Essentials for Anesthesiologists Historical Overview of CPR Guideline






















- Slides: 56
Essentials for Anesthesiologists: “Historical Overview of CPR Guideline: G 2005, G 2010 then G 2015 “ Annual Meeting of Vietnam Society of Anesthesiologists 2016, June 23, 24 @Quy Nhon, Vietnam International Liaison Committee on Resuscitation Keiichi TADA MD, Ph. D Deputy Director & Board of Trustee Hamawaki Orthopaedic Hospital Hiroshima, Japan Board of Japan Resuscitation Council
Let’s Talk about CPR

By the way・・・・・・ What was the major emphasis of G 2005 and G 2010? ? ?

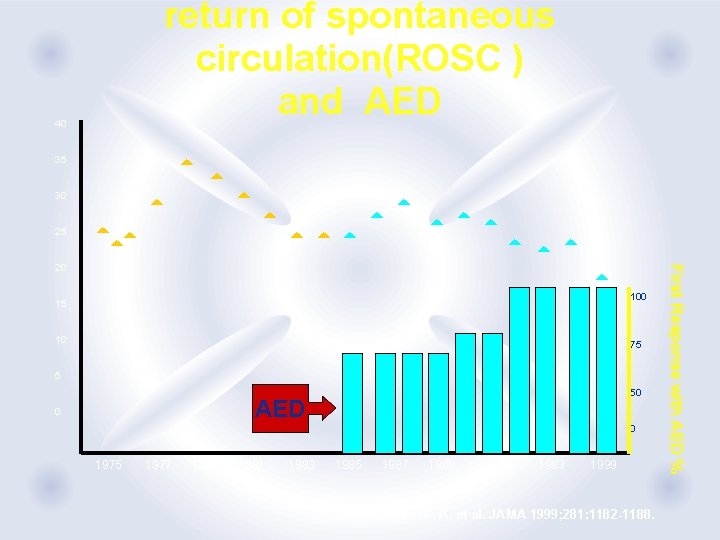
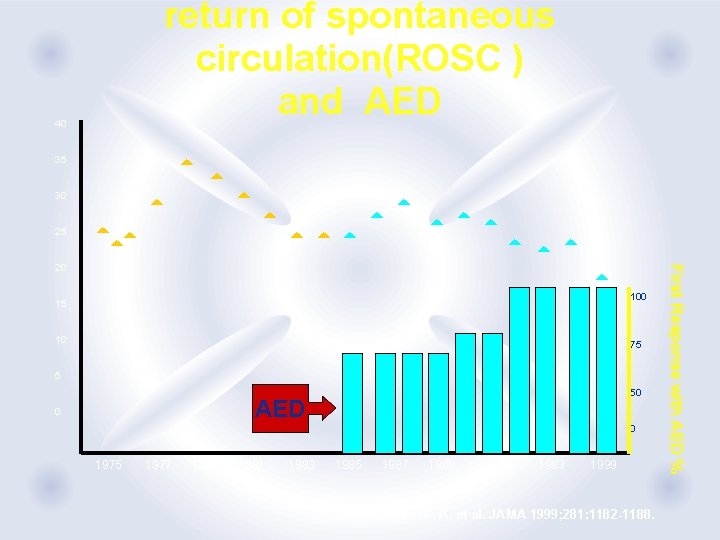
return of spontaneous circulation(ROSC ) and AED 40 35 30 25 100 15 10 75 5 50 AED 0 0 1975 1977 1979 1981 1983 1985 1987 1989 1991 1993 1999 Cobb, L. A. et al. JAMA 1999; 281: 1182 -1188. First Response with AED % 20
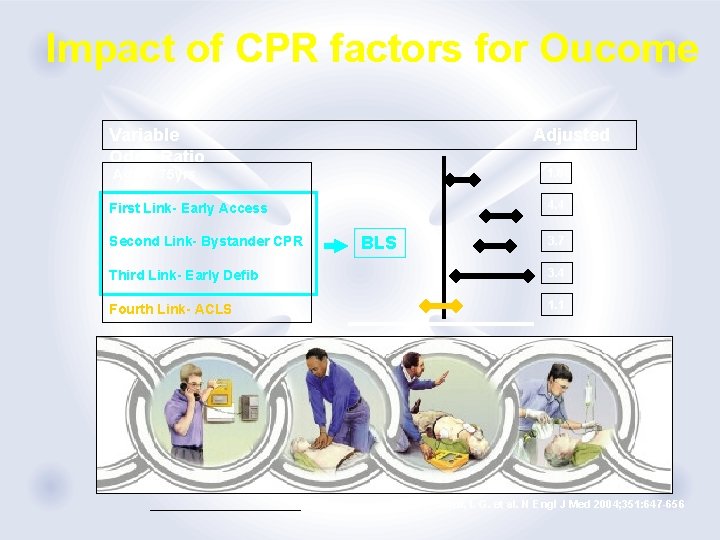
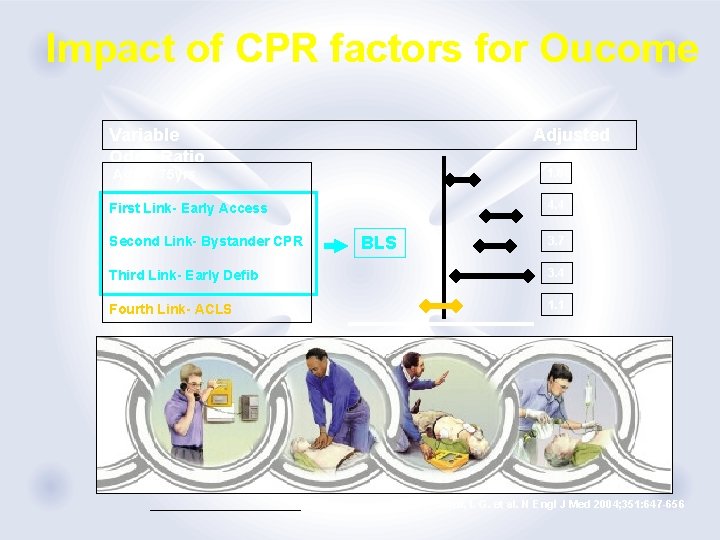
