EPDM 566 Congestive Heart Failure Synnove F Knutsen










- Slides: 56

EPDM 566 Congestive Heart Failure Synnove F. Knutsen, MD, MPH, Ph. D Modified from presentation by Jennifer Kwon, MPH, Dr. PH

Heart failure (HF): • Chronic and long-term condition • Usually secondary to another condition that has damaged or weakened the heart (MI, hypertension, etc) • The heart is not able to adequately pump blood throughout the body to meet its need for oxygen and nutrients
Heart failure (HF), cont. • Ventricles become stiff and fail to fill between beats • Ventricles dilate until the heart is unable to pump blood efficiently • Liver, abdomen, arms, legs, lungs become congested with fluid

Heart failure: classifications • Left-sided HF – Most common – Fluid builds up in lungs shortness of breath – Right-sided HF (cor pulmonale) • Often occurs together with left-sided HF • Due to pulmonary hypertension • Edema in lower extremities, ascites (fluid in the abdomen)
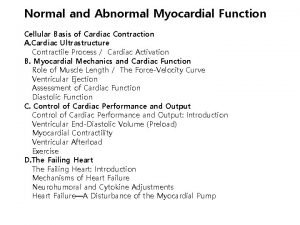
Heart failure: classifications • Systolic HF – Left ventricle unable to contract vigorously – Ejection fraction (EF) < 40% • Diastolic HF – Left ventricle unable to fill fully – Impedes blood flow into heart, backup in the lungs – Contraction may be normal (EF >40%) » 20 -50% of HF patients have preserved systolic function » Not studied as well as systolic HF
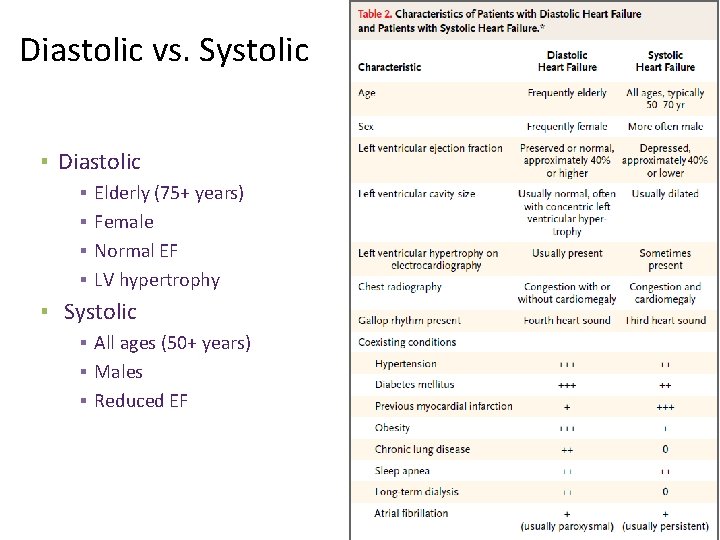
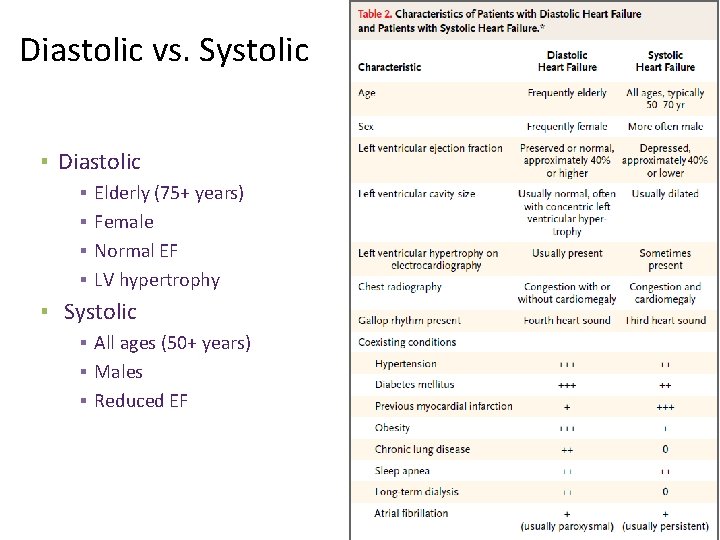
Diastolic vs. Systolic ▪ Diastolic ▪ ▪ Elderly (75+ years) Female Normal EF LV hypertrophy ▪ Systolic ▪ All ages (50+ years) ▪ Males ▪ Reduced EF
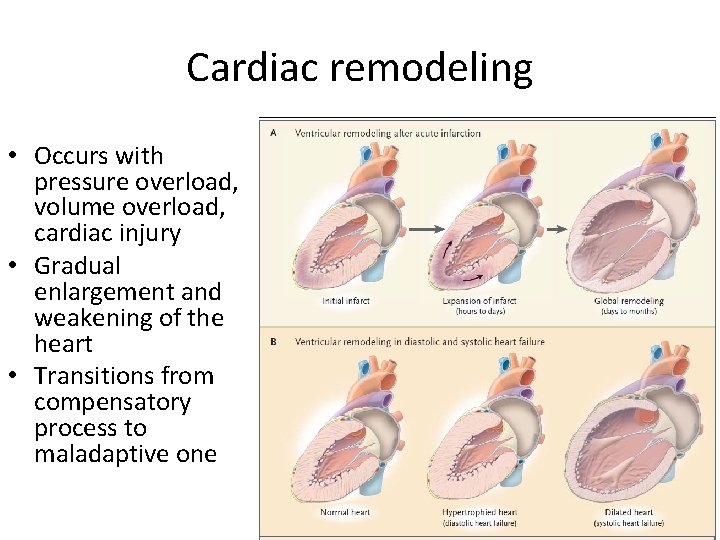
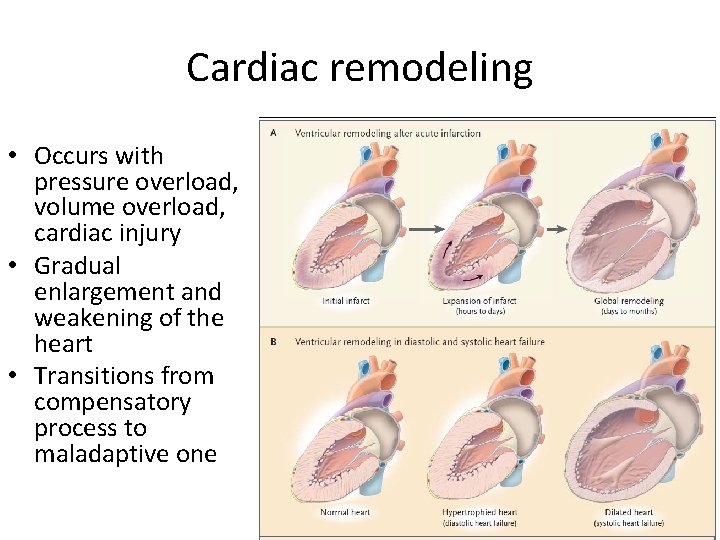
Cardiac remodeling • Occurs with pressure overload, volume overload, cardiac injury • Gradual enlargement and weakening of the heart • Transitions from compensatory process to maladaptive one

Heart failure: functional stages NYHA Class Level of Impairment I No symptom limitation with ordinary physical activity II Ordinary physical activity somewhat limited by dyspnea (shortness of breath) (e. g. , long-distance walking, climbing two flights of stairs) III Exercise limited by dyspnea with moderate workload (e. g. , short-distance walking, climbing one flight of stairs) IV Dyspnea (shortness of breath) at rest or with very little exertion
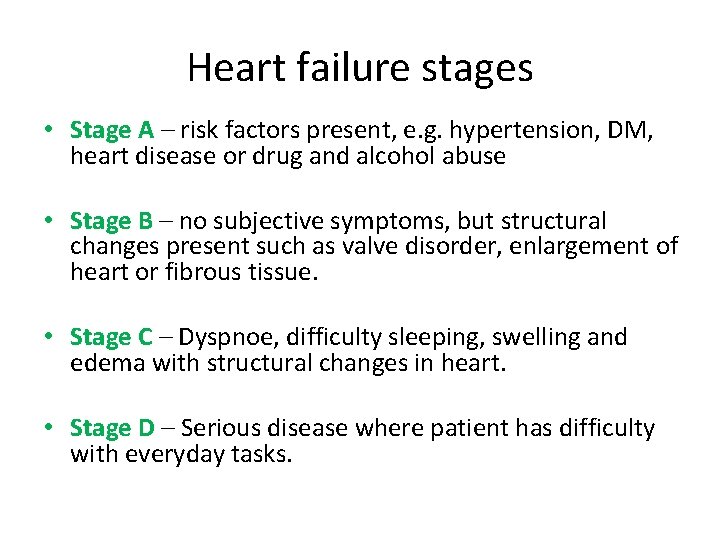
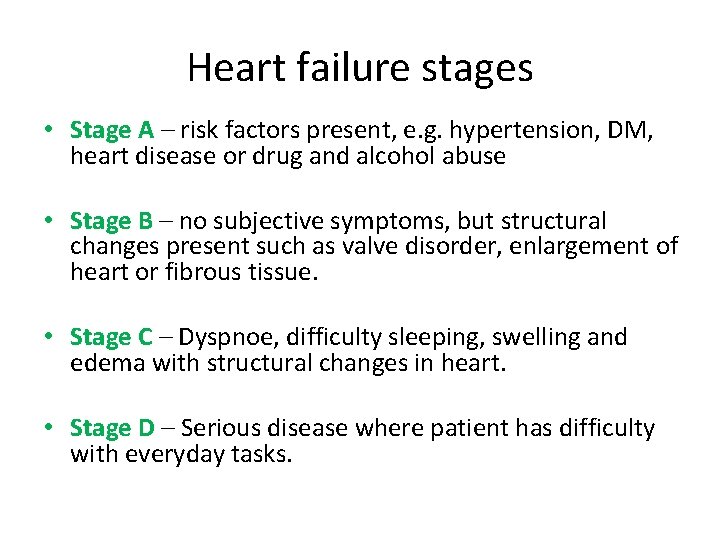
Heart failure stages • Stage A – risk factors present, e. g. hypertension, DM, heart disease or drug and alcohol abuse • Stage B – no subjective symptoms, but structural changes present such as valve disorder, enlargement of heart or fibrous tissue. • Stage C – Dyspnoe, difficulty sleeping, swelling and edema with structural changes in heart. • Stage D – Serious disease where patient has difficulty with everyday tasks.
