Essentials of Human Anatomy Physiology Unit 8 1
- Slides: 33
Essentials of Human Anatomy & Physiology Unit 8. 1 Blood
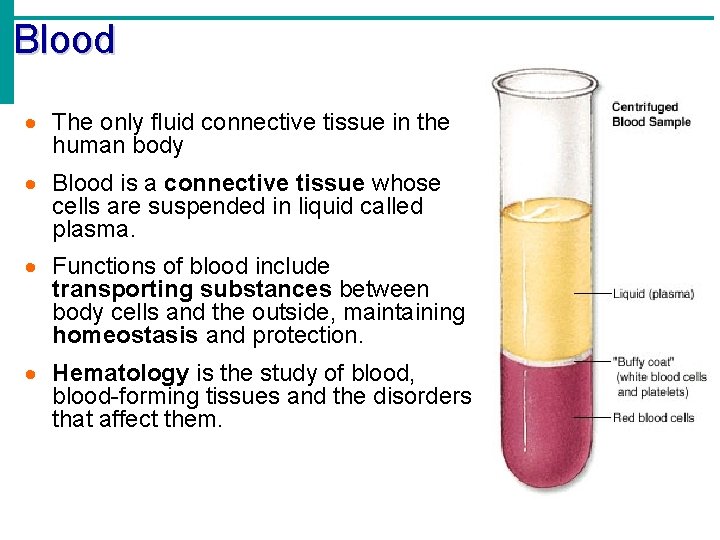
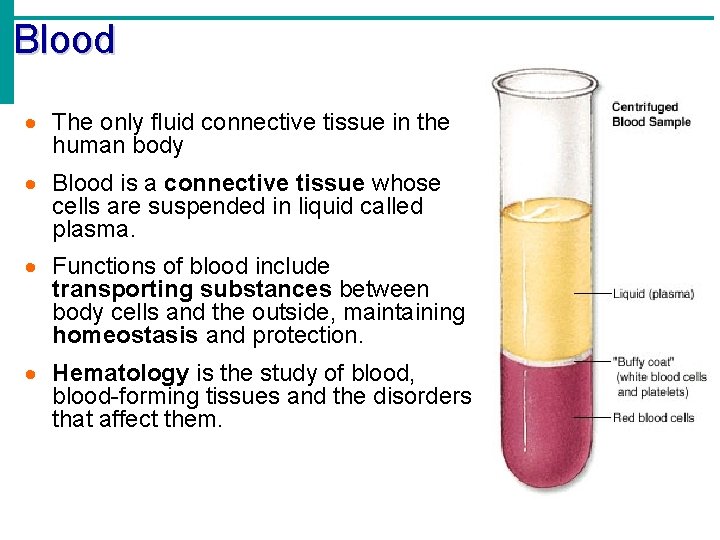
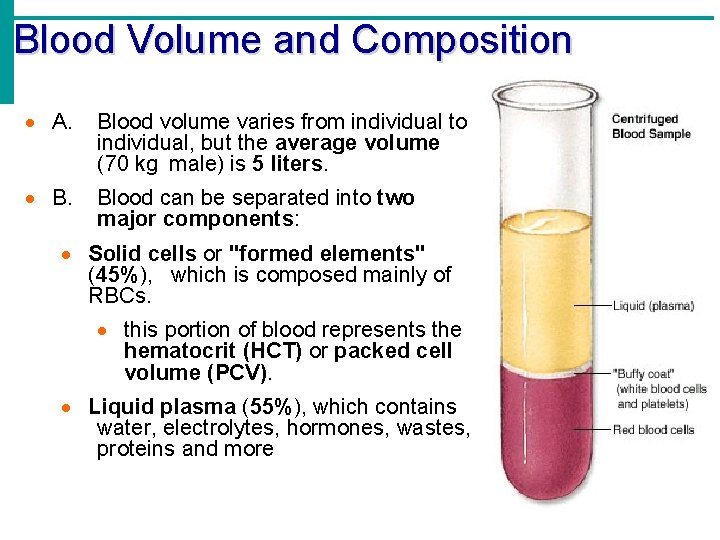
Blood · The only fluid connective tissue in the human body · Blood is a connective tissue whose cells are suspended in liquid called plasma. · Functions of blood include transporting substances between body cells and the outside, maintaining homeostasis and protection. · Hematology is the study of blood, blood-forming tissues and the disorders that affect them.
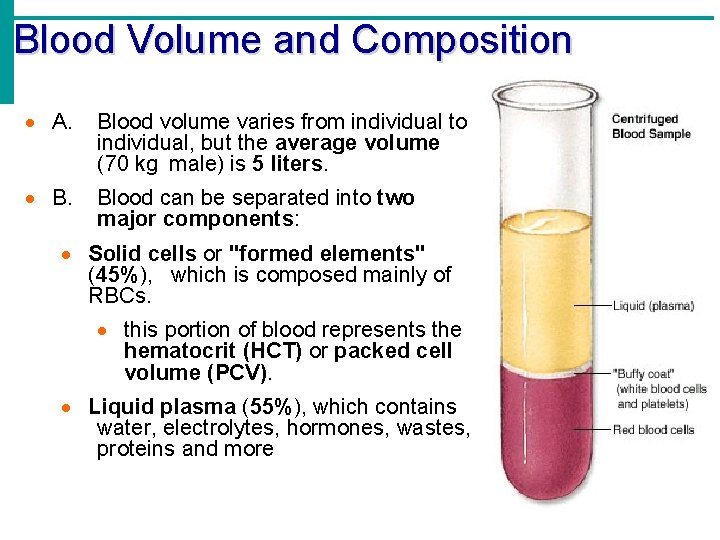
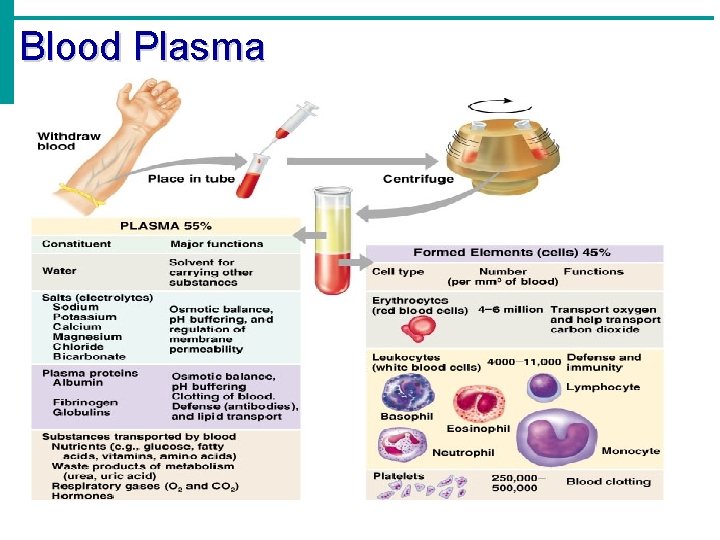
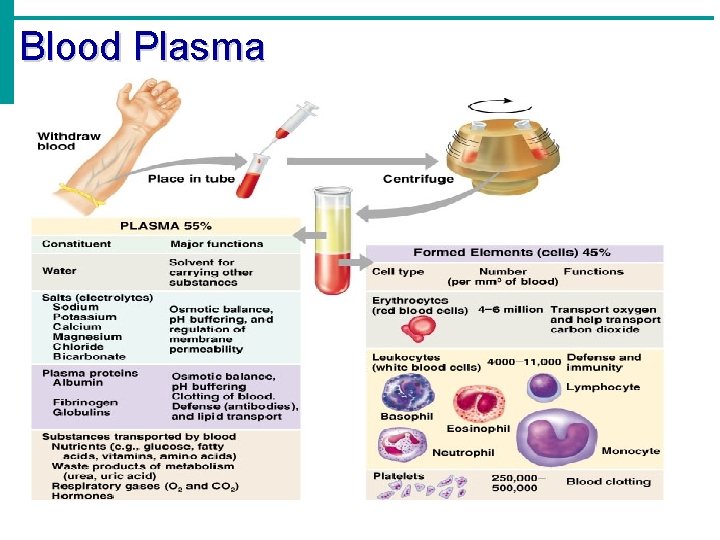
Blood Volume and Composition · A. Blood volume varies from individual to individual, but the average volume (70 kg male) is 5 liters. · B. Blood can be separated into two major components: · Solid cells or "formed elements" (45%), which is composed mainly of RBCs. · this portion of blood represents the hematocrit (HCT) or packed cell volume (PCV). · Liquid plasma (55%), which contains water, electrolytes, hormones, wastes, proteins and more
Physical Characteristics • Thicker (more viscous) than water and flows more slowly than water • Temperature of 100. 4 degrees F • p. H 7. 4 (7. 35 -7. 45) • 8 % of total body weight
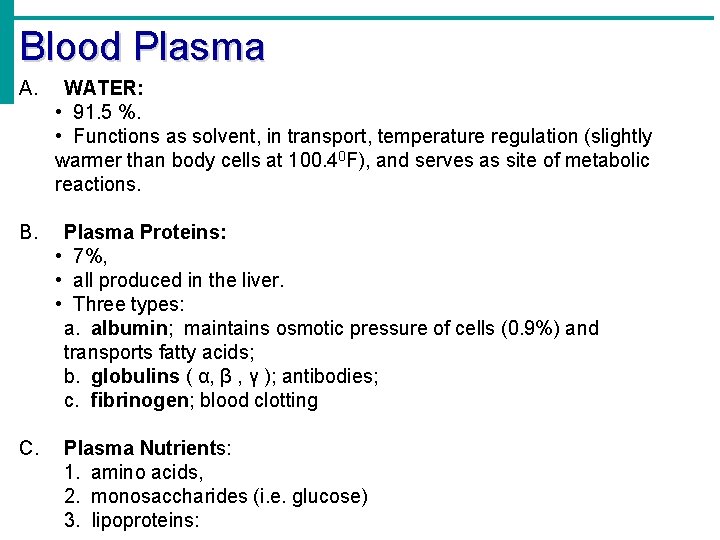