Impact of CPR factors for Oucome Variable Odds Ratio Adjusted 1. 6 Age < 75 yrs 4. 4 First Link- Early Access Second Link- Bystander CPR BLS 3. 7 Third Link- Early Defib 3. 4 Fourth Link- ACLS 1. 1 Stiell, I. G. et al. N Engl J Med 2004; 351: 647 -656
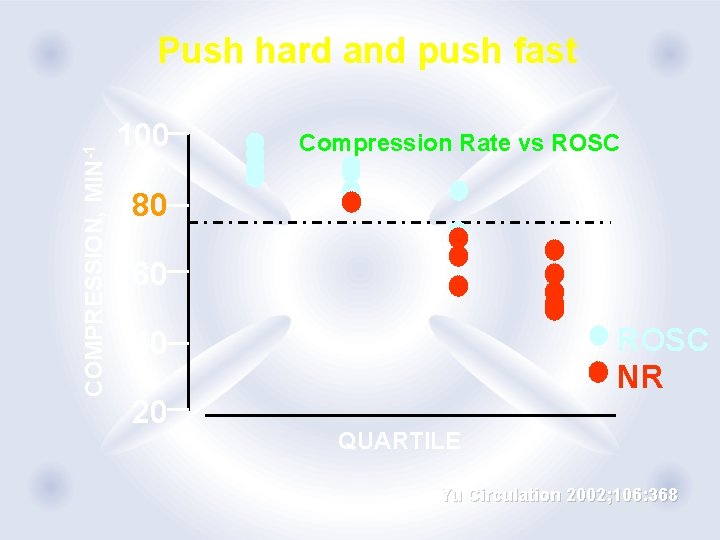
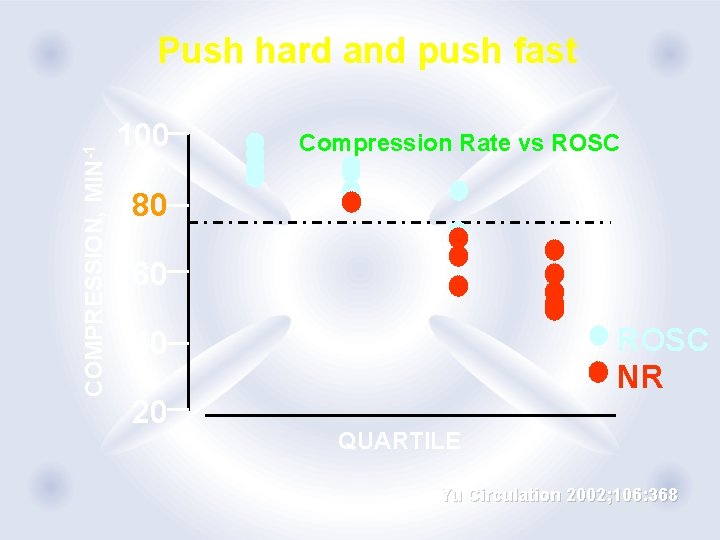
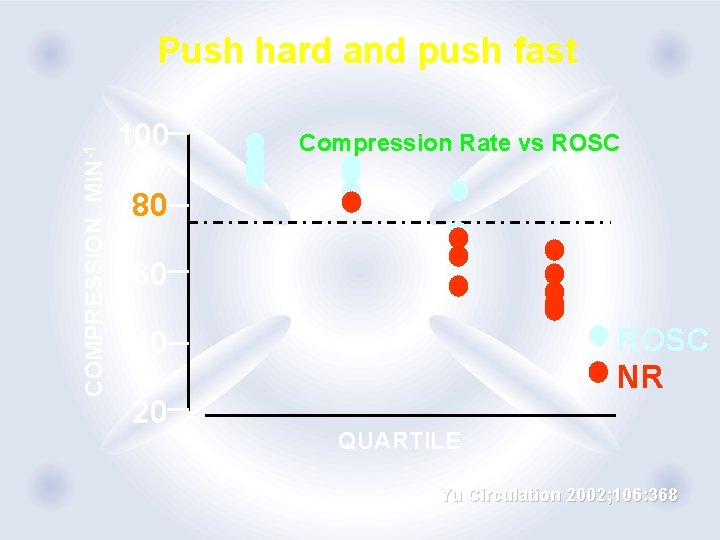
COMPRESSION, MIN-1 Push hard and push fast 100 Compression Rate vs ROSC 80 60 ROSC NR 40 20 QUARTILE Yu Circulation 2002; 106: 368

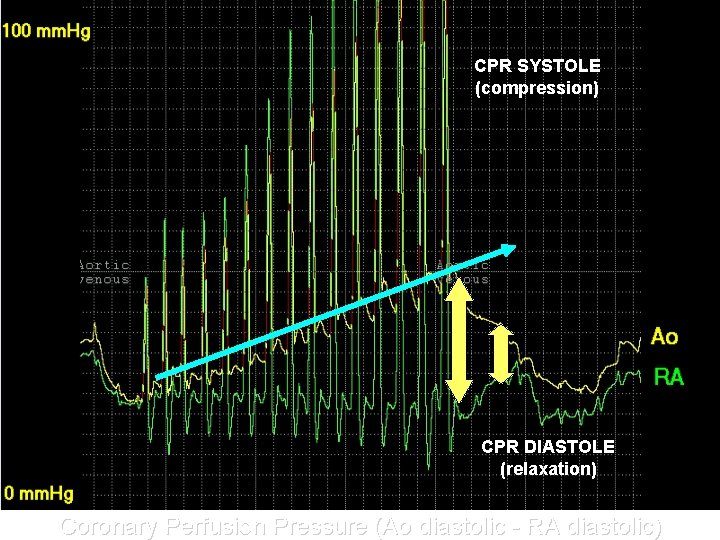
CPR SYSTOLE (compression) CPR DIASTOLE (relaxation) Coronary Perfusion Pressure (Ao diastolic - RA diastolic)
Essentials for Anesthesiologists: “Historical Overview of CPR Guideline: G 2005, G 2010 then G 2015 “ Annual Meeting of Vietnam Society of Anesthesiologists 2016, June 23, 24 @Quy Nhon, Vietnam International Liaison Committee on Resuscitation Keiichi TADA MD, Ph. D Deputy Director & Board of Trustee Hamawaki Orthopaedic Hospital Hiroshima, Japan Board of Japan Resuscitation Council
Let’s Talk about CPR
By the way・・・・・・ What was the major emphasis of G 2005 and G 2010? ? ?