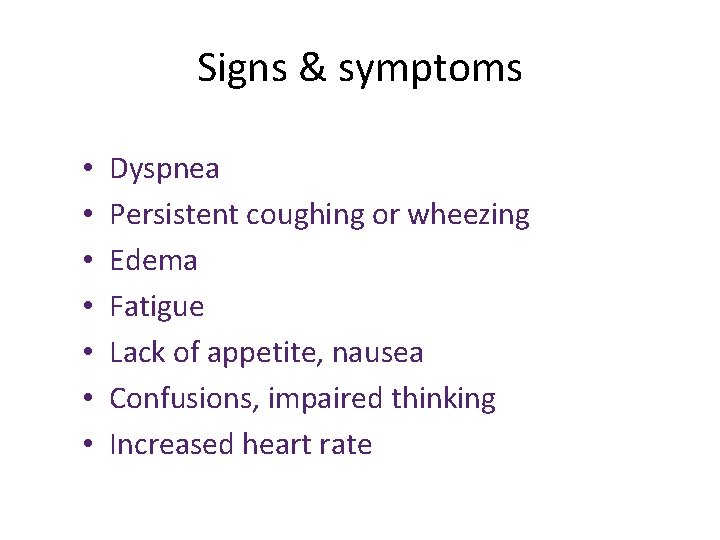
Signs & symptoms • • Dyspnea Persistent coughing or wheezing Edema Fatigue Lack of appetite, nausea Confusions, impaired thinking Increased heart rate
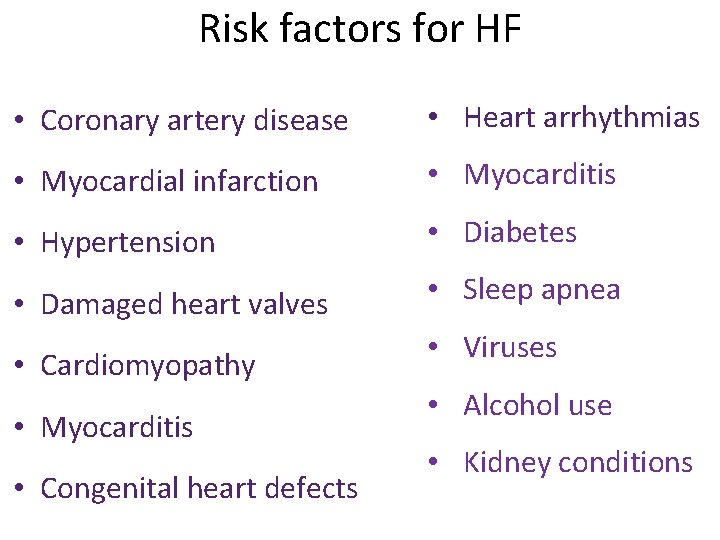
Risk factors for HF • Coronary artery disease • Heart arrhythmias • Myocardial infarction • Myocarditis • Hypertension • Diabetes • Damaged heart valves • Sleep apnea • Cardiomyopathy • Myocarditis • Congenital heart defects • Viruses • Alcohol use • Kidney conditions
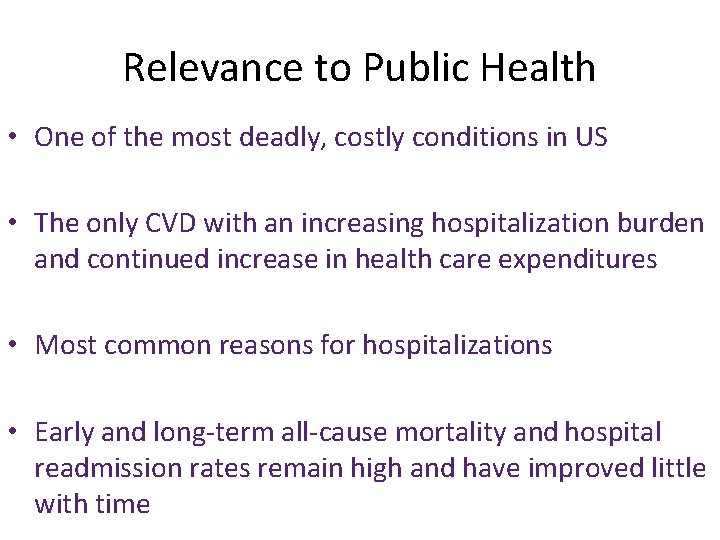
Relevance to Public Health • One of the most deadly, costly conditions in US • The only CVD with an increasing hospitalization burden and continued increase in health care expenditures • Most common reasons for hospitalizations • Early and long-term all-cause mortality and hospital readmission rates remain high and have improved little with time

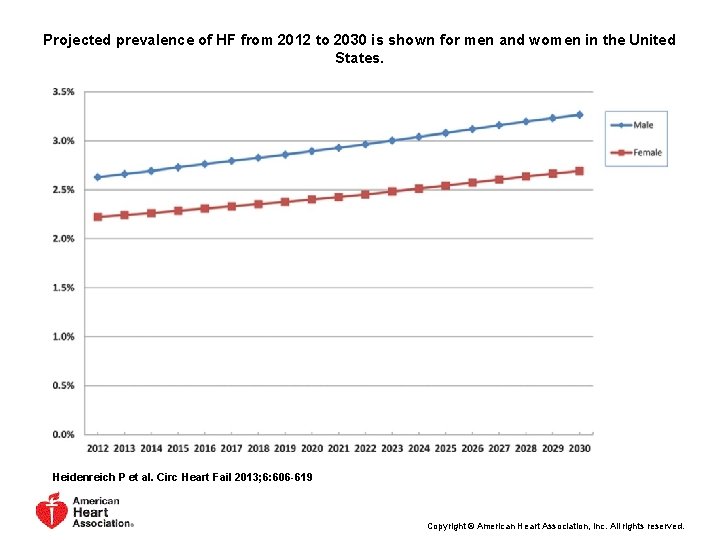
Descriptive epidemiology • Prevalence Increase over time and with age – > 5 million Americans with prevalent HF – By 2030: estimated 8 mill with prevalent HF
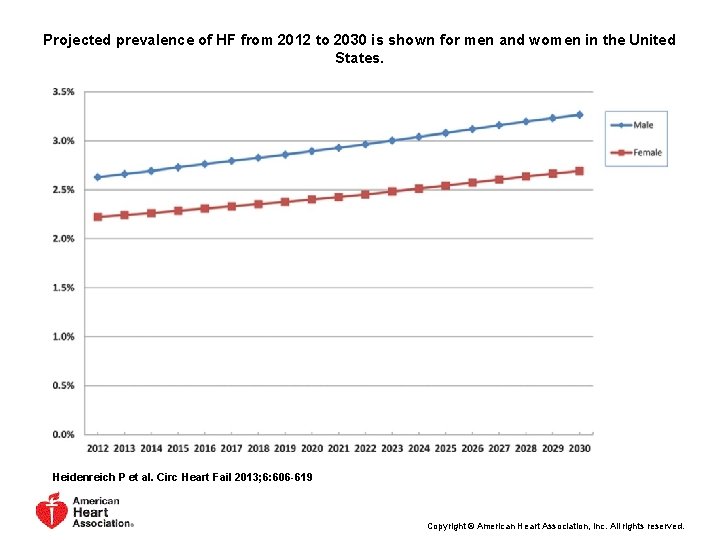
Projected prevalence of HF from 2012 to 2030 is shown for men and women in the United States. Heidenreich P et al. Circ Heart Fail 2013; 6: 606 -619 Copyright © American Heart Association, Inc. All rights reserved.
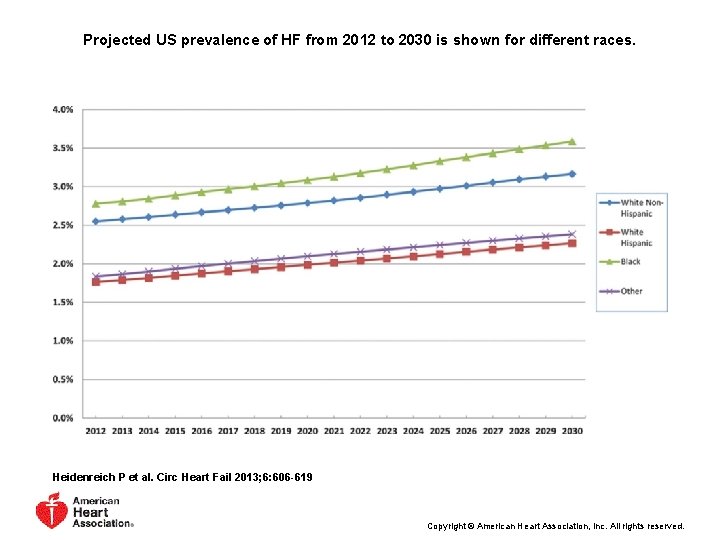
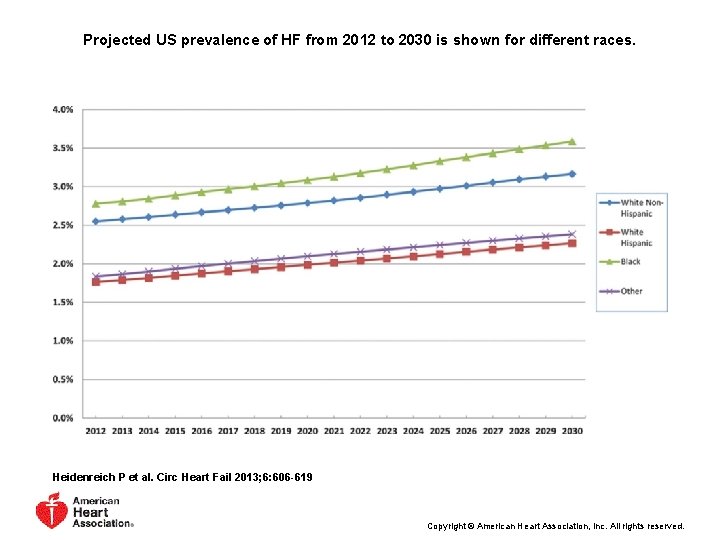
Projected US prevalence of HF from 2012 to 2030 is shown for different races. Heidenreich P et al. Circ Heart Fail 2013; 6: 606 -619 Copyright © American Heart Association, Inc. All rights reserved.
