Epilepsy Kate Mc GrawAllen Definition Seizure Spontaneous intermittent


- Slides: 25
Epilepsy Kate Mc. Graw-Allen
Definition Seizure- Spontaneous, intermittent electrical activity in the brain resulting in temporary signs and symptoms Epilepsy- The recurrent tendency for seizures 2 or more seizures separated by 24 hours without a clear cause
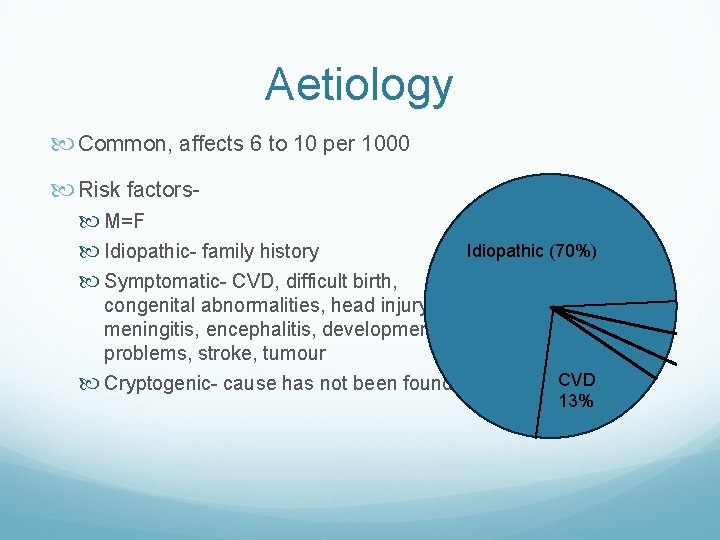
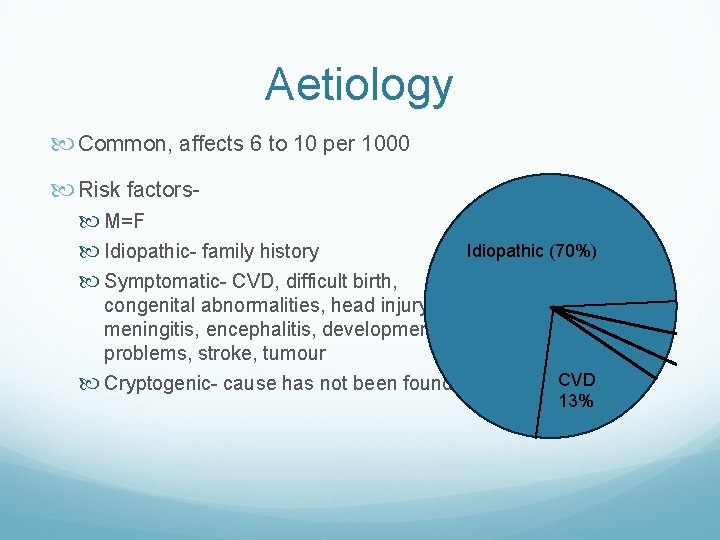
Aetiology Common, affects 6 to 10 per 1000 Risk factors M=F Idiopathic- family history Symptomatic- CVD, difficult birth, Idiopathic (70%) congenital abnormalities, head injury, meningitis, encephalitis, developmental problems, stroke, tumour Cryptogenic- cause has not been found CVD 13%

Aetiology Triggers Stress Lack of sleep Alcohol Drugs (medications and illicit) Flashing lights Menstruation Hyperventilation Illness
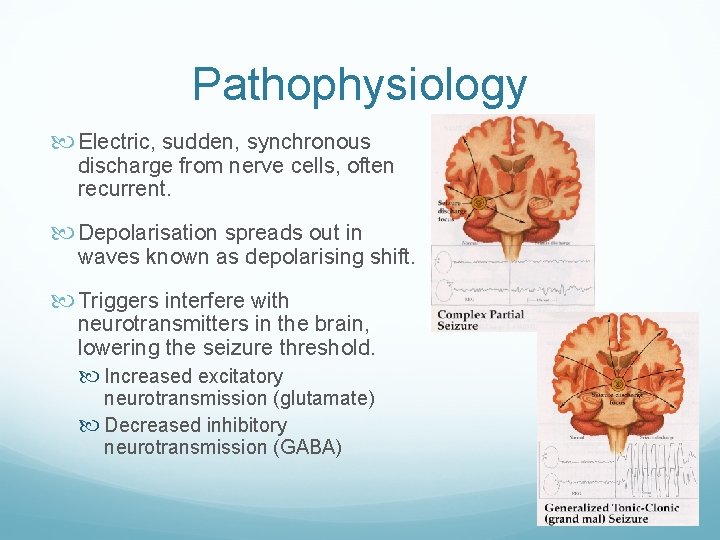