return of spontaneous circulation(ROSC ) and AED 40 35 30 25 100 15 10 75 5 50 AED 0 0 1975 1977 1979 1981 1983 1985 1987 1989 1991 1993 1999 Cobb, L. A. et al. JAMA 1999; 281: 1182 -1188. First Response with AED % 20

Impact of CPR factors for Oucome Variable Odds Ratio Adjusted 1. 6 Age < 75 yrs 4. 4 First Link- Early Access Second Link- Bystander CPR BLS 3. 7 Third Link- Early Defib 3. 4 Fourth Link- ACLS 1. 1 Stiell, I. G. et al. N Engl J Med 2004; 351: 647 -656
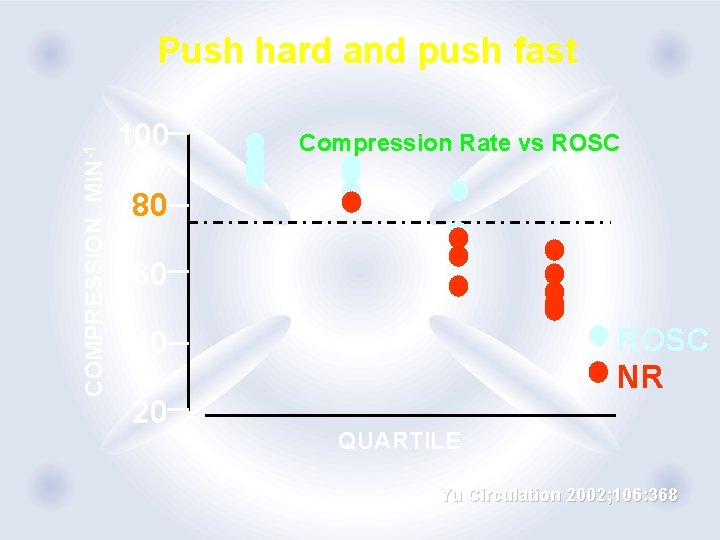
COMPRESSION, MIN-1 Push hard and push fast 100 Compression Rate vs ROSC 80 60 ROSC NR 40 20 QUARTILE Yu Circulation 2002; 106: 368
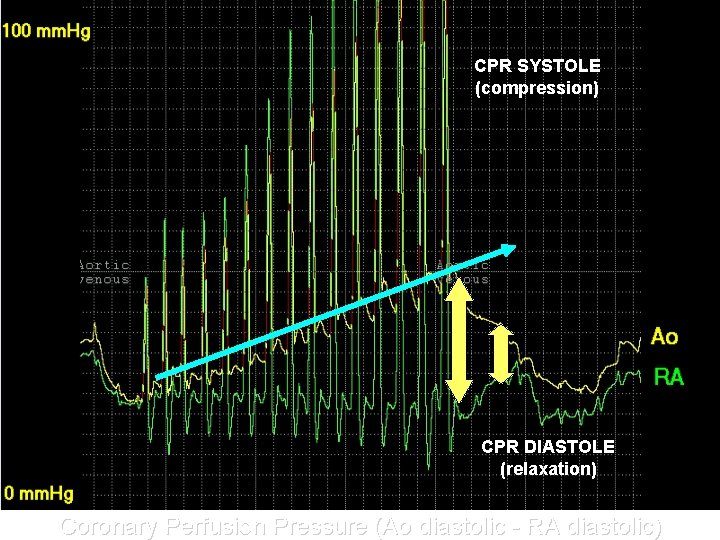
CPR SYSTOLE (compression) CPR DIASTOLE (relaxation) Coronary Perfusion Pressure (Ao diastolic - RA diastolic)
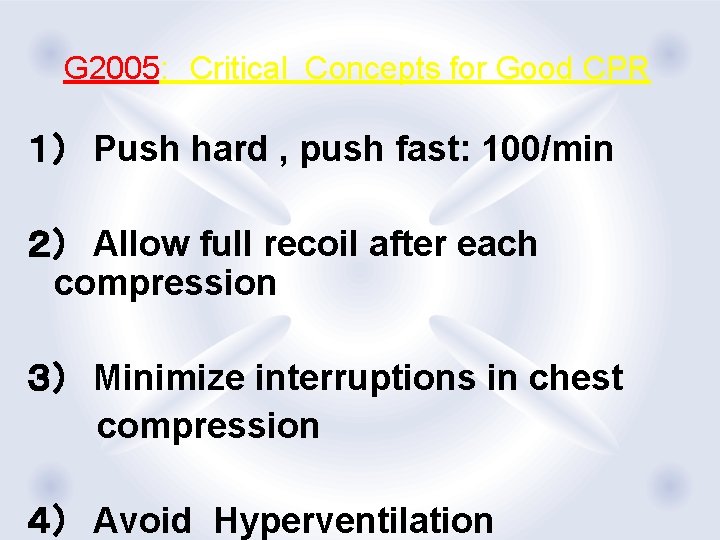
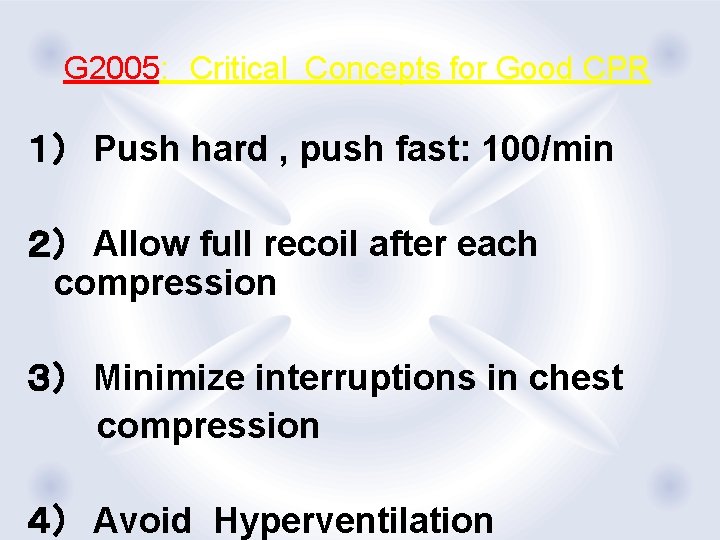
G 2005: Critical Concepts for Good CPR 1) Push hard , push fast: 100/min 2) Allow full recoil after each compression 3) Minimize interruptions in chest compression 4) Avoid Hyperventilation
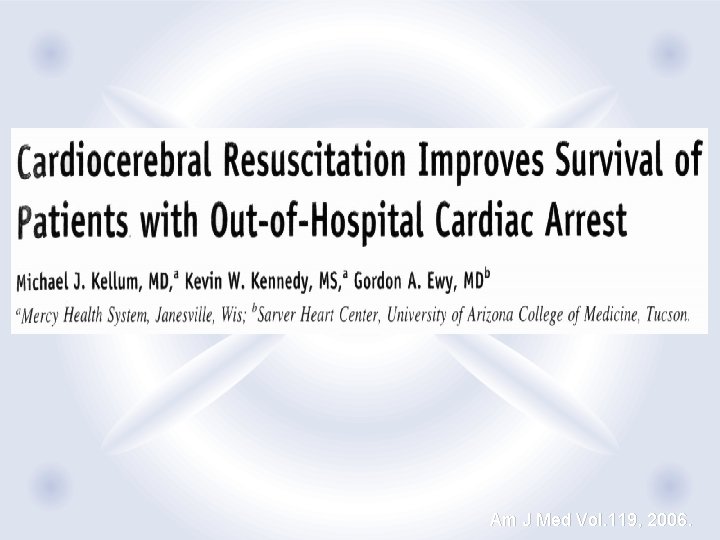
Am J Med Vol. 119, 2006.

