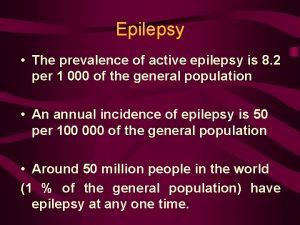
Epilepsy The prevalence of active epilepsy is 8










- Slides: 44

Epilepsy • The prevalence of active epilepsy is 8. 2 per 1 000 of the general population • An annual incidence of epilepsy is 50 per 100 000 of the general population • Around 50 million people in the world (1 % of the general population) have epilepsy at any one time.
Epilepsy is a chronic disorder, or group of chronic disorders, in which the indispensable feature is recurrence of seizures that are typically unprovoked and usually unpredictable.

What causes epilepsy? • Inheritance - genetic low seizure threshold • The injury of the brain (due to a road traffic accident, tumour, stroke or trauma at birth ) • An infection that affects the brain, such as meningitis or encephalitis
How is epilepsy diagnosed? • Unlike most other neurological conditions, there may be no physical sign that a person has epilepsy when they are not having a seizure. • Therefore the diagnosis is based on a history of more than one epileptic seizure. • An eyewitness account may provide useful information in reaching an accurate diagnosis, as the person experiencing the seizure will not usually remember what has happened.
• I. A. General seizures • • initial stage tonic stage clonic stage recovery stage • B. Without seizure attacks (Absentia epileptica) • II. Focal attacks.

Can epilepsy be treated? • With the appropriate drug treatment, seizures can be completely controlled in up to 80% of people • Some people continue to have seizures despite treatment. A small proportion of these people may benefit from neurosurgery (brain surgery).

TREATMENT FOR EPILEPSY § Drug treatment § Surgical treatment § Complementary treatment
• Epilepsy is the most common serious neurological condition. • Anyone can develop epilepsy; it occurs in all ages, races and social classes. • Labelling people as 'epileptics' on the basis of a medical diagnosis of epilepsy ignores the rest of their attributes and characteristics