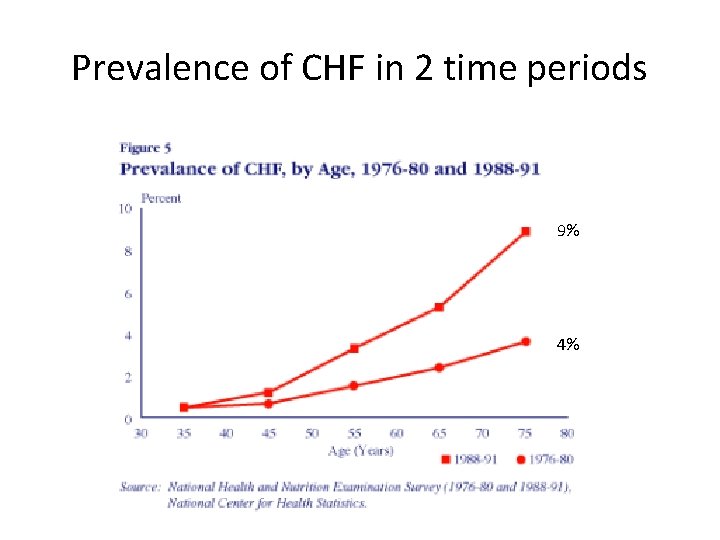
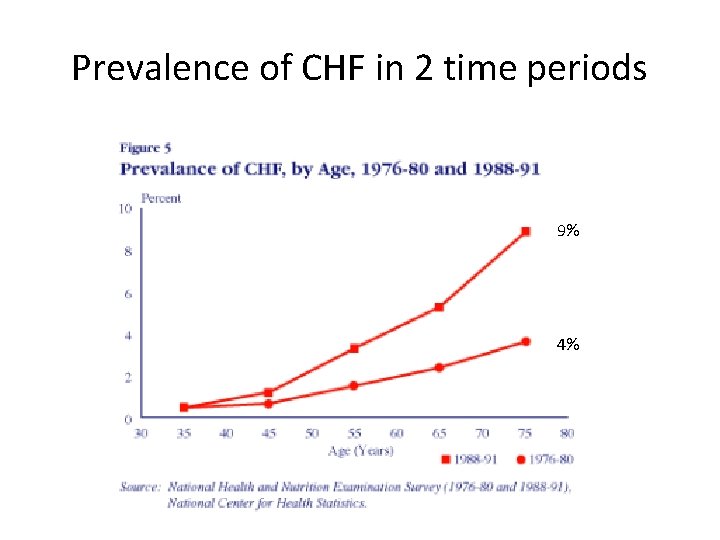
Prevalence of CHF in 2 time periods 9% 4%


Descriptive epidemiology Incidence – 400, 000 new cases annually –US incidence among elderly (≥ 65 years) was about 10 per 1000 population in 2006
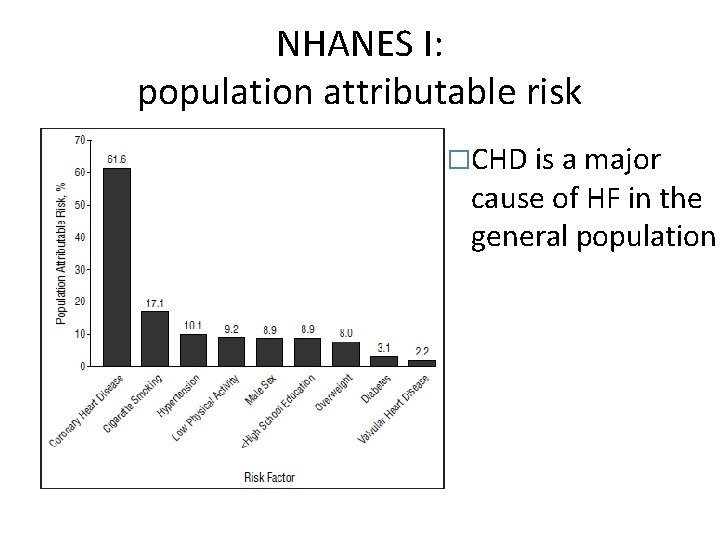
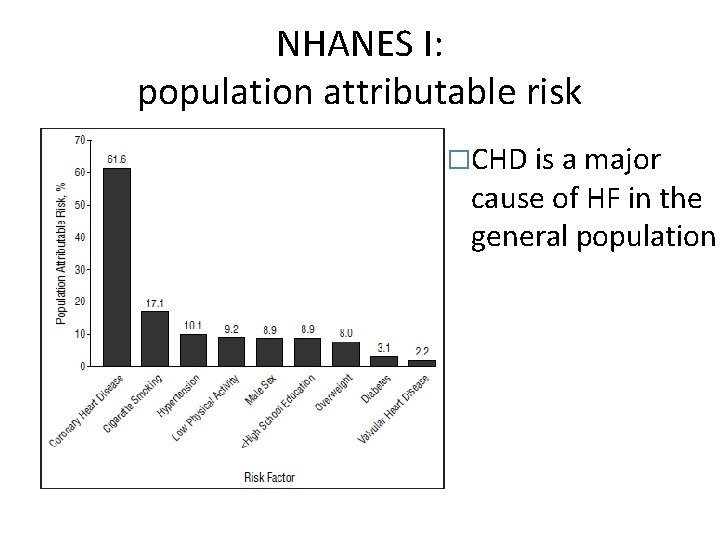
NHANES I: population attributable risk �CHD is a major cause of HF in the general population
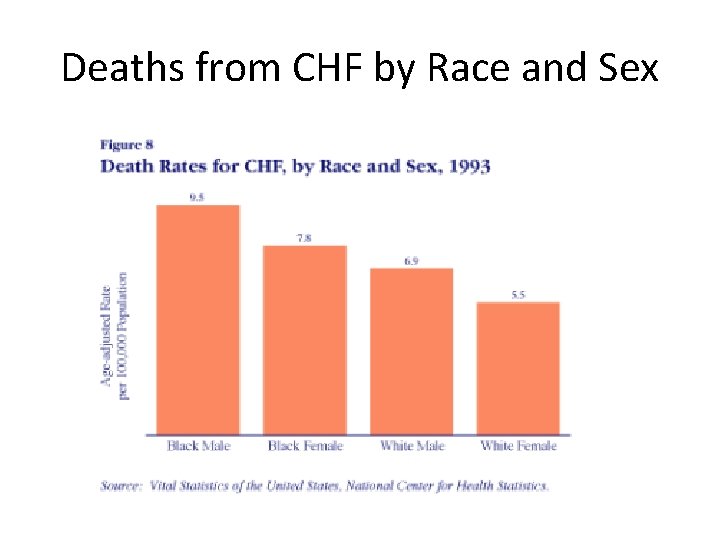
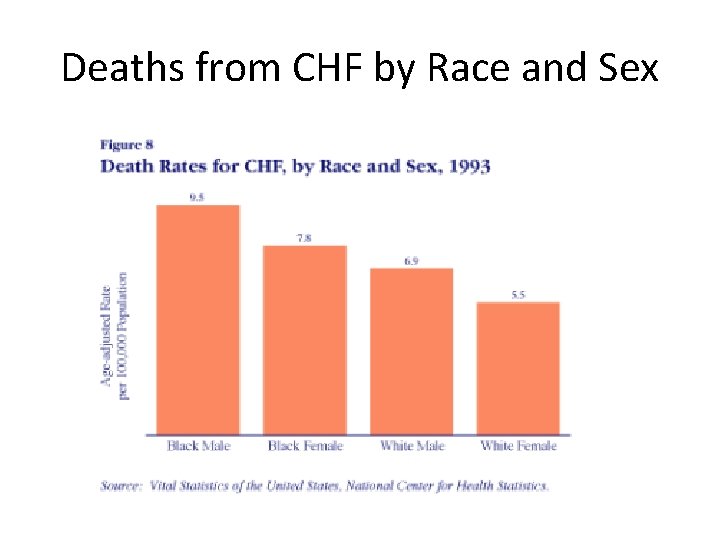
Deaths from CHF by Race and Sex
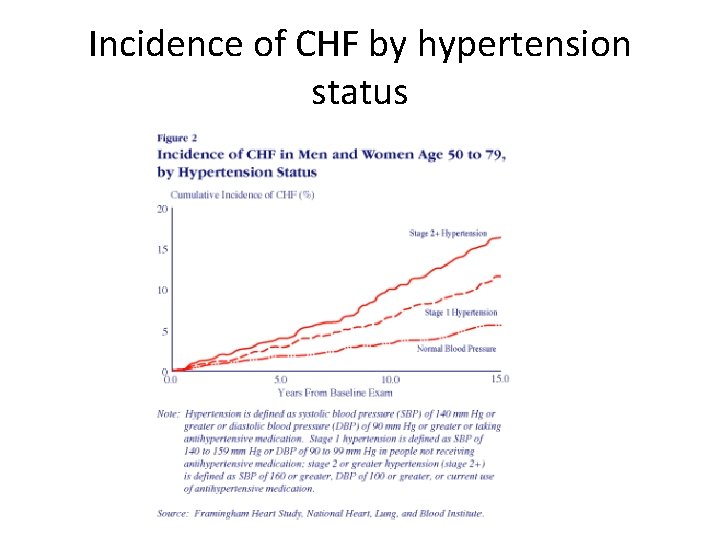
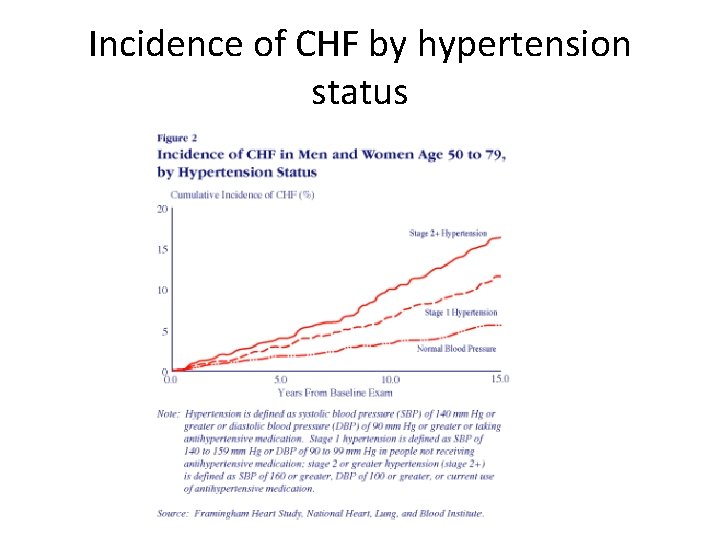
Incidence of CHF by hypertension status
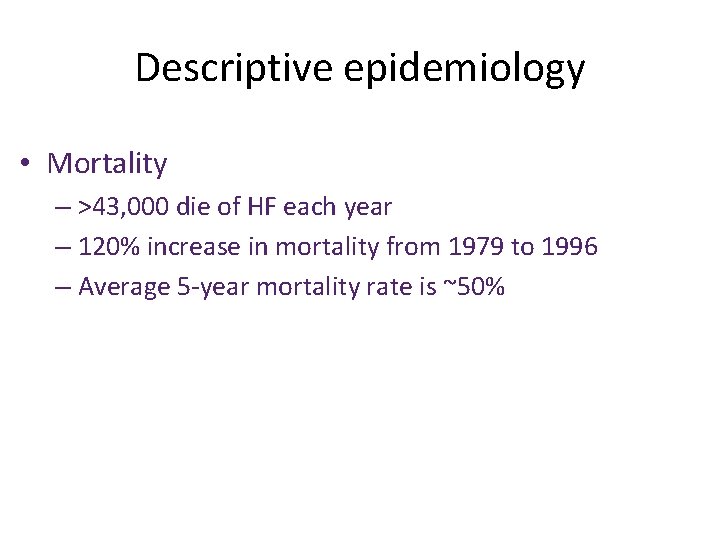
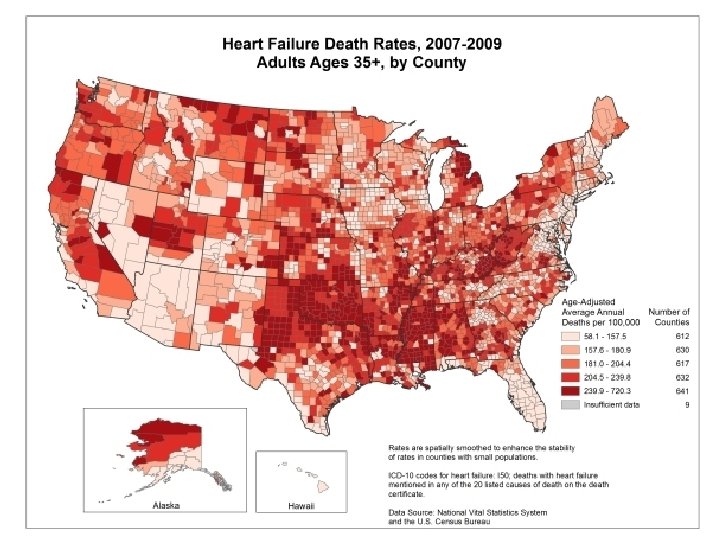
Descriptive epidemiology • Mortality – >43, 000 die of HF each year – 120% increase in mortality from 1979 to 1996 – Average 5 -year mortality rate is ~50%
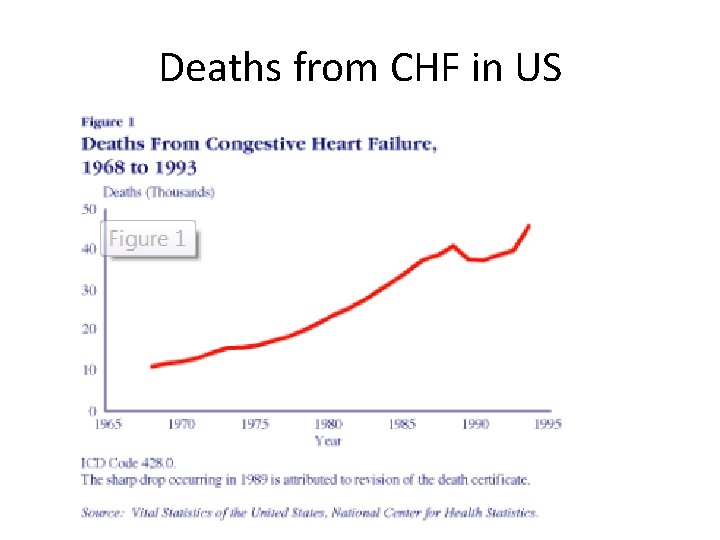
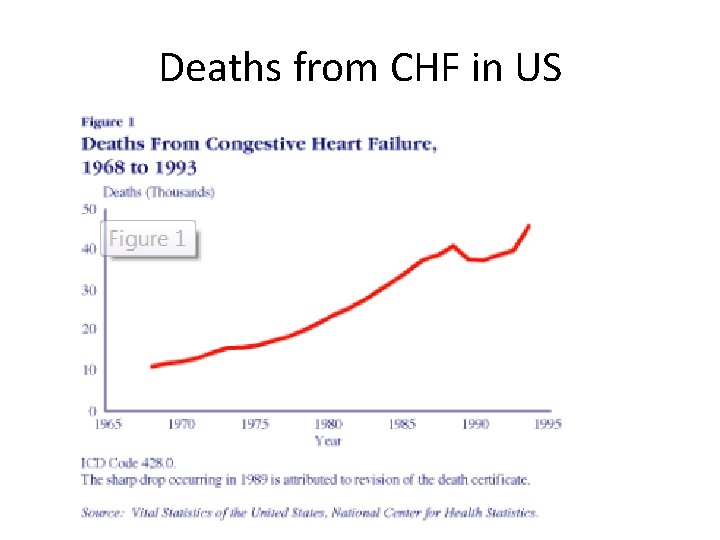
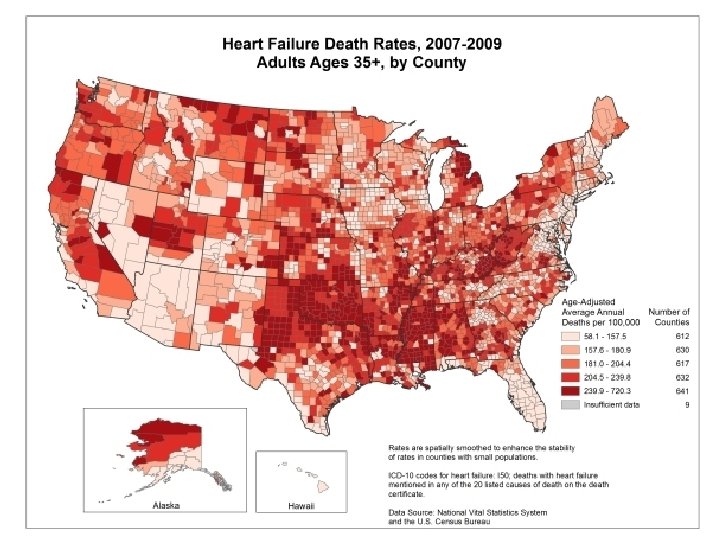
Deaths from CHF in US
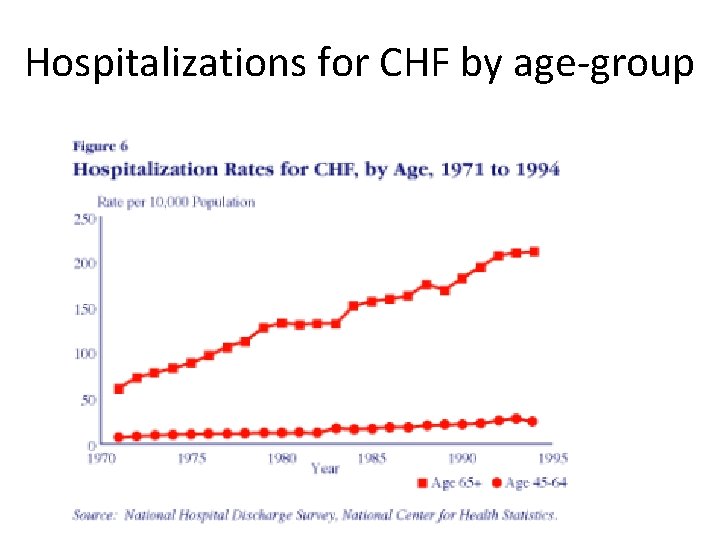
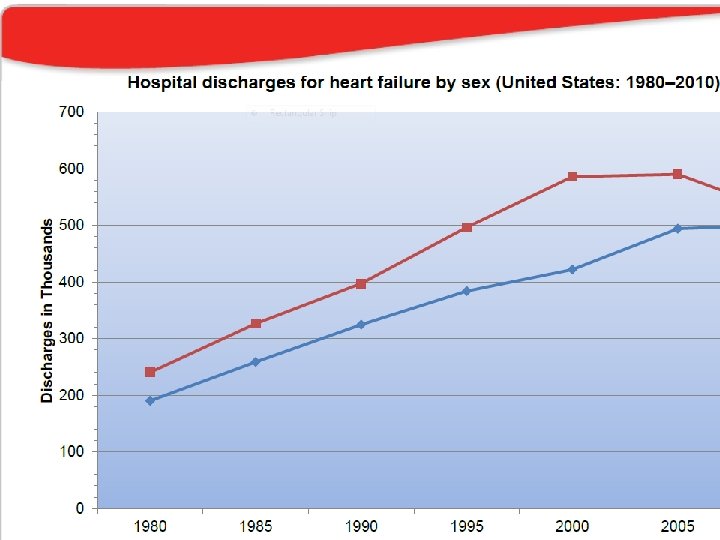
Descriptive epidemiology • Increase in hospitalizations – One of the top causes of hospitalizations – 377, 000 in 1979 to 870, 000 in 1996 (131% increase)
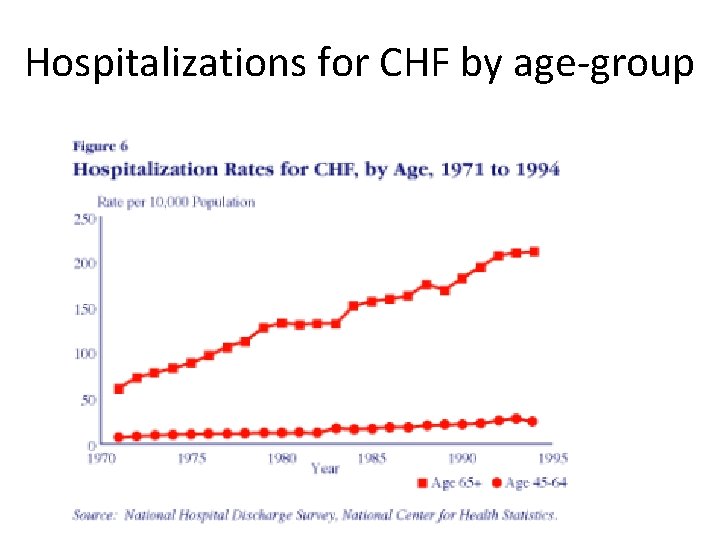
Hospitalizations for CHF by age-group