Blood Plasma A. WATER: • 91. 5 %. • Functions as solvent, in transport, temperature regulation (slightly warmer than body cells at 100. 40 F), and serves as site of metabolic reactions. B. Plasma Proteins: • 7%, • all produced in the liver. • Three types: a. albumin; maintains osmotic pressure of cells (0. 9%) and transports fatty acids; b. globulins ( α, β , γ ); antibodies; c. fibrinogen; blood clotting C. Plasma Nutrients: 1. amino acids, 2. monosaccharides (i. e. glucose) 3. lipoproteins:
Blood Plasma D. Plasma Wastes: 1. urea (amino acid metabolism), 2. uric acid (nucleotide metabolism), 3. creatinine (creatine metabolism), 4. creatine (CP to recycle ADP to ATP in muscle & brain), 5. bilirubin (hemoglobin metabolism). E. Plasma Gases: 1. oxygen (needed for cellular respiration), 2. carbon dioxide (produced by cell respiration), 3. nitrogen (use unknown) F. Plasma Electrolytes: 1. include sodium, potassium, calcium, magnesium, chloride, bicarbonate, phosphate, and sulphate; 2. Maintain osmotic pressure, Resting Membrane Potential, and p. H. G. Regulatory Substances: 1. enzymes, 2. hormones.
Blood Plasma
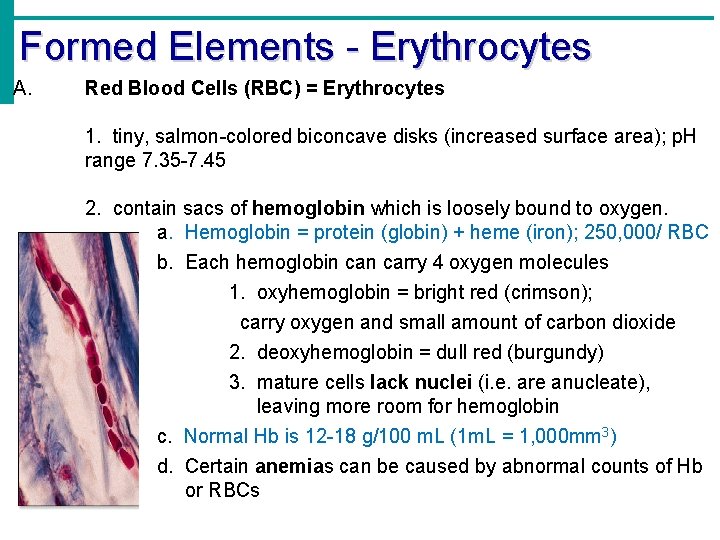
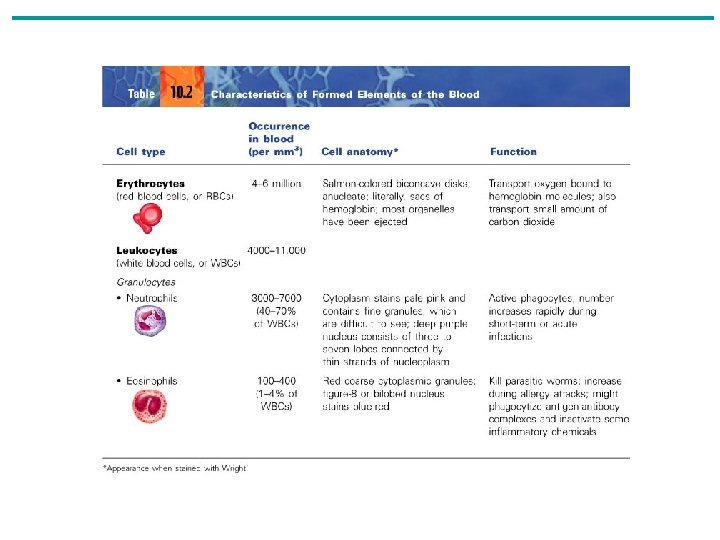
Formed Elements - Erythrocytes A. Red Blood Cells (RBC) = Erythrocytes 1. tiny, salmon-colored biconcave disks (increased surface area); p. H range 7. 35 -7. 45 2. contain sacs of hemoglobin which is loosely bound to oxygen. a. Hemoglobin = protein (globin) + heme (iron); 250, 000/ RBC b. Each hemoglobin carry 4 oxygen molecules 1. oxyhemoglobin = bright red (crimson); carry oxygen and small amount of carbon dioxide 2. deoxyhemoglobin = dull red (burgundy) 3. mature cells lack nuclei (i. e. are anucleate), leaving more room for hemoglobin c. Normal Hb is 12 -18 g/100 m. L (1 m. L = 1, 000 mm 3) d. Certain anemias can be caused by abnormal counts of Hb or RBCs
