ESOPHAGEAL SURGERY Dysphagia vs Odynophagia Oropharyngeal dysphagia Loss


- Slides: 39
ESOPHAGEAL SURGERY
Dysphagia vs Odynophagia Oropharyngeal dysphagia: Loss of tongue function (myasthenia gravis). • Pharyngeal dysfunction (myasthenia gravis, vascular brainstem disease, hyperthyroidism). • Mechanical obstruction (Zenker’s diverticulum, tumor, inflammatory stricture).
Oesophageal causes Intraluminal obstruction : Motility disorders vs Organic • Tumor. • • • Esophageal webs. Lower esophageal ring (Schatzki ring). Lower esophageal sphincter spasm (hypertensive sphincter). Inflammatory stricture (peptic stricture). Caustic stricture. Foreign body.
• Achalasia. • • • . Scleroderma. Diabetic neuropathy. Diffuse esophageal spasm. Amyloidosis. Parasitic infection (Chagas’ disease).
Extraluminal obstruction. • Compression by tumors, enlarged lymph nodes, retrosternal thyroid gland. • Vascular abnormalities (aortic aneurysm, aberrant right subclavian artery, right-sided aortic arch).
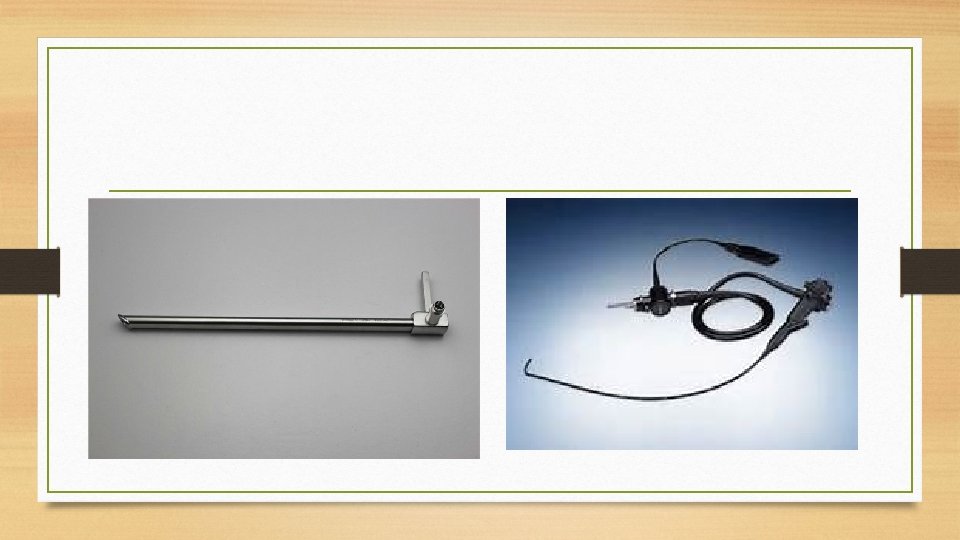
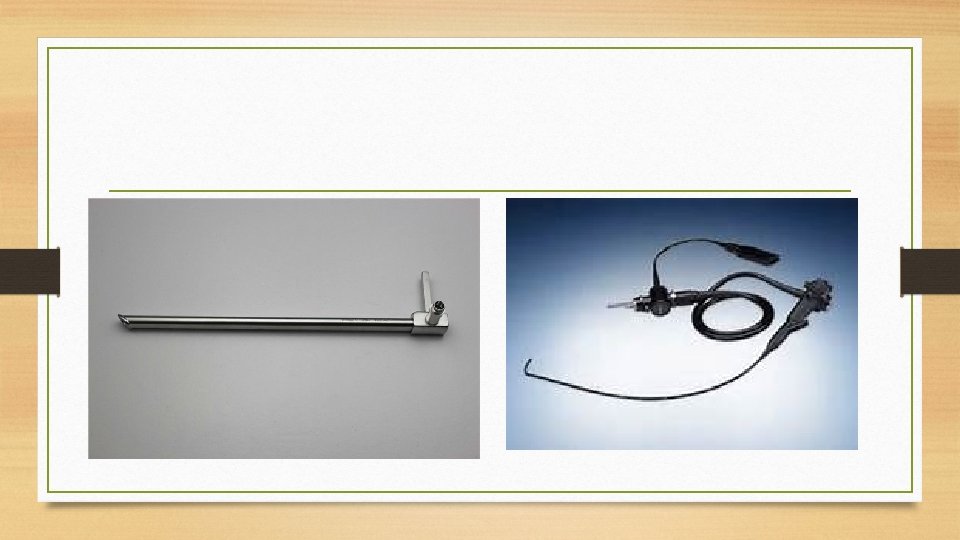
INVESTIGATIONS • • Eosophagoscopy Types: Rigid: done under general anesthesia Flexible, fiberoptic: done under conscious sedation
Indications • Diagnostic • • Cancer eosophagus: locate site, taking biopsy (bite , brush biopsy) Hiatal hernia: to access degree of reflux Achalasia: Identify cause of dysphagia and haematemesis • Therapeutic • • • Removal of foreign body Insertion of Stent in cancer eosophagus Sclerotherapy in haematemesis Dilatation of eosophageal stricture Laser therapy
ACHALASIA • failure of relaxation of the lower esophageal sphincter (LES) • and ineffective peristalsis in the body of the esophagus
Clinical Picture • Progressive dysphagia to liquids and solids over several years (first for fluids). • Regurgitation of undigested food especially in recumbent position. • Weight loss. (not common as food passes by its weight) • Coughing or wheezing secondary to aspiration.
