Escherichia coli Scientific classification Domain Bacteria Phylum Gamma
Escherichia coli Scientific classification: Domain: Bacteria Phylum: Gamma Proteobacteria Class: Proteobacteria Order: Enterobacteriales Family: Enterobacteriaceae Genus: Escherichia Species: E. coli

Theodor Escherich first described E. coli in 1885, as Bacterium coli commune, which he isolated from the feces of newborns. It was later renamed Escherichia coli.

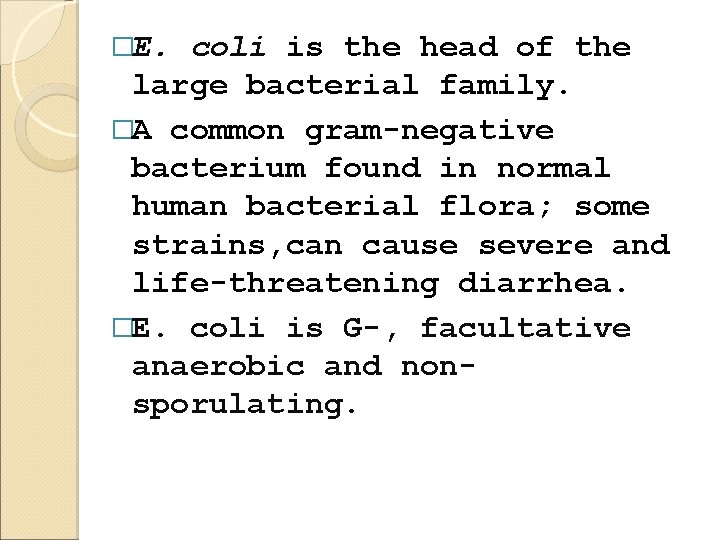
�E. coli is the head of the large bacterial family. �A common gram-negative bacterium found in normal human bacterial flora; some strains, can cause severe and life-threatening diarrhea. �E. coli is G-, facultative anaerobic and nonsporulating.
The cells are about 2 micrometres (μm) long and 0. 5 μm in diameter, with a cell volume of 0. 6 - 0. 7 μm 3. �Strains that possess flagella can swim and are motile, but other strains lack flagellum. •
• The flagella of E. coli have a peritrichous arrangement. • It can sense the presence or absence of chemicals and gases in its environment and swim towards or away from them. • It can stop swimming and grow fimbriae that will specifically attach it to a cell or surface receptor
�E. coli can grow in media with glucose as the sole organic constituent. �It can live on a wide variety of substrates. �Wild-type E. coli has no growth factor requirements, and metabolically it can transform glucose into all of the macromolecular components that make up the cell.
�The bacterium can grow in the presence or absence of O 2. • Under anaerobic conditions it will grow by means of fermentation. • E. coli uses mixed-acid fermentation in anaerobic conditions, producing lactate, succinate, ethanol, acetate and carbon dioxide.
�However, it can also grow by means of anaerobic respiration, since it is able to utilize NO 3, NO 2 or fumarate as final electron acceptors for respiratory electron transport processes.
�In part, this adapts E. coli to its intestinal (anaerobic) and its extraintestinal (aerobic or anaerobic) habitats. • Optimal growth of E. coli occurs at 37°C, but some laboratory strains can multiply at temperatures of up to 49°C. • Growth can be driven by aerobic or anaerobic respiration.
�Growth on Endo or Mac. Conkey media (lactose-positive colonies): media become red in color. �Pathogenic strains of E. coli are responsible for three types of infections in humans: urinary tract infections (UTI), neonatal meningitis, and intestinal diseases (gastroenteritis).
�The regular presence of E. coli in the human intestine and feces has led to tracking the bacterium in nature as an indicator of fecal pollution and water contamination. �As a pathogen, E. coli is best known for its ability to cause intestinal diseases.
