Epilepsy School Nurses Presentation Lucyna Zawadzki MD Meghan







- Slides: 31
Epilepsy School Nurses’ Presentation Lucyna Zawadzki, MD Meghan Furstenberg-Knauff, BSN, RN, MSN, FNPBC, APNP Kamilee Hobbs BSN, RN
Part 2: Treatment Options
What are they? • Medications – Anti Epileptic Drugs (AEDs) – IVIG • Epilepsy Surgery • Ketogenic Therapy • VNS

Medications • • • Making the choice as to what medication to use for seizure treatment is a difficult decision. Seizures are the result of abnormal electrical activity. This is the results of an imbalance between the excitation and inhibition. Anti-seizure medications impact the key players to prevent seizure activity.
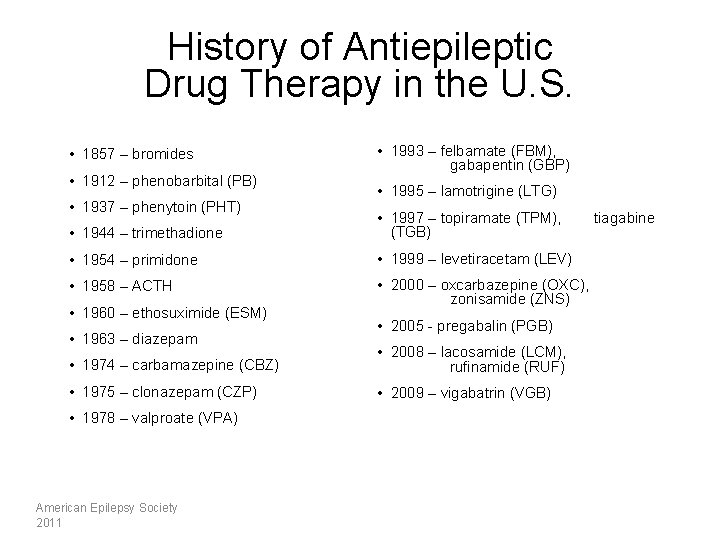
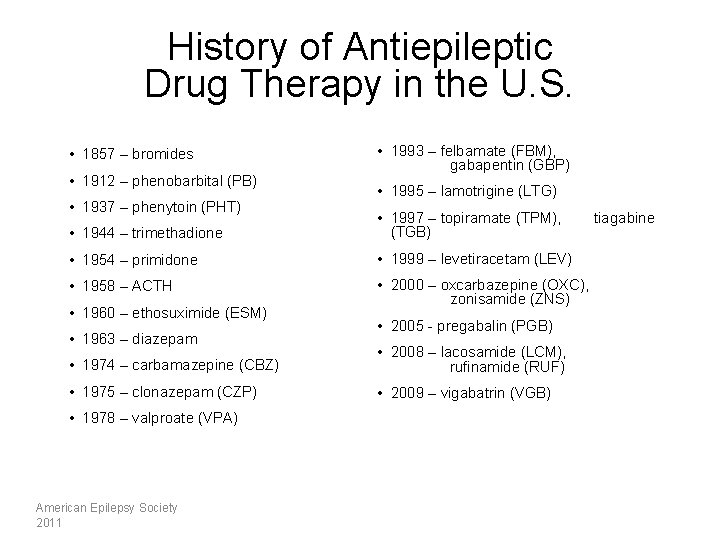