• • Complications Mucosal ulcerations by irritation of retained food. Aspiration which leads to pneumonitis. Malignancy in 2 -3% (squamous cell carcinoma usually at dilated site).
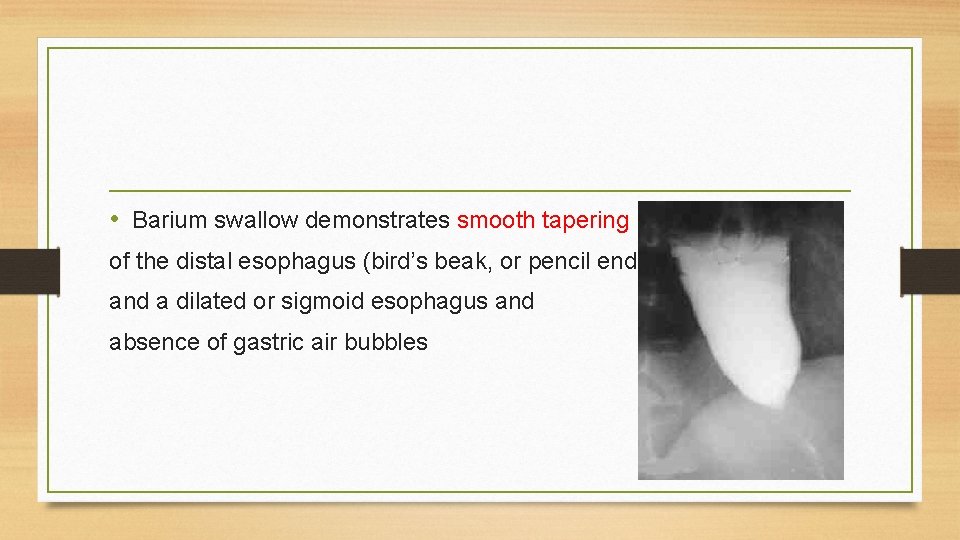
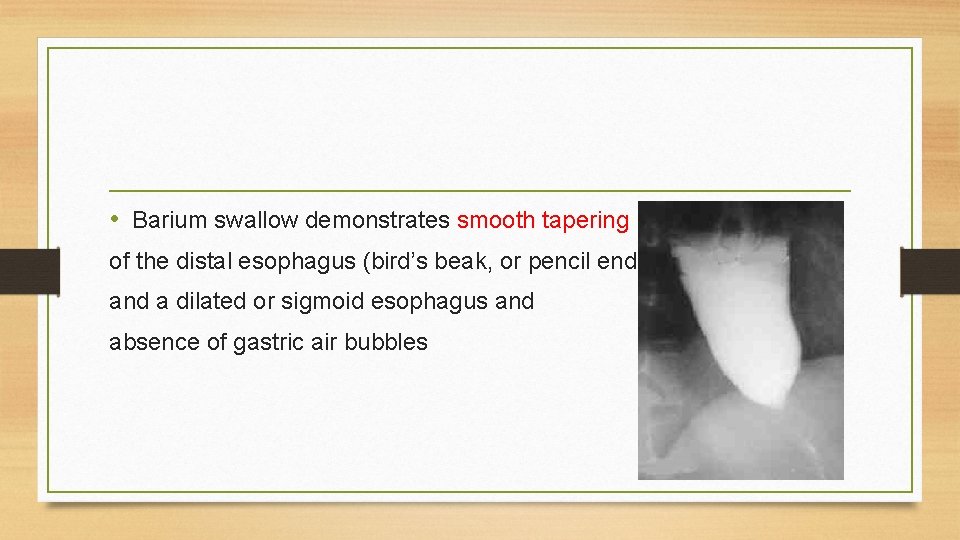
• Barium swallow demonstrates smooth tapering of the distal esophagus (bird’s beak, or pencil end) and a dilated or sigmoid esophagus and absence of gastric air bubbles
• Endoscopy: Dilated esophageal body containing food residue (despite fasting). • Easy passage of the rigid esophagoscope through the esophagogastric junction but failure of esophagogastric junction to open spontaneously with repeated air insufflation using the fiberoptic esophagoscope.
• Esophageal function studies: Esophageal manometry demonstrates incomplete relaxation of the LES with swallowing and ineffective peristalsis of the body of the esophagus
• Medical treatment: • Pneumonetic dilatation : Balloons here pneumatic dilatation produces a forceful disruption of the lower esophageal sphincter • Botulinum toxin: It is endoscopically injected into the lower sphincter to weaken it.
