Epidermolytic Hyperkeratosis EHK Bullous Congenital Ichthyosiform Erythroderma Brandon
Epidermolytic Hyperkeratosis (EHK) Bullous Congenital Ichthyosiform Erythroderma Brandon Newell, MD FIRST Family Conference Orlando, FL - June 27, 2010
Recently renamed Epidermolytic Ichthyosis (EI) FIRST Family Conference June 27, 2010
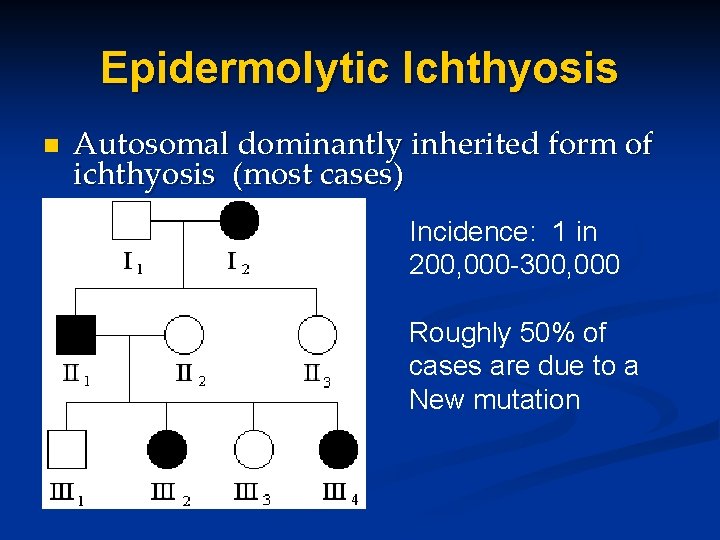
Epidermolytic Ichthyosis n Autosomal dominantly inherited form of ichthyosis (most cases) Incidence: 1 in 200, 000 -300, 000 Roughly 50% of cases are due to a New mutation
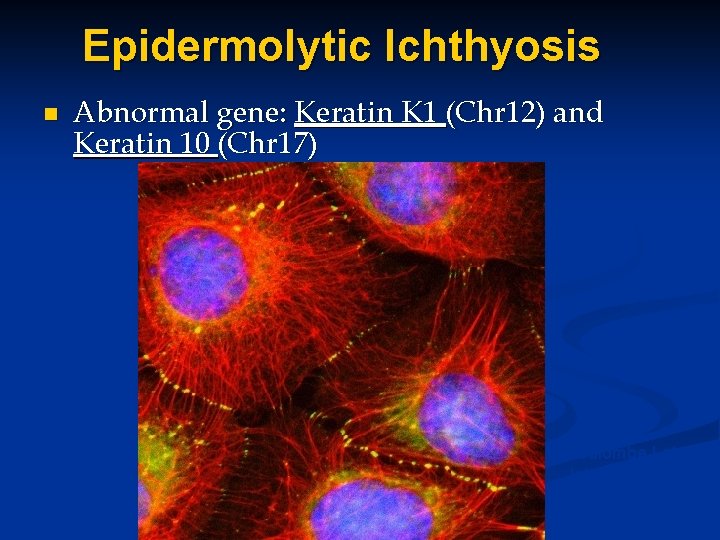
Epidermolytic Ichthyosis n Abnormal gene: Keratin K 1 (Chr 12) and Keratin 10 (Chr 17) Coulombe Lab Johns Hopkins