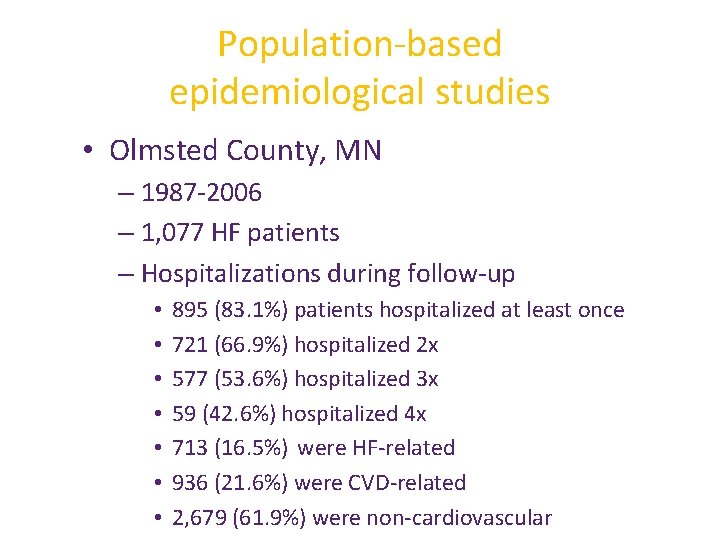
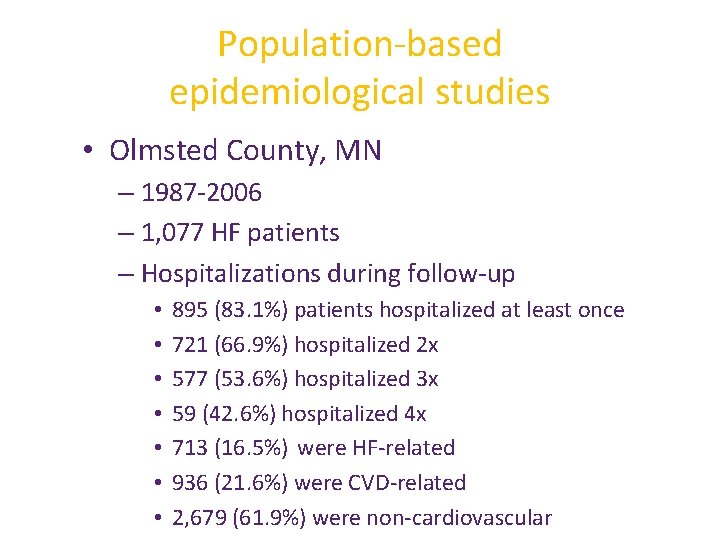
Population-based epidemiological studies • Olmsted County, MN – 1987 -2006 – 1, 077 HF patients – Hospitalizations during follow-up • • 895 (83. 1%) patients hospitalized at least once 721 (66. 9%) hospitalized 2 x 577 (53. 6%) hospitalized 3 x 59 (42. 6%) hospitalized 4 x 713 (16. 5%) were HF-related 936 (21. 6%) were CVD-related 2, 679 (61. 9%) were non-cardiovascular
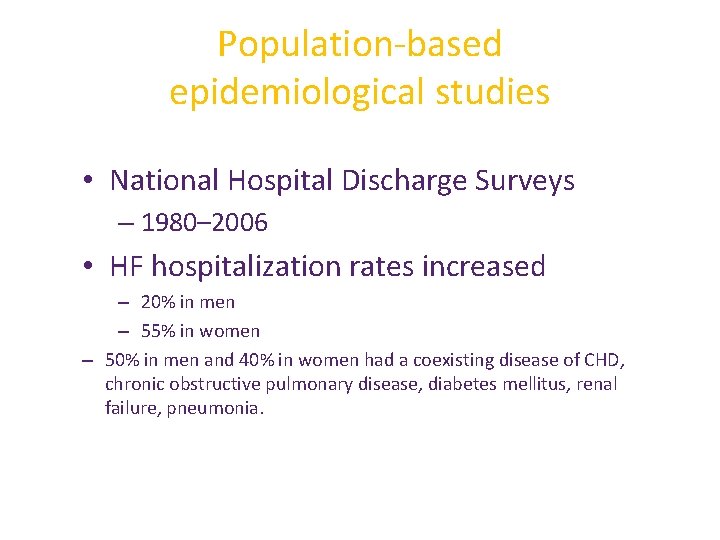
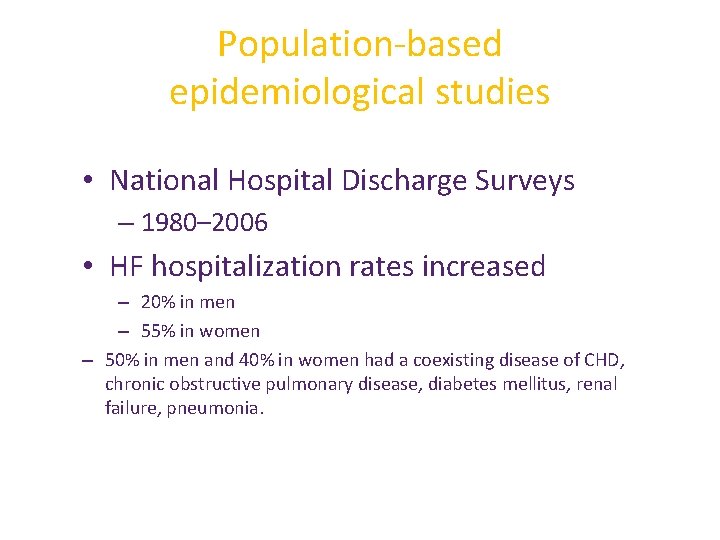
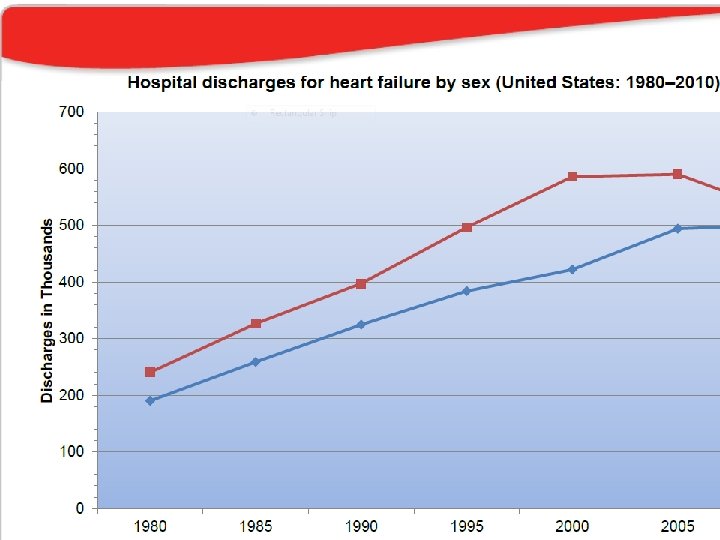
Population-based epidemiological studies • National Hospital Discharge Surveys – 1980– 2006 • HF hospitalization rates increased – 20% in men – 55% in women – 50% in men and 40% in women had a coexisting disease of CHD, chronic obstructive pulmonary disease, diabetes mellitus, renal failure, pneumonia.
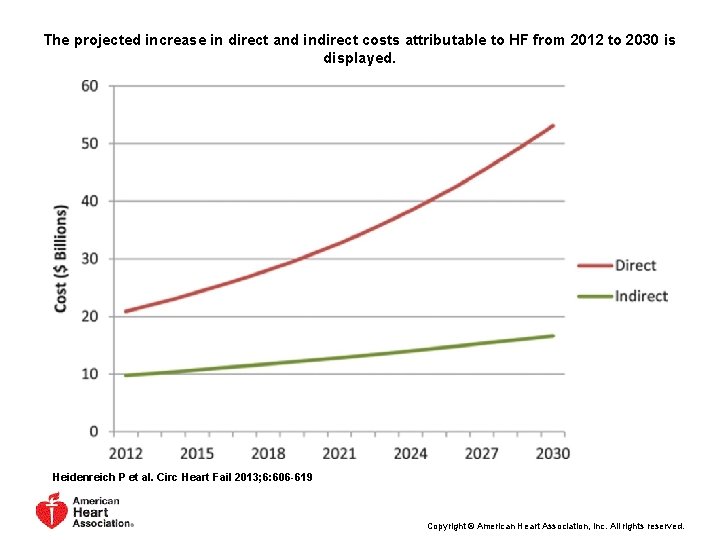
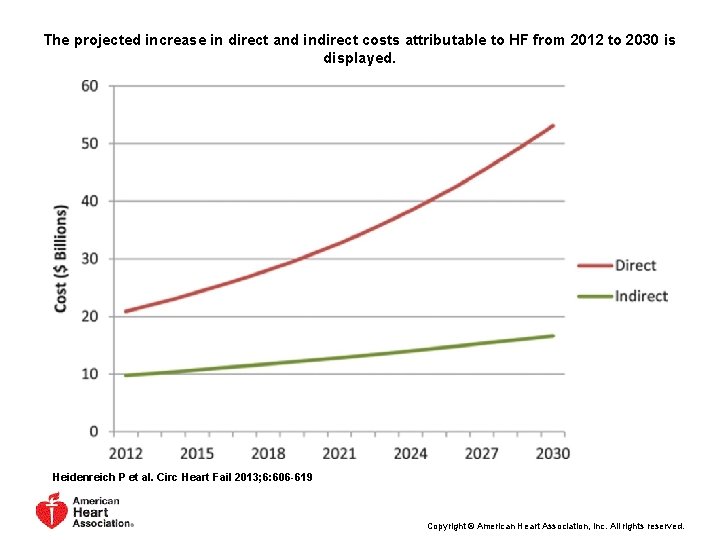
The projected increase in direct and indirect costs attributable to HF from 2012 to 2030 is displayed. Heidenreich P et al. Circ Heart Fail 2013; 6: 606 -619 Copyright © American Heart Association, Inc. All rights reserved.

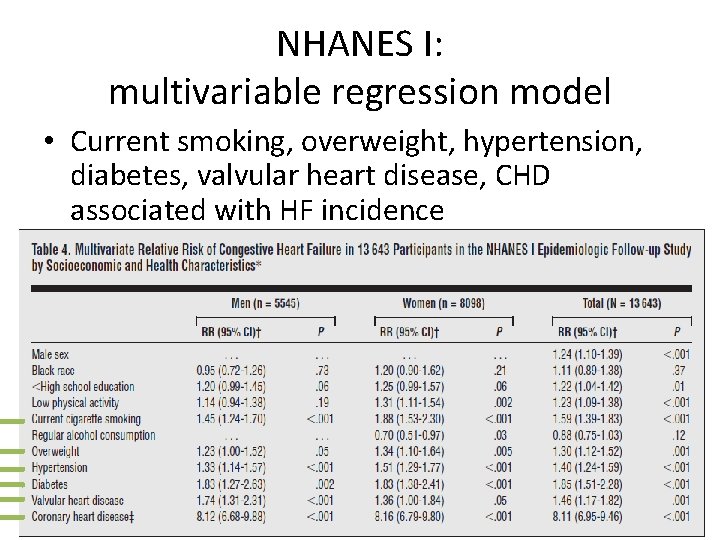
NHANES I: epidemiological follow-up study • Positive association between HF and lower education (less than HS), lower physical activity, current smoking, overweight, diabetes, hypertension, valvular heart disease
