EOR 7 Case Review Michael Funk PAC MPH




- Slides: 57
EOR 7 Case Review Michael Funk, PA-C, MPH, DFAAPA July 10, 2015
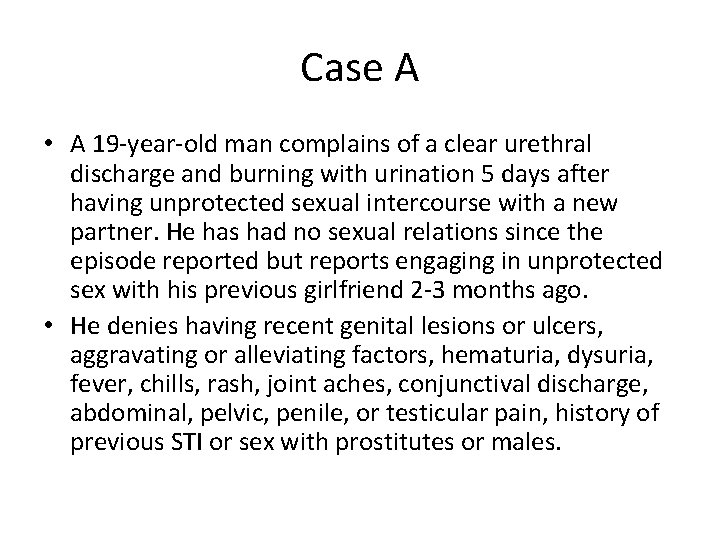
Case A • A 19 -year-old man complains of a clear urethral discharge and burning with urination 5 days after having unprotected sexual intercourse with a new partner. He has had no sexual relations since the episode reported but reports engaging in unprotected sex with his previous girlfriend 2 -3 months ago. • He denies having recent genital lesions or ulcers, aggravating or alleviating factors, hematuria, dysuria, fever, chills, rash, joint aches, conjunctival discharge, abdominal, pelvic, penile, or testicular pain, history of previous STI or sex with prostitutes or males.
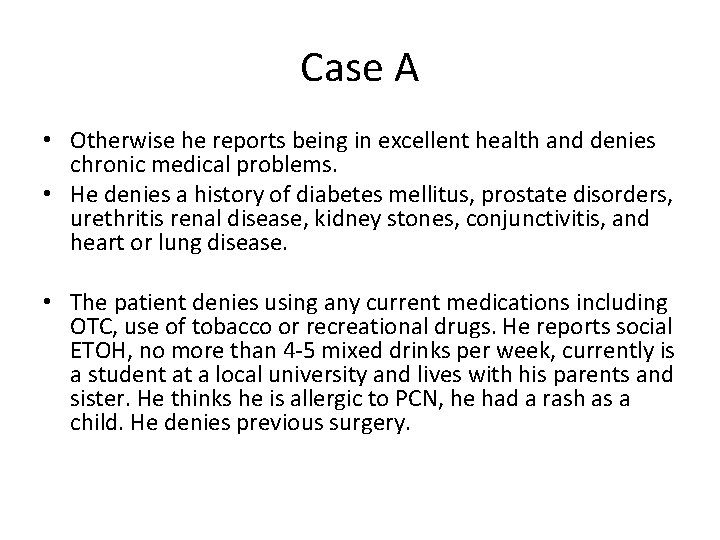
Case A • Otherwise he reports being in excellent health and denies chronic medical problems. • He denies a history of diabetes mellitus, prostate disorders, urethritis renal disease, kidney stones, conjunctivitis, and heart or lung disease. • The patient denies using any current medications including OTC, use of tobacco or recreational drugs. He reports social ETOH, no more than 4 -5 mixed drinks per week, currently is a student at a local university and lives with his parents and sister. He thinks he is allergic to PCN, he had a rash as a child. He denies previous surgery.
Case A • Physical Examination: • BP 120/80 HR 70 T 98. 2 F Ht 6’ 0” Ht 175# Resp 16 – (BMI 23. 7) • Gen: Well dressed/groomed, polite, cooperative, friendly, in no acute distress. • Skin: without jaundice • HEENT without schleral icterus, conjunctival injection, D/C. • Chest: S 1 S 2 without MRG, CTA • Abdomen: Without surgical scars, striae, B/S X 4, soft nontender without masses. • Without CVA tenderness • Without gross neurologic defects
Case A • GU: circumcised, meatal erythema with a clear urethral discharge. There are no penile lesions, ulcers, rash or inguinal adenopathy. There is no testicular mass, edema or tenderness. • Rectal tone is intact, symmetric. Prostate is smooth, non tender and 2. 5 cm with a palpable sulcus. No protrusion into rectum, masses or area of induration. Rectal exam is unremarkable with i. FOB negative stool.
