ESI TRIAGE V 4 Emergency Severity Index Triage

- Slides: 50
ESI TRIAGE V 4 Emergency Severity Index Triage Helen Kuhns, RN, CEN Emergency Room Educator 2012
Instructions This program is in intended for RNs working in Emergency Departments throughout SLUHN. Review the entire Power. Point® presentation including the content of the Nurse First Protocol Summary Sheet. Exit the Power. Point® and Take Test. Please note: The posttest is 25 questions. RNs must attain 90% on the first attempt. Although the Tracker Trainer system will allow those who score <90% to retest immediately, a report will be sent to the educator/manager follow up and scheduling of a remediation class.
Why is this education necessary? This education program has been developed to review the overall process of ESI Triage in the Emergency Departments. Approximately 46% of the overall ED patient population falls under the ESI Level 3. Random audits of the ESI Level 3 patients have shown that nurses tend to over triage to a Level 3 when the patient is really Level 4. Result: the patient spends an average of 1 -2 hours longer in the ED. Accurate triage is an essential functioning component of every ED. Assigning the patient the correct ESI Level places them in the right zone to receive the right resources in a reasonable amount of time. Accuracy in this process will increase ED through put and patient satisfaction.
OBJECTIVES After completing this program, the RN will be able to: List interventions that are considered resources Describe each ESI Level and the resources associated with each level Define criteria and interventions required for all Nurse First Protocols
What is ESI? Emergency Severity Index
History of ESI Developed in 1999 by 2 Emergency Room physicians Established to prioritize patients in the ED based on the urgency of the patient’s condition Levels are based on the number of resources the patient will need to move through the system
Goal Of ESI To establish patient urgency and patient streaming… What? Getting the right patient to the right resources at the right place and right time. Waiting room High side Psychiatric room OB Fast track Trauma Bay
Benefits of ESI Triage Rapid sorting of patients Improved patient flow through the ED Reliable resource management Standardized hand off tool
TOOLS USED TO TRIAGE Patient interview Age Past medial history Gross observation of the patient Nurses’ “Sixth Sense”
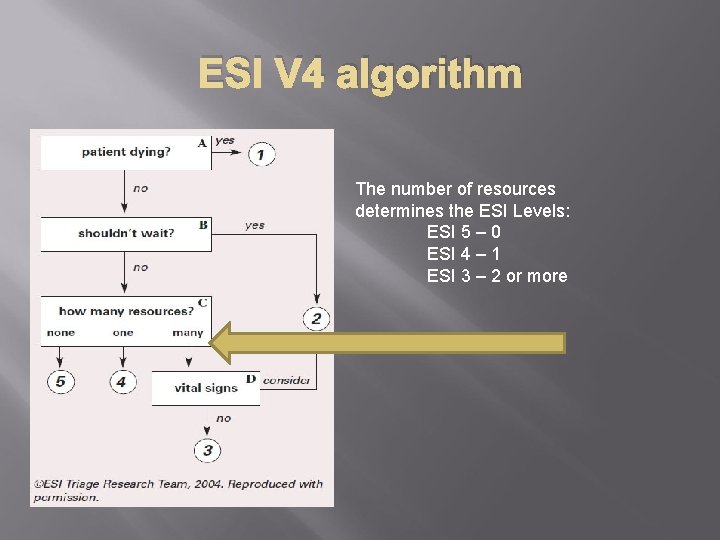
ESI TOOL The RN will utilize the 4 decision points on the ESI V 4 algorithm Does the patient require immediate life-saving interventions? Is this a patient that should not wait? How many different resources are needed? What are the patients vital signs?
Does the patient require life-saving intervention? Life-saving interventions are aimed at: Securing an airway Maintaining breathing Supporting circulation
