Esophageal Dysphagia Approach and Management Andrew S Ross

- Slides: 19
Esophageal Dysphagia: Approach and Management Andrew S. Ross MD
Disclosure Consultant/Speaker/Research: Boston Scientific © 2016 Virginia Mason Medical Center 2
Case Presentation - 56 Year old male with no previous medical history presents with progressive dysphagia - Solids and liquids - Found to have associated iron deficiency anemia - Next Step? - FIT test Colonoscopy +/-EGD Alone CT Esophageal Manometry Esophagram © 2016 Virginia Mason Medical Center 3
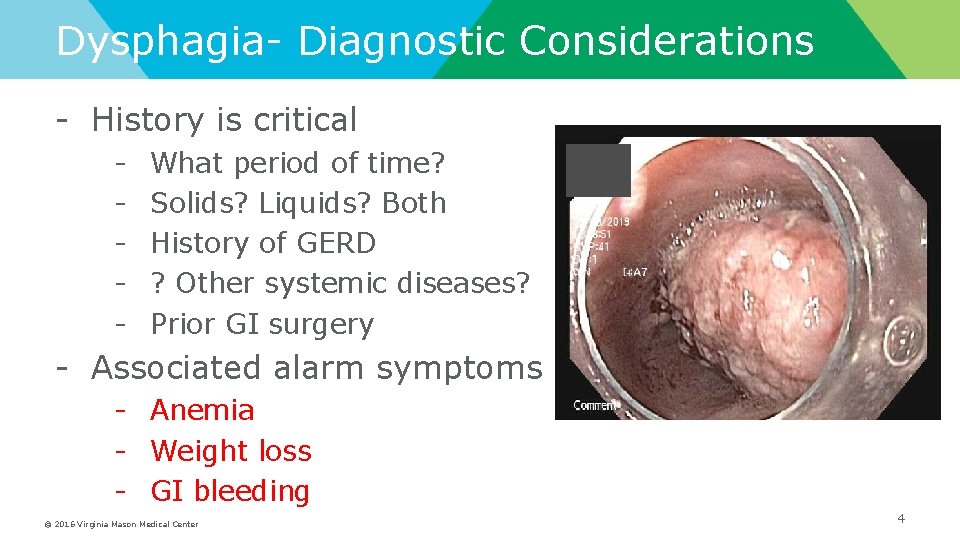
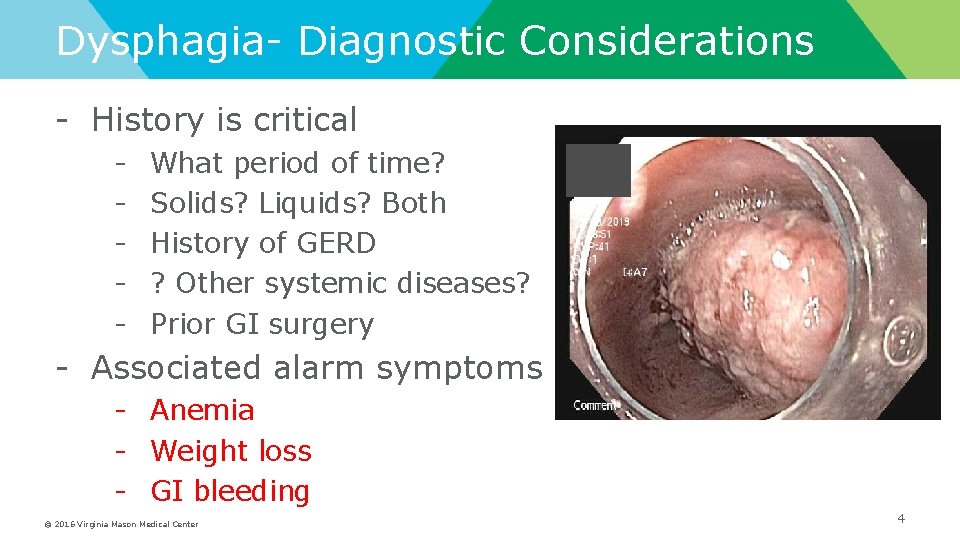
Dysphagia- Diagnostic Considerations - History is critical - What period of time? Solids? Liquids? Both History of GERD ? Other systemic diseases? Prior GI surgery - Associated alarm symptoms - Anemia - Weight loss - GI bleeding © 2016 Virginia Mason Medical Center 4
