Epidemiology of PNES CANADIAN LEAGUE AGAINST EPILEPSY MEETING









- Slides: 30

Epidemiology of PNES CANADIAN LEAGUE AGAINST EPILEPSY MEETING 2016 Jose F. Tellez Zenteno MD Ph. D, FRCP, Professor Division of Neurology, University of Saskatchewan
DISCLOSURE I have received honorariums from UCB, Sunovion and EISAI I have grants from the U of S, SHF, RUH foundation I do not have anything to disclose for this presentation

BACKGROUND • Nonepileptic seizures are episodes of seizure-like activity that are not associated with epileptiform discharges from the brain. They are considered to be a distress response. • Psychogenic nonepileptic seizures (PNES) are very common - cited as the third most frequent diagnosis in seizure clinic. [2] • One review found that of the 1% of the US population diagnosed with epilepsy, 5 -20% actually have undiagnosed PNES. [7] • Neurologists are extremely well placed to diagnose and arrange treatment for NES, however there are currently no evidence-based standard practices to guide clinicians.
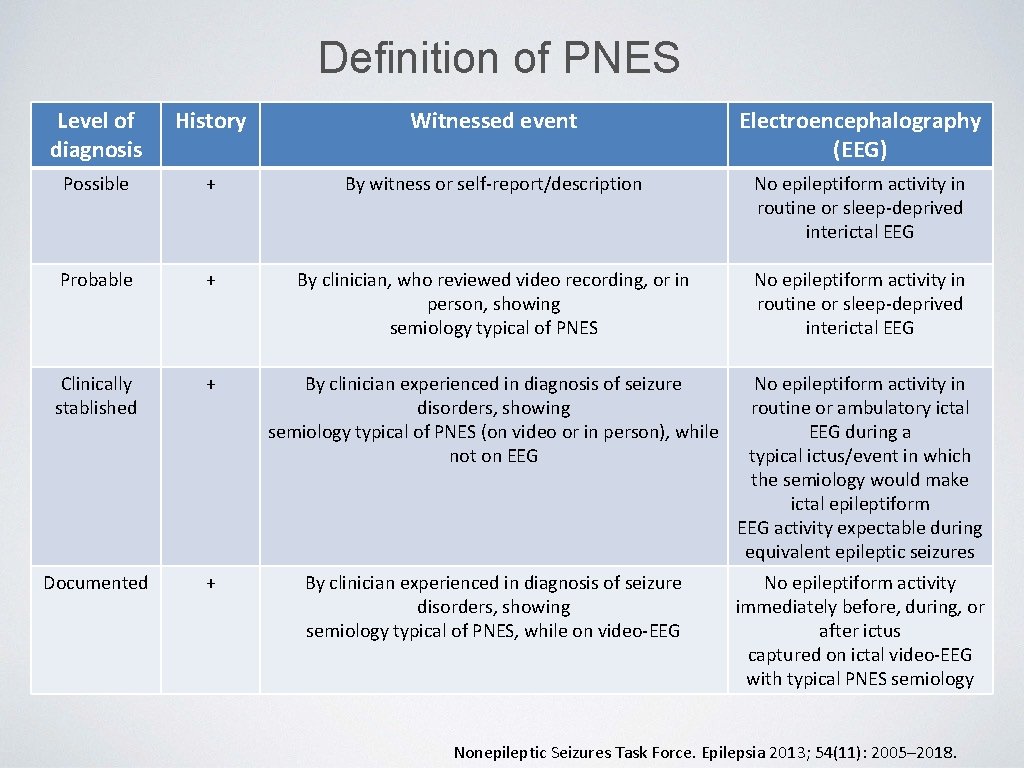
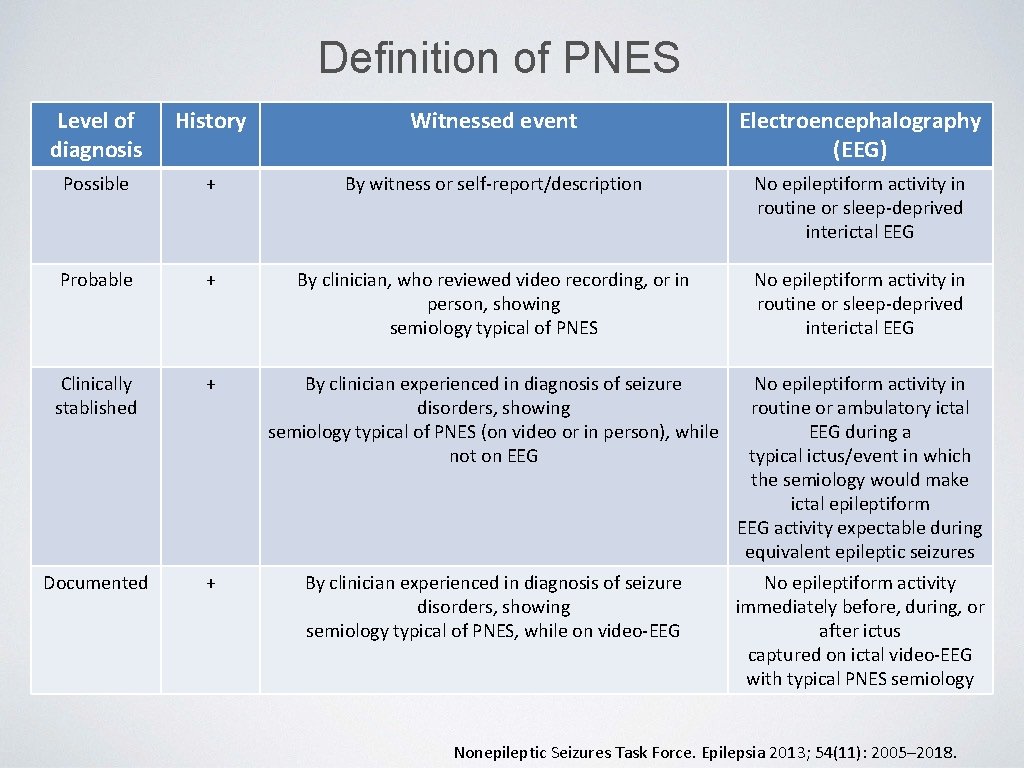
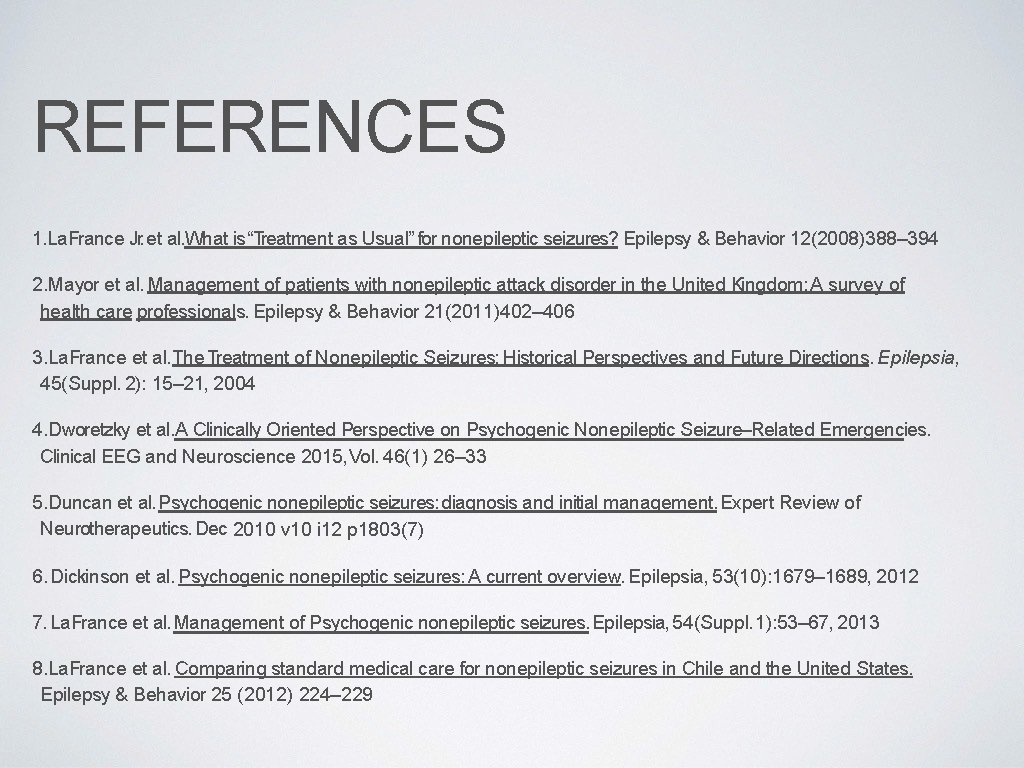
Definition of PNES Level of diagnosis History Witnessed event Electroencephalography (EEG) Possible + By witness or self-report/description No epileptiform activity in routine or sleep-deprived interictal EEG Probable + By clinician, who reviewed video recording, or in person, showing semiology typical of PNES No epileptiform activity in routine or sleep-deprived interictal EEG Clinically stablished + By clinician experienced in diagnosis of seizure disorders, showing semiology typical of PNES (on video or in person), while not on EEG No epileptiform activity in routine or ambulatory ictal EEG during a typical ictus/event in which the semiology would make ictal epileptiform EEG activity expectable during equivalent epileptic seizures Documented + By clinician experienced in diagnosis of seizure disorders, showing semiology typical of PNES, while on video-EEG No epileptiform activity immediately before, during, or after ictus captured on ictal video-EEG with typical PNES semiology Nonepileptic Seizures Task Force. Epilepsia 2013; 54(11): 2005– 2018.