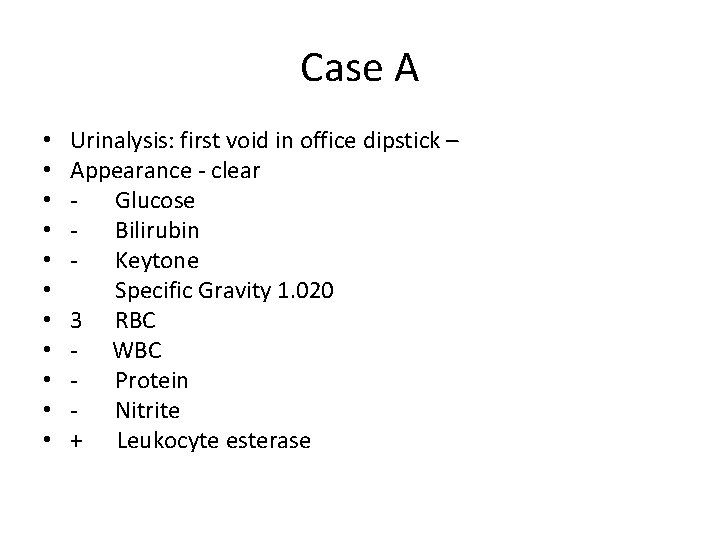
Case A • • • Urinalysis: first void in office dipstick – Appearance - clear - Glucose - Bilirubin - Keytone Specific Gravity 1. 020 3 RBC - WBC - Protein - Nitrite + Leukocyte esterase
Case A Differential Diagnosis • • Chlamydia urethritis Gonorrhea infection Lymphogranuloma venereum Acute prostatitis
Acute prostatitis • Most frequent urologic diagnosis in men <50 and 3 rd most common urologic dx. In men >50 • Commonly caused by E coli • Common symptoms are – Dysuria – urinary frequency – perineal discomfort • May also cause – Referred pain to genitalia, perineum, low back or suprapubic areas
Acute Prostatitis • Hx: UTI • PE: – Fever/chills, malaise – Tender prostate
Lymphogranuloma venereum • C trachomatis L 1, L 2, L 3 infection • Endemic in tropics but rare in developed regions – Primary manifestation is a painless penile or vulvar inflammation and ulceration, often unnoticed by patient • Dysuria is not a typical complaint – 5 -21 day incubation – Initial vesicular or ulcerative lesion on external genitalia may go unnoticed – Inguinal buboes, usually bilateral, appear 1 – 4 weeks post exposure which tend to fuse, soften, and break down to form draining sinuses

Gonorrhea Infection • Classically presents as an acute urethral D/C following unprotected sex with a new partner – Risk factors are: • New sex partner • Multiple sex partners • <25 YOA • Common – 3 -4 million clinic visits yearly in the USA (second most common reportable disease in the USA, after Chlamydia) • Highest incidence rates in: – – Women 15 -19 and men 20 -24 YOA Blacks 18. 7 X> whites Native American/Alaskan Native 4. 6> whites Hispanic 2. 2 X > whites
Chlamydia Urethritis • Similar presentation as gonorrhea • Chlamydia trachomatis is the most common reportable disease in the US – 1, 307, 893 reported to CDC in 2010, up 5. 1% from 2009 – Women 2. 5 X> men – Similar age group distribution as gonorrhea – Blacks 8 X>whites – Native American/Alaskan Native 4. 3 X> whites – Hispanics 2. 7 X> whites
Chlamydia Urethritis • Urethritis is an inflammatory condition – GU (gonoccocal urethritis) or NGU (nongonoccocal urthritis) – Unprotected vaginal, and insertive oral sex have all been associated – Can be transmitted to neonates • NGU – – 30% - 50% C trachomatis 10% - 40% Ureaplasma urealyticum 15% Mycoplasma genitalium (no test available) Rarely: Trichomonas vaginalis, HSV, Adenovirus, other bacteria