Does the patient meet any of the following criteria? Already intubated? Apneic? Pulseless? Severe respiratory distress? Sp. O 2<90%? Acute mental status changes? Unresponsive? …
If your patient has any of the previous situations/conditions they are an ESI LEVEL 1
ESI LEVEL 1 Requires immediate physician involvement Cardiac Pulseless Life threatening rhythm Respiratory Intubation required to maintain ventilation Level of consciousness P or U (use AVPU)
Examples of ESI Level 1 Cardiac/Respiratory arrest Overdose with a resp. rate of 6 Severe bradycardia or tachycardia with signs of hypoperfusion Hypotension with signs of hypoperfusion Chest pain, pale, diaphoretic, blood pressure 70/palp Anaphylactic reaction Flaccid baby
If the patient does not meet ESI level 1 criteria ask: Should the patient wait?
Ask yourself the next three questions to determine if the patient should wait ESI Level 2 Is this a high risk situation? Is the patient confused, lethargic, or disoriented? Is the patient in severe pain or distress The nurse obtains pertinent subjective and objective information to quickly answer these questions…
Is this a high risk situation? Condition could deteriorate (i. e. Overdose) Conditions requiring time-sensitive treatment (i. e. Symptomatic bradycardia/tachycardia) Potential major life or organ threat Describes a clinical portrait that the nurse recognizes as a high risk situation
Examples of high risk situations Active chest pain that does not meet criteria of Level 1 Stroke symptoms not meeting criteria of Level 1 “Rule out” ectopic pregnancy; hemodynamically stable Current chemotherapy with a fever Suicidal or homicidal ideation
Is the patient Confused, Lethargic, or Disoriented? Is this patient demonstrating an acute change in mental status? Confused: inappropriate response to stimuli, decrease in attention span or memory Lethargic: drowsy, sleeping more than usual, responds appropriately when stimulated Disoriented: unable to answer questions correctly about time, place, and person
Examples of Confused, Lethargic, or Disoriented patients New onset of confusion in an elderly patient The 3 -month-old whose mother reports the child is sleeping all the time The adolescent found confused and disoriented *These examples indicate that the brain may be either structurally or chemically compromised
Is this patient in Severe Pain or Distress? Yes Assess level of pain or distress Observation Self reported pain rating using standard scale (Severe pain is > 7 utilizing the 1 -10 rating scale ) No Move to the next step in the triage algorithm
Pain and Distress assessment Pain Clinical observation Distressed facial expression, diaphoresis, body posture, changes in vital signs RN observation of physical responses that supports the patient’s pain rating Distress Physical Psychological
Examples of pain and distress Sexual Assault Combative Suicidal Renal Colic with ↑ pain Fracture/Dislocation