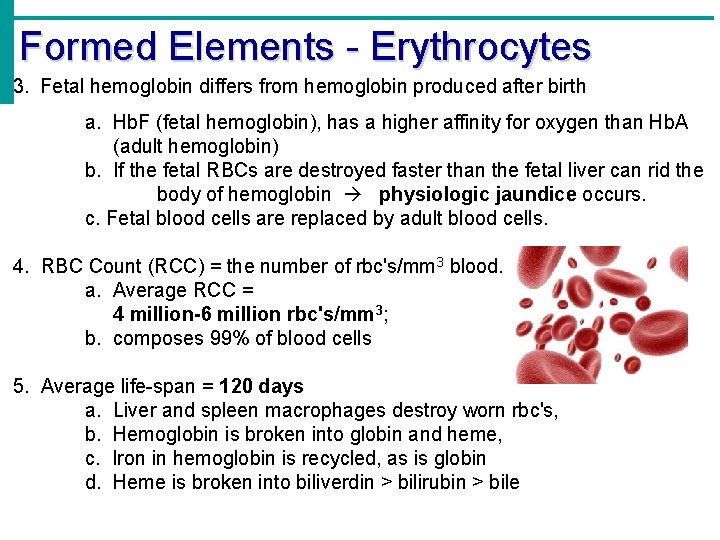
Formed Elements - Erythrocytes 3. Fetal hemoglobin differs from hemoglobin produced after birth a. Hb. F (fetal hemoglobin), has a higher affinity for oxygen than Hb. A (adult hemoglobin) b. If the fetal RBCs are destroyed faster than the fetal liver can rid the body of hemoglobin physiologic jaundice occurs. c. Fetal blood cells are replaced by adult blood cells. 4. RBC Count (RCC) = the number of rbc's/mm 3 blood. a. Average RCC = 4 million-6 million rbc's/mm 3; b. composes 99% of blood cells 5. Average life-span = 120 days a. Liver and spleen macrophages destroy worn rbc's, b. Hemoglobin is broken into globin and heme, c. Iron in hemoglobin is recycled, as is globin d. Heme is broken into biliverdin > bilirubin > bile
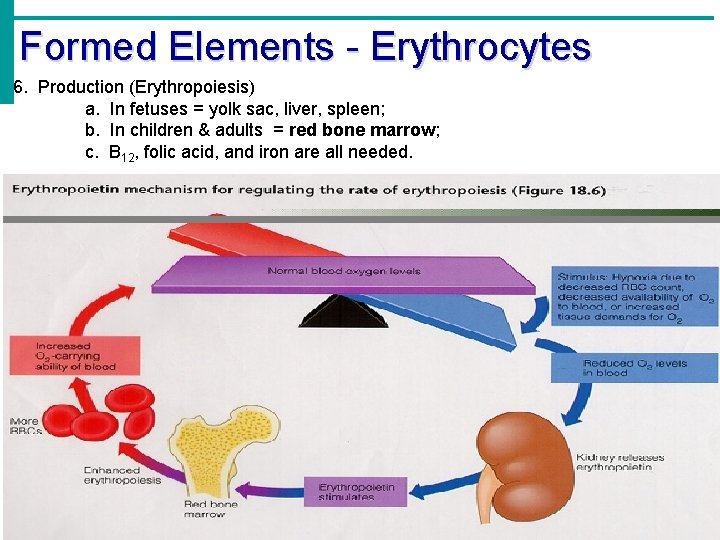
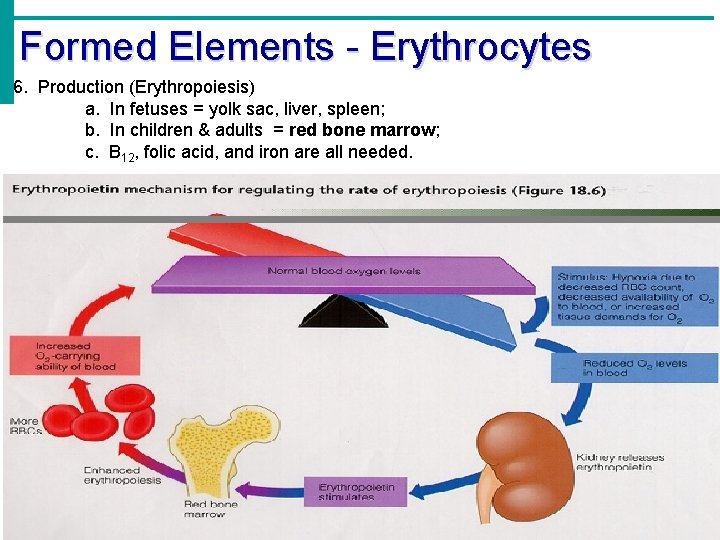
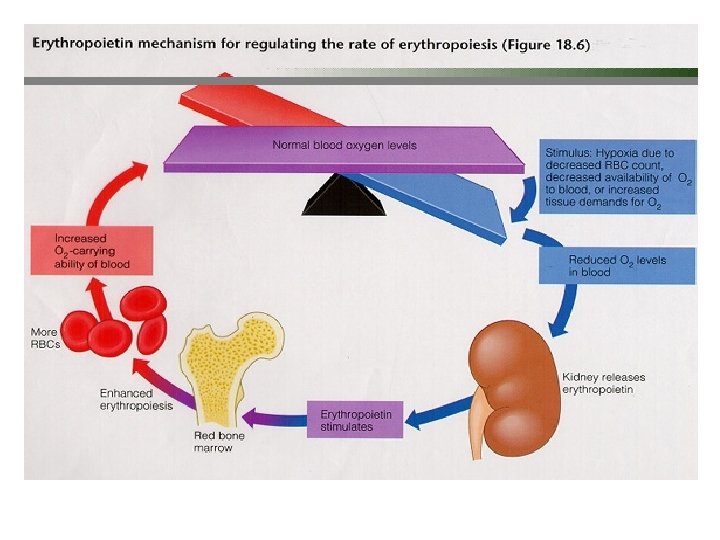
Formed Elements - Erythrocytes 6. Production (Erythropoiesis) a. In fetuses = yolk sac, liver, spleen; b. In children & adults = red bone marrow; c. B 12, folic acid, and iron are all needed.
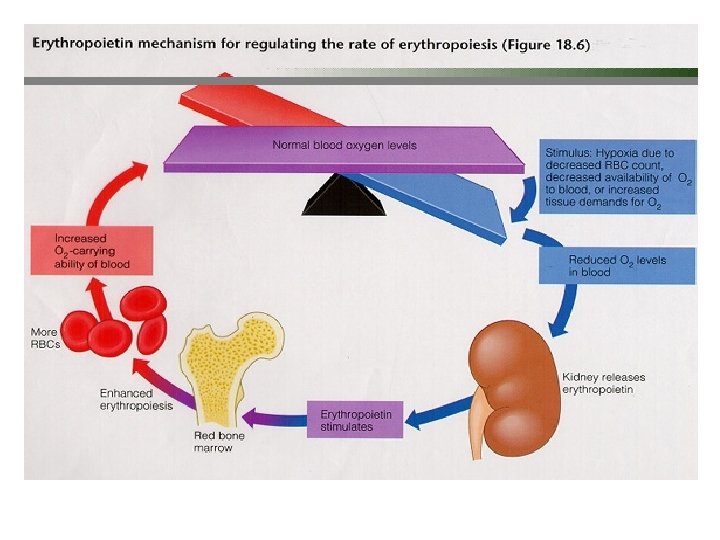
Formed Elements - Erythrocytes 7. Number of RBCs normally remains stable. a. Negative feedback mechanism involving the hormone erythropoietin, which is produced & secreted by special cells in the kidney b. Chemoreceptors in kidney and liver detect low blood oxygen, c. Erythropoietin is released from kidney and liver into circulation, d. Erythropoietin targets red bone marrow, stimulating erythropoiesis.