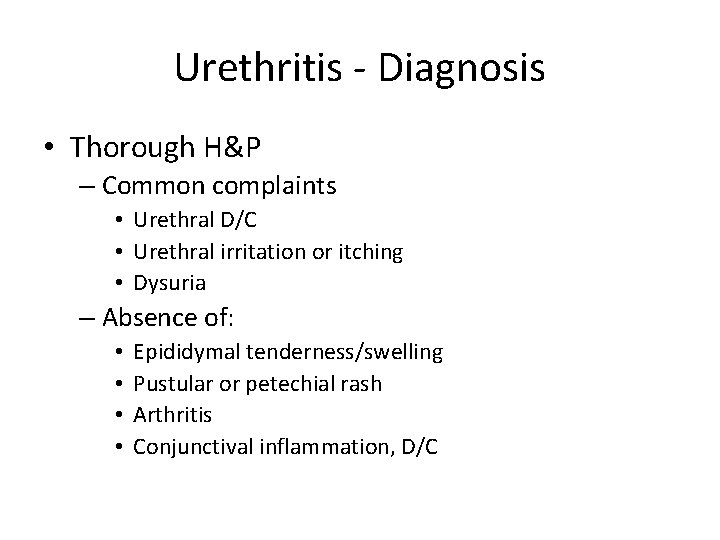
Urethritis - Diagnosis • Thorough H&P – Common complaints • Urethral D/C • Urethral irritation or itching • Dysuria – Absence of: • • Epididymal tenderness/swelling Pustular or petechial rash Arthritis Conjunctival inflammation, D/C
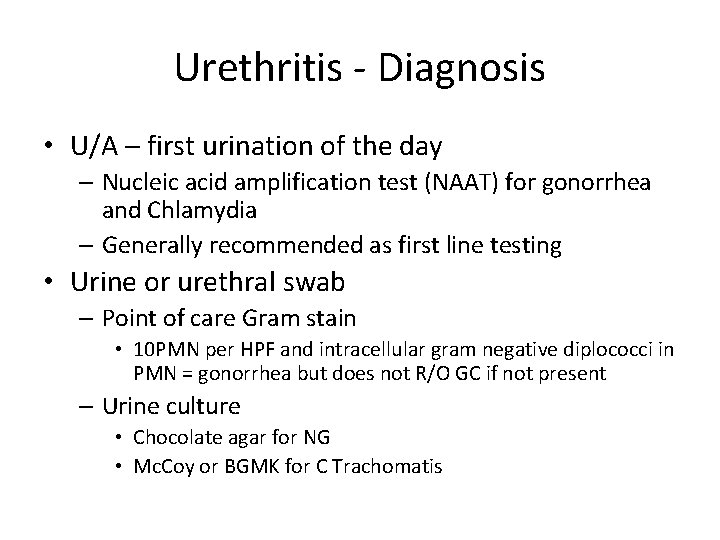
Urethritis - Diagnosis • U/A – first urination of the day – Nucleic acid amplification test (NAAT) for gonorrhea and Chlamydia – Generally recommended as first line testing • Urine or urethral swab – Point of care Gram stain • 10 PMN per HPF and intracellular gram negative diplococci in PMN = gonorrhea but does not R/O GC if not present – Urine culture • Chocolate agar for NG • Mc. Coy or BGMK for C Trachomatis
Urethritis – other tests • HIV, Hepatitis panel • VDRL – STI’s often travel together

Urethritis - treatment • Goal is to alleviate acute symptoms and to prevent transmission • Presumptive treatment for both GU and NGU should be given pending test results • Patients should abstain form sex during treatment
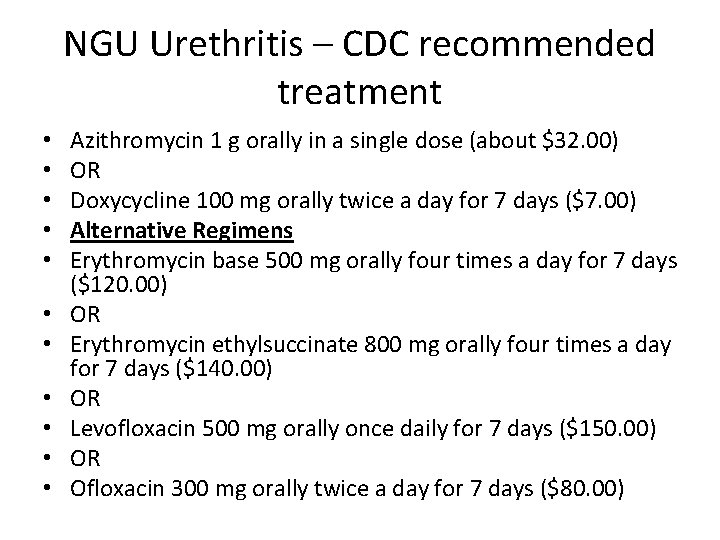
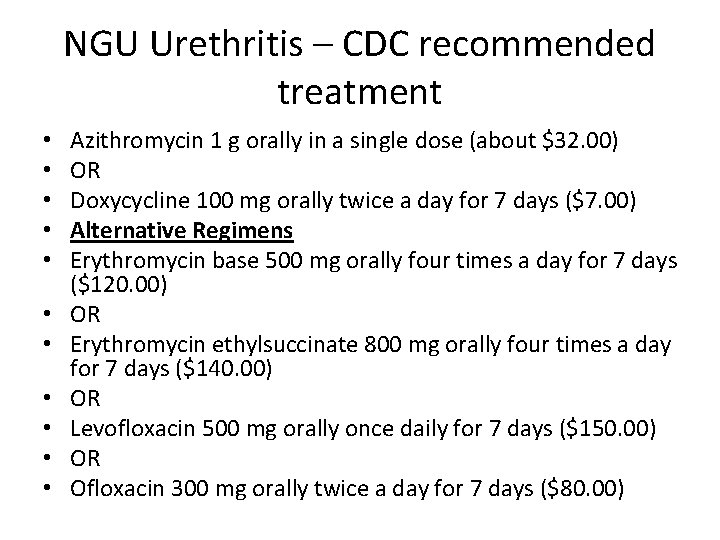
NGU Urethritis – CDC recommended treatment • • • Azithromycin 1 g orally in a single dose (about $32. 00) OR Doxycycline 100 mg orally twice a day for 7 days ($7. 00) Alternative Regimens Erythromycin base 500 mg orally four times a day for 7 days ($120. 00) OR Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days ($140. 00) OR Levofloxacin 500 mg orally once daily for 7 days ($150. 00) OR Ofloxacin 300 mg orally twice a day for 7 days ($80. 00)
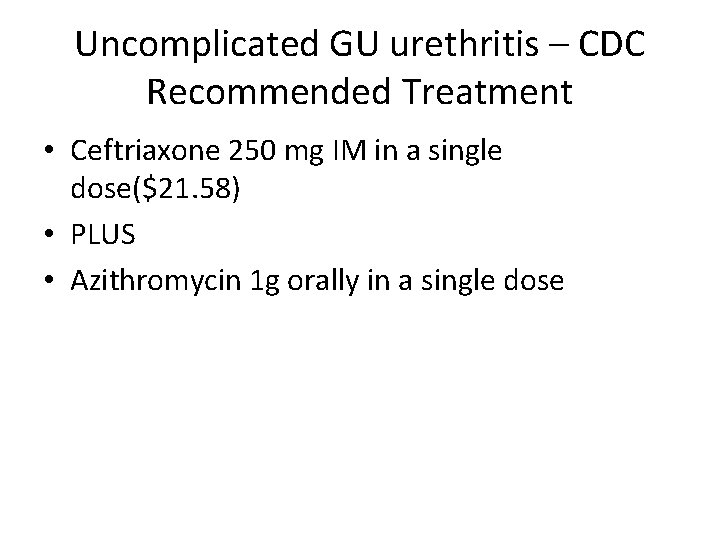
Uncomplicated GU urethritis – CDC Recommended Treatment • Ceftriaxone 250 mg IM in a single dose($21. 58) • PLUS • Azithromycin 1 g orally in a single dose
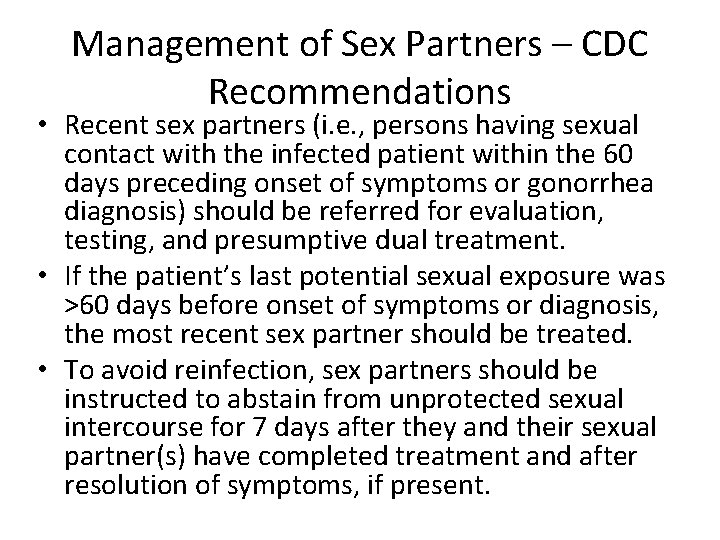
Management of Sex Partners – CDC Recommendations • Recent sex partners (i. e. , persons having sexual contact with the infected patient within the 60 days preceding onset of symptoms or gonorrhea diagnosis) should be referred for evaluation, testing, and presumptive dual treatment. • If the patient’s last potential sexual exposure was >60 days before onset of symptoms or diagnosis, the most recent sex partner should be treated. • To avoid reinfection, sex partners should be instructed to abstain from unprotected sexual intercourse for 7 days after they and their sexual partner(s) have completed treatment and after resolution of symptoms, if present.