The Treatment of Epilepsy • The incidence and prevalence • Aetiologies and risk factors • Aims of treatment • Clinical settings • Principles of treatment – Medical treatment – Surgical treatment • Guidelines • Conclusions
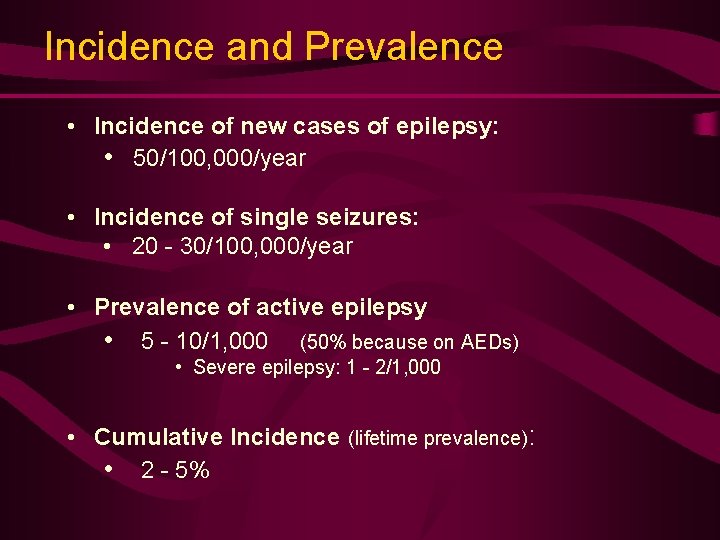
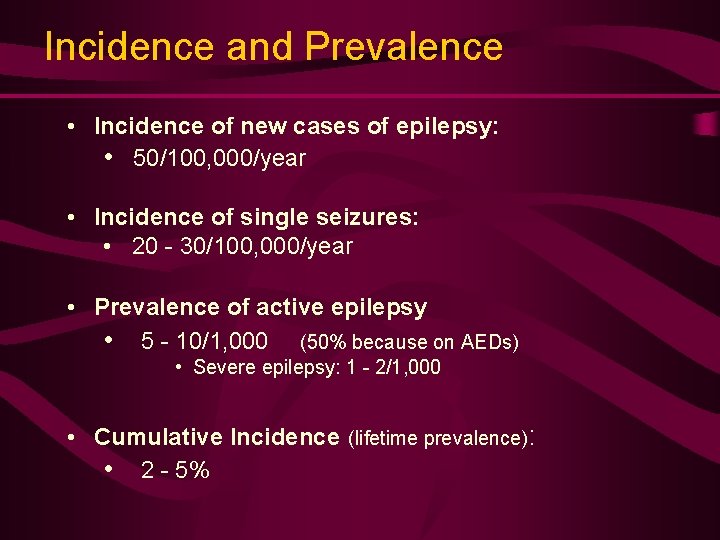
Incidence and Prevalence • Incidence of new cases of epilepsy: • 50/100, 000/year • Incidence of single seizures: • 20 - 30/100, 000/year • Prevalence of active epilepsy • 5 - 10/1, 000 (50% because on AEDs) • Severe epilepsy: 1 - 2/1, 000 • Cumulative Incidence (lifetime prevalence): • 2 - 5%
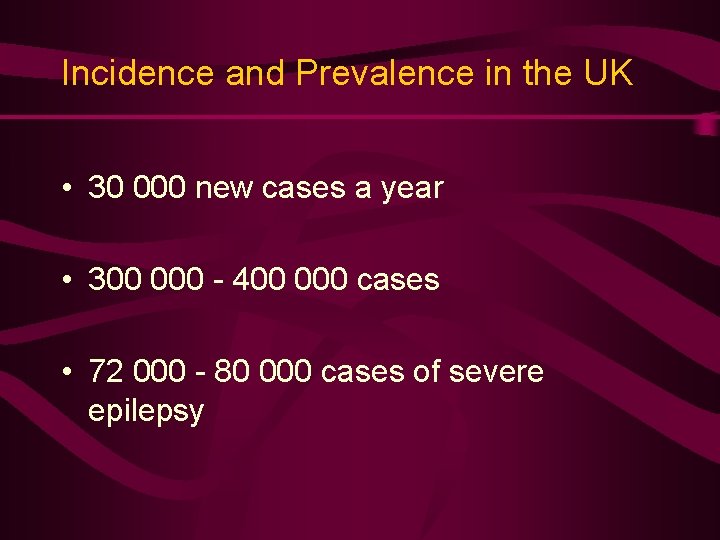
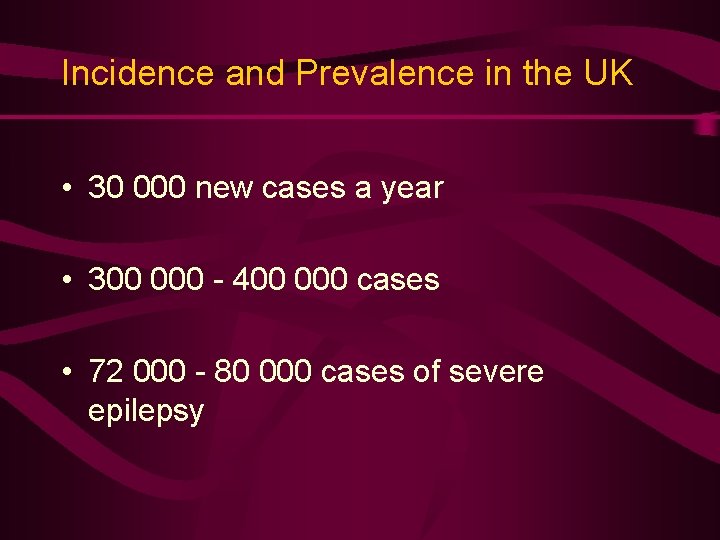
Incidence and Prevalence in the UK • 30 000 new cases a year • 300 000 - 400 000 cases • 72 000 - 80 000 cases of severe epilepsy
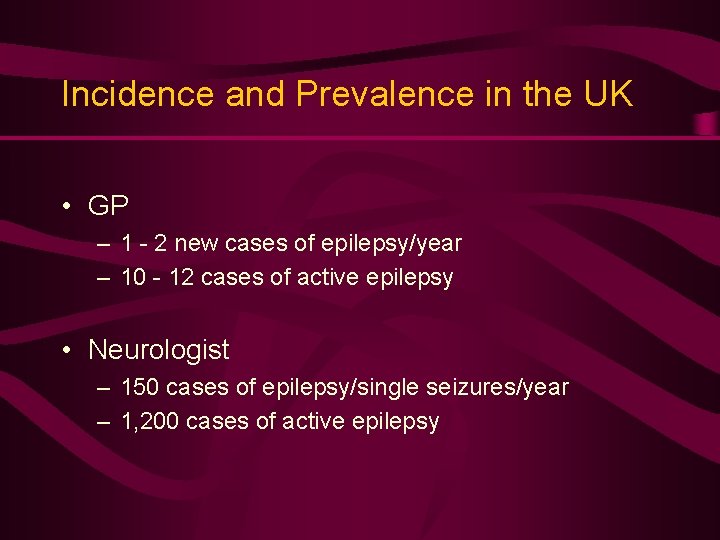
Incidence and Prevalence in the UK • GP – 1 - 2 new cases of epilepsy/year – 10 - 12 cases of active epilepsy • Neurologist – 150 cases of epilepsy/single seizures/year – 1, 200 cases of active epilepsy

Epilepsy: Aetiologies and Risk Factors • Risk factors varies with age and geographic location – Congenital, developmental and genetic conditions in childhood, adolescence and young adults – Head trauma, infection and tumours at any age although tumours more likely over age 40 – Cerebrovascular disease common in elderly – Endemic infections are associated with epilepsy in certain areas – malaria, neurocysticercosis, paragonomiasis, – no adequate large scale study of attributable risk yet

Antiepileptic Treatment • AEDs are mainstay treatment • Non-pharmacological options feasible in only few selected cases – Surgery • Curative • Palliative – Ketogenic diet (children) – Behaviour modification – Avoidance therapy in cases with clear precipitants
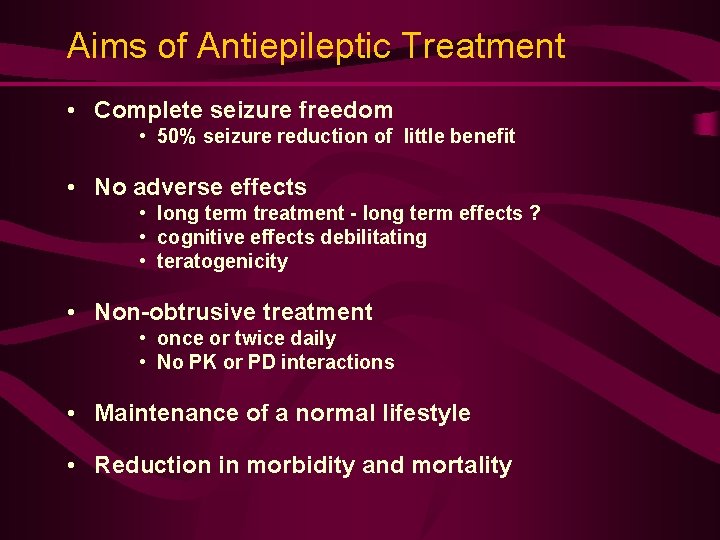