�Five classes (serogroups) of E. coli that cause diarrheal diseases are now recognized: ü Enterotoxigenic E. coli (ETEC), ü enteropathogenic E. coli (EPEC), ü enteroinvasive E. coli (EIEC), ü enterohemorrhagic E. coli (EHEC), and ü enteroaggregative E. coli (EAEC).
�Enterotoxigenic E. coli(ETEC) o is an important cause of diarrhea in infants and travelers in underdeveloped countries or regions of poor sanitation. o It has been implicated in sporadic waterborne outbreaks, as well as due to the consumption of soft cheeses and raw vegetables.
o The diseases vary from minor discomfort to a severe cholera-like syndrome. � o ETEC are acquired by ingestion of contaminated food and water, and adults in endemic areas evidently develop immunity.
• Enteropathogenic E. coli o induce a profuse watery, sometimes bloody, diarrhea. o They are a leading cause of infantile diarrhea. o Outbreaks have been linked to the consumption of contaminated drinking water as well as some meat products. (EPEC)
• Enteroinvasive E. coli (EIEC) � o closely resemble Shigella in their pathogenic mechanisms and the kind of clinical illness they produce. o EIEC penetrate and multiply within epithelial cells of the colon causing widespread cell destruction.
�The clinical syndrome is identical to Shigella dysentery and includes a dysentery-like diarrhea with fever.
�Enterohemorrhagic E. coli (EHEC) o are recognized as the primary cause of hemorrhagic colitis (HC) or bloody diarrhea, which can progress to the potentially fatal hemolytic uremic syndrome (HUS).
�EHEC infections are mostly food or water borne and have implicated undercooked ground beef, raw milk, cold sandwiches, water, unpasteurized apple juice and vegetables
• Enteroaggregative E. coli (EAEC) o The distinguishing feature of EAEC strains is their ability to attach to tissue culture cells in an aggregative manner. � o These strains are associated with persistent diarrhea in young children.
They resemble ETEC strains in that the bacteria adhere to the intestinal mucosa and cause non-bloody diarrhea without invading or causing inflammation. o They also produce a hemolysin related to the hemolysin produced by E. coli strains involved in urinary tract infections. o
Laboratory diagnosis q. The main method is bacteriological method. In stool samples microscopy will show Gram negative rods, with no particular cell arrangement. Then, either Mac. Conkey agar or Endo agar are inoculated with the stool.
�On both agars, deep red colonies are produced as the organism is lactose positive, and fermentation of this sugar will cause the medium's p. H to drop, leading to darkening of the medium. Growth on Levine EMB agar produces black colonies with greenish-black metallic sheen.
�This is diagnostic for E. coli. Biochemical identification: E. coli is also lysine positive, and grows on TSI slant; as it's indol positive (red ring) and methyl red positive (bright red), but VP negative (no changecolorless) and citrate negative (no change-green color).
Treatment q. Gram-negative organisms, qresistant to many antibiotics that are effective against Gram-positive organisms q. Antibiotics which may be used include amoxicillin as well as other semi-synthetic penicillins, cephalosporins, carbapenems, aztreonam, trimethoprim-sulfamethoxazole, ciprofloxacin, nitrofurantoin and the aminoglycosides
q. E. coli often carry multidrug resistant plasmids and under stress readily transfer those plasmids to other species.
Clostridium bacteria Scientific classification Domain: Bacteria Phylum: Firmicutes Class: Clostridia Order: Clostridiales Family: Clostridiaceae Genus: Clostridium
Clostridium bacteria �a genus of Gram-positive bacteria, belonging to the Firmicutes, obligate anaerobes capable of producing endospores.
Preventing Clostridium Bacteria �Observing basic hygiene. � Hand washing � Scrubbing foods and observing safe canning practices. �Follow medical recommendations carefully when receiving treatment � Patient is supported as he or she recovers.
� Clostridium consists of around 100 species that include common freeliving bacteria as well as important pathogens. There are four main species responsible for disease in humans:
1. )Clostridium botulinum Scientific classification Domain: Bacteria Division: Firmicutes Class: Clostridia Order: Clostridiales Family: Clostridiaceae Genus: Clostridium Species: C. botulinum
� A gram-positive, spore-forming, obligate, motile, anaerobic rod shaped bacterium. CAUSES: � botulism, a severe type of food poisoning caused by neurotoxin.