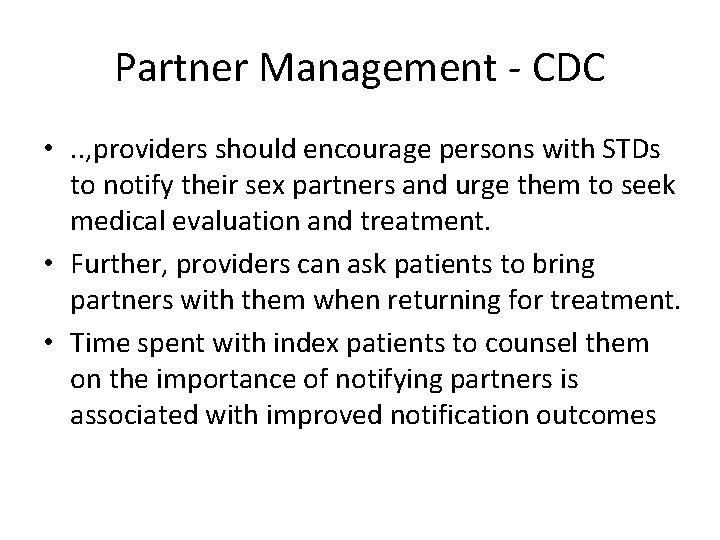
Partner Management - CDC • . . , providers should encourage persons with STDs to notify their sex partners and urge them to seek medical evaluation and treatment. • Further, providers can ask patients to bring partners with them when returning for treatment. • Time spent with index patients to counsel them on the importance of notifying partners is associated with improved notification outcomes
Partner Management - CDC • When patients diagnosed with chlamydia or gonorrhea indicate that their partners are unlikely to seek evaluation and treatment, providers can offer patient-delivered partner therapy (PDPT), a form of expedited partner therapy (EPT) in which partners of infected persons are treated without previous medical evaluation or prevention counseling. • Because EPT might be prohibited in some states and is the topic of ongoing legislation in others, providers should visit www. cdc. gov/std/ept to obtain updated information for their individual jurisdiction. • Any medication or prescription provided for PDPT should be accompanied by treatment instructions, appropriate warnings about taking medications (if the partner is pregnant or has an allergy to the medication), general health counseling, and a statement advising that partners seek personal medical evaluation, particularly women with symptoms of STDs or PID.

Urethritis – CDC guidelines for reporting • Syphilis, gonorrhea, chlamydia, chancroid, HIV infection, and AIDS are reportable diseases in every state.
Case B • A 71 -year-old man complains of a one month history of awakening at night about 3 times to urinate, having to urinate about every 3 hours, feeling as if he will have an accident if he doesn’t get to the bathroom quickly, difficulty starting and maintaining his urine stream and he has to push or strain more than half the time. He always feels like his bladder is not empty after urinating and he states he has dribbling and his urine stream may stop and then start again. He reports he tried taking saw palmetto without relief. • He denies painful urination, penile D/C, blood in his urine, fever, chills, joint pain, conjunctivitis, weight loss or gain, abdominal or back pain.
Case B • The patient reports he was diagnosed with Stage 1 HTN and elevated cholesterol 10 years ago but only takes lipitor • He denies history of diabetes mellitus, renal disease, kidney stones, or neurologic disease, or history of STI. The patient denies using any decongestants or other meds that can inhibit urination. • He is married and monogamous and sexually active 1/week with wife. They have 1 martini per day, he denies using recreational drugs or tobacco. There is a cat in the home. Recent travel to Europe 3 months ago without any health problems. 3 adult children are healthy. His parents died of “old age”.