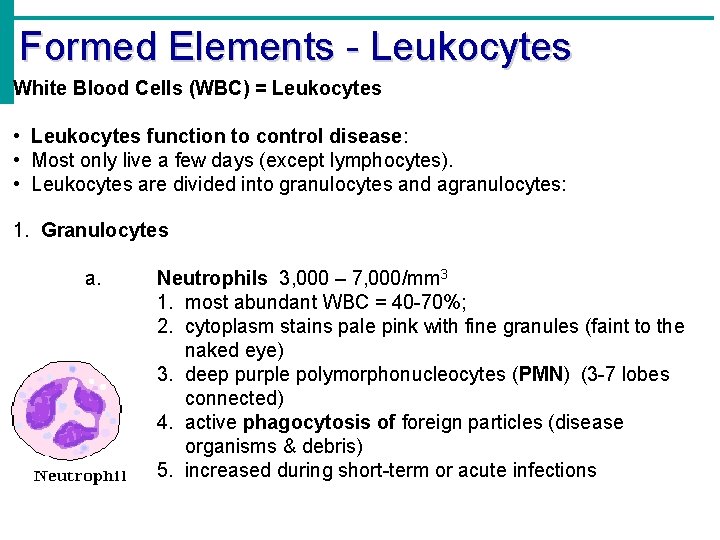
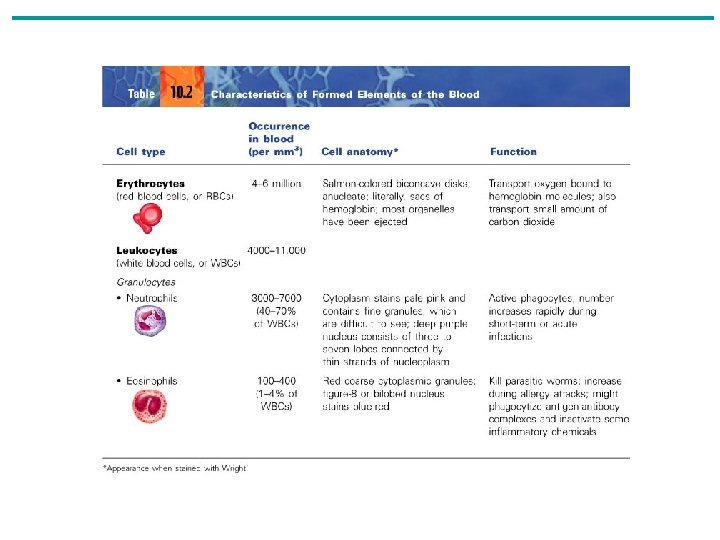
Formed Elements - Leukocytes White Blood Cells (WBC) = Leukocytes • Leukocytes function to control disease: • Most only live a few days (except lymphocytes). • Leukocytes are divided into granulocytes and agranulocytes: 1. Granulocytes a. Neutrophils 3, 000 – 7, 000/mm 3 1. most abundant WBC = 40 -70%; 2. cytoplasm stains pale pink with fine granules (faint to the naked eye) 3. deep purple polymorphonucleocytes (PMN) (3 -7 lobes connected) 4. active phagocytosis of foreign particles (disease organisms & debris) 5. increased during short-term or acute infections
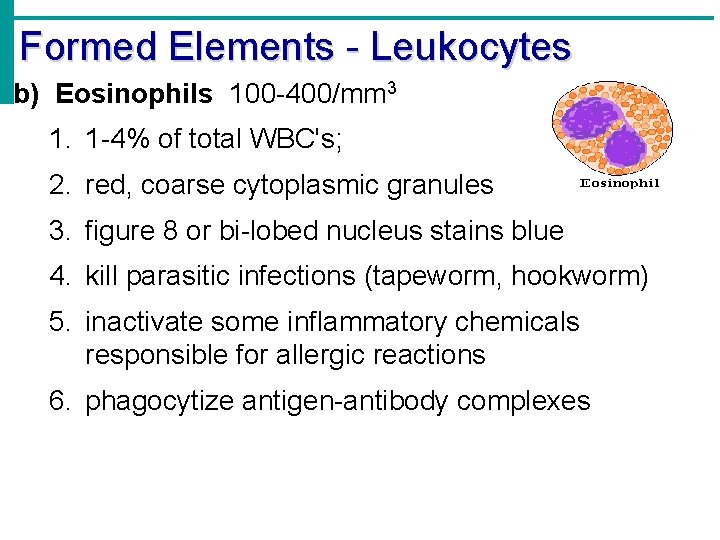
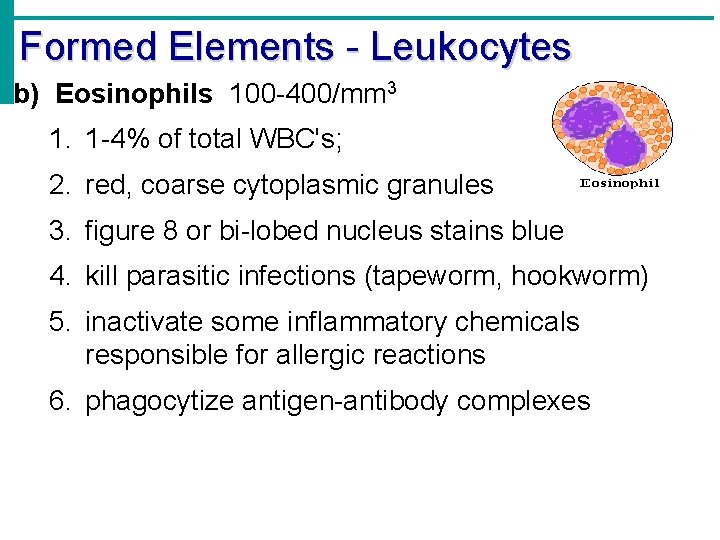
Formed Elements - Leukocytes b) Eosinophils 100 -400/mm 3 1. 1 -4% of total WBC's; 2. red, coarse cytoplasmic granules 3. figure 8 or bi-lobed nucleus stains blue 4. kill parasitic infections (tapeworm, hookworm) 5. inactivate some inflammatory chemicals responsible for allergic reactions 6. phagocytize antigen-antibody complexes
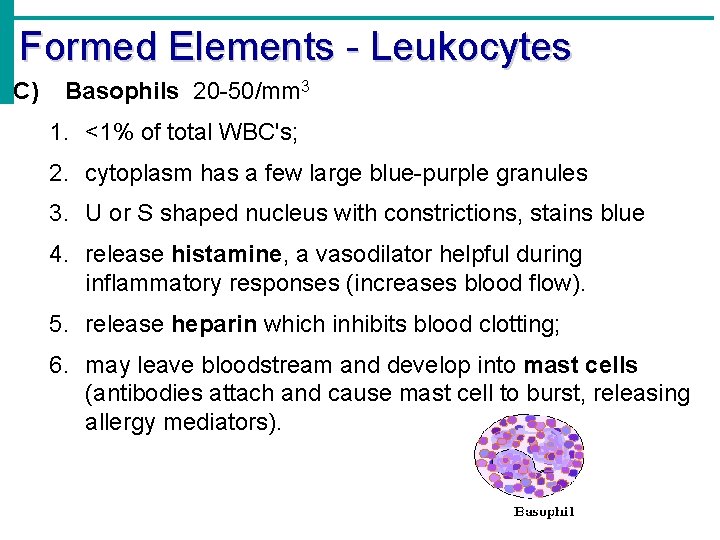
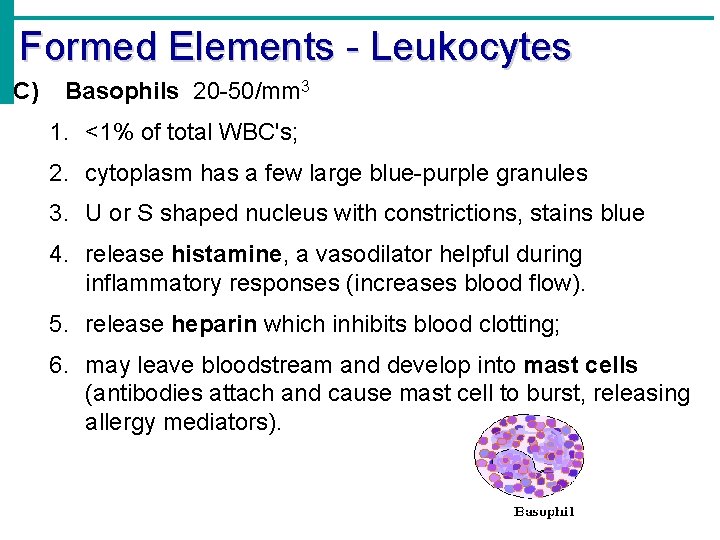
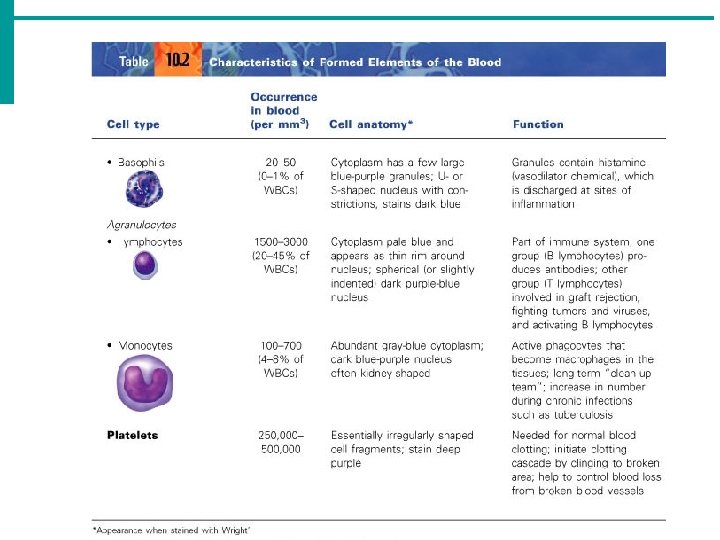
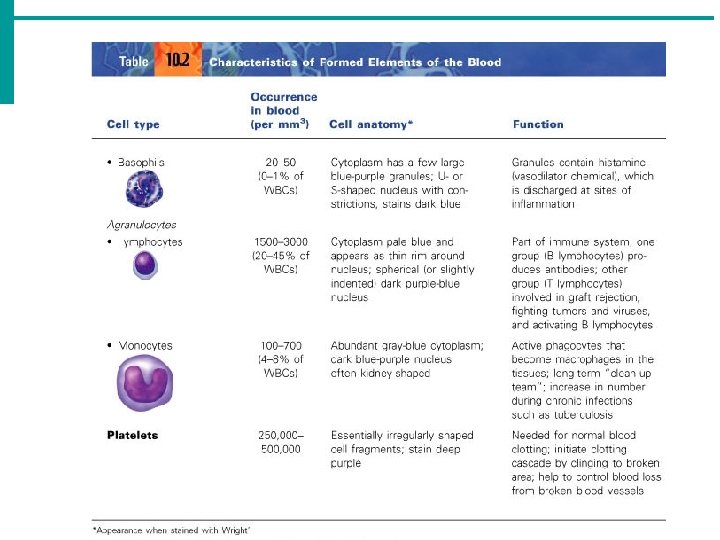