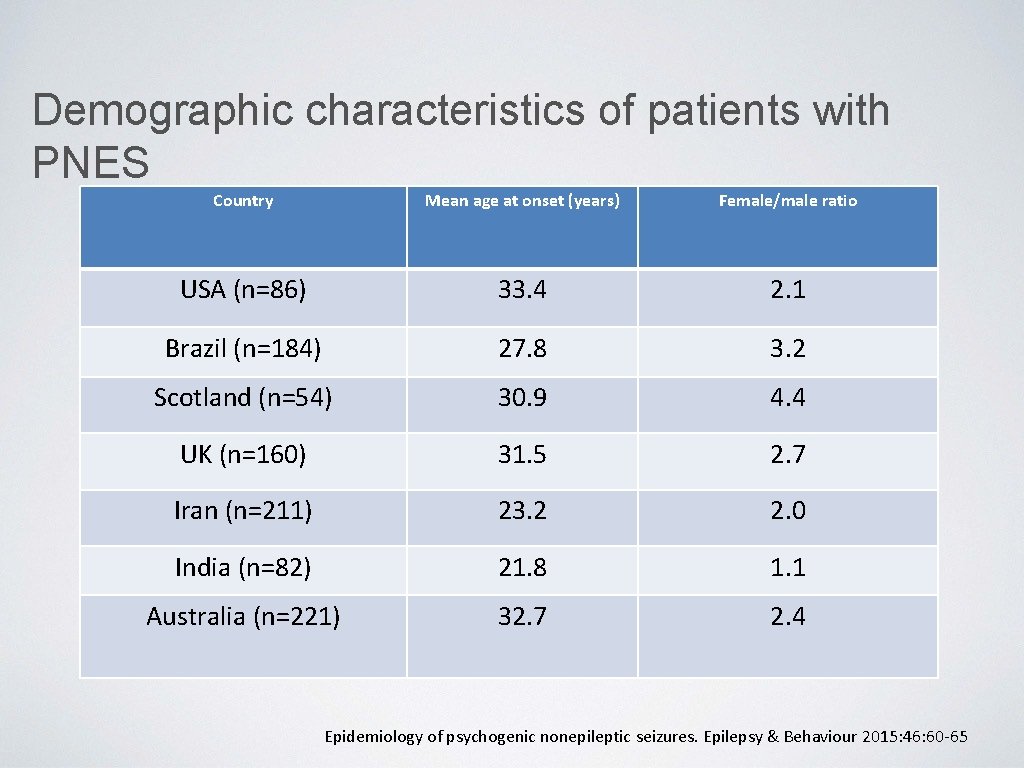
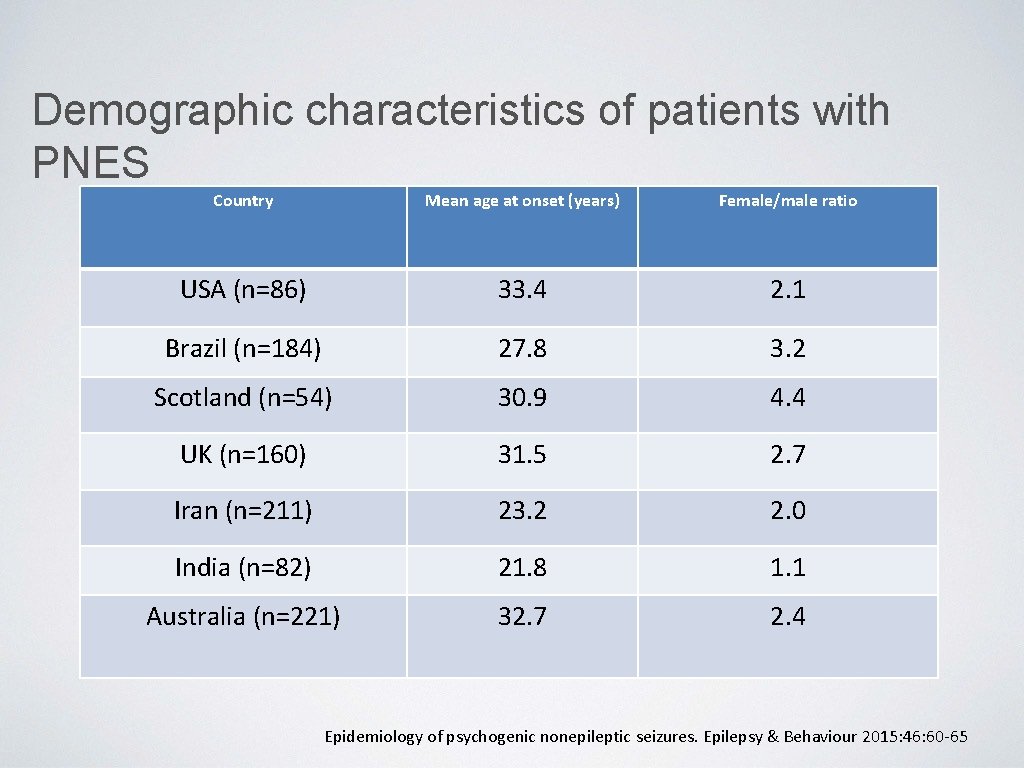
Demographic characteristics of patients with PNES Country Mean age at onset (years) Female/male ratio USA (n=86) 33. 4 2. 1 Brazil (n=184) 27. 8 3. 2 Scotland (n=54) 30. 9 4. 4 UK (n=160) 31. 5 2. 7 Iran (n=211) 23. 2 2. 0 India (n=82) 21. 8 1. 1 Australia (n=221) 32. 7 2. 4 Epidemiology of psychogenic nonepileptic seizures. Epilepsy & Behaviour 2015: 46: 60 -65
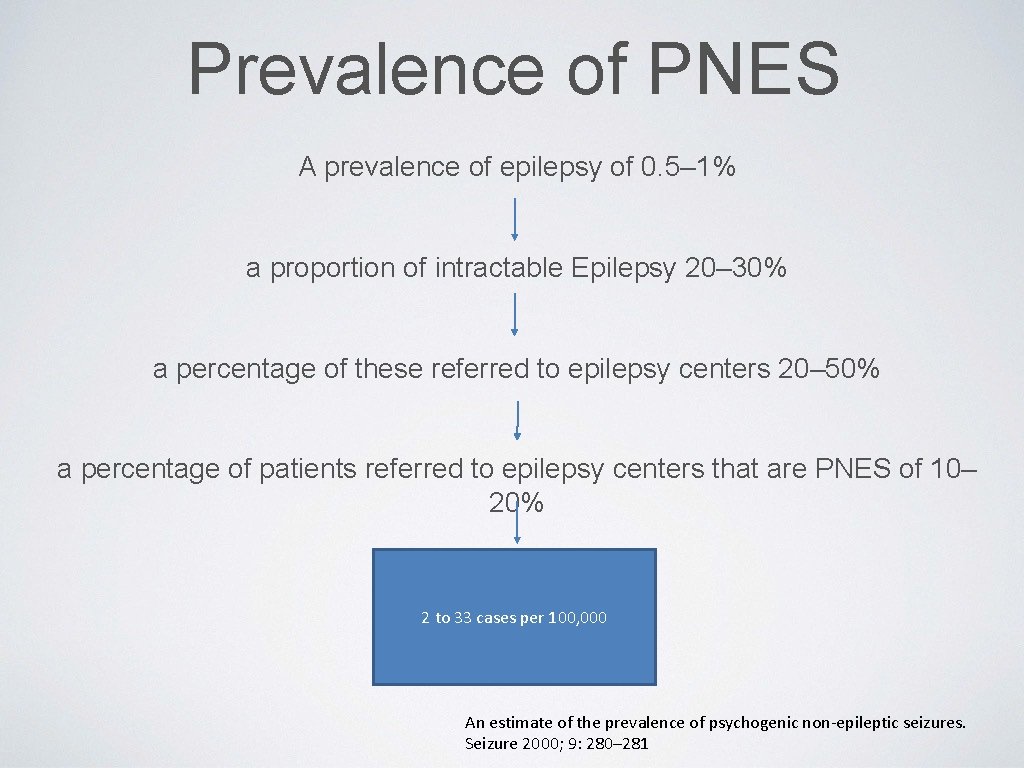
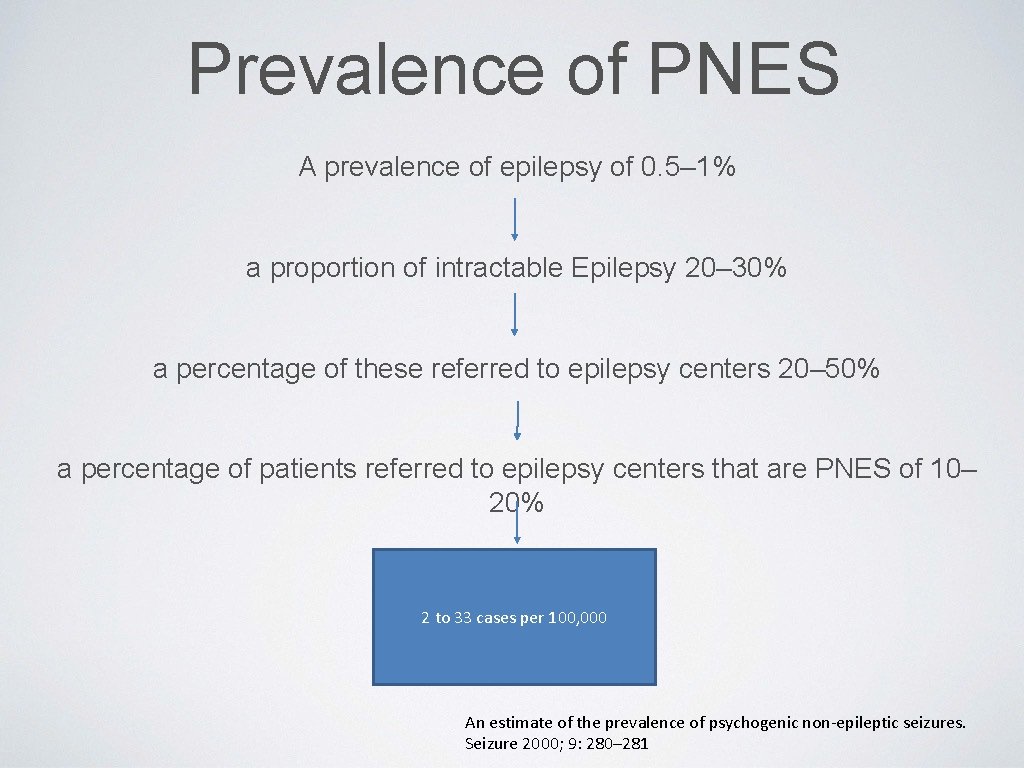
Prevalence of PNES A prevalence of epilepsy of 0. 5– 1% a proportion of intractable Epilepsy 20– 30% a percentage of these referred to epilepsy centers 20– 50% a percentage of patients referred to epilepsy centers that are PNES of 10– 20% 2 to 33 cases per 100, 000 An estimate of the prevalence of psychogenic non-epileptic seizures. Seizure 2000; 9: 280– 281
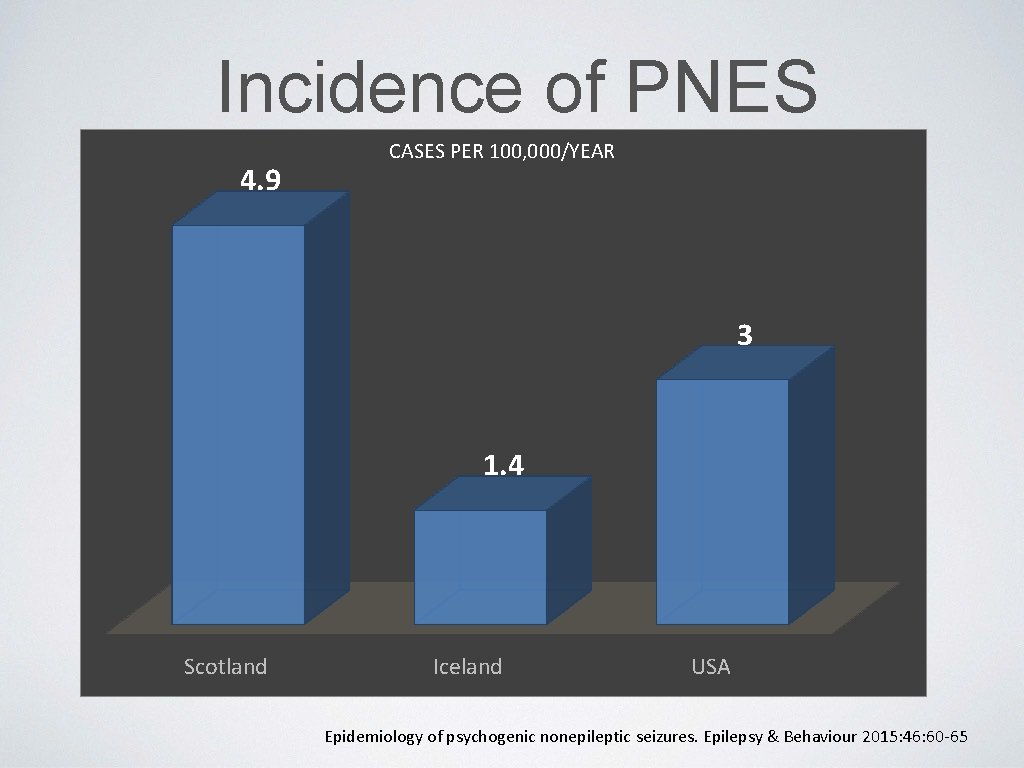
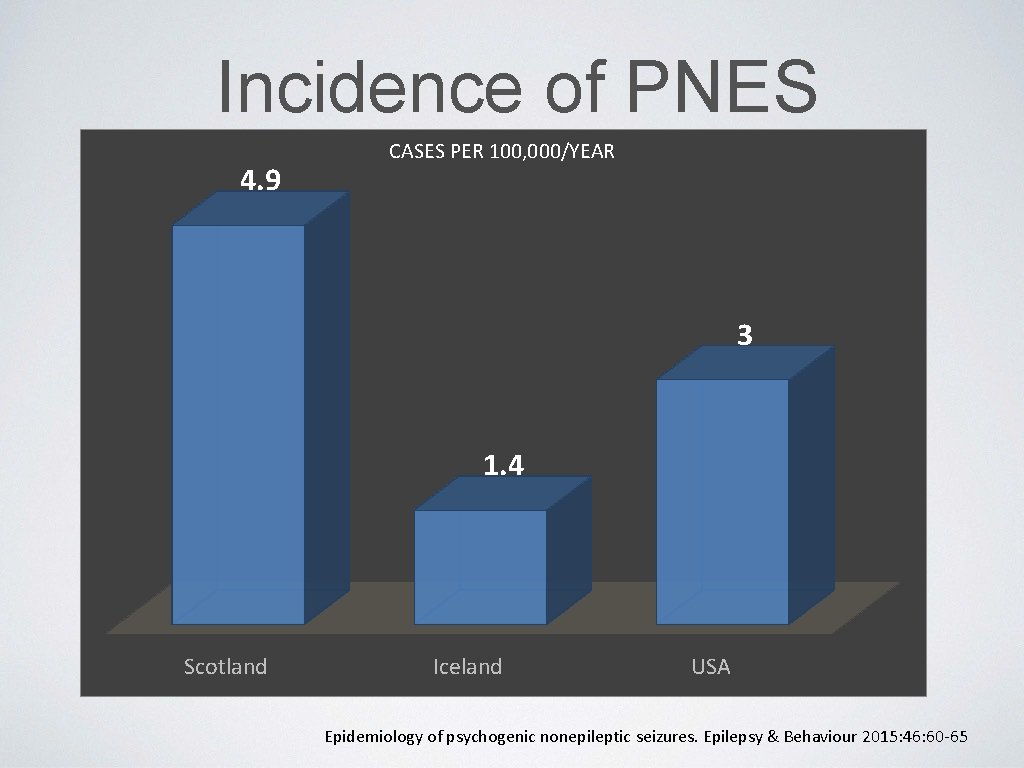
