specific Themes • Program Directors o o o Implementation Issues with DOHMH Model o o Enrollment Pressures Provider Cooperation Paperwork COBRA Battles • Care Coordinators • Patient Navigators o o o Relationships Client Complexities Barriers
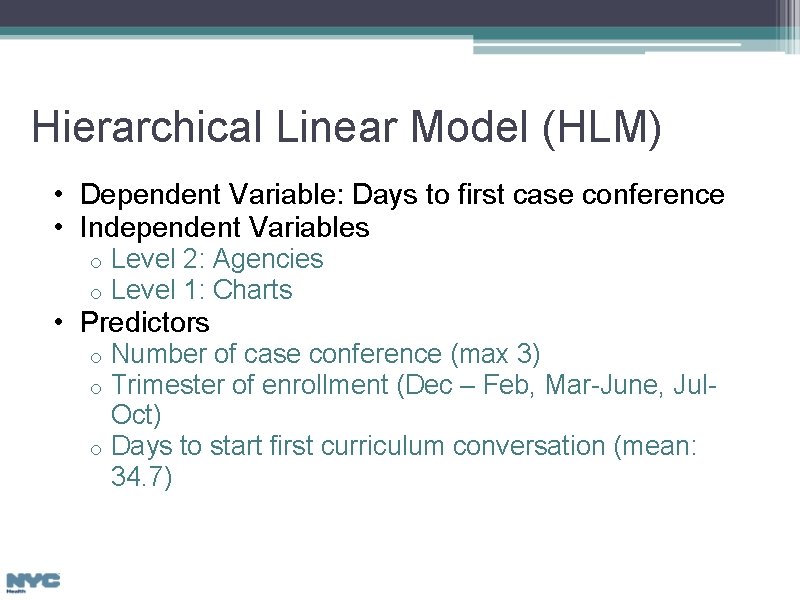
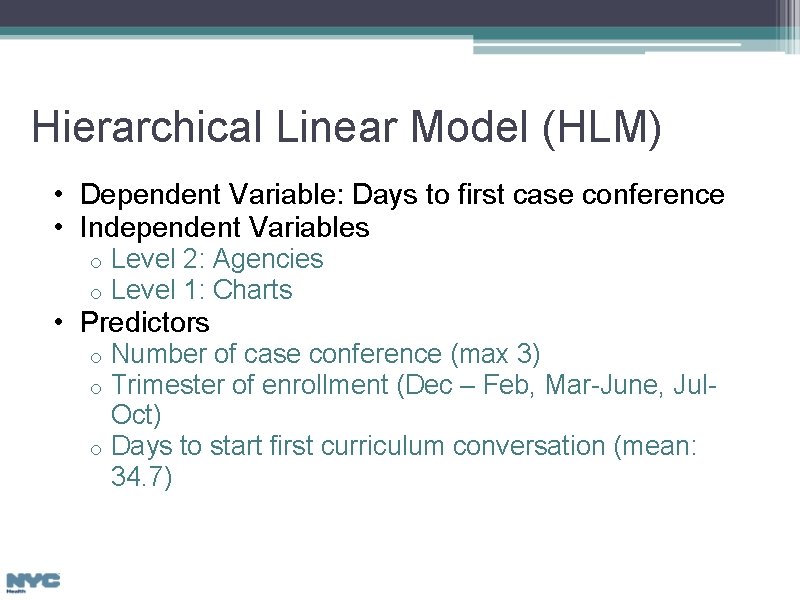
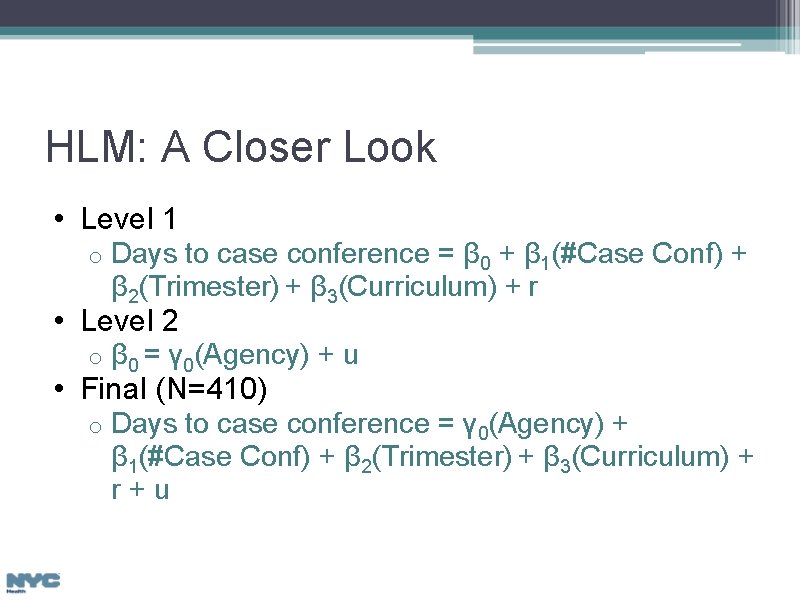
Hierarchical Linear Model (HLM) • Dependent Variable: Days to first case conference • Independent Variables o o Level 2: Agencies Level 1: Charts • Predictors Number of case conference (max 3) Trimester of enrollment (Dec – Feb, Mar-June, Jul. Oct) o Days to start first curriculum conversation (mean: 34. 7) o o