Formed Elements - Leukocytes C) Basophils 20 -50/mm 3 1. <1% of total WBC's; 2. cytoplasm has a few large blue-purple granules 3. U or S shaped nucleus with constrictions, stains blue 4. release histamine, a vasodilator helpful during inflammatory responses (increases blood flow). 5. release heparin which inhibits blood clotting; 6. may leave bloodstream and develop into mast cells (antibodies attach and cause mast cell to burst, releasing allergy mediators).
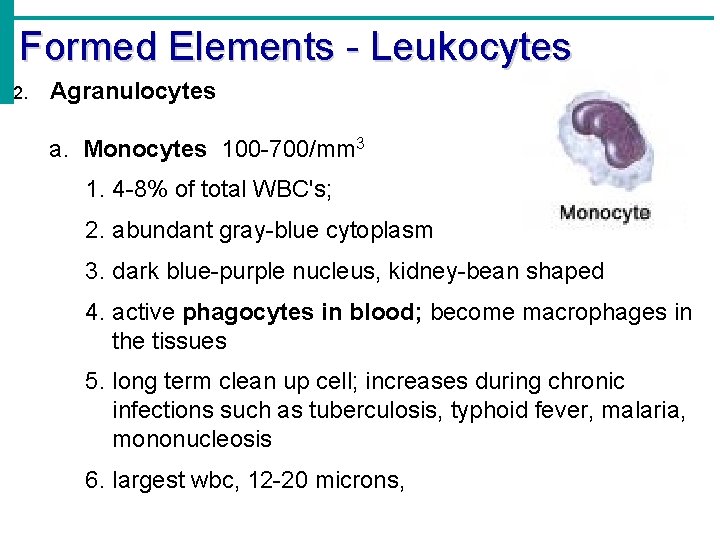
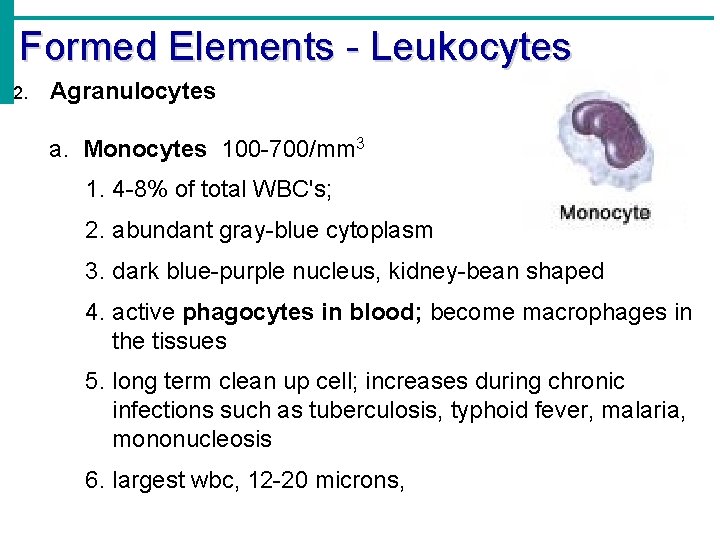
Formed Elements - Leukocytes 2. Agranulocytes a. Monocytes 100 -700/mm 3 1. 4 -8% of total WBC's; 2. abundant gray-blue cytoplasm 3. dark blue-purple nucleus, kidney-bean shaped 4. active phagocytes in blood; become macrophages in the tissues 5. long term clean up cell; increases during chronic infections such as tuberculosis, typhoid fever, malaria, mononucleosis 6. largest wbc, 12 -20 microns,
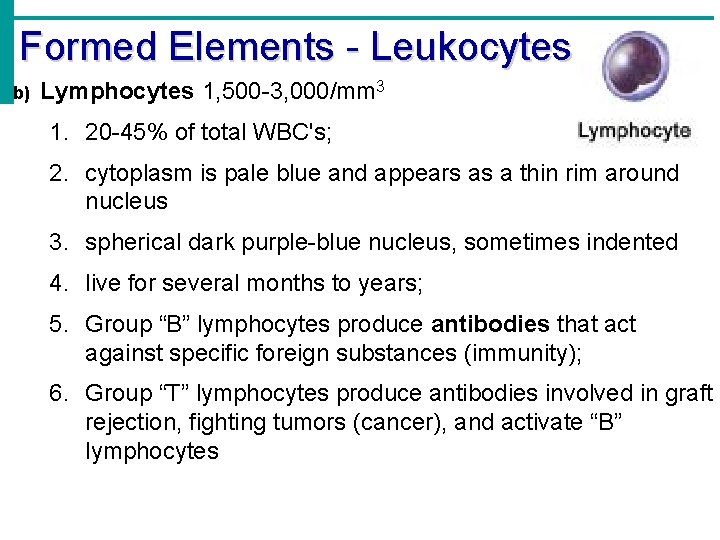
Formed Elements - Leukocytes b) Lymphocytes 1, 500 -3, 000/mm 3 1. 20 -45% of total WBC's; 2. cytoplasm is pale blue and appears as a thin rim around nucleus 3. spherical dark purple-blue nucleus, sometimes indented 4. live for several months to years; 5. Group “B” lymphocytes produce antibodies that act against specific foreign substances (immunity); 6. Group “T” lymphocytes produce antibodies involved in graft rejection, fighting tumors (cancer), and activate “B” lymphocytes