Case B • BP 150/95 HR 70 T 98. 2 R 16 Ht 6’ 0” Wt 180# (BMI 24. 4) • Gen: Well dressed/groomed/nourished, polite, cooperative, friendly, in no acute distress. • HEENT without conjunctival injection or D/C • Skin without jaundice • Chest S 1 S 2 without MRG. CTA • Abdomen: without scars, striae, masses, rashes or lesions. B/S X 4 without bruits, soft, mild suprapubic tenderness without masses, without CVA tenderness. • Neuro: There are no neurologic deficits in the lower extremities. • GU: Uncircumcised without penile D. /C, scrotal lesions, edema, tenderness • Rectal exam: Rectal tone is intact. Prostate is 4 + diffusely enlarged with no palpable masses, hardness or tenderness; Stool is guaiac negative • U/A dipstick in office WNL
Case B – Differential Diagnosis • • Prostate CA Prostatitis BPH Elevated BP
Prostate CA • Most common noncutaneous cancer in American men and the second leading cause of cancer-related death. • Over 241, 000 new cases diagnosed each year and around 28, 000 deaths. • However, more than 40% of men over 50 YOA have prostate carcinoma few are associated with regional or distant disease. • Incidence increases with age • Blacks, family history of prostate CA and high dietary fat increase risk • Current Medical Diagnosis and Treatment

Prostate CA • Most prostate cancers are associated with a palpably normal prostate gland are detected solely on the basis of elevated PSA. • Urinary retention is a rare presentation but large or locally extensive cancers can cause obstructive symptoms. • Lymph node metastasis can lead to lower extremity lymphedema
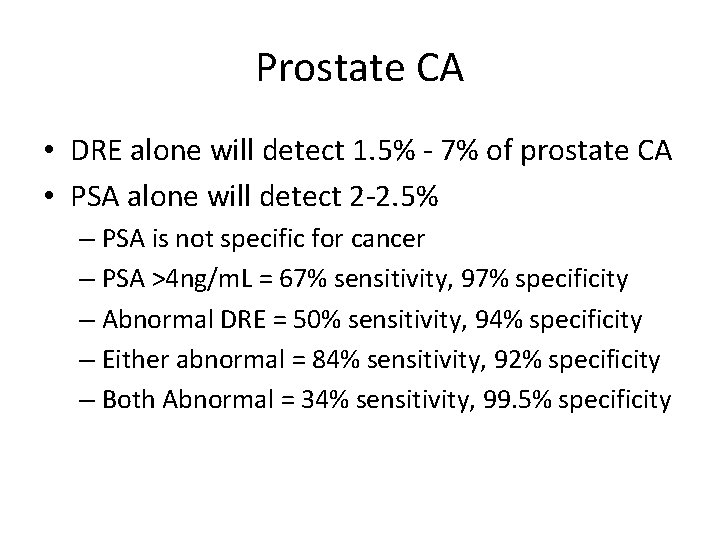
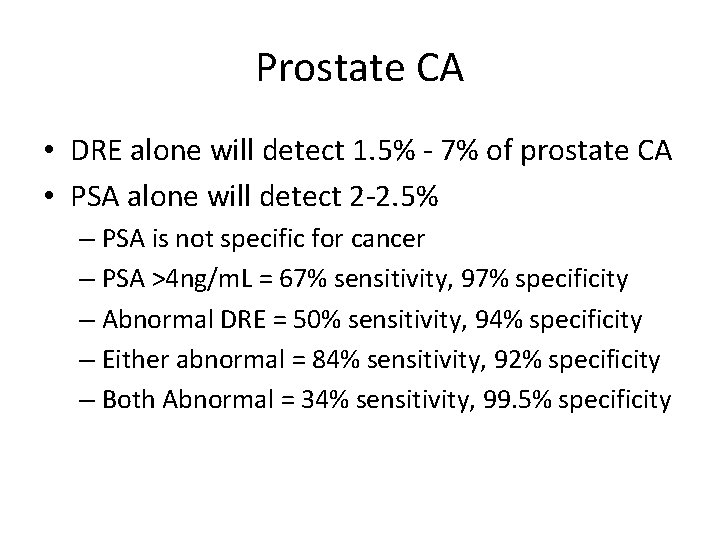
Prostate CA • DRE alone will detect 1. 5% - 7% of prostate CA • PSA alone will detect 2 -2. 5% – PSA is not specific for cancer – PSA >4 ng/m. L = 67% sensitivity, 97% specificity – Abnormal DRE = 50% sensitivity, 94% specificity – Either abnormal = 84% sensitivity, 92% specificity – Both Abnormal = 34% sensitivity, 99. 5% specificity
Prostatitis • Discussed previously
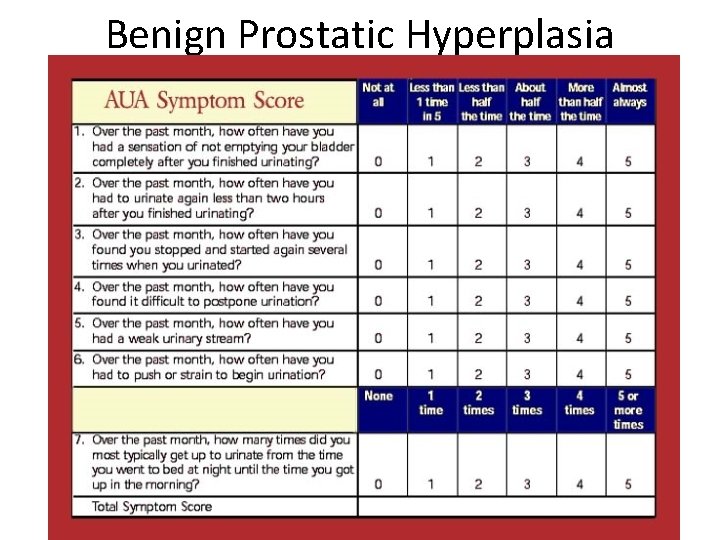
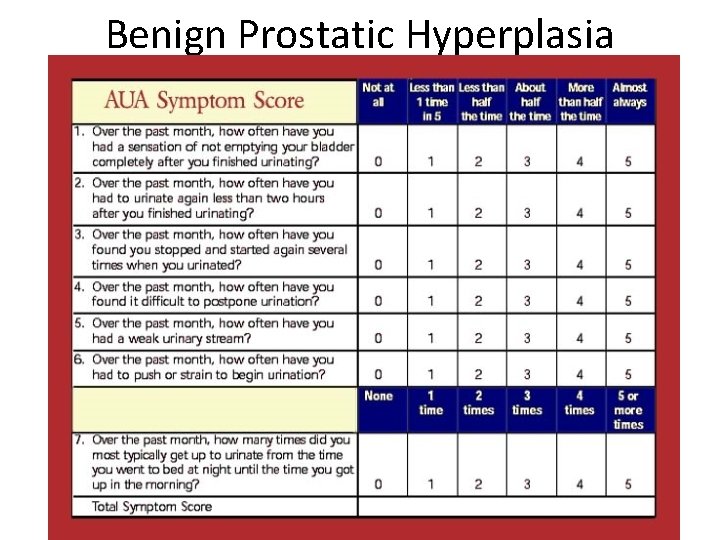
Benign Prostatic Hyperplasia