ESI LEVEL 2 Placement and treatment should occur within 10 minutes of arrival Nurse First Protocols should be initiated without delay Notify the physician of the patient’s condition Pain/distress should be addressed upon placement in a treatment area
How many resources are needed? How many resources will be needed for the physician to reach a disposition decision? RN needs to draw on past experiences in caring for similar patients Based on prudent and customary practices What Nurse First Protocol will be used if any( see Nurse First Protocol Summary Sheet)? Based on brief objective and subjective interview Age, PMH, allergies, age, gender and medications Individual physician practice patterns should not be considered
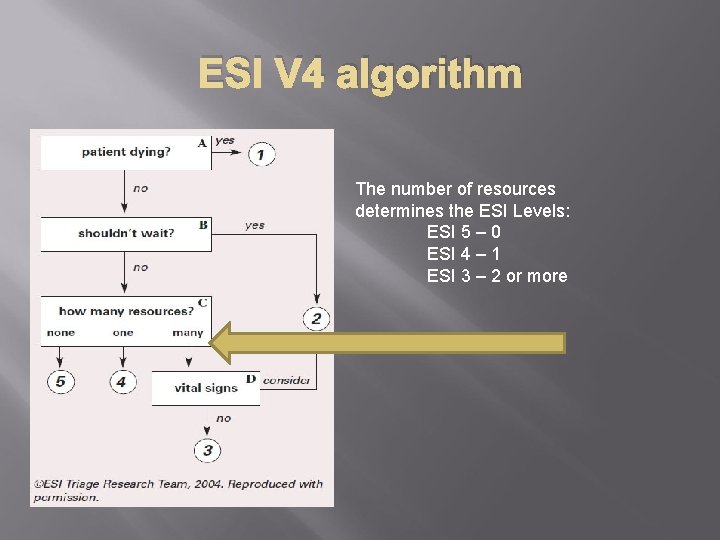
ESI V 4 algorithm The number of resources determines the ESI Levels: ESI 5 – 0 ESI 4 – 1 ESI 3 – 2 or more
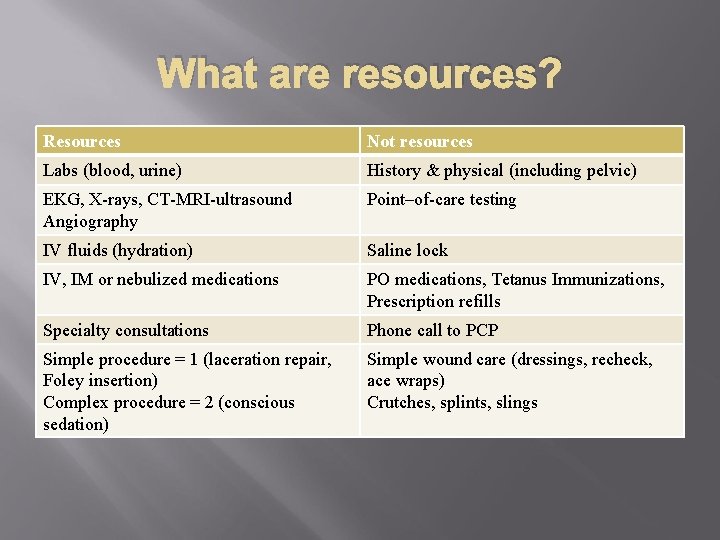
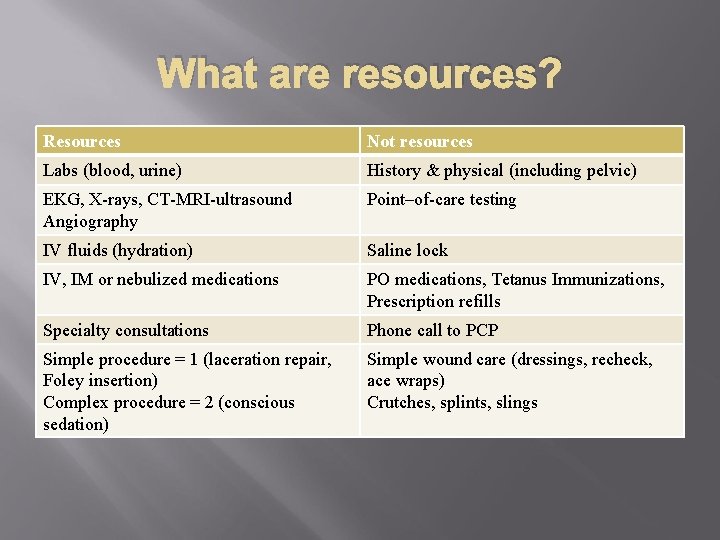
What are resources? Resources Not resources Labs (blood, urine) History & physical (including pelvic) EKG, X-rays, CT-MRI-ultrasound Angiography Point–of-care testing IV fluids (hydration) Saline lock IV, IM or nebulized medications PO medications, Tetanus Immunizations, Prescription refills Specialty consultations Phone call to PCP Simple procedure = 1 (laceration repair, Foley insertion) Complex procedure = 2 (conscious sedation) Simple wound care (dressings, recheck, ace wraps) Crutches, splints, slings
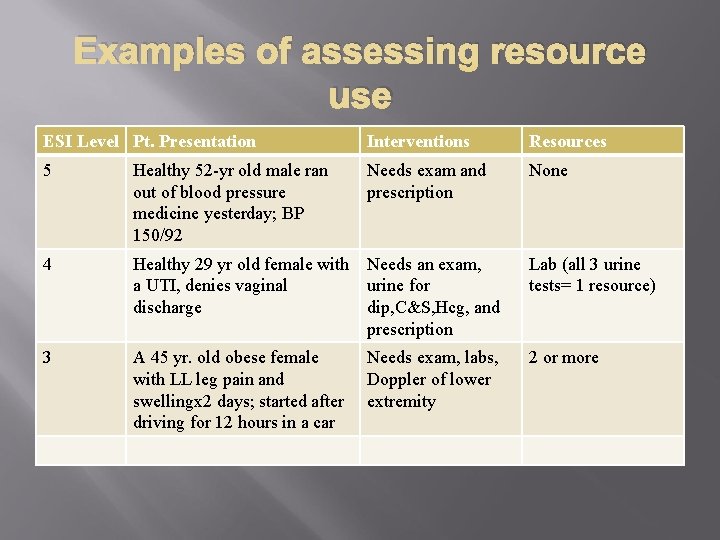
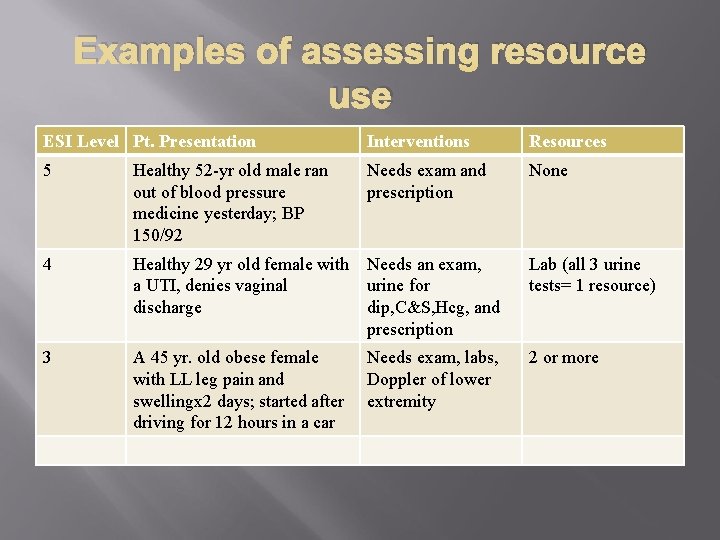
Examples of assessing resource use ESI Level Pt. Presentation Interventions Resources 5 Healthy 52 -yr old male ran out of blood pressure medicine yesterday; BP 150/92 Needs exam and prescription None 4 Healthy 29 yr old female with Needs an exam, a UTI, denies vaginal urine for discharge dip, C&S, Hcg, and prescription Lab (all 3 urine tests= 1 resource) 3 A 45 yr. old obese female with LL leg pain and swellingx 2 days; started after driving for 12 hours in a car 2 or more Needs exam, labs, Doppler of lower extremity
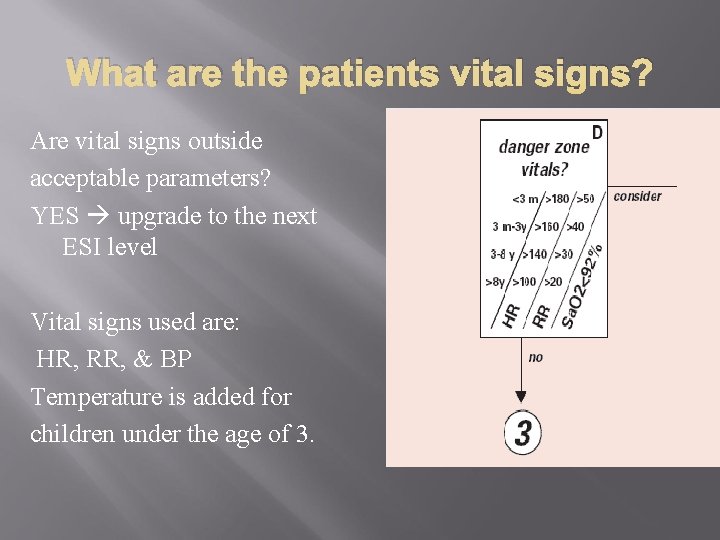
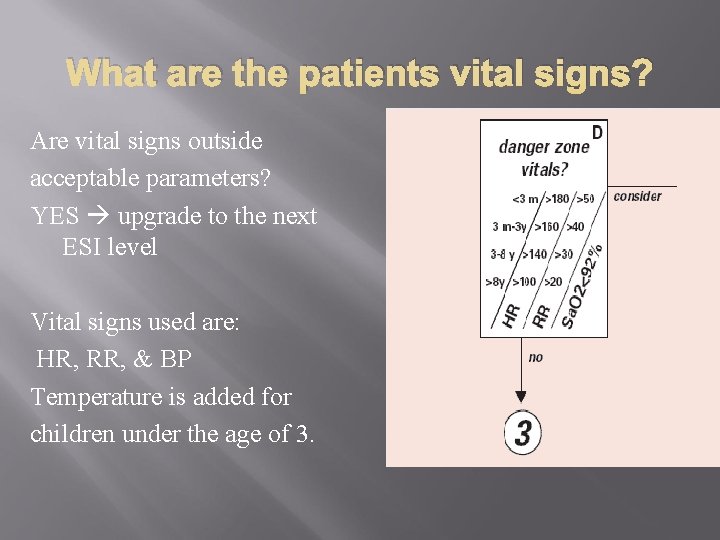
What are the patients vital signs? Are vital signs outside acceptable parameters? YES upgrade to the next ESI level Vital signs used are: HR, RR, & BP Temperature is added for children under the age of 3.
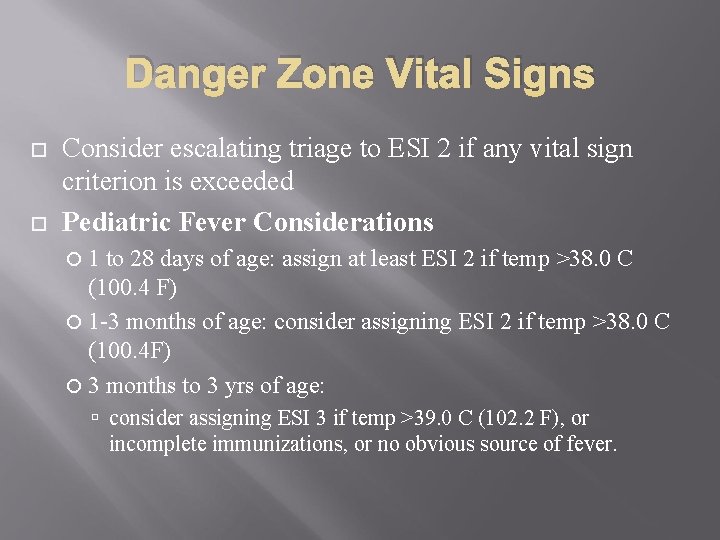
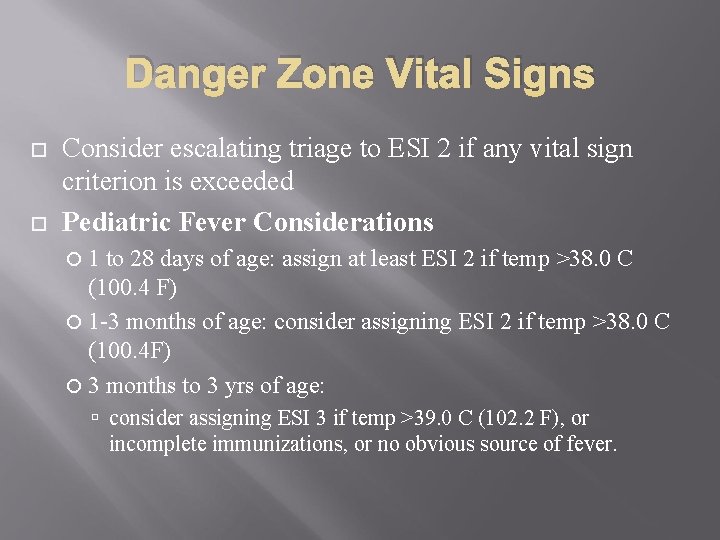
Danger Zone Vital Signs Consider escalating triage to ESI 2 if any vital sign criterion is exceeded Pediatric Fever Considerations 1 to 28 days of age: assign at least ESI 2 if temp >38. 0 C (100. 4 F) 1 -3 months of age: consider assigning ESI 2 if temp >38. 0 C (100. 4 F) 3 months to 3 yrs of age: consider assigning ESI 3 if temp >39. 0 C (102. 2 F), or incomplete immunizations, or no obvious source of fever.