SOURCES: �Forest soils �Bottom sediments of streams, lakes, and coastal waters �Intestinal tracts of fish and mammals �Gills and viscera of crabs and other shellfish.
Symptoms & duration of illness �weakness and vertigo �double vision �difficulty in speaking �swallowing and breathing �muscle weakness/flaccid paralysis �abdominal distention �constipation
� There are three different forms of botulism: (with their treatments) 1. Foodborne botulism - ingestion of preformed neurotoxins Treatment, administering antitoxin. 2. Infant botulism - affects infants and rarely, adults with altered gastrointestinal anatomy or microflora. Treatment, by inducing vomiting and enemas. 3. Wound botulism - occurs when an open wound is contaminated with botulinum spores. Treatment, administration of antitoxins
2. Clostridium difficile Scientific classification Domain: Bacteria Phylum: Firmicutes Class: Clostridia Order: Clostridiales Family: Clostridiaceae Genus: Clostridium
�A Gram-positive bacteria of the genus Clostridium. Clostridia are anaerobic, spore-forming rods (bacillus). CAUSES: �Antibiotic-associated diarrhea (AAD) �Pseudomembranous colitis, a severe infection of the colon
SOURCES: �Feces. �Items or surfaces that are contaminated with feces �Healthcare workers through hand contact.
Symptoms and signs �watery diarrhea �fever �loss of appetite �nausea �abdominal pain/tendernes
Preventing Clostridium difficile �wash hands with soap and water, especially after using the restroom and before eating; �clean surfaces in bathrooms, kitchens and other areas on a regular basis with household detergent/disinfectants.
3. )Clostridium perfringens Scientific classification Kingdom: Bacteria Division: Firmicutes Class: Clostridia Order: Clostridiales Family: Clostridiaceae Genus: Clostridium Species: perfringens
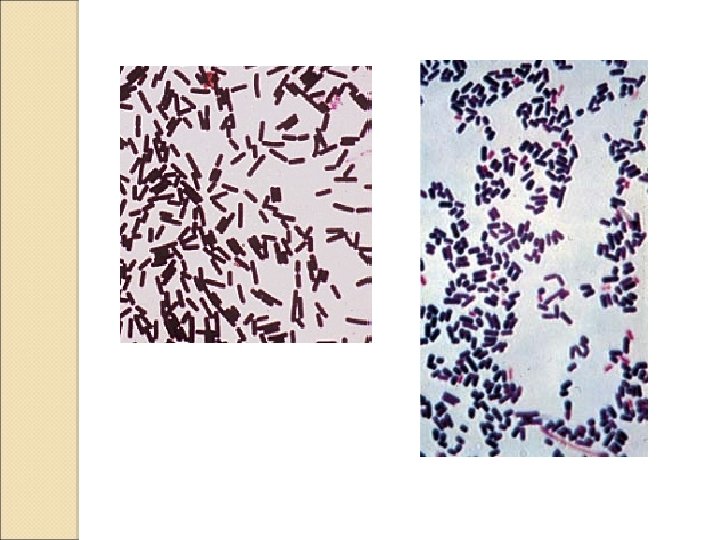
�a Gram-positive, rod-shaped, anaerobic, spore-forming bacterium of the genus Clostridium. SOURCES: �Decaying vegetation �Marine sediment �The intestinal tract of humans �Other vertebrates, insects, and soil
CAUSES: �severe gastroenteritis that can damage the small intestine SOURCE: �Contaminated meat
Symptoms and signs �Intense abdominal cramps and diarrhoea. �Dehydration can occur with this type of food borne illness. Diagnosis and Treatment �A doctor usually suspects the diagnosis when a local outbreak of the disease has occurred. �The testing of contaminated food or the stool. �Leftover cooked meat should be refrigerated promptly and reheated �The person is given fluids and is encouraged to rest. � Antibiotics are not given.