BPH • Symptoms: – Obstructive: • • • Hesitancy Decreased force and caliber of stream Sensation of incomplete bladder emptying Double voiding (again within 2 hours) Straining to urinate Postvoid dribbling – Irritative: • Urgency • Frequency • Nocturia
BPH • PE: – DRE • Size • Consistency – Neither correlates with severity of symptoms – Smooth, firm, elastic, non-tender enlargement – Focused LE neuro exam should be documented
BPH – lab tests • U/A to exclude infection or hematuria • PSA optional – Consider if life expectancy is >10 years
BPH - treatment • AUA score 0 -7 – Watchful waiting • Men with moderate or severe symptoms can also be observed if they so chose. – The optimal interval for follow-up is not defined, nor are the specific end points for intervention
BPH – Medical Therapy • α-Blockers – Terazosin is long acting and has been shown to be more effective with less side effects (orthostatic hypotension, dizziness, tiredness, retrograde ejaculation, rhinitis, headache) – Alpha 1 blocker is not a first line drug for HTN if patient has CV risks. In this case it could be appropriate, but the alpha 1 blockers are not considered first line as there is a higher mortality – $4. 00 generic program • Epocrates • Α 1 a-blockers result in less systemic side effects – Tamsulosin • Available as generic • 0. 4 mg (30 each): $139. 23 – Epocrates
BPH – Medical Therapy • 5α-Reductase inhibitors (decreased libido, decrease in volume of ejaculate, erectile dysfunction) – Finasteride (decreases prostate size) – 6 months therapy for maximum results • $4. 00 generic program – Dutasteride equally effective, available as generic but not on $4. 00 program
BPH –Medical therapy • Tadalafil (Cialis) – Improvement in urinary symptoms within 2 – 4 weeks – 5 mg (10 each): $57. 59 • Epocrates
BPH – surgical treatment • • Transurethral resection of the prostate (TURP) Transurethral incision of the prostate (TUIP) Open simple prostatectomy Laser therapy – Transurethral laser-induced prostatectomy (TULIP) – Photovaporization of the prostate (PVP) • Advantages of laser therapy: – – Minimal blood loss Rare occurrence of transurethral resection syndrome Ability to treat patients on anticoag therapy Outpatient surgery • Disadvantages: – Lack of tissue for path examination – Longer post-op catheterization time – Expense
BPH –Surgical Treatment • Transurethral needle ablation of the prostate (TUNA) – Similar improvement results as TURP • Transurethral electrovaporization of the prostate – Takes longer than TURP • Hyperthermia – Microwave hyperthermia
BPH – When to Refer • Progression to urinary retention • Patient dissatisfaction with medical therapy • Need for surgical intervention or further evaluation (cystoscopy)