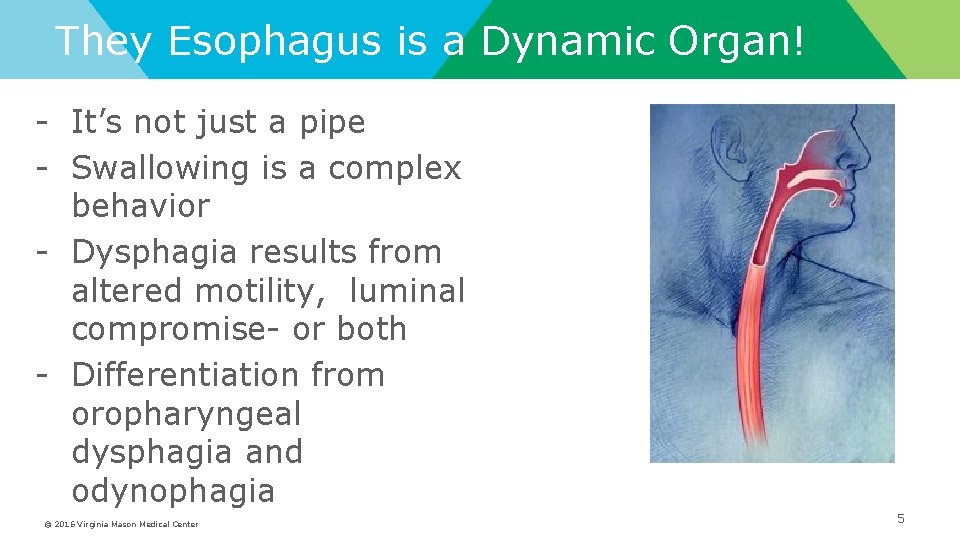
They Esophagus is a Dynamic Organ! - It’s not just a pipe - Swallowing is a complex behavior - Dysphagia results from altered motility, luminal compromise- or both - Differentiation from oropharyngeal dysphagia and odynophagia © 2016 Virginia Mason Medical Center 5
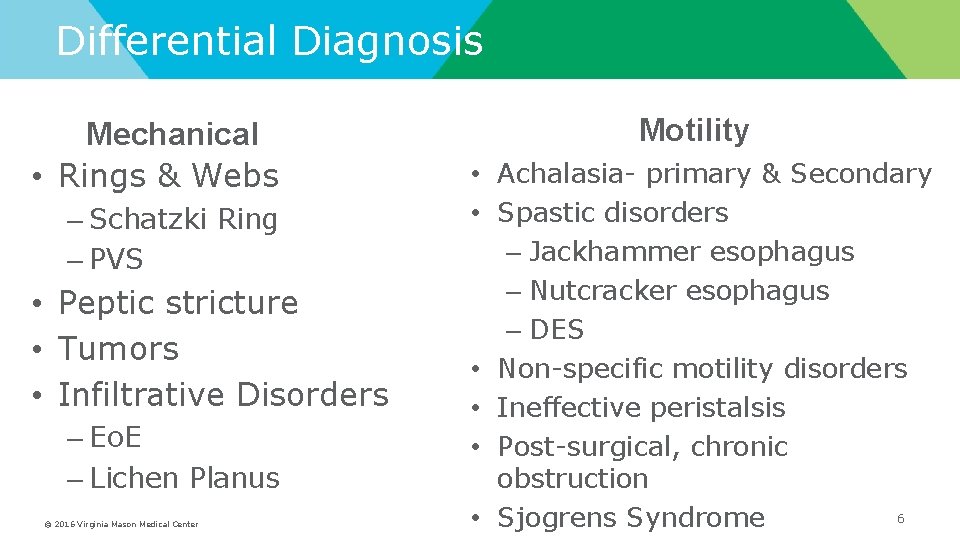
Differential Diagnosis Mechanical • Rings & Webs – Schatzki Ring – PVS • Peptic stricture • Tumors • Infiltrative Disorders – Eo. E – Lichen Planus © 2016 Virginia Mason Medical Center Motility • Achalasia- primary & Secondary • Spastic disorders – Jackhammer esophagus – Nutcracker esophagus – DES • Non-specific motility disorders • Ineffective peristalsis • Post-surgical, chronic obstruction 6 • Sjogrens Syndrome