Incidence of PNES 4. 9 CASES PER 100, 000/YEAR 3 1. 4 Scotland Iceland USA Epidemiology of psychogenic nonepileptic seizures. Epilepsy & Behaviour 2015: 46: 60 -65
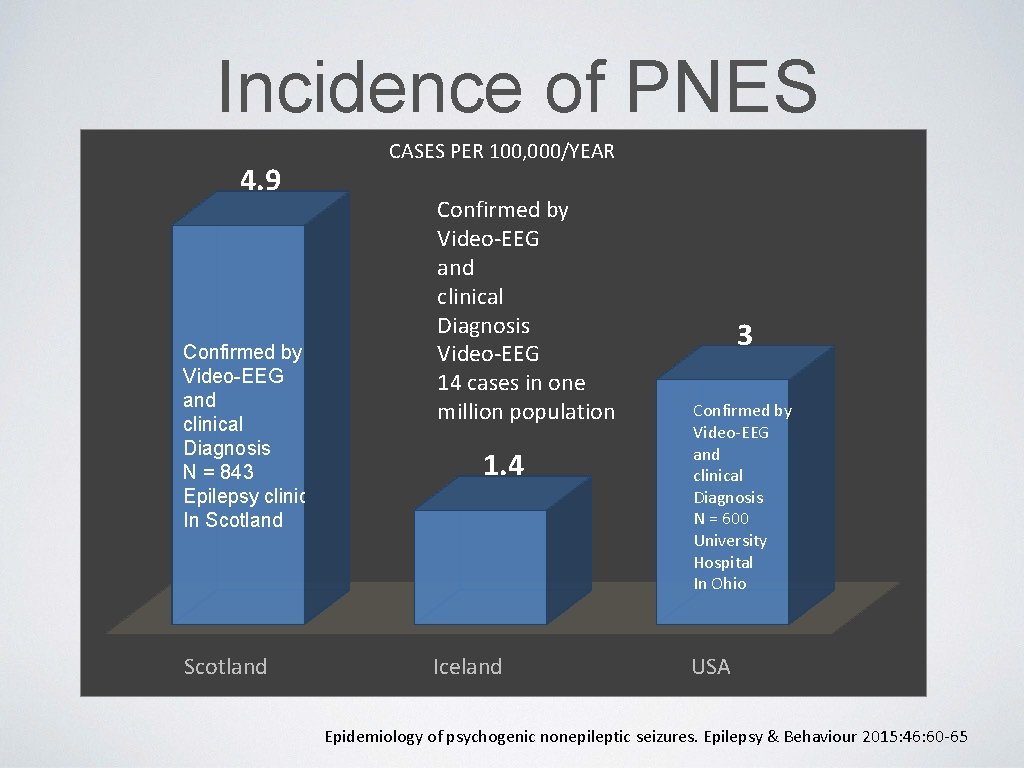
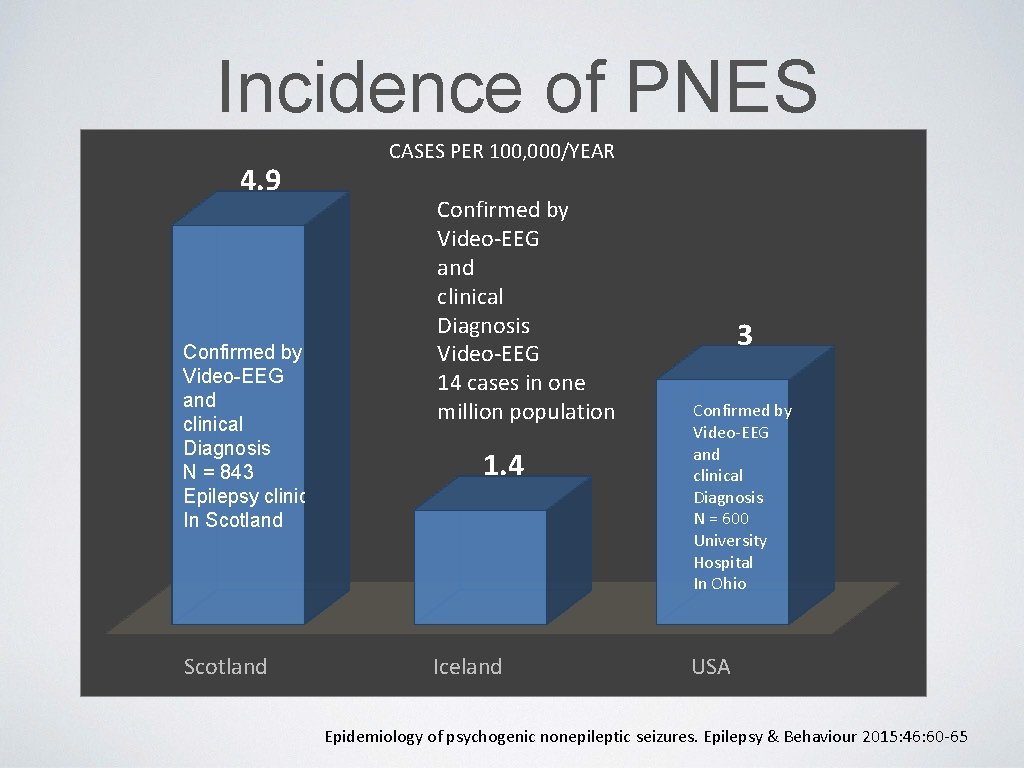
Incidence of PNES 4. 9 Confirmed by Video-EEG and clinical Diagnosis N = 843 Epilepsy clinic In Scotland CASES PER 100, 000/YEAR Confirmed by Video-EEG and clinical Diagnosis Video-EEG 14 cases in one million population 1. 4 Iceland 3 Confirmed by Video-EEG and clinical Diagnosis N = 600 University Hospital In Ohio USA Epidemiology of psychogenic nonepileptic seizures. Epilepsy & Behaviour 2015: 46: 60 -65

The most commonly reported psychogenic nonepileptic seizures associated factors Sexual Abuse 70 60 50 40 67 30 20 24 32. 5 36. 3 10 8. 1 0 Asadi-Pooya Alper Duncan Selkirk Bowman
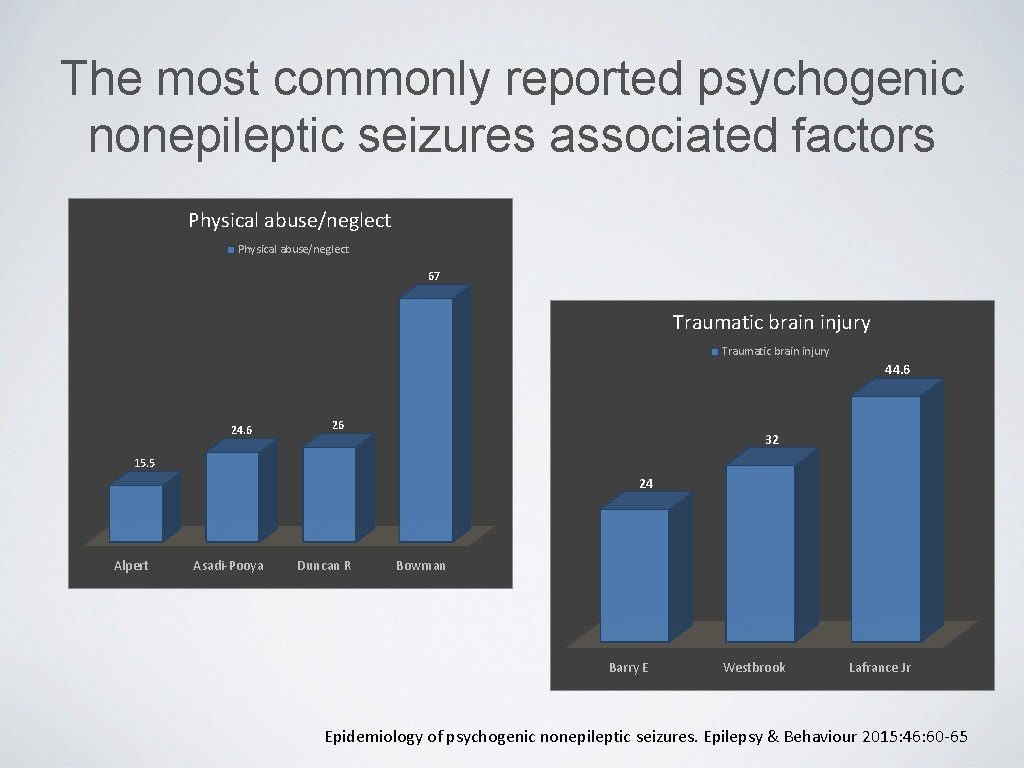
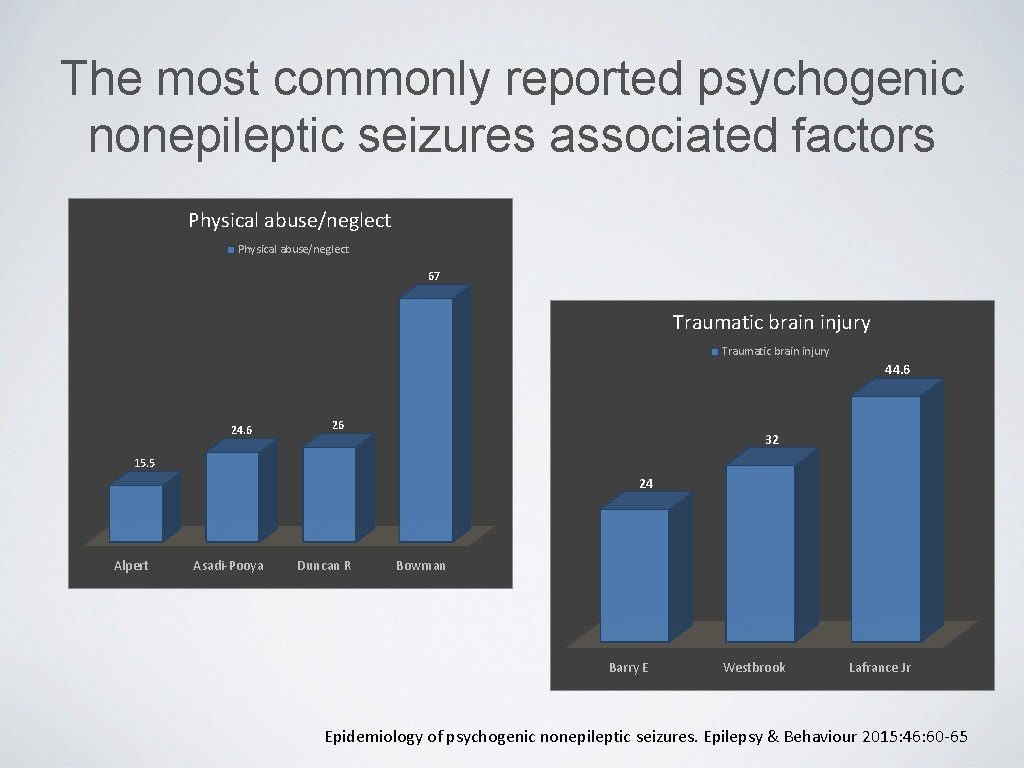
The most commonly reported psychogenic nonepileptic seizures associated factors Physical abuse/neglect 67 Traumatic brain injury 44. 6 26 32 15. 5 24 Alpert Asadi-Pooya Duncan R Bowman Barry E Westbrook Lafrance Jr Epidemiology of psychogenic nonepileptic seizures. Epilepsy & Behaviour 2015: 46: 60 -65
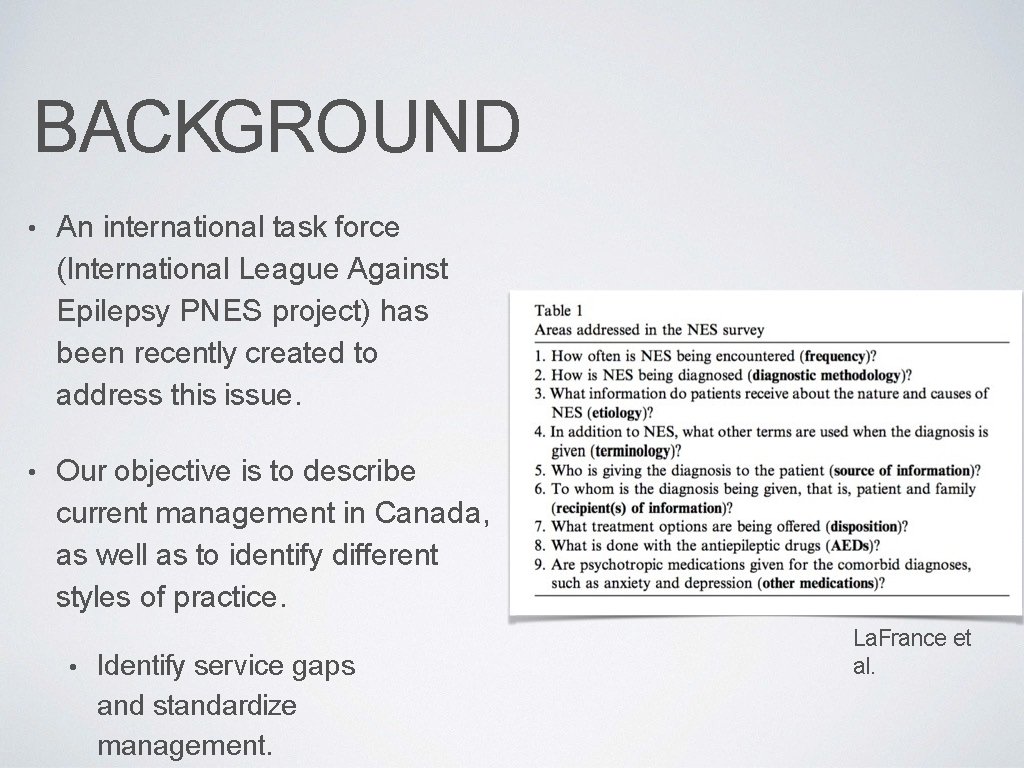
BACKGROUND • An international task force (International League Against Epilepsy PNES project) has been recently created to address this issue. • Our objective is to describe current management in Canada, as well as to identify different styles of practice. • Identify service gaps and standardize management. La. France et al.
METHODS • The Canadian League Against Epilepsy (CLAE) has 131 members, comprised of adult and pediatric neurologists, epileptologists, psychiatrists, psychologists, neurosurgeons, nurses, EEG technologists etc. • 35 question survey was sent, via email, to the members of the CLAE. • Questions are designed to assess diagnosis and treatment practices for PNES, including methodology, etiology, frequency encountered, communication practices, disposition and follow-up. • The response format was categorical for close-ended questions (multiple choice format) and “check what applies” format for lists.