Does time to triage influence ESI triage category? ESI does not mandate specific time standards in which a patient must be evaluated by a physician ESI 1 patients need to be seen upon arrival based on their presenting problem ESI 2 should be seen as soon as possible ESI 3 can wait to be seen based on the fact that their vital signs are stable and they will require a more in depth evaluation process ESI 4 & 5 are stable and could wait hours to be seen
Key concepts to remember Trauma Levels and ESI levels are separate systems and should not be confused Do not under triage patients based on physician practice or the volume in the ED When faced with multiple ESI level 2 patients: Evaluate based on the ESI algorithm Inform the charge nurse of the order of priority based on those with the highest risk
Summary ESI is a 5 level triage system that is simple to use and divides patients by acuity and resources needed. The ESI algorithm is based on four key decision points The experienced ED nurse will be able to rapidly and accurately triage patients using this system

NURSE FIRST PROTOCOL REVIEW
NURSE FIRST PROTOCOLS Please review the Nurse First Protocols prior to taking the test. Knowledge of the inclusion criteria and the resources required for specific conditions is key to assigning the correct ESI level to the patient.
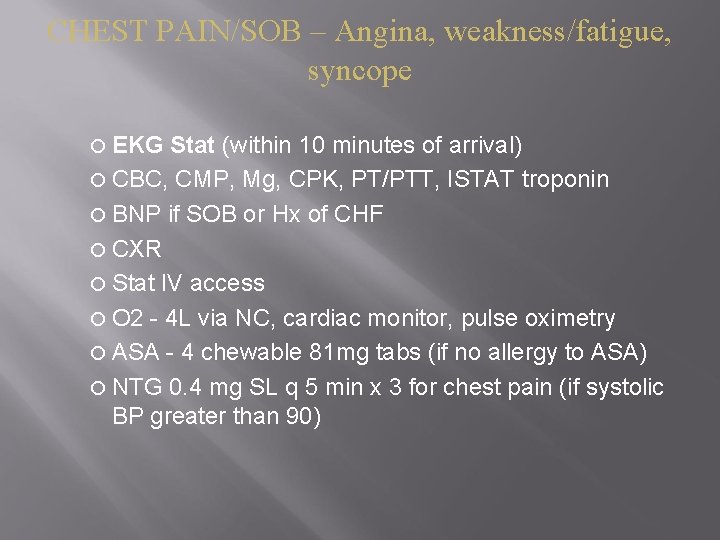
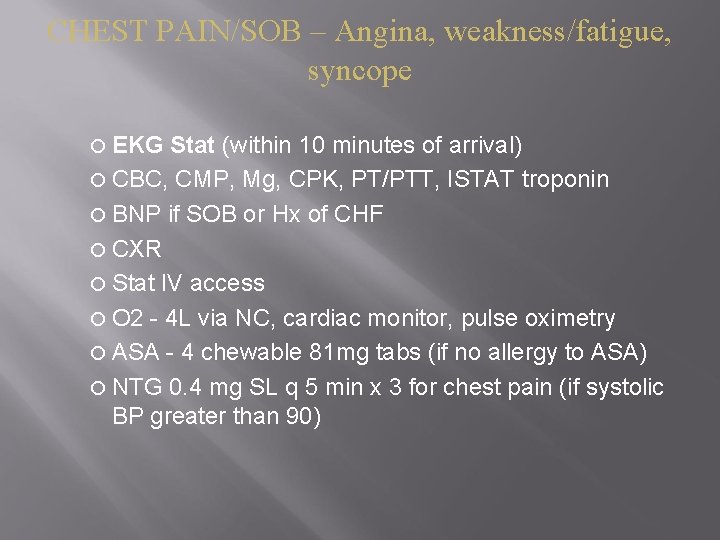