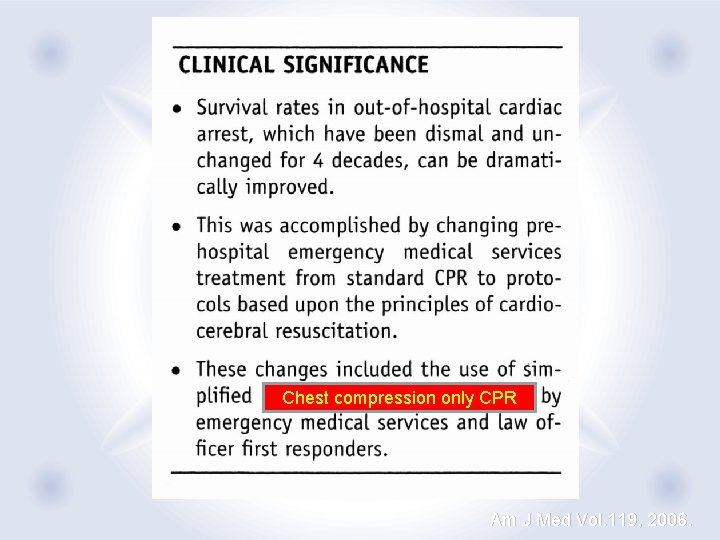
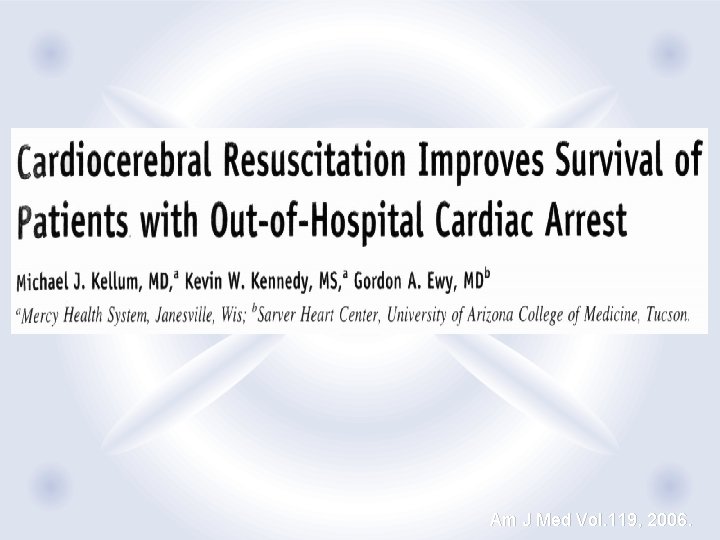
“Cardiocerebral Resuscitation improves Survival of Patients with Out-of-Hospital Cardiac Arrest” Michael J. Kellum et. al. : The American Journal of Medicine, 2006, vol 119. p. 335 -340 200 uninterrupted chest compression Single shock No post shock rhythm and pulse check Result: 1) Preceding 3 years: 92 shockable VF patients 18(20%) survived, 14(15%) CNS Intact 2) New Protocol Group: 33 shockable VF patients 200 uninterrupted 19(57%) chest survived, 16(48%) CNS Intact compression ** initial airway management was limited to an oral pharyngeal device and supplemental oxygen
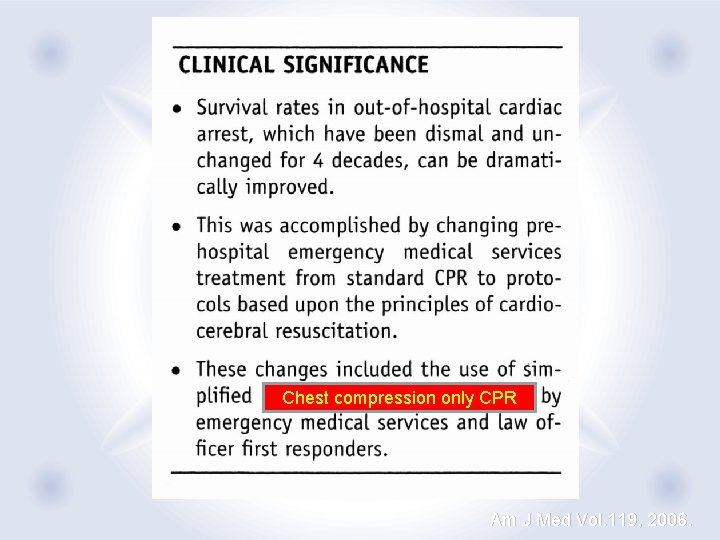
Chest compression only CPR Am J Med Vol. 119, 2006.

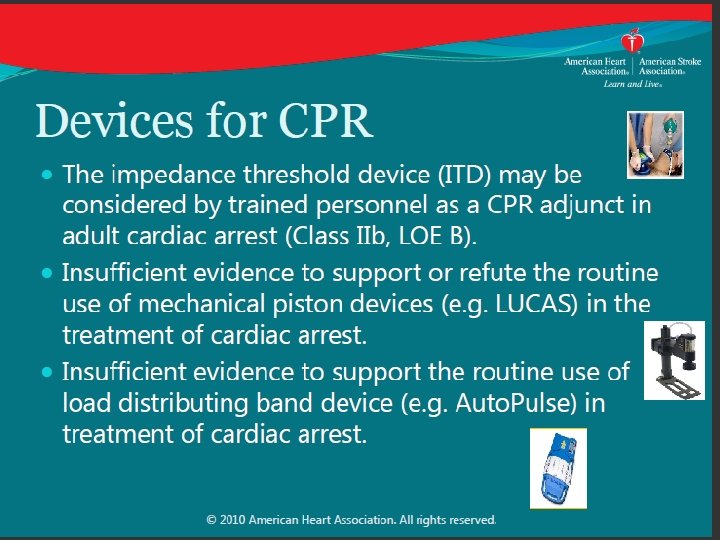
Scientific Knowledge Gaps Nadkarmi et al. Circulation 2007, 116 Since 2005 G・・・・ ① Medical emergency team rapid response teams increase outcome of adult& pediatric CPA patients?? ② Recognition of Cardiac Arrest and its causes Recognition of Agonal respiration ? ? , Detection of cardiac arrest ? ? Effectiveness of prone position? ? ? Quick detection of cervical spine injury ?? ③ Body position What is optimal position of patients during and post CPR ④ DC Shock: Optimal shock energy ? ? Optimal shock interval ? ? Long-term after-effect of DC shock for cardiac function ⑤ Blood Flow Generation compression-only CPR , effectiveness?? Effectiveness and safety of Autopulse & Airway Impedance Threshold Device ⑥ Airway Management・・・・・・・Best artificial AIRWAY ⑦ Compression & Respiration Optimal compression vs Respiration ratio ? ? For child? ? For neonate? ? ?? ⑧ Oxygenation How to give optimal oxygen in BLS ⑨ Drug: ⑩ Post CPR treatment Effectiveness of ECPR ? ? Optimal blood sugar level in and after CPR??










低体温のレベル -°C 36 -37=平常体温 36. 5 = 血管収縮 33 -36=軽度低体温 34 -35. 5 = シバリング Therapeutic Hypothermia After Cardiac Arrest < 34. 0 = NO SHIVERING! 26 -32=中等度低体温 13 -25=重度低体温 12>超低体温

G 2015 !!!