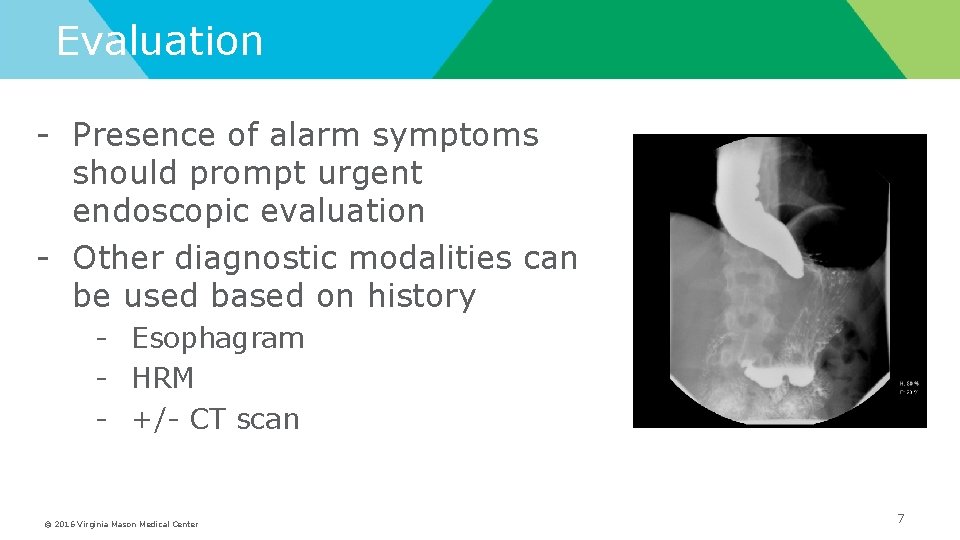
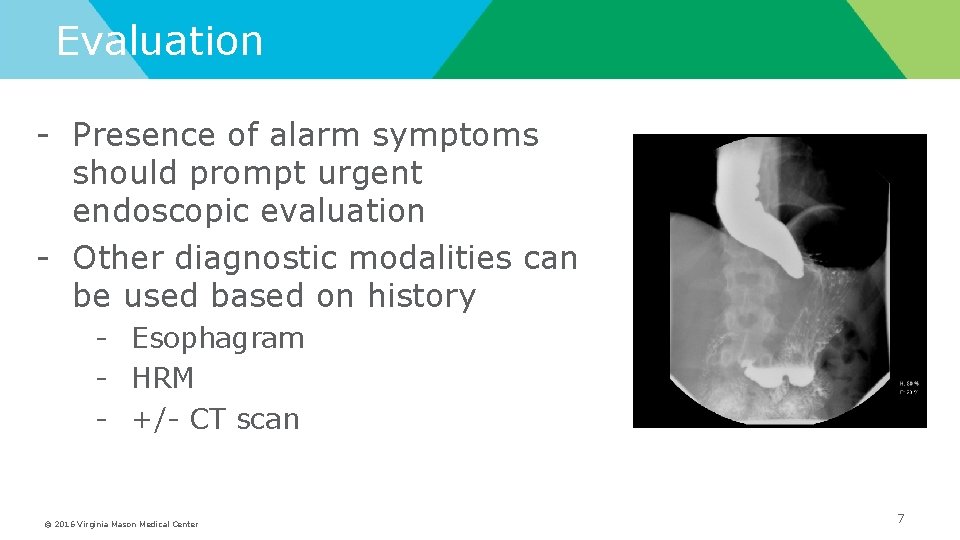
Evaluation - Presence of alarm symptoms should prompt urgent endoscopic evaluation - Other diagnostic modalities can be used based on history - Esophagram - HRM - +/- CT scan © 2016 Virginia Mason Medical Center 7

Rings & Benign Strictures - Schatzki rings often missed on endoscopy; esophagram more sensitive - Almost always associated with a hiatal hernia - Initial treatment: Dilation with >50 Fr bougie or 18 -20 mm balloon - Acid suppression - High rate of recurrence - Incisional therapy Biopsy obliteration Repeat dilation PRN “Laser” ablation © 2016 Virginia Mason Medical Center 8
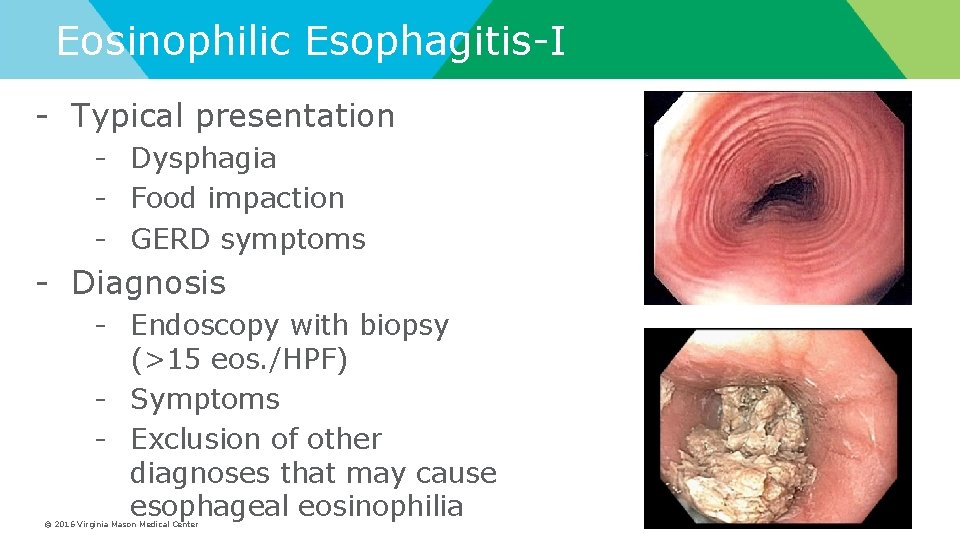
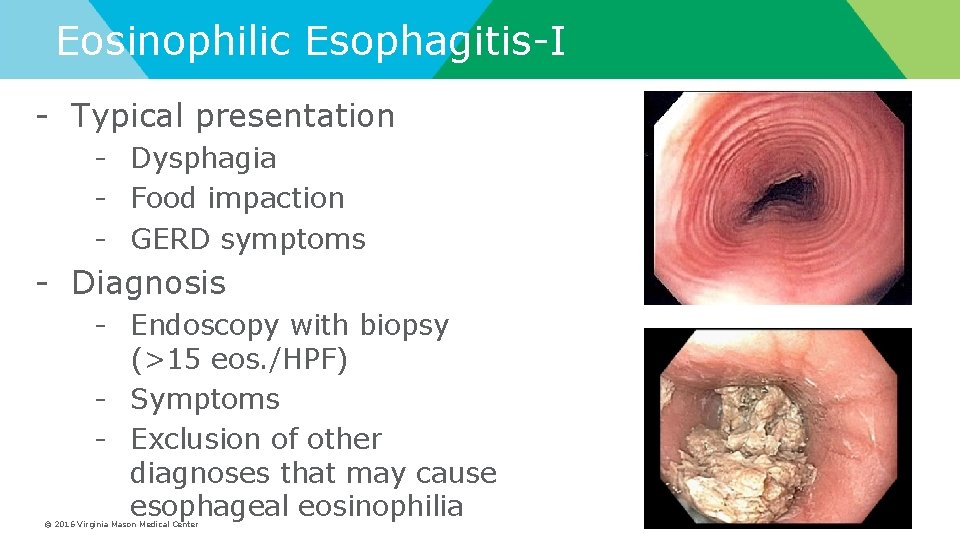