CHEST PAIN/SOB – Angina, weakness/fatigue, syncope EKG Stat (within 10 minutes of arrival) CBC, CMP, Mg, CPK, PT/PTT, ISTAT troponin BNP if SOB or Hx of CHF CXR Stat IV access O 2 - 4 L via NC, cardiac monitor, pulse oximetry ASA - 4 chewable 81 mg tabs (if no allergy to ASA) NTG 0. 4 mg SL q 5 min x 3 for chest pain (if systolic BP greater than 90)
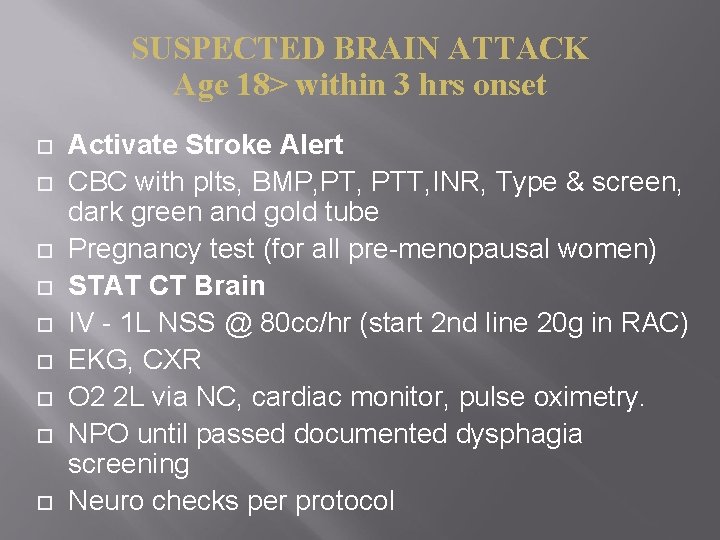
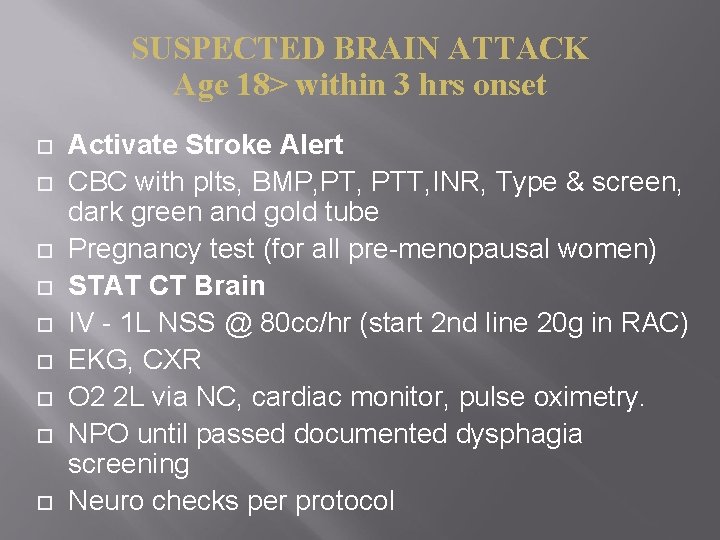
SUSPECTED BRAIN ATTACK Age 18> within 3 hrs onset Activate Stroke Alert CBC with plts, BMP, PTT, INR, Type & screen, dark green and gold tube Pregnancy test (for all pre-menopausal women) STAT CT Brain IV - 1 L NSS @ 80 cc/hr (start 2 nd line 20 g in RAC) EKG, CXR O 2 2 L via NC, cardiac monitor, pulse oximetry. NPO until passed documented dysphagia screening Neuro checks per protocol
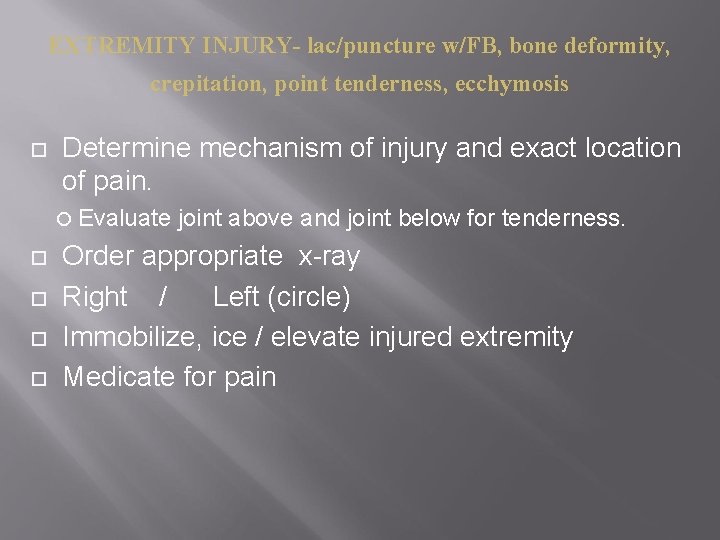
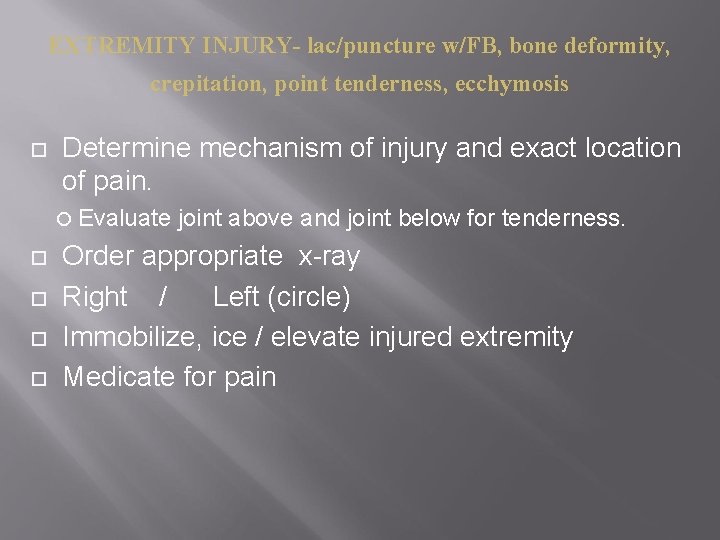
EXTREMITY INJURY- lac/puncture w/FB, bone deformity, crepitation, point tenderness, ecchymosis Determine mechanism of injury and exact location of pain. Evaluate joint above and joint below for tenderness. Order appropriate x-ray Right / Left (circle) Immobilize, ice / elevate injured extremity Medicate for pain
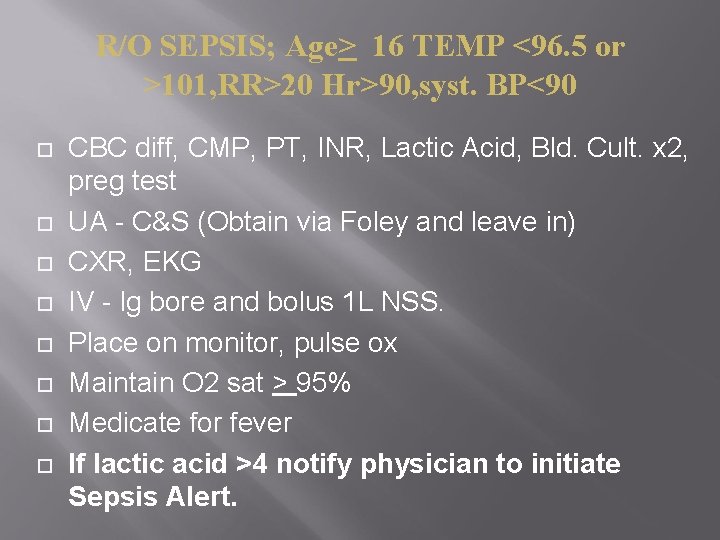
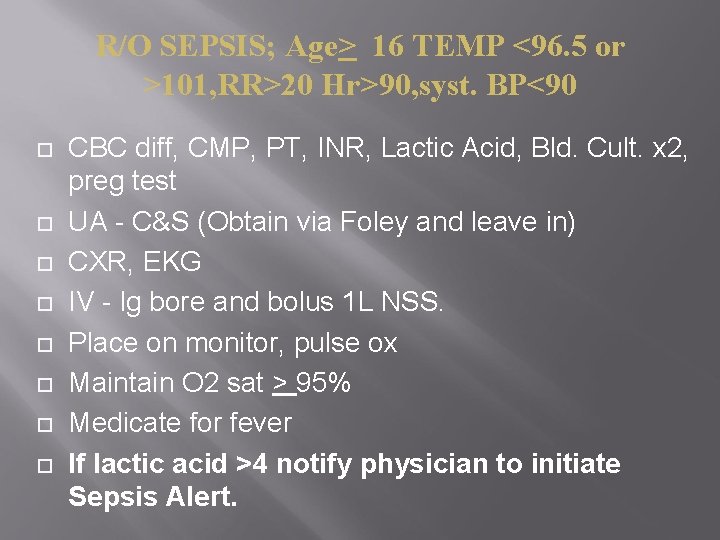
R/O SEPSIS; Age> 16 TEMP <96. 5 or >101, RR>20 Hr>90, syst. BP<90 CBC diff, CMP, PT, INR, Lactic Acid, Bld. Cult. x 2, preg test UA - C&S (Obtain via Foley and leave in) CXR, EKG IV - lg bore and bolus 1 L NSS. Place on monitor, pulse ox Maintain O 2 sat > 95% Medicate for fever If lactic acid >4 notify physician to initiate Sepsis Alert.
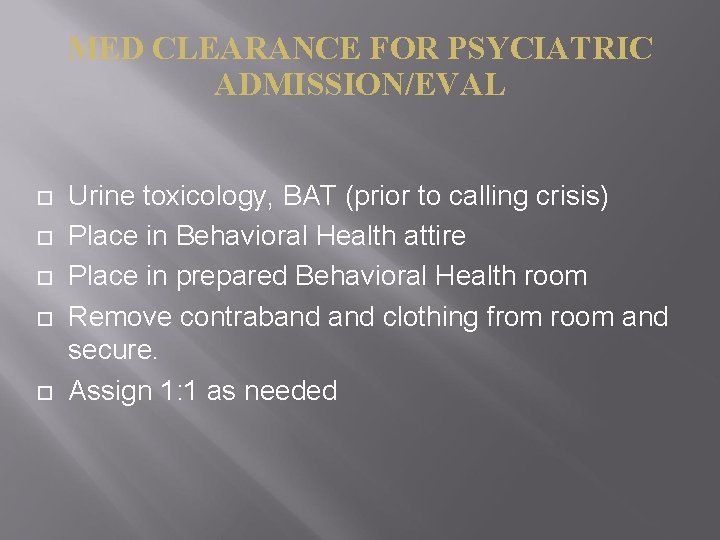
MED CLEARANCE FOR PSYCIATRIC ADMISSION/EVAL Urine toxicology, BAT (prior to calling crisis) Place in Behavioral Health attire Place in prepared Behavioral Health room Remove contraband clothing from room and secure. Assign 1: 1 as needed
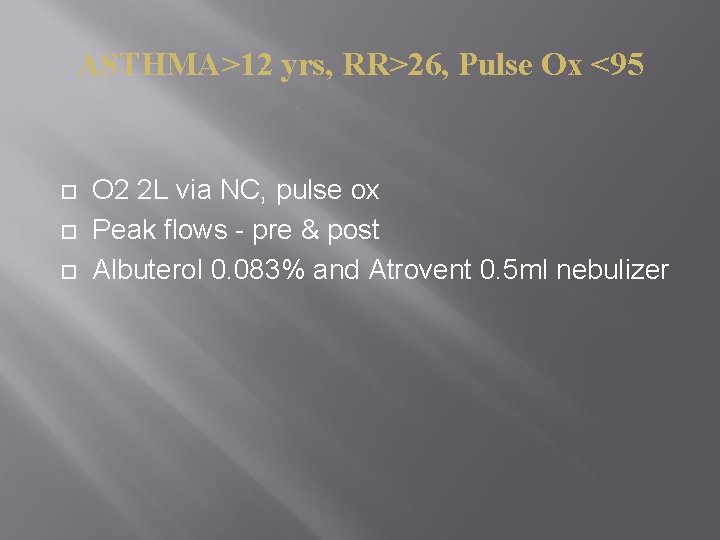
ASTHMA>12 yrs, RR>26, Pulse Ox <95 O 2 2 L via NC, pulse ox Peak flows - pre & post Albuterol 0. 083% and Atrovent 0. 5 ml nebulizer
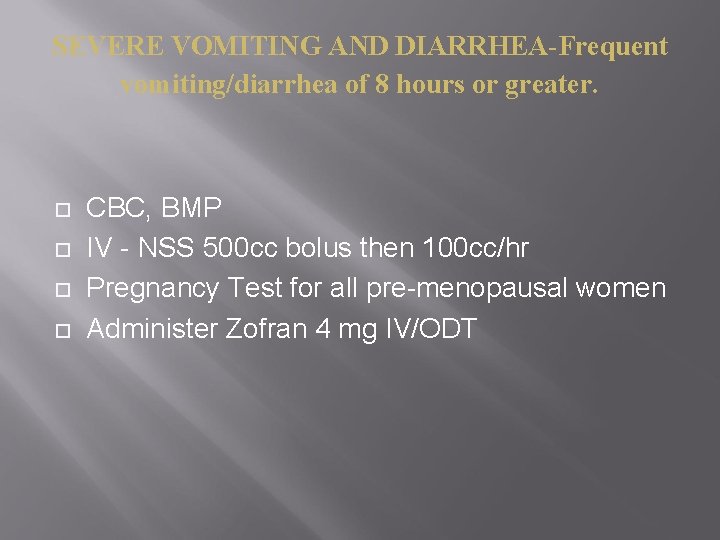
SEVERE VOMITING AND DIARRHEA-Frequent vomiting/diarrhea of 8 hours or greater. CBC, BMP IV - NSS 500 cc bolus then 100 cc/hr Pregnancy Test for all pre-menopausal women Administer Zofran 4 mg IV/ODT
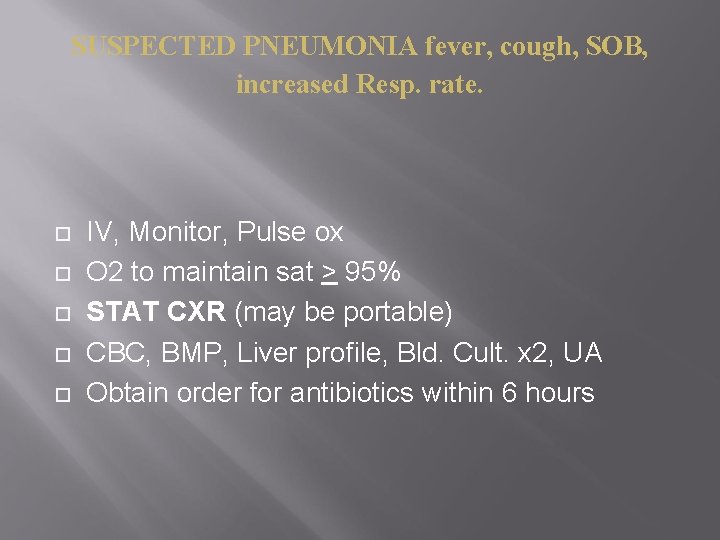
SUSPECTED PNEUMONIA fever, cough, SOB, increased Resp. rate. IV, Monitor, Pulse ox O 2 to maintain sat > 95% STAT CXR (may be portable) CBC, BMP, Liver profile, Bld. Cult. x 2, UA Obtain order for antibiotics within 6 hours
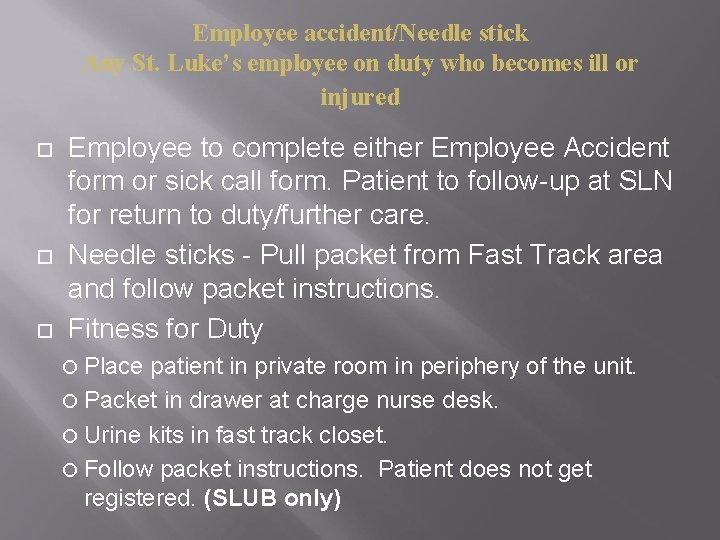
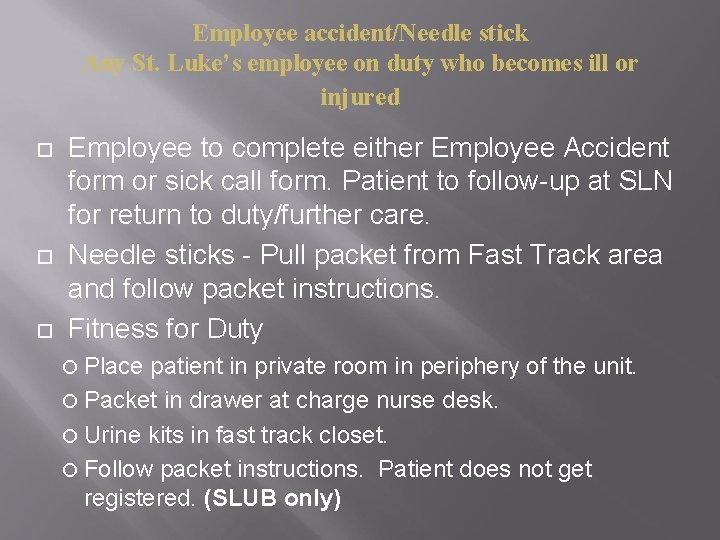
Employee accident/Needle stick Any St. Luke’s employee on duty who becomes ill or injured Employee to complete either Employee Accident form or sick call form. Patient to follow-up at SLN for return to duty/further care. Needle sticks - Pull packet from Fast Track area and follow packet instructions. Fitness for Duty Place patient in private room in periphery of the unit. Packet in drawer at charge nurse desk. Urine kits in fast track closet. Follow packet instructions. Patient does not get registered. (SLUB only)
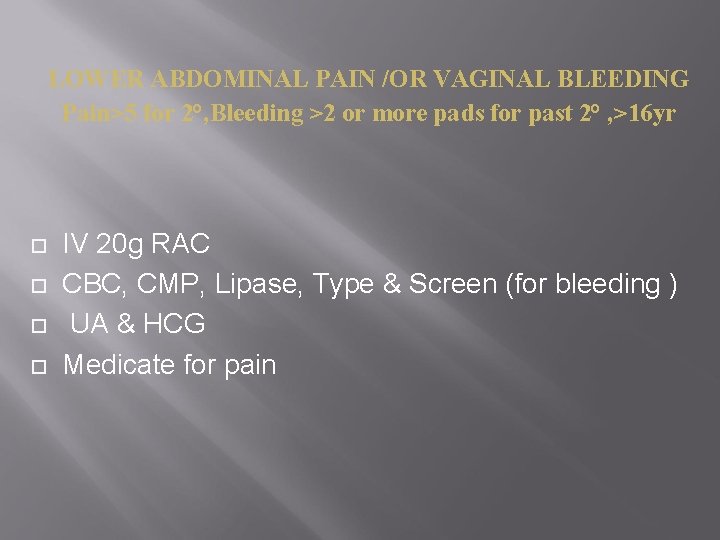
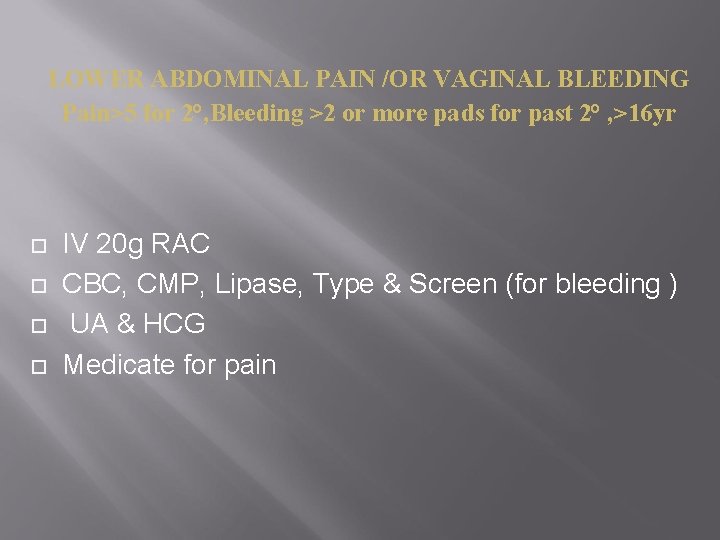
LOWER ABDOMINAL PAIN /OR VAGINAL BLEEDING Pain>5 for 2°, Bleeding >2 or more pads for past 2° , >16 yr IV 20 g RAC CBC, CMP, Lipase, Type & Screen (for bleeding ) UA & HCG Medicate for pain
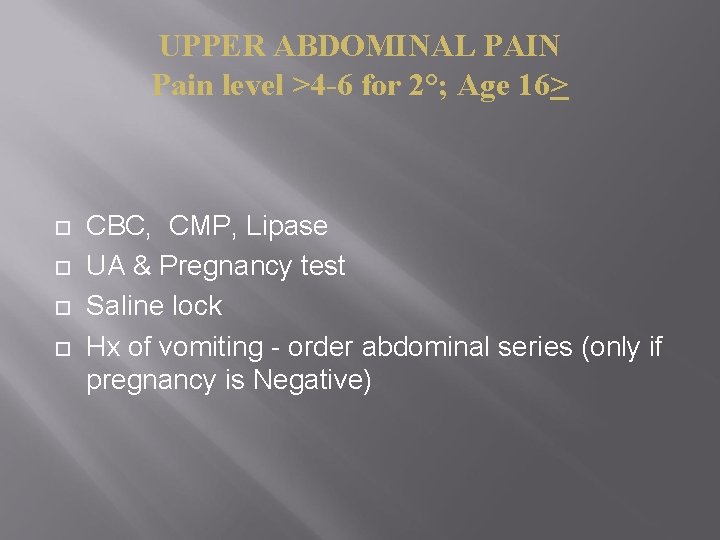
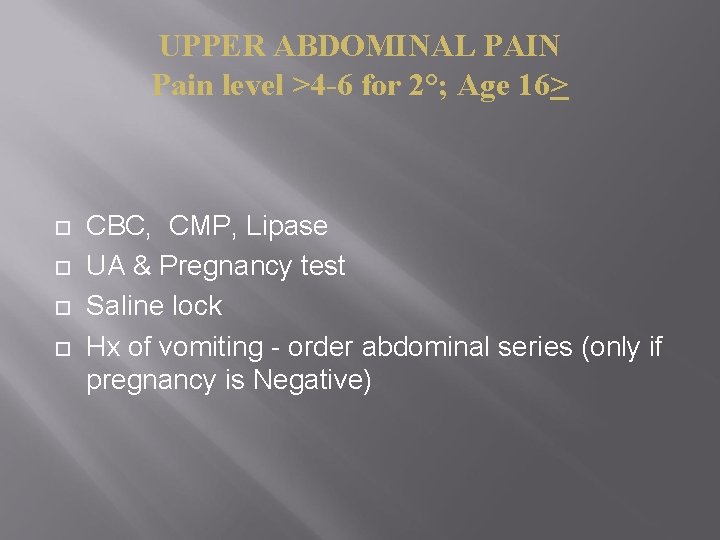
UPPER ABDOMINAL PAIN Pain level >4 -6 for 2°; Age 16> CBC, CMP, Lipase UA & Pregnancy test Saline lock Hx of vomiting - order abdominal series (only if pregnancy is Negative)
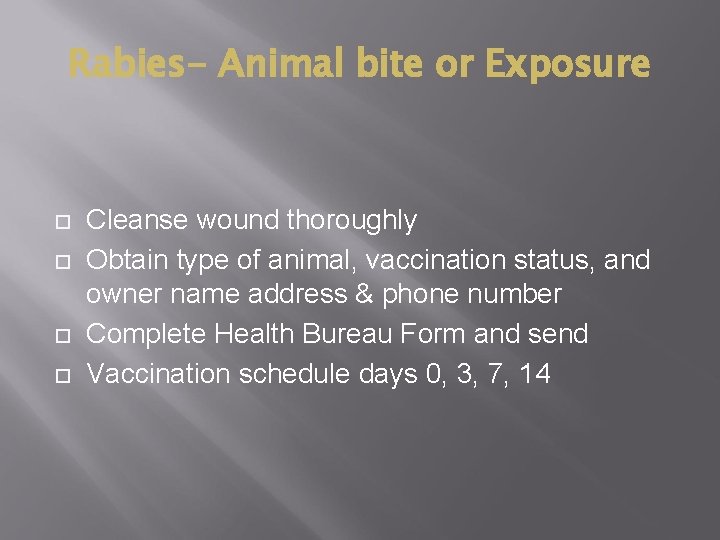
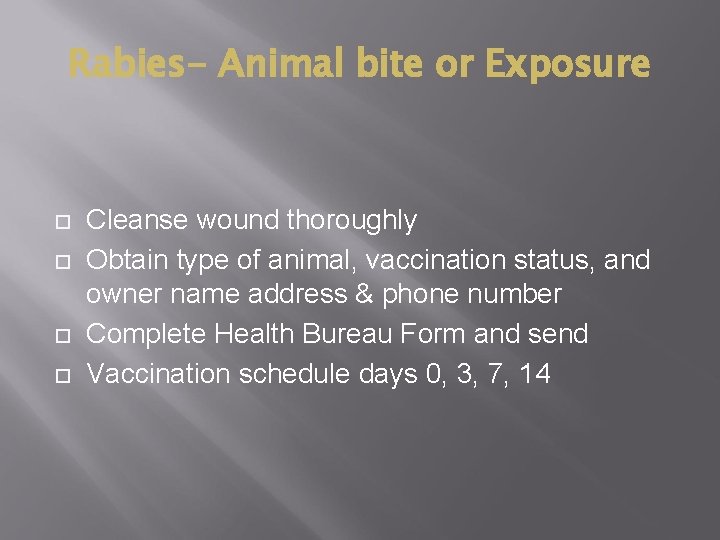
Rabies- Animal bite or Exposure Cleanse wound thoroughly Obtain type of animal, vaccination status, and owner name address & phone number Complete Health Bureau Form and send Vaccination schedule days 0, 3, 7, 14
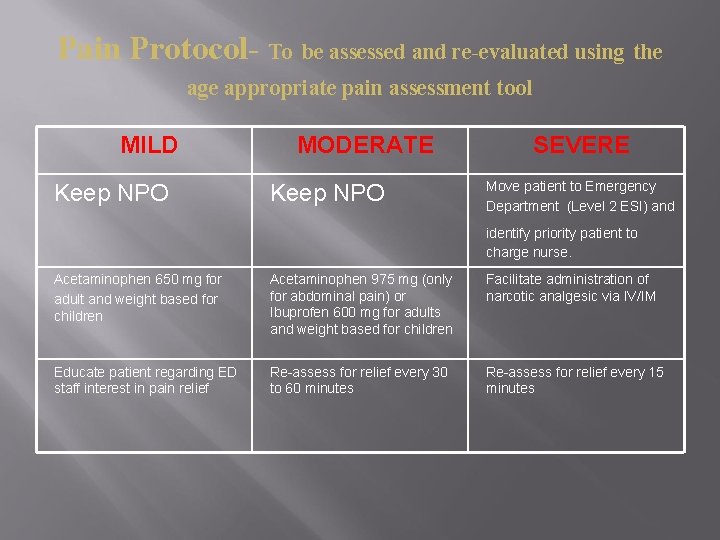
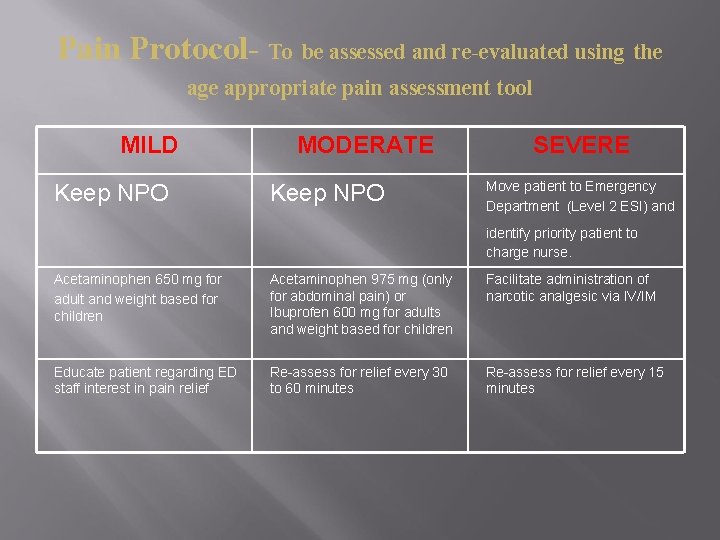
Pain Protocol- To be assessed and re-evaluated using the age appropriate pain assessment tool MILD Keep NPO MODERATE Keep NPO SEVERE Move patient to Emergency Department (Level 2 ESI) and identify priority patient to charge nurse. Acetaminophen 650 mg for adult and weight based for children Acetaminophen 975 mg (only for abdominal pain) or Ibuprofen 600 mg for adults and weight based for children Facilitate administration of narcotic analgesic via IV/IM Educate patient regarding ED staff interest in pain relief Re-assess for relief every 30 to 60 minutes Re-assess for relief every 15 minutes
Please proceed to Tracker Trainer to complete the post test.