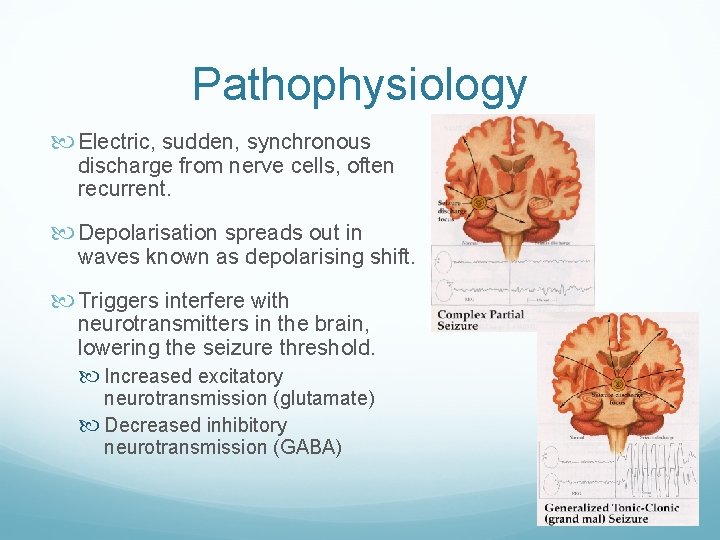
Pathophysiology Electric, sudden, synchronous discharge from nerve cells, often recurrent. Depolarisation spreads out in waves known as depolarising shift. Triggers interfere with neurotransmitters in the brain, lowering the seizure threshold. Increased excitatory neurotransmission (glutamate) Decreased inhibitory neurotransmission (GABA)
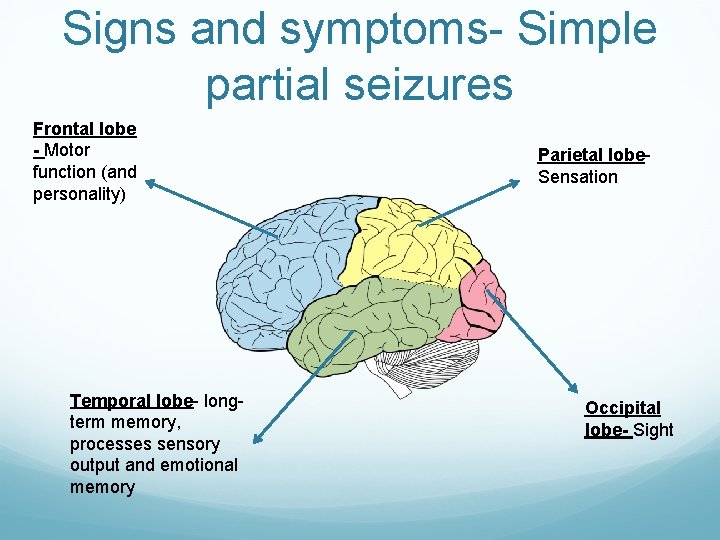
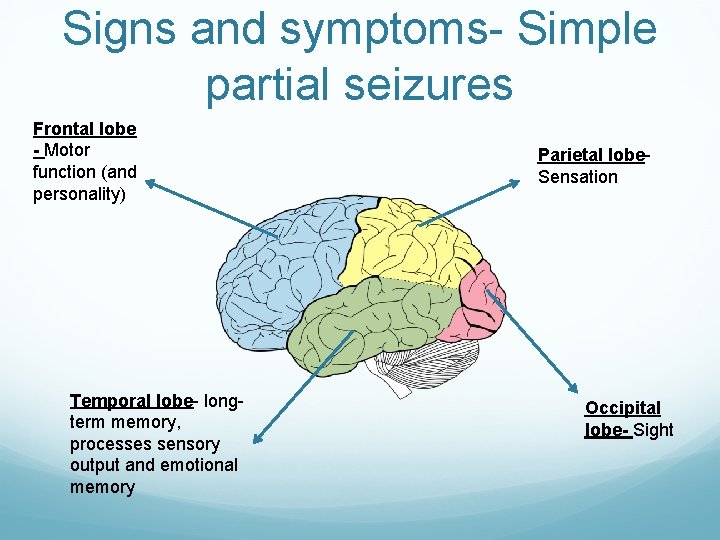
Signs and symptoms- Simple partial seizures Frontal lobe - Motor function (and personality) Temporal lobe- longterm memory, processes sensory output and emotional memory Parietal lobe. Sensation Occipital lobe- Sight
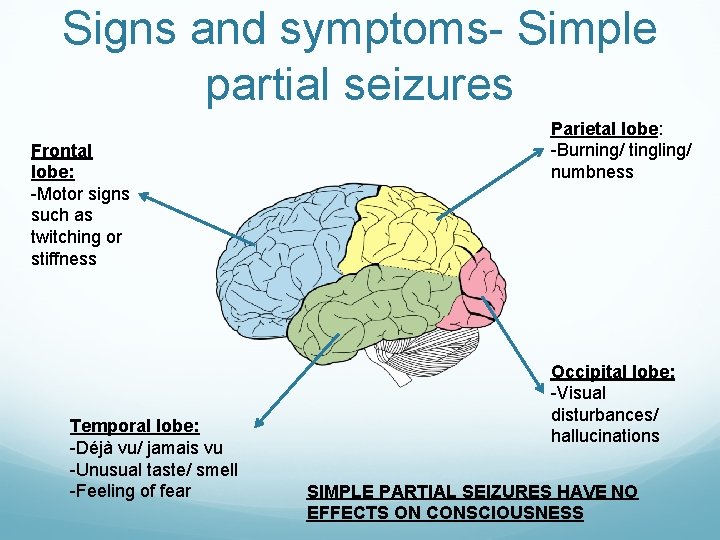
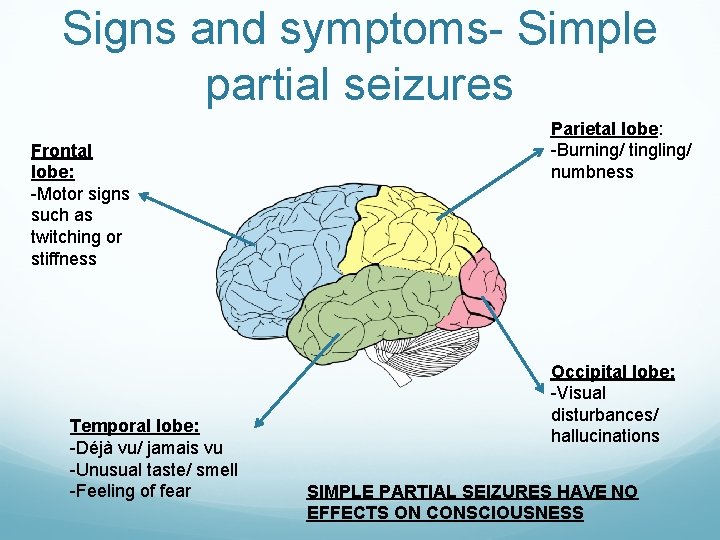