History of Antiepileptic Drug Therapy in the U. S. • 1857 – bromides • 1912 – phenobarbital (PB) • 1937 – phenytoin (PHT) • 1993 – felbamate (FBM), gabapentin (GBP) • 1995 – lamotrigine (LTG) • 1944 – trimethadione • 1997 – topiramate (TPM), (TGB) • 1954 – primidone • 1999 – levetiracetam (LEV) • 1958 – ACTH • 2000 – oxcarbazepine (OXC), zonisamide (ZNS) • 1960 – ethosuximide (ESM) • 1963 – diazepam • 2005 - pregabalin (PGB) • 1974 – carbamazepine (CBZ) • 2008 – lacosamide (LCM), rufinamide (RUF) • 1975 – clonazepam (CZP) • 2009 – vigabatrin (VGB) • 1978 – valproate (VPA) American Epilepsy Society 2011 tiagabine
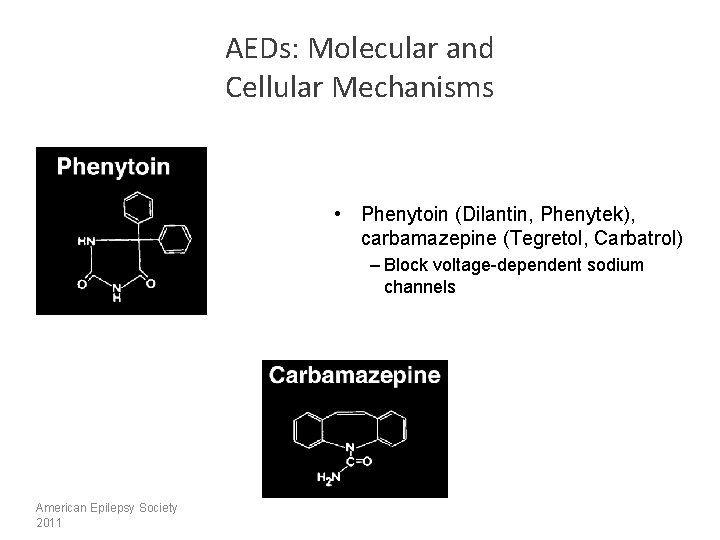
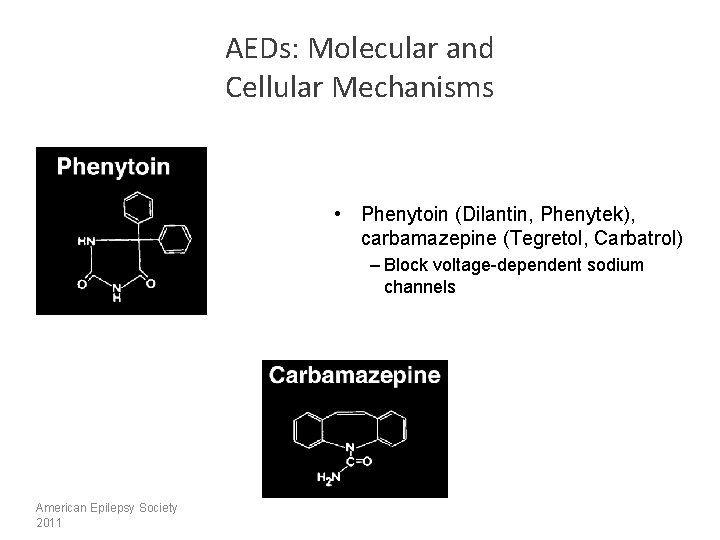
AEDs: Molecular and Cellular Mechanisms • Phenytoin (Dilantin, Phenytek), carbamazepine (Tegretol, Carbatrol) – Block voltage-dependent sodium channels American Epilepsy Society 2011