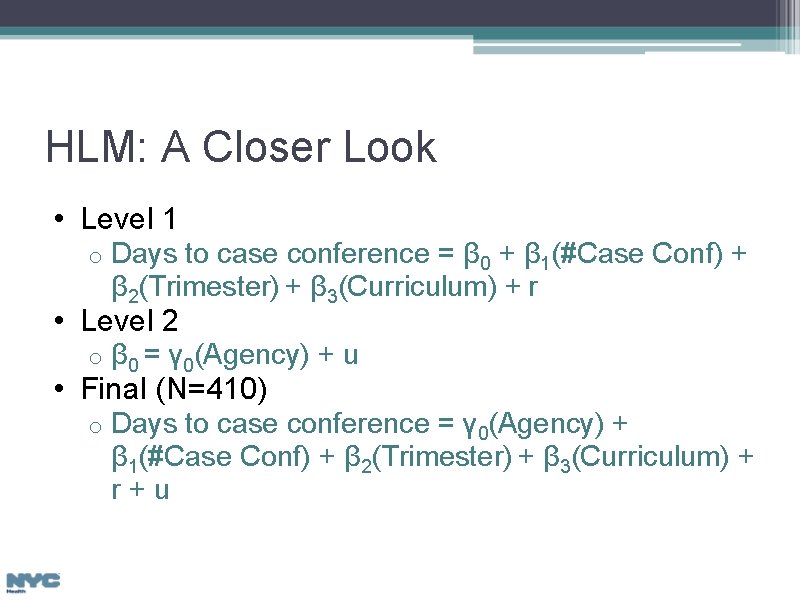
HLM: A Closer Look • Level 1 o Days to case conference = β 0 + β 1(#Case Conf) + β 2(Trimester) + β 3(Curriculum) + r • Level 2 o β 0 = γ 0(Agency) + u o Days to case conference = γ 0(Agency) + β 1(#Case Conf) + β 2(Trimester) + β 3(Curriculum) + r+u • Final (N=410)
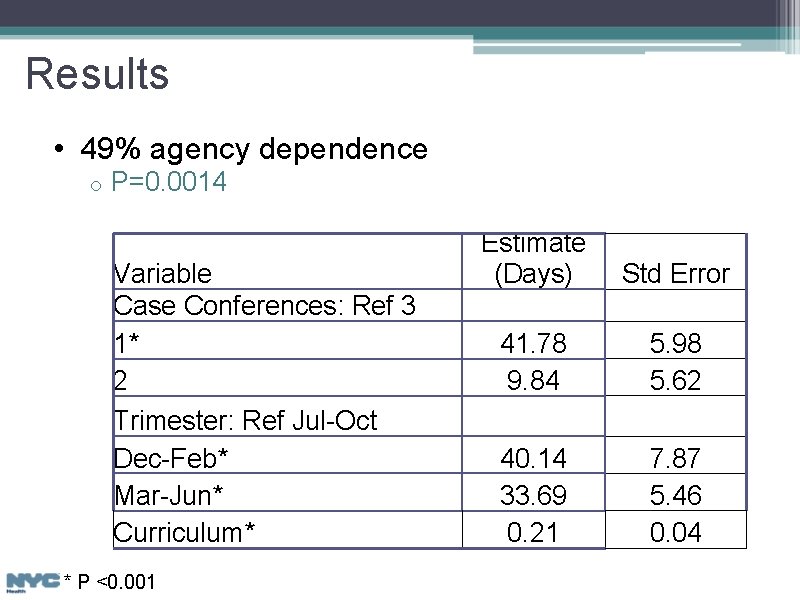
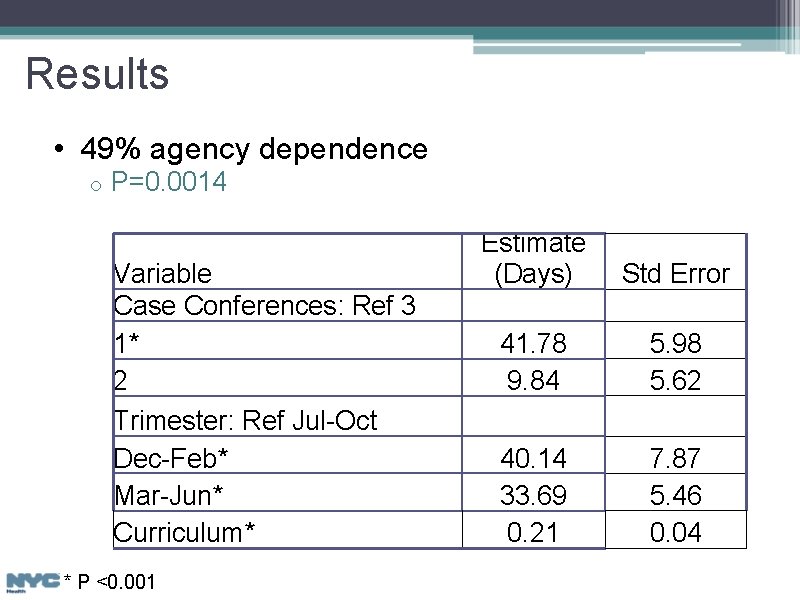
Results • 49% agency dependence o P=0. 0014 Variable Case Conferences: Ref 3 1* 2 Trimester: Ref Jul-Oct Dec-Feb* Mar-Jun* Curriculum* * P <0. 001 Estimate (Days) Std Error 41. 78 9. 84 5. 98 5. 62 40. 14 33. 69 0. 21 7. 87 5. 46 0. 04