Elevated BP • Serial BP away from the clinic, keep a log, return in 7 days. • CMP, Lipids, CBC, TSH – Have the patient return the following morning for fasting lab studies – Review at F/U in one week • Fundoscopic exam, carotid and renal bruits
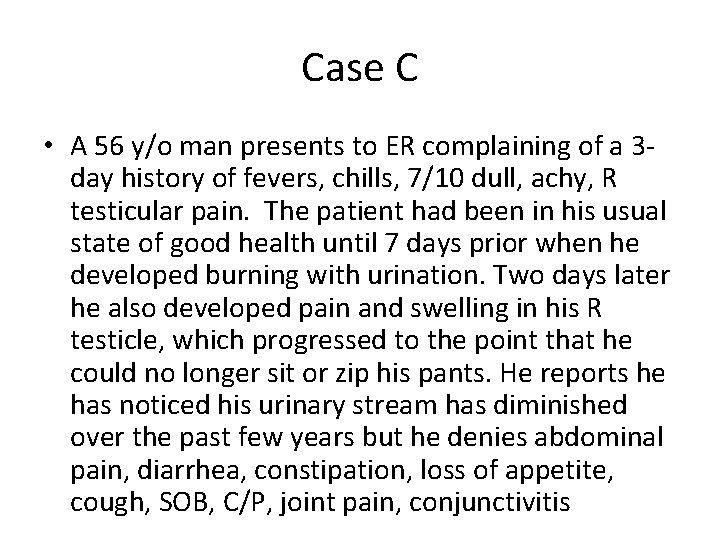
Case C • A 56 y/o man presents to ER complaining of a 3 day history of fevers, chills, 7/10 dull, achy, R testicular pain. The patient had been in his usual state of good health until 7 days prior when he developed burning with urination. Two days later he also developed pain and swelling in his R testicle, which progressed to the point that he could no longer sit or zip his pants. He reports he has noticed his urinary stream has diminished over the past few years but he denies abdominal pain, diarrhea, constipation, loss of appetite, cough, SOB, C/P, joint pain, conjunctivitis
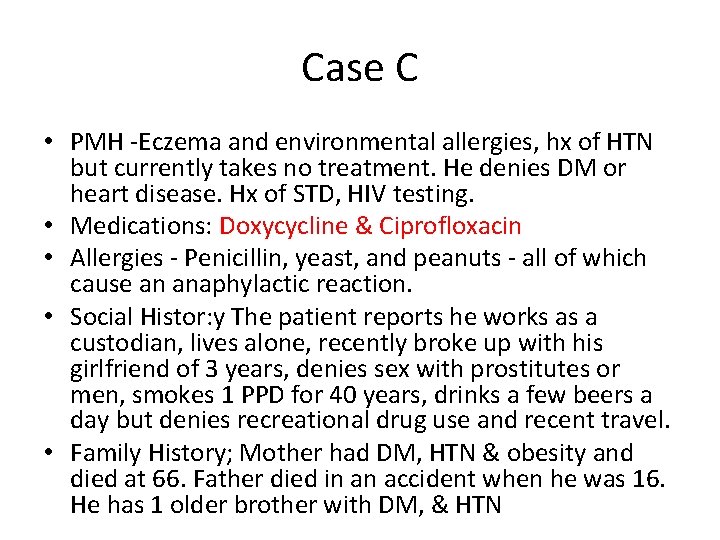
Case C • PMH -Eczema and environmental allergies, hx of HTN but currently takes no treatment. He denies DM or heart disease. Hx of STD, HIV testing. • Medications: Doxycycline & Ciprofloxacin • Allergies - Penicillin, yeast, and peanuts - all of which cause an anaphylactic reaction. • Social Histor: y The patient reports he works as a custodian, lives alone, recently broke up with his girlfriend of 3 years, denies sex with prostitutes or men, smokes 1 PPD for 40 years, drinks a few beers a day but denies recreational drug use and recent travel. • Family History; Mother had DM, HTN & obesity and died at 66. Father died in an accident when he was 16. He has 1 older brother with DM, & HTN
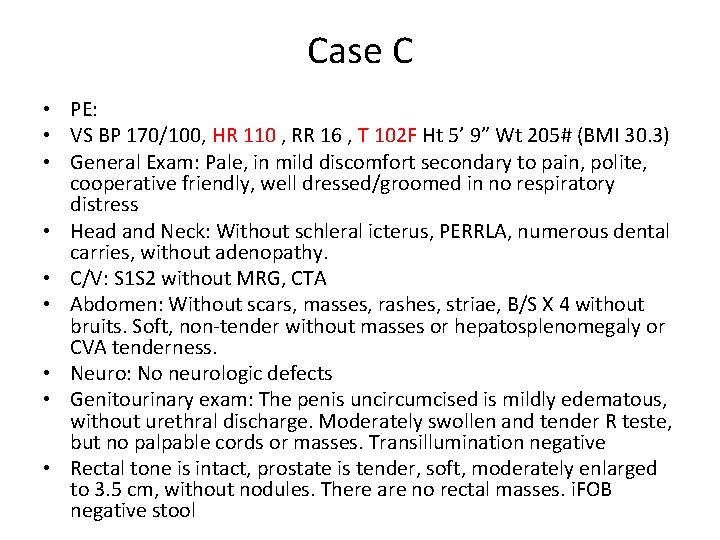
Case C • PE: • VS BP 170/100, HR 110 , RR 16 , T 102 F Ht 5’ 9” Wt 205# (BMI 30. 3) • General Exam: Pale, in mild discomfort secondary to pain, polite, cooperative friendly, well dressed/groomed in no respiratory distress • Head and Neck: Without schleral icterus, PERRLA, numerous dental carries, without adenopathy. • C/V: S 1 S 2 without MRG, CTA • Abdomen: Without scars, masses, rashes, striae, B/S X 4 without bruits. Soft, non-tender without masses or hepatosplenomegaly or CVA tenderness. • Neuro: No neurologic defects • Genitourinary exam: The penis uncircumcised is mildly edematous, without urethral discharge. Moderately swollen and tender R teste, but no palpable cords or masses. Transillumination negative • Rectal tone is intact, prostate is tender, soft, moderately enlarged to 3. 5 cm, without nodules. There are no rectal masses. i. FOB negative stool