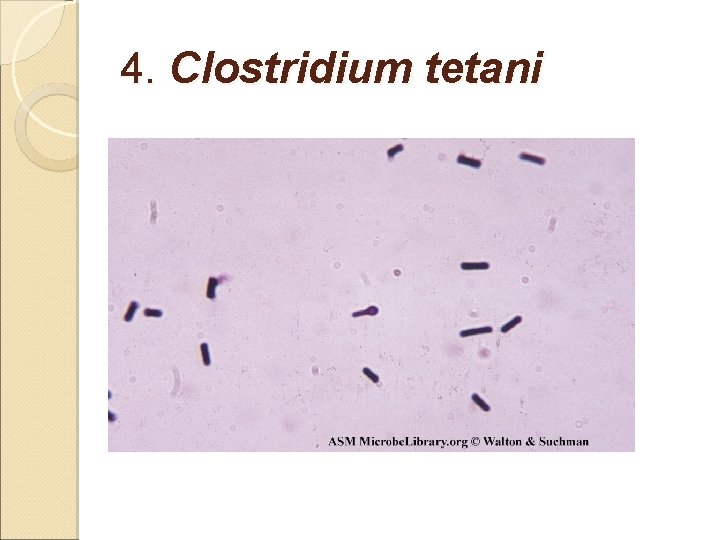
4. Clostridium tetani
CAUSES: �Tetanus or lockjaw, acute infectious disease of the central nervous system. SOURCES: �Soil �Human and animal feces �Digestive tracts of animals and humans.
�Anaerobic bacteria �Anyone who cuts himself with a dirty object is at risk. �As the bacteria grow and multiply, they produce a nerve toxin.
Symptoms and Complications of Tetanus �chills �difficulty swallowing �headache �irritability �jaw and neck stiffness �low fever �restlessness �sore throat �stiff arms and legs �Generally spastic paralysis
Haemophilus influenzae
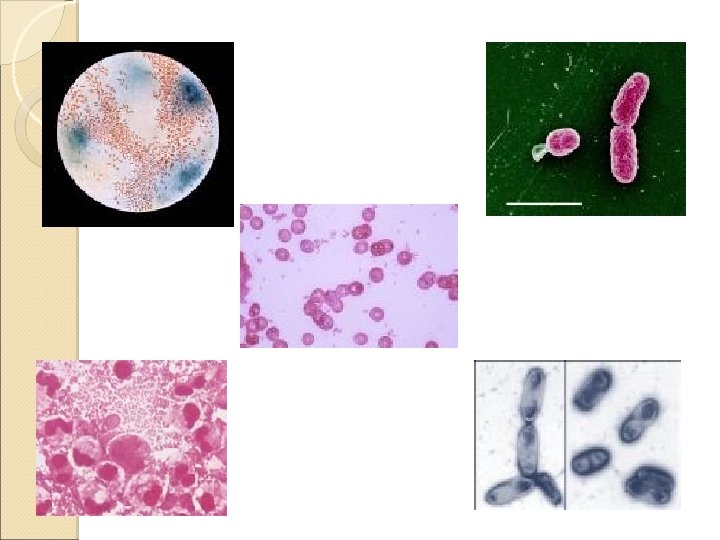
DESCRIPTION Haemophilus influenzae � - is a non-motile Gram • negative rod shaped bacterium. - A member of the Pasteurellaceae family. �
�most commonly causes ear, eye, or sinus infections, and pneumonia in infants and children.
• First described in 1892 by Richard Pfeiffer. • Formerly called Pfeiffer’s bacillus or Bacillus influenzae. �
�In 1995, it was the first freeliving organism to have its entire genome sequenced.
• H. influenzae are mostly opportunistic pathogens. �they usually live in their host without causing disease
�Causes bacteremia, pneumonia, and acute bacterial meningitis. • It is present in the nasopharynx. • It is rarely encountered in the oral cavity.
• Usually transmitted by close contact. • Droplets in the air from sneeze may also cause infections.
• H. influenzae appear as convex, smooth, pale, gray, or transparent colonies. • Show Gram-negative Bacilli, with no specific arrangement.
TREATMENT • H. influenzae produces beta lactamases. • In severe cases, cefotaxime and ceftriaxone are delivered directly into the bloodstream • For the less severe cases, ampicillin and sulbactam, cephalosporins, or flouroquinolones.
PREVENTION Immunization � - is routinely administered in a threeor four-part series. • A Booster ◦ - is given between 12 and 15 months of age. •
• Other populations that should be encouraged to receive the vaccine include the following: � - individuals without a spleen �
�adults and children with weakened immune disease � - individuals who are HIV positive �
Neisseria meningitidis
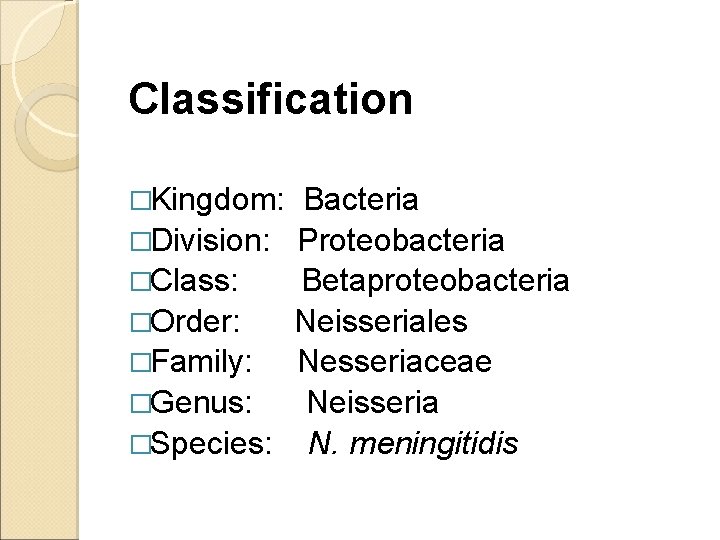
Classification �Kingdom: Bacteria �Division: Proteobacteria �Class: Betaproteobacteria �Order: Neisseriales �Family: Nesseriaceae �Genus: Neisseria �Species: N. meningitidis
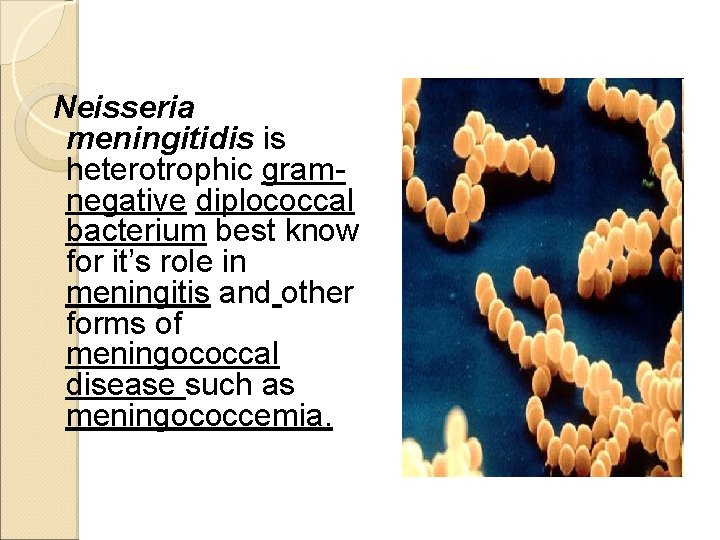
Neisseria meningitidis is heterotrophic gramnegative diplococcal bacterium best know for it’s role in meningitis and other forms of meningococcal disease such as meningococcemia.