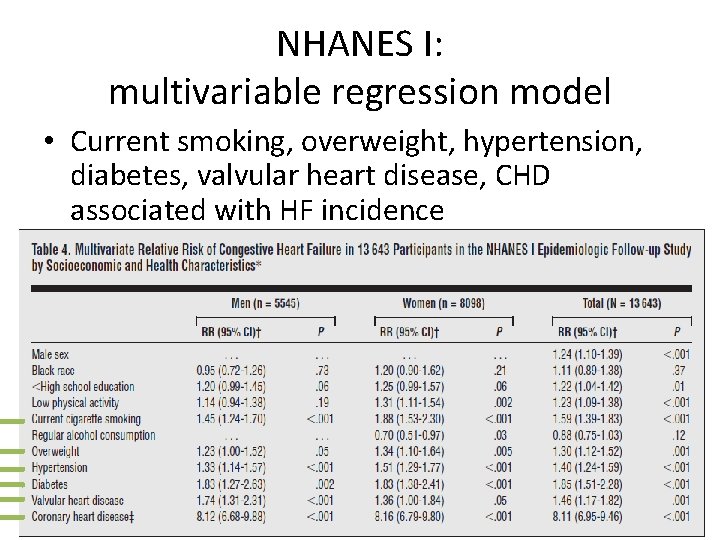
NHANES I: multivariable regression model • Current smoking, overweight, hypertension, diabetes, valvular heart disease, CHD associated with HF incidence
Current literature
Diet and heart failure
Whole-grain, dairy , egg • • • The Atherosclerosis Risk in Communities (ARIC) Study 13 year study Multivariable adjustment for energy intake, demographics, lifestyle factors, prevalent CVD, diabetes, hypertension Whole-grain intake HR=0. 93 [0. 87, 0. 99] Eggs HR=1. 23 [1. 08, 1. 41] High-fat dairy HR=1. 08 [1. 01, 1. 16]
Polyunsaturated fatty acids �Experimental trials show that PUFA improve left ventricular function may
Polyunsaturated fatty acids: clinical trial • 133 HF patients with non-ischemic dilated cardiomyopathy • Randomized to 2 grams of n-3 PUFAs or placebo • Assessed at baseline and at 12 months • Conclusion: N-3 PUFAs may improve LV systolic function, functional capacity, and reduce hospitalizations
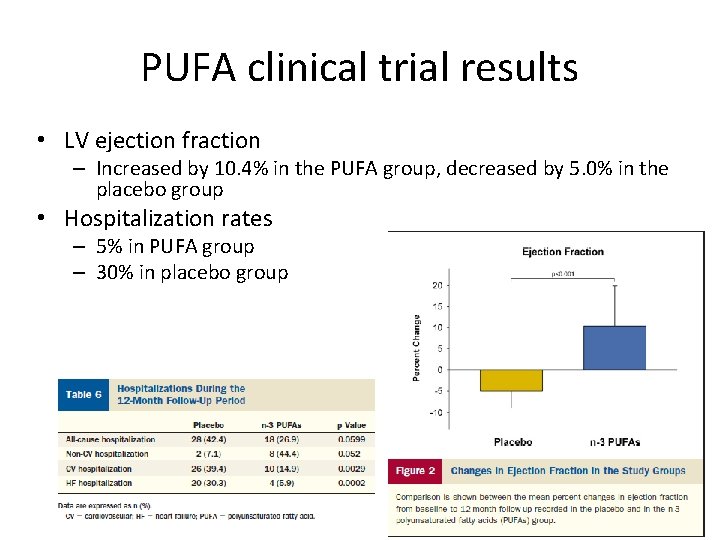
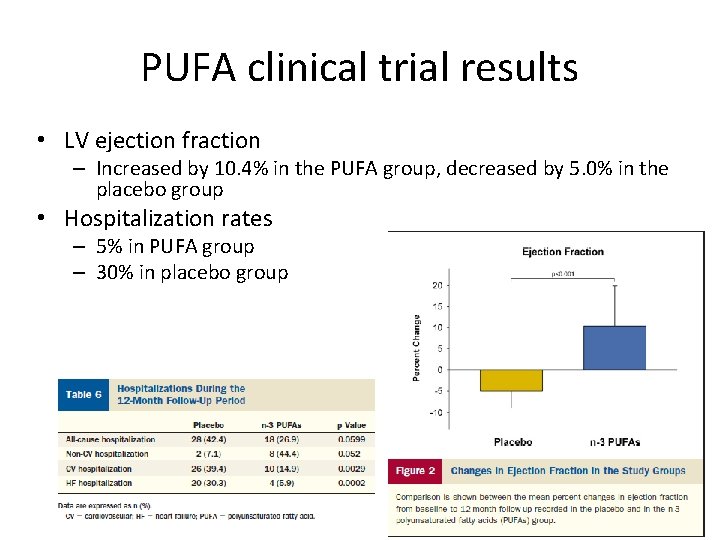
PUFA clinical trial results • LV ejection fraction – Increased by 10. 4% in the PUFA group, decreased by 5. 0% in the placebo group • Hospitalization rates – 5% in PUFA group – 30% in placebo group
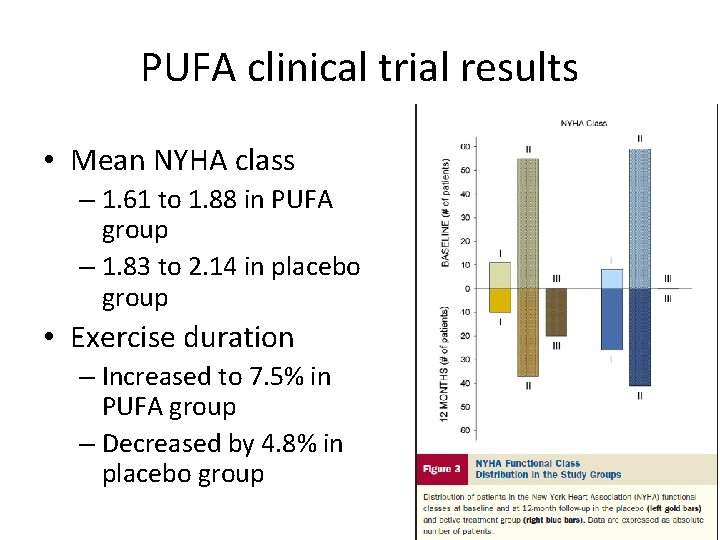
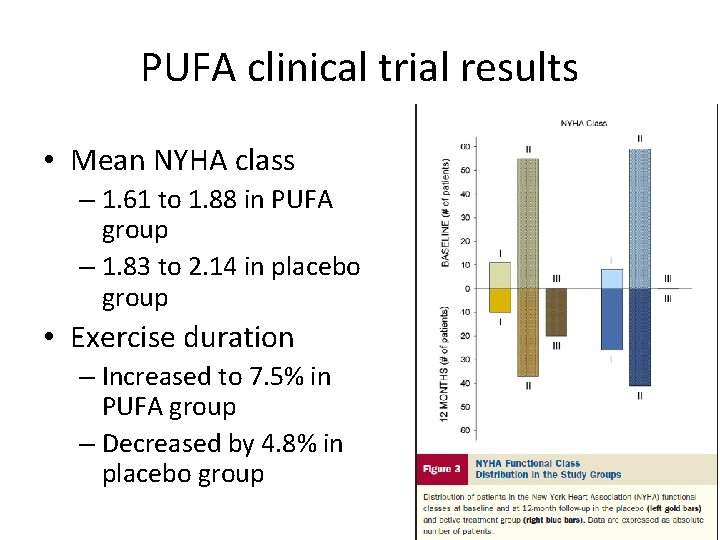