EHK: Keratin function n n Keratins form intermediate filaments Intermediate filaments provide structural stability to keratinocytes n Mutations=defective keratin proteins n Intermediate filaments, function poorly n Skin cell collapses blistering occurs n The thickening of the skin is thought to be compensatory to protect against blistering
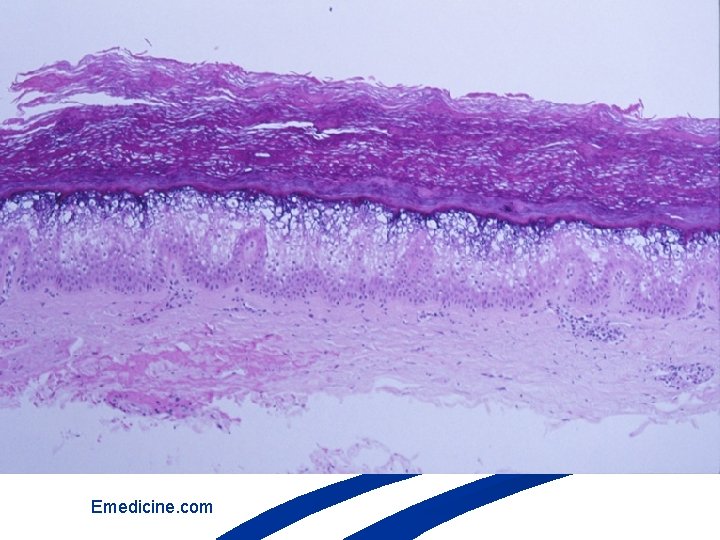
Emedicine. com
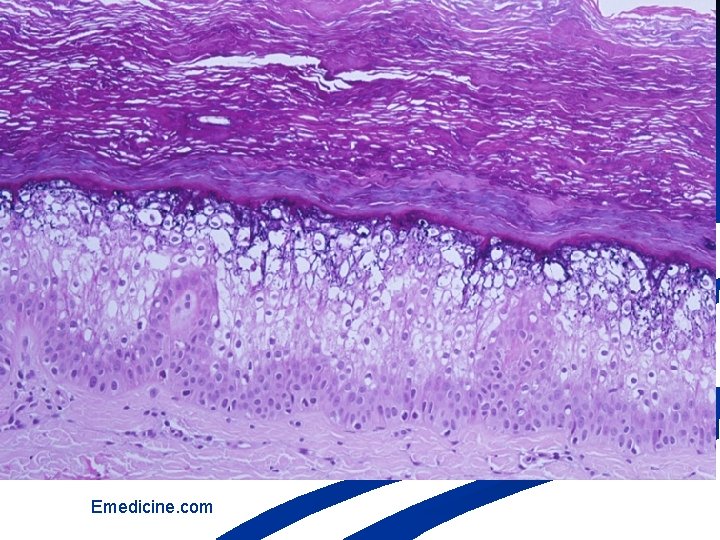
Emedicine. com
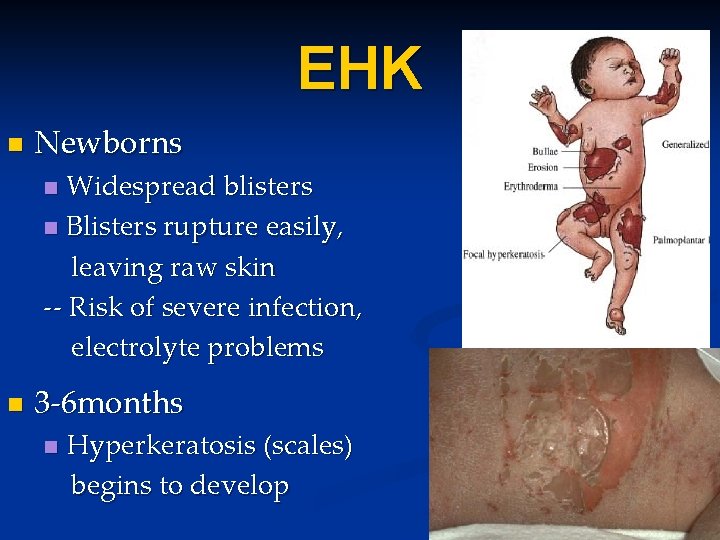
EHK n Newborns Widespread blisters n Blisters rupture easily, leaving raw skin -- Risk of severe infection, electrolyte problems n n 3 -6 months n Hyperkeratosis (scales) begins to develop