Signs and symptoms- Simple partial seizures Frontal lobe: -Motor signs such as twitching or stiffness Temporal lobe: -Déjà vu/ jamais vu -Unusual taste/ smell -Feeling of fear Parietal lobe: -Burning/ tingling/ numbness Occipital lobe: -Visual disturbances/ hallucinations SIMPLE PARTIAL SEIZURES HAVE NO EFFECTS ON CONSCIOUSNESS
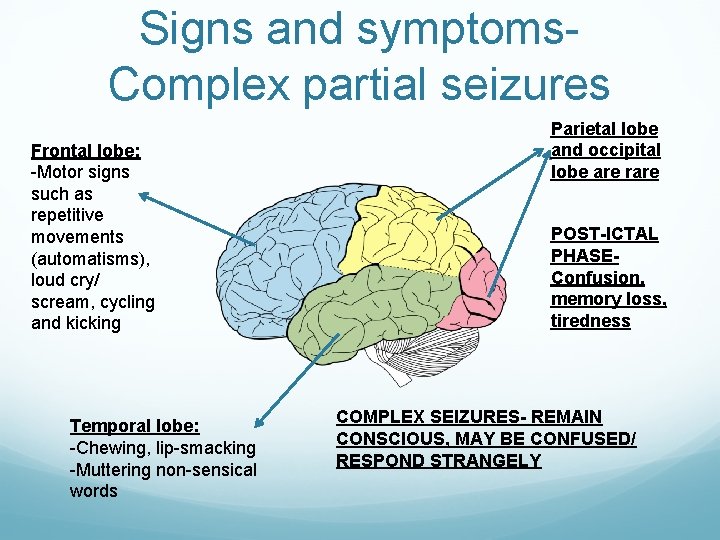
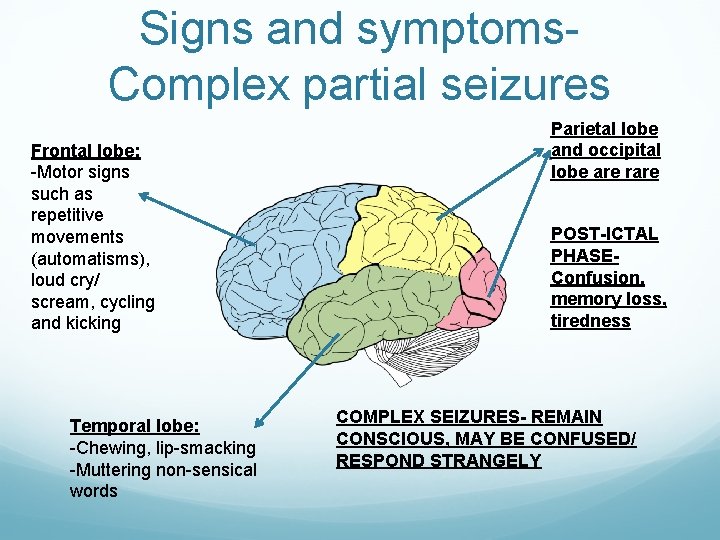
Signs and symptoms. Complex partial seizures Frontal lobe: -Motor signs such as repetitive movements (automatisms), loud cry/ scream, cycling and kicking Temporal lobe: -Chewing, lip-smacking -Muttering non-sensical words Parietal lobe and occipital lobe are rare POST-ICTAL PHASEConfusion, memory loss, tiredness COMPLEX SEIZURES- REMAIN CONSCIOUS, MAY BE CONFUSED/ RESPOND STRANGELY
Signs and Symptoms. Generalised seizures Activity across brain, person is unconscious Can come on after a simple seizure- secondary generalised seizure Absences https: //www. youtube. com/watch? v=H 3 i. LQi 6 wt 94
Signs and symptoms. Generalised seizures Tonic Clonic Tonic phase: Unconscious Become stiff and fall backwards Often cry out Often bite tongue/ cheek https: //www. youtube. com/w atch? v=Nds 2 U 4 Czv. C 4 Clonic phase: Jerk and shake as muscles relax and contract Breathing becomes difficult Blue skin Urination Post-ictal phase: Tired Confused Headache
Signs and symptoms. Generalised seizures Tonic Stiff muscles Fall backwards Atonic Muscles relax and go floppy Fall forwards Clonic Similar to clonic phase in tonic-clonic seizure Myoclonic Muscle jerks Often in morning- juvenile myoclonic epilepsy Consciousness not affected
Investigations History Warning symptoms- visual, olfactory, sweating, lightheadedness, nausea Loss of consciousness? Time periods Recovery- post ictal phase? Period of amnesia? Combatative? Medications? Drugs? Alcohol? Other health issues Driving and Job!