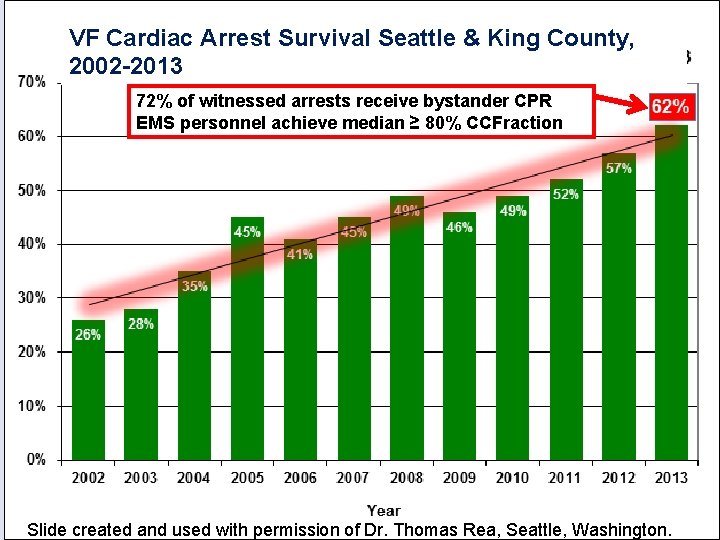
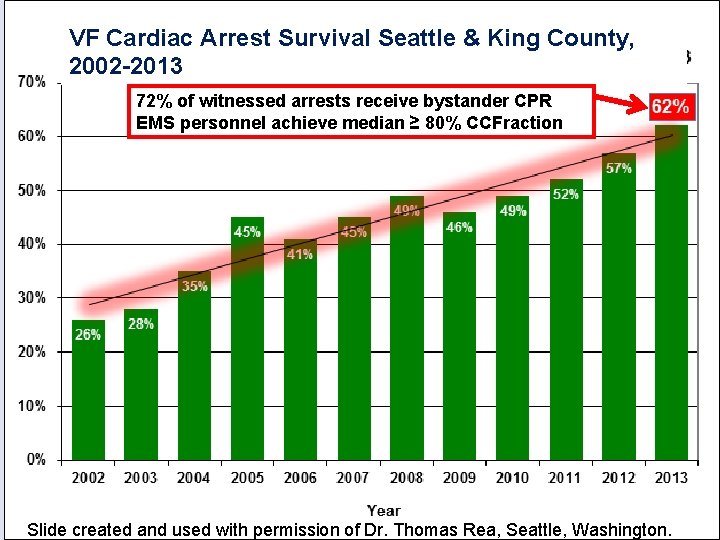
VF Cardiac Arrest Survival Seattle & King County, 2002 -2013 72% of witnessed arrests receive bystander CPR EMS personnel achieve median ≥ 80% CCFraction Slide created and used with permission of Dr. Thomas Rea, Seattle, Washington.
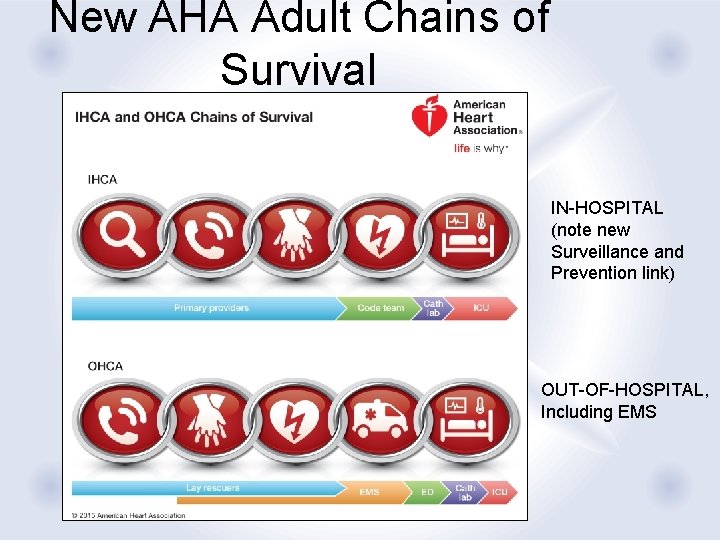
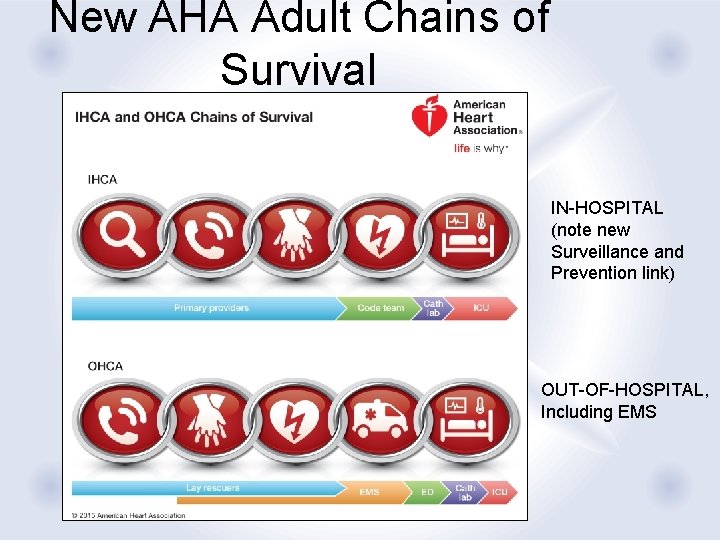
New AHA Adult Chains of Survival IN-HOSPITAL (note new Surveillance and Prevention link) OUT-OF-HOSPITAL, Including EMS
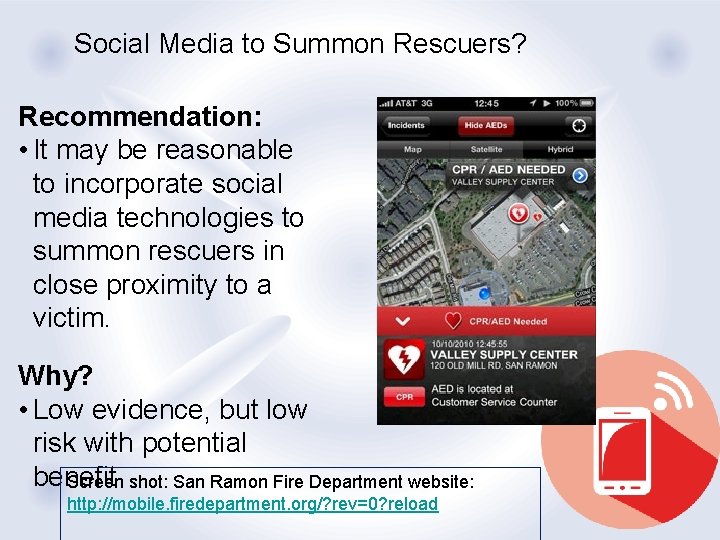
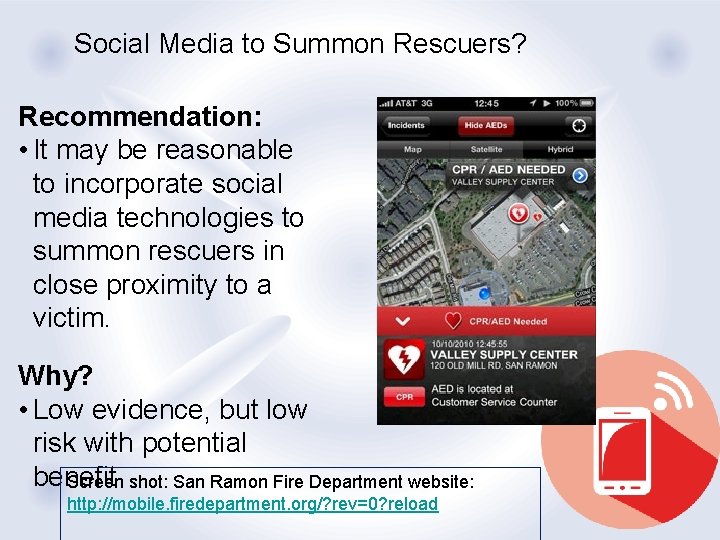
Social Media to Summon Rescuers? Recommendation: • It may be reasonable to incorporate social media technologies to summon rescuers in close proximity to a victim. Why? • Low evidence, but low risk with potential benefit Screen shot: San Ramon Fire Department website: http: //mobile. firedepartment. org/? rev=0? reload
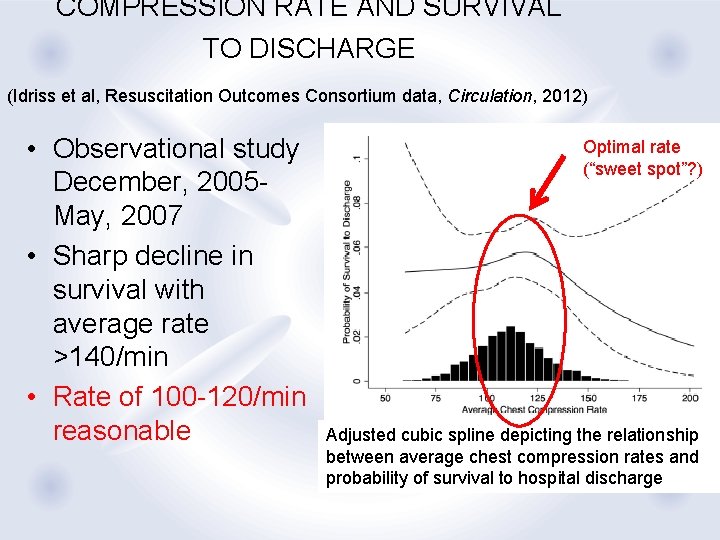
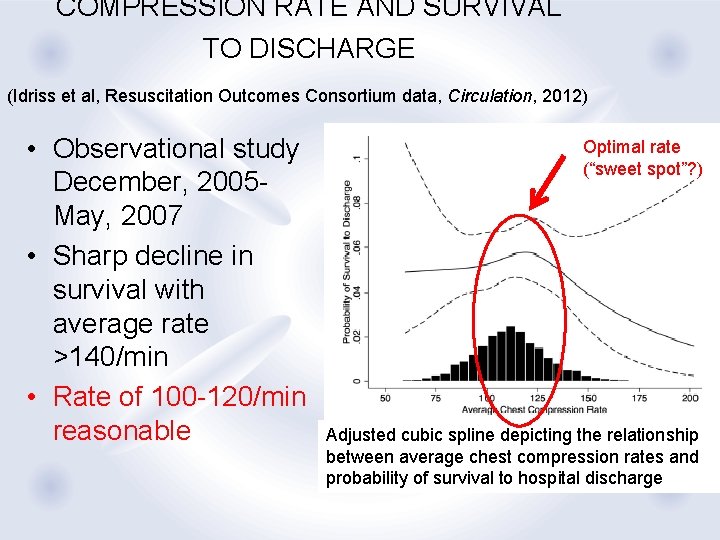
COMPRESSION RATE AND SURVIVAL TO DISCHARGE (Idriss et al, Resuscitation Outcomes Consortium data, Circulation, 2012) • Observational study December, 2005 May, 2007 • Sharp decline in survival with average rate >140/min • Rate of 100 -120/min reasonable Optimal rate (“sweet spot”? ) Adjusted cubic spline depicting the relationship between average chest compression rates and probability of survival to hospital discharge
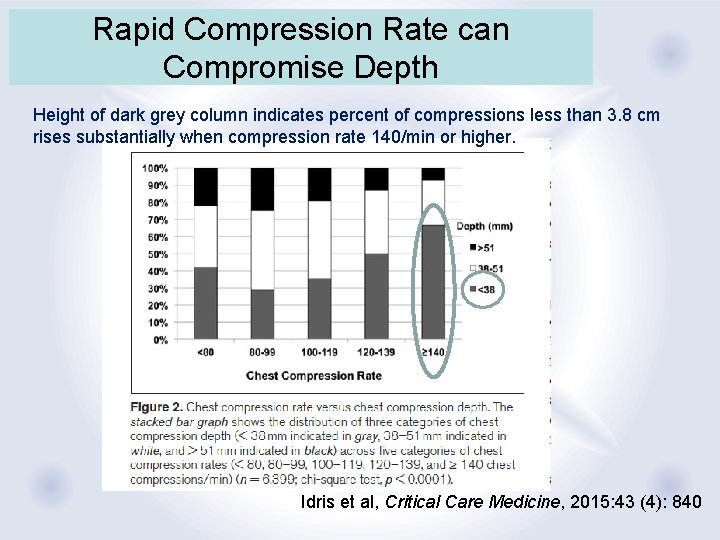
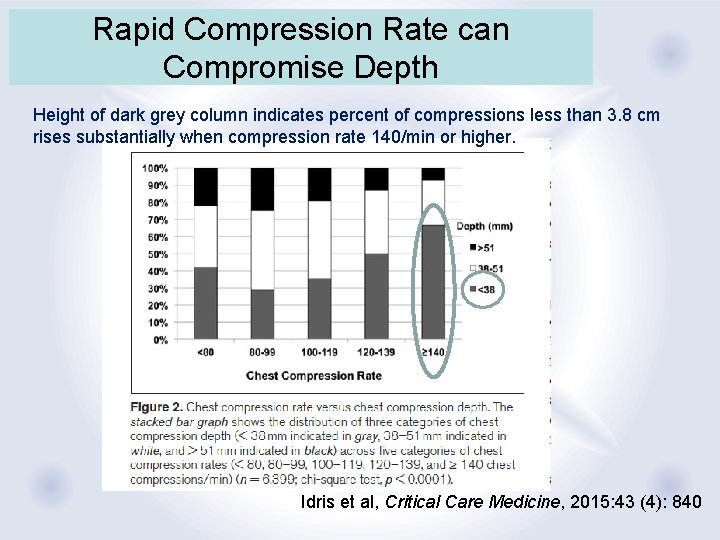
Rapid Compression Rate can Compromise Depth Height of dark grey column indicates percent of compressions less than 3. 8 cm rises substantially when compression rate 140/min or higher. Idris et al, Critical Care Medicine, 2015: 43 (4): 840
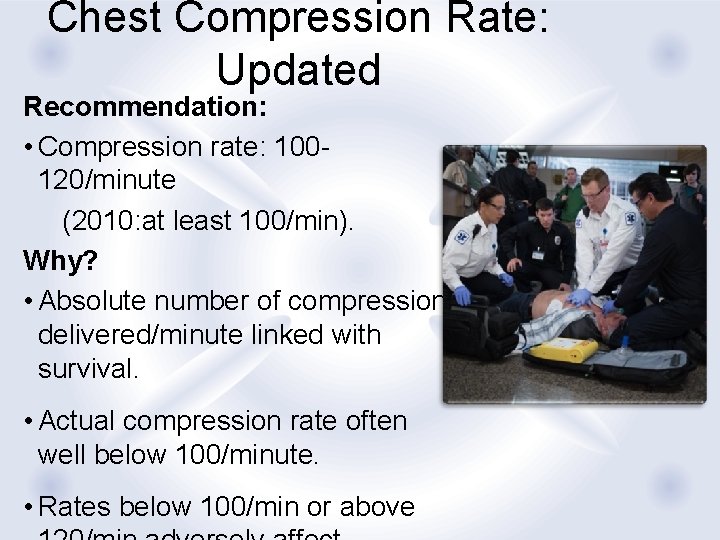
Chest Compression Rate: Updated Recommendation: • Compression rate: 100120/minute (2010: at least 100/min). Why? • Absolute number of compressions delivered/minute linked with survival. • Actual compression rate often well below 100/minute. • Rates below 100/min or above
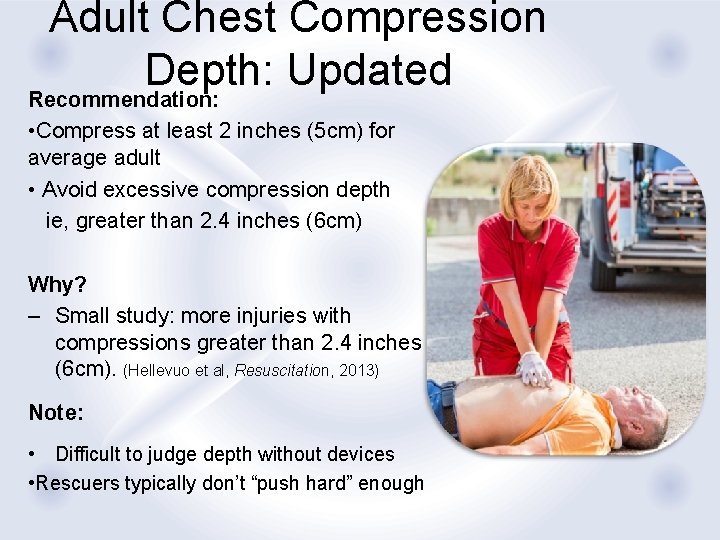
Adult Chest Compression Depth: Updated Recommendation: • Compress at least 2 inches (5 cm) for average adult • Avoid excessive compression depth ie, greater than 2. 4 inches (6 cm) Why? – Small study: more injuries with compressions greater than 2. 4 inches (6 cm). (Hellevuo et al, Resuscitation, 2013) Note: • Difficult to judge depth without devices • Rescuers typically don’t “push hard” enough

Bystander Naloxone for Opioid Overdose: New Recommendation: In additional to standard BLS care, it may be reasonable for appropriately trained rescuers (lay or HCP) to give IM or IN naloxone for life-threatening emergency with suspected opioid overdose. Why? Naloxone may reverse opioid-associated respiratory depression. Note that standard resuscitation measures take priority.