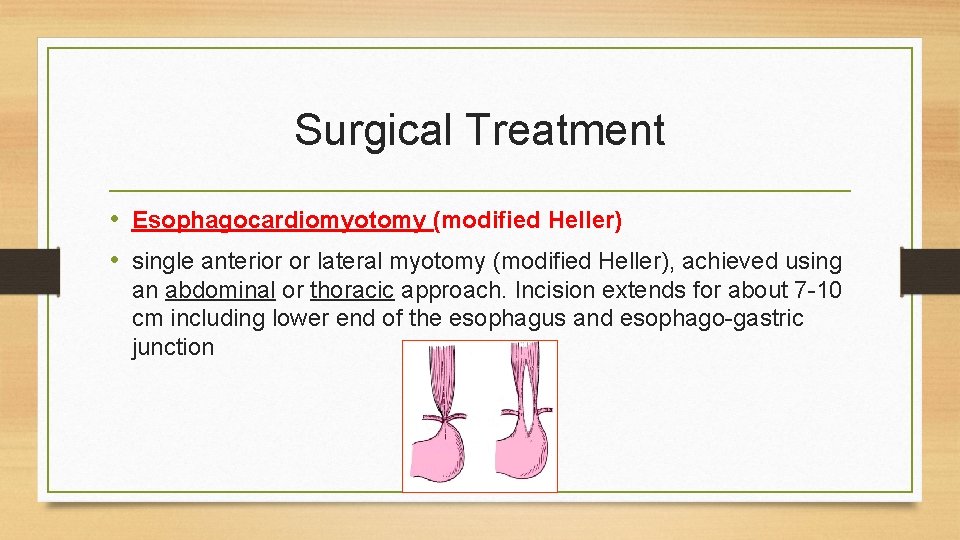
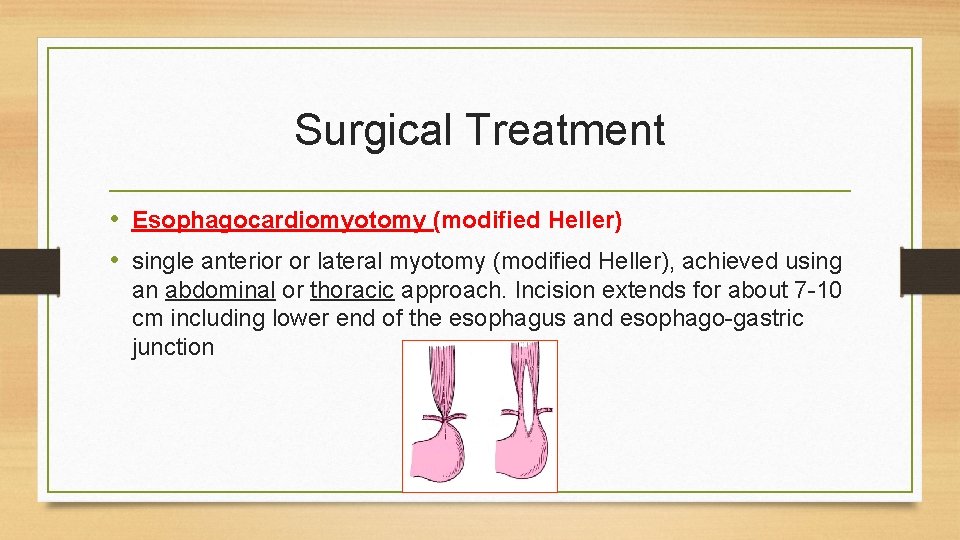
Surgical Treatment • Esophagocardiomyotomy (modified Heller) • single anterior or lateral myotomy (modified Heller), achieved using an abdominal or thoracic approach. Incision extends for about 7 -10 cm including lower end of the esophagus and esophago-gastric junction
• Recently, minimally invasive surgical approaches (laparoscopic or thoracoscopic myotomy) are used. • Esophageal resection and reconstruction is considered in patients who have failed esophageal myotomy (or re-myotomy), or who have an end-stage megaesophagus.
ESOPHAGEAL CANCER
Pathology of esophageal cancer • • Squamous cell carcinoma : 80% of all primary esophageal cancers. Mid-third (50%), lower-third (25%), upper-third (15%). Macroscopic types: Fungating, ulcerating, infiltrating, polypoid.
• Adenocarcinoma : • 20 - 40% of primary esophageal cancer. • Should be distinguished from adenocarcinoma of gastric origin. Criteria in favour of esophageal origin include: • Associated Barrett’s epithelium
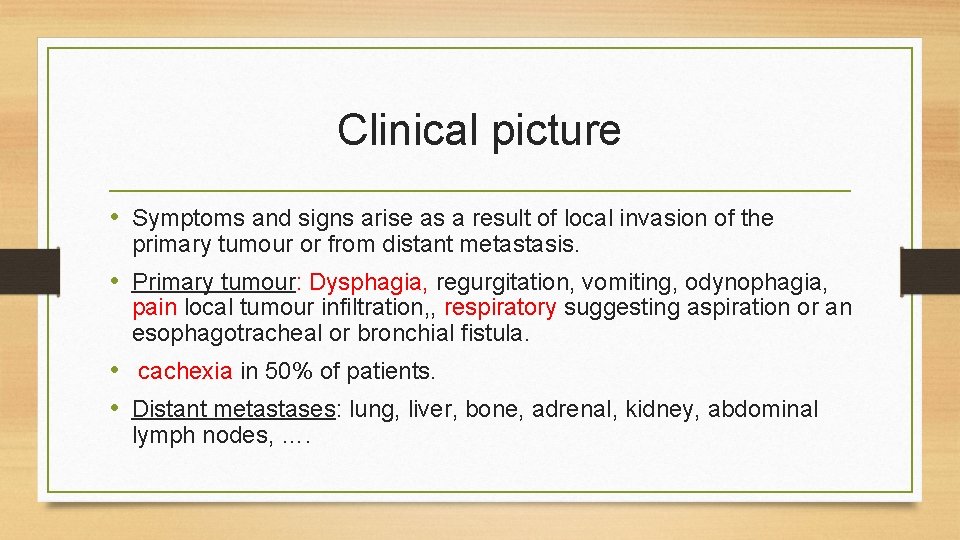
Clinical picture • Symptoms and signs arise as a result of local invasion of the primary tumour or from distant metastasis. • Primary tumour: Dysphagia, regurgitation, vomiting, odynophagia, pain local tumour infiltration, , respiratory suggesting aspiration or an esophagotracheal or bronchial fistula. • cachexia in 50% of patients. • Distant metastases: lung, liver, bone, adrenal, kidney, abdominal lymph nodes, ….