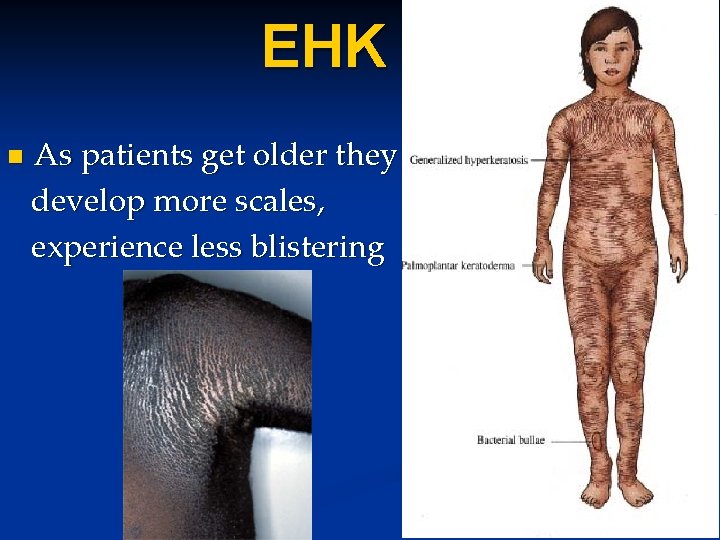
EHK n As patients get older they develop more scales, experience less blistering
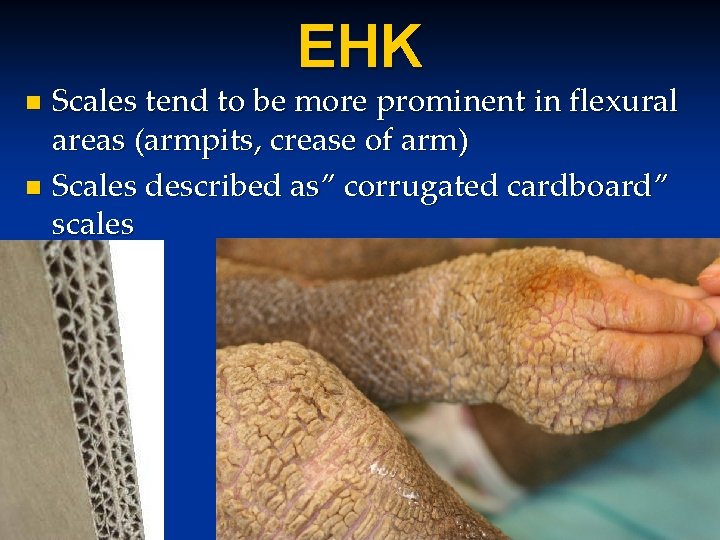
EHK Scales tend to be more prominent in flexural areas (armpits, crease of arm) n Scales described as” corrugated cardboard” scales n

EHK groups n Patients with Keratin 1 mutations n Severe palm and sole involvement • Patients with Keratin 10 mutations – Less severe palm involvement
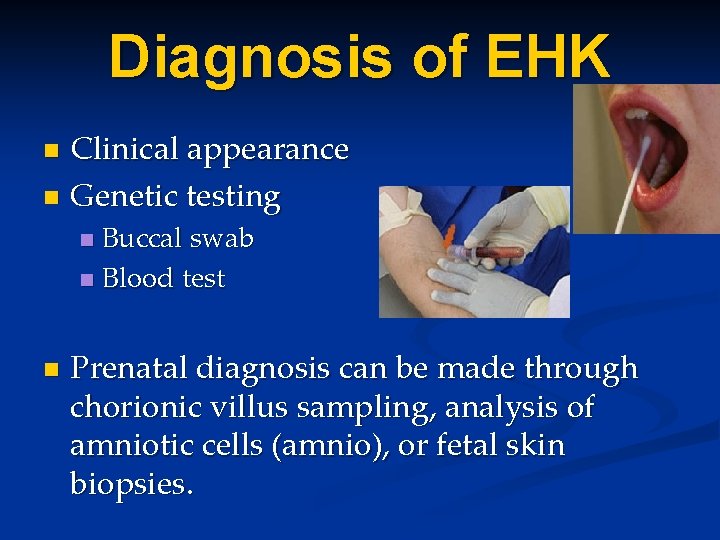
Diagnosis of EHK Clinical appearance n Genetic testing n Buccal swab n Blood test n n Prenatal diagnosis can be made through chorionic villus sampling, analysis of amniotic cells (amnio), or fetal skin biopsies.

