EQUIPMENTS FOR EXTRACORPOREAL MEMBRANE OXYGENATION AN INTRODUCTION TO
EQUIPMENTS FOR EXTRACORPOREAL MEMBRANE OXYGENATION – AN INTRODUCTION TO PERFUSION TECHNOLOGY Dr. Chan King-chung Pamela Youde Nethersole Eastern Hospital
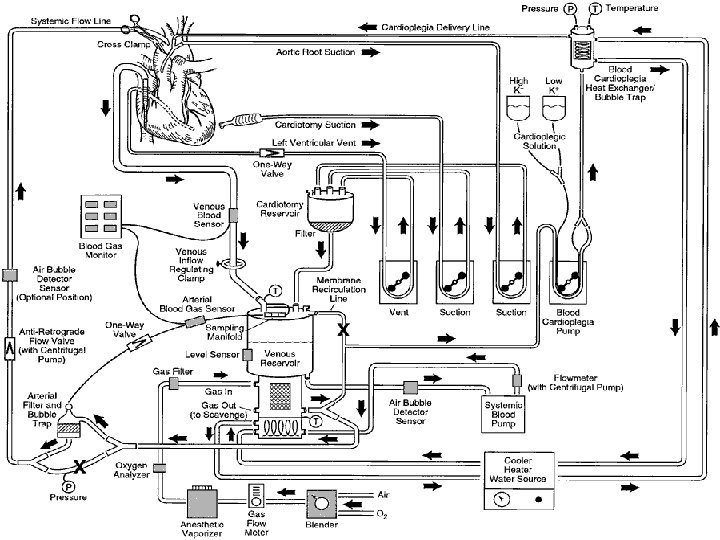
What is Perfusion Technology? Perfusion Technology is the study of physiology, pathology and associated equipment used to support and/or assume the function of the heart and/or lungs during medical procedures. The perfusionist measures various blood and other parameters to identify appropriate mechanical, pharmacological and thermal manipulation to maintain tissue viability, as directed by physicians. Operation of cardiopulmonary bypass machine
Brief History of Perfusion 1813 – Le Gallois First proposed extracorporeal circulation to preserve viability of tissue 1858 – Brown-Sequard Draw his own venous blood Beating venous blood vigorously For oxygenation & defibrination Perfusing an animal limb with syringe able to restore local reflexes 1882 – Waldemar von Schroder Bubbling of blood for oxygenation Problem with foaming / gas embolism
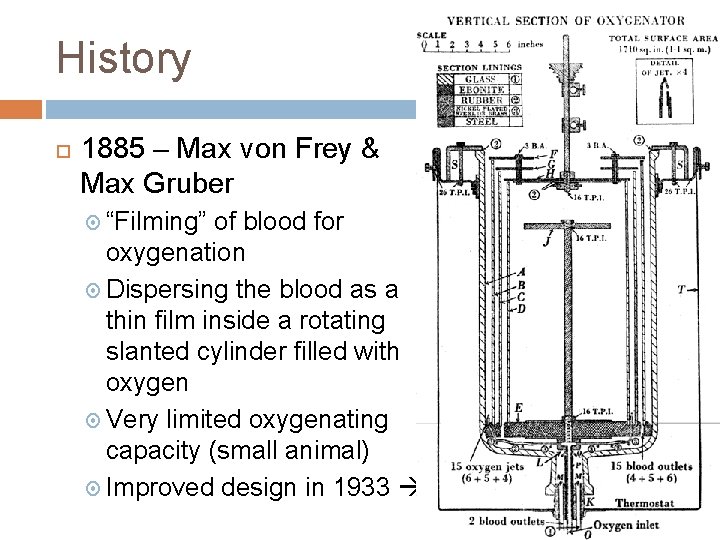
History 1885 – Max von Frey & Max Gruber “Filming” of blood for oxygenation Dispersing the blood as a thin film inside a rotating slanted cylinder filled with oxygen Very limited oxygenating capacity (small animal) Improved design in 1933
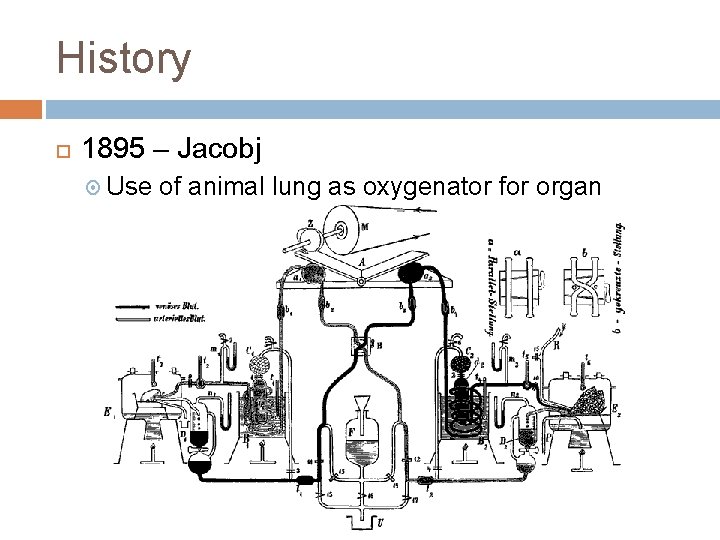
History 1895 – Jacobj Use of animal lung as oxygenator for organ perfusion