Aims of Antiepileptic Treatment • Complete seizure freedom • 50% seizure reduction of little benefit • No adverse effects • long term treatment - long term effects ? • cognitive effects debilitating • teratogenicity • Non-obtrusive treatment • once or twice daily • No PK or PD interactions • Maintenance of a normal lifestyle • Reduction in morbidity and mortality
AED Treatment: Clinical Settings • Prophylactic Treatment • Newly Diagnosed Epilepsy • Single seizure • Recurrent seizures • Chronic Epilepsy

Prophylactic use of AEDs • Often advocated after • Head injury • Craniotomy h There are considerable compliance problems • There is no evidence of a protective effect of this policy • No place for this! • Better wait for the event to happen
Is it Epilepsy ? • Newly diagnosed or suspected cases at Primary Care level > 50% not epilepsy commonest differential diagnosis: syncope • Chronic cases 15 - 20% not epilepsy mostly psychological in nature § Careful diagnostic assessment a must in all cases
The Single Seizure • A controversial area! • Single unprovoked attack usually not treated: practice to defer treatment until 2 or more seizures, although patients at high risk may be treated after a first attack • Incidence of epilepsy much greater than of single seizures • Community-based studies show that overall risk of a second seizure greater than previously accepted • selection bias § Patients § Seizure type è time to entry bias
The Single Seizure • AED treatment following a single seizure reduce risk of recurrence in the short term although long term prognosis not changed • This may eventually lead to changes in the way single seizures are managed • treatment after first seizure • - for six months, for a year? • tailored treatment and not symptomatic • Meanwhile, involve patient and or guardians in the decision
Recurrent Seizures • Treatment recommended after two or more seizures v Exceptions: - Long interval between seizures - Clear identifiable precipitant factor - Patient against treatment - Unlikely compliance
Precipitating Factors ü Fever ü Drugs ü Alcohol ü Photo-Sensitivity ü Sleep Deprivation ü Reflex Mechanisms ü Acute Metabolic Stress ü Emotional Stress/Major Life Events
Starting an AED • Starting AED treatment is a major event and should not be undertaken without careful evaluation of all relevant factors • Therapy is a long term prospect • All implications must be fully explained to the individual and or guardian • Paramount that the patient or guardians are kept informed about the treatment process and the rationale behind it
Starting Treatment • Treatment should always be started with a single drug at a small dose • All common side-effects must be discussed • teratogenicity and contraception if applicable • Importance of compliance should be stressed • Careful titration is a must - start low, go slow
Choice of AEDs treatment • Choice of AED influenced by: • • Type of seizure and or epileptic syndrome Individual circumstances of patient Side effect profile of drug Personal preferences • No clear cut evidence based medicine is available! • Clinical practice is based more on dogmatic teaching than on scientific knowledge • Empirical rather than rational
Principles of AED treatment • Diagnosis clearly established • Appropriate first line drug for syndrome and patient • One drug at a time as a rule: – If first drug ineffective add another first line drug and then withdraw first drug • Combination therapy only when single drug ineffective

What Is Chronic Epilepsy ? • Active 2 years after onset • Failed 2 first line AEDs • Great number of seizure in early history
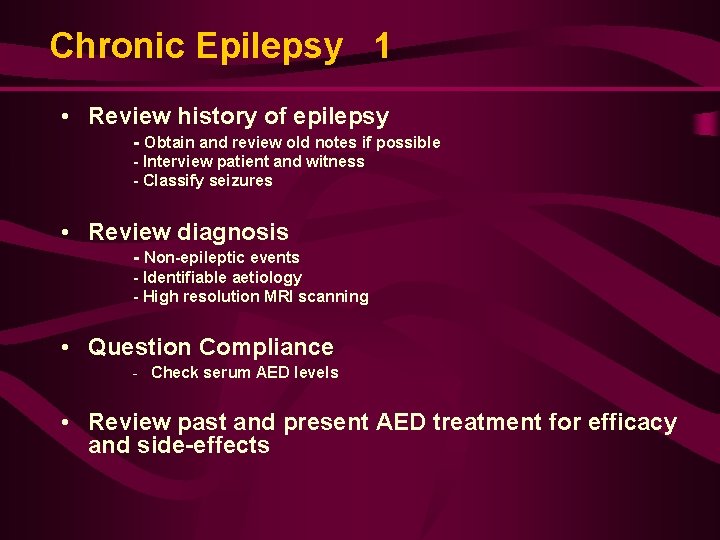
Chronic Epilepsy 1 • Review history of epilepsy - Obtain and review old notes if possible - Interview patient and witness - Classify seizures • Review diagnosis - Non-epileptic events - Identifiable aetiology - High resolution MRI scanning • Question Compliance - Check serum AED levels • Review past and present AED treatment for efficacy and side-effects
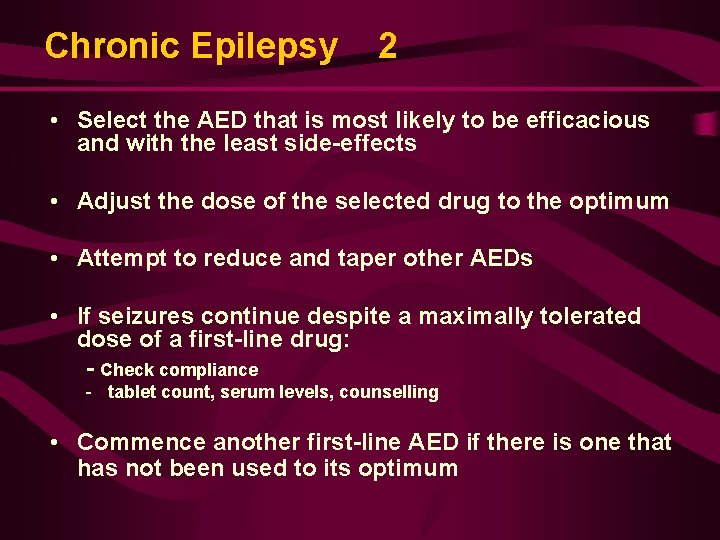
Chronic Epilepsy 2 • Select the AED that is most likely to be efficacious and with the least side-effects • Adjust the dose of the selected drug to the optimum • Attempt to reduce and taper other AEDs • If seizures continue despite a maximally tolerated dose of a first-line drug: - Check compliance - tablet count, serum levels, counselling • Commence another first-line AED if there is one that has not been used to its optimum
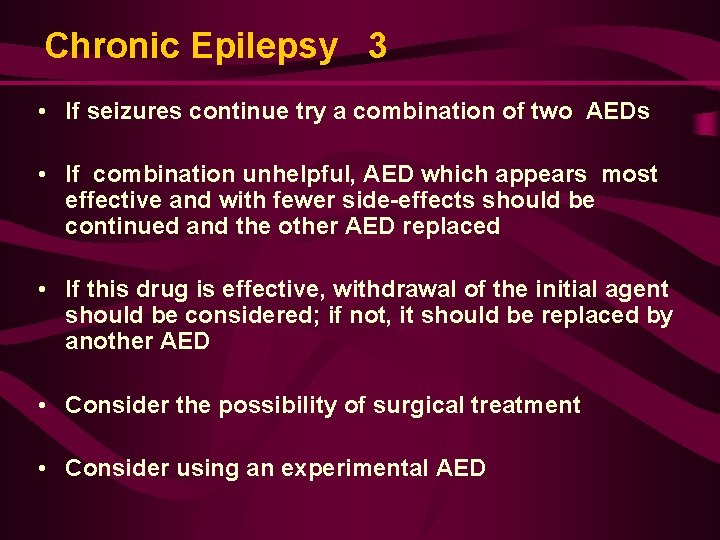
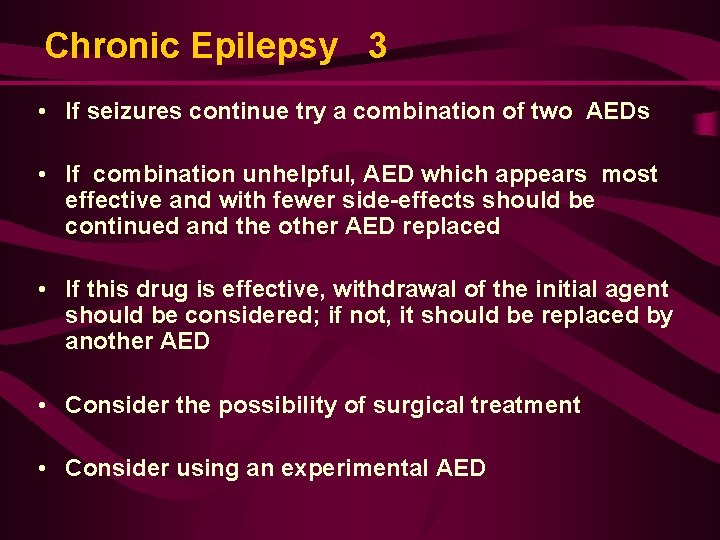
Chronic Epilepsy 3 • If seizures continue try a combination of two AEDs • If combination unhelpful, AED which appears most effective and with fewer side-effects should be continued and the other AED replaced • If this drug is effective, withdrawal of the initial agent should be considered; if not, it should be replaced by another AED • Consider the possibility of surgical treatment • Consider using an experimental AED
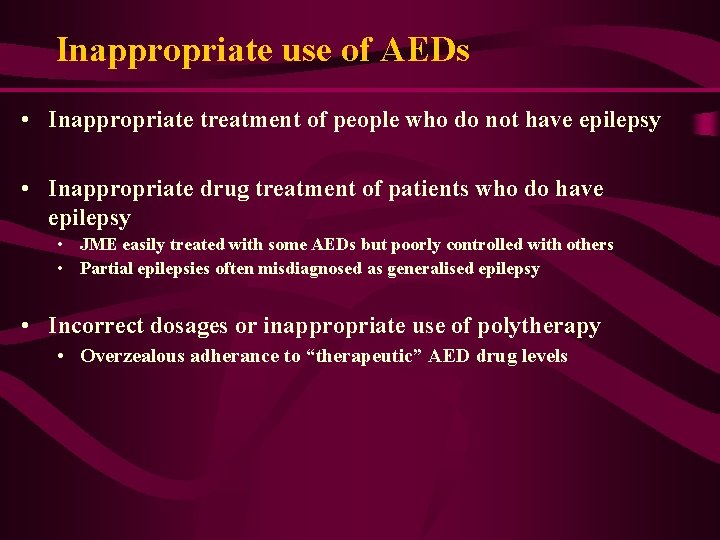
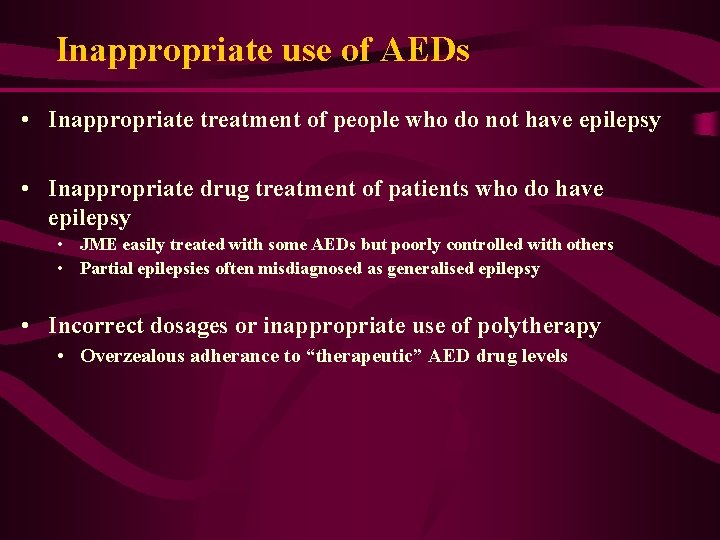
Inappropriate use of AEDs • Inappropriate treatment of people who do not have epilepsy • Inappropriate drug treatment of patients who do have epilepsy • JME easily treated with some AEDs but poorly controlled with others • Partial epilepsies often misdiagnosed as generalised epilepsy • Incorrect dosages or inappropriate use of polytherapy • Overzealous adherance to “therapeutic” AED drug levels
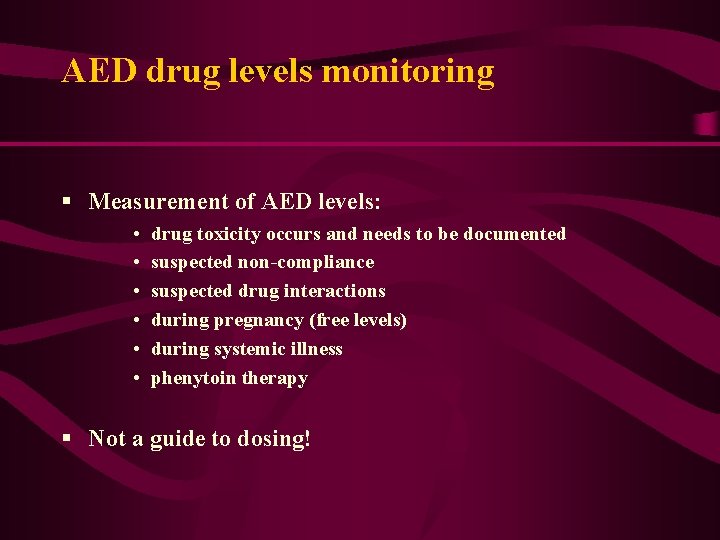
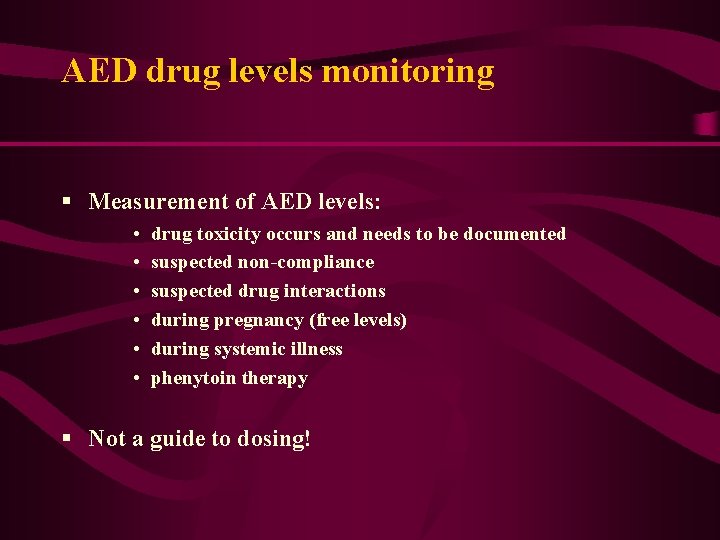
AED drug levels monitoring § Measurement of AED levels: • • • drug toxicity occurs and needs to be documented suspected non-compliance suspected drug interactions during pregnancy (free levels) during systemic illness phenytoin therapy § Not a guide to dosing!

Who Should be Evaluated for Surgery • Partial seizures: simple, complex, sec gen. • Stereotyped onset • No non-epileptic attacks • No contraindication for Neurosurgery • Active epilepsy for >2 -3 yr, despite 3 + AEDs • Inadequate seizure control: > 1 -2 c p s /month • Acceptance of best risk / benefit ratio
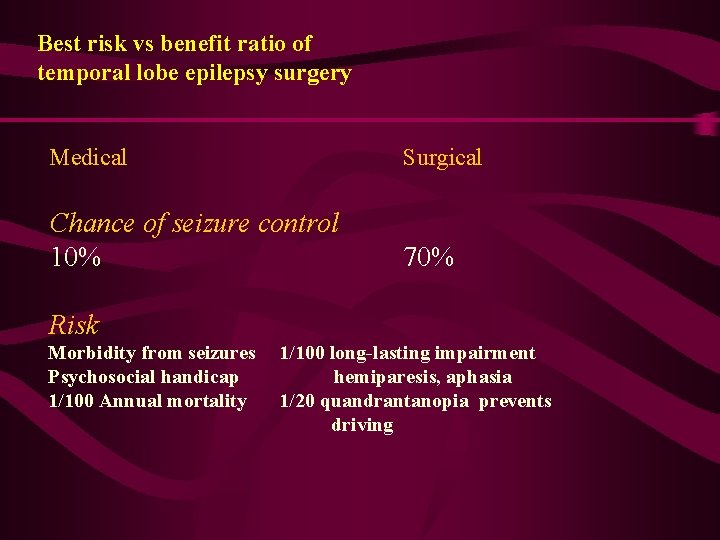
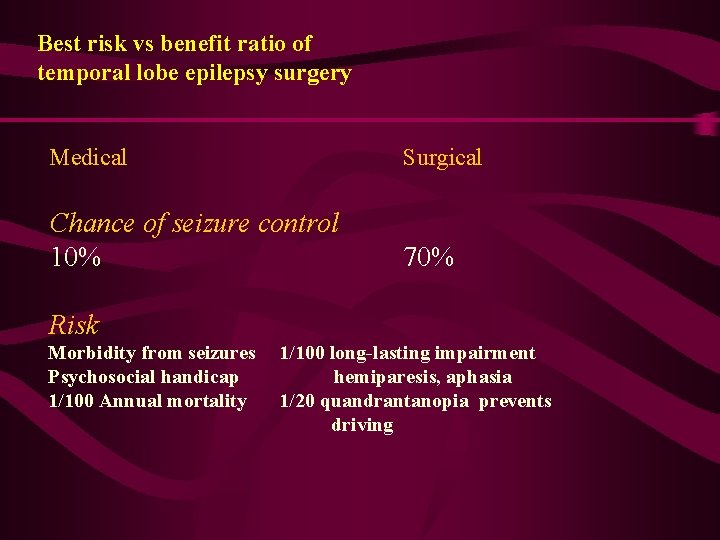
Best risk vs benefit ratio of temporal lobe epilepsy surgery Medical Surgical Chance of seizure control 10% 70% Risk Morbidity from seizures 1/100 long-lasting impairment Psychosocial handicap hemiparesis, aphasia 1/100 Annual mortality 1/20 quandrantanopia prevents driving
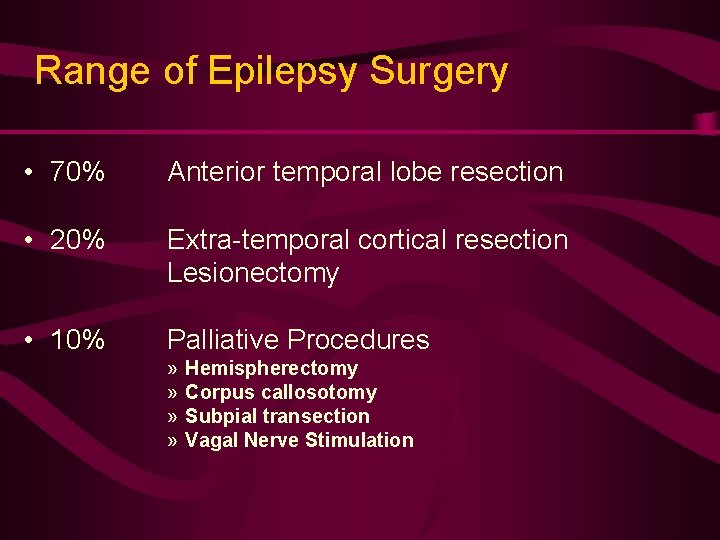
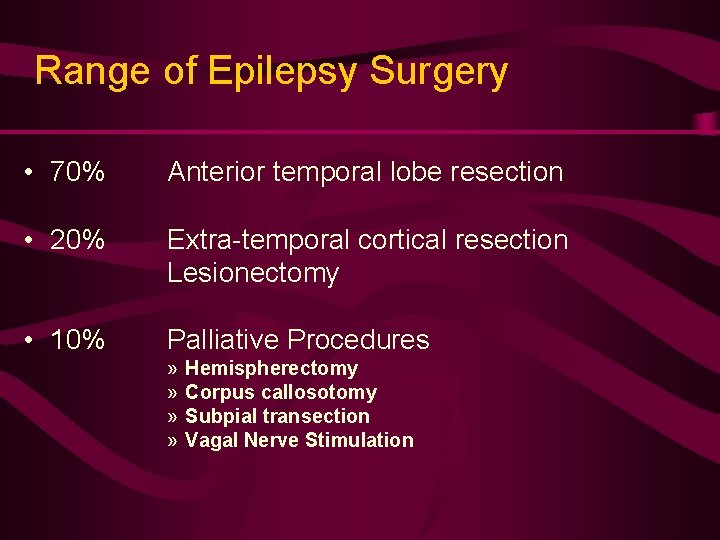
Range of Epilepsy Surgery • 70% Anterior temporal lobe resection • 20% Extra-temporal cortical resection Lesionectomy • 10% Palliative Procedures » » Hemispherectomy Corpus callosotomy Subpial transection Vagal Nerve Stimulation
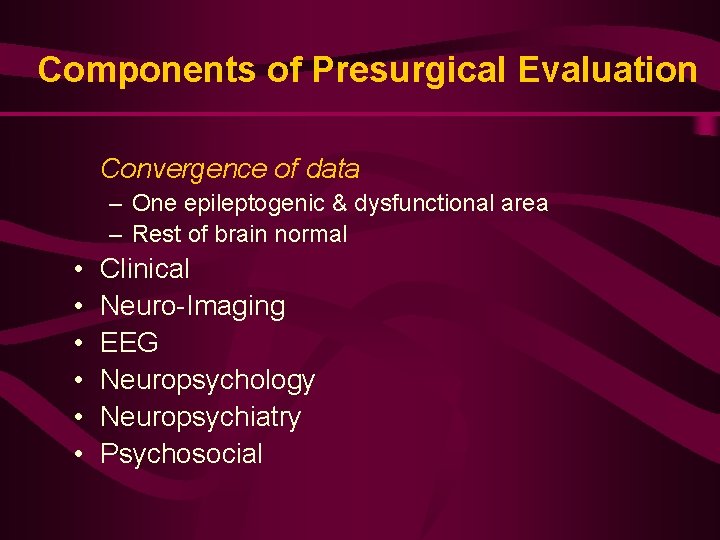
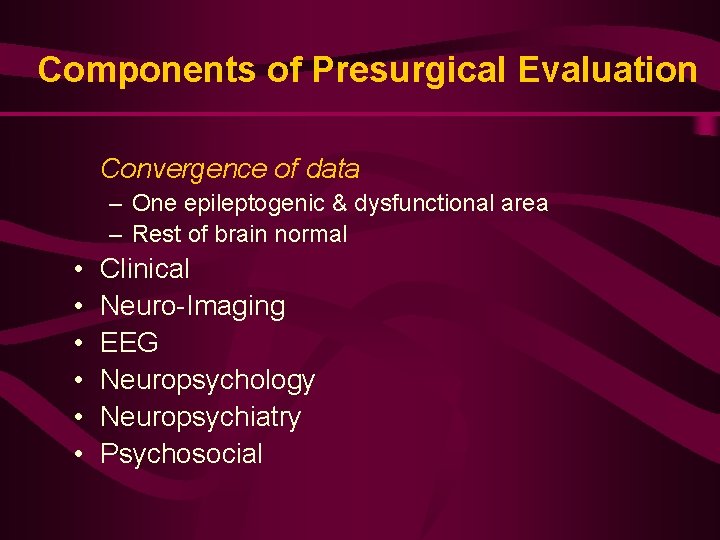
Components of Presurgical Evaluation Convergence of data – One epileptogenic & dysfunctional area – Rest of brain normal • • • Clinical Neuro-Imaging EEG Neuropsychology Neuropsychiatry Psychosocial

Psychosocial • • Realistic expectations? Improvement in life from seizure control? Intelligence, memory will not improve Not more attractive, employable Need to continue AEDs after Social support • Family, friends, community, finances
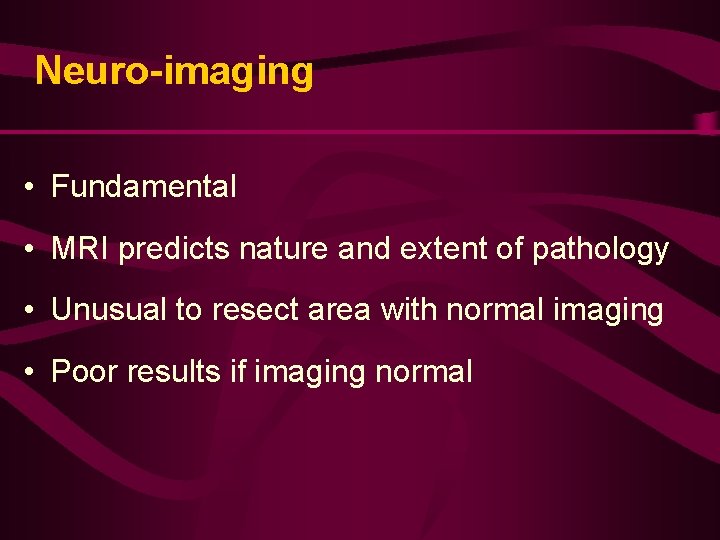
Neuro-imaging • Fundamental • MRI predicts nature and extent of pathology • Unusual to resect area with normal imaging • Poor results if imaging normal
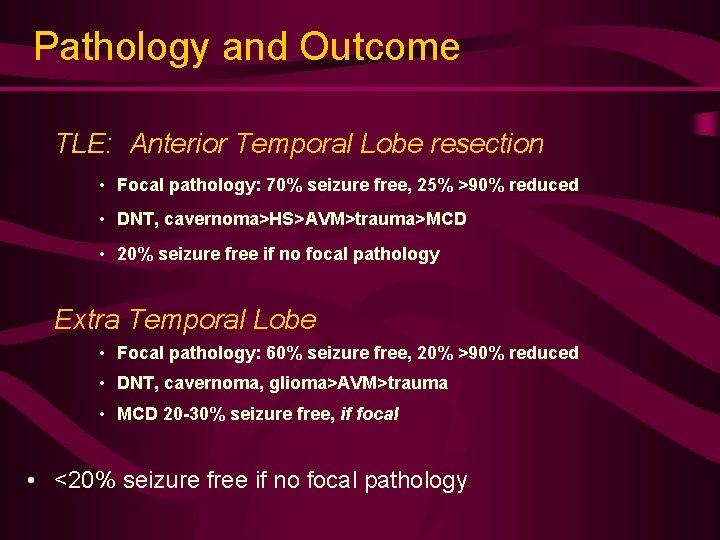
Pathology and Outcome TLE: Anterior Temporal Lobe resection • Focal pathology: 70% seizure free, 25% >90% reduced • DNT, cavernoma>HS>AVM>trauma>MCD • 20% seizure free if no focal pathology Extra Temporal Lobe • Focal pathology: 60% seizure free, 20% >90% reduced • DNT, cavernoma, glioma>AVM>trauma • MCD 20 -30% seizure free, if focal • <20% seizure free if no focal pathology
Treatment Guidelines for Epilepsy • NICE = www. nice. org. uk – National Institute for Clinical Excellence (England Wales) • SIGN = www. sign. ac. uk – Scottish Intercollegiate Guidelines Network (Scotland) • AAN = www. aan. com – American Academy of Neurology (USA)
Primary Care Guidelines for Epilepsy • Referral of ALL who experience a suspected seizure – Seen within 14 days by specialist • • Risk and safety precautions documented Care Plan in place At least a yearly review Early re-referral if – – – Treatment failure Seizures not controlled Diagnostic uncertainty Considering pregnancy Considering drug withdrawal
Managing People With Epilepsy § Holistic issues: - Interest and continuity of care - Clear plan - Information provision - SUDEP - Easy access - Practical Issues: • Cooking, Bathing, Driving, Contraception, Conception - Reasonable Expectations: • Prognosis, Independent Living, Employment
AED Treatment: Conclusions § Correct diagnosis and classification paramount to treatment § AEDs are mainstay treatment § Treatment empirical rather than rational! § > 70% of patients become seizure free § Potential complications: toxicity § Low threshold for s/effects
AED Treatment: Conclusions § Potential for misuse of AEDs not to be dismissed § New AEDs may be better tolerated, but more effective? § Chronic side effect profile of new AEDs not fully known § Surgical treatment very successful but only possible in a few selected cases § Consider stopping AED if seizure free for years § New treatment still needed!
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Defination of proportion