PUFA clinical trial results • Mean NYHA class – 1. 61 to 1. 88 in PUFA group – 1. 83 to 2. 14 in placebo group • Exercise duration – Increased to 7. 5% in PUFA group – Decreased by 4. 8% in placebo group
Nuts and HF – preliminary findings from AHS. • The AHS overlap population (participated in both AHS-1 and AHS-2) • Overall, nut consumption was associated with lower risk of HF (unpublished data): – Dose-response – Compared to rarely or never eating nuts in AHS -1: – Eating 1 -6 times/wk -69% reduced risk – Eating nuts daily - 84% reduced risk
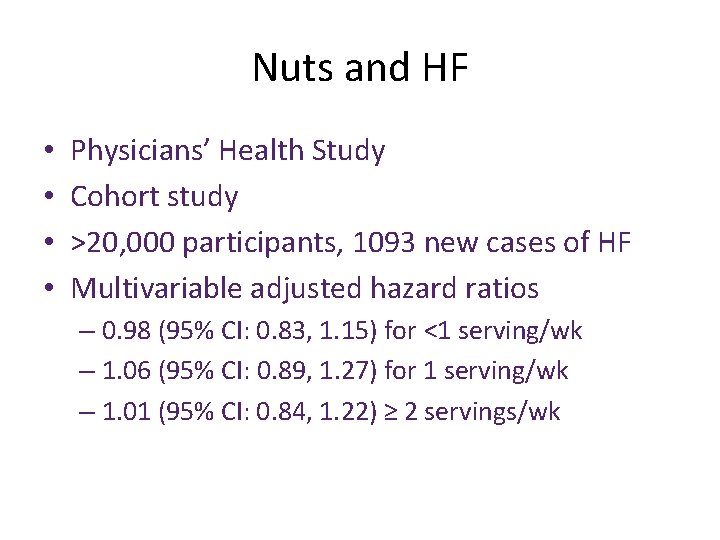
Nuts and HF • • Physicians’ Health Study Cohort study >20, 000 participants, 1093 new cases of HF Multivariable adjusted hazard ratios – 0. 98 (95% CI: 0. 83, 1. 15) for <1 serving/wk – 1. 06 (95% CI: 0. 89, 1. 27) for 1 serving/wk – 1. 01 (95% CI: 0. 84, 1. 22) ≥ 2 servings/wk
Heart Pilot clinic – AHS-2 • 200 AHS-2 subjects > 60 yrs living locally • Echo, blood, FFQ • 25% Blacks, 75% non-Blacks
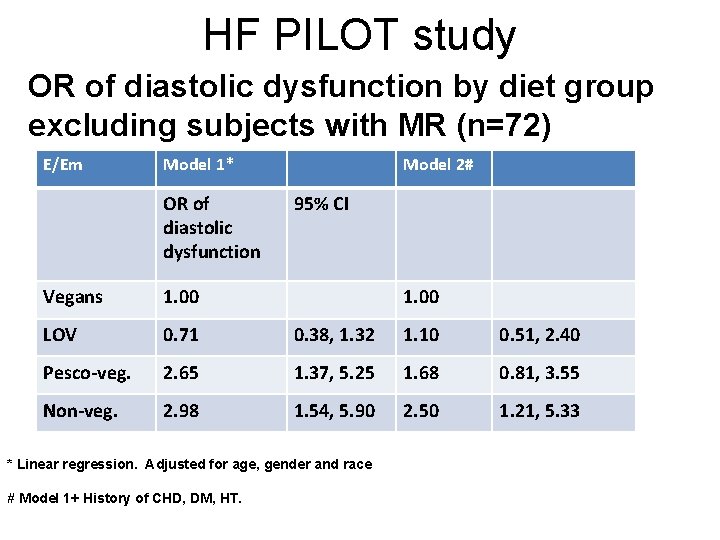
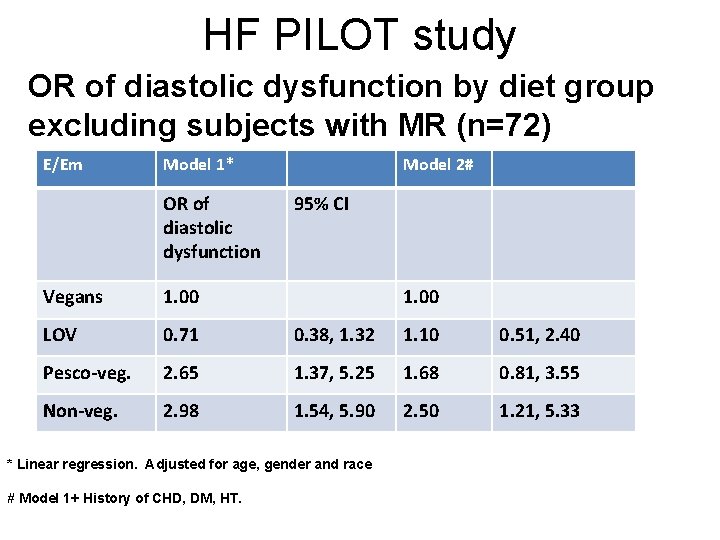
HF PILOT study OR of diastolic dysfunction by diet group excluding subjects with MR (n=72) E/Em Model 1* OR of diastolic dysfunction Model 2# 95% CI Vegans 1. 00 LOV 0. 71 0. 38, 1. 32 1. 10 0. 51, 2. 40 Pesco-veg. 2. 65 1. 37, 5. 25 1. 68 0. 81, 3. 55 Non-veg. 2. 98 1. 54, 5. 90 2. 50 1. 21, 5. 33 * Linear regression. Adjusted for age, gender and race # Model 1+ History of CHD, DM, HT.