History 1916 – Mc. Lean Discovery for heparin for anticoagulation (1870 – Miescher discovered protamine) 1929 – Brukhonenko & Tchetchuline Perfusion of guillotined head of a dog by cross- perfusion
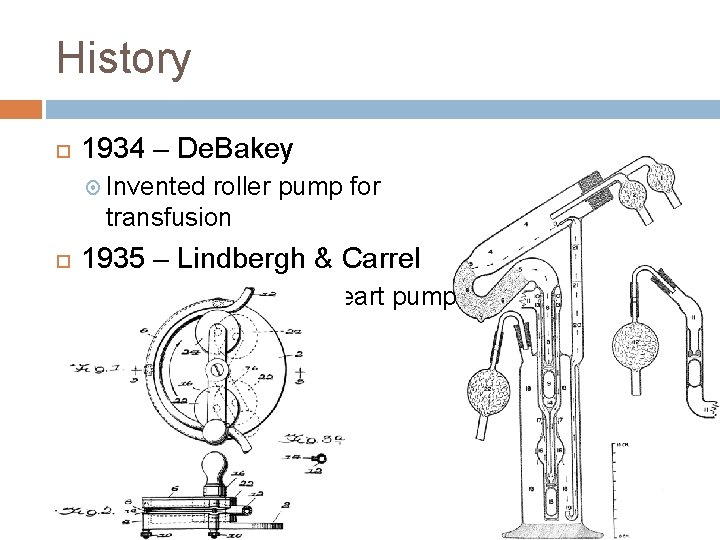
History 1934 – De. Bakey Invented roller pump for transfusion 1935 – Lindbergh & Carrel Sterile mechanical heart pump
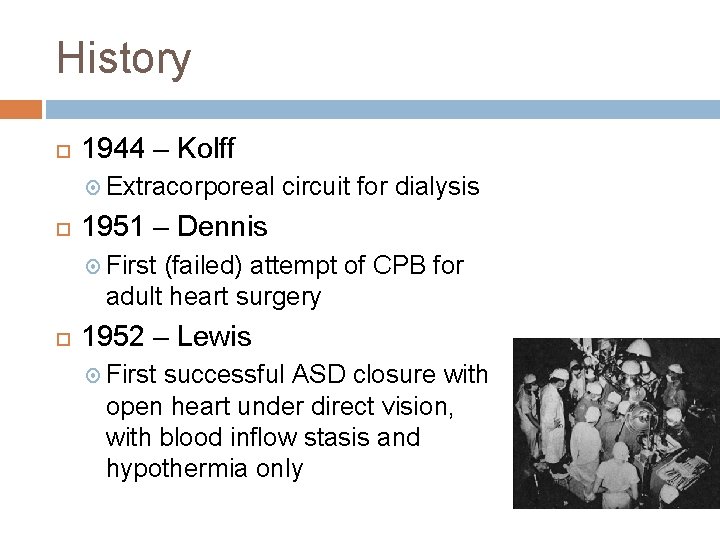
History 1944 – Kolff Extracorporeal circuit for dialysis 1951 – Dennis First (failed) attempt of CPB for adult heart surgery 1952 – Lewis First successful ASD closure with open heart under direct vision, with blood inflow stasis and hypothermia only
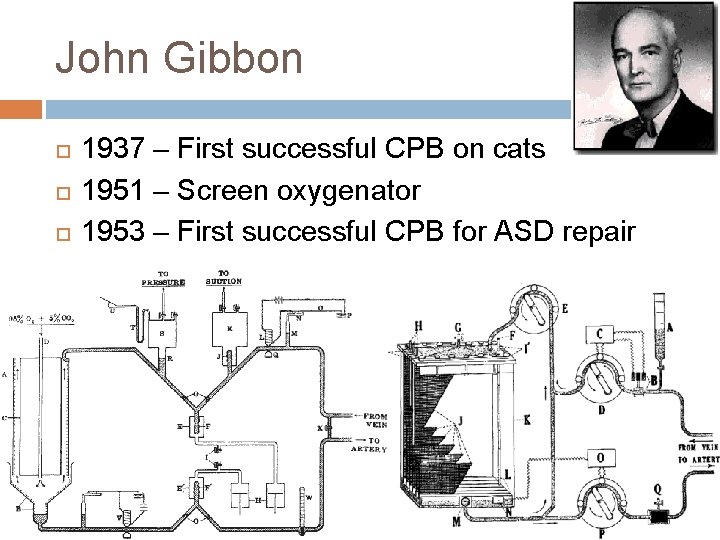
John Gibbon 1937 – First successful CPB on cats 1951 – Screen oxygenator 1953 – First successful CPB for ASD repair
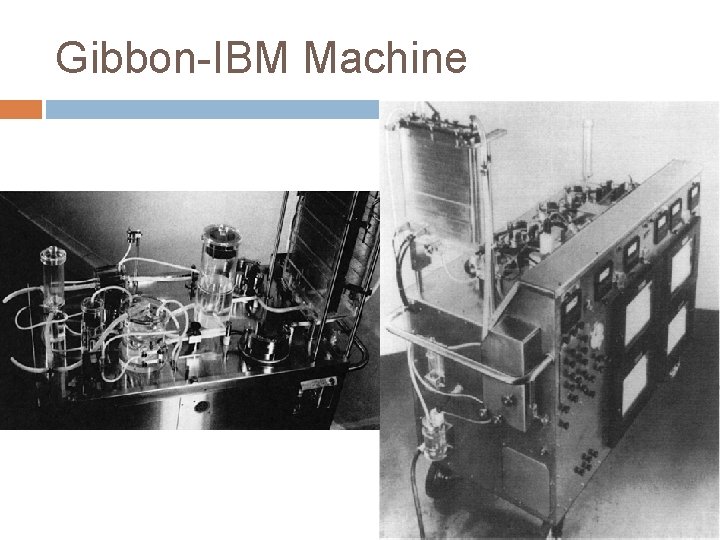
Gibbon-IBM Machine
History 1955 – Lillehei Repaired intracardiac defects in 32 infants & young children, using a donor adult to provide oxygenation (with cross circulation) 1955 – Mustard Animal lungs used as oxygenator during human cardiac surgery
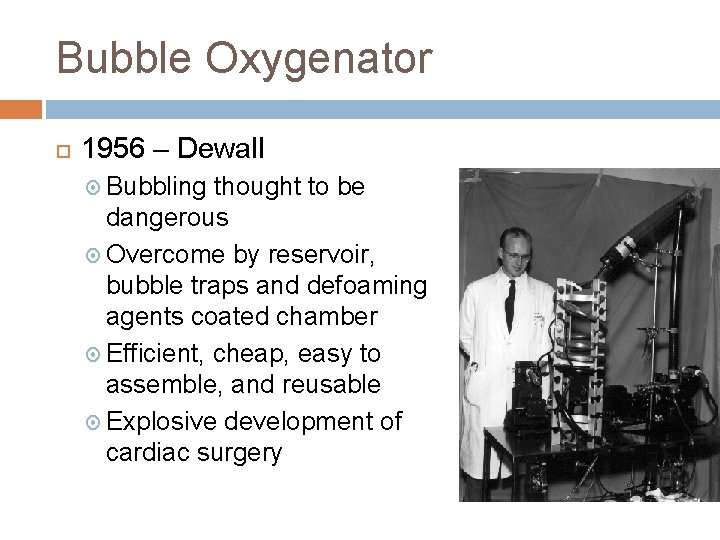
Bubble Oxygenator 1956 – Dewall Bubbling thought to be dangerous Overcome by reservoir, bubble traps and defoaming agents coated chamber Efficient, cheap, easy to assemble, and reusable Explosive development of cardiac surgery
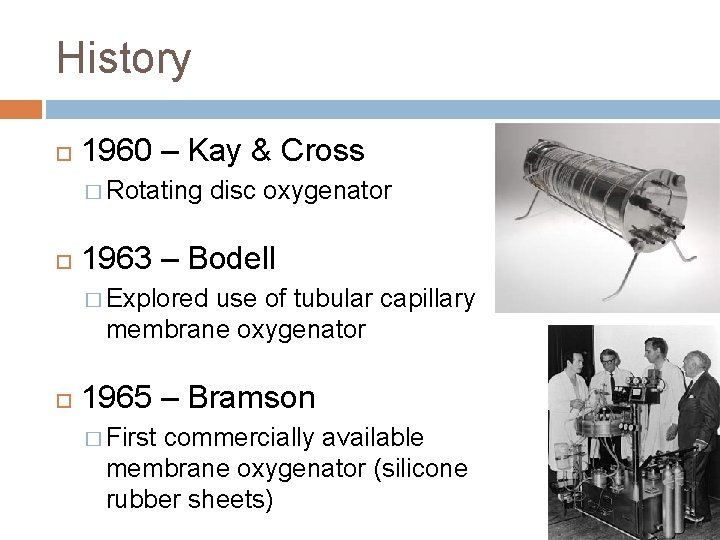
History 1960 – Kay & Cross � Rotating disc oxygenator 1963 – Bodell � Explored use of tubular capillary membrane oxygenator 1965 – Bramson � First commercially available membrane oxygenator (silicone rubber sheets)