METHODS • This survey was designed with the intent of quantifying common practices regarding nonepileptic seizures in Canada. • The questions were designed after literature review and discussion with Dr. Markus Reuber, lead author of the ILAE PNES project. • This survey is validated in the UK and has been applied in different international populations, including the UK, US and Chile. [2, 1, 8]

t pilt. JSY M l. i. Y'lof 21 (2011) 402 400 Epilepsy 8 i Behavior Journ al h o m e p • g e : w w w. el aev ler. c o m/ loce te /y e b e h Managemen t of patients with nonepileptic attack disorder in the United Kingdom: A survey of health care professionals Rebec. C<I Mayor "*, Phil E. Smith b, Markus Reuber • • . . -. . . . _. . . Ulll. LWw 1 • t 1, . . _ Sfld. Wt I. II' • LW 111 l 1'0. . . . ff/ W * C. . . LC . Epi lepsy a; hfarv 1 or • LX Science. Direct • IJ '>I Vll R What is "treatment as usual" for nonepileptic seizu res? W. Curt La. France Jr. • · , Mark D. Rusch b , Jason T. Machan • • /Ht"' • fl/ /ton; n'l'f)'f lt iatrf u"41 lklut 1 ton» l. , , o. Jov, . / ( rltnult l, /lilql. J , . . , , . . . , O. , . t iu. . . i, , 11 ' - ' l/osplto/, , _ , / r. Jlnl. 1£ 1 1. ( , . _. , , , _ l l. A ' p/. , tll' , o; , , 7. , Alt. Ji<al Co l k , t. j II r. . k Milo. t t t MI L l. A • NJ. . . 1 atu 1 i. u. /. w. J Jlt. Ulllui. L P , . . dn. , , V 111 fl/ Mil l'11, , _ , , l, Epilepsy 8 i Behavior. _. . , : 11: . R 1 ourn • I ho m e pag e w w w. Csev 11 r c o m , 1 o c a t e fy e b e h Comparing standard medical care for nonepileptic seizures in Chile and the United States W. Curt Lafr. . ice Jr. . . <. $. Alejandro J. de M<l. r inis d. . <, Anne Frank Webb • . jasoo T. Mark D. Rusch • . Andres M. K. lnoer h . '
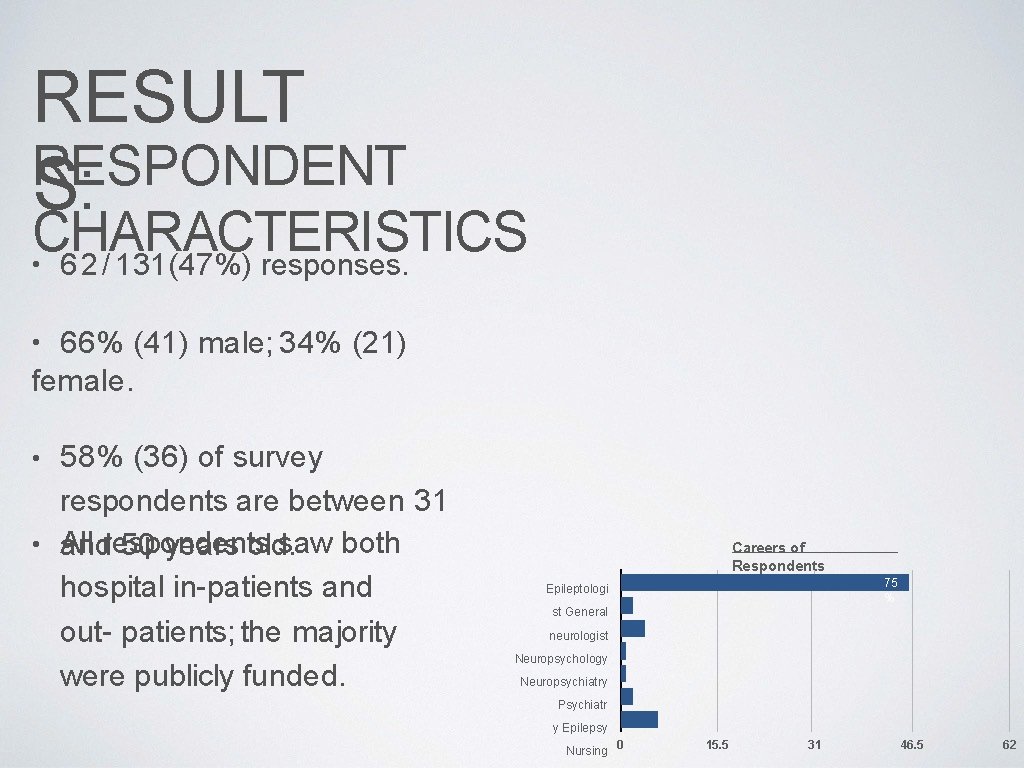
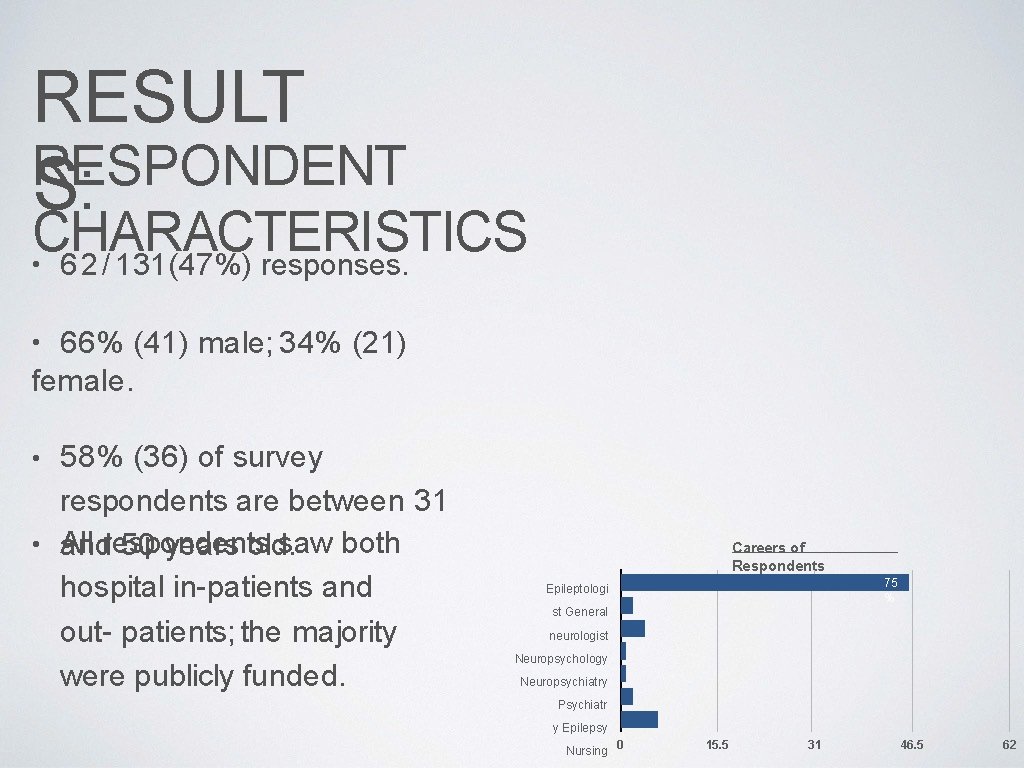