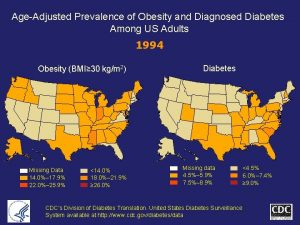
Defination of proportion Age adjusted prevalence
Age adjusted prevalence Ocd ego syntonic
Ocd ego syntonic Adhd prevalence by country
Adhd prevalence by country Obesity prevalence europe
Obesity prevalence europe Incidence and prevalence meaning
Incidence and prevalence meaning Prevalence
Prevalence Prevalence rate formula
Prevalence rate formula Calculate relative risk
Calculate relative risk Epirates
Epirates Attack rate epidemiology formula
Attack rate epidemiology formula Prevalence ratio
Prevalence ratio Uuuu_limited
Uuuu_limited Prevalence ratio
Prevalence ratio Prevalence calculation
Prevalence calculation Who global estimates on prevalence of hearing loss 2020
Who global estimates on prevalence of hearing loss 2020 Ukuran frekuensi epidemiologi
Ukuran frekuensi epidemiologi Prevalence of schizophrenia
Prevalence of schizophrenia Prevalence
Prevalence Cvst prevalence
Cvst prevalence Measures of association in epidemiology
Measures of association in epidemiology Ocd vs anxiety
Ocd vs anxiety Prevalence vs incidence
Prevalence vs incidence Who global estimates on prevalence of hearing loss 2020
Who global estimates on prevalence of hearing loss 2020 Point prevalence rate adalah
Point prevalence rate adalah Cross sectional study
Cross sectional study Prevalence of obesity
Prevalence of obesity Prevalence
Prevalence Hyperinsulinemia
Hyperinsulinemia 3 to 8 decoder truth table
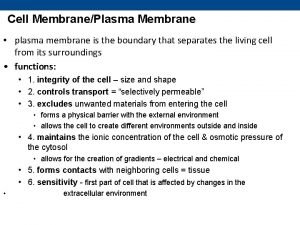
3 to 8 decoder truth table Primary active transport and secondary active transport
Primary active transport and secondary active transport Primary active transport vs secondary active transport
Primary active transport vs secondary active transport Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính thế năng
Công thức tính thế năng Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8