Treatments n Treatment is a Balance act of risks and benefits n n Too much scale=decreased mobility, infection/odor Too little scale=more blistering, pain, infections
Treatments n Newborns High risk of infection n Monitor for electrolyte abnormalities/dehydration n Moisturizers n Maximize nutritional intake n n Nutritionist n Higher calorie formulas or calorie added breastmilk n Basic wound care n Moisturizers, antibiotics if indicated
Treatments n Moisturizers are mainstay of maintenance therapy n Ointments (more greasy) n Vaseline, white petroleum jelly n Aquaphor ointment n Creams (less greasy) n Cetaphil cream n Vanicream n Eucerin cream
Treatments n Moisturizers are mainstay of maintenance therapy n Oils n Baby oil, mineral oil, olive oil n Robathol bath oil n Dermasmooth oil (without steroid)
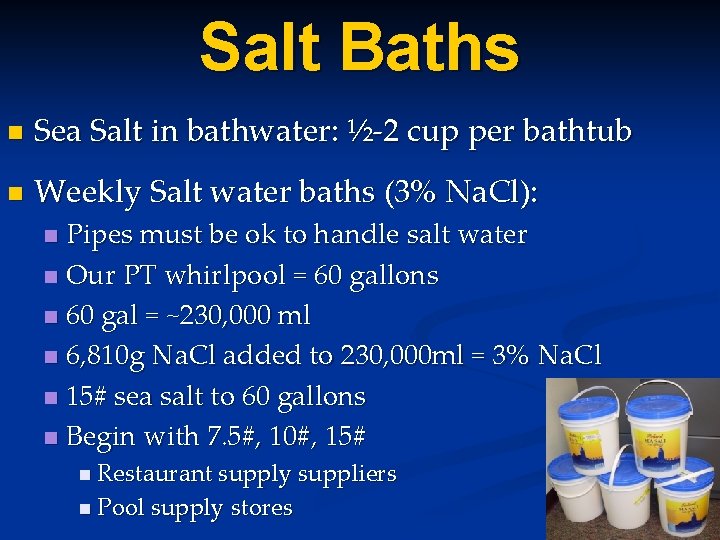
Salt Baths n Sea Salt in bathwater: ½-2 cup per bathtub n Weekly Salt water baths (3% Na. Cl): Pipes must be ok to handle salt water n Our PT whirlpool = 60 gallons n 60 gal = ~230, 000 ml n 6, 810 g Na. Cl added to 230, 000 ml = 3% Na. Cl n 15# sea salt to 60 gallons n Begin with 7. 5#, 10#, 15# n n Restaurant supply suppliers n Pool supply stores
Treatments n Topical Keratolytics (to reduce scaling in older patients) n Lactic acid containing products n Lac. Hydrin (Rx) n Am. Lactin n Ulactin n Lacticare n Eucerin plus cream n Problem: can sting and burn initially, gradually improves with continued use

Treatments n Compounded medications Medications must be mixed at the pharmacy n Can tailor ingredients based on need/patient n 10% lactic acid + 10% urea in vaseline 2 x/day n 20% lactic acid + 20% urea in vaseline 2 x/day n Severely thick palms and soles n n 50% salicylic acid + 20% urea in vaseline 1 x/day
Treatments n Topical Retinoids (“Retin A”) Typically used for acne n Cream formulation better for skin n Gel formulation better for hair bearing areas (scalp) n n Tazorac (Tazarotene) n Strong synthetic retinoid n Helps reduce scaling n Can be used around the eye to help loosen the skin around the eye to allow the eye to close shut n Pregnancy classification X n Comes in 60 g and 100 g tubes n $$$$$ very expensive
Oral “Retinoids” Accutane (isotretinoin) n Soriatane (acitretin) n Requires monitoring of bloodwork n Numerous side-effects exists n Risk vs benefits n Not for everyone n Many can tolerate this for years n Can diffusely reduce scale n
n Treatments Infections n Antibacterial soaps n Cetaphil antibacterial soap n Oilatum AD n Chlorhexidine soaps (Hibiclens) n Clorox Bleach in bathwater “Bleach Baths” n Kills bacteria on contact in a few minutes n ¼ cup per half average bathtub of water n ½ cup per full bathtub of water n 2 times/week up to daily n Generic unscented Clorox is inexpensive n Dilute bleach in spray bottle can be sprayed on in shower n Clorox Anywhere spray
Treatments n Infections n Fungal infections can occur n Wet moist areas: finger and toe web spaces, feet n White, scaly plaques n May be treated with: n n Topical antifungals: Lotrimin cream, ketoconazole cream Oral antifungal medications
Treatments n Infections n Topical antibiotics n Bacitracin, Double antibiotic ointment (Polysporin): OTC n Bactroban (mupirocin): Rx n Altabax: Rx n Oral antibiotics n Treat staph or strep infections n Recommend having your doctor obtain a skin culture (swab) to monitor for resistant bacteria
Treatments n Infections n Topical antibiotics n Bacitracin, Double antibiotic ointment (Polysporin): OTC n Bactroban (mupirocin): Rx n Altabax: Rx n Oral antibiotics n Treat staph or strep infections n Recommend having your doctor obtain a skin culture (swab) to monitor for resistant bacteria
- Slides: 25