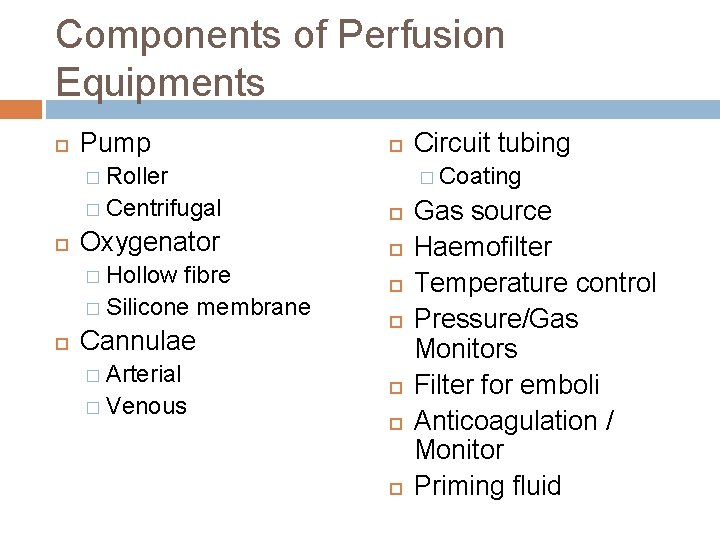
Components of Perfusion Equipments Pump � Roller � Coating � Centrifugal Oxygenator � Hollow fibre � Silicone membrane Cannulae � Arterial � Venous Circuit tubing Gas source Haemofilter Temperature control Pressure/Gas Monitors Filter for emboli Anticoagulation / Monitor Priming fluid
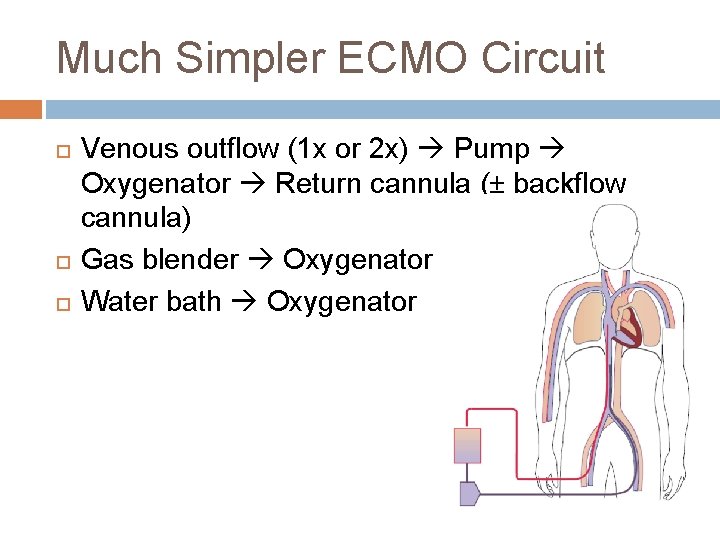
Much Simpler ECMO Circuit Venous outflow (1 x or 2 x) Pump Oxygenator Return cannula (± backflow cannula) Gas blender Oxygenator Water bath Oxygenator
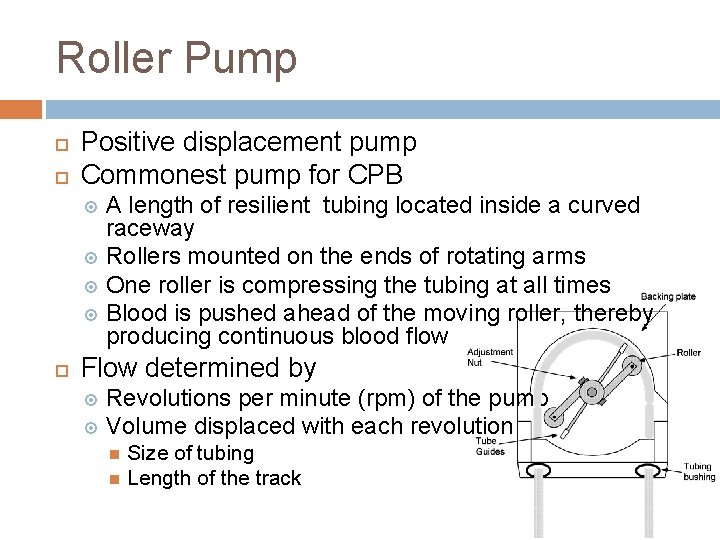
Roller Pump Positive displacement pump Commonest pump for CPB A length of resilient tubing located inside a curved raceway Rollers mounted on the ends of rotating arms One roller is compressing the tubing at all times Blood is pushed ahead of the moving roller, thereby producing continuous blood flow Flow determined by Revolutions per minute (rpm) of the pump Volume displaced with each revolution Size of tubing Length of the track
Types of Roller Pump Single-roller pump Used for CPB in the 1950 s and early 1960 s Produce more pulsatility Double-roller pump Most commonly used pump 210 -degree semicircular backing plate 2 rollers with the rotating arms set 180 degrees apart one of the two rollers is always compressing the tubing a relatively nonpulsatile flow Multiple-roller pump Not clinically available because it causes more haemolysis