Eosinophilic Esophagitis-I - Typical presentation - Dysphagia - Food impaction - GERD symptoms - Diagnosis - Endoscopy with biopsy (>15 eos. /HPF) - Symptoms - Exclusion of other diagnoses that may cause esophageal eosinophilia © 2016 Virginia Mason Medical Center 9
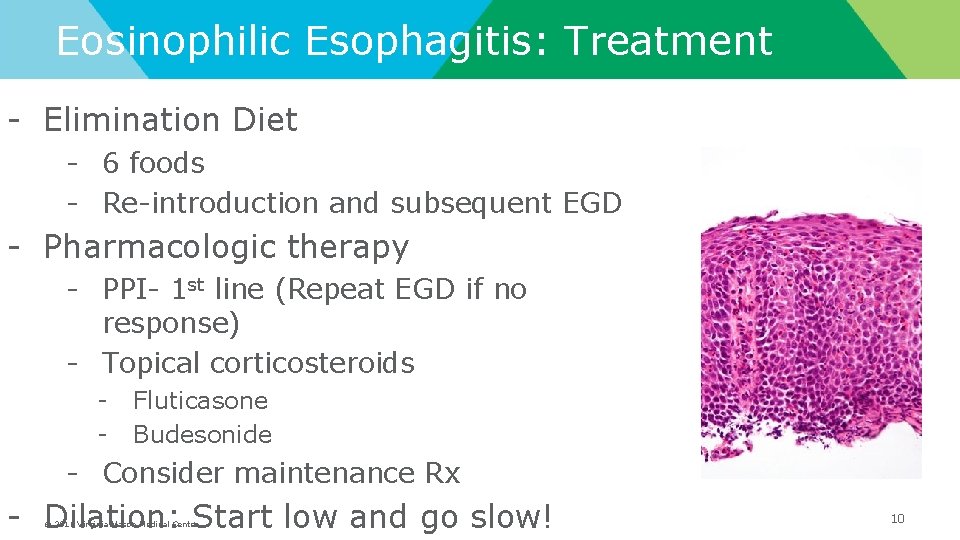
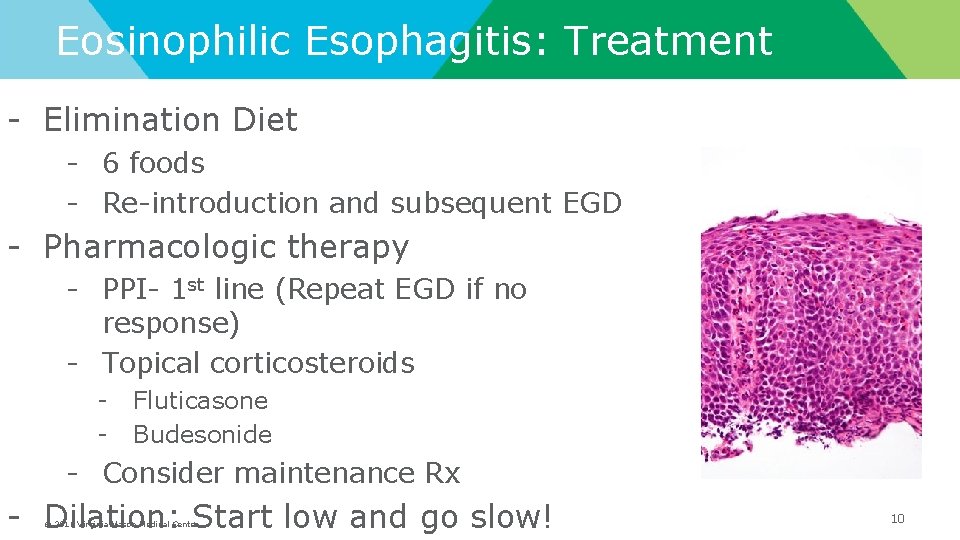
Eosinophilic Esophagitis: Treatment - Elimination Diet - 6 foods - Re-introduction and subsequent EGD - Pharmacologic therapy - PPI- 1 st line (Repeat EGD if no response) - Topical corticosteroids - Fluticasone Budesonide - Consider maintenance Rx - Dilation: Start low and go slow! © 2016 Virginia Mason Medical Center 10
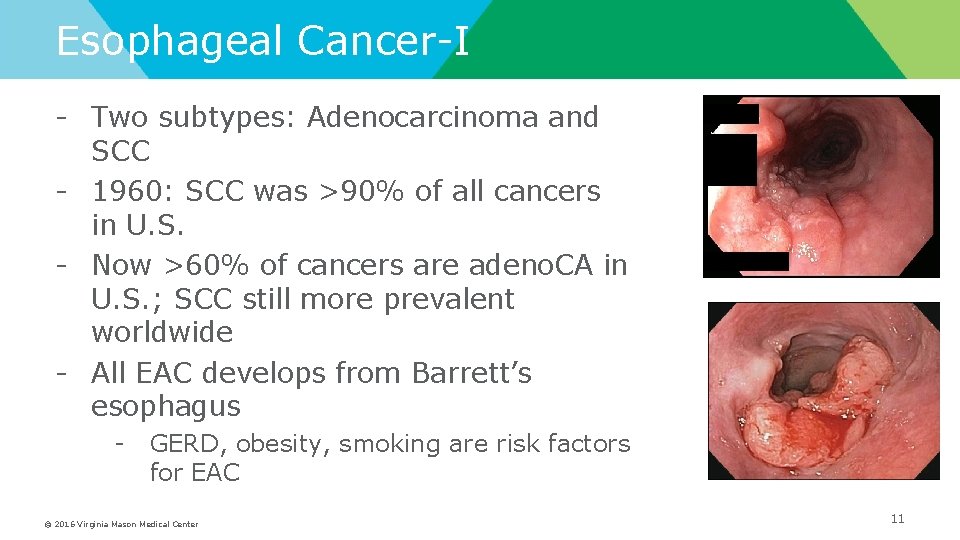
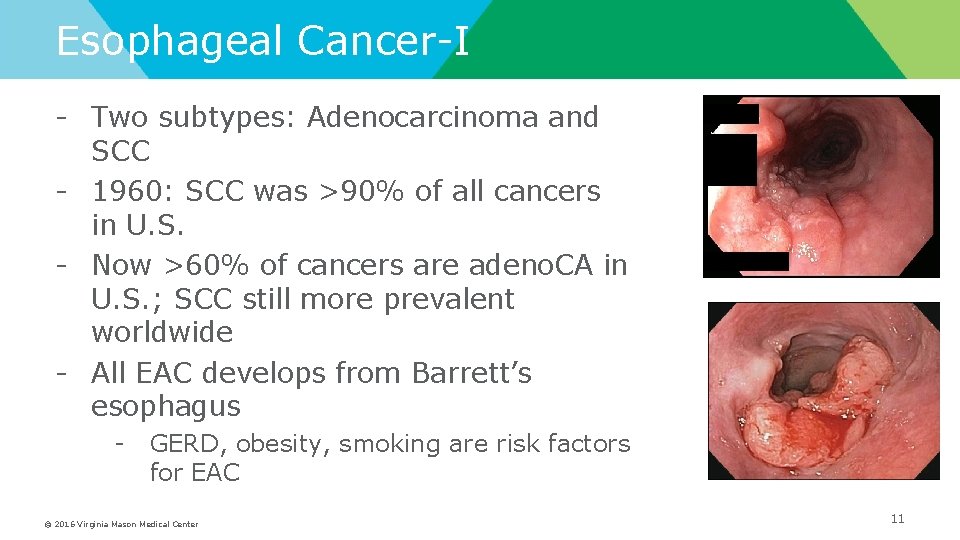