Delayed Ventilation by some ems providers Recommendation: • For witnessed OHCA with a shockable rhythm, EMS systems with priority-based multi-tiered response may use a strategy of up to 3 cycles of 200 continuous compressions with passive oxygen insufflation and airway adjuncts. Why? • For victims with witnessed, sudden arrest and shockable rhythm, delaying PPV shown to be effective in these systems. • In studies cited, providers received additional
Ventilation During CPR with an Advanced Airway: Updated Recommendation: • May be reasonable to deliver 1 breath every 6 seconds (10 breaths/min) while continuous chest compressions are being performed (infants, children and adults). Why? • Simplified from range of 1 breath every 6 -8 seconds (8 -10 breaths/min). • Should be easier to learn, remember, and perform Note • Report of new study of ventilation during CPR tomorrow at Re. SS
Mechanical Chest Compression Devices Recommendation: • Manual chest compressions remain standard of care over mechanical chest compression devices. • Mechanical piston/compression devices may be a reasonable alternative to conventional CPR in specific settings (eg, where the delivery of manual compressions may be challenging or dangerous to the provider). Why? • Three large randomized trials comparing mechanical chest compression devices to conventional CPR demonstrated survival similar to that with conventional
Vasopressors in Cardiac Arrest Recommendations: • Vasopressin + epinephrine offers no advantage over standard dose epinephrine—vasopressin has been deleted from AHA ACLS Cardiac Arrest Algorithm. • It may be reasonable to administer epinephrine as soon as feasible after the onset of cardiac arrest with initial nonshockable rhythm Why? • No benefit of vasopressin over epinephrine • Very large observational study found association of better outcome (increased ROSC, survival to hospital discharge, and neurologically intact survival) with earlier epinephrine for
LOW ETCO 2 one element Predicting Failed Resucitation? Recommendation: • In intubated patients, failure to achieve an ETCO 2 greater than 10 mm Hg by waveform capnography after 20 minutes of CPR may be considered one component of a multimodal approach to decide when to end resuscitative efforts, but it should not be used in isolation • Efforts should be made to optimize CPR quality Why? • Failure to achieve an ETCO 2 greater than 10 mm Hg after 20 minutes has been associated with poor outcome in case series • Low ETCO 2 likely indicates very low cardiac output and pulmonary blood flow during CPR
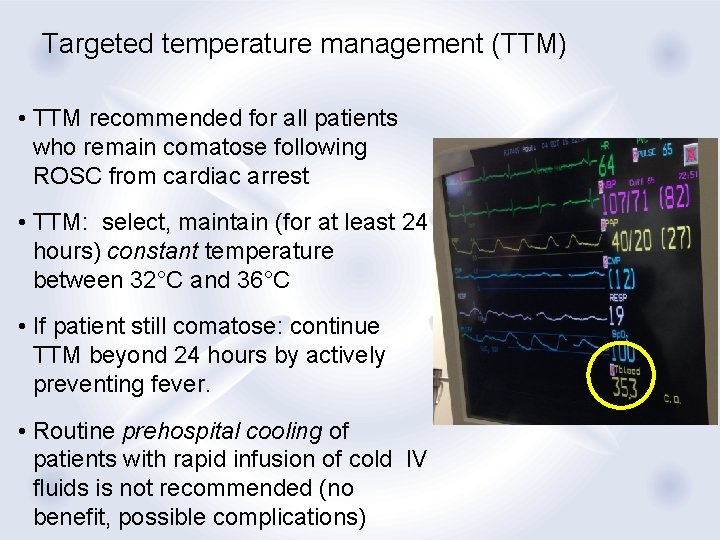
Targeted temperature management (TTM) • TTM recommended for all patients who remain comatose following ROSC from cardiac arrest • TTM: select, maintain (for at least 24 hours) constant temperature between 32°C and 36°C • If patient still comatose: continue TTM beyond 24 hours by actively preventing fever. • Routine prehospital cooling of patients with rapid infusion of cold IV fluids is not recommended (no benefit, possible complications)
Key TOPICS • Naloxone administration in combination with BLS care for opioidassociated life-threatening emergencies • Intravenous lipid emulsion considered for treatment of local anesthetic systemic toxicity • Refined recommendations regarding uterine displacement for CPR during pregnancy
Pediatric Resuscitation • Reaffirmed C-A-B sequence • Reaffirmed that compressions + ventilation needed for most pediatric arrest (unless sudden, witnessed collapse) • Rescuers unwilling or unable to deliver breaths should perform compressions • Updated 1 -rescuer and multi-rescuer algorithms
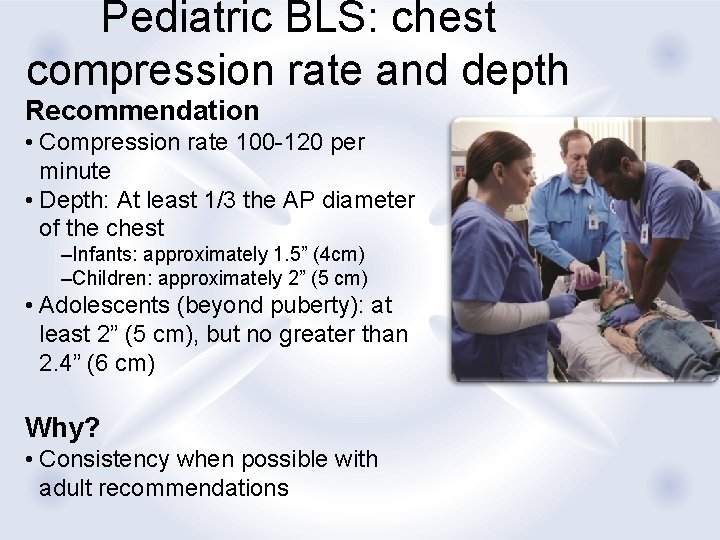
Pediatric BLS: chest compression rate and depth Recommendation • Compression rate 100 -120 per minute • Depth: At least 1/3 the AP diameter of the chest –Infants: approximately 1. 5” (4 cm) –Children: approximately 2” (5 cm) • Adolescents (beyond puberty): at least 2” (5 cm), but no greater than 2. 4” (6 cm) Why? • Consistency when possible with adult recommendations
Atropine no longer routine premedication for emergent intubation Why? • No evidence to support the routine use of atropine as a premedication to prevent bradycardia during emergent intubation. • No evidence to support minimum dose of atropine for premedication • Note that recommendation for use of atropine for treatment of bradycardia is unchanged.

Amiodarone OR lidocaine for pediatric vt/vf arrest • Amiodarone and lidocaine are equally acceptable for VF/p. VT, so both are included in PALS Pediatric Cardiac Arrest Algorithm. Note that amiodarone is not yet cleared by the FDA for labeling for use in pediatric cardiac arrest.
Targeted temperature management IN CHILDREN Recommended • For children who are comatose following ROSC --5 days of normothermia (36°C - 37. 5°C) OR --2 days of continuous hypothermia (32°C 34°C) followed by 3 days of normothermia • Prevent or aggressively treat fever during postcardiac arrest care Why? New study published
Approaches to learning • BLS skills seem to be learned as easily through self-instruction (video or computer based) plus hands-on practice as with traditional courses • Blended learning (self-instruction + instructor-led courses with hands-on training) can be alternative to instructor-led courses. • Pre-course preparation may optimize learning for ACLS, PALS

Thank you 56 Education of CPR
 Guideline anamnesa
Guideline anamnesa Kdigo 2012 aki
Kdigo 2012 aki Bpfk cosmetic guideline
Bpfk cosmetic guideline What is a guideline for hoisting a hoseline?
What is a guideline for hoisting a hoseline? Asean stability guideline