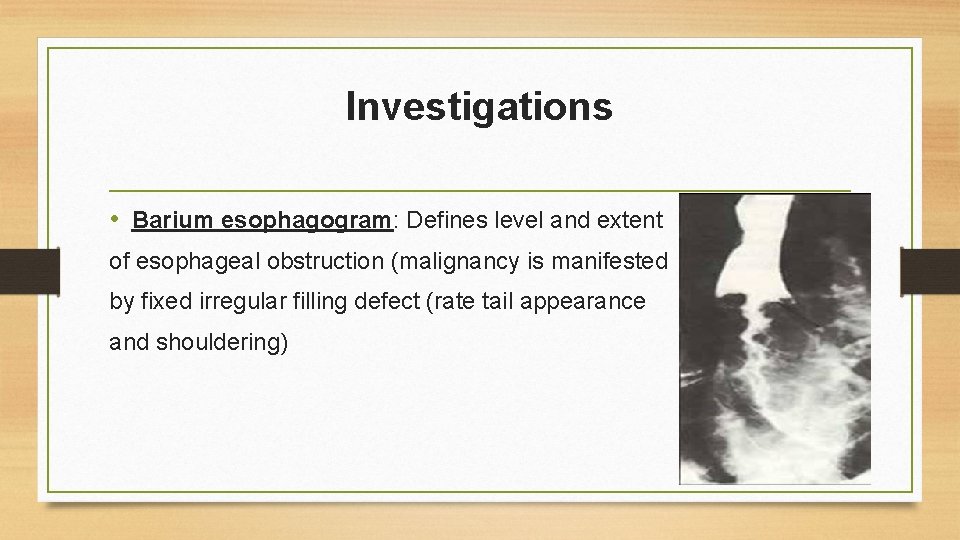
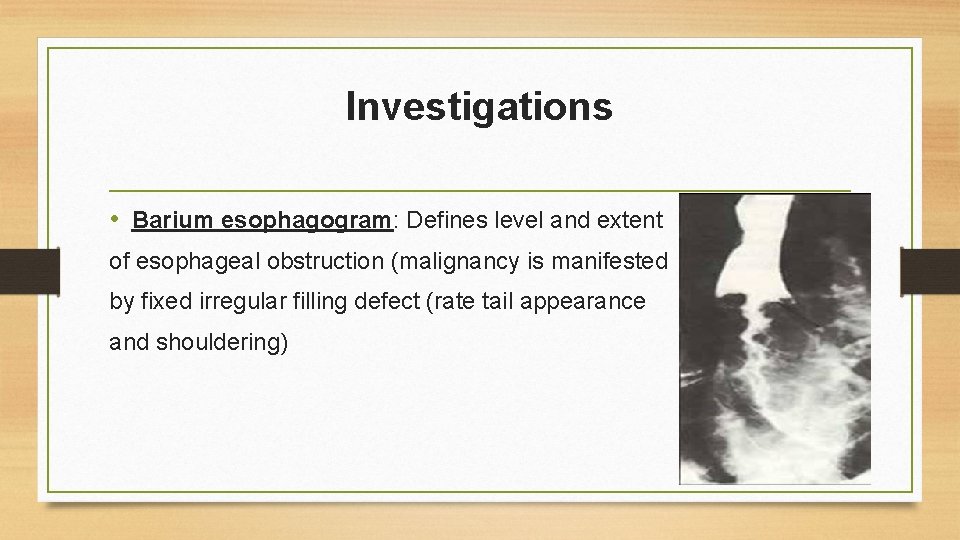
Investigations • Barium esophagogram: Defines level and extent of esophageal obstruction (malignancy is manifested by fixed irregular filling defect (rate tail appearance and shouldering)
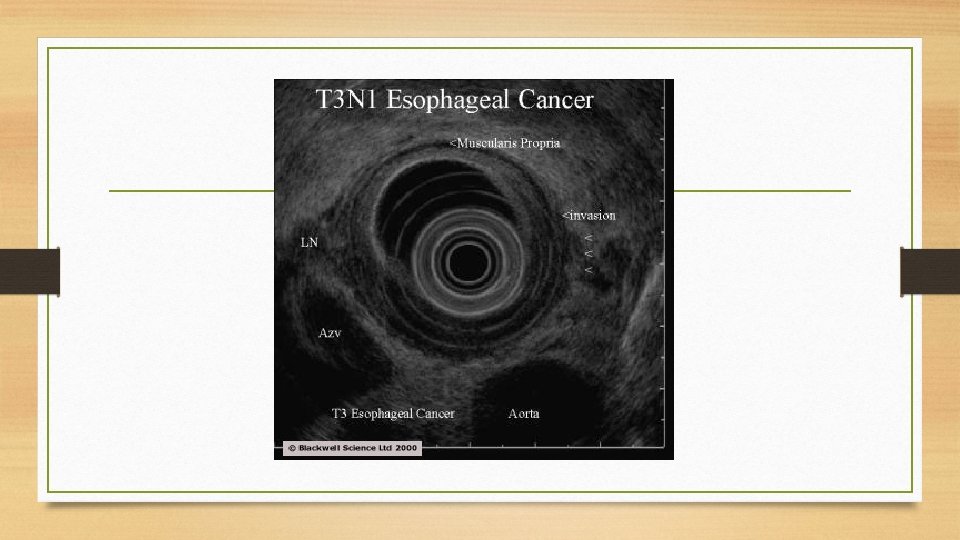
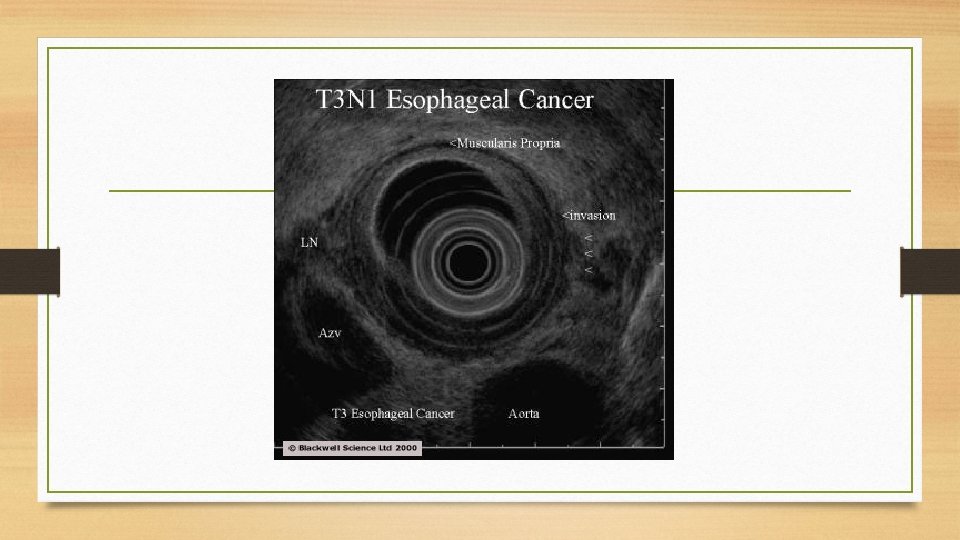
• • Esophagogastroscopy defines the site and extent of the tumor. Multiple biopsies are taken to obtain a histologic diagnosis. Obstructing tumors may be dilated or stented during esophagoscopy • Endoscopic ultrasound: To assess the depth of tumor penetration and peri-esophageal lymph node metastasis