Formed Elements - Leukocytes 3. Average WBC count (WCC) = 4000 -11, 000 wbc's / mm 3 blood; a. Number of wbc's increases during infections; 1. leukocytosis = WCC > 11000; • Generally indicates an infection 2. leukopenia = WCC < 4000; • Commonly caused by certain drugs 4. Movement: a. Diapedesis = leukocytes move through blood vessel walls to enter tissues b. Amoeboid motion https: //www. youtube. com/watch? v=qx 8 v. HFw 6 Izk c. Chemotaxis
Formed Elements - Leukocytes 5. Leukocyte levels in the blood a. Leukemia = abnormal (uncontrolled) production of specific types of immature leukocytes • cancer of the bone marrow; causes a rapid increase in WBCs. these WBCs are immature and incapable of fighting infection. b. Leukocytosis (see above) c. Leukopenia (see above)
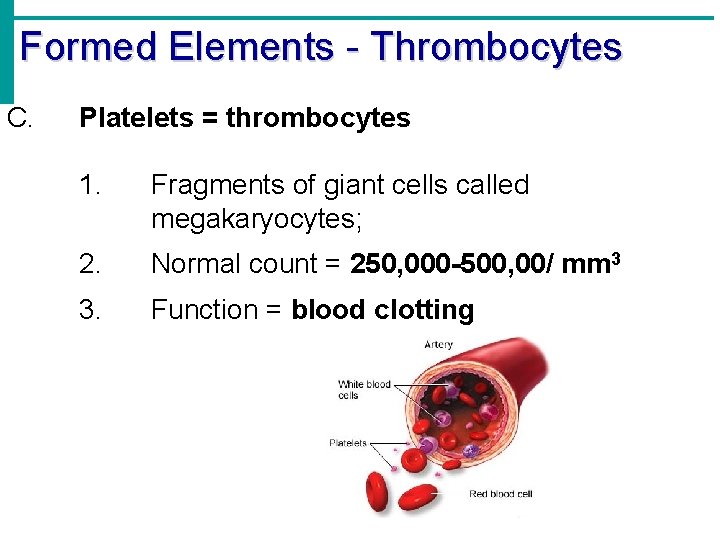
Formed Elements - Thrombocytes C. Platelets = thrombocytes 1. Fragments of giant cells called megakaryocytes; 2. Normal count = 250, 000 -500, 00/ mm 3 3. Function = blood clotting
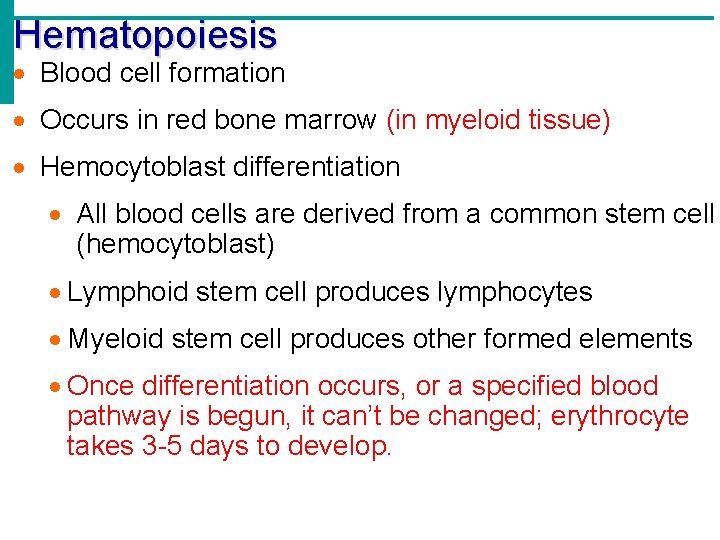
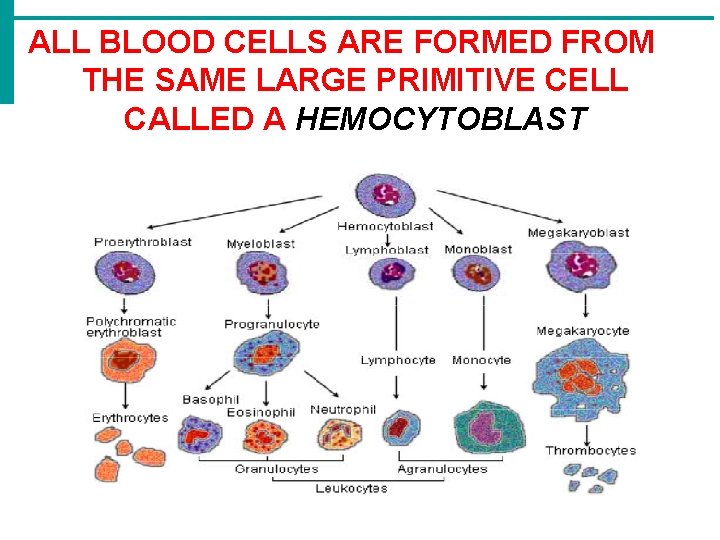
Hematopoiesis · Blood cell formation · Occurs in red bone marrow (in myeloid tissue) · Hemocytoblast differentiation · All blood cells are derived from a common stem cell (hemocytoblast) · Lymphoid stem cell produces lymphocytes · Myeloid stem cell produces other formed elements · Once differentiation occurs, or a specified blood pathway is begun, it can’t be changed; erythrocyte takes 3 -5 days to develop.