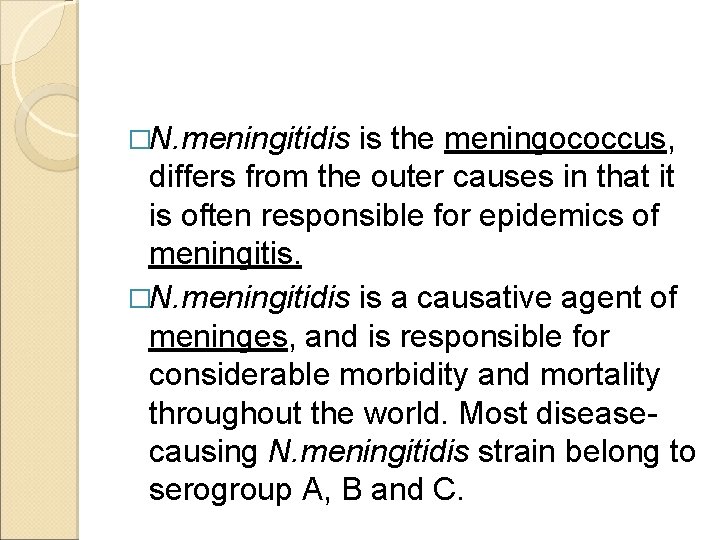
�N. meningitidis is the meningococcus, differs from the outer causes in that it is often responsible for epidemics of meningitis. �N. meningitidis is a causative agent of meninges, and is responsible for considerable morbidity and mortality throughout the world. Most diseasecausing N. meningitidis strain belong to serogroup A, B and C.
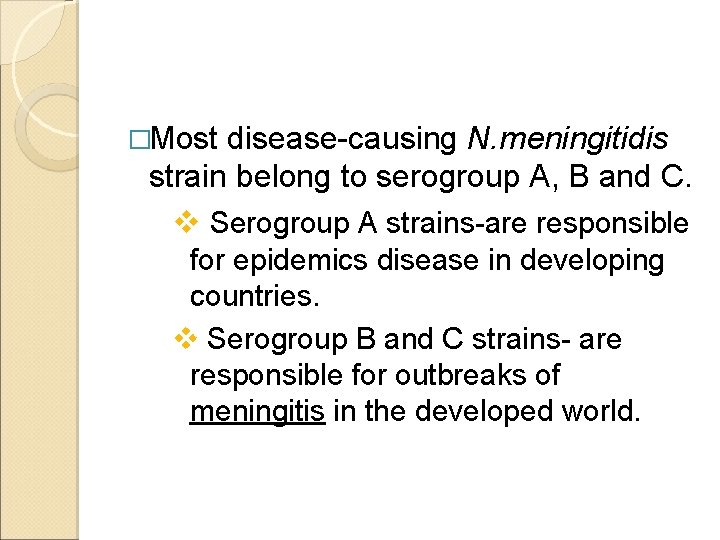
�Most disease-causing N. meningitidis strain belong to serogroup A, B and C. v Serogroup A strains-are responsible for epidemics disease in developing countries. v Serogroup B and C strains- are responsible for outbreaks of meningitis in the developed world.
�This disease that has appeared to date back to the 16 th century. However, the disease was only first described in 1805 by swiss physician Gaspard Vieusseaux. �Following Vieusseaux, Italian pathologist Ettore Marchiafava and Angelo Celli also decribed the micrococci in a sample of cerebral spinal fluid (CSF).
�In 1887, the bacteria was isolated by Anton Weichselbaum. �In 1909, immunologically distinct serotypes of the meningococcus were identified. This established the basis for serum therapy, which was instituted by Flexner in 1913.
�N. meningitidis exist as normal flora in the nasopharynx of up to 40% of adults. It causes the only form of bacterial meningitis known to cause epidemics. �N. meningitidis will attach to the microvilli of nonciliated columnar epithelial cell that reside in the nasal region of humans.
�The bacteria are then able to invade to mucous membrane that lines the nasopharynx. � N. meningitidis then has access to the bloodstream of the individual and from there usually more into the meninges of the brain.
�The CSF tested in the laboratory by trying to grow more of the bacteria on a special agar plate. This type of agar plate is called a chocolate agar because of its color. � It is composed of approximately 510% mammalian blood.