AEDs: Molecular and Cellular Mechanisms • barbiturates – Prolong GABA-mediated chloride channel openings – Phenobarbital • benzodiazepines – Increase frequency of GABAmediated chloride channel openings – Clobazepam – Clobazam (Onfi) American Epilepsy Society 2011

AEDs: Molecular and Cellular Mechanisms • felbamate (Felbatol) – Blocks voltage-dependent sodium channels – Modulates NMDA receptor and GABA receptors • gabapentin (Neurontin) – Blocks calcium channels – Suppressed presynaptic vesicle release American Epilepsy Society 2011
AEDs: Molecular and Cellular Mechanisms • lamotrigine (Lamictal, Lamictal XR) – Blocks voltage-dependent sodium channels American Epilepsy Society 2011

AEDs: Molecular and Cellular Mechanisms • Ethosuximide (Zarontin) – Blocks low threshold, “transient” (T-type) calcium channels in thalamic neurons • Valproate, Divalproex Sodium – May enhance GABA transmission in specific circuits – Blocks voltage-dependent sodium channels – Modulates T-type calcium channels American Epilepsy Society 2011
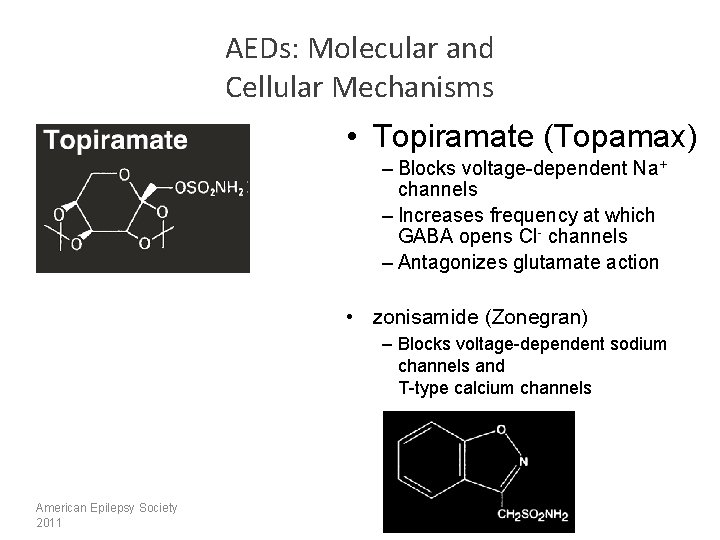
AEDs: Molecular and Cellular Mechanisms • Topiramate (Topamax) – Blocks voltage-dependent Na+ channels – Increases frequency at which GABA opens Cl- channels – Antagonizes glutamate action • zonisamide (Zonegran) – Blocks voltage-dependent sodium channels and T-type calcium channels American Epilepsy Society 2011
AEDs: Molecular and Cellular Mechanisms • Levetiracetam (Keppra, Keppra XR) – Action is unknown, suspect it acts on GABA • Oxcarbazepine (Trileptal, Oxtellar XR) – Blocks voltage-dependent sodium channels – Exerts effect on K+ channels American Epilepsy Society 2011
AEDs: Molecular and Cellular Mechanisms • Lacosamide (Vimpat) –Enhances slow inactivation of voltage gated sodium channels American Epilepsy Society 2011
AEDs: Molecular and Cellular Mechanisms • rufinamide – Unclear: Possibly stabilization of the sodium channel inactive state • vigabatrin – Irreversibly inhibits GABAtransaminase American Epilepsy Society 2011
• For Generalized seizures: – – – • Levetiracetam (Keppra) Lamotrigine Topiramate Zonegran Valproic Acid Ethosuximidate – specifically used for absence seizures For Partial seizures: – Oxcarbazepine
IVIG Therapy • Inflammation is known to cause several neurological disorders. • Recently, it is being acknowledged to have a role in Epilepsy. • IVIG – Intravenous immunoglobulin – contains pooled, polyvalent, Ig. G antibodies that work to suppress inflammation. • It’s on the horizon as an effective treatment for Epilepsy.

Medication Alternatives

Epilepsy Surgery Seizure Epilepsy diagnosis Medication trials Imaging for pathology Medical intractability Surgical Consideration Surgical workup Surgery American Epilepsy Society 2011
Ketogenic Therapy • This is a rigid, mathematically calculated, doctorsupervised diet. It can only be attempted under close medical and dietary supervision. • Who is a candidate? – In general, individuals with uncontrolled seizures that have failed at least two medications for seizure control can be considered for this therapy. – Research shows that it is more effective for certain seizures types. These include infantile spasms, Doose Syndrome, Rett Syndrome, and tuberous sclerosis complex.
Ketogenic Therapy • The Basics: – The ketogenic diet is a medical treatment for controlling seizures by switching the body's primary energy source to fat-based (ketones) verses sugar-based (glucose). – We are not sure why this diet is successful. – The diet can be adapted using table foods or given formula based. – There are potential side effects associated with the diet, however, all are treatable and reversible without having to stop the diet. • They include, lack of weight gain, slightly decreased growth, somewhat high cholesterol, constipation, kidney stones, and acidosis. • There a number of common misunderstandings about this therapy. • Additional Resources: – On the Web - The Charlie Foundation - www. charliefoundation. org
Vagus Nerve Stimulation • The Basics – The vagus nerve is one of the primary communication pathways between the body and the brain. – This is not drug therapy! VNS Therapy is delivered by a surgically implanted generator and lead. It's best to think of it as similar to a pacemaker. • Side Effects: – – – – – Cough* Hoarseness* Paraesthesia Shortness of Breath Vocal Cord Paralysis/weakness Infection Increased/Improved Mood Increased Alertness Improved Memory
Part 3: Safety
During a Seizure Caring for a child during a seizure is all about safety. The following is needed of you: • Keep calm. • Time the seizure. • Don't hold the child down or try to stop any movements. • Clear the area of any hard or sharp objects and loosen ties or anything around the neck that may make breathing difficult. • Place something flat and soft under the head. • Turn the child gently onto one side. This will help keep the airway clear. • Do not try to force the mouth open with any hard objects or with fingers. A person having a seizure CANNOT swallow their tongue. Efforts to hold the tongue down can injure teeth or the jaw. • Remain with child the entire time. • The child may be disoriented and confused as they wake from the seizure, be reassuring during this time. • Assess for injury and respiratory status. • If the child is sleepy following the seizure, allow them to rest. • Nothing to eat or drink until able to swallow.
When to Call 911 • When seizures approach 5 minutes in duration or per patient's seizure action plan (administering rescue med for the first time). • If the child has seizures back to back • If it's the child's first seizure • If injury is suspected • If child is pregnant or diabetic • If child does not return to baseline in an expected amount of time post seizure activity 24
Potential Injuries from Seizures • Immediate: lacerations, bruises, burns, head trauma, fractures, and drowning/near drowning. • Delayed: fever, aspiration pneumonia, subdural hematomas, and fractures. 25