Tubing of Roller Pump Polyvinyl chloride (PVC) Most widely used Durable Some spallation (release of plastic microparticles) Latex rubber More haemolysis than PVC Silicone rubber Less haemolysis than PVC More spallation then PVC
Occlusiveness Adjustable in CPB machine Excessive occlusion Inadequate Haemolysis and tubing wear Compromises forward flow Target “barely nonocclusive” Holding the outflow line with fluid level 60 to 75 cm above the pump Adjust occlusiveness until the fluid level falls at a rate between 1 and 12 cm/min Cause less haemolysis than centrifugal pump in some study
Complication Malocclusion (over- or under-occlusion) Miscalibration Fracture of the tubing Loss of power Spallation Capacity to pump grossly visible air Tubing or connectors break with outflow obstruction Microscopic air bubbles ("cavitation") with inflow obstruction Pinhole leaks from fracture in tubing, leading to microscopic air embolism
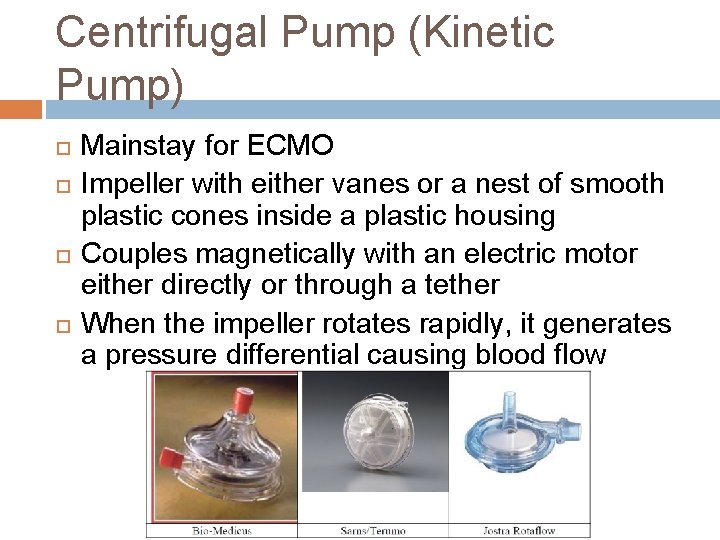
Centrifugal Pump (Kinetic Pump) Mainstay for ECMO Impeller with either vanes or a nest of smooth plastic cones inside a plastic housing Couples magnetically with an electric motor either directly or through a tether When the impeller rotates rapidly, it generates a pressure differential causing blood flow
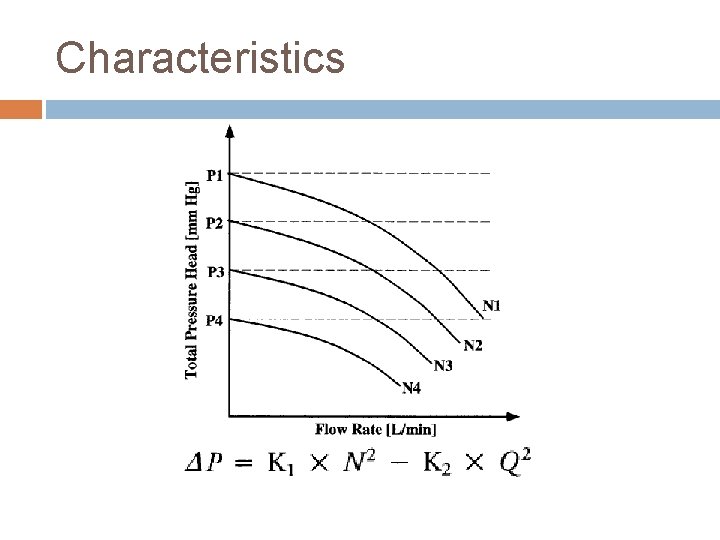
Characteristics