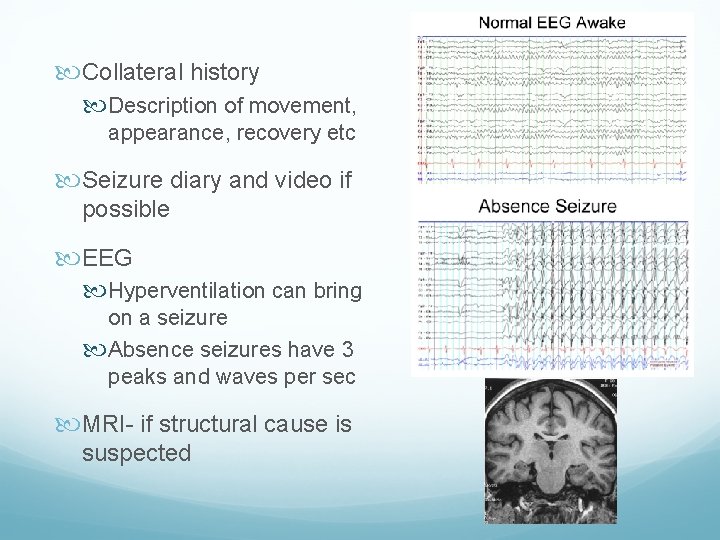
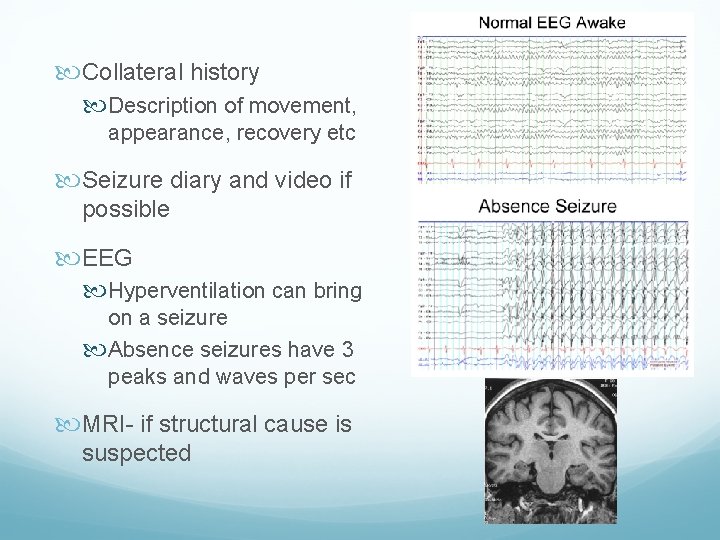
Collateral history Description of movement, appearance, recovery etc Seizure diary and video if possible EEG Hyperventilation can bring on a seizure Absence seizures have 3 peaks and waves per sec MRI- if structural cause is suspected
Complications Status epilepticus Injuries during fit Todd’s paralysis Depression/ anxiety
Alternative diagnosis Vasovagal syncope Hypo/ hyperglycaemia Electrolyte imbalance (Na+, K+, Ca+) Space occupying lesion Cardiac arrhythmias Postural hypotension Toxins (eg alcohol, drugs) Dissociative seizures
Additional Investigations Blood glucose Bloods- FBC, U+Es Drug screen ECG and further cardiac testing
Management Conservative Education Avoid triggers Notify DVLA Seizure free for 1 year before being able to drive again. Seizure free for 10 years without taking medication before driving HGV Medical alert bracelet Psychiatric help if struggling