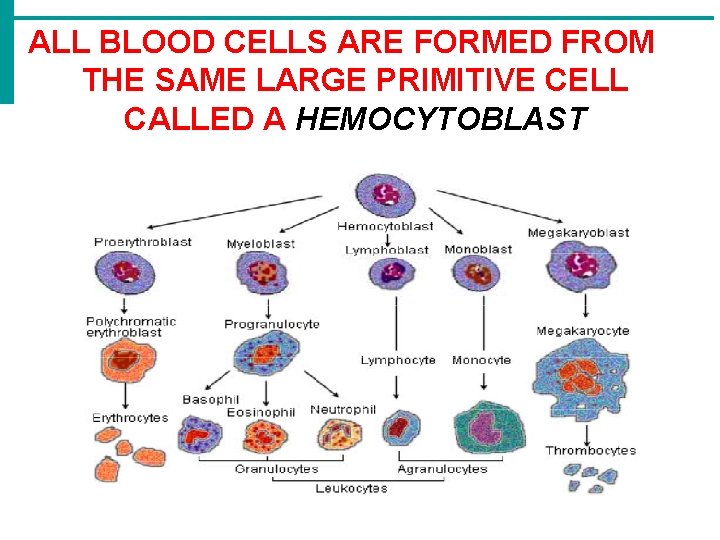
ALL BLOOD CELLS ARE FORMED FROM THE SAME LARGE PRIMITIVE CELL CALLED A HEMOCYTOBLAST
Blood Loss and Transfusions 1. Consequence of blood loss 15 -30 % Loss of 15 to 30 percent causes weakness > 30 % Loss of over 30 percent causes shock, which can be fatal 2. Blood transfusions must be of the same “type” of blood 3. The most vigorous transfusion reactions are caused by ABO and Rh blood group antigens 4. Hemolysis (rupture of RBCs) of the transfused blood occurs and hemoglobin is released 5. Transfusion reactions include fever, chills, nausea, vomiting, possible kidney failure (death) · Transfusions are the only way to replace blood quickly · Also given for severe anemia and thrombocytopenia
Blood Groups and Transfusions 1. There are genetically determined proteins called antigens present on the cell membrane surface of our erythrocytes 2. Our plasma contains substances called antibodies that are produced against nonself antigens · A foreign protein (also called an antigen) may be attacked by the immune system · The body will recognize its own antigens, but will attack another person’s RBC’s that contain different antigens. 3. If the RBC antigen (donor) and plasma antibody (recipient) are the same, the serious condition of hemolysis (bursting) of RBCs will occur a. In the laboratory, this situation can be simulated or “typed” by using antibodies that will cause blood with certain proteins to clump; however the result is termed agglutination = clumping of red blood cells. b. Non-self Antigen + self antibody = agglutination
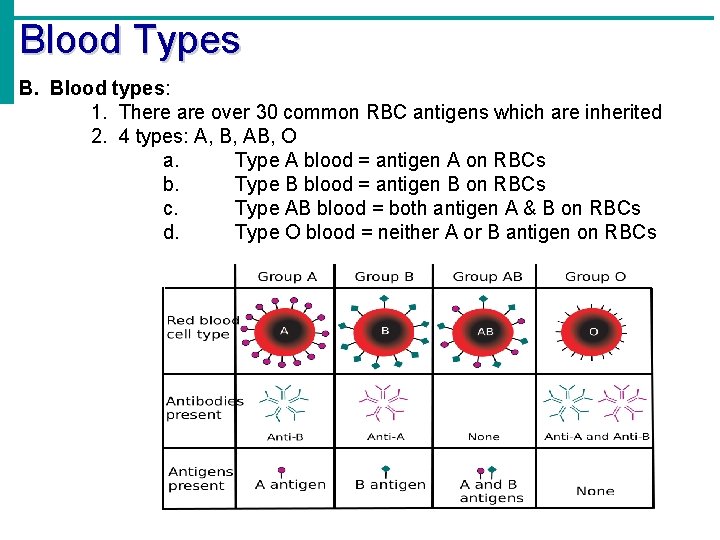
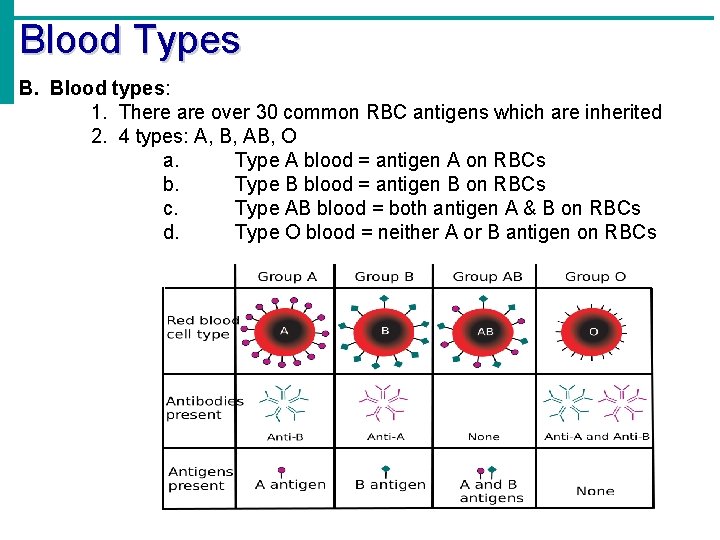
Blood Types B. Blood types: 1. There are over 30 common RBC antigens which are inherited 2. 4 types: A, B, AB, O a. Type A blood = antigen A on RBCs b. Type B blood = antigen B on RBCs c. Type AB blood = both antigen A & B on RBCs d. Type O blood = neither A or B antigen on RBCs
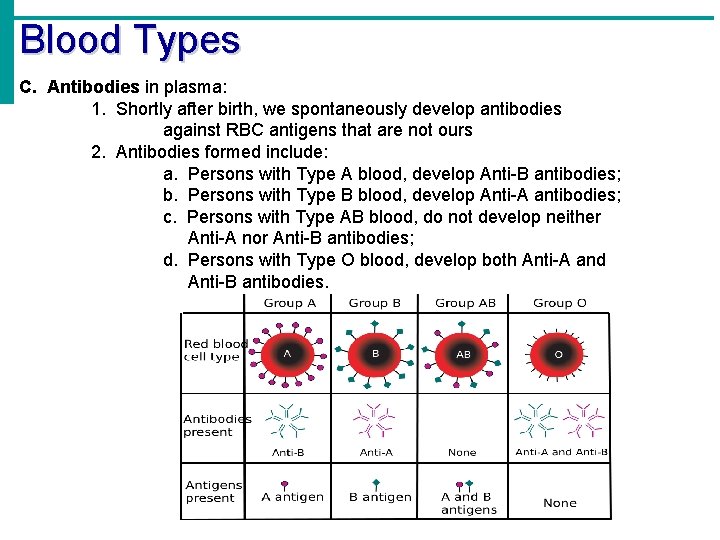
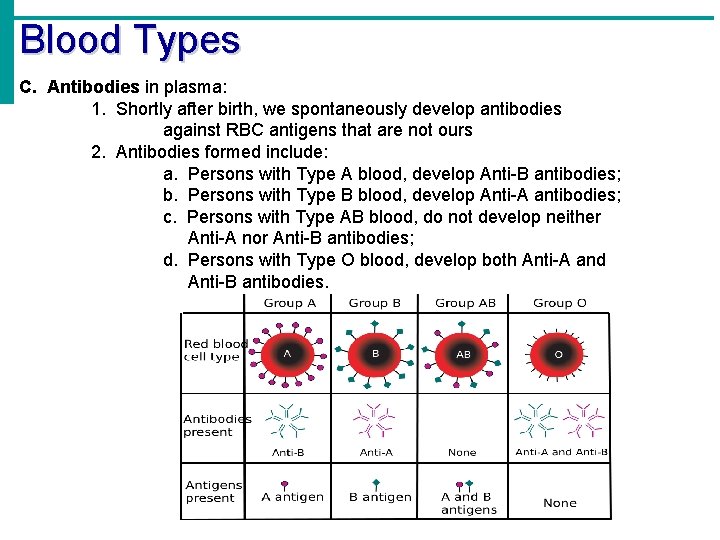
Blood Types C. Antibodies in plasma: 1. Shortly after birth, we spontaneously develop antibodies against RBC antigens that are not ours 2. Antibodies formed include: a. Persons with Type A blood, develop Anti-B antibodies; b. Persons with Type B blood, develop Anti-A antibodies; c. Persons with Type AB blood, do not develop neither Anti-A nor Anti-B antibodies; d. Persons with Type O blood, develop both Anti-A and Anti-B antibodies.