Esophageal Cancer-I - Two subtypes: Adenocarcinoma and SCC - 1960: SCC was >90% of all cancers in U. S. - Now >60% of cancers are adeno. CA in U. S. ; SCC still more prevalent worldwide - All EAC develops from Barrett’s esophagus - GERD, obesity, smoking are risk factors for EAC © 2016 Virginia Mason Medical Center 11
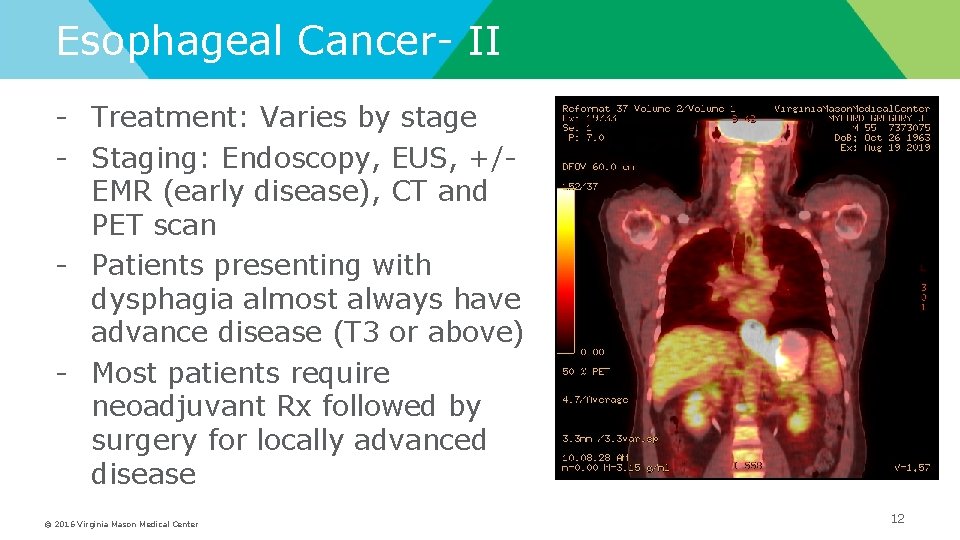
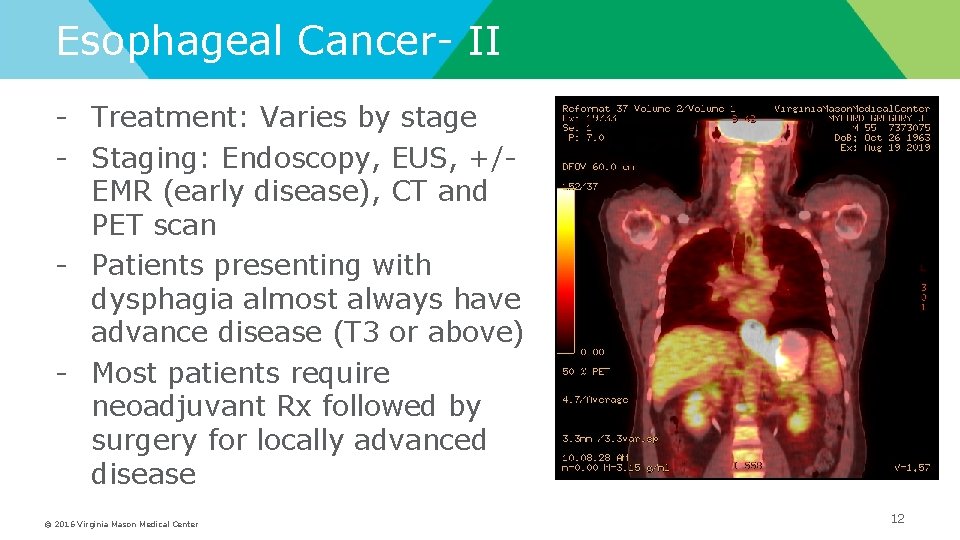
Esophageal Cancer- II - Treatment: Varies by stage - Staging: Endoscopy, EUS, +/EMR (early disease), CT and PET scan - Patients presenting with dysphagia almost always have advance disease (T 3 or above) - Most patients require neoadjuvant Rx followed by surgery for locally advanced disease © 2016 Virginia Mason Medical Center 12
Ideal Device for Palliation of Dysphagia in Malignancy - Effective Easily applied Minimally invasive Rapid in onset of effect Minimal need for re-intervention Minimal side effects (which are tolerable) Few or no complications © 2016 Virginia Mason Medical Center Dua K, Gastrointes Endosc 2007; 65(1): 77
Stenting for Malignancy: Efficacy - Technical success rate nears 100% – Guidewire passage=stent placement - Improvement in dysphagia is nearly universal – Tumors that cross GE junction are an exception - Procedure-related adverse events in 10% – Perforation, bleeding, aspiration, pain - Delayed complications: 35% – Bleeding, fistula, GE reflux, stent migration, stent occlusion, granulation, migration © 2016 Virginia Mason Medical Center
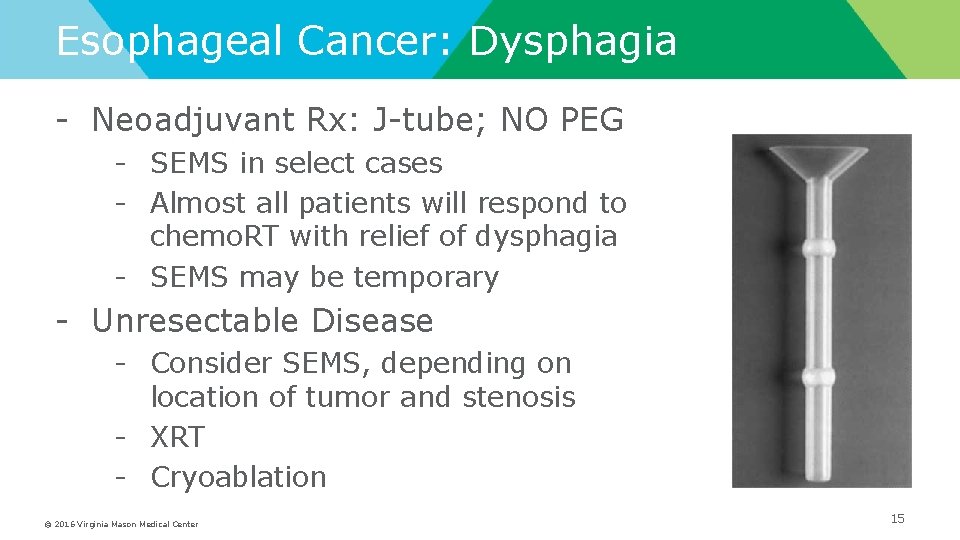
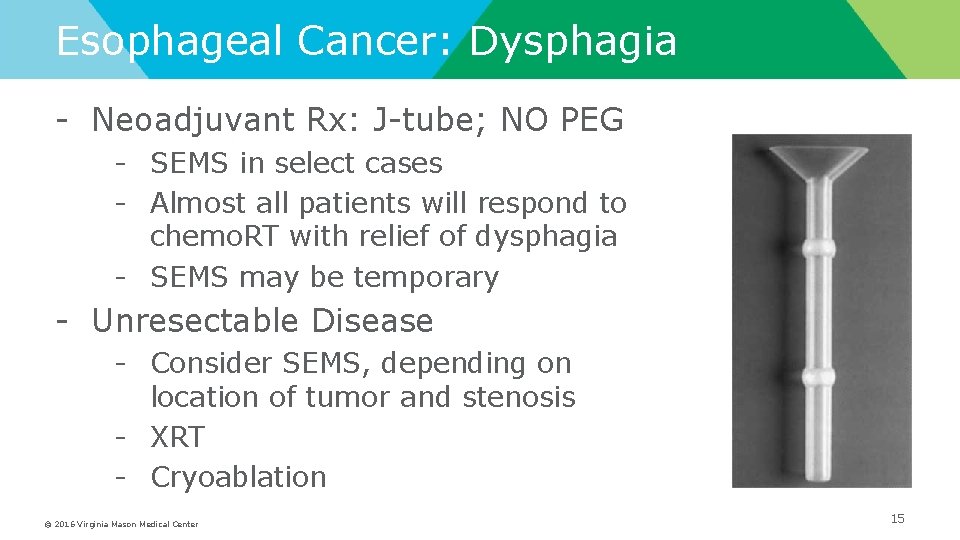
Esophageal Cancer: Dysphagia - Neoadjuvant Rx: J-tube; NO PEG - SEMS in select cases - Almost all patients will respond to chemo. RT with relief of dysphagia - SEMS may