Management Medical Carbamazepine Partial seizures Stabilises sodium channels and potentiate GABA receptors Therapeutic monitoring needed S/E- rash, sedation, dizziness, neutropenia Sodium Valproate Sodium channel blocker and inhibits enzymes breaking down GABA Generalised seizures S/E- weight gain, sedation, platelet dysfunction Teratogenicity
Management Medical Lamotrigine Sodium channel blocker Partial and generalised seizures S/E- rash leading to Steven Johnson’s syndrome, sedation Phenytoin Sodium channel blocker Partial and generalised seizures Therapeutic monitoring needed S/E- rash, sedation, diplopia,
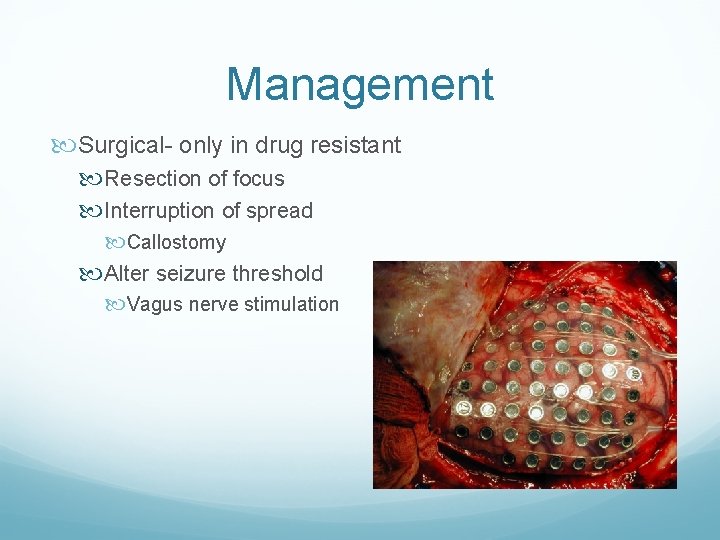
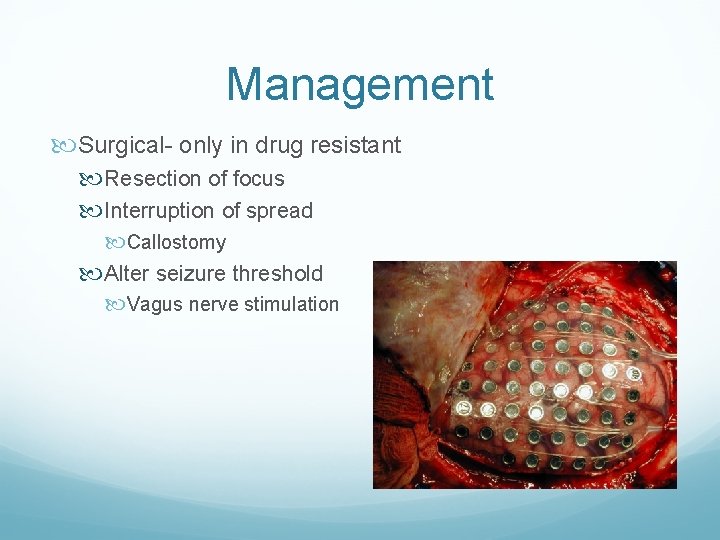
Management Surgical- only in drug resistant Resection of focus Interruption of spread Callostomy Alter seizure threshold Vagus nerve stimulation
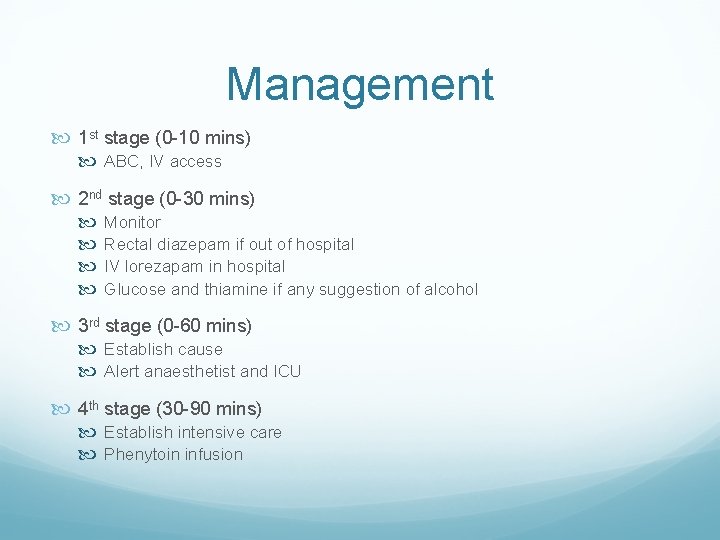
Status epilepticus Seizures normally last a set amount of time If it lasts >30 mins without regaining consciousness it is classed as status epilepticus This is a MEDICAL EMERGENCY