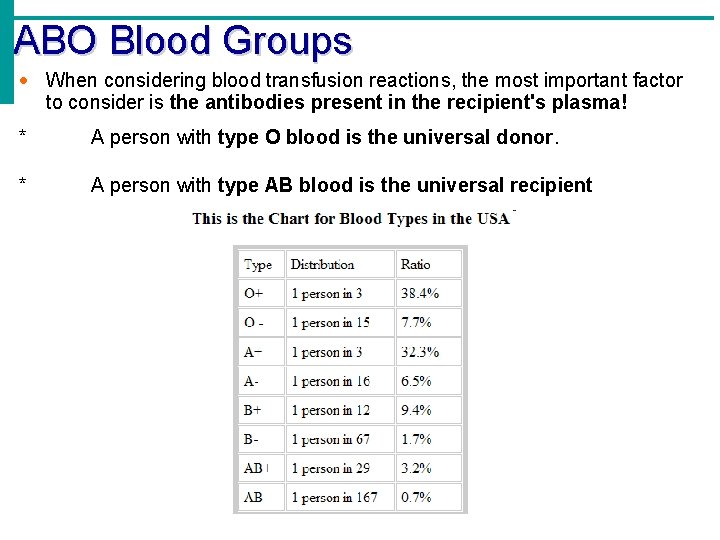
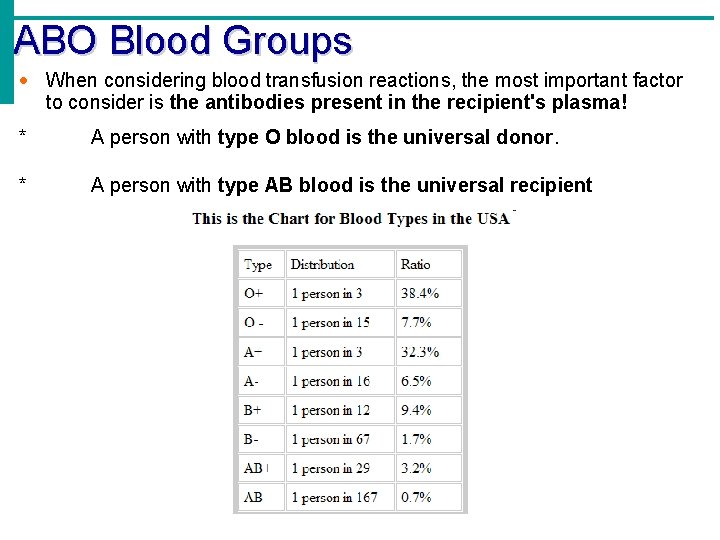
ABO Blood Groups · When considering blood transfusion reactions, the most important factor to consider is the antibodies present in the recipient's plasma! * A person with type O blood is the universal donor. * A person with type AB blood is the universal recipient
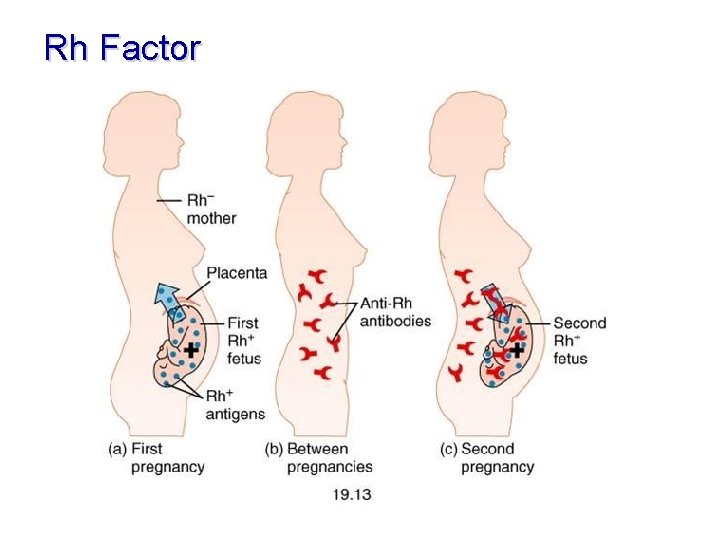
Rh Factor 1. Named because of the presence or absence of 1 -8 Rh antigens (agglutinogen D) 2. Most Americans are Rh+ (meaning they have 1 -8 Rh antigens) 3. Problems can occur in mixing Rh+ blood into a body with Rh– blood 4. Antibodies against the Rh proteins are not automatically formed in the blood of Rh- individuals. 5. Antibodies are only formed after exposure to the Rh antigen. What does this mean in terms of transfusions?
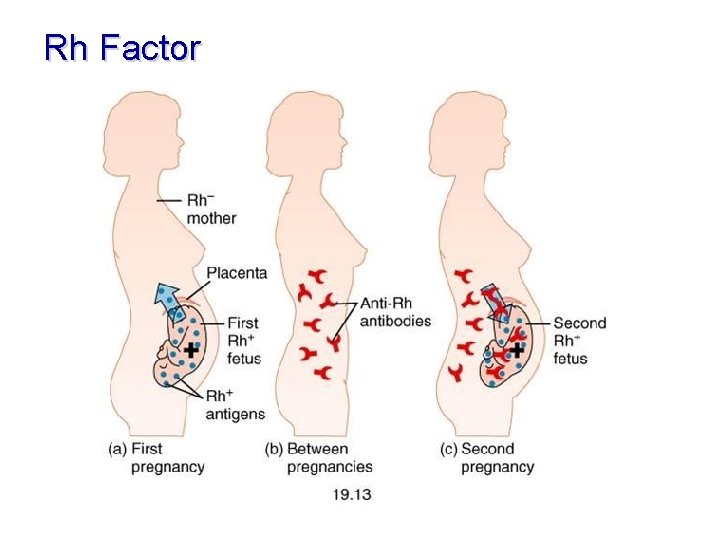
Rh Factor 6. Danger when the mother is Rh– and the father is Rh+, and the child inherits the Rh+ factor 7. The mismatch of an Rh– mother carrying an Rh+ baby can cause problems for the unborn child 8. The first pregnancy usually proceeds without problems because the mother doesn’t have anti-Rh antibodies 9. During birth Rh+ antigens pass to mother’s blood stream from placenta. 10. The immune system is sensitized after the first pregnancy
Rh Factor 11. In a second pregnancy, the mother’s immune system produces antibodies to attack the Rh+ blood 12. Called hemolytic disease of the newborn or erythroblastosis fetalis and can cause anemia, hypoxia, brain damage, and death without fetal transfusions. 13. To avoid hemolytic disease in future pregnancies Rho. GAM, an immune serum that prevents the formation of anti-Rh antibodies, can be given. How the Body Works : The Rh Factor http: //www. youtube. com/watch? v=7 OWp 8 d 8 WKkg&feature=related
Rh Factor