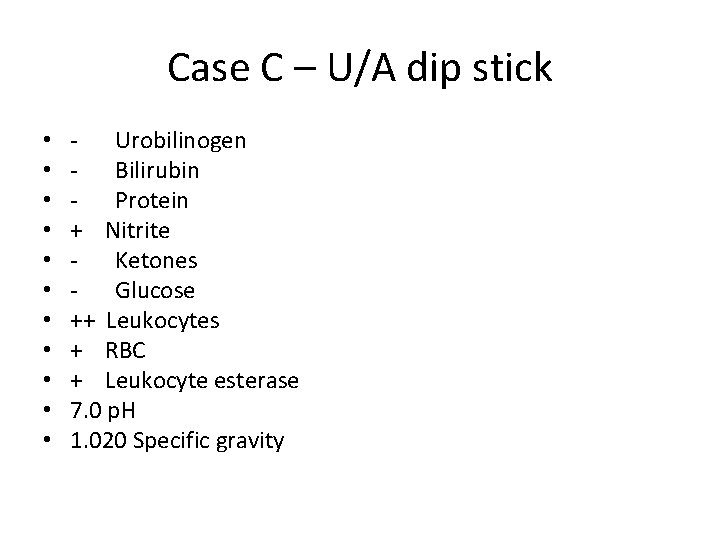
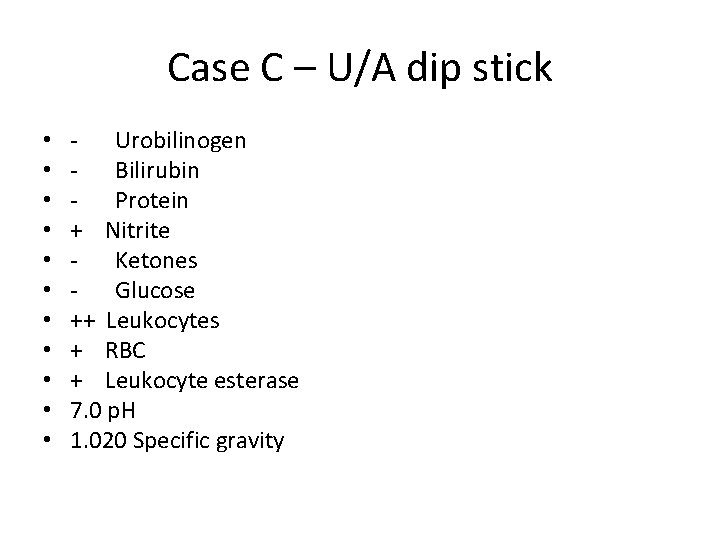
Case C – U/A dip stick • • • - Urobilinogen - Bilirubin - Protein + Nitrite - Ketones - Glucose ++ Leukocytes + RBC + Leukocyte esterase 7. 0 p. H 1. 020 Specific gravity
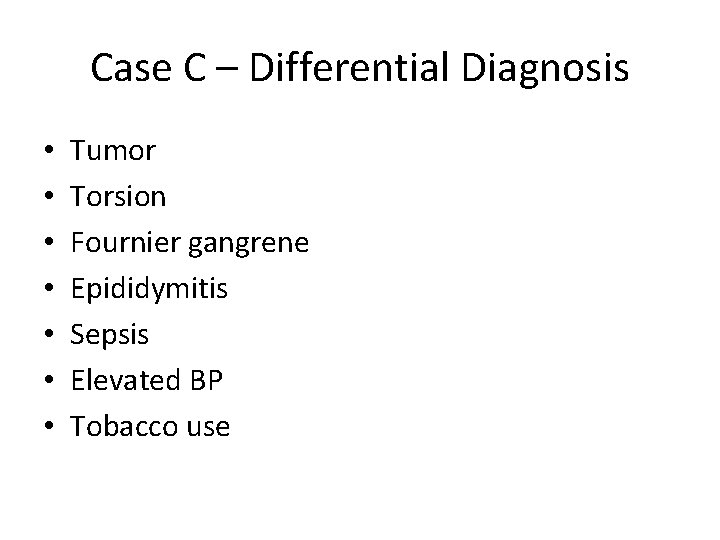
Case C – Differential Diagnosis • • Tumor Torsion Fournier gangrene Epididymitis Sepsis Elevated BP Tobacco use
Tumor • Usually painless, unilateral – U/A will be negative – Normal PE of epididymis – TSE is considered a “D” category at any age by the USPSTF
Torsion • Usually prepubertal • Acute onset of symptoms • Negative U/A
Fournier gangrene • Rare but life threatening • DM and ETOH abuse (immune compromised) are most at risk but anyone is susceptible • Mixed infection of aerobic and anaerobic bacteria • Nidus: – GI tract 30 -50% – GU 20 – 40% – Cutaneous 20% • Very rapid progression causing multiple organ failure and death • Antibiotic and aggressive is the standarddebridement treatment – Mortality rate is high
Epididymitis - History • Most cases are infectious – Sexually transmitted • <40 • With associated urethritis • C trachomatis or N gonorrhea – Non-sexually transmitted • >40 • Associated with UTI, obstructive urinary disease and prostatitis • Gram - rods
Epididymitis - PE • Scrotal tenderness and swelling • May have pain radiating along the spermatic cord to the flank • Early the epididymis may be distinguishable from the testis but later they may appear as one enlarged, tender mass • Prehn’s sign (elevation of the testicle relieves pain) is not reliable for differentiating between epididymitis and testicular torsion (loss of cremasteric reflex is more accurate)
Epididymitits - Tests • U/A – Pyuria, bacturia, hematuria • Urine culture to identify offending organism • Scrotal U/S
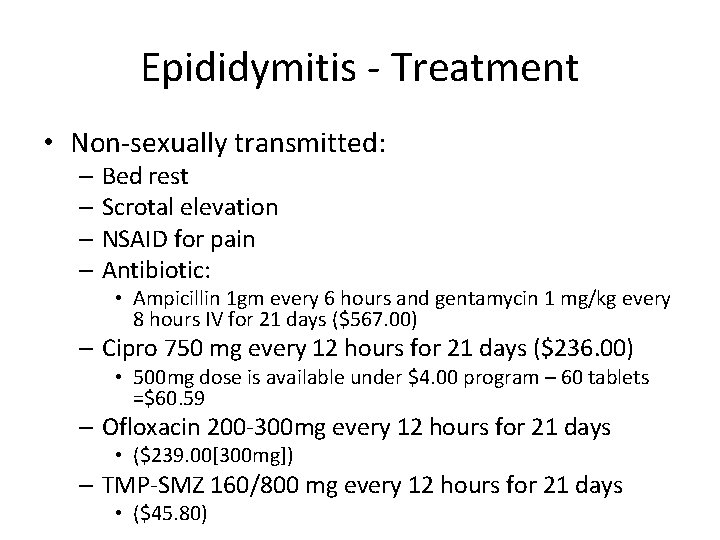
Epididymitis - Treatment • Non-sexually transmitted: – Bed rest – Scrotal elevation – NSAID for pain – Antibiotic: • Ampicillin 1 gm every 6 hours and gentamycin 1 mg/kg every 8 hours IV for 21 days ($567. 00) – Cipro 750 mg every 12 hours for 21 days ($236. 00) • 500 mg dose is available under $4. 00 program – 60 tablets =$60. 59 – Ofloxacin 200 -300 mg every 12 hours for 21 days • ($239. 00[300 mg]) – TMP-SMZ 160/800 mg every 12 hours for 21 days • ($45. 80)
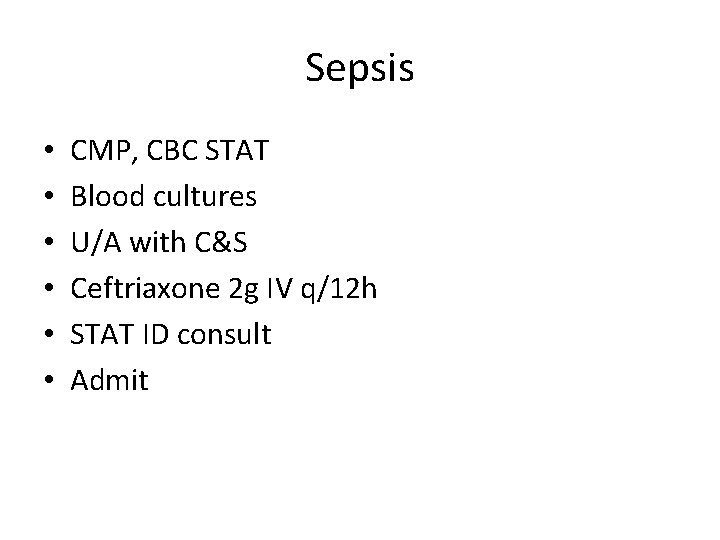
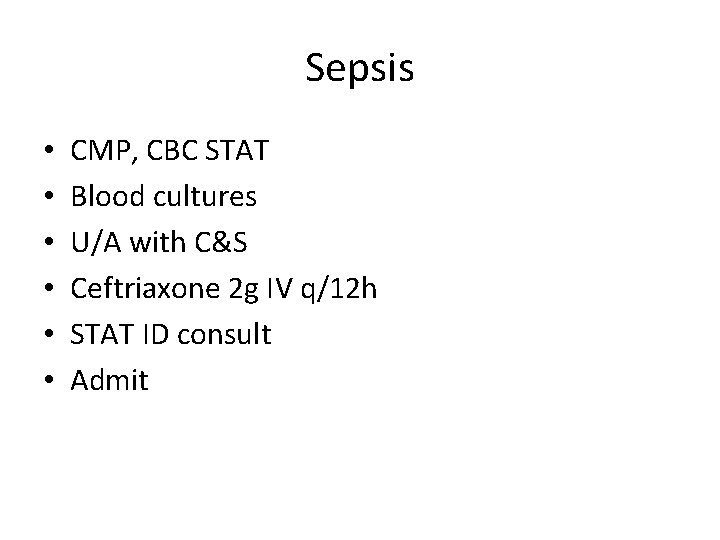
Sepsis • • • CMP, CBC STAT Blood cultures U/A with C&S Ceftriaxone 2 g IV q/12 h STAT ID consult Admit