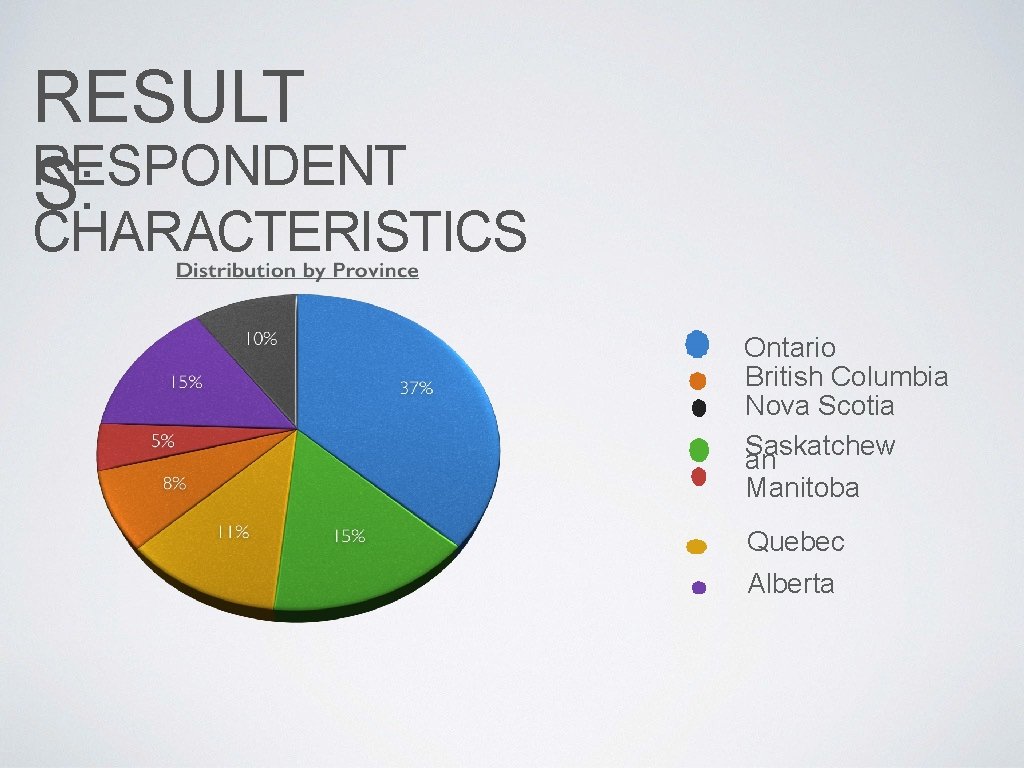
RESULT RESPONDENT S: CHARACTERISTICS • 6 2 / 131(47%) responses. 66% (41) male; 34% (21) female. • • 58% (36) of survey respondents are between 31 • All saw both andrespondents 50 years old. hospital in-patients and out- patients; the majority were publicly funded. Careers of Respondents 75 % Epileptologi st General neurologist Neuropsychology Neuropsychiatry Psychiatr y Epilepsy Nursing 0 15. 5 31 46. 5 62
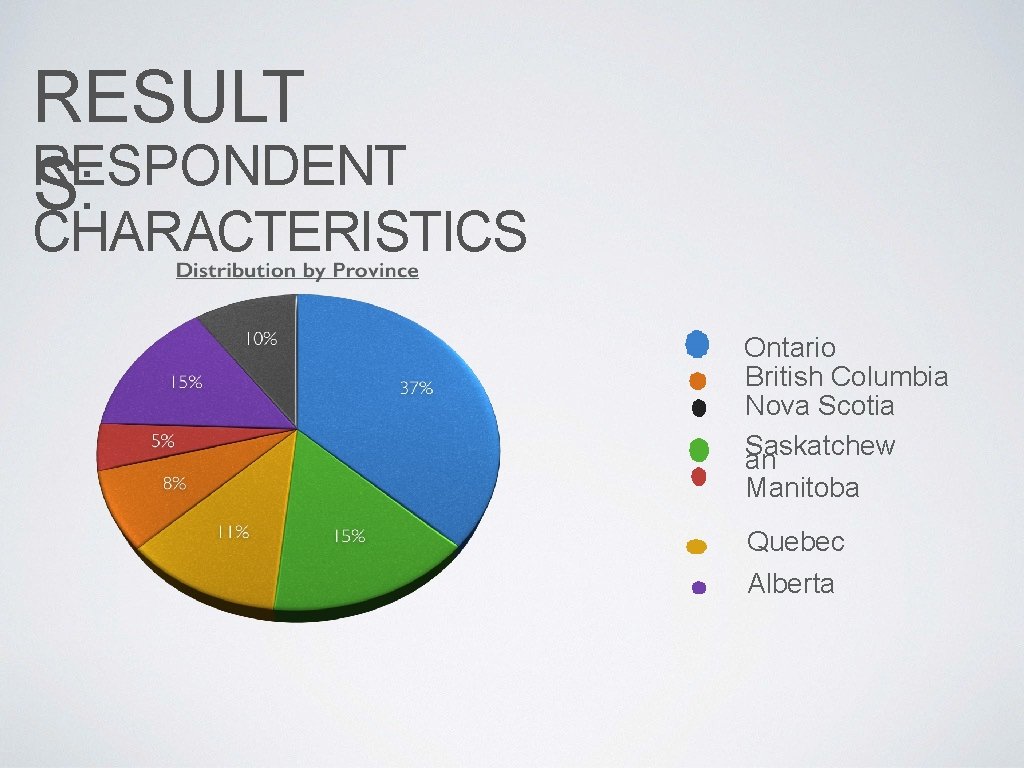
RESULT RESPONDENT S: CHARACTERISTICS Ontario British Columbia Nova Scotia Saskatchew an Manitoba Quebec Alberta
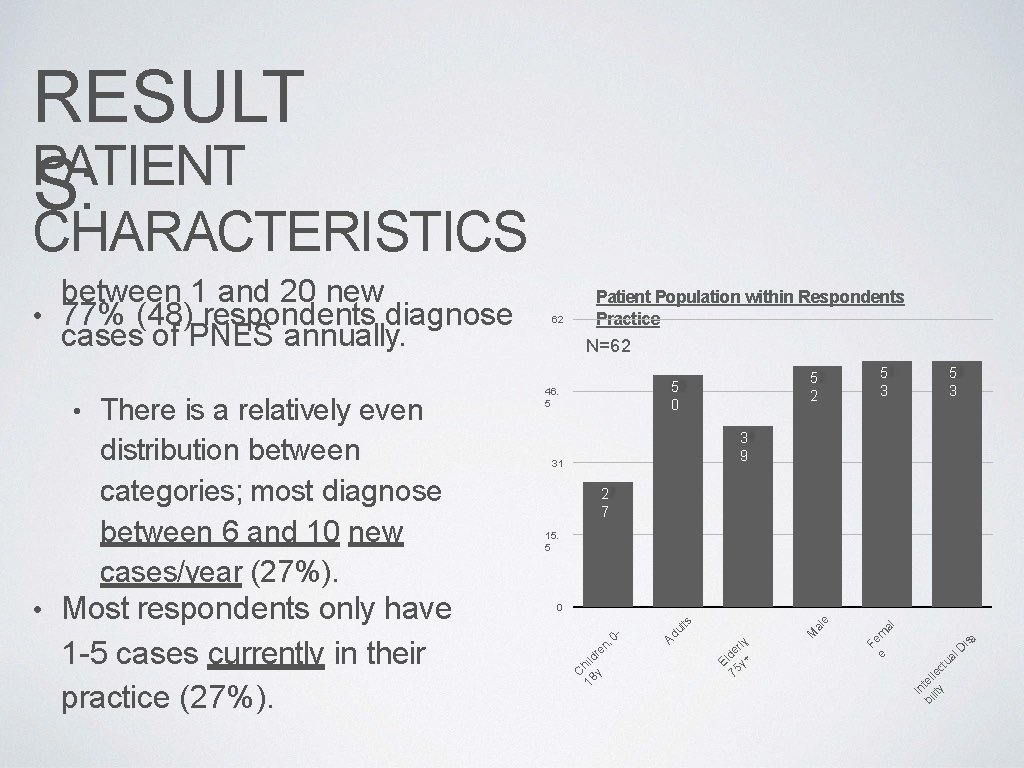
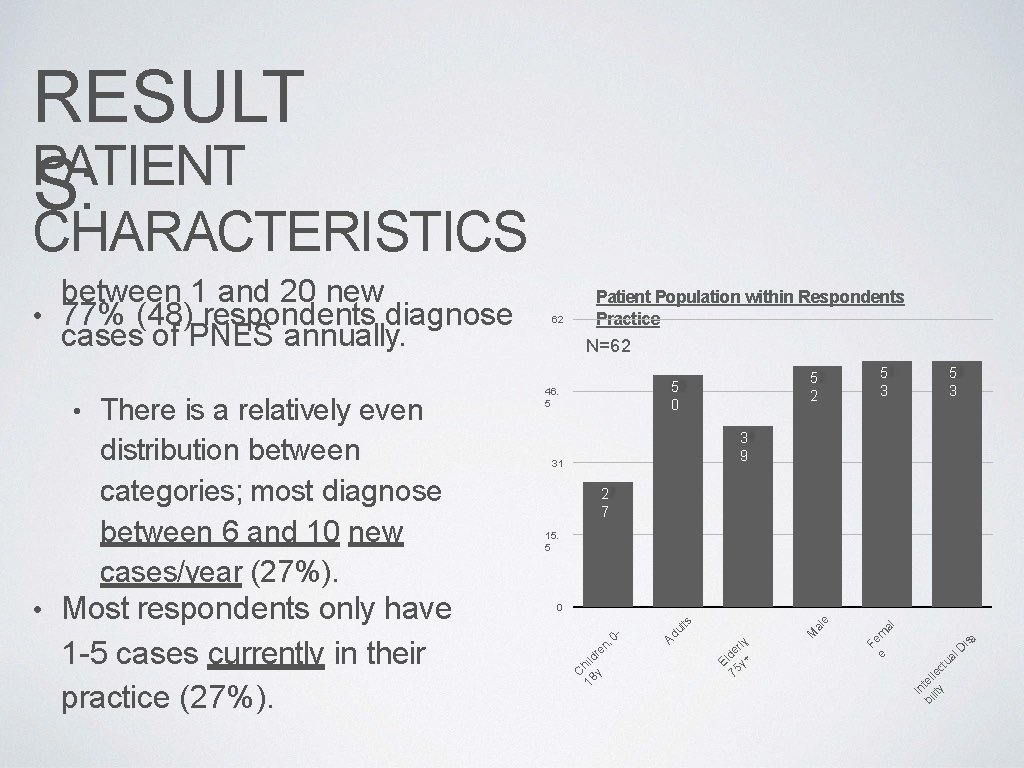
RESULT PATIENT S: CHARACTERISTICS 5 3 3 9 31 2 7 15. 5 D is In bi tell lity ec tu al , F e em al 0 M al e Most respondents only have 1 -5 cases currently in their practice (27%). 46. 5 E 75 lde y+ rly • 5 2 5 0 Ad ul ts distribution between categories; most diagnose between 6 and 10 new cases/year (27%). N=62 0 - • There is a relatively even 62 Patient Population within Respondents Practice C 18 hild y re n, between 1 and 20 new • 77% (48) respondents diagnose cases of PNES annually. a
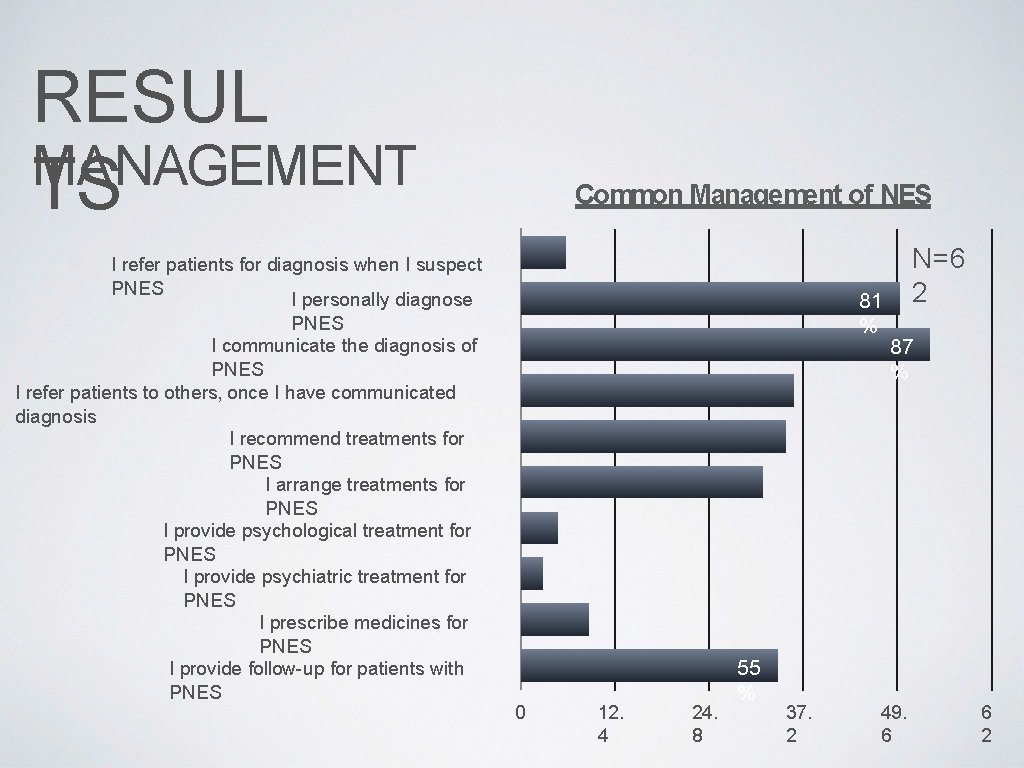
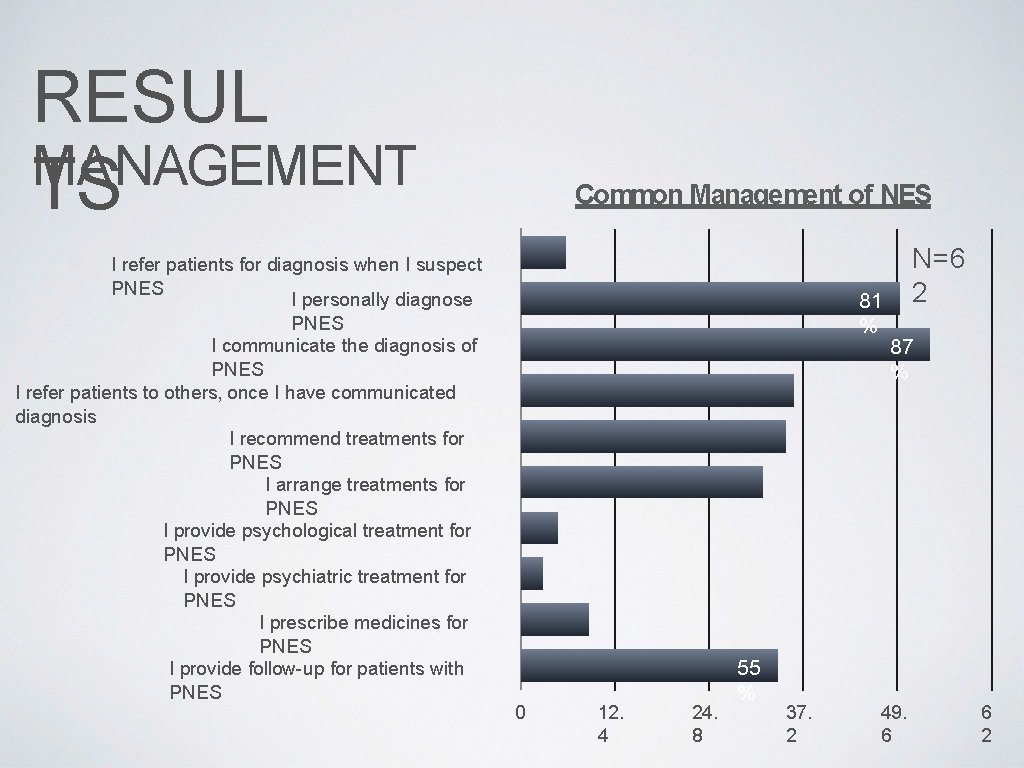
RESUL MANAGEMENT TS I refer patients for diagnosis when I suspect PNES I personally diagnose PNES I communicate the diagnosis of PNES I refer patients to others, once I have communicated diagnosis I recommend treatments for PNES I arrange treatments for PNES I provide psychological treatment for PNES I provide psychiatric treatment for PNES I prescribe medicines for PNES I provide follow-up for patients with PNES Common Management of NES 81 % 0 12. 4 24. 8 55 % 37. 2 N=6 2 87 % 49. 6 6 2
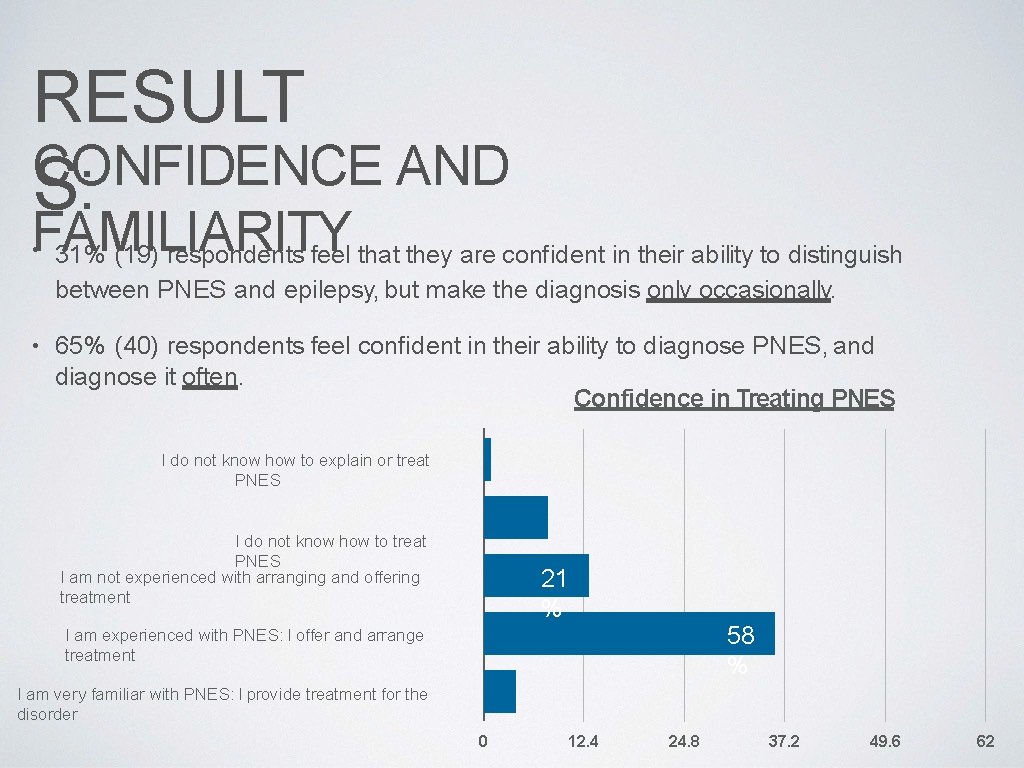
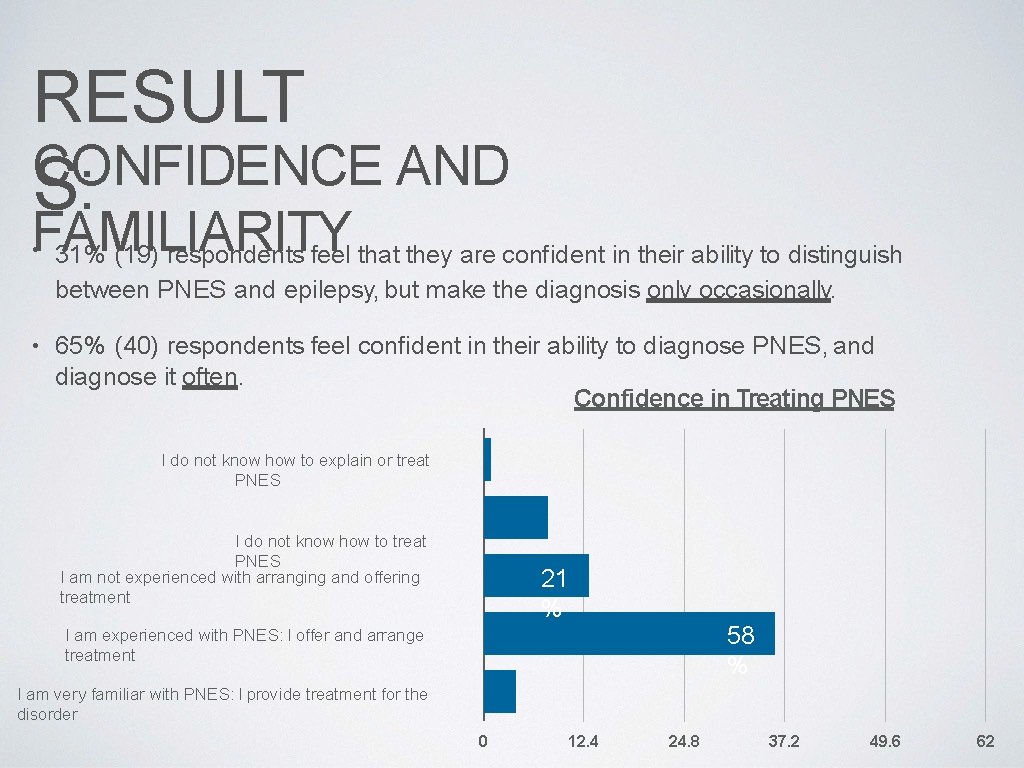
RESULT CONFIDENCE AND S: FAMILIARITY 31% (19) respondents feel that they are confident in their ability to distinguish • between PNES and epilepsy, but make the diagnosis only occasionally. • 65% (40) respondents feel confident in their ability to diagnose PNES, and diagnose it often. Confidence in Treating PNES I do not know how to explain or treat PNES I do not know how to treat PNES I am not experienced with arranging and offering treatment 21 % 58 % I am experienced with PNES: I offer and arrange treatment I am very familiar with PNES: I provide treatment for the disorder 0 12. 4 24. 8 37. 2 49. 6 62

RESUL RISK FACTORS FOR NONEPILEPTIC TS SEIZURES • Respondents scored all etiological factors as relatively low relevance (<30%). • Respondents felt that the most relevant factors in the future development of PNES in an individual are childhood neglect and abuse, followed by co-morbid psychiatric conditions, such as anxiety and depression. Reported Significant Factors for PNES Highly Relevan t (>70%) Childhood emotional/ physical neglect Childhood emotional/ physical abuse Childhood sexual abuse Epileps y Anxiety Depressio n Accumulated life stress Moderate Relevanc e (4060%) Low Relevanc e (<30%) 23 % 31 % 40 % 34 % 21 % 37 % 15 % 11 % 18 % 16 % 18 % 29 % 23 % 39 % 35 % 32 % 60 % 21 % 40 % 35 %
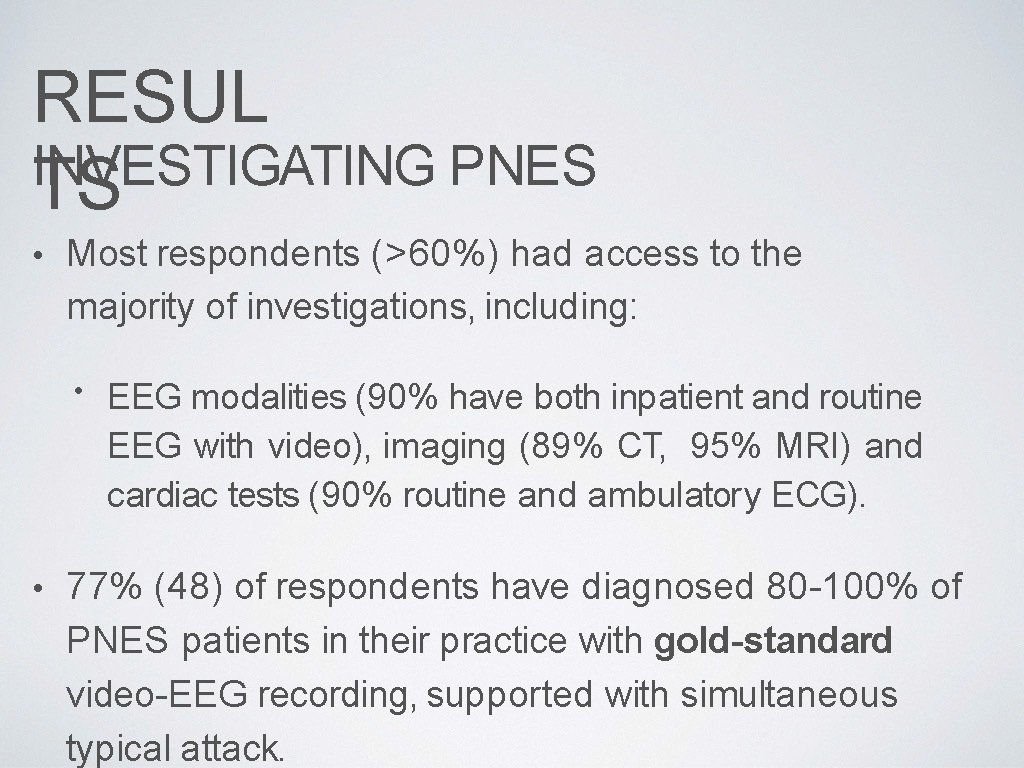
RESUL INVESTIGATING PNES TS • Most respondents (>60%) had access to the majority of investigations, including: • • EEG modalities (90% have both inpatient and routine EEG with video), imaging (89% CT, 95% MRI) and cardiac tests (90% routine and ambulatory ECG). 77% (48) of respondents have diagnosed 80 -100% of PNES patients in their practice with gold-standard video-EEG recording, supported with simultaneous typical attack.
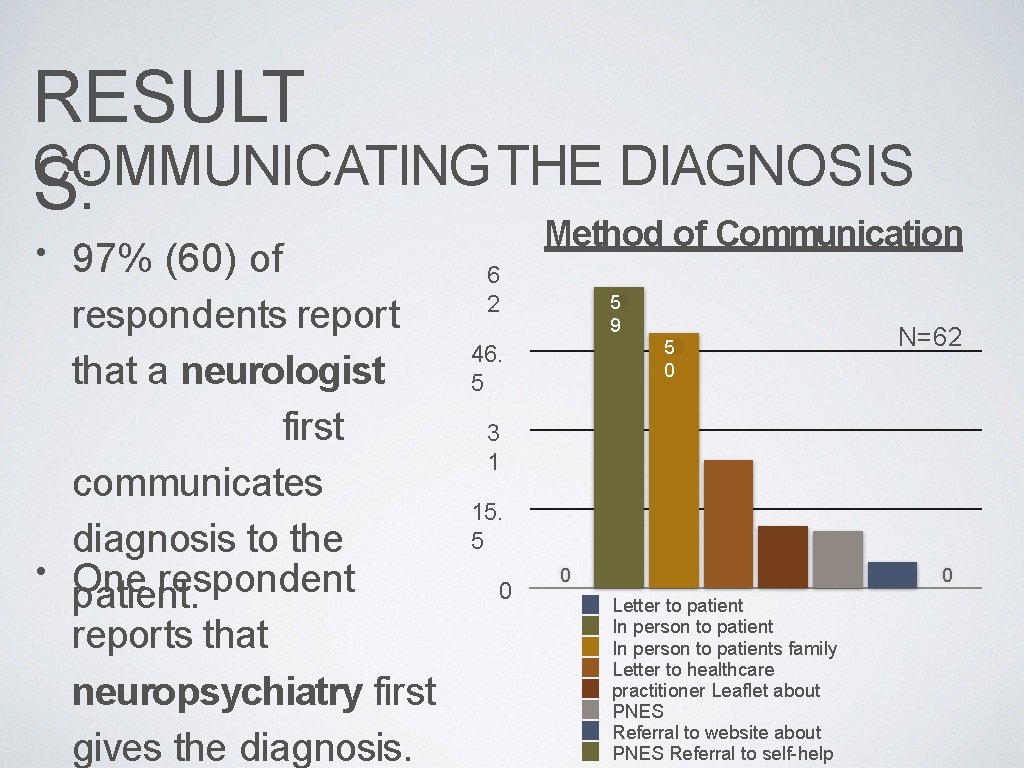
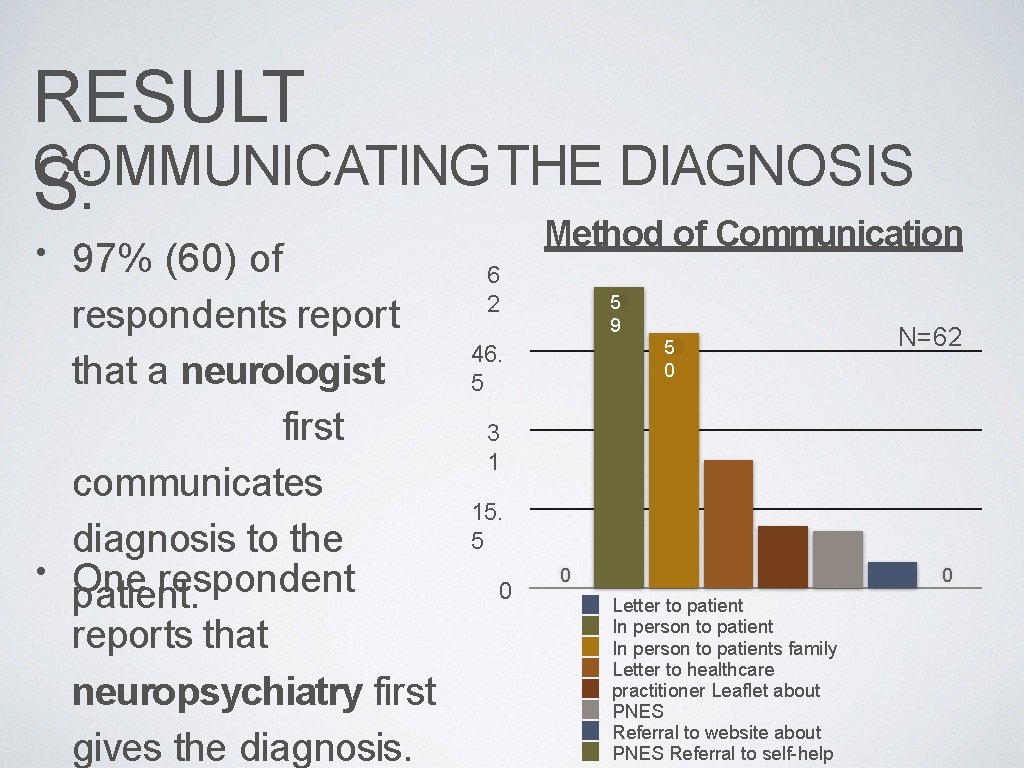
RESULT COMMUNICATING THE DIAGNOSIS S: • 97% (60) of respondents report that a neurologist first communicates diagnosis to the • One respondent patient. reports that neuropsychiatry first gives the diagnosis. Method of Communication 6 2 5 9 5 0 46. 5 N=62 3 1 15. 5 0 0 0 Letter to patient In person to patients family Letter to healthcare practitioner Leaflet about PNES Referral to website about PNES Referral to self-help

RESUL COMMUNICATING THE TS DIAGNOSIS 16 different statements explaining NES • were provided to the respondents, who were invited to select all that were applicable to their usual practice. • These six most commonly diagnosis to the patient. statements used are to reportedly communicate the N=62 The events are a response to stress The events may be a sign of suppressed traumas from the past or ongoing conflicts The causes of PNES are complicated and that there may be predisposing factors The events are not a form of epilepsy and do not cause any lasting damage The person is not deliberately producing those events Antiepileptic drugs do not work for PNES

RESULT FOLLOW UP AFTER THE DIAGNOSIS S: • 60% (37) of respondents offer patients at least one follow- up appointment after the diagnosis is initially explained. • Most (79%) provide follow-up to those patients with concomitant epilepsy, but otherwise follow-up rates are low. • 84% of respondents feel that individualized psychological therapy, (i. e. CBT) is the most
DISCUSSION • Our response rate was significantly higher than those of the UK study (8. 6%) [2], or of the American study (18%) [1]. • We observed a good distribution of responses across Canada from Nova Scotia to BC. • We observed a relatively even distribution of factors contributing to onset and maintenance of PNES, which is supported by the literature: PNES is a heterogenous disorder with multifactorial etiology. • Psychiatric co-morbidities are the rule and not the exception in PNES.
DISCUSSION • Follow-up and psychiatric treatment: many studies have found that once the diagnosis is made, patients are discharged from the neurological service without appropriate psychiatric referral in place. • This may lead to “bounce-back” and repeated ER visits: Potential for adverse events with inappropriate use of AEDs. • Inappropriate allocation of resources. • • One expert suggests that neurologists should continue to provide follow up for at least 6 months following diagnosis, to ensure successful transition of patient care to another

CONCLUSIONS • Comparisons with the UK and USA studies yielded several interesting observations: [2, 1] • Most patients are diagnosed with gold-standard investigations in all three countries. • Neurology communicates the diagnosis first, and it is explained similarly. • Canada and the UK reported low follow-up rates (50 -60%), as well as low referral rates to psychology and psychiatry (~35% UK, ~51% Canada). • The USA study reported that most neurologists routinely provide follow-up after the diagnosis (70%). As well, most refer to psychiatry

FUTURE DIRECTIONS • We hope to use this data to help establish guidelines for the diagnosis and management of psychogenic NES. • • The goal is to increase standardization of practice across the country, in order to provide the best care for these patients. Recently, randomized control trials are exploring best practices for PNES: we hope to contribute Canadian data to these trials.
REFERENCES 1. La. France Jr. et al. What is “Treatment as Usual” for nonepileptic seizures? Epilepsy & Behavior 12(2008)388– 394 2. Mayor et al. Management of patients with nonepileptic attack disorder in the United Kingdom: A survey of health care professionals. Epilepsy & Behavior 21(2011)402– 406 3. La. France et al. The Treatment of Nonepileptic Seizures: Historical Perspectives and Future Directions. Epilepsia, 45(Suppl. 2): 15– 21, 2004 4. Dworetzky et al. A Clinically Oriented Perspective on Psychogenic Nonepileptic Seizure–Related Emergencies. Clinical EEG and Neuroscience 2015, Vol. 46(1) 26– 33 5. Duncan et al. Psychogenic nonepileptic seizures: diagnosis and initial management. Expert Review of Neurotherapeutics. Dec 2010 v 10 i 12 p 1803(7) 6. Dickinson et al. Psychogenic nonepileptic seizures: A current over view. Epilepsia, 53(10): 1679– 1689, 2012 7. La. France et al. Management of Psychogenic nonepileptic seizures. Epilepsia, 54(Suppl. 1): 53– 67, 2013 8. La. France et al. Comparing standard medical care for nonepileptic seizures in Chile and the United States. Epilepsy & Behavior 25 (2012) 224– 229
Epileptologists Salah Almubarak Jose Tellez-Zenteno Gary Hunter Surgeons Adam Wu Alex Vitali EEG techs Dianne Dash Chelsea Dash Sara Crawford Sara Primrose Kyla K Tabrez Hussein Theresa Harder Dough Isely Liana Regehr Research coordinator Lizbeth Hernandez Nurse Karen Watherhouse Administrative support Janice Morelli Clarissa Penner f. MRI Marla M. Ron B. Neuropshicologist Mirna Vrbancic Psychiatgris Huma Aftab
 Canadian league against epilepsy
Canadian league against epilepsy Lorna myers pnes
Lorna myers pnes Canadian premier softball cricket league
Canadian premier softball cricket league American epilepsy society annual meeting 2017
American epilepsy society annual meeting 2017 What is meeting and types of meeting
What is meeting and types of meeting Today meeting or today's meeting
Today meeting or today's meeting Proposal kickoff meeting agenda
Proposal kickoff meeting agenda What is meeting and types of meeting
What is meeting and types of meeting Epidemiology person place time
Epidemiology person place time Formula for attack rate
Formula for attack rate Seven uses of epidemiology
Seven uses of epidemiology Difference between descriptive and analytic epidemiology
Difference between descriptive and analytic epidemiology Distribution in epidemiology
Distribution in epidemiology What is descriptive study in epidemiology
What is descriptive study in epidemiology Causal vs association
Causal vs association How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology Prevalence calculation
Prevalence calculation Defination of incidence
Defination of incidence Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Epidemiology triad
Epidemiology triad Ramboman analysis
Ramboman analysis Spurious association in epidemiology
Spurious association in epidemiology Perbedaan odds ratio dan prevalence ratio
Perbedaan odds ratio dan prevalence ratio Cbic recertification
Cbic recertification Formula for attack rate
Formula for attack rate Epi
Epi Descriptive vs analytic epidemiology examples
Descriptive vs analytic epidemiology examples Distribution in epidemiology
Distribution in epidemiology Defination of epidemiology
Defination of epidemiology