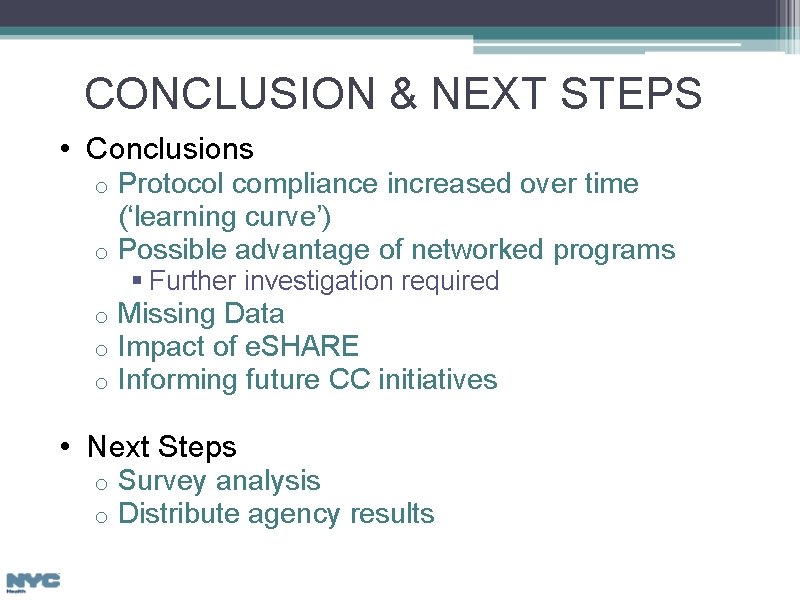
CONCLUSION & NEXT STEPS • Conclusions Protocol compliance increased over time (‘learning curve’) o Possible advantage of networked programs o § Further investigation required o o o Missing Data Impact of e. SHARE Informing future CC initiatives • Next Steps o o Survey analysis Distribute agency results
Acknowledgements • Mc. Kaylee Robertson, MPH • Stephanie Boarden, MPH • Mary Irvine, Dr. PH • Kevin Dugan, MPH • Beau Mitts, MPH • Graham Harriman, MA
Yoran T. Grant Ph. D MPH Senior Analyst, Research & Evaluation Care Treatment and Housing Program Bureau of HIV/AIDS Prevention and Control ygrant@health. nyc. gov