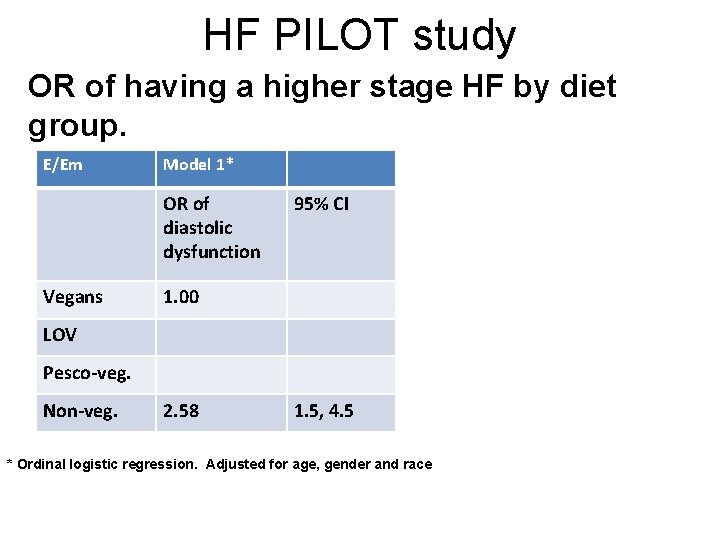
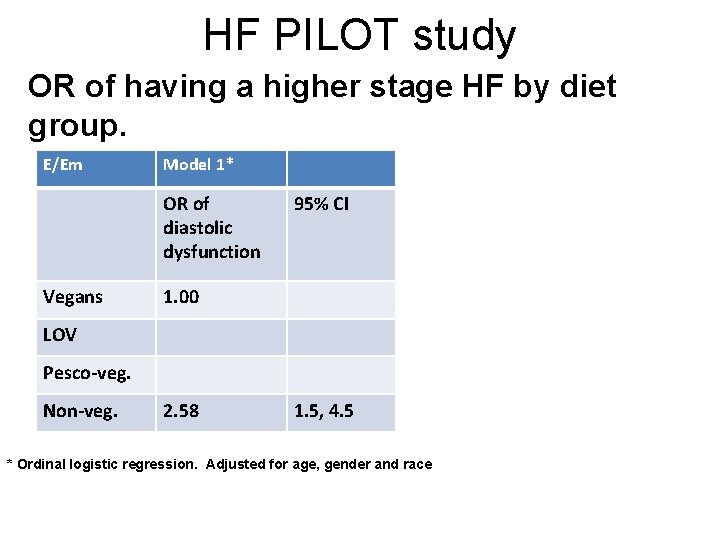
HF PILOT study OR of having a higher stage HF by diet group. E/Em Model 1* OR of diastolic dysfunction Vegans 95% CI 1. 00 LOV Pesco-veg. Non-veg. 2. 58 1. 5, 4. 5 * Ordinal logistic regression. Adjusted for age, gender and race
Exercise and heart failure
HF and exercise • Exercise intervention Significant exercise capacity. • Studies have mostly been small, short term, in men, in subjects with stable chronic heart failure • Current guidelines for exercise training in HF acknowledge the benefits of aerobic training, but there is no protocol in place

Experimental trial • Randomized, unblinded, controlled trial • Mean follow-up of 3. 4 years • Cardiology institute and hospital • 55 subjects allocated to exercise training
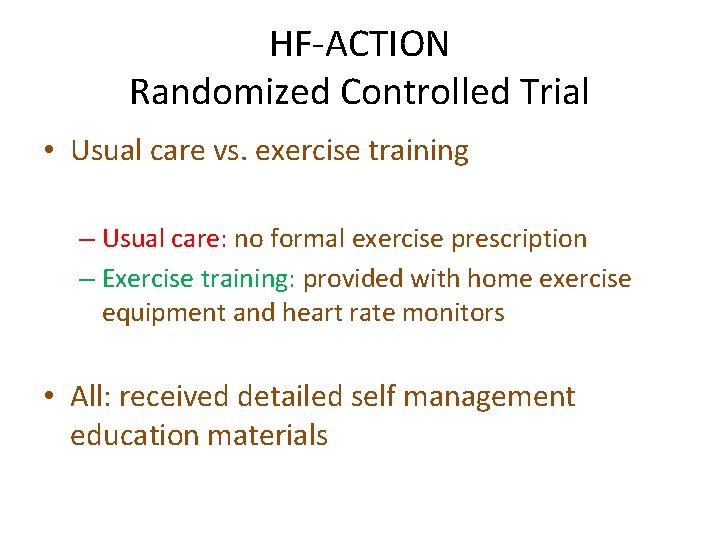
HF-ACTION Randomized Controlled Trial • Usual care vs. exercise training – Usual care: no formal exercise prescription – Exercise training: provided with home exercise equipment and heart rate monitors • All: received detailed self management education materials
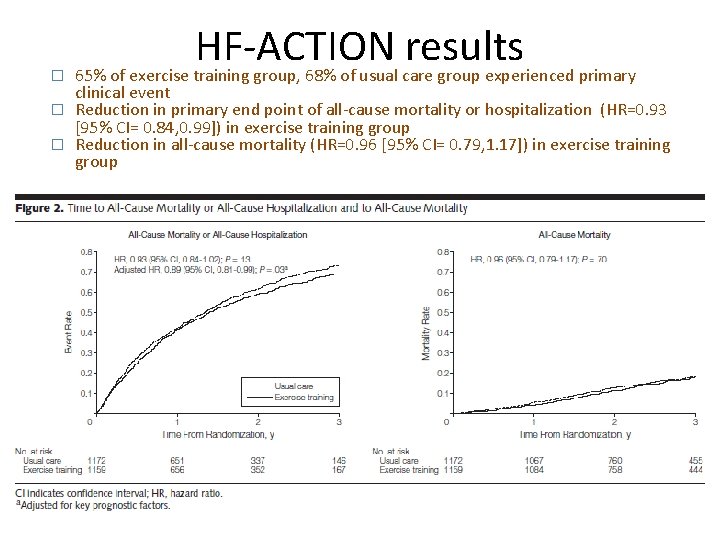
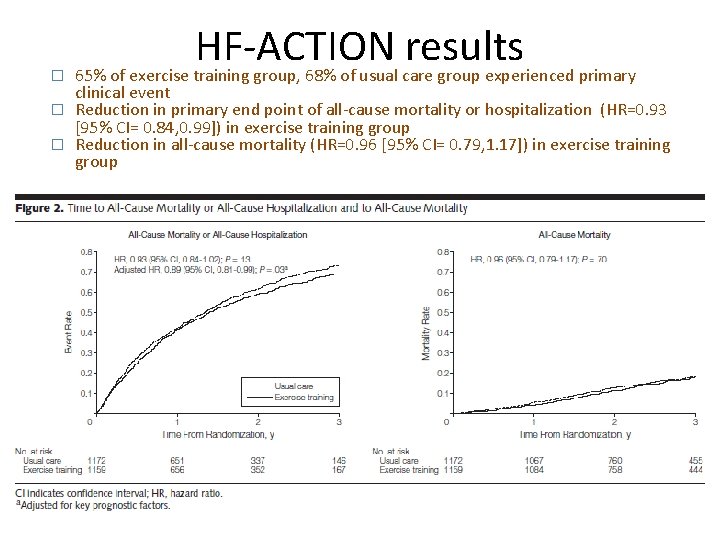
� HF-ACTION results 65% of exercise training group, 68% of usual care group experienced primary clinical event � Reduction in primary end point of all-cause mortality or hospitalization (HR=0. 93 [95% CI= 0. 84, 0. 99]) in exercise training group � Reduction in all-cause mortality (HR=0. 96 [95% CI= 0. 79, 1. 17]) in exercise training group
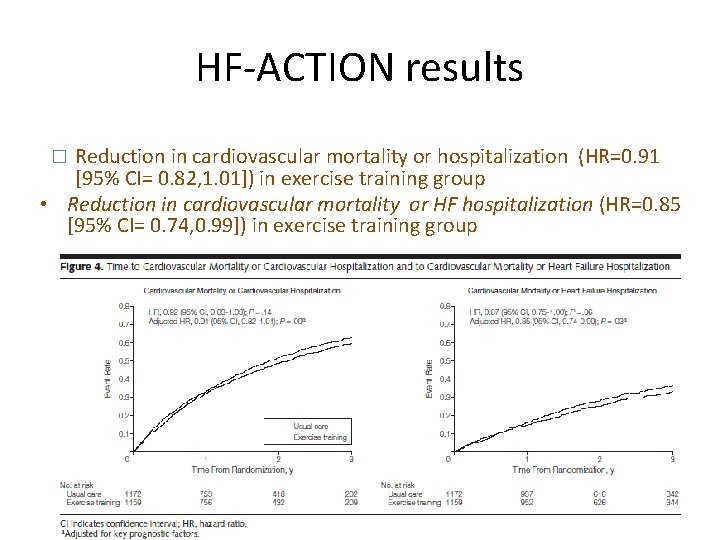
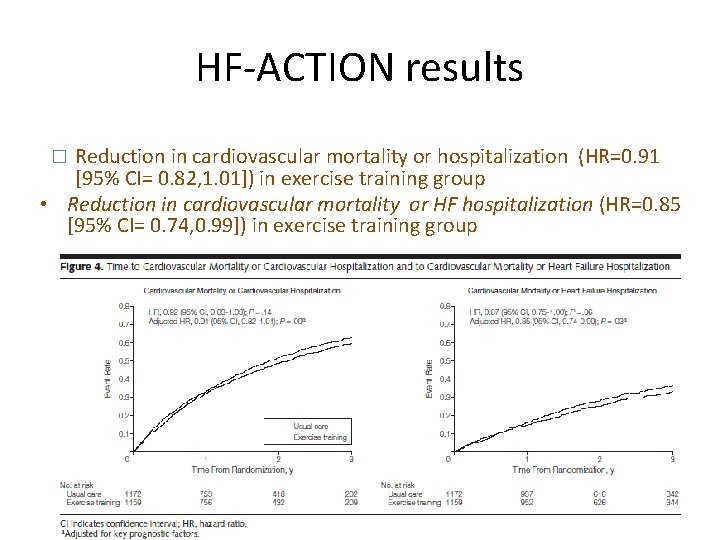
HF-ACTION results Reduction in cardiovascular mortality or hospitalization (HR=0. 91 [95% CI= 0. 82, 1. 01]) in exercise training group • Reduction in cardiovascular mortality or HF hospitalization (HR=0. 85 [95% CI= 0. 74, 0. 99]) in exercise training group �
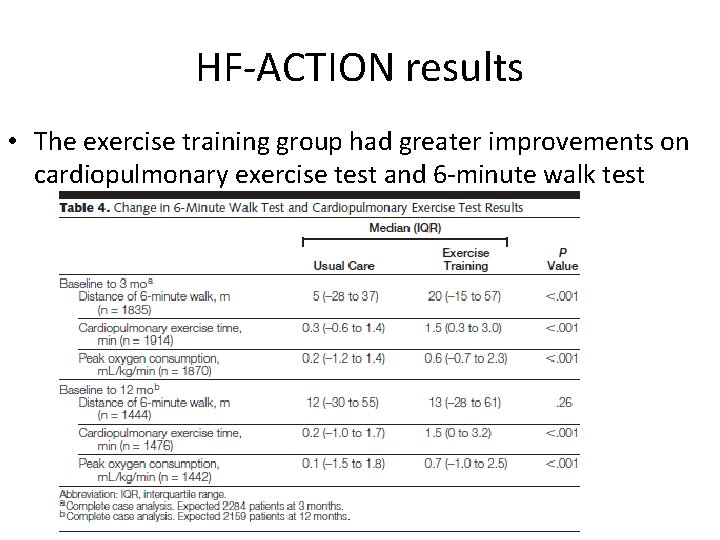
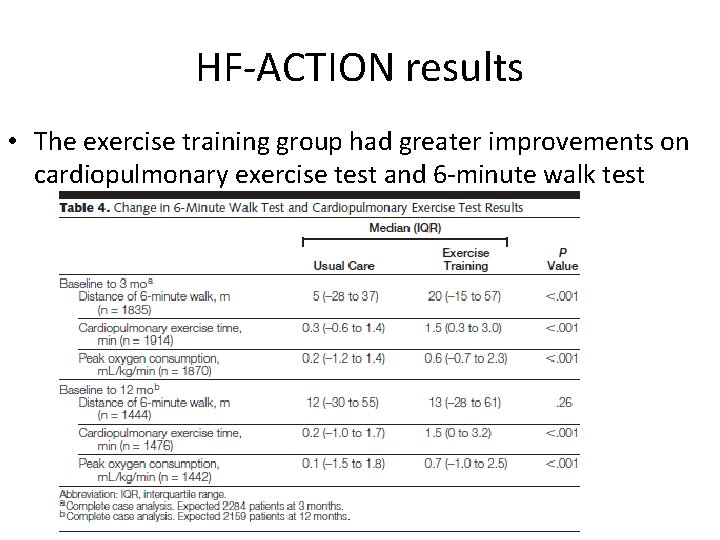
HF-ACTION results • The exercise training group had greater improvements on cardiopulmonary exercise test and 6 -minute walk test
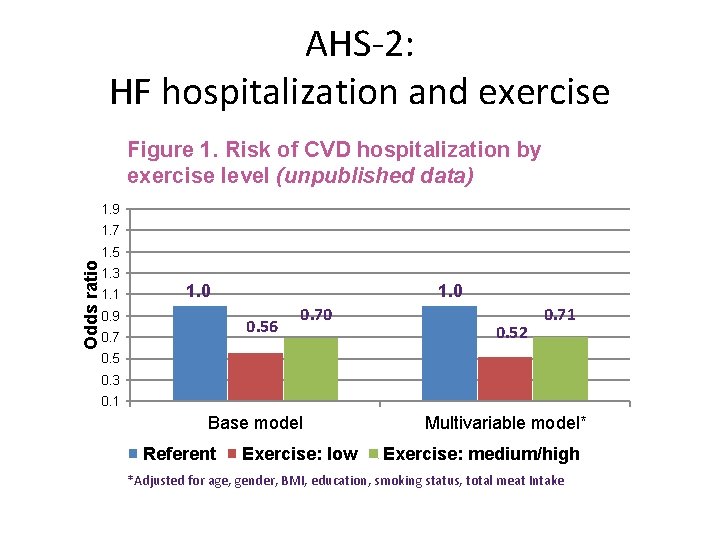
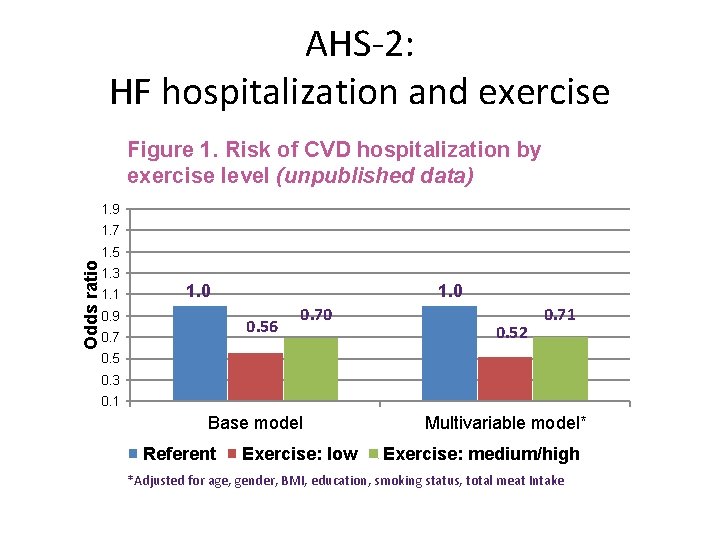
AHS-2: HF hospitalization and exercise Figure 1. Risk of CVD hospitalization by exercise level (unpublished data) 1. 9 1. 7 Odds ratio 1. 5 1. 3 1. 1 1. 0 0. 9 0. 56 0. 70 0. 52 0. 71 0. 5 0. 3 0. 1 Base model Referent Exercise: low Multivariable model* Exercise: medium/high *Adjusted for age, gender, BMI, education, smoking status, total meat Intake
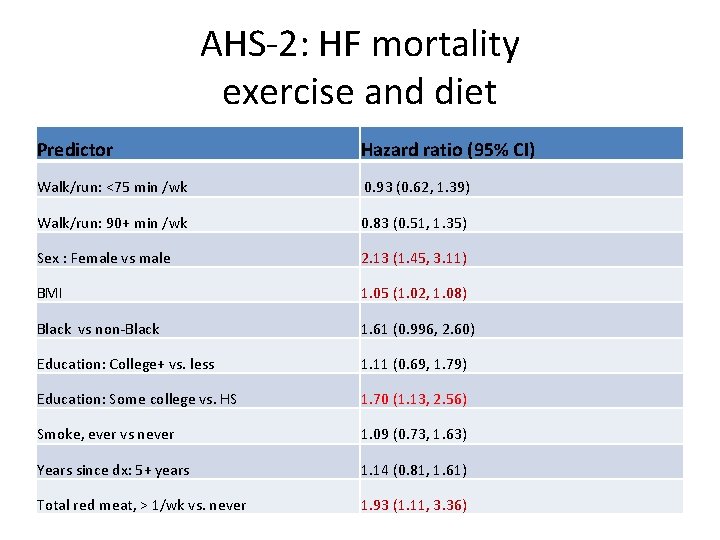
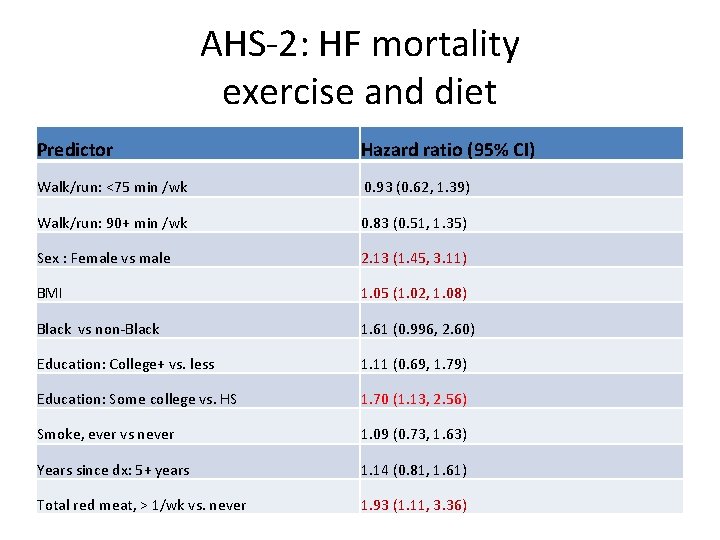
AHS-2: HF mortality exercise and diet Predictor Hazard ratio (95% CI) Walk/run: <75 min /wk 0. 93 (0. 62, 1. 39) Walk/run: 90+ min /wk 0. 83 (0. 51, 1. 35) Sex : Female vs male 2. 13 (1. 45, 3. 11) BMI 1. 05 (1. 02, 1. 08) Black vs non-Black 1. 61 (0. 996, 2. 60) Education: College+ vs. less 1. 11 (0. 69, 1. 79) Education: Some college vs. HS 1. 70 (1. 13, 2. 56) Smoke, ever vs never 1. 09 (0. 73, 1. 63) Years since dx: 5+ years 1. 14 (0. 81, 1. 61) Total red meat, > 1/wk vs. never 1. 93 (1. 11, 3. 36)
Conclusions • Patients with HF have poorer quality of life and shorter life expectancy compared to the general population • Modern treatment methods for HF has improved – Medication – Rehab programs – At-home guidance – More research needed • It is unclear to what degree diet and lifestyle can contribute to prevention as well as course of disease. – Standardized, large-scale primary and secondary intervention trials are needed