Roller vs. Centrifugal Pump Roller Pump Advantages Reusable pump with inexpensive disposable parts Ease of sterilization Simple flow rate determination Variable SV for different-sized patients Disadvantage Blood trauma s Possibility of circuit disruption and termination from excessive line pressure Particulate microemboli from tubing spallation Possibility of massive air emboli Occlusion variability affecting flow rate and blood trauma Centrifugal Pump No possibility of disruption from excessive line pressure buildup Decreased blood trauma Less risk of massive air emboli Less cavitation More expensive non-reusable pump Retrograde flow when pump slows or stops Flowmeter is necessary (poor performance at low flow)
Complications Generally safe Allows retrograde flow Exsanguinate a patient by siphon into reservoir Draw air into the arterial line at the cannulation site
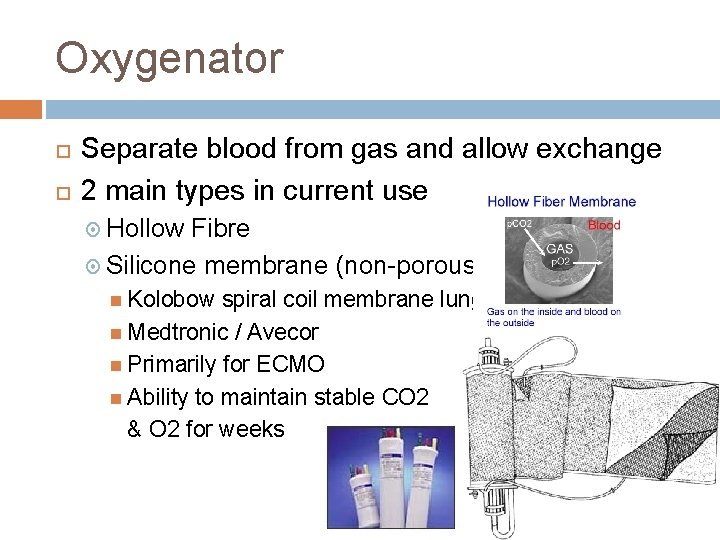
Oxygenator Separate blood from gas and allow exchange 2 main types in current use Hollow Fibre Silicone membrane (non-porous) Kolobow spiral coil membrane lung Medtronic / Avecor Primarily for ECMO Ability to maintain stable CO 2 & O 2 for weeks
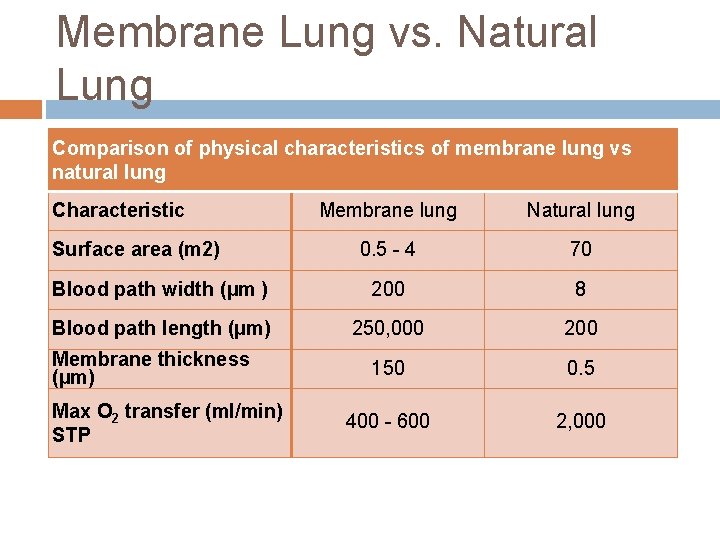
Membrane Lung vs. Natural Lung Comparison of physical characteristics of membrane lung vs natural lung Characteristic Membrane lung Natural lung 0. 5 - 4 70 Blood path width (µm ) 200 8 Blood path length (µm) 250, 000 200 150 0. 5 400 - 600 2, 000 Surface area (m 2) Membrane thickness (µm) Max O 2 transfer (ml/min) STP
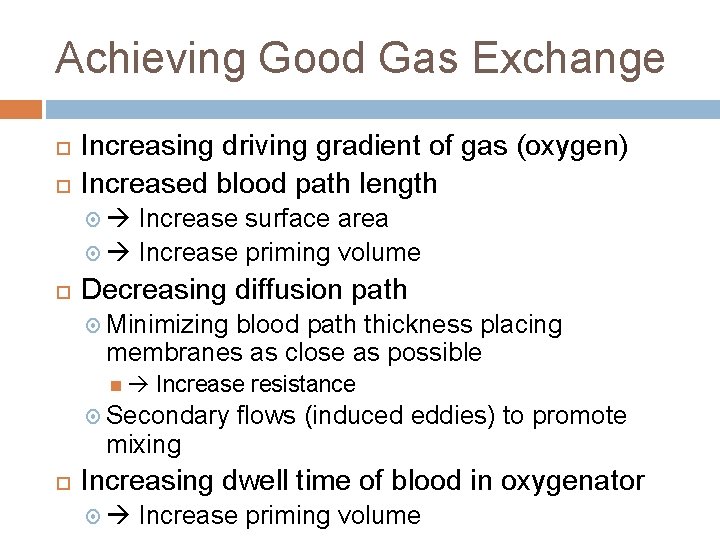
Achieving Good Gas Exchange Increasing driving gradient of gas (oxygen) Increased blood path length Increase surface area Increase priming volume Decreasing diffusion path Minimizing blood path thickness placing membranes as close as possible Increase resistance Secondary flows (induced eddies) to promote mixing Increasing dwell time of blood in oxygenator Increase priming volume
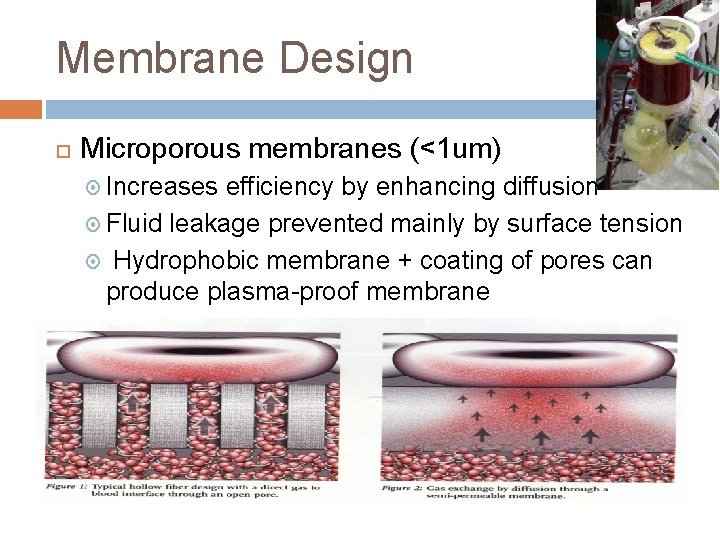
Membrane Design Microporous membranes (<1 um) Increases efficiency by enhancing diffusion Fluid leakage prevented mainly by surface tension Hydrophobic membrane + coating of pores can produce plasma-proof membrane
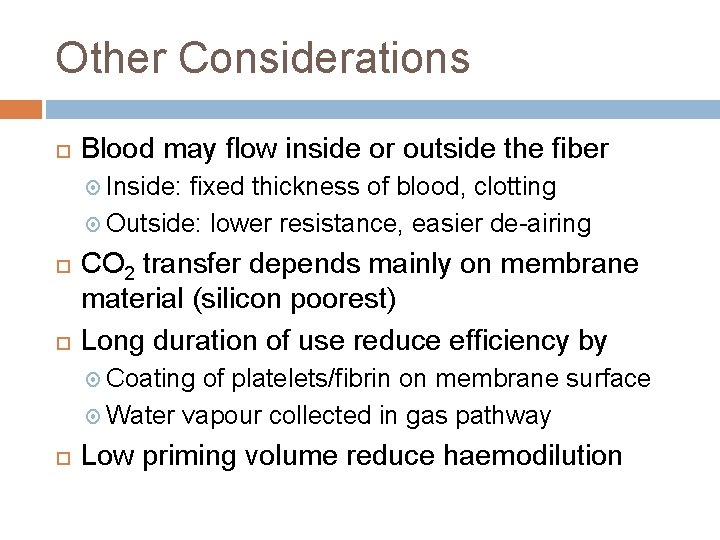
Other Considerations Blood may flow inside or outside the fiber Inside: fixed thickness of blood, clotting Outside: lower resistance, easier de-airing CO 2 transfer depends mainly on membrane material (silicon poorest) Long duration of use reduce efficiency by Coating of platelets/fibrin on membrane surface Water vapour collected in gas pathway Low priming volume reduce haemodilution
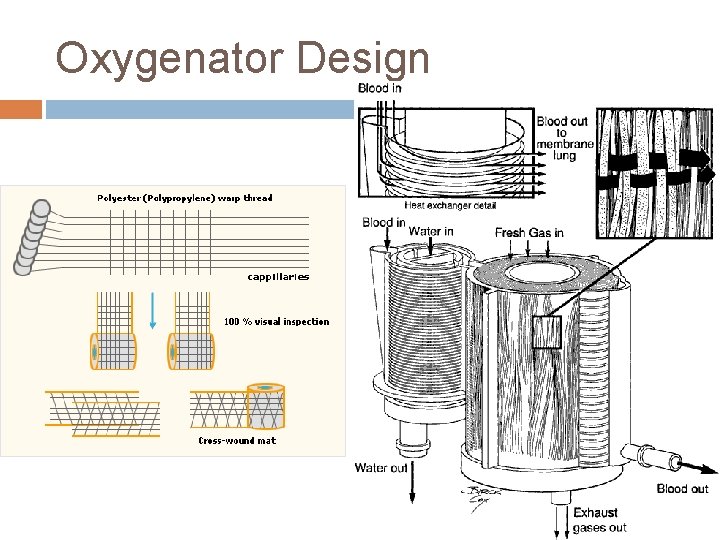
Oxygenator Design
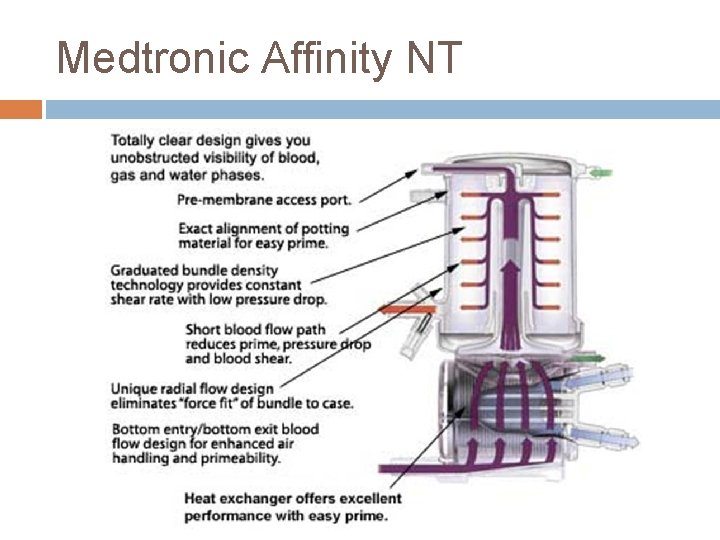
Medtronic Affinity NT
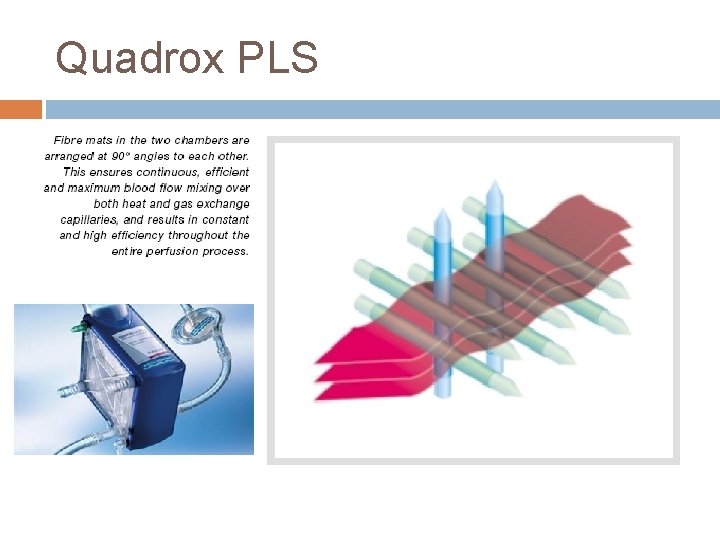
Quadrox PLS
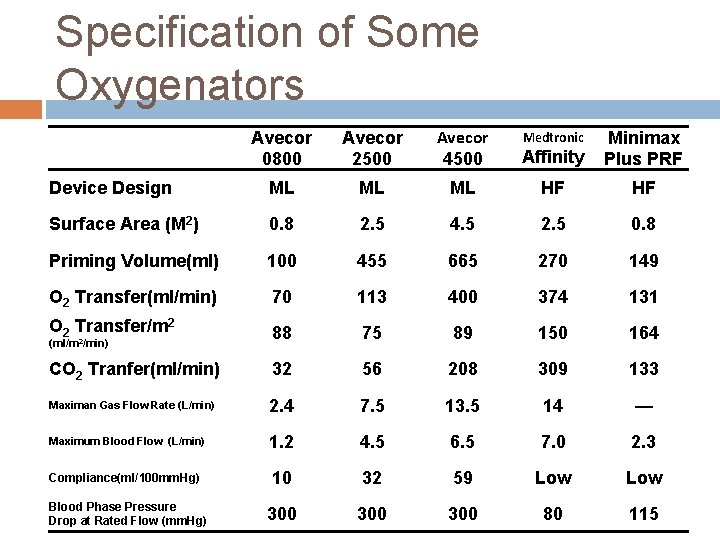
Specification of Some Oxygenators Avecor 0800 Avecor 2500 Avecor 4500 Affinity Minimax Plus PRF Device Design ML ML ML HF HF Surface Area (M 2) 0. 8 2. 5 4. 5 2. 5 0. 8 Priming Volume(ml) 100 455 665 270 149 O 2 Transfer(ml/min) 70 113 400 374 131 O 2 Transfer/m 2 88 75 89 150 164 CO 2 Tranfer(ml/min) 32 56 208 309 133 Maximan Gas Flow Rate (L/min) 2. 4 7. 5 13. 5 14 — Maximum Blood Flow (L/min) 1. 2 4. 5 6. 5 7. 0 2. 3 Compliance(ml/100 mm. Hg) 10 32 59 Low 300 300 80 115 (ml/m 2/min) Blood Phase Pressure Drop at Rated Flow (mm. Hg) Medtronic
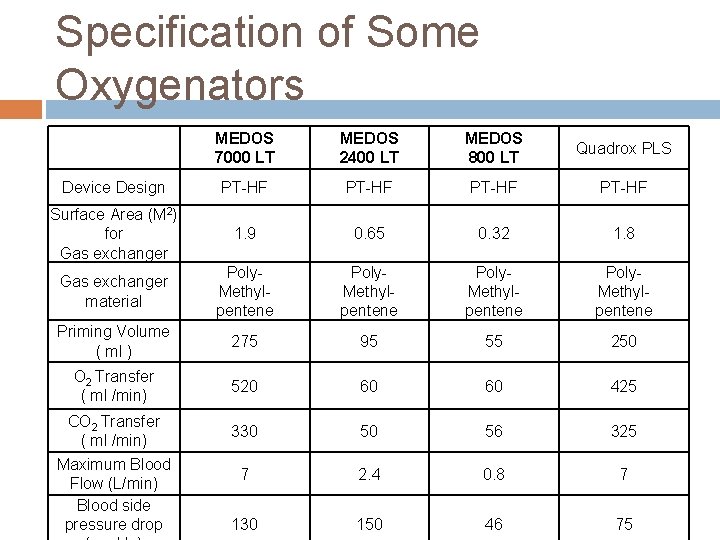
Specification of Some Oxygenators MEDOS 7000 LT MEDOS 2400 LT MEDOS 800 LT Quadrox PLS Device Design PT-HF Surface Area (M 2) for Gas exchanger 1. 9 0. 65 0. 32 1. 8 Gas exchanger material Poly. Methylpentene Priming Volume ( ml ) 275 95 55 250 O 2 Transfer ( ml /min) 520 60 60 425 330 50 56 325 7 2. 4 0. 8 7 130 150 46 75 CO 2 Transfer ( ml /min) Maximum Blood Flow (L/min) Blood side pressure drop
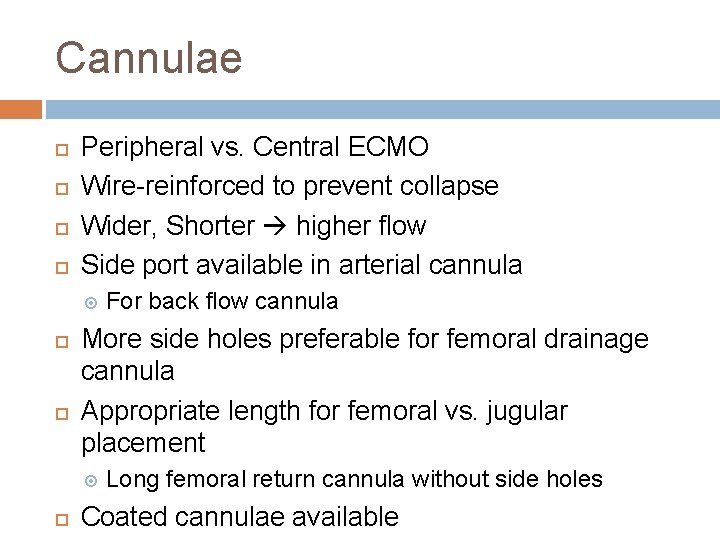
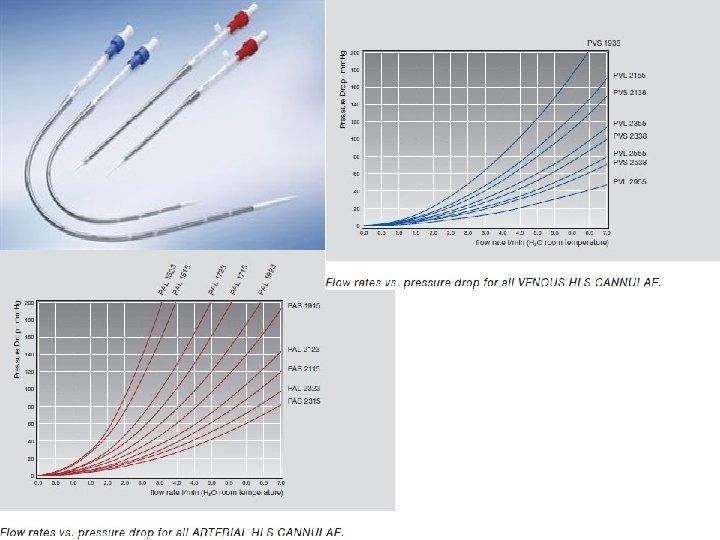
Cannulae Peripheral vs. Central ECMO Wire-reinforced to prevent collapse Wider, Shorter higher flow Side port available in arterial cannula More side holes preferable for femoral drainage cannula Appropriate length for femoral vs. jugular placement For back flow cannula Long femoral return cannula without side holes Coated cannulae available
Tubing Standard tubing of 3/8 inch or ½ inch for adult application 3/8 inch was be used mostly in HK for ECMO Coating available
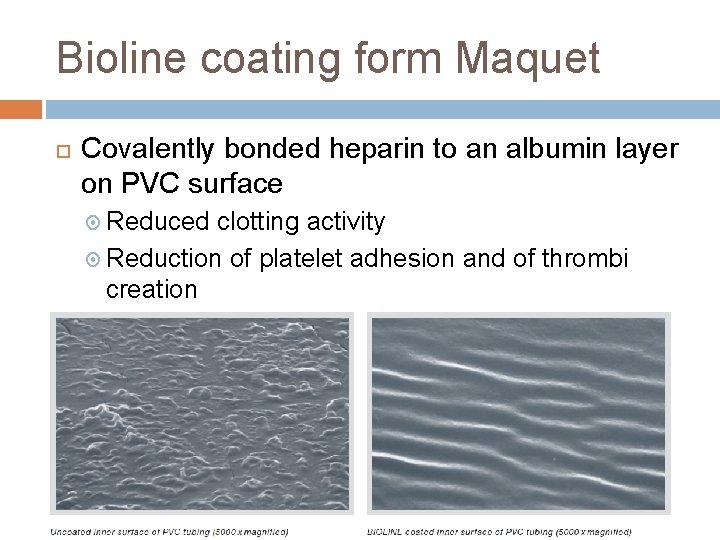
Bioline coating form Maquet Covalently bonded heparin to an albumin layer on PVC surface Reduced clotting activity Reduction of platelet adhesion and of thrombi creation Less complement activation & neutrophil activation
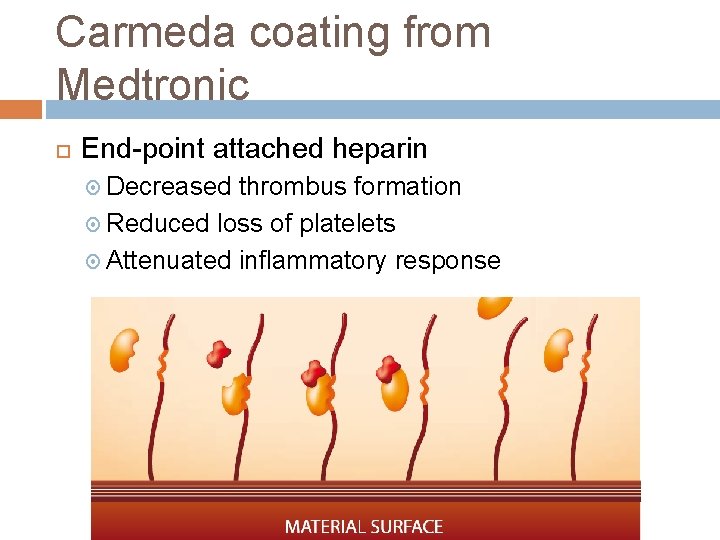
Carmeda coating from Medtronic End-point attached heparin Decreased thrombus formation Reduced loss of platelets Attenuated inflammatory response
Gas Source Usually a simple oxygen blender for ECMO O 2 flowmeter may suffice during transport
Hemofilter Used in operation to remove fluid CRRT machine for ICU patient on ECMO Attachment to post-pump, pre-oxygenator preferable Avoid shunting Avoid risk of air embolism Cannot tolerate a positive A-pressure for Prisma machine (Meaning of A & V are different in CRRT & ECMO circuit)
Temperature Control Thermo-controlled water bath necessary Avoid a high water bath temperature if possible Bubble formation with heating of blood Not more than 4 C compared with blood
Pressure Monitors Venous pressure Detect insucking Arterial pressure Detect obstruction to outflow Pressure drop across oxygenator Detect oxygenator clotting Risk of thrombosis / infection as a segment of stagnant blood is introduced Integrated senor in the Cardiohelp system (cannot recalibrate)
Gas Monitor Fi. O 2 monitor Venous O 2 saturation Provide continuous ABG data Haemoglobin concentration Detects failure of oxygenator Inline p. H/p. CO 2/p. O 2 monitor Detects recirculation Arterial O 2 saturation Detects hypoxic sweep gas Detects change in blood volume Bubble detector Prevent gas embolism
Others Filter / bubble trapper Anticoagulation / Monitor Heparin ? Lower dose than recommendation by manufacture Higher need for anticoagulation when flow is low Monitor with ACT/APTT/Thromboelastography Priming fluid Colloid / Blood prime in children / infants
- Slides: 46