Asean stability guideline Guideline anamnesa
Guideline anamnesa Outside counsel guidelines template
Outside counsel guidelines template Who guideline on country pharmaceutical pricing policies
Who guideline on country pharmaceutical pricing policies Mfmea example
Mfmea example East practice management guidelines
East practice management guidelines Guideline clinical nutrition in patients with stroke
Guideline clinical nutrition in patients with stroke Waikato stormwater management guideline
Waikato stormwater management guideline Turnbull directions
Turnbull directions Asam national practice guideline
Asam national practice guideline Patient safety incident reporting form
Patient safety incident reporting form Ccgi guidelines
Ccgi guidelines Acromegaly an endocrine society clinical practice guideline
Acromegaly an endocrine society clinical practice guideline Enteral feeding guideline
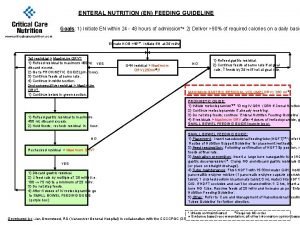
Enteral feeding guideline Disconnected epidural catheter guideline
Disconnected epidural catheter guideline Interview guideline template
Interview guideline template 5 guideline for cumbersome calculations
5 guideline for cumbersome calculations Msqh standard
Msqh standard Srm process flow
Srm process flow Acg chronic pancreatitis
Acg chronic pancreatitis Used to create one-length and low-elevation haircuts.
Used to create one-length and low-elevation haircuts. Escardio guideline
Escardio guideline Anemia in pregnancy guideline
Anemia in pregnancy guideline 5% guideline for cumbersome calculations
5% guideline for cumbersome calculations Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Jätte råtta
Jätte råtta Kanaans land
Kanaans land Slyngexcision
Slyngexcision Tillitsbaserad ledning
Tillitsbaserad ledning Romarriket tidslinje
Romarriket tidslinje Boverket ka
Boverket ka Vad är verksamhetsanalys
Vad är verksamhetsanalys Typiska novell drag
Typiska novell drag Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden Matematisk modellering eksempel
Matematisk modellering eksempel Texter för hinduer tantra
Texter för hinduer tantra Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Påbyggnader för flakfordon
Påbyggnader för flakfordon Jag har gått inunder stjärnor text
Jag har gått inunder stjärnor text Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Sura för anatom
Sura för anatom Egg för emanuel
Egg för emanuel Beräkna standardavvikelse
Beräkna standardavvikelse Rutin för avvikelsehantering
Rutin för avvikelsehantering Tack för att ni har lyssnat
Tack för att ni har lyssnat Läkarutlåtande för livränta
Läkarutlåtande för livränta Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Myndigheten för delaktighet
Myndigheten för delaktighet Tack för att ni lyssnade
Tack för att ni lyssnade Debattinlägg mall
Debattinlägg mall Tobinskatten för och nackdelar
Tobinskatten för och nackdelar