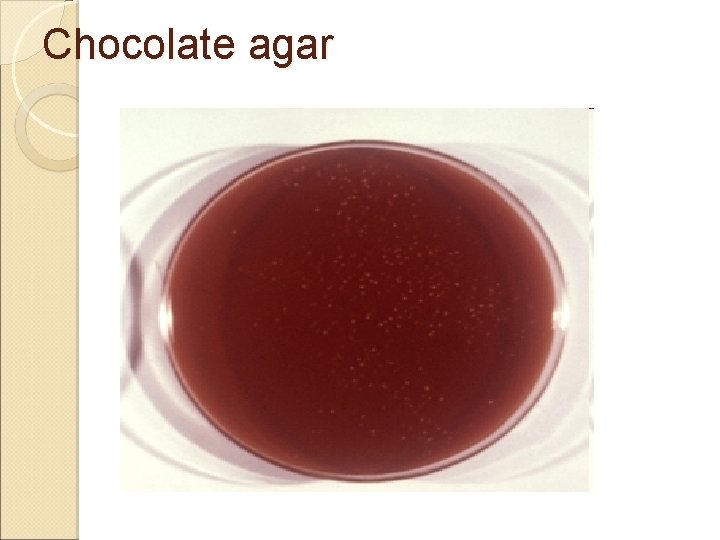
Chocolate agar
Virulence factors of N. menigitidis contribute to some clinical manifestation during infections. �Lipopolysaccharide (LPS)-is a component of the cell wall of N. meningitidis which as an endotoxin. �Exotoxins-are actively secreted by some bacteria and have a wide range of affects including inhibitions of certain biochemical pathway in the hosts.
�Immunoglobulin (lg) proteases-are antibodies expressed and secreted by hosts in response to an infection. �Polysaccharide capsule-prevents hosts phagocytosis and aids in evasion of the host immune response. �Fimbriae-which mediate attachment of the bacterium to the epithelial cells of the nasopharynx.
N. meningitidis can be the cause of three major diseases. These three are nasopharyngitis, menigicoccal septicemia and meningicoccal meningitis. �Nasopharyngitis-is usually a very short illness and sometimes there aren’t even an symtoms.

Meningococcal septicemia-typically causes a purpuric rash that does not lose it’s color when pressed with a glass and does cause the classical symptoms of meninditis.
�Meningococcal meningitis-or more commonly known as bacterial menigitis. It is also known as epidemic meningitis. Symptoms of Meningococcal meningitis �The disease usually comes an quickly with severe headaches, high fever, pain and stiffness of the neck, back and shoulders and nausea follows after all of these initial symptoms.
Clinical Manifestations �In a prospective observational cohort study, classic meningitis triad of fever, neck stiffness and altered mental status was present in 70 of the 258 patients (27 percents) with meningococcal meningitis. �When rash was added, 89 percent of the patient had at least two of these four sign. The classic triad is much more common in preumoumococcal meningitidis (58 percent in the same cohort study.
�This especially include young children and their child caregivers or nurseryschool contact, as well as anyone who had direct exposure to the patient through kissing, sharing utensils, or medical intervention such as mouth- to -mouth resuscitation.
�The information available has shown that the humoral immunity does indeed play a key role in protection against N. meningitidis infection that carriage of the bacterium results in an increased bactericidal anitbody response.
Treatment �All recent contacts of the infected patients over the 7 days before onset should receive medication (rifampin, ceftriaxone, or ciprofloxacin) to prevent them from contracting the infection. �Anyone who frequently ate, slept or stayed at the patients home during the 7 days before the onset of symptom, or those who sat beside the patient or an airplane flight of 8 hours or longer, should also receive chemoprophylaxis
Prevention Meningococcal Vaccine There are two vaccines to prevent meningococcal disease. �Menactre-is licensed for use in people aged 11 to 55. �Menomune-is used for people outside of this age group and for travellers.
- Slides: 86