be temporary - Unresectable Disease - Consider SEMS, depending on location of tumor and stenosis - XRT - Cryoablation © 2016 Virginia Mason Medical Center 15
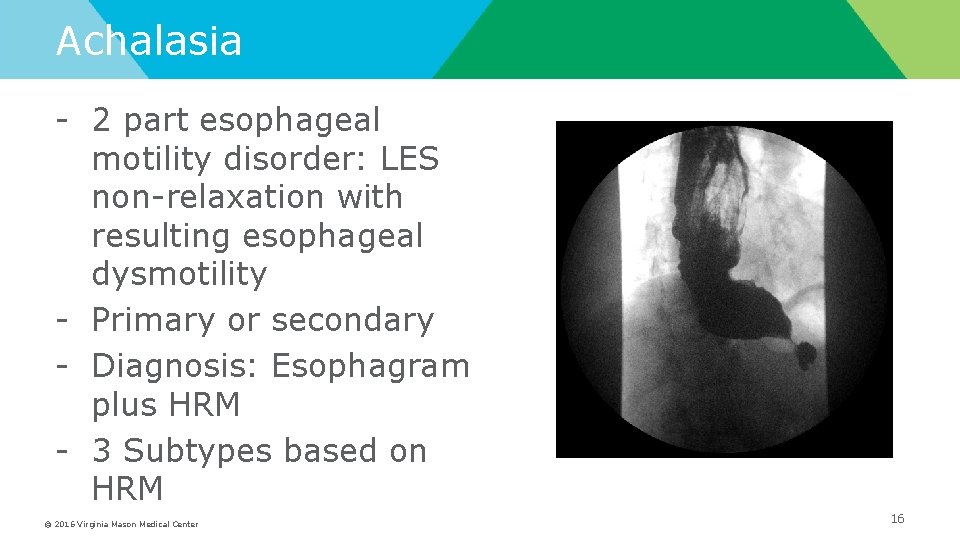
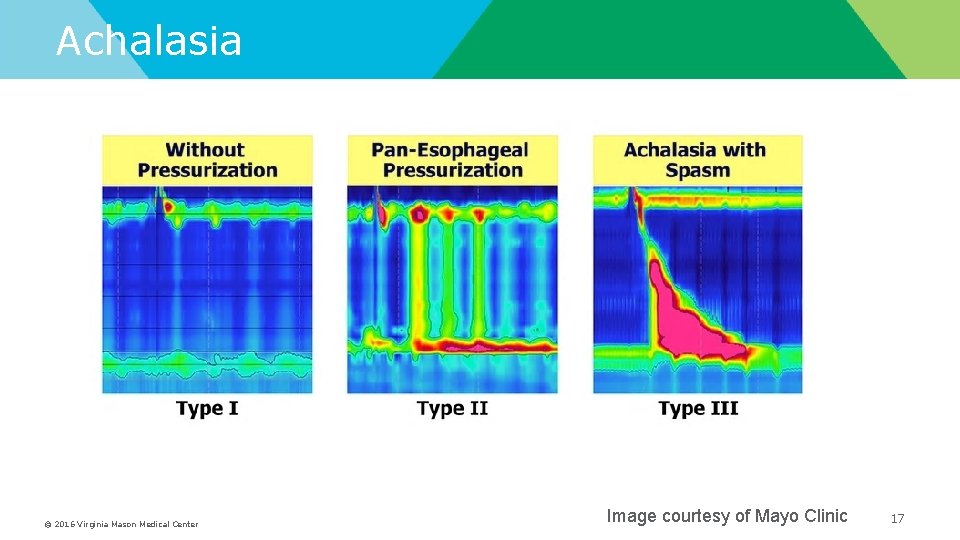
Achalasia - 2 part esophageal motility disorder: LES non-relaxation with resulting esophageal dysmotility - Primary or secondary - Diagnosis: Esophagram plus HRM - 3 Subtypes based on HRM © 2016 Virginia Mason Medical Center 16
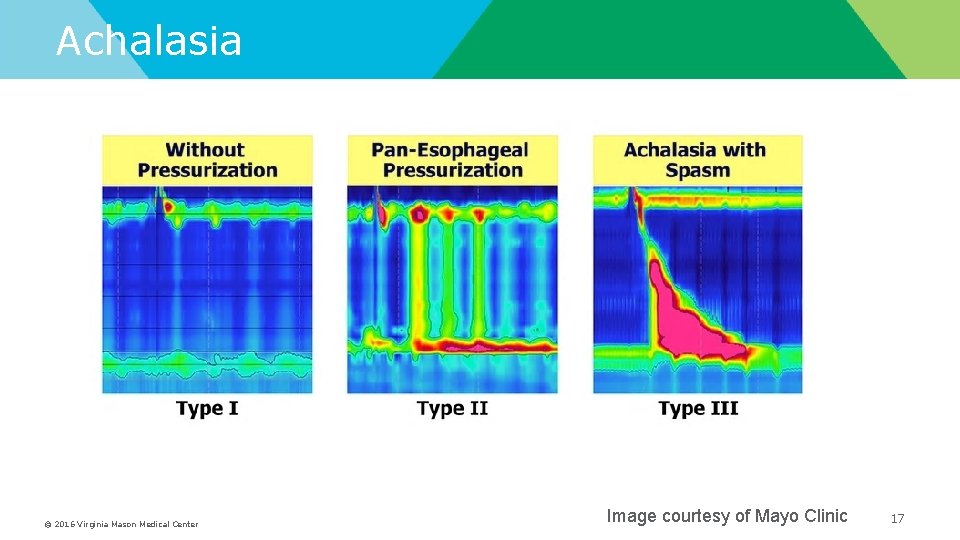
Achalasia © 2016 Virginia Mason Medical Center Image courtesy of Mayo Clinic 17
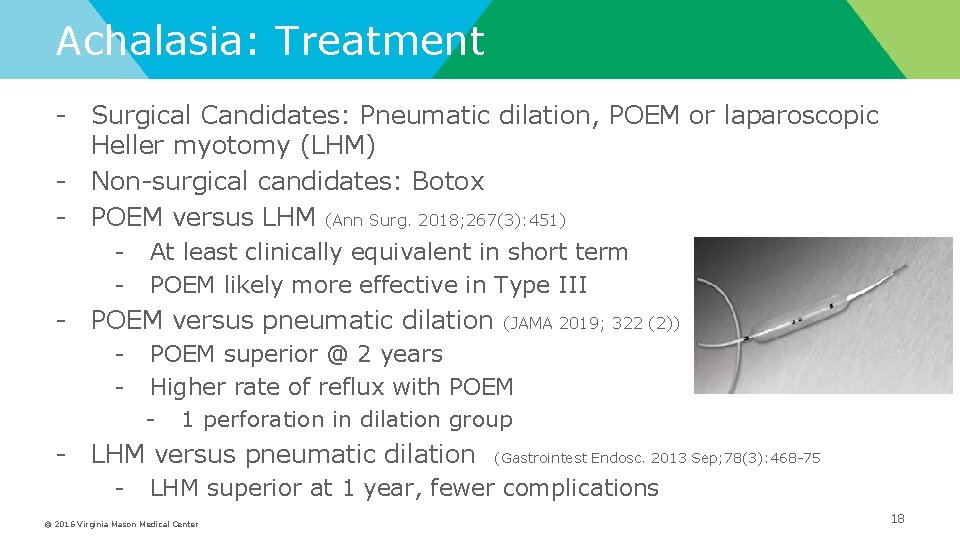
Achalasia: Treatment - Surgical Candidates: Pneumatic dilation, POEM or laparoscopic Heller myotomy (LHM) - Non-surgical candidates: Botox - POEM versus LHM (Ann Surg. 2018; 267(3): 451) - At least clinically equivalent in short term POEM likely more effective in Type III - POEM versus pneumatic dilation - POEM superior @ 2 years Higher rate of reflux with POEM - 1 perforation in dilation group - LHM versus pneumatic dilation - (JAMA 2019; 322 (2)) (Gastrointest Endosc. 2013 Sep; 78(3): 468 -75 LHM superior at 1 year, fewer complications © 2016 Virginia Mason Medical Center 18
Summary - The differential diagnosis for dysphagia is wide - Patient history, presence of alarm symptoms is key in directing work-up - Contrast-enhanced imaging, endoscopy and manometry are the critical diagnostic tools required as part of the work-up of dysphagia - Treatment approaches are directed at the underlying etiology and vary widely based on the clinical scenario © 2016 Virginia Mason Medical Center 19