Tips for Seizure Observation and Documentation • What happened before, during, and after the event • Be detailed • Include lots of information from the start to the end 26
Seizure Safety • There are some restrictions that must be in place for a period of time following a seizure in order to keep the child safe. These restrictions are in place for 90 days, they include: – No driving a motor vehicle or operating heavy machinery (this is mandated by the State of Wisconsin Department of Transportation). – No high climbing, this means nothing higher then 2 steps off the ground or the child’s height. – No swimming in lakes or rivers due to concerns with currents and the worry that if a seizure occurred the child could be swept away or under. – If swimming in a pool or soaking in a hot tub, must have an adult in the water at all times within an arms reach. – No tub baths. Children should only shower during this period. • Any individual who is being treated for seizures should avoid sports where a moment’s inattention could lead to injury these include such activities as skydiving, bungee-jumping, scuba-diving, or motor racing. • We strongly encourage Medical Alert use.
Home “Rescue” Medications • We typically prescribe a specific medication to be used when a child has a prolonged seizure or a cluster of seizure activity (a series of seizures in a short amount of time) that can be used at home. This medication is a rescue medication. • These medications can be administered in a variety of ways. We typically used two routes, buccal or rectal. • The medication that is prescribed depends on the type of seizure a child has and the age of the child. We prescribed either rectal Diastat or buccal Midazolam.
Diastat • Diastat is a rectal form of diazepam that is used to stop a seizure. • It is effective, well tolerated, and side effects such as changes in breathing are not common. • Dosing of this medication is dependent on a child’s age and weight. • The biggest advantage of giving a medication rectally during a seizure is that it can be given and absorbed quickly. • Education on Diastat administration should be preformed while inpatient. The drug company provides a DVD as well as teaching sheets.
Midazolam • Midazolam is a short acting benzodiazepine. • It can be administered in two ways for rescue with a single prolonged seizure or cluster, buccal or intranasal. • The most common side effects are drowsiness, tiredness, weakness, and nausea. There is a chance that a child may experience breathing problems following this medication. We advise families that the first time they use this, they call 911 to ensure it is well tolerated. • To administer buccally, simply divide the prescribed dose in half, giving on each side between the cheek and gum.
Communication and Collaboration with Healthcare Providers • Medication Administration Forms • Any concerns about medication compliance or safety risks. • Any letters for special privileges (water bottles, activity restrictions, etc. ) • Any general questions about medications • Any general questions about plan of care • We encourage you to fax us updates or concerns. This is recommended as we know we will likely recieve this correspondence.
 Aleksander zawadzki umk
Aleksander zawadzki umk Tadeusz zawadzki
Tadeusz zawadzki Dr zawadzki
Dr zawadzki Lucyna wronska
Lucyna wronska Lucyna moari
Lucyna moari Universal security audit programme
Universal security audit programme Naviance eanes
Naviance eanes Meghan vogel
Meghan vogel Meghan troup dalhousie
Meghan troup dalhousie Meghan miller unt
Meghan miller unt Fish bone nursing
Fish bone nursing Coleman block test
Coleman block test Meghan anzelc
Meghan anzelc Meghan flores
Meghan flores Meghan stasz
Meghan stasz Nasn vision vouchers
Nasn vision vouchers Alabama association of school nurses
Alabama association of school nurses Epilepsy ilae 2017
Epilepsy ilae 2017 Hau yee
Hau yee Canadian league against epilepsy
Canadian league against epilepsy Migraine vs epilepsy
Migraine vs epilepsy Inflatable helmet for epilepsy
Inflatable helmet for epilepsy Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Aremco epilepsy
Aremco epilepsy Vanderbilt nurse residency interview questions
Vanderbilt nurse residency interview questions Benign rolandic epilepsy rch
Benign rolandic epilepsy rch Epilepsy trigger
Epilepsy trigger Epilepsy and seizure services near walnut creek
Epilepsy and seizure services near walnut creek European epilepsy database
European epilepsy database Difference between seizure and epilepsy
Difference between seizure and epilepsy Catastrophic epilepsy infancy
Catastrophic epilepsy infancy Post itical
Post itical