References • Congestive Heart Failure. http: //www. mayoclinic. org/congestive-heartfailure/. Accessed March 8, 2010. • L Djousee, et Al. Nut consumption and risk of heart failure in the Physicians’ Health Study I 1. (2008) American Journal of Clinical Nutrition. 88: 930 – 3. • Liu L, Changes in Cardiovascular Hospitalization and Comorbidity of Heart Failure in the United States: Findings from the National Hospital Discharge Surveys 1980– 2006, Int J Cardiol (2010), doi: 10. 1016/j. ijcard. 2009. 11. 037 • Nettleton, J, et Al. Incident Heart Failure Is Associated with Lower Whole. Grain Intake and Greater High-Fat Dairy and Egg Intake in the Atherosclerosis Risk in Communities (ARIC) Study. J Am Diet Assoc. 2008 November ; 108(11): 1881– 1887. doi: 10. 1016/j. jada. 2008. 015. • Rees K, et Al. Exercise based rehabilitation for heart failure (Review). (2009) The Cochrane Library. 1: 1 -38.
 Cor pulmonale
Cor pulmonale Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Right sided heart failure
Right sided heart failure Congestive heart failure zones for management
Congestive heart failure zones for management Steenkorf goedkoop
Steenkorf goedkoop Anders knutsen
Anders knutsen Herman dikland
Herman dikland Non conducted pac ecg
Non conducted pac ecg Failure to fire pacemaker
Failure to fire pacemaker Ductile vs brittle fracture surface
Ductile vs brittle fracture surface Ortec 566 tac
Ortec 566 tac Decreto legislativo 566/20
Decreto legislativo 566/20 Classification of ejection fraction
Classification of ejection fraction Diabetes and heart failure
Diabetes and heart failure Heart failure
Heart failure Right vs left-sided heart failure chart
Right vs left-sided heart failure chart Acute pulmonary congestion histology
Acute pulmonary congestion histology Causes of cardiomegaly in child
Causes of cardiomegaly in child Heart failure definition
Heart failure definition Compensatory mechanism of heart failure
Compensatory mechanism of heart failure Lmnop heart failure
Lmnop heart failure Heart failure forward vs backward
Heart failure forward vs backward Heart failure complications
Heart failure complications Apetm
Apetm Keith rn heart failure case study
Keith rn heart failure case study Forrester classification heart failure
Forrester classification heart failure Chlorpromide
Chlorpromide Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Acute vs chronic heart failure
Acute vs chronic heart failure Ecg findings of heart failure
Ecg findings of heart failure Star plowhorse puzzle dog
Star plowhorse puzzle dog Dullness of heart
Dullness of heart How to dissect a sheep heart
How to dissect a sheep heart Principles of information security 5th edition pdf
Principles of information security 5th edition pdf Failure of homeostasis
Failure of homeostasis Agile failure stories
Agile failure stories Patriot missile failure
Patriot missile failure Brittle failure
Brittle failure Failure in ddbms
Failure in ddbms What is failure demand
What is failure demand Define long term memory
Define long term memory Acute liver failure criteria
Acute liver failure criteria Types of market failure
Types of market failure Ib economics market failure questions
Ib economics market failure questions Water pump failure causes
Water pump failure causes Respiratory failure type
Respiratory failure type Blind to failure summary
Blind to failure summary Splendid failure definition
Splendid failure definition Fatigue failure beach marks
Fatigue failure beach marks Midwest iconography
Midwest iconography Kegagalan pasar adalah
Kegagalan pasar adalah Chain hoist failure
Chain hoist failure Schools without failure
Schools without failure Define market failure
Define market failure Daniel mahzonni
Daniel mahzonni Infrastructure failure definition
Infrastructure failure definition Memeriksa keakuratan dan validasi data disebut:
Memeriksa keakuratan dan validasi data disebut: