Ethical and Human Rights Issues of HIV and





- Slides: 30
Ethical and Human Rights Issues of HIV and TB Surveillance Timothy H. Holtz, M. D. , M. P. H. International Research and Programs Branch Division of TB Elimination & Health and Human Rights Working Group Centers for Disease Control and Prevention USA
Outline • Definitions • Ethics and Human Rights Documents • Ethics of Public Health Surveillance and • • Research Surveillance: Practice or Research? Strategies for HIV Serosurveys HIV testing in TB patients Questions for Consideration
Definitions • Anonymous – No identifiers ever collected • Anonymized – Identifiers removed • Confidential – Identifying information kept confidential
Definitions • Linked • – Test data and specimen linked to patient by a code or name Informed consent – Risks/benefits of participation clearly explained – Participant gives written or verbal consent – Voluntary – Community consent now recognized
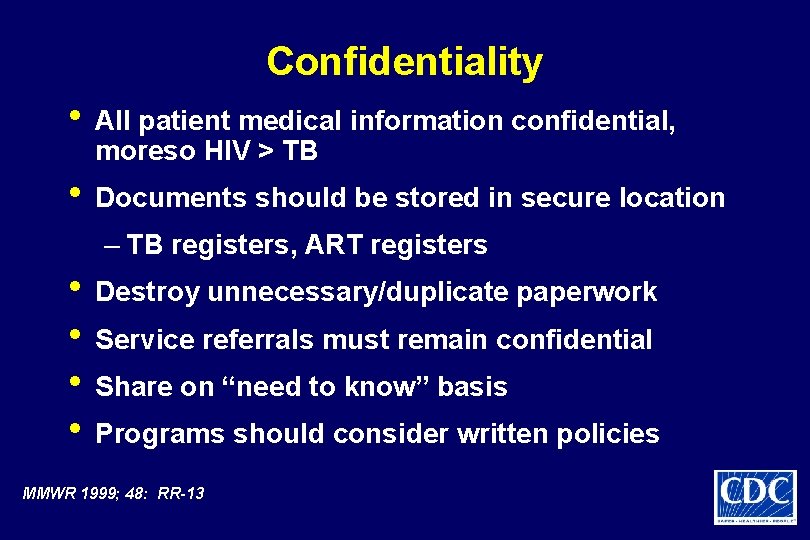
Confidentiality • All patient medical information confidential, moreso HIV > TB • Documents should be stored in secure location – TB registers, ART registers • Destroy unnecessary/duplicate paperwork • Service referrals must remain confidential • Share on “need to know” basis • Programs should consider written policies MMWR 1999; 48: RR-13

Opt-In and Opt-Out • Opt-In – Patient self-refers, VCT, Useful in non-medical sites – Provider initiates testing, may not be highly utilized in medical settings • Opt-Out – Passive – Provider informs patient they will be tested unless they refuse • Possibility of coercion? – Active – Patient not informed, must actively tell provider they refuse test • Borders on mandatory? – Necessity in settings of generalized epidemics? – Breach of autonomy?
Linked data • Remove personal identifiers as soon as possible – Generally not needed for surveillance beyond facility level • Collect and report disaggregated data where possible • Databases with passwords/encryption
Brief History of Medical Ethics • Nuremberg Code (1947) • • – Voluntary participation of subjects with their informed consent Declaration of Helsinki (1964) – Therapeutic vs. nontherapeutic research – Institutional review mechanisms World Medical Association revisions (2000) – Fully informed consent
Relevant Human Rights Documents: International Bill of Human Rights • Universal Declaration of Human Rights (UDHR 1948) • International Covenant on Civil and Political Rights (ICCPR-1966) • International Covenant on Economic, Social, and Cultural Rights (ICESCR-1966)

Siracusa Principles (1984) • States “may impose restrictions on some rights, in narrowly defined circumstances, if such restrictions are necessary to achieve overriding goals, such as public health or to the protect the rights of others…and the general welfare. ” • Restrictions must be “proportional to the interest and constitute the least intrusive and least restrictive measure available. ”

“TB is deeply rooted in populations where human rights and dignity are limited. The disease thrives on the most vulnerable – the marginalized, discriminated against populations, and people living in poverty. World Health Organization 2001
Human rights approach to TB • The principle of nondiscrimination is • • • fundamental to public health and human rights practice Neglect of the right to information can have substantial health impacts Prisons are an environment that increases vulnerability to TB Necessity of addressing TB and HIV together in light of the human rights dimensions of both diseases
HR approach to TB cont’d • The dual epidemic of HIV and TB raises issues • • • of individual choice and confidentiality Human rights can be used as a tool for data collection and analysis Human rights approach presented as an avenue for social mobilization to STOP TB Health care systems should take human rights norms and standards into account
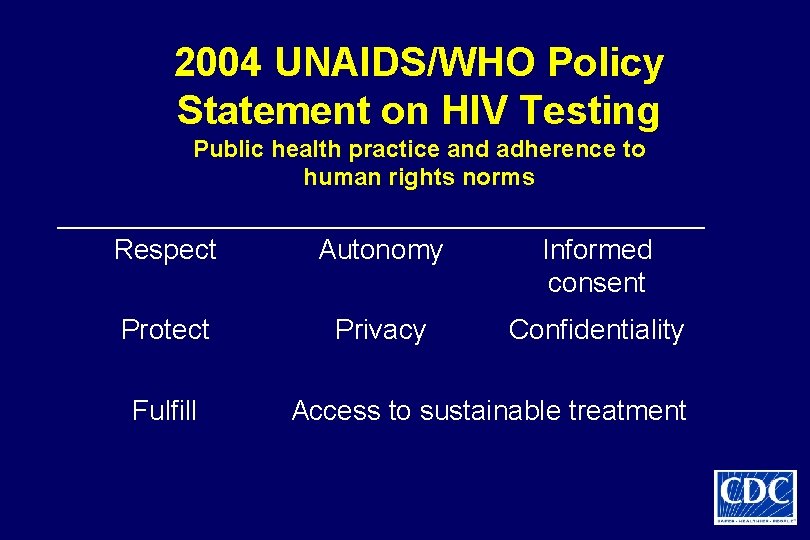
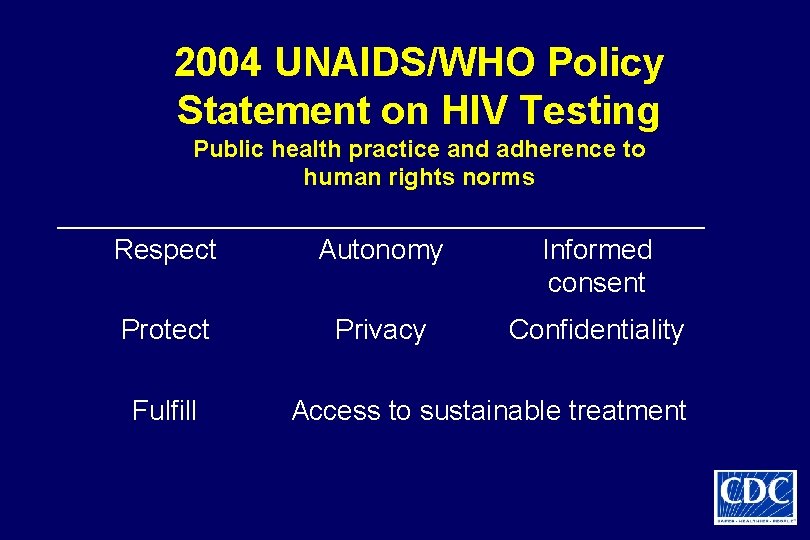
2004 UNAIDS/WHO Policy Statement on HIV Testing Public health practice and adherence to human rights norms Respect Autonomy Informed consent Protect Privacy Confidentiality Fulfill Access to sustainable treatment

Medical Ethics Documents Relevant to Research • Council for International Organizations of Medical Sciences (CIOMS) – Guidelines for Biomedical Research Involving Human Subjects (1993/2002) • Culturally-sensitive informed consent • Protection from exploitation • Protection of confidentiality – Guidelines for Ethical Review of Epidemiologic Studies (1991)
Goals of Public Health Practice and Research • Beneficence – Goal to do good • Nonmaleficence – Protect participants from • • harm (primum non nocere) Justice – Equal treatment and the fair distribution of benefits and burdens Ensure that participants share in scientific advancement and its benefits (UDHR Article 27)
Public Health Surveillance/Research • • • Vital statistics – Legally established function of nation-states Notifiable diseases – TB, STIs, cancer Mandatory notification of some infectious diseases Ethics of public health surveillance largely unquestioned until HIV/AIDS UNHCR/UNAIDS (1984) – “strict rules of data protection & confidentiality” Use of individual names – Need for name must be substantiated Gostin et al. , JAMA 1996; 275: 1921
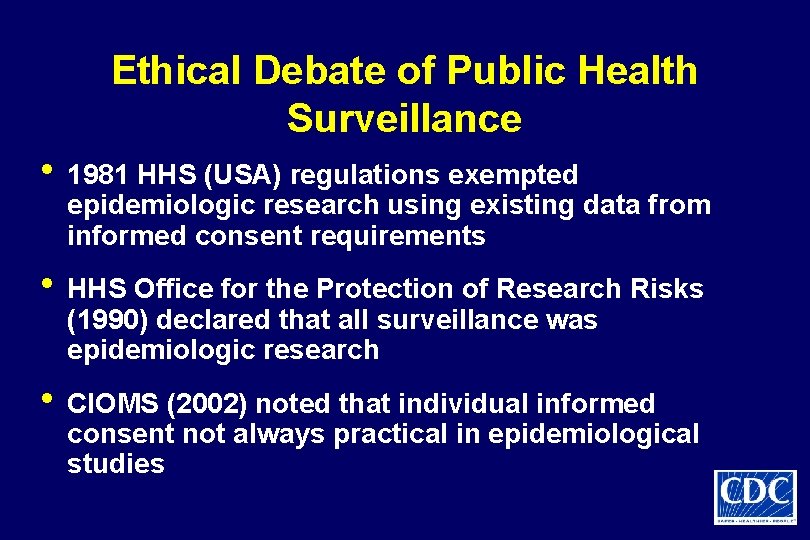
Ethical Debate of Public Health Surveillance • 1981 HHS (USA) regulations exempted epidemiologic research using existing data from informed consent requirements • HHS Office for the Protection of Research Risks (1990) declared that all surveillance was epidemiologic research • CIOMS (2002) noted that individual informed consent not always practical in epidemiological studies
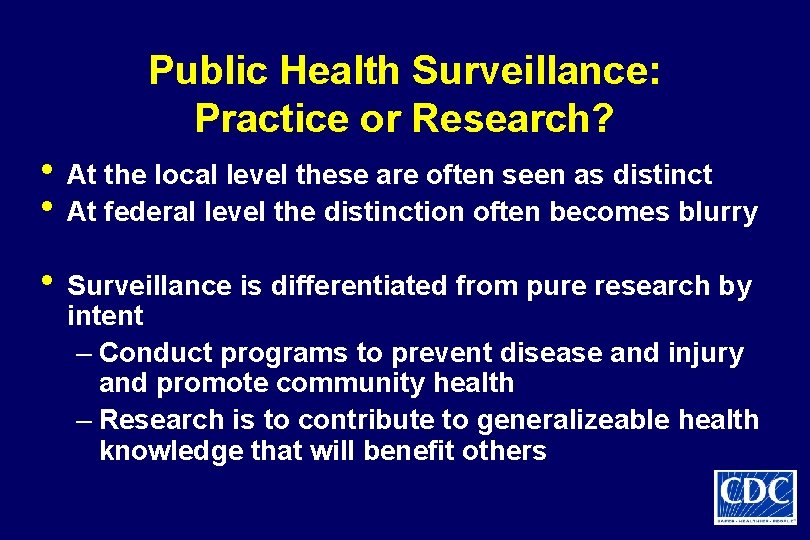
Public Health Surveillance: Practice or Research? • At the local level these are often seen as distinct • At federal level the distinction often becomes blurry • Surveillance is differentiated from pure research by intent – Conduct programs to prevent disease and injury and promote community health – Research is to contribute to generalizeable health knowledge that will benefit others
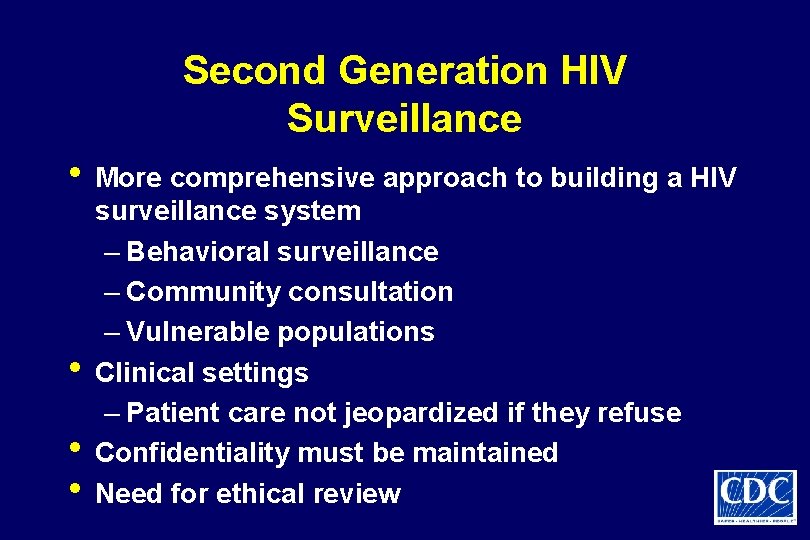
Second Generation HIV Surveillance • More comprehensive approach to building a HIV • • • surveillance system – Behavioral surveillance – Community consultation – Vulnerable populations Clinical settings – Patient care not jeopardized if they refuse Confidentiality must be maintained Need for ethical review
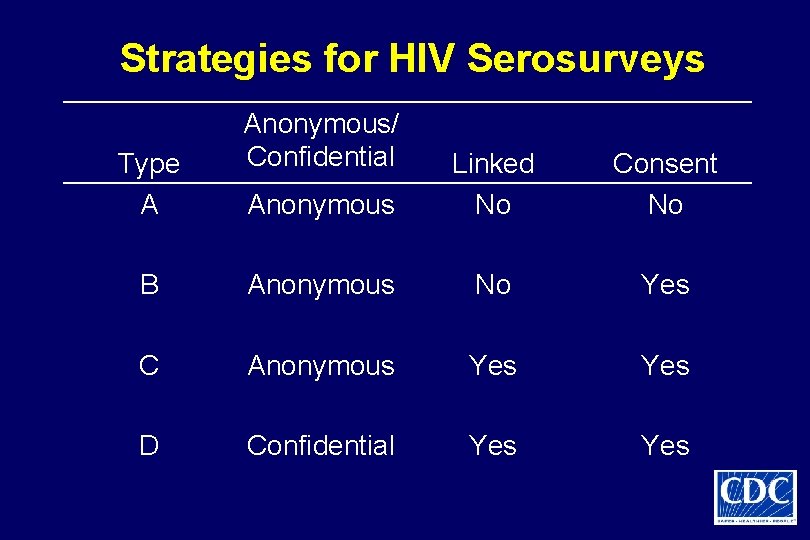
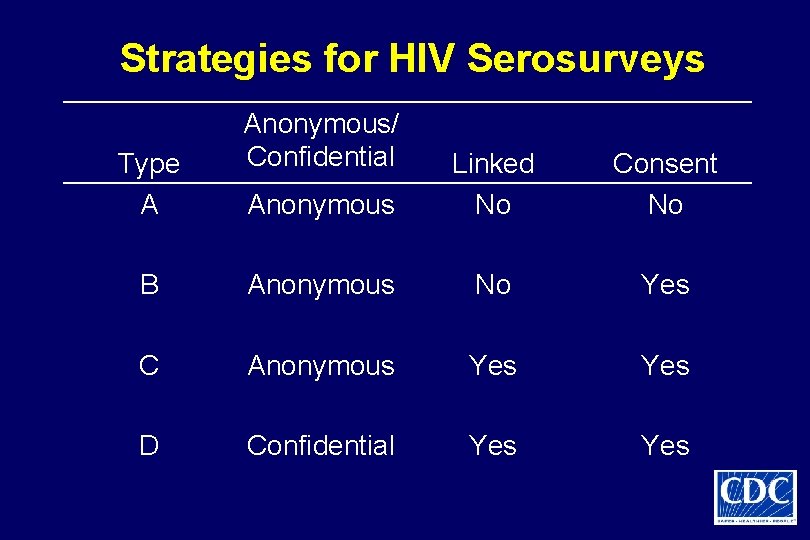
Strategies for HIV Serosurveys Type A Anonymous/ Confidential Anonymous Linked No Consent No B Anonymous No Yes C Anonymous Yes D Confidential Yes
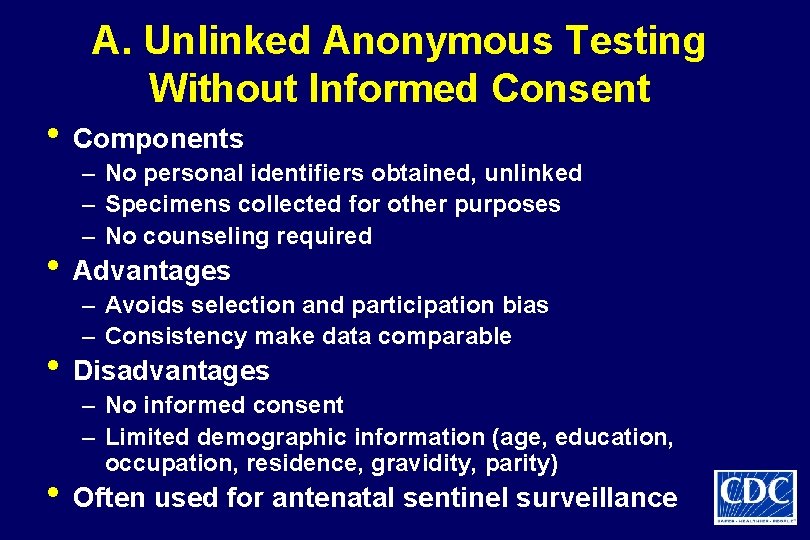
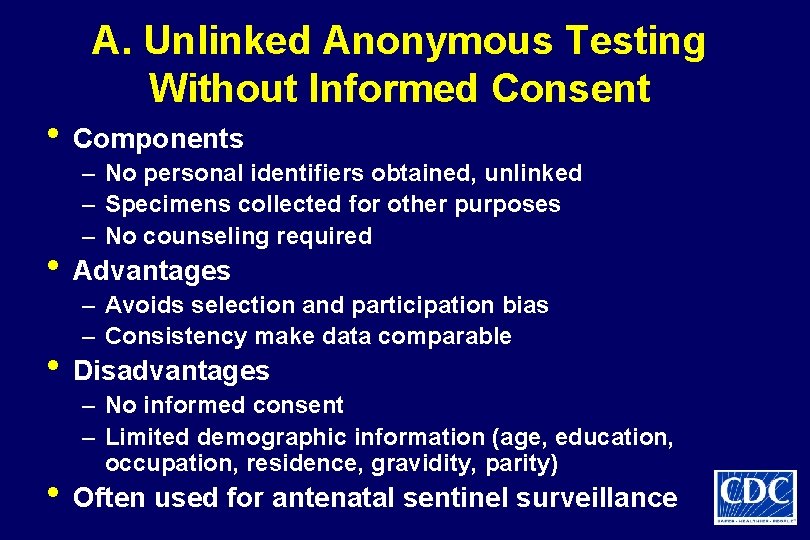
A. Unlinked Anonymous Testing Without Informed Consent • Components – No personal identifiers obtained, unlinked – Specimens collected for other purposes – No counseling required • Advantages – Avoids selection and participation bias – Consistency make data comparable • Disadvantages – No informed consent – Limited demographic information (age, education, occupation, residence, gravidity, parity) • Often used for antenatal sentinel surveillance
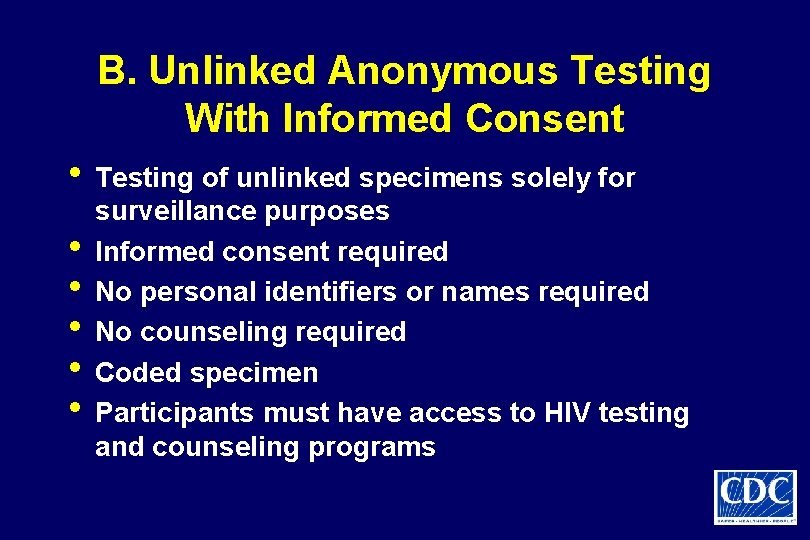
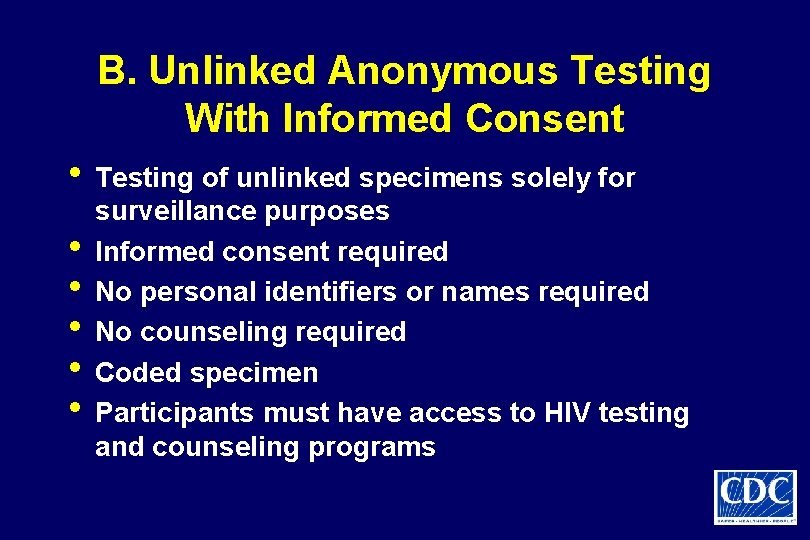
B. Unlinked Anonymous Testing With Informed Consent • Testing of unlinked specimens solely for • • • surveillance purposes Informed consent required No personal identifiers or names required No counseling required Coded specimen Participants must have access to HIV testing and counseling programs
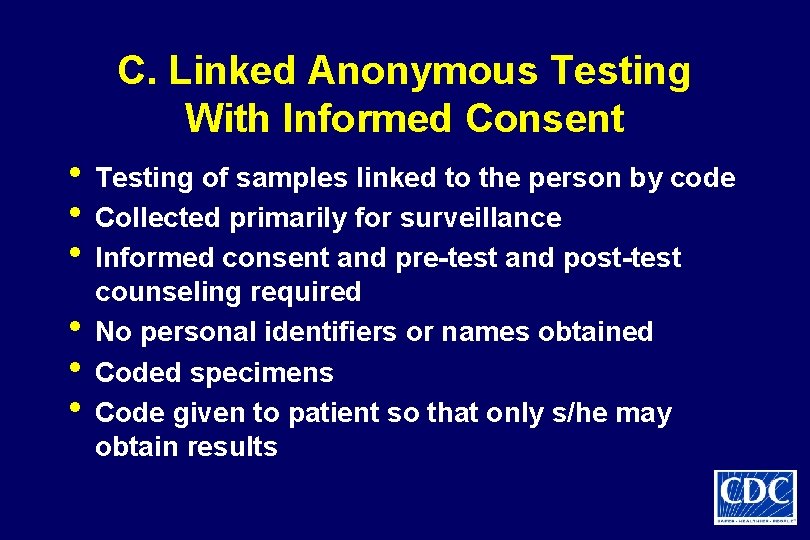
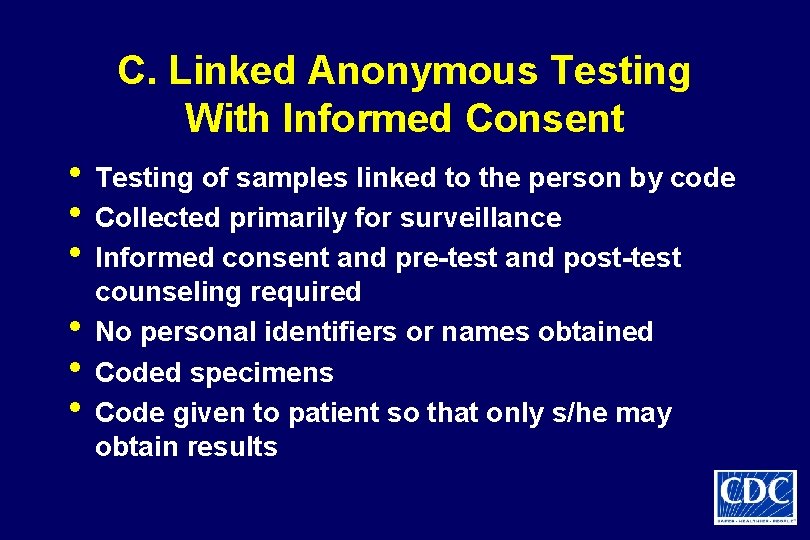
C. Linked Anonymous Testing With Informed Consent • Testing of samples linked to the person by code • Collected primarily for surveillance • Informed consent and pre-test and post-test • • • counseling required No personal identifiers or names obtained Coded specimens Code given to patient so that only s/he may obtain results

D. Linked Confidential Testing With Informed Consent • Test of samples linked to the person by name • Collected for clinical care and surveillance • Personal identifiers or names obtained • Coded specimens - linked to personal • identifying information Ethical obligation to return results to patient
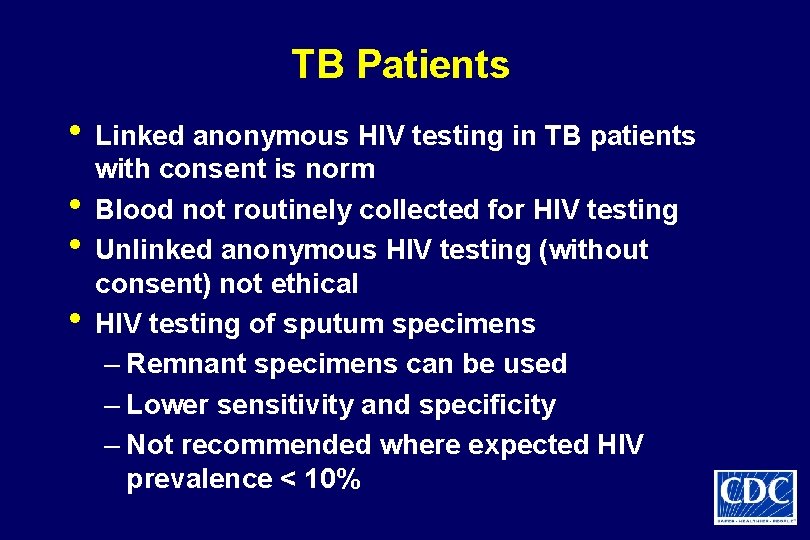
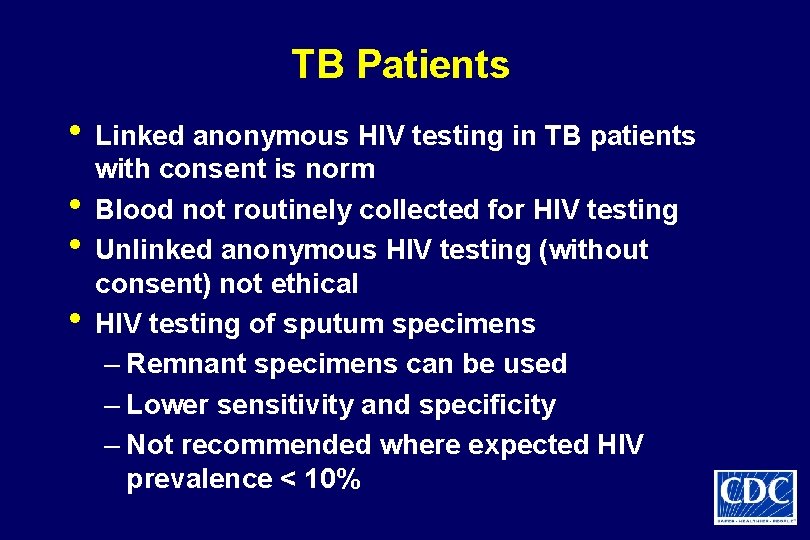
TB Patients • Linked anonymous HIV testing in TB patients • • • with consent is norm Blood not routinely collected for HIV testing Unlinked anonymous HIV testing (without consent) not ethical HIV testing of sputum specimens – Remnant specimens can be used – Lower sensitivity and specificity – Not recommended where expected HIV prevalence < 10%
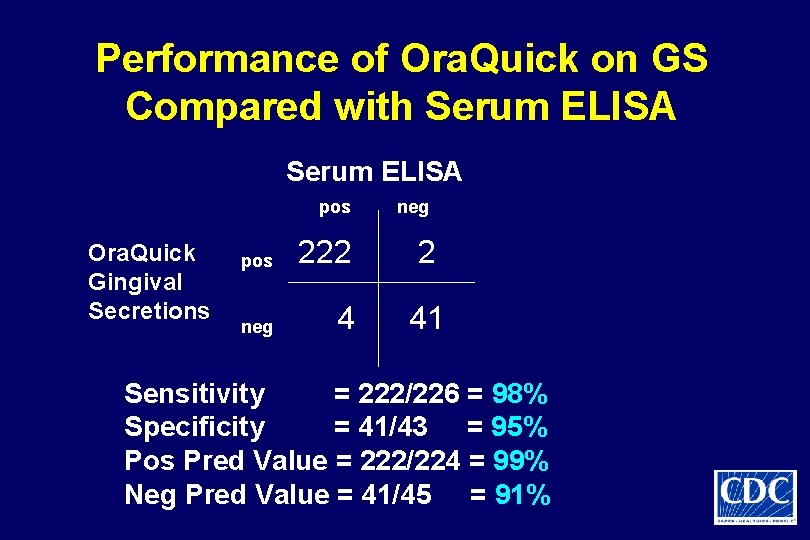
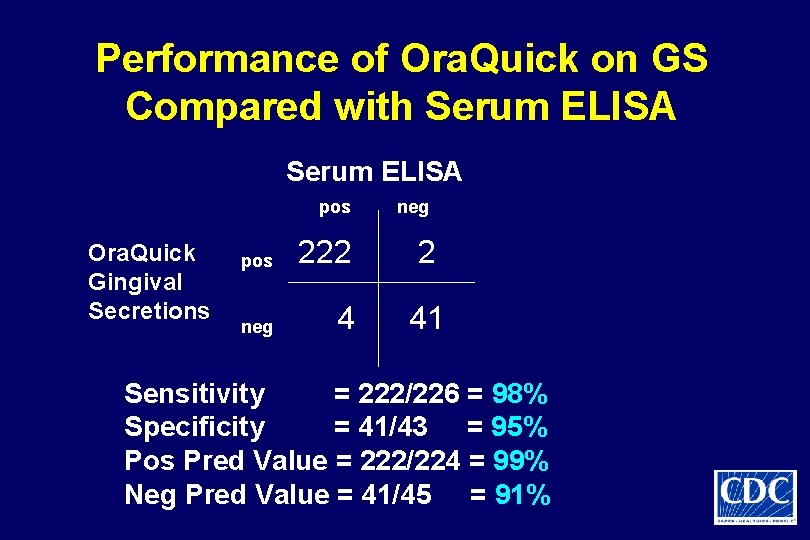
Performance of Ora. Quick on GS Compared with Serum ELISA pos Ora. Quick Gingival Secretions neg pos 222 2 neg 4 41 Sensitivity = 222/226 = 98% Specificity = 41/43 = 95% Pos Pred Value = 222/224 = 99% Neg Pred Value = 41/45 = 91%
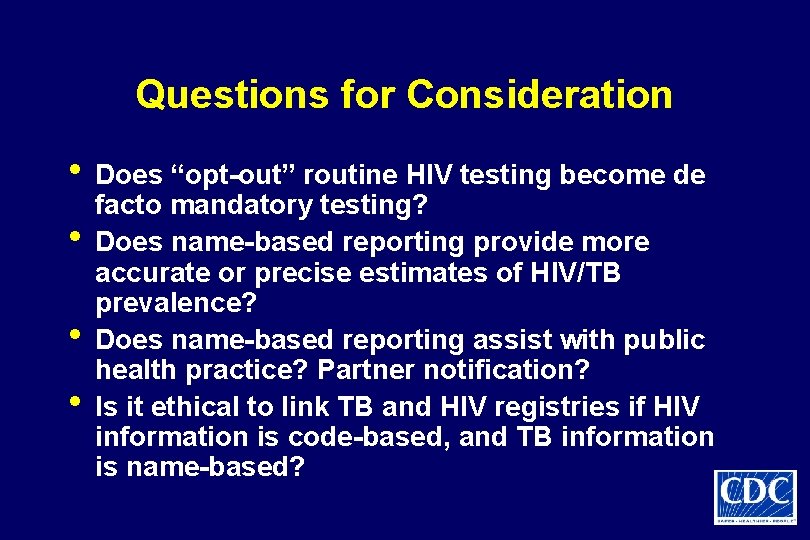
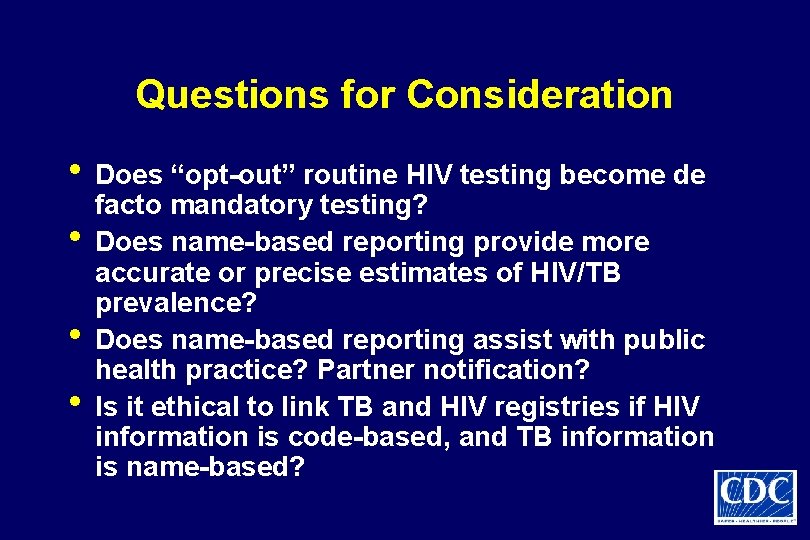
Questions for Consideration • Does “opt-out” routine HIV testing become de • • • facto mandatory testing? Does name-based reporting provide more accurate or precise estimates of HIV/TB prevalence? Does name-based reporting assist with public health practice? Partner notification? Is it ethical to link TB and HIV registries if HIV information is code-based, and TB information is name-based?