• Computed tomography (CT): Scanning of the primary tumor to assess extent of local disease and enlarged nodes (mediastinal, upper abdominal). Scanning of the brain, lung, and liver for the possibility of metastases.
TNM STAGING
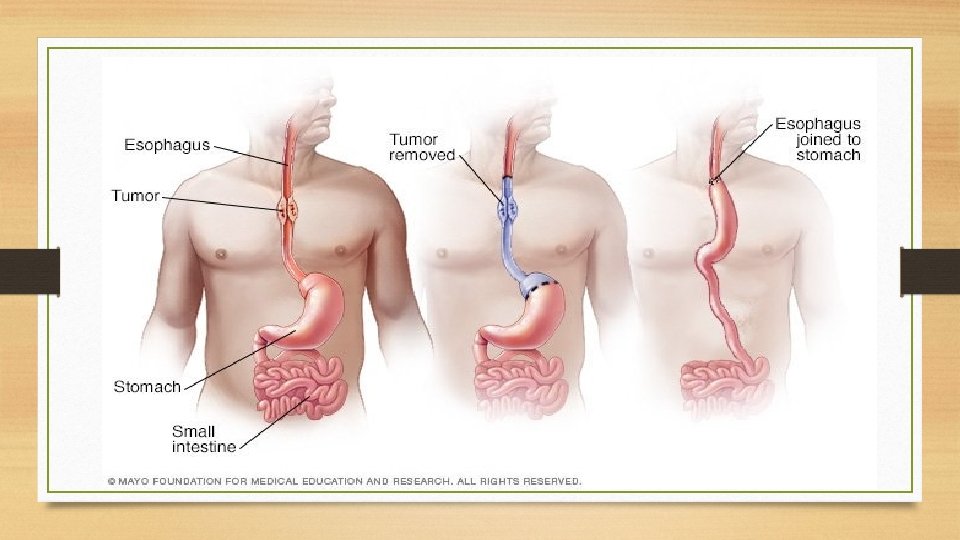
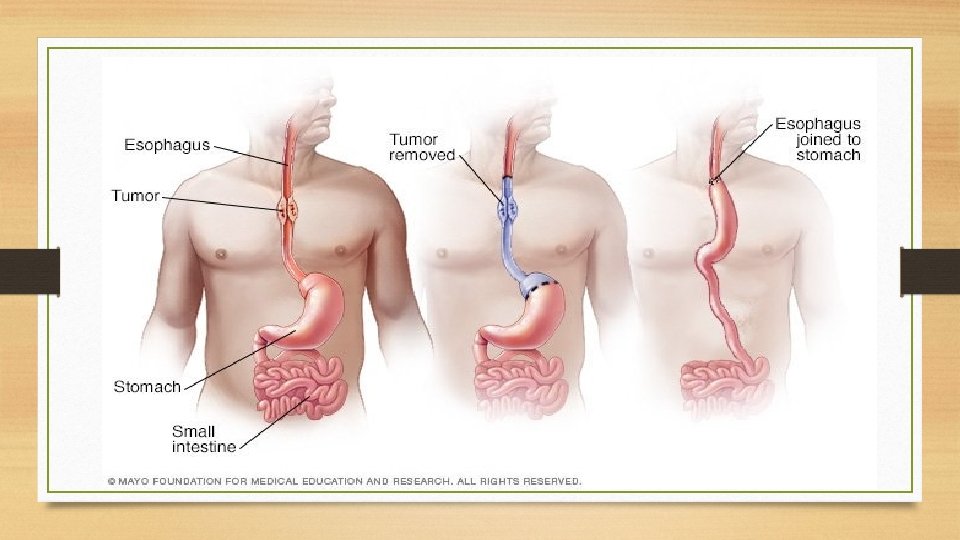
TREATMENT • Early stage tumors (Tis, Stage I): Surgical resection Curative • Eosophagectomy with gastric pull up and Eosophagogastric anastomosis.
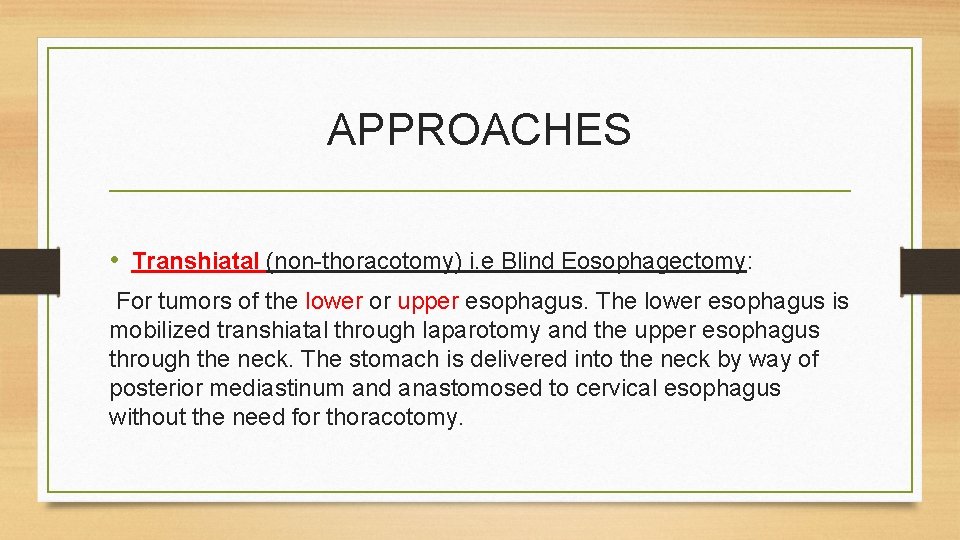
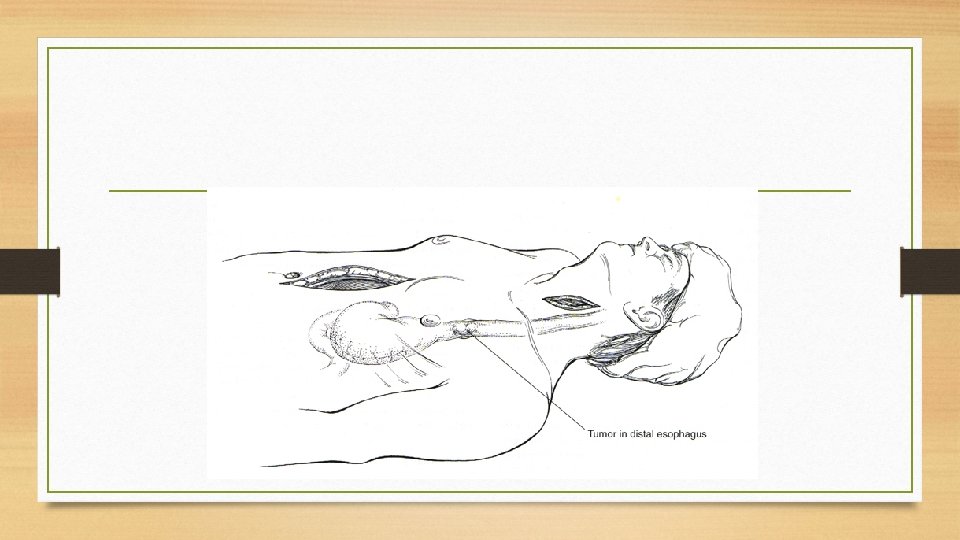
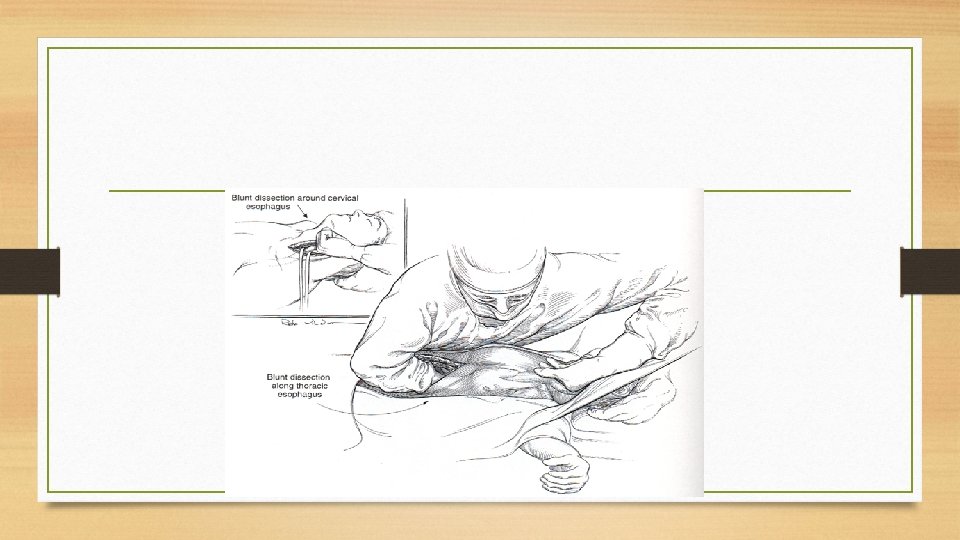