Management 1 st stage (0 -10 mins) ABC, IV access 2 nd stage (0 -30 mins) Monitor Rectal diazepam if out of hospital IV lorezapam in hospital Glucose and thiamine if any suggestion of alcohol 3 rd stage (0 -60 mins) Establish cause Alert anaesthetist and ICU 4 th stage (30 -90 mins) Establish intensive care Phenytoin infusion
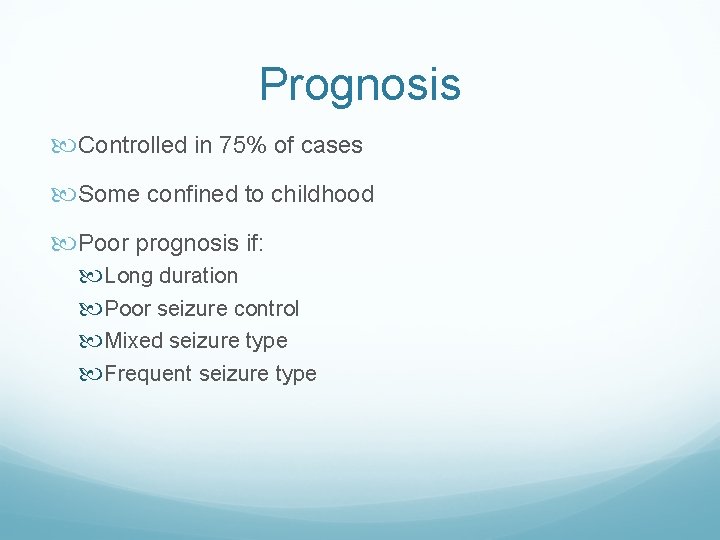
Prognosis Controlled in 75% of cases Some confined to childhood Poor prognosis if: Long duration Poor seizure control Mixed seizure type Frequent seizure type
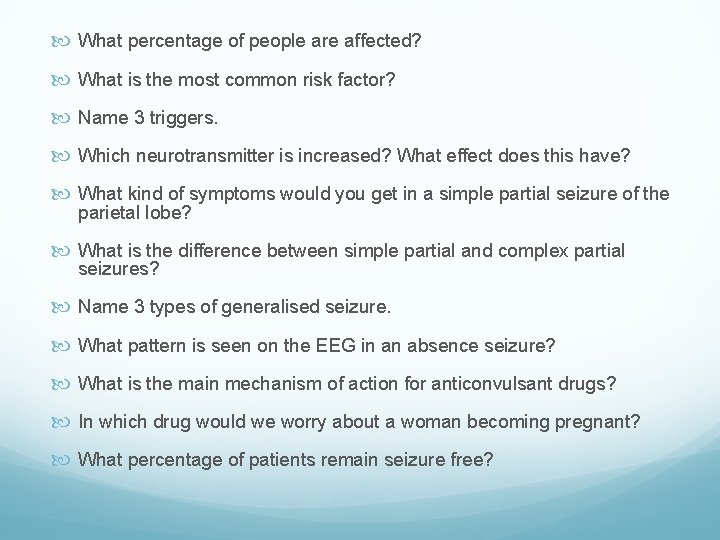
What percentage of people are affected? What is the most common risk factor? Name 3 triggers. Which neurotransmitter is increased? What effect does this have? What kind of symptoms would you get in a simple partial seizure of the parietal lobe? What is the difference between simple partial and complex partial seizures? Name 3 types of generalised seizure. What pattern is seen on the EEG in an absence seizure? What is the main mechanism of action for anticonvulsant drugs? In which drug would we worry about a woman becoming pregnant? What percentage of patients remain seizure free?

Questions?