References • • International Guidelines for Ethical Review of Epidemiological Studies. Bankowski Z, Ed. Geneva: Council for International Organizations of Medical Sciences, 1991. ISBN 92 9036 048 8. International Ethical Guidelines for Biomedical Research Involving Human Subjects. Bankowski Z, Ed. Geneva: Council for International Organizations of Medical Sciences, 2002 Rev. ISBN 92 9036 056 9. De Cock KM, et al. Lancet 2002; 360: 67 -72. Fairchild AL, Bayer R. Science 2004; 303: 631 -632. London L. Amer J Public Health 2002; 92: 1079 -1084. Mac. Queen KM, Buehler JW. Amer J Public Health 2004; 94: 928 -931. Roberts MJ, Reich MR. Lancet 2002; 359: 1055 -1059.
 Ethical media issues
Ethical media issues Law and ethics in information security
Law and ethics in information security The perceived relevance or importance of an ethical issue
The perceived relevance or importance of an ethical issue Negative rights vs positive rights
Negative rights vs positive rights Duties towards self
Duties towards self Legal rights vs moral rights
Legal rights vs moral rights Positive rights and negative rights
Positive rights and negative rights Legal issues of ict in education
Legal issues of ict in education Ethical and legal issues in e-business
Ethical and legal issues in e-business Legal and ethical issues in computer security
Legal and ethical issues in computer security Professional and ethical issues during internship
Professional and ethical issues during internship Itgs social ethical issues
Itgs social ethical issues Ethical issues in accounting and finance
Ethical issues in accounting and finance Key technology trends that raise ethical issues
Key technology trends that raise ethical issues Ethical and legal issues chapter 2
Ethical and legal issues chapter 2 Ethical and social issues in information systems doc
Ethical and social issues in information systems doc Chapter 3 medical legal and ethical issues
Chapter 3 medical legal and ethical issues Chapter 3 legal and ethical issues
Chapter 3 legal and ethical issues Legal and ethical issues in computer security
Legal and ethical issues in computer security How ethical social and political issues are connected
How ethical social and political issues are connected Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Legal and ethical issues chapter 3
Legal and ethical issues chapter 3 Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Chapter 5 legal and ethical responsibilities
Chapter 5 legal and ethical responsibilities Chapter 4 ethical and social issues in information systems
Chapter 4 ethical and social issues in information systems Nflpn code of ethics
Nflpn code of ethics Ethical and legal issues chapter 2
Ethical and legal issues chapter 2 Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 5 legal and ethical issues
Chapter 5 legal and ethical issues Ethical and legal issues affecting the nursing assistant
Ethical and legal issues affecting the nursing assistant What is the difference between ethical and legal issues
What is the difference between ethical and legal issues