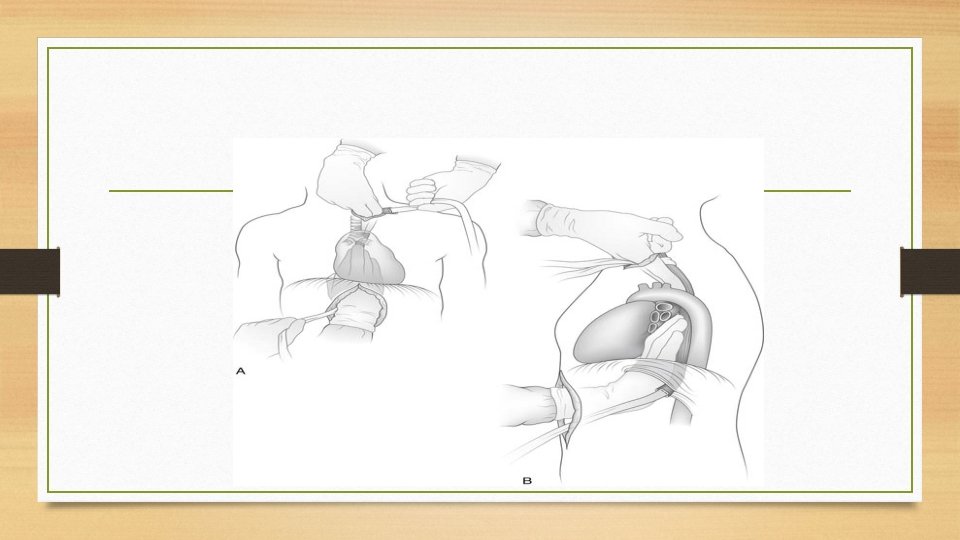
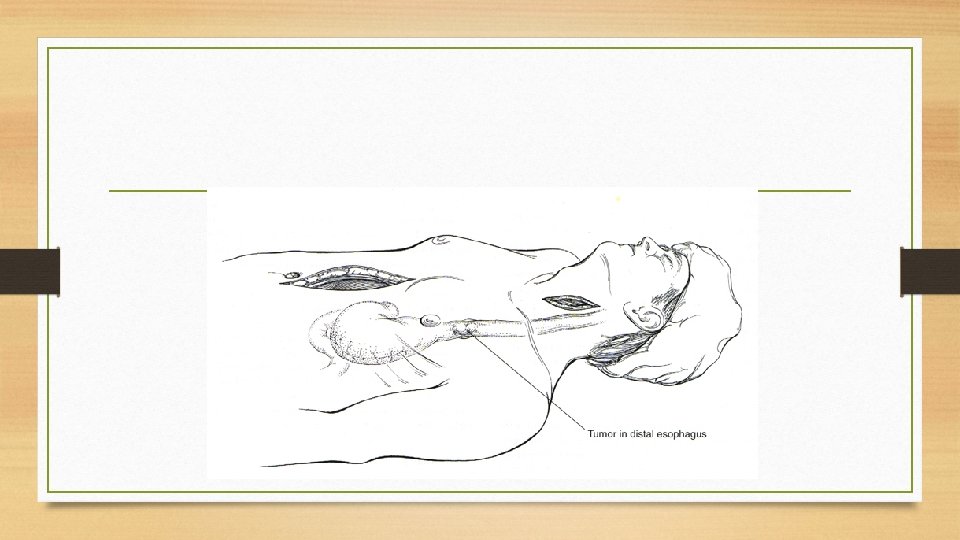
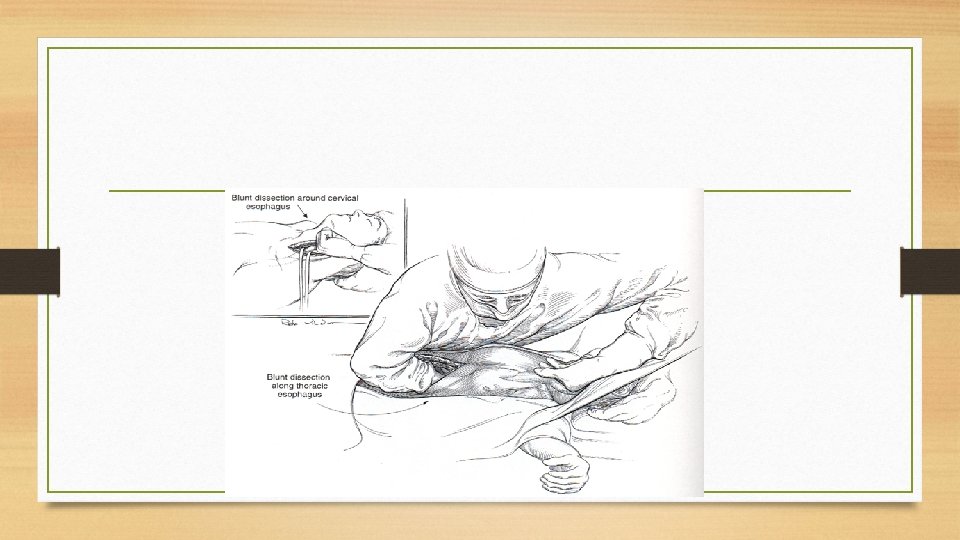
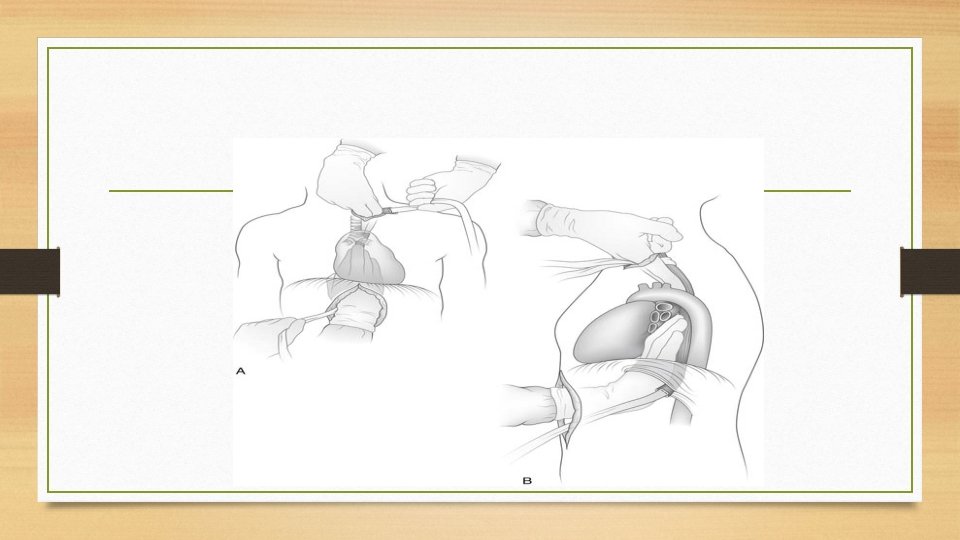
APPROACHES • Transhiatal (non-thoracotomy) i. e Blind Eosophagectomy: For tumors of the lower or upper esophagus. The lower esophagus is mobilized transhiatal through laparotomy and the upper esophagus through the neck. The stomach is delivered into the neck by way of posterior mediastinum and anastomosed to cervical esophagus without the need for thoracotomy.

• Trans thoracic: Laparotomy to exclude abdominal metastasis and mobilize the stomach. Right thoracotomy to resect the esophagus. The stomach is delivered through the hiatus and esophago-gastric anastomosis made intrathoracic, or through neck incision, the stomach is anastomosed to cervical esophagus.
• Left thoracotomy or Thoracoabdominal : For tumors in the distal esophagus or esophagogastric junction. Getting into the abdomen is either by incising the diaphragm or extending the incision across the costal margin. • Minimally invasive video assisted thoracoscopic surgery (VATS): Right-sided VATS is utilized to mobilize the entire intrathoracic esophagus avoiding formal thoracotomy. Esophageal reconstruction is done in the usual manner through laparotomy and left neck incisions.
Palliative Care • Locally advanced (T 4) & metastatic (M 1) tumors : Are excluded from surgery. Esophageal dilatation. • Esophageal stents: • Covered self-expandable metallic stents, inserted through endoscopy , Mousseau Barbin intubation, inserted through laparotomy
• • Radiochemotherapy. Endoluminal brachytherapy. Laser therapy. Surgery: • Feeding gastrostomy • Retrosternal Colon interposition or eosophagogastrectomy. Those 2 aggressive surgeries are rarely used as palliation.

THANK YOU